Abstract
Background
Burnout in health care professionals could have serious negative consequences on quality of patient care, professional satisfaction and personal life. Our aim was to investigate the burnout prevalence, work and lifestyle factors potentially affecting burnout amongst European oncologists ≤40 (YOs).
Methods
A survey was conducted using the validated Maslach Burnout Inventory (MBI) and additional questions exploring work/lifestyle factors. Statistical analyses were carried out to identify factors associated with burnout.
Results
Total of 737 surveys (all ages) were collected from 41 European countries. Countries were divided into six regions. Results from 595 (81%) YOs were included (81% medical oncologists; 52% trainees, 62% women). Seventy-one percent of YOs showed evidence of burnout (burnout subdomains: depersonalization 50%; emotional exhaustion 45; low accomplishment 35%). Twenty-two percent requested support for burnout during training and 74% reported no hospital access to support services. Burnout rates were significantly different across Europe (P < 0.0001). Burnout was highest in central European (84%) and lowest in Northern Europe (52%). Depersonalization scores were higher in men compared with women (60% versus 45% P = 0.0001) and low accomplishment was highest in the 26–30 age group (P < 0.01). In multivariable linear regression analyses, European region, work/life balance, access to support services, living alone and inadequate vacation time remained independent burnout factors (P < 0.05).
Conclusions
This is the largest burnout survey in European Young Oncologists. Burnout is common amongst YOs and rates vary across Europe. Achieving a good work/life balance, access to support services and adequate vacation time may reduce burnout levels. Raising awareness, support and interventional research are needed.
Keywords: burnout, work-life balance, young oncologists, European
Introduction
Burnout is a stress-induced, occupational-related syndrome characterized by emotional exhaustion (EE), feelings of cynicism (depersonalization, DEP) and a loss of purpose and meaning in work (personal accomplishment, PA). It is listed in the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) under the category ‘Problems related to life-management difficulty’. Burnout has been recognized as an issue amongst healthcare professionals across specialties for several decades [1–3]. Physician burnout rates have been shown to vary across medical specialities [4, 5]. However, despite initial reports since the 1990s of burnout as a potential, serious risk for individual oncologists [1], it remains a neglected problem for the oncology profession. In addition to working in an environment of increasing workload, administrative tasks and facing medico-legal issues in an era of reduced resources, there are occupational factors integral to cancer care that put oncologists at risk of burnout. These include constantly communicating with patients about life-changing treatment decisions, delivering bad news and supervising toxic therapies where often there is limited ability to prolong life substantially for many patients. In addition, there are pressures to keep at the forefront of scientific advances and deliver research at a time of reducing workforce and resources and increasing workload and litigation. The potential consequences of burnout are both personal and professional. Substance abuse [6], depression and suicide [7] have all been linked with burnout [8]. Medical errors [9], professional misconduct [10], departure from the oncology profession and early retirement [8, 11] are associated with burnout and ultimately will have a significant, negative impact on the quality of patient care.
There has been increased recognition that doctors treating cancer patients are at risk of burnout. Most recently, in a US survey conducted by the American Society of Clinical Oncology (ASCO), although the majority of oncologists reported satisfaction with their career and speciality, 44.7% of oncologists were classed as burned out [12]. Only 33% were satisfied with their work-life balance [11] and almost 30% planned to retire early [11].
Oncologists 40 years old or younger make up a significant proportion of the oncology profession. For example, in 2016, ∼40% of the European Society for Medical Oncology (ESMO), the largest European organisation for medical oncologists, were Young Oncologists (defined as <40 years of age). Reports indicate that younger age may be a risk factor for burnout [13]. Studies thus far have not specifically set out to establish burnout rates in younger oncologists. This group of oncologists is key for the future oncology workforce to deliver patient care, drive research and train the next generation of oncologists. Therefore, it is important to establish the extent of burnout in this group, whether there are inequalities in burnout rates across countries and to identify factors associated with burnout could potentially be addressed to lower the risks of burnout.
The aim of the ESMO Young Oncologists (YO) Committee survey was to investigate the burnout prevalence, work and lifestyle factors amongst European oncologists ≤40 (YOs).
