Abstract
We are in the midst of a digital revolution in health care, although the application of new and useful technology in routine clinical practice is variable. The Characterizing Atrial fibrillation by Translating its Causes into Health Modifiers in the Elderly (CATCH ME) Consortium, in collaboration with the European Society of Cardiology (ESC), has funded the creation of two applications (apps) in atrial fibrillation (AF) for use in smartphones and tablets. The patient app aims to enhance patient education, improve communication between patients and health care professionals, and encourage active patient involvement in the management of their condition. The health care professional app is designed as an interactive management tool incorporating the new ESC Practice Guidelines on AF and supported by the European Heart Rhythm Association (EHRA), with the aim of improving best practice approaches for the care of patients with AF. Both stand-alone apps are now freely available for Android and iOS devices though the Google Play, Amazon, and Apple stores. In this article, we outline the rationale for the design and implementation of these apps. Our objective is to demonstrate the value of integrating novel digital technology into clinical practice, with the potential for patient engagement, optimization of pharmacological and interventional therapy in AF, and ultimately to improve patient outcomes.
Keywords: Atrial fibrillation, Smartphone, Mobile, Application, App, Education, Management, Treatment, Guidelines
What’s new?
The 2016 European Society of Cardiology (ESC) Guidelines on atrial fibrillation (AF) recommend patient-centred care and an integrated, multidisciplinary treatment approach.
Smartphone and tablet apps can provide education, encourage behaviour change, and increase treatment adherence in patients as well as deliver interactive treatment algorithms to aid clinicians.
The patient app aims to enhance patient education on AF, self-management, and shared decision-making.
The health care professional app is designed around the 2016 ESC Guidelines on AF to simplify the choice of treatment and optimize guideline adherence.
Introduction
Smartphones, tablet computers, and their applications (apps) have become ubiquitous in modern life all across the world. In Europe and North America, approximately two-thirds of the population own mobile devices, with year-on-year increases. Their role in our lives has continually changed, and for many people, smartphones and tablets are the primary method for communication and accessing online information. Although lagging behind social networking, the popularity of interactive health communication applications is growing, not only to provide health information but also to combine education with the goal of behaviour change.1 Better patient understanding has the potential to improve health outcomes.2 In patients with heart disease, education allows better appreciation of individual risk and facilitates commencement of and compliance with treatment.3 The use of computer or web-based patient tools appears to have positive effects across a range of outcomes, including patient knowledge, behaviour, and even clinical outcomes (e.g. improved diabetic control or less disability from asthma).4 On the other side of the consultation, there are many medical apps available to assist doctors, although few, to-date, have been specifically written by and for clinicians.5
Atrial fibrillation (AF) is the most common heart rhythm disorder and poses a considerable burden to health care services, with rising incidence and prevalence, and high rates of morbidity and mortality.6 Aside from the prognostic benefit of oral anticoagulation therapy and management of cardiovascular risk, treatment of AF is targeted towards the relief of symptoms, including the control of heart rate and rhythm.7 Adherence to long-term therapy is of particular importance, supported by a multidisciplinary team that includes primary care practitioners, cardiologists, electrophysiologists, stroke physicians, allied health professionals, and support staff. Management of AF is therefore uniquely suited to a process of shared decision-making,8 to support the patients’ understanding of the disease and available therapies.9 Patient education can improve anticoagulation control in AF patients,10 and integrated AF management is a cost-effective means of reducing unnecessary hospital admissions and adverse clinical outcomes.11,12 From the perspective of health care professionals, adherence to clinical practice guidelines have been shown to improve prognosis in patients with AF.13–15
In concert with the 2016 European Society of Cardiology (ESC) Guidelines on AF,7 we are launching mobile applications for patients with AF and their health care professionals (Figure 1). The patient app aims to enhance patient education, optimize communication between patients and health care providers, increase patient involvement in management decisions, and encourage self-management activities. The health care professional app is designed to interactively apply the new ESC AF Guidelines to individual patients, facilitating the adoption of best practice management of AF, with the aim of improving patient outcomes.
Figure 1.

QR scan codes—download the apps now! Scan these codes to download the apps (iOS or Android).
Rationale
The patient and health care professional apps for AF were developed to disseminate the new 2016 ESC AF Guidelines through different formats to reach a wide and expanding audience. Our approach had three main foundations that are discussed in detail below:
(i) Apps in other health care settings have had a positive impact on patient behaviour and clinical outcomes; (ii) digital learning in the context of educational theory affords a new pathway of providing supportive patient education; and (iii) education of health care professionals and encouraging guideline-adherent care can contribute to enhanced professional standards and improved management of patients with AF.
