Abstract
Background
Circulating tumor cells (CTCs) have been proposed as a marker for predicting the prognosis of cancer. However, the prognostic value of CTCs detected with the CellSearch System in patients with gastric cancer (GC) remains controversial. We performed a meta-analysis of available studies to investigate this topic.
Methods
Two authors systematically searched the studies independently in PubMed, Science Citation Index, Cochrane Database, Embase, and the references in relevant studies (up to September 2017) using keywords. Our meta-analysis was performed in Stata software, version 12.0 (2011; Stata Corp, College Station, TX, USA), with the risk ratio (RR), hazard ratio (HR), and 95% CI as the effect measures. Subgroup analyses and meta-regression were also conducted.
Results
Seven studies (including eight sets of data) containing 579 patients with GC from four countries were included in this meta-analysis. The pooled results showed CTC-positive status detected by the CellSearch System was significantly associated with poor overall survival (HR =2.09, 95% CI [1.71, 2.55], P<0.001, I2=31.5%) and progression-free survival (HR =2.11, 95% CI [1.25, 3.57], P=0.005, I2=75.6%) of patients with GC, regardless of sampling time. The disease control rate of CTC-positive group was lower than that of CTC-negative group for both baseline and intra-therapy, although no statistical difference existed at both sampling time points (baseline: 69.5% versus 81.8%, RR=0.79, 95% CI [0.54, 1.16], P=0.23, I2=68.0%; intra-therapy: 50.0% versus 85.9%, RR=0.24, 95% CI [0.02, 3.13], P=0.28, I2=87.4%).
Conclusion
Our meta-analysis demonstrated that CTCs detected with the CellSearch System from the peripheral blood had significant prognostic value and might predict poor response to chemotherapy for patients with GC.
Keywords: circulating tumor cells, gastric cancer, chemotherapy, prognosis, meta-analysis
Introduction
Gastric cancer (GC) ranks the fourth most common cancer and the third leading cause of cancer-associated mortality worldwide, with over 951,600 new cases and 723,100 deaths estimated to have occurred (GLOBOCAN 2012).1 Although recent diagnosis and treatment advances have improved the clinical outcome of GC patients, the 5-year survival rate is still <30%.2 Also, recurrence or metastasis after curative resection is the main reason for GC-related deaths.3 Unfortunately, the lack of effective predictors prevents doctors from identifying recurrence and metastasis timely during therapy and review, which leads to missing the best time of intervention and thus affects the therapeutic effect. Nowadays, circulating tumor cells (CTCs), which shed from the primary tumor mass and are circulated in the blood, have gradually been accepted as a new and efficient prognostic marker to evaluate the relapse and metastasis, monitor the therapeutic responsiveness, and predict the prognosis, due to their advantage of earlier and more reproducible indication of disease status than that of current imaging methods.4
Numerous studies have shown that the presence of CTCs in the peripheral blood (PB) is a poor prognostic indicator of overall survival (OS) and progression-free survival (PFS) in patients with GC.5–8 In those studies, the methods of detecting CTCs were predominantly immunocytochemistry (ICC)5,6 and reverse transcription-polymerase chain reaction (RT-PCR).7,8 However, these detection methods vary across laboratories and the optimal cutoff value for CTCs has not yet been confirmed. Currently, the CellSearch System (Veridex, Raritan, NJ, USA), a semi-automated immunological assay for enumeration of CTCs based on the epithelial cell adhesion molecule, is the first and only standardized system approved by the US Food and Drug Administration for applying to detect CTCs in patients with breast, prostate, and colorectal cancer.9–11 Moreover, the prognostic significance of CTCs detected with CellSearch System in patients with breast, prostate, and colorectal cancer had been quantitatively and comprehensively summarized by previous meta-analyses.12–14 With regard to GC, although there were many studies designed to find out the relationship between CTCs detected with the CellSearch System and prognosis, the lack of statistical power together with their different study design and results limited its individual clinical value and prognostic effect. Therefore, a combined analysis of available studies on this topic is required to provide a more precise estimate of the prognostic relevance of CTC detection in the PB of patients with GC.
The aim of our study was to conduct a meta-analysis to quantitatively summarize the clinical evidence and prognostic value of CTCs detected with the standardized CellSearch System in GC patients.
Methods
Data sources and search strategy
Our meta-analysis was conducted according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement.15 Two authors (CG Yang and K Zou) systematically searched the literature independently from the following databases: PubMed, MEDLINE, EMBASE, Science Citation Index, and Cochrane Library (up to September 2017). The main keywords and MeSH terms used were “circulating tumor cells”, “disseminated tumor cells”, “isolated tumor cells”, “occult tumor cells”, “gastric cancer”, “stomach carcinoma”, “gastrointestinal cancer”, “digestive cancer”, and “CellSearch System”. An additional search through Google Scholar and the clinical trial registration website was conducted to obtain information identifying other potentially relevant publications. The reference lists of the relevant studies (review studies and included studies) were also checked for potentially relevant articles. Discrepancies were resolved by the third author (ZW Yuan).
Inclusion and exclusion criteria
To be included in the meta-analysis, studies had to match the following criteria: 1) used only the CellSearch System to explore the prognostic role of CTC detection in GC patients; 2) at least one of the outcome measures of interest was reported in the article or could be calculated from the published data; and 3) samples being collected from the PB. When multiple studies were published with the same patient population, we included the most informative study.