Methods
An online survey was available on the ESMO website between January 2013 and January 2014. There was targeted promotion to European YOs via YO Corner on esmo.org [14], YO E-news, national YO group representatives and members of the ESMO Young Oncologist Committee. Participation was voluntary and there was no incentive to participate offered. The online survey consisted of 48 questions which included a standardized burnout instrument Maslach Burnout Inventory (MBI) [15] and additional questions exploring a range of personal and professional demographics which were agreed by the ESMO Young Oncologist Committee (Tables 1 and 2, supplementary Figure S1, available at Annals of Oncology online).
Table 1.
Participant demographics
| Number (%) | |
|---|---|
| Gender | |
| Male | 225 (38) |
| Female | 370 (62) |
| Region | |
| Eastern Europe | 74 (12) |
| Southeastern Europe | 76 (13) |
| Central Europe | 95 (16) |
| Western Europe | 93 (16) |
| Northern Europe and British Isles | 128 (22) |
| Southwestern Europe | 129 (22) |
| Trainee | |
| Yes | 308 (52) |
| No | 287 (48) |
| ESMO Member | |
| Yes | 289 (49) |
| No | 306 (51) |
| Hospital type | |
| University hospital | 295 (50) |
| Cancer centre | 185 (31) |
| General hospital | 90 (15) |
| Private clinic | 21 (4) |
| Other | 4 (1) |
Table 2.
Lifestyle and work factors
| Number (%) | |
|---|---|
| Currently in a relationship | |
| Yes | 483 (81%) |
| No | 112 (19%) |
| Has children | |
| Yes | 256 (43%) |
| No | 339 (57%) |
| Good work-life balance | |
| Yes | 223 (37%) |
| No | 373 (63%) |
| Lives alone | |
| Yes | 135 (23%) |
| No | 460 (77%) |
| Adequate vacation time | |
| Yes | 240 (40%) |
| No | 355 (60%) |
| Hospital offers support services | |
| Yes | 156 (26%) |
| No | 439 (74%) |
| Time to work (min) | |
| 0–15 | 158 (27%) |
| 15–30 | 208 (35%) |
| 30–45 | 115 (19%) |
| 45–60 | 72 (12%) |
| 60–90 | 31 (5%) |
| 90–120 | 8 (1%) |
| >120 | 3 (1%) |
Burnout was measured using the validated MBI [15] which is a 22-item questionnaire. The MBI has three subscales to evaluate each domain of burnout: EE, depersonalization and low PA. The standard scoring for health care workers was used: ≥27 on the EE subscale, ≥10 on the depersonalization (DEP) subscale, or <33 on the PA subscale is considered to have a high level of burnout in that subscale [4]. Burnout defined as high levels of EE, high levels of depersonalization or low levels of PA [16] was used to establish an overall burnout score [17–19].
Surveys included in the statistical analysis were those filled out by those who met the following criteria: 40 years or younger and live and work in Europe, including Israel and Turkey. All eligible countries were assigned to a region. Six regions were created by consensus amongst the ESMO Young Oncologist Committee, based on the United Nations regional division for Europe. The following regions were created: Eastern Europe (Belarus, Estonia, Latvia, Lithuania, Georgia, Moldova, Russian Federation, Ukraine), Southwestern Europe (Italy, Portugal, Spain), Southeastern Europe (Albania, Bosnia-Herzegovina, Bulgaria, Croatia, Cyprus, Greece, Israel, Macedonia, Montenegro, Serbia, Turkey), Central Europe (Austria, Czech Republic, Germany, Hungary, Poland, Romania, Slovakia, Slovenia, Switzerland), Western Europe (France, Belgium, Luxemburg, The Netherlands), and Northern Europe and the British Isles (Denmark, Finland, Sweden, Norway, Ireland, UK).
In order to assess the association between burnout and work/lifestyle factors, two analyses were carried out: logistic regression analysis to assess the effect of factors on the presence of burnout (yes or no) and linear regression using the overall burnout score (total of three individual subscales) as a continuous variable. The associations of the subscale (EE, DEP, PA) scores and work/lifestyle factors were assessed as continuous variables using linear regression analysis. Variables that were significantly associated with the presence of burnout or burnout/subscale scores in univariate analysis were included in the multivariable analysis. Non-parametric comparisons were done using either the Mann–Whitney or Kruskal–Wallis test. For categorical data the χ2 test was used. Results were considered statistically significant when two-tailed P-values were <0.05. A Bonferroni correction was applied to correct for multiple testing where appropriate. All statistical analyses were done using Stata v13 software (StataCorp, TX).
