Abstract
Although High-intensity interval training (HIIT) has shown its effectiveness in improving body composition, cardio-respiratory fitness and lipid profile in obese adults, evidences remain limited in overweight/obese youth. This study was conducted to investigate the effect of a 12-week HIIT program without caloric restriction on body composition and lipid profile among young overweight/obese men. Twenty healthy obese youth were randomly allocated into two groups; experimental group (HIIT) and control group. The HIIT program consisted in 3 exercises sessions per week (30 sec of work at 100% maximal aerobic velocity [MAV]) interspersed by 30 sec of active recovery at 50% MAV, starting by 15 repetitions to reach 27 by the end of the program. Aerobic capacity (MAV and maximum oxygen uptake [VO2max]), body composition (body mass index [BMI], waist circumference [WC], and fat mass percent) and lipid profile (triglycerides [TG] and total, high-density lipoprotein [HDL] and low-density lipoprotein [LDL] cholesterol) were determined before and after the HIIT program. Following 12 weeks of HIIT, WC, BMI (P<0.01), and fat mass percent (P<0.05) were significantly decreased. MAV and VO2max were significantly improved in the HIIT group, only. Total cholesterol (P<0.05) and TG (P<0.05) decreased significantly in the HIIT group, while LDL and HDL cholesterol levels remained unchanged in both groups. HIIT may be particularly useful in overweight/obese youth to improve body composition, aerobic fitness and lipid profile.
Keywords: High-intensity interval training, Body composition, Lipid pro-file, Overweight, Obesity, Youth
INTRODUCTION
While physical inactivity has a wide range of adverse health consequences such as obesity, hypertension and various metabolic disorders (Kannan et al., 2014), nearly 31% of people aged 15 and older show insufficient physical activity (men 28% and women 34%) according to the World Health Organization (2008), Moreover, this lack of physical activity is accompanied by an increasing availability and consumption of energy dense food, rich in lipids and carbohydrates, seriously damaging cardiovascular health.
Physical training and especially aerobic training, is considered to be one of the angular stones for cardiovascular protection, but its effectiveness depends on numerous factors, such as age, sex, body composition, and nutrition, as well as training duration and intensity (Ouerghi et al., 2014). Recently, high-intensity interval training (HIIT) has attracted attention as a time-efficient exercise option to improve cardiovascular and metabolic health (Little and Francois, 2014). This method of training has led to a promising reduction of cardio-metabolic risk factors in adolescents, and thus became an interesting alternative approach to improve youth’s health (Logan et al., 2014). Most studies questioning the effect of HIIT programs on body composition remain however sometimes contradictory in youth. Indeed, while Keating et al. (2014) have reported that 12 weeks of HIIT has no meaningful effect on body fat (BF) levels in inactive overweight adults, Gillen et al. (2013) found improved body composition in response to a 6-week HIIT intervention in obese adults. According to previous studies, HIIT improves plasma lipids in overweight and obese adults (Alahmadi, 2014; Fisher et al., 2015; Koubaa et al., 2013), which remains unclear in adolescents and youth with obesity. Indeed, although Batacan et al. (2017) have demonstrated that long-term HIIT (≥12 weeks) significantly improved maximum oxygen uptake (VO2max) and resting heart rate in overweight/obese populations, they missed to find any total cholesterol (TC), high-density lipoprotein (HDL) and low-density lipoprotein (LDL) cholesterol, and triglycerides (TG) changes. Similarly, Heydari et al. (2012) reported that a 12-week HIIT program has no effect on insulin, glucose, homeostatic model assessment-insulin resistance, TC, LDL and HDL cholesterol, and TG in overweight young males. By cons, other studies have shown that 8-week HIIT positively changes blood lipids in young men (Musa et al., 2009; Ouerghi et al., 2017a; Ouerghi et al., 2017b). Collectively; these conflicting results clearly indicate the need for more researches questioning the effects of HIIT on body composition and metabolic health in youth with obesity.
Although there is a growing interest in the effects of HIIT in obese patients, most of the studies have been conducted among adults; to a lesser extent among adolescents, and evidence remain limited in young adults. As recently highlighted during the last European Congress of Obesity (ECO, Porto, Portugal, May 2017), there is a need for more research for the treatment of obesity among young adults, whose obesity history and dynamic is midway between what is seen in adolescents and in adults (Hutchesson et al., 2013; Steinbeck et al., 2017).
While weight gain in early adulthood increases the risk factors for developing a chronic disease (Hutchesson et al., 2013), the literature regarding the effect of physical activity intervention remains limited in this population. In 2008, Trapp et al. (2008) showed that 15 weeks of intermittent training (45 sessions of HIIT) without any food intake control, favored a significant weight loss in women in early adulthood (combining exercise with a low or high-energy dense diet). Song et al. (2010) found improved body weight and BF percentage after a 4-week intervention in slightly overweight young women. While evidences remain limited regarding the effect of HIIT in early adulthood, the present study aimed at assessing the effects of a 12-week HIIT on body composition and lipid profile in sedentary healthy overweight/obese young males.