Studies were excluded from the meta-analysis if 1) the outcomes of interest were not reported or could not be calculated from the original published data; 2) the samples came from the lymph nodes, bone marrow, mesenteric/portal blood, or peritoneal cavity; 3) studies were based on overlapping patients; and 4) enough data was not available after contacting the original author or magazine.
Data extraction
Two investigators (CG Yang and K Zou) independently extracted the following data from each eligible study: the first author’s name, year of publication, country of patients, characteristics of the study population (ie, number, sex, age), sampling time, cutoff value, positive rate of CTC detection, and prognostic outcomes (OS and PFS), hazard ratio (HR), and disease control rate (DCR) of chemotherapy. According to the Response Evaluation Criteria In Solid Tumors guideline (complete response [CR], partial response [PR], stable disease [SD], and progressive disease [PD]),16 DCR=(CR+PR+SD)/(CR+PR+SD+PD). For the studies with multiple arms (ie, training set and validation set), each of them was considered as an independent data set. For the studies with multiple time points (ie, baseline and intra-therapy), we used data from “baseline” samples prior to the data from “intra-therapy” samples because these data were usually dependent. If the HR and its 95% CI were not reported directly in the original article, these values were calculated from available data using the methods reported by Tierney et al.17 Disagreements between two reviewers were resolved by discussion or consultation.
Quality assessment
Two reviewers (CG Yang and K Zou) used the Newcastle–Ottawa scale, which was recommended by the Cochrane Library for nonrandom controlled studies, to assess the quality of included studies independently.18 Any disagreements on quality assessment were resolved via comprehensive discussion. Based on the Newcastle–Ottawa scale criterion, a score of 5–9 means high quality, whereas a score of 1–4 means low quality.
Statistical analysis
Stata 12.0 software (Stata Corp, College Station, TX, USA) was used for all analyses in our meta-analysis. The estimated HR was used to evaluate the prognostic indicators (PFS and OS) as demonstrated by Parmar et al,19 and HR >1 denoted more deaths or progression in CTCs-positive arm. The estimated risk ratio (RR) was used to evaluate the DCR. All statistical values were reported with 95% CIs, and the two-sided P-value threshold for statistical significance was set at 0.05. Heterogeneity among the studies was calculated with the Q test and I2 statistic, and the I2 value indicated the degree of heterogeneity.20 A P-value <0.1 for the Q statistic and/or I2>50% were considered significant heterogeneity, and a random-effects model was used. Otherwise, a fixed-effects model was used.21 Furthermore, subgroup analyses were conducted according to the difference in the data retrieved, such as year of publication, country of patients, sampling time, cutoff value, positive rate of CTC detection, and quality of included studies. Meta-regression was performed to explore the potential variables that contributed heterogeneity. Additionally, Galbraith plot was used to further explore which study would contribute substantial heterogeneity to our meta-analysis. Additionally, potential publication bias was detected by Begg’s and Egger’s test.22 P<0.05 was considered to be significant publication bias.
Results
Baseline characteristics of the included studies
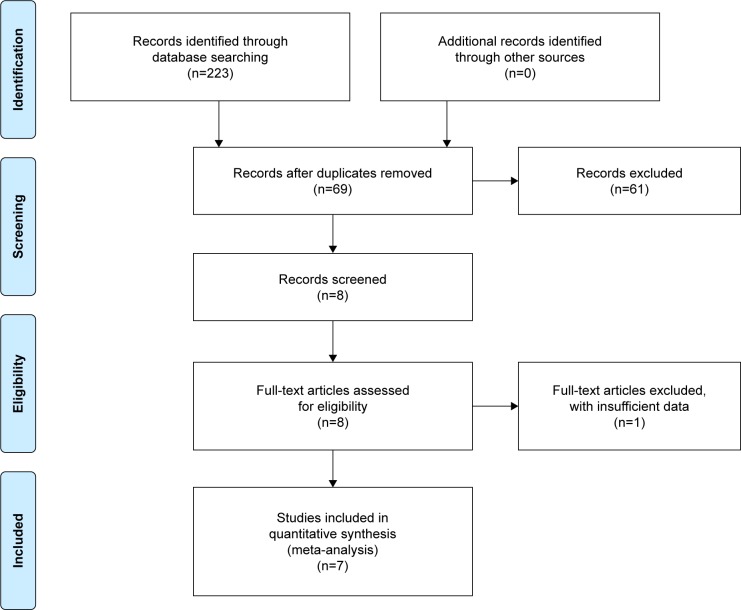
According to the above-mentioned retrieval method, a total of 69 studies were initially identified during a systematic literature search. By screening the titles and abstracts, 61 studies were excluded and 8 potential studies were retrieved. One study was then excluded after full-text articles, as it had insufficient data. Finally, seven studies were eligible for our meta-analysis (Figure 1).
Figure 1.
Flow chart of study selection.
Note: Copyright ©2009. Adapted from Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.36
Abbreviation: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses.
Seven eligible studies, including eight sets of data, contained 579 patients with GC.23–29 These studies came from four countries (China, Japan, Korea, and UK) and were published between 2008 and 2016. According to the sampling time points, four studies only assessed CTCs at baseline,25–28 one study only assessed CTCs at intra-therapy,23 and two studies assessed CTCs combined at both time points.24,29 HRs for OS and PFS were available in eight sets of data from seven studies23–29 and six sets of data from six studies,24–29 respectively. Among all the included studies, two studies were of low quality and the other five studies were of high quality. The baseline characteristics and results of quality assessment of included studies are summarized in Table 1.