Results
Participant demographics
Seven hundred and thirty-seven completed surveys from 40 European Countries were submitted. Eighty-one percent (595) of the participants were ≤ 40 years old (YO). The analyses were limited to the YO group. The participants were divided into six geographical regions. The proportion of participants in each region ranged from 12% to 22% of the total number across Europe. The majority of participants were female (62%) and worked in a university hospital or cancer centre (81%). Eighty-two percent specialized in medical oncology (12% radiation oncology, 3% surgical oncology, 3% combined medical and radiation oncology). There were neither significant differences between the number of trainees (52%) and those who completed training (48%) nor between ESMO members (49%) and non-members (51%). At the time of the survey, 81% of respondents were in a relationship, 43% had children and 22% lived alone. The travel time to work was 30 min or less for the majority of participants (61.6%). The results are summarized in Tables 1 and 2.
Thirty-seven percent of YOs considered themselves as having a good work/life balance and 40% felt they had sufficient vacation time. The majority of YOs worked in organizations that did not offer psychological support services for doctors (74%). Seventy-three percent and 82% reported that they had never asked for support for distress of burnout as a trainee or post training, respectively.
Burnout rates
The overall burnout rate of European YOs was 71% (425/595). There was a significant difference in burnout rates across European regions—the highest rate were in Central Europe (84%) and Southeastern Europe (83%); lowest in Northern Europe and British Isles (52%) (Kruskal–Wallis test: P = 0.0001) (Table 3; Figure 1). Studies have also used high scores on the DEP and/or EE subscales as an indication of burnout in order to establish a burnout rate [12]. The rates using this definition were lower than when all three subscales were used (overall burnout rate 71% versus 62%; χ2 test P < 0.001; supplementary Table S1, available at Annals of Oncology online) but the difference between European regions remained.
Table 3.
Burnout and subscale rates and scores in European regions
| Region | No. of participants | Burnout rate n, % | EE rate n, % | DEP rate n, % | PA rate n, % |
|---|---|---|---|---|---|
| Eastern Europe | 74 | 54 (73.0%) | 35 (47.3%) | 44 (59.5%) | 28 (37.8%) |
| Southeastern Europe | 76 | 63 (82.9%) | 43 (56.6%) | 54 (71.1%) | 28 (36.8%) |
| Central Europe | 95 | 80 (84.2%) | 51 (53.7%) | 57 (60.0%) | 30 (31.6%) |
| Western Europe | 93 | 59 (63.4%) | 30 (32.3%) | 34 (36.6%) | 33 (35.5%) |
| Northern Europe and British Isles | 128 | 67 (52.3%) | 45 (35.2%) | 45 (35.2%) | 26 (20.3%) |
| Southwestern Europe | 129 | 102 (79.1%) | 62 (48.1%) | 66 (51.2%) | 60 (46.5%) |
| TOTAL | 595 (100%) | 425 (71.4%) | 266 (44.7%) | 300 (50.4%) | 205 (34.5%) |
| Region | No. of participants | Burnout score | EE score | DEP score | PA score |
| Eastern Europe | 74 | 71.5±16.6 | 25.6±11.7 | 11.6±6.2 | 34.3±6.8 |
| (32–110) | (2–52) | (0–25) | (20–48) | ||
| Southeastern Europe | 76 | 76.1±14.7 | 29.1±9.7 | 13.0±5.8 | 33.9±7.0 |
| (44–106) | (8–46) | (1–25) | (9–48) | ||
| Central Europe | 95 | 73.9±17.7 | 27.1±11.6 | 11.6±5.5 | 34.6±7.6 |
| (0–110) | (0–48) | (0–26) | (0–46) | ||
| Western Europe | 93 | 65±11.7 | 21.6±9.4 | 8.3±4.9 | 35.1±6.9 |
| (35–98) | (2–43) | (1–22) | (14–47) | ||
| Northern Europe and British Isles | 128 | 69.5±13.6 | 23.8±10.7 | 8.2±5.6 | 37.6±5.3 |
| (32–105) | (2–50) | (0–24) | (22–48) | ||
| Southwestern Europe | 129 | 68.1±16.2 | 25.3±11.6 | 10.2±5.9 | 32.6±7.0 |
| (29–107) | (4–54) | (0–26) | (12–47) | ||
| TOTAL | 595 | 70.3±15.5 | 25.3±11.6 | 10.2±5.9 | 34.8±6.9 |
| (0–110) | (0–54) | (0–26) | (0–48) | ||
Scores are reported as mean ± standard deviation (range).