MATERIALS AND METHODS
Design
The study was conducted from September to December 2016 and was spread over a period of 14 weeks (2 weeks of evaluation and 12 weeks of training).
One week before the start of the training program (T0), anthropometric parameters (height, weight, body mass index [BMI], and waist circumference [WC], fat mass percentage, and physical fitness; maximal aerobic velocity [MAV], VO2max, and maximal heart rate [HRmax]) were assessed and fasting blood sample were drawn. The participants were then randomly assigned to whether a control group (CON; without any intervention) or a training group (HIIT) for 12 weeks. All the aforementioned measurements were realized once more by the end of the 12 weeks.
Subjects
Twenty healthy untrained overweight/obese males (BMI≥25 kg/m2), aged between 18 and 21 years participated in this study. The participants, who were randomly selected, undergo 3 hr of weekly physical activity as part of the school physical education program. To be included, the participants had to be nonsmokers, nonalcoholic drinkers, and without any previous history of disease that could have interfered with the results. Following a complete verbal explanation of the protocol, potential risks, and benefits of the experiments, all subjects signed a written informed consent prior their participation to the experimental protocol. The study protocol was performed in accordance with the ethical standards of the Helsinki Declaration and was fully approved by the Scientific and Ethics Committee of High Institute of Sports and Physical Education of Kef (HISPE_EC2016).
Measurements
Anthropometric measures and body composition
Weight and height were measured to the nearest 0.1 kg and 0.5 cm respectively using a TPRO 3100 Terraillon electronic balance (Terraillon SA, Survilliers, France) and a SECA 216 Wall Mounted Stadiometer (SECA SA, Semur-en-Auxois, France). BMI was calculated using the following formula: weight/height2 (kg/m2). WC was measured with a nondeformable tape ruler between the last rib margin and the superior iliac crest. Skinfold thickness of each subjects was measured in triplicate by a Harperden’s skinfold calipers (Baty International, West Sussex, England) at four sites (biceps, triceps, subscapular, and supra iliac). Subsequently, and from the measurement of the skin-fold thickness, the percentage of BF was estimated according to the equation of Durnin and Womersley (1974).
Aerobic capacity
Incremental running test: Vameval test (Cazorla, 1990) was adopted to determine the MAV and to estimate the VO2max. It was performed on a 400-m running track marked every 20 m. Each participant begins with a running speed of 8.5 km/hr, with consecutive speed increases of 0.5 km/hr every minute until exhaustion (Cazorla, 1990). Each participant has to adjust his running velocity, to reach the correspondent cone concomitantly with the sound track signal. The test ended when the subject could no longer maintain the required speed imposed by the beep, or when he was not able to reach the following cone in due time. During the Vameval test, heart rate was recorded using a heart rate monitor (S810, Polar, Kempele, Finland).
Training program
The intervention lasted 12 consecutive weeks with three sessions per week (36 sessions in total) according to Ouerghi et al. (2016), Ouerghi et al. (2017a), and Ouerghi et al. (2017b) (Table 1 details the intervention). Each training session started with a standard warm-up including 15 min of running at low intensity (at 50% of MAV), 3 repetitions of 30-sec acceleration followed by 30 sec of cool down running and 5 min of dynamic stretching.
Table 1.
Training program
| Weeks (1+2+3) | Weeks (4+5+6) | Weeks (7+8+9) | Weeks (10+11+12) | |
|---|---|---|---|---|
| HIIT | 3×(5×30 sec) (1:1) | 3×(7×30 sec) (1:1) | 3×(7×30 sec) (1:1) | 3×(9×30 sec) (1:1) |
| (100%:50% MAV) | (100%:50% MAV) | (110%:50% MAV) | (110%:50% MAV) | |
| R=5 min | R=5 min | R=5 min | R=5 min |
Example: 3×(5×30 sec) (1:1) (100%:50% MAV) means that each subject of intermittent group must run for 30 sec at 100% of MAV followed by 30 sec of active recovery at 50% of the MAV with each repetition. Each training session is composed of three sets at five repetitions each. (1:1): represents the ratio of the exercise period and the recovery period, which indicates that the period of work is equal to the period of active recovery.
HIIT, high-intensity interval training; MAV, maximal aerobic velocity; R, recovery between sets.
Short duration 30-30 HIIT program
All participants were instructed to alternate 30 sec of running at 100% of MAV and 30 sec of active recovery at 50% of MAV. Following the rules of progression when it comes to exercise interventions, the number of repetitions and the intensity were increased over time (Ouerghi et al., 2016; Ouerghi et al., 2017a; Ouerghi et al., 2017b), as described by the Table 1.