Table 1.
Baseline characteristics of included studies
| Reference | Year | Country | Number (male/female) | Age (years)a | Tumor stageb | Sampling time | Cutoff | Positive rate, n (%) | End point | Treatment regimens | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hiraiwa et al23 | 2008 | Japan | 27 (NR) | NR | IV | Intra-therapy | ≥2/7.5 mL | 15 (55.6) | OS | Chemotherapy | Low |
| Matsusaka et al29 | 2010 | Japan | 52 (44/8) | 62 (24–78) | IV | Baseline | ≥4/7.5 mL | 17 (32.7) | OS, PFS | Chemotherapy | High |
| 51 (NR) | NR | Intra-therapy (2 weeks) | ≥4/7.5 mL | 7 (17.3) | OS, PFS | ||||||
| 48 (NR) | NR | Intra-therapy (4 weeks) | ≥4/7.5 mL | 9 (18.8) | OS, PFS | ||||||
| Uenosono et al28 (1) (training set) | 2013 | Japan | 148 (99/49) | NR | I–III | Baseline | ≥1/7.5 mL | 16 (10.8) | OS, PFS | Surgery | High |
| Uenosono et al28 (2) (validation set) | 2013 | Japan | 103 (NR) | NR | IV | Baseline | ≥1/7.5 mL | 62 (61.8) | OS | Chemotherapy | High |
| Sclafani et al27 | 2014 | UK | 18 (16/2) | 61 (38–78) | IV | Baseline | ≥2/7.5 mL | 8 (44.4) | OS, PFS | Chemotherapy | Low |
| Lee et al25 | 2015 | Korea | 95 (63/32) | 57 (36–85) | IV | Baseline | ≥5/7.5 mL | 27 (28.4) | OS, PFS | Chemotherapy | High |
| Okabe et al26 | 2015 | Japan | 136 (87/49) | NR | I–IV | Baseline | ≥1/7.5 mL | 25 (18.4) | OS, PFS | Surgery + chemotherapy | High |
| Li et al24 | 2016 | China | 136 (89/47) | 59 (25–80) | IV | Baseline | ≥3/7.5 mL | 57 (41.9) | OS, PFS | Chemotherapy | High |
| 106 (NR) | NR | Intra-therapy | ≥3/7.5 mL | 26 (24.5) | OS, PFS |
Notes:
Median (range).
The seventh edition of the AJCC cancer staging.
Abbreviations: AJCC, American Joint Committee on Cancer; NR, not reported; OS, overall survival; PFS, progression-free survival.
Impact of CTCs detection on prognostic outcomes (OS and PFS)
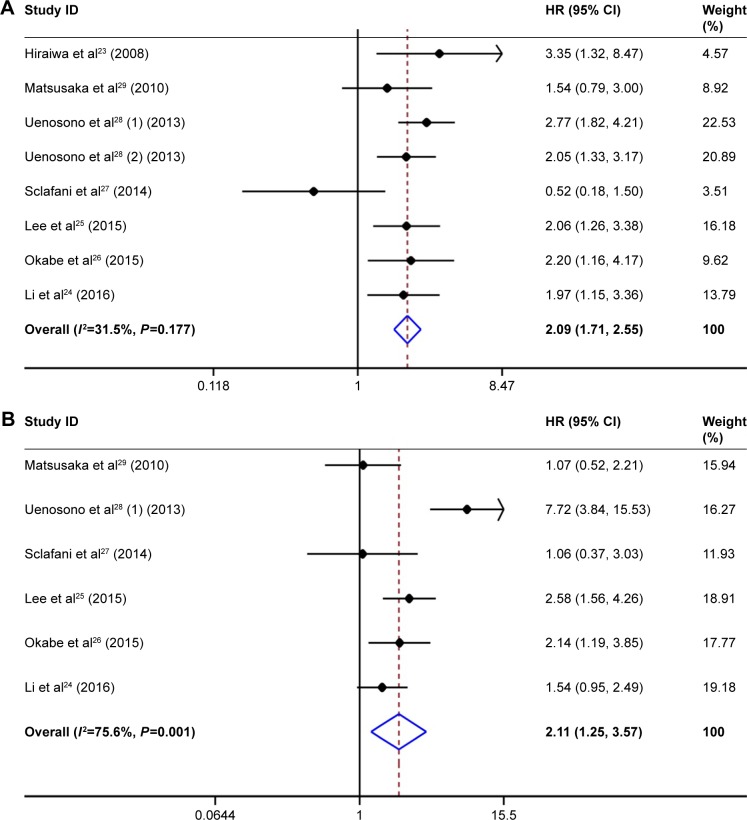
The pooled analysis showed that CTC-positive status detected by the CellSearch System in GC patients was associated with poor OS (HR =2.09, 95% CI [1.71, 2.55], P<0.001; Figure 2A), without any statistical significance in between-study heterogeneity (I2=31.5%, P=0.177). The HRs for PFS were available in six sets of data from six studies; the result of pooled analysis using the random-effects model showed that CTC positivity was also associated with poor PFS (HR =2.11, 95% CI [1.25, 3.57], P=0.005; Figure 2B), and between-study heterogeneity was obvious (I2=75.6%, P=0.001).