EE, emotional exhaustion; DEP, depersonalization; PA, personal accomplishment.
Figure 1.
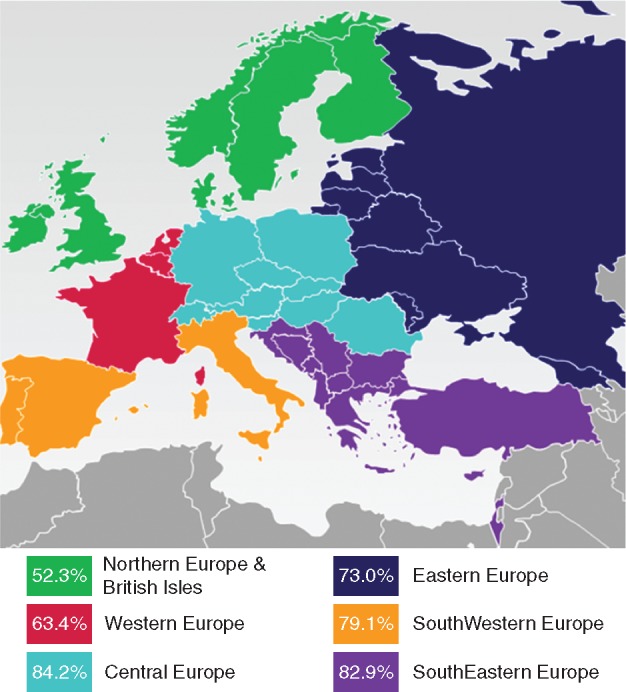
Burnout scores in European regions. Burnout rate defines as high score EE, DEP and/or low PA.
EE scores were significantly lower in Western Europe than other regions. Depersonalization, scores were lower in the British Isles & Northern Europe and Western Europe compared with other regions. Personal achievement scores were higher in the British Isles and Northern Europe region, with no differences between the other regions (Kruskal–Wallis test: P = 0.0001 for all tested parameters) (Table 3).
Factors associated with burnout
There was no significant difference in burnout prevalence between men and women (75% versus 69%, P = 0.12). However, men showed higher depersonalization scores compared with women (60% versus 45%, P < 0.001). Within YOs, there was no association with burnout rate and age although low accomplishment was found to be highest in the 26–30 age group (45% 26–30 years versus 27% 36–40, P = 0.008).
When looking at overall burnout scores, female gender (P = 0.032), having no access to support services (P < 0.0001), not having a good work-life balance (P < 0.0001), living alone (P = 0.006), not having adequate vacation time (P < 0.0001) and geographical region were all significantly associated with increased burnout scores in univariate linear regression analysis (supplementary Table S2, available at Annals of Oncology online). In the subsequent multivariable linear regression analysis, having no access to support services (P = 0.002), not having a good work-life balance (P < 0.0001), living alone (P = 0.024), not having adequate vacation time (P = 0.002) and geographical region all remained significantly associated with increased burnout scores (Table 4). EE, DEP and PA scores were all significantly affected by not having a good work-life balance (P < 0.0001). Not having access to support services (P = 0.002), not having enough vacation (P < 0.0001) and living alone (P = 0.04) showed only to negatively impact EE. In addition, DEP and PA were significantly affected by geographical regions (Table 4).
Table 4.
Multivariable linear regression analysis of overall burnout scores and subscale (EE, DEP and PA) scores
| Coefficient (95% CI); P-value |
||||
|---|---|---|---|---|
| Variable | Burnout score | EE score | DEP score | PA score |
| No access to support services | 3.32 (0.53–6.12) | 2.86 (1.01–4.71) | NS | NS |
| P<0.0020 | P=0.002 | |||
| No good work-life balance | 9.70 (7.15–12.23) | 9.50 (7.80–11.20) | 2.55 (1.55–3.55) | 2.62 (1.62–3.62) |
| P<0.0001 | P<0.0001 | P<0.0001 | P<0.0001 | |
| Not living alone | −3.17 (−5.92 to − 0.42) | −2.30 (−4.50 to 0.11) | NS | – |
| P=0.024 | P=0.040 | |||
| No adequate vacation | 4.01 (1.49–6.64) | 3.40 (1.70–5.10) | NS | NS |
| P<0.002 | P<0.0001 | |||
| Region | ||||
| Southeastern Europe | NS | NS | 3.24 (1.49–4.99) | 3.44 (1.78–5.11) |
| P<0.0001 | P<0.0001 | |||
| Central Europe | NS | NS | 2.29 (0.74–3.84) | 2.48 (0.94–4.02) |
| P=0.004 | P=0.002 | |||
| Western Europe | −6.62 (−10.39 to − 2.85) | −4.13 (−6.64 to − 1.62) | NS | NS |
| P=0.001 | P=0.001 | |||
| Eastern Europe | NS | NS | 2.33 (0.67–3.99) | 2.48 (0.81–4.41) |
| P=0.006 | P=0.004 | |||
| Southwestern Europe | −5.83 (−9.44 to 2.21) | −2.47 (4.95–0.12) | NS | NS |
| P=0.001 | P=0.051 | |||
Factors that were significant for at least one of the scores are shown.