Although food intake and daily physical activity were not recorded, the participants were asked to maintain their usual diet and physical activity outside the sessions.
Blood sampling and analysis
Fasting blood were drawn from antecubital vein in dry tubes (fasting 12 hr) while the participants rested in sitting position, before and after the 12 weeks. After centrifugation, samples were stored at −80°C until analysis. TC, HDL cholesterol (HDL-C), and TG were assessed by the enzymatic colorimetric method on an Architect C8000 system (Abbott Laboratories, Abbott Park, IL, USA) using the respective reagent kits. LDL cholesterol (LDL-C) was calculated as described by the Friedewald formula (Friedewald et al., 1972).
Statistical analysis
The statistical analyses have been performed using StatView ver. 5.0 (SAS Institute Inc., Cary, NC, USA). All data are expressed as mean±standard deviation. Data was checked for normality using the Kolmogorov–Smirnov test. A two-way analysis of variance (ANOVA) with repeated measures has been performed to compare the data from the two groups before and after the intervention. Test de Mann–Whitney has been used to compare deltas (T1–T0) between groups.
RESULTS
Sixteen young overweight/obese males (19.4±1.1 years) with a mean weight of 90.2 kg (±10.9) and mean BMI of 29.2 kg/m2 (±2.3) participated in this study. There were no significant pretraining differences between CON and HIIT groups for body weight, BMI, WC and BF as well as for physical fitness and metabolic indicators (Table 2). Following the training program, the HIIT group showed significant improvement in Δweight (−3.9± 3.2, P>0.01), ΔBMI (−1.2±1, P<0.01), ΔBF (%) (−1.6±1.3, P<0.05) and ΔWC (−5±3.6, P<0.01) compared to CON group (Fig. 1).
Table 2.
Physical, physiological and blood variables before and after 12 weeks in control (CON) and high-intensity interval training (HIIT) groups
| Variable | CON | HIIT | ANOVA | ||
|---|---|---|---|---|---|
|
|
|
||||
| Before | After | Before | After | ||
| Weight (kg) | 89.3±10.5 | 88.2±11.0 | 91.2±12.1 | 87.3±10.5 | 0.96 |
|
| |||||
| BMI (kg/m2) | 29.0±2.2 | 29.2±2.2 | 29.3±2.5 | 28.0±1.9 | 0.67 |
|
| |||||
| BF (%) | 21.4±1.8 | 21.6±1.9 | 22.2±1.6 | 20.7±1.2 | 0.90 |
|
| |||||
| WC (cm) | 97.5±8.7 | 97.9±9.3 | 99.5±8.9 | 95.1±7.9 | 0.93 |
|
| |||||
| MAV (km/hr) | 11.7±1.5 | 11.4±1.4 | 11.3±1.0 | 12.8±1.5 | 0.43 |
|
| |||||
| VO2max (mL/kg/min) | 42.7±5.3 | 41.6±4.9 | 41.8±4.7 | 46.6±5.1 | 0.40 |
|
| |||||
| FC max (bpm) | 193.8±9.6 | 192.4±8.5 | 191.0±10.3 | 190±9.7 | 0.66 |
|
| |||||
| TC (mg/dL) | 171.6±35.3 | 174.4±42.9 | 176.6±34.4 | 151.7±18.0 | 0.59 |
|
| |||||
| TG (mg/dL) | 120.5±41.8 | 124.4±42.1 | 127.0±36.3 | 88.4±22.1 | 0.37 |
|
| |||||
| HDL-C (mg/dL) | 38.4±5.3 | 37.7±5.9 | 36.6±2.7 | 36.7±3.9 | 0.55 |
|
| |||||
| LDL-C (mg/dL) | 109.1± 32.9 | 111.7±42.0 | 114.6±33.2 | 97.3±19.1 | 0.78 |
Values are presented as mean±standard deviation.
ANOVA, analysis of variance; BMI, body mass index; BF, body fat; WC, Waist circumference; MAV, maximal aerobic velocity; VO2max, maximum oxygen uptake; FC max, maximum cardiac frequency; TC, total cholesterol, TG, triglycerides; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Fig. 1.