Figure 2.
Summary estimates of HR for OS and PFS of GC patients with CTC positivity.
Notes: (A) Forest plot of OS. (B) Forest plot of PFS. Weights are from random-effects analysis.
Abbreviations: CTCs, circulating tumor cells; GC, gastric cancer; HR, hazard ratio; OS, overall survival; PFS, progression-free survival.
Furthermore, we stratified the included studies based on variables (year of publication, country of patients, sampling time, cutoff value, positive rate of CTC detection, and quality of included studies). The results of pooled analysis demonstrated that CTC positivity was a significant prognostic effect for OS and PFS for most of subgroups (Table 2). Additionally, the between-study heterogeneity was eliminated in subgroups by exclusion of studies coming from countries other than Japan, and with a cutoff value ≤2, positive rate of CTC detection ≥41.9%, or low quality for OS. However, all the above variables did not positively contribute to the heterogeneity for PFS.
Table 2.
Results of subgroup analyses on OS and PFS
| Variable | n | OS
|
n | PFS
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | P-valuea | I2 | P-valueb | HR (95% CI) | P-valuea | I2 | P-valueb | |||
| Yearc | ||||||||||
| > Median | 4 | 1.84 (1.36, 2.49) | <0.001 | 50.2% | 0.111 | 3 | 2.02 (1.48, 2.76) | <0.001 | 8.1% | 0.337 |
| ≤ Median | 4 | 2.30 (1.77, 2.99) | <0.001 | 0.7% | 0.388 | 3 | 2.11 (0.52, 8.51) | 0.293 | 88.8% | <0.001 |
| Country | ||||||||||
| Japan | 5 | 2.28 (1.79, 2.91) | <0.001 | 0.0% | 0.552 | 3 | 2.61 (0.89, 7.63) | 0.081 | 87.1% | <0.001 |
| Other | 3 | 1.75 (1.24, 2.47) | 0.001 | 64.6% | 0.060 | 3 | 1.80 (1.14, 2.84) | 0.011 | 40.0% | 0.189 |
| Sampling time | ||||||||||
| Baseline | 7 | 2.04 (1.67, 2.50) | <0.001 | 34.7% | 0.163 | 6 | 2.11 (1.25, 3.57) | 0.005 | 75.6% | 0.001 |
| Intra-therapy | 1 | 3.35 (1.32, 8.47) | 0.011 | – | – | 0 | – | – | – | – |
| Cutoff valued | ||||||||||
| > Median | 3 | 1.90 (1.38, 2.61) | <0.001 | 0.0% | 0.780 | 3 | 1.70 (1.06, 2.73) | 0.029 | 54.1% | 0.113 |
| ≤ Median | 5 | 2.22 (1.72, 2.86) | <0.001 | 56.3% | 0.058 | 3 | 2.72 (0.93, 7.94) | 0.067 | 83.4% | 0.002 |
| Positive ratee | ||||||||||
| ≥ Median | 4 | 1.91 (1.41, 2.58) | <0.001 | 58.9% | 0.063 | 3 | 1.33 (0.92, 1.94) | 0.131 | 0.0% | 0.641 |
| < Median | 4 | 2.24 (1.72, 2.91) | <0.001 | 0.0% | 0.512 | 3 | 3.39 (1.67, 6.88) | 0.001 | 76.7% | 0.014 |
| Quality | ||||||||||
| High | 6 | 2.15 (1.75, 2.65) | <0.001 | 0.0% | 0.770 | 5 | 2.32 (1.32, 4.09) | 0.004 | 78.6% | 0.001 |
| Low | 2 | 1.49 (0.74, 3.00) | 0.264 | 85.1% | 0.010 | 1 | 1.06 (0.37, 3.03) | 0.914 | – | – |
| Overall | 8 | 2.09 (1.71, 2.55) | <0.001 | 31.5% | 0.177 | 6 | 2.11 (1.25, 3.57) | 0.005 | 75.6% | 0.001 |
Notes:
P-value for estimates of HR.
P-value for heterogeneity.
The median year of OS and PFS was 2013 and 2014, respectively.
The median cutoff value of OS and PFS was 2 and 2, respectively.
The median positive rate of OS and PFS was 41.9% and 31.7%, respectively. –, not available.
Abbreviations: HR, hazard ratio; OS, overall survival; PFS, progression-free survival.
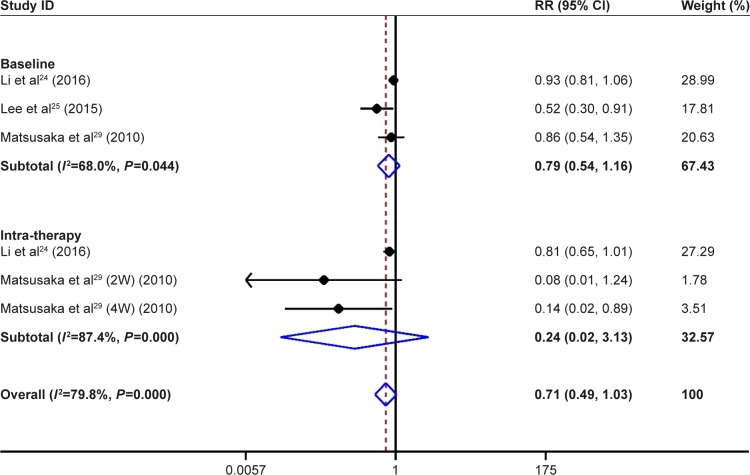
Impact of CTC detection on DCR
Only three studies evaluated the correlation between CTCs and DCR in patients receiving adjuvant chemotherapy.24,25,29 The pooled results demonstrated that the DCR for the CTC-positive groups was lower than that for the CTC-negative groups at baseline and intra-therapy, although there was no statistical difference (baseline: 69.5% versus 81.8%, RR=0.79, 95% CI [0.54, 1.16], P=0.23, I2=68.0%; intra-therapy: 50.0% versus 85.9%, RR=0.24, 95% CI [0.02, 3.13], P=0.28, I2=87.4%; Figure 3).