NS, non-significant. Reference region—Northern Europe and British Isles.
Using the constant and coefficients obtained from the multivariable regression analysis, a predictive model for burnout scores was derived. For six risk factors (NS = no access to support services, WLB = having a poor work-life balance, LA = living alone, AV = not having adequate vacation time, WE = living in Western Europe, SE = living in Southwestern Europe), a score is assigned of either 0 if absent or 1 if present. This provided an estimated burnout score based on a specific risk profile.
This model significantly predicted burnout scores (P < 0.001). The model also explained a significant proportion of variance in burnout scores R2 = 0.19, F(9, 585) = 16.58, P < 0.0001.
Discussion
The findings of this study, which analysed responses from nearly 600 young oncologists from 40 European countries of which over 80% were medical oncologists, indicate that burnout is a significant, problem among oncologists. Our results show that the overall burnout prevalence amongst young oncologists is exceeding 70%, but also indicate that there is a substantial difference in burnout prevalence between the different European regions. In addition to exposing the geographical differences in burnout, work/life balance, access to support services, living alone and vacation time were identified as being key factors that contribute to burnout in this study. These results are of importance as identification of these factors could play a pivotal role in strategies on prevention of burnout. The implications of the variation in burnout rates across Europe are that measures to combat burnout may need to be tailored to the individual needs of a region as well as more universal strategies. The specific reasons for European regional variation are not entirely clear from this survey and are an area to be explored further in the future.
The high prevalence of burnout found in the European study exceeds the results of a similar study conducted among US oncologists by Shanafelt et al. [12]. Here, the authors reported a 45% prevalence of burnout. Of note, the median age of responders was 52 years and 5.8% were < 40 years old. In another survey of US oncology fellows in training, the burnout rate was 34% [6]. Similar burnout rates have been reported by Blanchard et al. in oncology residents in France [20].
A potential factor contributing to the higher burnout rates in the ESMO burnout survey and those carried out earlier is the fact that burnout rates are actually increasing over time. In 2015, Medscape published the result from its annual Medscape Physician Lifestyle Report, in which burnout was shown to affect around 46% of all respondents [5] compared with just under 40% in 2013 [18]. Another survey of 35 922 physicians showed an increase from 46% in 2011 to 54% in 2014 [19]. It is noteworthy that in the same survey, minimal change in the burnout rate was observed over the same time period in probability-based samples of working US adults [19].
Methodological differences could influence reported burnout rates. There has been some controversy in the literature over the best tools to measure burnout and which components of the MBI are to be included [12]. Both studies conducted by Shanafelt [12] and Blanchard [20] used the MBI, however, two components (DEP and EE) were used to class burnout, whereas all three were used in the ESMO survey. The burnout rates were also calculated using the definition incorporating two components and although the overall rate was lower (71% versus 62%), it remained a high burnout rate and the differences across European regions were also noted.
In this survey, there was a higher proportion of female participants than male but there was no difference in burnout rates between men and women. However, interestingly, depersonalization rates were significantly higher in men. It is perhaps not surprising that work/life balance, vacation time and travel time to work were factors significantly associated with burnout. Whilst geographical region may be more challenging to address, the above lifestyle factors related to work are areas that can be adapted. Cultural differences between countries towards work/life balance are likely to be a factor affecting burnout and is worth further study.