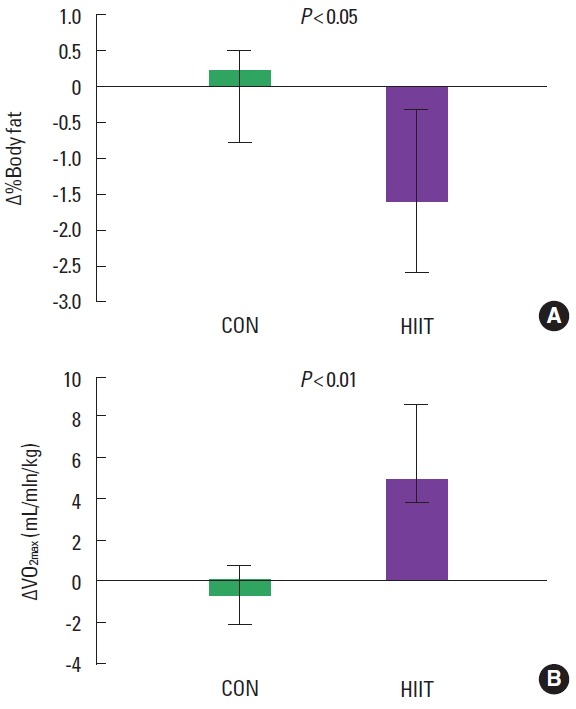
Delta variation differences between T0 and T1 for the control and HIIT for body fat % (A) and maximum oxygen uptake (VO2max) (B). CON, control group; HIIT, intervention group.
No significant change was observed in MAV and VO2max in both CON and HIIT group between T0 and T1 (without difference between groups) (Table 2). The results however revealed significant differences in ΔMAV and ΔVO2max (P<0.01) between the HIIT (1.5±1.0 and 4.8±3.8, respectively) and CON (−0.3±0.5 and −1.1±1.9, respectively) groups.
Similarly lipid profile did not change between T0 and T1 in both groups (Table 2). However, when considering the deltas (Δ), ΔTC (2.7±19.1 vs. −24.9±25.5 for CON and HIIT respectively) and ΔTG (3.9±40.5 vs. −38.6±27.2 for CON and HIIT respectively) are both significantly different between groups (P<0.05).
Our results also show a positive relationship between ΔMAV, ΔVO2max, and initial body weight. Initial BMI was negatively correlated to Δweight and ΔBMI. The initial BF (T0) was found negatively related to Δweight, ΔBMI, and ΔBF. Initial WC was additionally negatively related to Δweight and ΔBF (Table 3).
Table 3.
Correlations between weight, BMI, %BF, and waist circumference at T0 and Δweight, ΔBMI, ΔBF, Δwaist circumference, ΔMAV, and Δ VO2max in HIIT group
| Variable | Correlation (r) | |||
|---|---|---|---|---|
| Weight (kg) T0 | BMI (kg/m2) T0 | BF (%) T0 | WC (cm) T0 | |
| ΔWeight (kg) | −0.72 | −0.80* | −0.84* | −0.72* |
| ΔBMI (kg/m2) | −0.71 | −0.83* | −0.83* | −0.69 |
| ΔBF (%) | −0.73 | −0.71 | −0.82* | −0.86* |
| ΔWC (cm) | −0.42 | −0.67 | −0.42 | −0.46 |
| ΔMAV (km/hr) | 0.74* | 0.55 | 0.67 | 0.29 |
| ΔVO2max (mL/kg/min) | 0.81* | 0.46 | 0.73 | 0.22 |
Δ, Difference between two averages (T1–T0); T0, before the intervention; T1, after 12 weeks of training programs; BMI, body mass index; BF, body fat; MAV, maximal aerobic velocity; VO2max, maximum oxygen uptake; HIIT, high-intensity interval training; WC, Waist circumference.
P<0.05.
DISCUSSION
The purpose of the present study was to analyze the effect of 12 weeks of HIIT without caloric restriction on body composition and lipid profile in sedentary healthy overweight and obese youth. While most of the available literature concerns whether adults or children and adolescents, data are missing among young adults experiencing the physiological transition between childhoods to adulthood, during which interventions are of clinical importance (Hutchesson et al., 2013; Steinbeck et al., 2017).
According to our results, the proposed HIIT intervention favored clinically significant improvements of body composition, physical fitness, and blood lipid profile in overweight/obese youth. Although our initial group-based analysis (ANOVA) missed to show any difference between our HIIT and CON groups, all the parameters under study have been found significantly improved in the HIIT group compared with the CON one (using a delta approach).