Figure 3.
Summary estimates of RR for DCR of patients with CTC positivity.
Note: Weights are from random-effects analysis.
Abbreviations: CTCs, circulating tumor cells; DCR, disease control rate; RR, risk ratio; W, week.
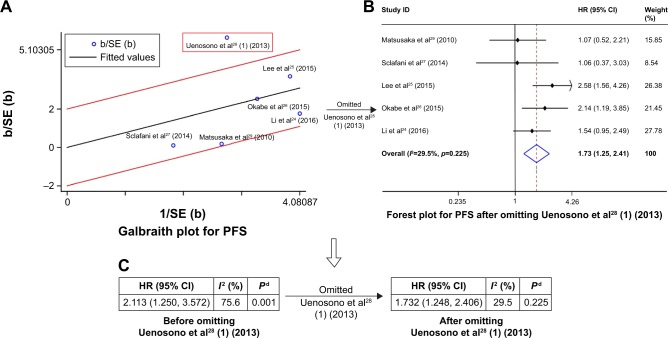
The source of heterogeneity
To explore the potential sources of heterogeneity, we conducted a meta-regression that considered the variables of year of publication, country, sampling time, cutoff value, and quality of included studies. As shown in Table 3, in a univariate analysis, none of these variables was significantly correlated with the heterogeneity across studies in OS and PFS. However, the results of meta-regression may be affected by the limited number of studies in the analysis (n=6). Therefore, we used Galbraith plot to further explore the source of heterogeneity in PFS, and the result showed that the training set of the study by Uenosono et al28 might have mainly contributed substantial heterogeneity to PFS (Figure 4A). After omitting this study, the pooled HR was not affected obviously (HR =1.73, 95% CI [1.25, 2.41], P=0.001; Figure 4B), but the heterogeneity for PFS dropped to an insignificant level (from I2=75.6%, P=0.001 to I2=29.5%, P=0.225; Figure 4C).
Table 3.
Results of meta-regression on OS and PFS
| Variable | OS
|
PFS
|
||||||
|---|---|---|---|---|---|---|---|---|
| Coef | SE | P-value | Adjusted R2 | Coef | SE | P-value | Adjusted R2 | |
| Year | −0.0234 | 0.0652 | 0.731 | −27.06% | 0.0392 | 0.1679 | 0.827 | −34.46% |
| Country | −0.0588 | 0.1123 | 0.619 | −22.55% | −0.1298 | 0.2703 | 0.656 | −28.19% |
| Sampling time | −0.4929 | 0.6007 | 0.443 | −10.16% | – | – | – | – |
| Cutoff value | −0.0555 | 0.0822 | 0.525 | −16.89% | −0.1640 | 0.2014 | 0.461 | −12.55% |
| Quality | 0.3685 | 0.4615 | 0.455 | −10.11% | 0.7849 | 0.9145 | 0.439 | −5.75% |
Notes: Adjusted R2, proportion of between-study variance explained. –, not available.
Abbreviations: Coef, coefficient; OS, overall survival; PFS, progression-free survival; SE, standard error.
Figure 4.
Process of exploring the potential sources of heterogeneity on PFS.
Notes: (A) Galbraith plot for PFS. (B) Forest plot for PFS after Uenosono et al28 (1) (2013) is omitted. (C) Change of heterogeneity before and after Uenosono et al28 (1) (2013) is omitted. Weights are from random-effects analysis. Pd value for heterogeneity.
Abbreviations: HR, hazard ratio; PFS, progression-free survival; SE, standard error.
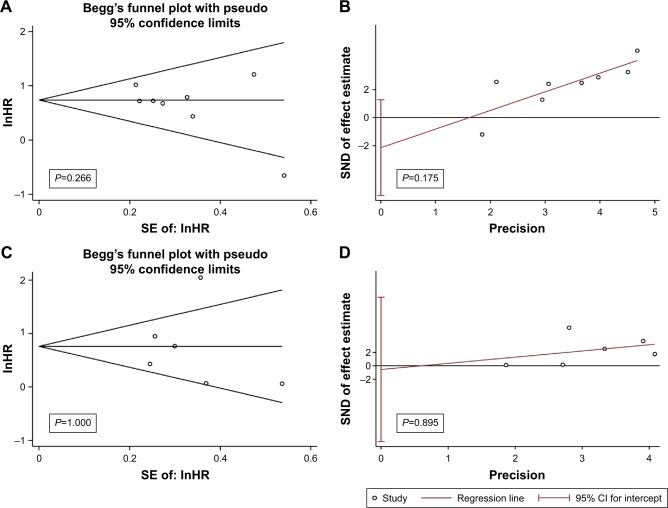
Assessment of publication bias
Potential publication bias was assessed by Begg’s and Egger’s tests. There was no evidence of publication bias for the pooled analysis of OS (PBegg’s=0.266, Figure 5A; PEgger’s=0.175, Figure 5B) and PFS (PBegg’s=1.000, Figure 5C; PEgger’s=0.899, Figure 5D).