A limitation of this survey is that the number of participants varied between countries and therefore countries were grouped geographically before the analysis in order to have adequate participants in the regions. Another point is that the proportion of participants in relation to the total number of young oncologists in Europe is not known. This is by nature of the method of distribution of the survey and therefore there is the potential of bias amongst those that participated. Of note, there was an equal proportion of ESMO members and non-members that took part. In the USA, Danish and French burnout surveys, between 50% and 67% of the total number of oncologists responded [12, 20, 21]. Regardless of the proportion of responders, the number of YO’s was high and the survey revealed that a significant number of oncologists under 40 within Europe are considered to have burnout. These include trainees and practicing oncologists within the early years post-training.
There are serious consequences from burnout in young oncologists for the oncology profession and ultimately care of cancer patients. In a 2011 Medscape report, 79% oncologists would choose oncology again as their specialty, but in 2015, this number dropped drastically to 51% [22]. These findings emphasise the need for strategies to enhance job satisfaction and maintain oncology as a rewarding profession throughout one’s career. There are also potential serious personal sequelae of burnout such as anxiety, depression and suicide which have been reviewed elsewhere [8]. It is important to recognise that the presence of burnout itself is not a psychiatric disease. However, burnout may be associated with depression and suicidal ideation [7]. The ESMO Young Oncologist Committee survey did not assess suicidal ideation or symptoms of depression.
An important step is to enhance the awareness of the need for self-care strategies. In 2009, Wallace et al. discussed how the well-being of physicians directly affects the performance of healthcare systems and even proposes that physician well-being should be routinely measured as an integral part of health care quality assessments [23]. Interventions on prevention and management of burnout need to be initiated on multiple levels: individual, family, hospitals/institutions, and professional societies all have roles and responsibilities.
A recent study of residents across specialities in a tertiary academic hospital reported a burnout rate of 69% and concluded that although residents acknowledge that work-life balance contributes to burnout, they are reluctant to seek help. Interestingly, program directors underestimated the burnout rate [24]. Interventions that alter this attitude are urgently needed, as are strategies to cope with the inherent difficulties that specifically arise in the field of medical oncology. Ideally, basic stress management skills should be acquired in medical school with job specific skills implemented later in specialty training.
This was the largest survey of Young Oncologists (majority medical oncologists) conducted on a pan-European level. It shows that burnout is not a phenomenon which is limited to oncologists who have been practicing for many years. This has important implications as burnout is a gradual process that can develop and last over time. Therefore, it is critical that measures addressing burnout are widely available throughout one’s career, and as with any disease, early recognition and treatment is essential. A significant step in tackling burnout is the awareness of the extent of the problem in the oncology profession. It is encouraging that over the last couple of years, since the reports of burnout in US oncologists and the presentation of the preliminary results of the European burnout survey, international congresses such as ASCO, the European Cancer Organisation (ECCO) and ESMO have included sessions related to burnout and work/life balance. This will help fuel the impetus for local, national and international organizations to invest in measures to reduce burnout. More and more initiatives are being created to make oncology an attractive profession for young doctors [25] as this is vital to ensure the highest quality of oncologists in the short and long-term so that the care of cancer patients is not compromised. It is unlikely that there will be a ‘one size fits all’ solution for burnout. A range of strategies which may change at different times over one’s career is necessary. The next step is to focus on implementing burnout prevention and management methods accessible to young oncologists and beyond.
Supplementary Material
Acknowledgements
The authors would like to thank all participants for taking part and national societies and organizations who helped distribute the survey. They also thank Katharine Fumasoli, Lone Kristoffersen and Marina Cogo for their support from ESMO Head Office. SB also personally acknowledges the Association of Cancer Physicians, UK and the National Institute for Health Research (NIHR) Royal Marsden/ICR Biomedical Research Centre.
Funding
ESMO: For license to use MBI and publication of figure fee.
Disclosure
The authors have declared no conflicts of interest.
References
- 1. Whippen DA, Canellos GP.. Burnout syndrome in the practice of oncology: results of a random survey of 1,000 oncologists. J Clin Oncol 1991; 9(10): 1916–1920. [DOI] [PubMed] [Google Scholar]
- 2. Campbell DA, Sonnad SS, Eckhauser FE. et al. Burnout among American surgeons. Surgery 2001; 130(4): 696–702–5. [DOI] [PubMed] [Google Scholar]
- 3. Golin M. Physician burnout: when the healer is wounded. Am Med News 1981; 24(29): suppl 1–suppl 2. http://www.ncbi.nlm.nih.gov/pubmed/10252614. Accessed December 13, 2016. [PubMed] [Google Scholar]
- 4. Shanafelt TD, Boone S, Tan L. et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 2012; 172(18): 1377–1385. [DOI] [PubMed] [Google Scholar]
- 5. Medscape 2015 Physician Lifestyle Report. www.medscape.com/sites/public/lifestyle/2015 (14 February 2017, date last accessed).