Although the benefits of moderate intensity continuous physical activity on body composition are well documented (Irving et al., 2008; Green et al., 2004), results remain unclear for HIIT, especially among obese youth (Lambrick et al., 2016). Yet HIIT is today widely used as a time-efficient strategy for the management of body weight in overweight and obese patients (Wewege et al., 2017), further evidence are still needed to clarify its real impact on body composition (Alahmadi et al., 2014; Kong et al., 2016). Racil et al. (2013) have used a training program similar to ours (30–30) for 12 weeks (2 sets of 6×30 sec at 100%–110% [MAV]with a recovery interval of 30 sec at 50% MAV with 4 min of recovery between series), and found a significant reduction in body mass and WC (−3.58%) in obese adolescent females. Molina et al. (2016) showed that 12 sessions of HIIT associated with nutrition counseling are effective in reducing BF in overweight and obese subjects. However, others missed to observe any effect of HIIT interventions on body composition or body weight among sedentary obese adults (Astorino et al., 2013; Skleryk et al., 2013). A recent systematic review and meta-analysis conducted by Keating et al. (2017) concluded that neither short-term HIIT or sprint interval training favor any clinically meaningful reductions in BF in obese patients. According to our results a 12-week HIIT intervention favored a clinically and statistically significant improvement of several obesity indicators such as body weight, BMI, WC, and BF in our sample of overweight and obese youth. Interestingly our results also indicate that the observed beneficial effect of our HIIT program on obesity indicators might depend on the patient’s initial degree of obesity. Indeed, we found significantly positive correlations between the initial body weight, BMI, and WC (as an indicator for abdominal obesity) and their improved corpulence and BF by the end of the intervention. These observed beneficial effects can be explained by the fact that our sample was composed of highly sedentary and inactive participants. Indeed, as recently pointed out, HIIT might have a great effect on body composition and body weight among sedentary obese individuals compared with active ones (Astorino et al., 2017). Such beneficial results can also be explained by the recently described effects of intensive exercise and especially HIIT on appetite control and eating behaviors in similar populations (Alkahtani et al., 2014; Thivel et al., 2016). Indeed, Alkahtani et al. (2014) have recently showed that HIIT interventions favor decreased hunger and desire to eat in individuals with obesity. More interestingly, their results indicate a decreased food intake with a 16% reduced fat intake after their HIIT intervention while this fat intake increased by 38% following a moderate intensity intervention (Alkahtani et al., 2014). Further studies are need to better understand the exact effects of HIIT on both sides of the energy balance and optimize its role as a weight loss strategy. Not only physical activity interventions have to be designed to favor body weight and body composition improvements in obese patients, it also has to improve their physical fitness.
It is evidently that the factors that induce an improvement in exercise capacity following training are complicated and multiparametric. Indeed, exercise capacity is determined by physiological (cardiovascular, ionic, metabolic, neural, respiratory, etc.) and psychological (mood, motivation, perception of effort, etc.) parameters (Gibala, 2007). In our study we missed to find any significant improvement in MAV and VO2max. Although these results join up with previously published ones (Burgomaster et al., 2005; Gibala et al., 2007; Smith-Ryan et al., 2015), they are in contradiction with the majority of the literature (Kong et al., 2016; Milanović et al., 2015; Ouerghi et al., 2017a; Ouerghi et al., 2017b; Weston et al., 2014) However this lack of modification in VO2max does not mean that there is no improvement in exercise capacity. Indeed Gibala (2007) reported similar results to ours, with a VO2max that does not change in response to HIIT program, noting however an improvement in exercise capacity (time to exhaustion at 80% of pretraining VO2max [Burgomaster et al., 2005]). Moreover after ours intervention ΔVO2max was significantly improved compared to ΔVO2max in the CON (P<0.01), clearly pointing out a beneficial effect of the intervention.
Interestingly, our results show a significant and positive correlation between the participants’ initial body weight and the aerobic capacities improvements (MAV and VO2max) in the HIIT group, suggesting that such an intervention may have greater effects on these variables depending on the patients’ initial obesity degree (as described below for body composition). Further studies are then needed to explore this potential implication of the degree of obesity in the success of HIIT programs. Finally, we also aimed at exploring the effects of our HIIT intervention on our participant’s metabolic profile.
There is a large controversy regarding the impact of HIIT on lipid profile. According to our results, the 12 weeks of HIIT led to an improvement in lipid profile in overweight and obese youth, although it was not statistically significant. The same results were also observed in the study by Sawyer et al. (2016), which reported that 8 weeks of HIIT (10×1 min, 90%–95% HRmax, 1-min active recovery) have no significant effects on TC, LDL-C, HDL-C, and TG in obese adults. In the same way Smith-Ryan et al. (2015) have shown that 8 weeks of HIIT were unable to demonstrate any positive effects on different parameters of lipid profile in overweight/obese adults (aged from 18 to 50 years). A systematic review and meta-analysis conducted by Batacan et al. (2017) concluded that long-term HIIT has no effect on lipid profile in overweight/obese populations. Contrary to our results, a study conducted by Ouerghi et al. (2017a) and Ouerghi et al. (2017b) have shown that 8 weeks of HIIT (2 sets of 8×30 sec runs at 100%–110% of MAV with a recovery interval of 30 sec runs at 50% of MAV) induced a significant decrease in TC, LDL-C, and TG on overweight/obese young men (BMI=30.8±4.6 kg/m2). Likewise, Fisher et al. (2015) reported that 6 weeks of HIIT are effective in improving TC and TG in sedentary overweight or obese youth (BMI=30±3.1 kg/m2). These discrepancies in the results might be associated with the diversity of training programs, measurement techniques used, gender (woman or man), age category (child, adolescent, adult, elderly) or the degree of obesity (moderate, severe, or morbid), among others. The present results highlight the ability of HIIT to elicit improvements in lipid profile; Indeed the comparison between the two groups showed significantly better TG and TC changes in our intervention group (compared with the control one) (P<0.05). Our results also show decreased levels of TC, LDL-C, and TG of approximately 12.4%, 12%, and 27%, respectively. These changes have profound clinical and health implications. Indeed, a reduction by 1% in plasma concentrations of LDL and TC leads to a decrease in coronary heart disease (CHD) by 2% (Pedersen et al., 1998). This suggests that our training program has succeeded in reducing the risk of CHD by about 24% in overweight/obese young adults.