Figure 5.
Funnel plots of included studies reporting OS and PFS.
Notes: (A) Begg’s funnel plot on OS. (B) Egger’s funnel plot on OS. (C) Begg’s funnel plot on PFS. (D) Egger’s funnel plot on PFS.
Abbreviations: HR, hazard ratio; OS, overall survival; PFS, progression-free survival; SE, standard error; SND, standard normal deviate.
Discussion
Although curative surgery in combination with chemoradiotherapy and targeted therapy has greatly developed in recent years, the occurrence of metastasis and relapse of GC is still a great challenge for both surgeons and patients. The presence of CTCs in the PB may provide a reasonable explanation for metastasis and relapse by the “seed and soil” theory.30 From the clinical perspective, CTCs enumeration can supply important prognostic information for the patients on solid tumor. Besides, due to its advantages of saving time and cost and providing comfort and repeatability, CTCs detection from PB can be used as an effective tool for monitoring therapeutic effect. Several previous meta-analyses have reported the prognostic and clinicopathologic significance of CTCs detection from PB in patients with GC; however, the methods of detecting CTCs were mainly RT-PCR and ICC in the studies included by them.31–33 Recently, the clinical utility of CTC detection in the PB with the standardized CellSearch System has been demonstrated in several studies.24–26 Therefore, it is essential to conduct a meta-analysis to quantitatively summarize the clinical value of CTCs detected with the standardized CellSearch System in GC patients.
To our knowledge, this was the first comprehensive meta-analysis to assess the prognostic and predictive value of CTC detection with the CellSearch System only in GC. Although the previous meta-analysis by Zou et al explored the clinicopathologic significance of CTC detection with cytological techniques (including CellSearch) in GC and the selected studies of our meta-analysis matched part of their included studies,31 there are some important differences between the two studies. First, we processed the data more finely compared to the previous study. In fact, the study by Uenosono et al included two independent sets of data (training set and validation set) and both of them had to be incorporated into the meta-analysis;28 however, Zou et al did not do so, which affected the accuracy of their results. More importantly, we further explored the between-study heterogeneity through subgroup analysis, meta-regression, and Galbraith plot and eventually concluded that the training set of Uenosono et al28 was the main source of the heterogeneity in PFS. In a previous study, the between-study heterogeneity was not obvious, however, as it did not include the training set of Uenosono et al.28 As we all know, when between-study heterogeneity is obvious, clarifying the source of heterogeneity is the premise of conducting a meta-analysis. Therefore, our results were more reliable than the previous study, although both studies came to the same conclusion. In our meta-analysis, the results suggested that patients with CTC positivity have poorer OS and PFS than CTC-negative patients. Moreover, these results were also found in most of the subgroups when we stratified the included studies based on variables (Table 2). Additionally, the pooled analysis showed the DCR of CTC-positive groups was lower than that of CTC-negative groups for both baseline and intra-therapy, indicating that CTCs detected at baseline or intra-therapy might predict the response to chemotherapy. However, no statistical difference existed in both baseline and intra-therapy time points. This was inconsistent with the results of a previous meta-analysis by Huang et al,32 which might be due to the smaller studies used in our meta-analysis to evaluate the correlation between CTC counts and tumor responses on imaging according to the Response Evaluation Criteria In Solid Tumors criteria.24,25,29 Taken together, these results indicated that CTCs detected by the CellSearch System have great clinical value in evaluating prognosis, guiding therapeutic decision, and monitoring therapeutic effect for GC patients. For the CTC-positive patients, more aggressive treatment and frequent efficacious assessments might be needed.
Compared to traditional ICC and RT-PCR techniques, the CellSearch System has the advantages of easy operation, time effectiveness, and higher specificity and reproducibility for CTCs enrichment. Although our meta-analysis of studies had used the CellSearch System to reduce the heterogeneity caused by different detection methods, a significant heterogeneity was still found in our meta-analysis, specifically in the pooled analysis of PFS. In addition, subgroup analyses and meta-regression were conducted to explore the potential sources of heterogeneity; however, the results failed to clarify the heterogeneity among the involved studies. Furthermore, the Galbraith plot showed that heterogeneity in the pooled analysis PFS was mainly caused by the training set of the study by Uenosono et al.28 The reason might be that the positive rate of CTC detection was relatively low, even with more patients included in this study.