- 6. Shanafelt TD, Raymond M, Horn L. et al. Oncology fellows’ career plans, expectations, and well-being: do fellows know what they are getting into? J Clin Oncol 2014; 32(27): 2991–2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dyrbye LN1, Thomas MR, Massie FS. et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med 2008; 149(5): 334–341. [DOI] [PubMed] [Google Scholar]
- 8. Shanafelt T, Dyrbye L.. Oncologist burnout: causes, consequences, and responses. J Clin Oncol 2012; 30(11): 1235–1241. [DOI] [PubMed] [Google Scholar]
- 9. Shanafelt TD, Balch CM, Bechamps G. et al. Burnout and medical errors among American surgeons. Ann Surg 2010; 251(6): 995–1000. [DOI] [PubMed] [Google Scholar]
- 10. Dyrbye LN, Massie FS, Eacker A. et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA 2010; 304(11): 1173–1180. [DOI] [PubMed] [Google Scholar]
- 11. Shanafelt TD, Raymond M, Kosty M. et al. Satisfaction with work-life balance and the career and retirement plans of US oncologists. J Clin Oncol 2014; 32(11): 1127–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shanafelt TD, Gradishar WJ, Kosty M. et al. Burnout and career satisfaction among US oncologists. J Clin Oncol 2014; 32(7): 678–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Amoafo E, Hanbali N, Patel A, Singh P.. What are the significant factors associated with burnout in doctors? Occup Med (Lond) 2015; 65(2): 117–121. [DOI] [PubMed] [Google Scholar]
- 14. Welcome to the Young Oncologists Corner | ESMO. http://www.esmo.org/Career-Development/Young-Oncologists-Corner (13 December 2016, date last accessed).
- 15. Maslach C, Jackson S, Leiter M.. Maslach Burnout Inventory Manual, 3rd edition Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 16. Grunfeld E, Whelan TJ, Zitzelsberger L. et al. Cancer care workers in Ontario: prevalence of burnout, job stress and job satisfaction. CMAJ 2000; 163(2): 166–169. [PMC free article] [PubMed] [Google Scholar]
- 17. Glasberg J, Horiuti L, Novais MA. et al. Prevalence of the burnout syndrome among Brazilian medical oncologists. Rev Assoc Med Bras (1992) 2007; 53(1): 85–89. [DOI] [PubMed] [Google Scholar]
- 18. Medscape 2013 Physician Lifestyle Report. www.medscape.com/sites/public/lifestyle/2013 (7 February 2017, date last accessed).
- 19. Shanafelt TD, Hasan O, Dyrbye LN. et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015; 90(12): 1600–1613. [DOI] [PubMed] [Google Scholar]
- 20. Blanchard P, Truchot D, Albiges-Sauvin L. et al. Prevalence and causes of burnout amongst oncology residents: a comprehensive nationwide cross-sectional study. Eur J Cancer 2010; 46(15): 2708–2715. [DOI] [PubMed] [Google Scholar]
- 21. Andreassen CN, Eriksen JG.. The psychosocial work environment among physicians employed at Danish oncology departments in 2009. A nationwide cross-sectional study. Acta Oncol 2013; 52(1): 138–146. [DOI] [PubMed] [Google Scholar]
- 22. Medscape Oncologist Compensation Report 2015 www.medscape.com/features/slideshow/compensation/2015/oncology (1 December 2016, date last accessed).
- 23. Wallace JE, Lemaire JB, Ghali WA.. Physician wellness: a missing quality indicator. Lancet 2009; 374(9702): 1714–1721. [DOI] [PubMed] [Google Scholar]
- 24. Holmes EG, Connolly A, Putnam KT.. Taking care of our own: a multispecialty study of resident and program director perspectives on contributors to burnout and potential interventions. Acad Psychiatry 2017; 41(2): 159–166. [DOI] [PubMed] [Google Scholar]
- 25. Morgan G, Lambertini M, Kourie HR. et al. Career opportunities and benefits for young oncologists in the European Society for Medical Oncology (ESMO). ESMO Open 2016; 1(6): e000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