The main limitations were the reduced study sample. This may underpowered the detection of significant changes in some variables. The VO2max estimation using a field test ‘Vameval’ constitutes also another limit. Indeed, although this is a widely used field testing procedure, the use of a direct maximal aerobic testing using indirect calorimetry would have been more précised (yet less accessible for most of the practitioners). In addition, as suggested below, it would have been interesting to assess our participants’ energy intake at regular intervals during the intervention and by the end of the program to evaluate any potential compensatory responses.
To conclude, this pilot study indicates that a 12-week HIIT intervention can induce clinically significant improvements in body composition, physical fitness and blood lipid profile in young obese. While our results also suggest that the initial degree of obesity might affect the efficacy of such interventions, further studies are needed in this field to improve our weight loss strategies.
ACKNOWLEDGMENTS
The authors would like to extend their gratitude to all participants who volunteered to participate in this study.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- Alahmadi MA. High-intensity interval training and obesity. J Nov Physiother. 2014;4:1000211. https://doi.org/10.4172/2165-7025.1000211. [Google Scholar]
- Alkahtani SA, Byrne NM, Hills AP, King NA. Interval training intensity affects energy intake compensation in obese men. Int J Sport Nutr Exerc Metab. 2014;24:595–604. doi: 10.1123/ijsnem.2013-0032. [DOI] [PubMed] [Google Scholar]
- Astorino TA, Heath B, Bandong J, Ordille GM, Contreras R, Montell M, Schubert MM. Effect of periodized high intensity interval training (HIIT) on body composition and attitudes towards hunger in active men and women. J Sports Med Phys Fitness. 2017 Jun 21; doi: 10.23736/S0022-4707.17.07297-8. [Epub]. https://doi.org/10.23736/S0022-4707.17.07297-8. [DOI] [PubMed] [Google Scholar]
- Astorino TA, Schubert MM, Palumbo E, Stirling D, McMillan DW. Effect of two doses of interval training on maximal fat oxidation in sedentary women. Med Sci Sports Exerc. 2013;45:1878–1886. doi: 10.1249/MSS.0b013e3182936261. [DOI] [PubMed] [Google Scholar]
- Batacan RB, Jr, Duncan MJ, Dalbo VJ, Tucker PS, Fenning AS. Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. Br J Sports Med. 2017;51:494–503. doi: 10.1136/bjsports-2015-095841. [DOI] [PubMed] [Google Scholar]
- Burgomaster KA, Hughes SC, Heigenhauser GJ, Bradwell SN, Gibala MJ. Six sessions of sprint interval training increases muscle oxidative potential and cycle endurance capacity in humans. J Appl Physiol (1985) 2005;98:1985–1990. doi: 10.1152/japplphysiol.01095.2004. [DOI] [PubMed] [Google Scholar]
- Cazorla G. Proceedings of the International Symposium of Guadeloupe. 1990. Field tests to evaluate aerobic capacity and maximal aerobic speed; pp. 151–173. [Google Scholar]
- Durnin JV, Womersley J. Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr. 1974;32:77–97. doi: 10.1079/bjn19740060. [DOI] [PubMed] [Google Scholar]
- Fisher G, Brown AW, Bohan Brown MM, Alcorn A, Noles C, Winwood L, Resuehr H, George B, Jeansonne MM, Allison DB. High intensity interval- vs moderate intensity- training for improving cardiometabolic health in overweight or obese males: a randomized controlled trial. PLoS One. 2015;10:e0138853. doi: 10.1371/journal.pone.0138853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- Gibala MJ. High-intensity interval training: new insights. Sports Sci Exch. 2007;20(2) [Google Scholar]
- Gillen JB, Percival ME, Ludzki A, Tarnopolsky MA, Gibala MJ. Interval training in the fed or fasted state improves body composition and muscle oxidative capacity in overweight women. Obesity (Silver Spring) 2013;21:2249–2255. doi: 10.1002/oby.20379. [DOI] [PubMed] [Google Scholar]
- Green JS, Stanforth PR, Rankinen T, Leon AS, Rao Dc, Skinner JS, Bouchard C, Wilmore JH. The effects of exercise training on abdominal visceral fat, body composition, and indicators of the metabolic syndrome in postmenopausal women with and without estrogen replacement therapy: the HERITAGE family study. Metabolism. 2004;53:1192–1196. doi: 10.1016/j.metabol.2004.04.008. [DOI] [PubMed] [Google Scholar]