Potential heterogeneity may also result from difference in sampling time, standard of CTC positivity, treatment regimens, or clinicopathologic data of included patients. Theoretically, intra-therapy CTC status may provide relatively more information because it reflects the combined information on baseline CTCs and tumor cells’ release during surgical manipulation.34 The study by Ikeguchi and Kaibara found that CTC-positive patients had better prognosis than CTC-negative patients if the blood samples were postoperatively collected within 48 hours.35 However, owing to loss of survival microenvironment in PB, these freshly released CTCs may be rapidly apoptotic and release mass tumor antigens, leading to certain degree of detection bias. Additionally, there is no consensus on the optimal cutoff value for CTCs in the PB for predicting the prognosis of patients with GC. Although most studies used the cutoff value of CTCs ≥1/7.5 or ≥2/7.5 mL of PB in our meta-analysis and subgroup analyses also demonstrated that CTC positivity at both cutoff values strongly tended to have an unpleasant prognosis, the optimal cutoff value of defining CTC positivity in GC patients is still not confirmed. The studies by Li et al and Matsusaka et al showed that the cutoff value of CTCs ≥3/7.5 mL or ≥4/7.5 mL was also associated with poor prognosis in patients with GC.24,29 Thus, further well-designed, large-scale multicenter studies are needed to confirm the optimal sampling time and cutoff value of CTC detection. Furthermore, the genomic and functional heterogeneity of CTCs was also a source of heterogeneity. Different design types of the cohort studies also generated non-negligible heterogeneity.
Limitations
Several limitations remained in our meta-analysis. First, our meta-analysis used the data extracted from the included studies and the original data from the individual patients was hard to get. Moreover, several studies did not provide HRs and we estimated them from the reported data. Second, there was considerable heterogeneity in our study. We addressed the issue of heterogeneity by a rigorous method that used the relatively conservative random-effect model. As is well known, the prognosis of GC patients with and without surgery is different. However, the small number of studies (only the training set of Uenosono et al)28 included in our meta-analysis may have been insufficient to conduct subgroup analysis to explore the different prognostic significance of CTC detection in surgical and nonsurgical groups. Third, the effects of racial disparity of GC patients from different regions on the outcome need to be considered. In our study, six of seven included studies were reported from Asian countries, which made our findings have no broad representation. Fourth, the total number of patients was relatively small in this meta-analysis. Therefore, although our pooled analysis showed CTC positivity detected with the CellSearch System was an indicator of poor prognosis in GC patients, however, the results should be interpreted with caution and it requires larger samples, multiple regions, and more accurate study data for further verification.
Conclusion
Altogether, our meta-analysis demonstrated that CTCs detected with the CellSearch System from PB had significant prognostic value and might predict poor response to chemotherapy for patients with GC, which indicated CTC detection might have great clinical potential for guiding individualized therapy, monitoring therapeutic effect, and predicting prognosis of GC patients. Further high-quality, well-designed multicenter studies are required to confirm the more accurate clinical value of CTCs detected with the CellSearch System in GC patients.
Footnotes
Author contributions
BX: concept and study design. CY, KZ, and ZY: publication retrieval and data extraction. CY, KZ, and TG: statistical analyses. CY: manuscript writing. All authors approved the submission, contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Correia M, Machado JC, Ristimaki A. Basic aspects of gastric cancer. Helicobacter. 2009;14(Suppl 1):36–40. doi: 10.1111/j.1523-5378.2009.00696.x. [DOI] [PubMed] [Google Scholar]
- 3.Marrelli D, De Stefano A, de Manzoni G, Morgagni P, Di Leo A, Roviello F. Prediction of recurrence after radical surgery for gastric cancer: a scoring system obtained from a prospective multicenter study. Ann Surg. 2005;241(2):247–255. doi: 10.1097/01.sla.0000152019.14741.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Budd GT, Cristofanilli M, Ellis MJ, et al. Circulating tumor cells versus imaging-predicting overall survival in metastatic breast cancer. Clin Cancer Res. 2006;12(21):6403–6409. doi: 10.1158/1078-0432.CCR-05-1769. [DOI] [PubMed] [Google Scholar]
- 5.Kubisch I, de Albuquerque A, Schuppan D, Kaul S, Schaich M, Stolzel U. Prognostic role of a multimarker analysis of circulating tumor cells in advanced gastric and gastroesophageal adenocarcinomas. Oncology. 2015;89(5):294–303. doi: 10.1159/000437373. [DOI] [PubMed] [Google Scholar]
- 6.Xia P, Song CL, Liu JF, Wang D, Xu XY. Prognostic value of circulating CD133(+) cells in patients with gastric cancer. Cell Prolif. 2015;48(3):311–317. doi: 10.1111/cpr.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qiu MZ, Li ZH, Zhou ZW, et al. Detection of carcinoembryonic antigen messenger RNA in blood using quantitative real-time reverse transcriptase-polymerase chain reaction to predict recurrence of gastric adenocarcinoma. J Transl Med. 2010;8:107. doi: 10.1186/1479-5876-8-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seo JH, Choi CW, Kim BS, et al. Follow-up study of peripheral blood carcinoembryonic antigen mRNA using reverse transcription-polymerase chain reaction as an early marker of clinical recurrence in patients with curatively resected gastric cancer. Am J Clin Oncol. 2005;28(1):24–29. doi: 10.1097/01.coc.0000139018.47930.a5. [DOI] [PubMed] [Google Scholar]
- 9.Miller MC, Doyle GV, Terstappen LW. Significance of circulating tumor cells detected by the CellSearch System in patients with metastatic breast colorectal and prostate cancer. J Oncol. 2010;2010:617421. doi: 10.1155/2010/617421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen SJ, Punt CJ, Iannotti N, et al. Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26(19):3213–3221. doi: 10.1200/JCO.2007.15.8923. [DOI] [PubMed] [Google Scholar]
- 11.Riethdorf S, Fritsche H, Muller V, et al. Detection of circulating tumor cells in peripheral blood of patients with metastatic breast cancer: a validation study of the CellSearch system. Clin Cancer Res. 2007;13(3):920–928. doi: 10.1158/1078-0432.CCR-06-1695. [DOI] [PubMed] [Google Scholar]
- 12.Janni WJ, Rack B, Terstappen LW, et al. Pooled analysis of the prognostic relevance of circulating tumor cells in primary breast cancer. Clin Cancer Res. 2016;22(10):2583–2593. doi: 10.1158/1078-0432.CCR-15-1603. [DOI] [PubMed] [Google Scholar]
- 13.Ma X, Xiao Z, Li X, et al. Prognostic role of circulating tumor cells and disseminated tumor cells in patients with prostate cancer: a systematic review and meta-analysis. Tumour Biol. 2014;35(6):5551–5560. doi: 10.1007/s13277-014-1731-5. [DOI] [PubMed] [Google Scholar]
- 14.Huang X, Gao P, Song Y, et al. Meta-analysis of the prognostic value of circulating tumor cells detected with the CellSearch System in colorectal cancer. BMC Cancer. 2015;15:202. doi: 10.1186/s12885-015-1218-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 16.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92(3):205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 17.Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. doi: 10.1186/1745-6215-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 19.Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17(24):2815–2834. doi: 10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 21.Asimit J, Day-Williams A, Zgaga L, Rudan I, Boraska V, Zeggini E. An evaluation of different meta-analysis approaches in the presence of allelic heterogeneity. Eur J Hum Genet. 2012;20(6):709–712. doi: 10.1038/ejhg.2011.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295(6):676–680. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- 23.Hiraiwa K, Takeuchi H, Hasegawa H, et al. Clinical significance of circulating tumor cells in blood from patients with gastrointestinal cancers. Ann Surg Oncol. 2008;15(11):3092–3100. doi: 10.1245/s10434-008-0122-9. [DOI] [PubMed] [Google Scholar]
- 24.Li Y, Gong J, Zhang Q, et al. Dynamic monitoring of circulating tumour cells to evaluate therapeutic efficacy in advanced gastric cancer. Br J Cancer. 2016;114(2):138–145. doi: 10.1038/bjc.2015.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee SJ, Lee J, Kim ST, et al. Circulating tumor cells are predictive of poor response to chemotherapy in metastatic gastric cancer. Int J Biol Markers. 2015;30(4):e382–e386. doi: 10.5301/jbm.5000151. [DOI] [PubMed] [Google Scholar]
- 26.Okabe H, Tsunoda S, Hosogi H, et al. Circulating tumor cells as an independent predictor of survival in advanced gastric cancer. Ann Surg Oncol. 2015;22(12):3954–3961. doi: 10.1245/s10434-015-4483-6. [DOI] [PubMed] [Google Scholar]
- 27.Sclafani F, Smyth E, Cunningham D, Chau I, Turner A, Watkins D. A pilot study assessing the incidence and clinical significance of circulating tumor cells in esophagogastric cancers. Clin Colorectal Cancer. 2014;13(2):94–99. doi: 10.1016/j.clcc.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 28.Uenosono Y, Arigami T, Kozono T, et al. Clinical significance of circulating tumor cells in peripheral blood from patients with gastric cancer. Cancer. 2013;119(22):3984–3991. doi: 10.1002/cncr.28309. [DOI] [PubMed] [Google Scholar]
- 29.Matsusaka S, Chin K, Ogura M, et al. Circulating tumor cells as a surrogate marker for determining response to chemotherapy in patients with advanced gastric cancer. Cancer Sci. 2010;101(4):1067–1071. doi: 10.1111/j.1349-7006.2010.01492.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fidler IJ. The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nat Rev Cancer. 2003;3(6):453–458. doi: 10.1038/nrc1098. [DOI] [PubMed] [Google Scholar]
- 31.Zou K, Yang S, Zheng L, Wang S, Xiong B. Prognostic role of the circulating tumor cells detected by cytological methods in gastric cancer: a meta-analysis. Biomed Res Int. 2016;2016:2765464. doi: 10.1155/2016/2765464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang X, Gao P, Sun J, et al. Clinicopathological and prognostic significance of circulating tumor cells in patients with gastric cancer: a meta-analysis. Int J Cancer. 2015;136(1):21–33. doi: 10.1002/ijc.28954. [DOI] [PubMed] [Google Scholar]
- 33.Wang S, Zheng G, Cheng B, et al. Circulating tumor cells (CTCs) detected by RT-PCR and its prognostic role in gastric cancer: a meta-analysis of published literature. PLoS One. 2014;9(6):e99259. doi: 10.1371/journal.pone.0099259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Balic M, Williams A, Dandachi N, Cote RJ. Micrometastasis: detection methods and clinical importance. Cancer Biomark. 2010;9(1–6):397–419. doi: 10.3233/CBM-2011-0161. [DOI] [PubMed] [Google Scholar]
- 35.Ikeguchi M, Kaibara N. Detection of circulating cancer cells after a gastrectomy for gastric cancer. Surg Today. 2005;35(6):436–441. doi: 10.1007/s00595-004-2978-z. [DOI] [PubMed] [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. https://doi.org/10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]