- Heydari M, Freund J, Boutcher SH. The effect of high-intensity intermittent exercise on body composition of overweight young males. J Obes. 2012;2012:480467. doi: 10.1155/2012/480467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchesson MJ, Hulst J, Collins CE. Weight management interventions targeting young women: a systematic review. J Acad Nutr Diet. 2013;113:795–802. doi: 10.1016/j.jand.2013.01.015. [DOI] [PubMed] [Google Scholar]
- Irving BA, Davis CK, Brock DW, Weltman JY, Swift D, Barrett EJ, Gaesser GA, Weltman A. Effect of exercise training intensity on abdominal visceral fat and body composition. Med Sci Sports Exerc. 2008;40:1863–1872. doi: 10.1249/MSS.0b013e3181801d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kannan U, Vasudevan K, Balasubramaniam K, Yerrabelli D, Shanmugavel K, John NA. Effect of exercise intensity on lipid profile in sedentary obese adults. J Clin Diagn Res. 2014;8:BC08–BC10. doi: 10.7860/JCDR/2014/8519.4611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keating SE, Johnson NA, Mielke GI, Coombes JS. A systematic review and meta-analysis of interval training versus moderate-intensity continuous training on body adiposity. Obes Rev. 2017;18:943–964. doi: 10.1111/obr.12536. [DOI] [PubMed] [Google Scholar]
- Keating SE, Machan EA, O’Connor HT, Gerofi JA, Sainsbury A, Caterson ID, Johnson NA. Continuous exercise but not high intensity interval training improves fat distribution in overweight adults. J Obes. 2014;2014 doi: 10.1155/2014/834865. Article ID 834865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong Z, Fan X, Sun S, Song L, Shi Q, Nie J. Comparison of high-intensity interval training and moderate-to-vigorous continuous training for cardiometabolic health and exercise enjoyment in obese young women: a randomized controlled trial. PLoS One. 2016;11:e0158589. doi: 10.1371/journal.pone.0158589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koubaa A, Trabelsi H, Masmoudi L, Elloumi M, Sahnoun Z, Zeghal KM, Hakim A. Effect of intermittentand continuous training on body composition cardio-respiratory fitnessand lipid profile in obese adolescents. IOSR J Pharm. 2013;3:31–37. [Google Scholar]
- Lambrick D, Stoner L, Faulkner J. High-intensity interval training (HIIT) or miss: is HIIT the way forward for obese children? Perspect Public Health. 2016;136:335–336. doi: 10.1177/1757913916663147. [DOI] [PubMed] [Google Scholar]
- Little JP, Francois ME. High-intensity interval training for improving postprandial hyperglycemia. Res Q Exerc Sport. 2014;85:451–456. doi: 10.1080/02701367.2014.963474. [DOI] [PubMed] [Google Scholar]
- Logan GR, Harris N, Duncan S, Schofield G. A review of adolescent high-intensity interval training. Sports Med. 2014;44:1071–1085. doi: 10.1007/s40279-014-0187-5. [DOI] [PubMed] [Google Scholar]
- Milanović Z, Sporis G, Weston M. Effectiveness of high-intensity interval training (HIT) and continuous endurance training for VO2max improvements: a systematic review and meta-analysis of controlled trials. Sports Med. 2015;45:1469–1481. doi: 10.1007/s40279-015-0365-0. [DOI] [PubMed] [Google Scholar]
- Molina C, Cifuentes G, Martínez C, Mancilla R, Díaz E. Effects of 12 sessions of high intensity intermittent training and nutrition counseling on body fat in obese and overweight participants. Rev Med Chil. 2016;144:1254–1259. doi: 10.4067/S0034-98872016001000003. [DOI] [PubMed] [Google Scholar]
- Musa DI, Adeniran SA, Dikko AU, Sayers SP. The effect of a high-intensity interval training program on high-density lipoprotein cholesterol in young men. J Strength Cond Res. 2009;23:587–592. doi: 10.1519/JSC.0b013e318198fd28. [DOI] [PubMed] [Google Scholar]
- Ouerghi N, Ben Fradj MK, Bezrati I, Feki M, Kaabachi N, Bouassida A. Effect of high-intensity interval training on plasma omentin-1 concentration in overweight/obese and normal-weight youth. Obes Facts. 2017b;10:323–331. doi: 10.1159/000471882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouerghi N, Fradj MK, Khammassi M, Feki M, Kaabachi N, Bouassida A. Plasma chemerin in young untrained men: association with cardio-metabolic traits and physical performance, and response to intensive interval training. Neuro Endocrinol Lett. 2017a;38:59–66. [PubMed] [Google Scholar]
- Ouerghi N, Khammassi M, Boukorraa S, Feki M, Kaabachi N, Bouassida A. Effects of a high-intensity intermittent training program on aerobic capacity and lipid profile in trained subjects. Open Access J Sports Med. 2014;5:243–248. doi: 10.2147/OAJSM.S68701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouerghi N, Selmi O, Ben Khalifa W, Ben Fradj MK, Feki M, Kaabachi N, Bouassida A. Effect of high-intensity intermittent training program on mood state in overweight/obese young men. Iran J Public Health. 2016;45:951–952. [PMC free article] [PubMed] [Google Scholar]
- Pedersen TR, Olsson AG, Faergeman O, Kjekshus J, Wedel H, Berg K, Wilhelmsen L, Haghfelt T, Thorgeirsson G, Pyörälä K, Miettinen T, Christophersen B, Tobert JA, Musliner TA, Cook TJ. Lipoprotein changes and reduction in the incidence of major coronary heart disease events in the Scandinavian Simvastatin Survival Study (4S) Circulation. 1998;97:1453–1460. doi: 10.1161/01.cir.97.15.1453. [DOI] [PubMed] [Google Scholar]
- Racil G, Ben Ounis O, Hammouda O, Kallel A, Zouhal H, Chamari K, Amri M. Effects of high vs. moderate exercise intensity during interval training on lipids and adiponectin levels in obese young females. Eur J Appl Physiol. 2013;113:2531–2540. doi: 10.1007/s00421-013-2689-5. [DOI] [PubMed] [Google Scholar]
- Sawyer BJ, Tucker WJ, Bhammar DM, Ryder JR, Sweazea KL, Gaesser GA. Effects of high-intensity interval training and moderate-intensity continuous training on endothelial function and cardiometabolic risk markers in obese adults. J Appl Physiol (1985) 2016;121:279–288. doi: 10.1152/japplphysiol.00024.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skleryk JR, Karagounis LG, Hawley JA, Sharman MJ, Laursen PB, Watson G. Two weeks of reduced-volume sprint interval or traditional exercise training does not improve metabolic functioning in sedentary obese men. Diabetes Obes Metab. 2013;15:1146–1153. doi: 10.1111/dom.12150. [DOI] [PubMed] [Google Scholar]
- Smith-Ryan AE, Melvin MN, Wingfield HL. High-intensity interval training: Modulating interval duration in overweight/obese men. Phys Sportsmed. 2015;43:107–113. doi: 10.1080/00913847.2015.1037231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song SW, Bae YJ, Lee DT. Effects of caloric restriction with varying energy density and aerobic exercise on weight change and satiety in young female adults. Nutr Res Pract. 2010;4:414–420. doi: 10.4162/nrp.2010.4.5.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinbeck K, Poobalan A, Aucott L, Thomee S, Nikolaou C, Hill A, Baur L, Gill T. Young adult obesity: the transition from adolescence to emerging adulthood. Obesity Facts. 2017;10(S1):1–274. [Google Scholar]
- Thivel D, Rumbold PL, King NA, Pereira B, Blundell JE, Mathieu ME. Acute post-exercise energy and macronutrient intake in lean and obese youth: a systematic review and meta-analysis. Int J Obes (Lond) 2016;40:1469–1479. doi: 10.1038/ijo.2016.122. [DOI] [PubMed] [Google Scholar]
- Trapp EG, Chisholm DJ, Freund J, Boutcher SH. The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women. Int J Obes (Lond) 2008;32:684–691. doi: 10.1038/sj.ijo.0803781. [DOI] [PubMed] [Google Scholar]
- Weston M, Taylor KL, Batterham AM, Hopkins WG. Effects of low-volume high-intensity interval training (HIT) on fitness in adults: a meta-analysis of controlled and non-controlled trials. Sports Med. 2014;44:1005–1017. doi: 10.1007/s40279-014-0180-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wewege M, van den Berg R, Ward RE, Keech A. The effects of high-intensity interval training vs. moderate-intensity continuous training on body composition in overweight and obese adults: a systematic review and meta-analysis. Obes Rev. 2017;18:635–646. doi: 10.1111/obr.12532. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Physical inactivity: a global public health problem. Geneva (Switzerland): World Health Organization; 2008. Global strategy on diet, physical activity and health. [Google Scholar]