Evidence from other health care apps
The impact of health-related apps have been studied in numerous randomized controlled trials. During our design phase, we performed a keyword search of PubMed and Google Scholar to identify apps with published health outcomes (April 2016; search terms apps/mobile and randomized) and summarize some key trials here. An app providing cognitive behavioural therapy skills demonstrated reduced symptoms of depression and less work absence compared with those randomized to website support (n = 300).16 In 597 adults with back pain, a mobile app successfully encouraged self-management skills, leading to a reduction in back pain at 4 months.17 A web-based app on healthy lifestyle interventions had a positive impact on physical activity over 14 weeks in 56 participants compared with 29 controls (63 ± 21 min vs. −30 ± 28 min; P = 0.02), leading to more weight loss and higher success in maintaining a healthy lifestyle. The frequency of app use was significantly related to a higher success score.18 Short-term benefits over an 8-week period were also seen with an app that encouraged physical activity using social networking (n = 110).19 In patients at risk of diabetes, a combined mobile app and pedometer increased physical activity, reduced blood pressure, and improved dietary intake in 30 patients compared with 31 controls.20 However, in another randomized trial, a mobile phone app was unable to elicit any improvement in physical activity at 8 weeks (n = 51).21 An app designed to improve adherence to medications in elderly patients led to fewer missed doses compared with the controls (n = 48 and 51, respectively), and 88% of those using the app felt more independent in managing their therapy.22
The studies discussed earlier have important limitations, including highly motivated and selected populations, and only short-term evaluation. A systematic review of mobile health interventions suggests a benefit from various types of intervention but also a clear need for further robust evidence.23
Context of educational theory
Learning theories have progressed from purely behaviourist (passive learning in response to external stimuli; e.g. Pavlov’s conditioning), through cognitivist learning (internalization of knowledge), and more recently constructivist models (learning through the experience of knowledge).24,25 These theories have formed the basis for optimal teaching methods during the last century26; however, the availability of new technology has the potential to embed digital-aided learning within routine clinical practice.27 Although access to information and technology systems has increased exponentially, the corresponding levels of use within education remains modest.28 There are also important limitations that can impede digital learning, such as language, culture, and baseline knowledge, as well as app functionality and readability.29–31
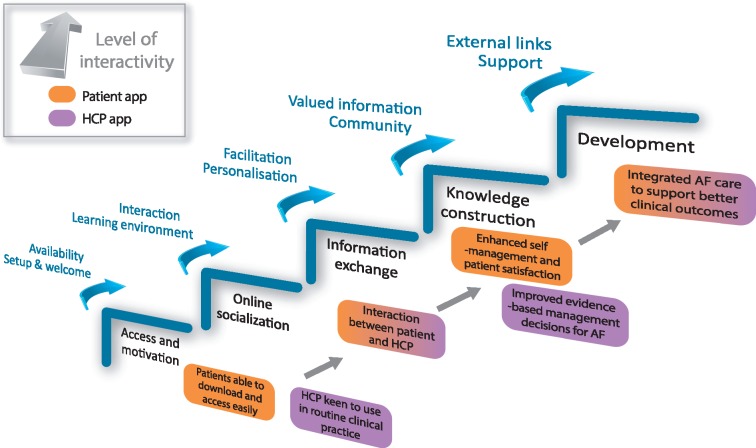
So what are the theoretical implications for app development to assist patients with AF? Figure 2 adapts Salmon’s five-stage model of online learning32 to illustrate the key points of a structured developmental process. These can lead to patient enablement (provision of appropriate context for new knowledge and skills)33 and, hence, supported and successful learning (as described by Vygotsky’s Zone of Development).34 Reflecting on the learning classification described by Bloom,35 users start to understand new concepts and apply knowledge to their own circumstances. One of the aims of our app is to allow independent patient evaluation of treatment options, enabling an informed choice and partnership-in-care between patients and their health care providers. Such a model has the potential to encourage satisfaction with treatment, increase self-management, reduce cost, and improve patient well-being.
Figure 2.
Learning framework applied to the AF apps. Process and facilitation of online learning associated with smartphone applications for AF. Adapted from the five-stage model as proposed by Salmon (2013).32 AF, atrial fibrillation; HCP, health care professional.
Context of professional standards
Physician education
Professional standards frameworks across Europe highlight the importance of ongoing education. In this context, mobile applications are an important part of integrating and internalizing knowledge as well as transmitting this learning to others.36–39 The general direction of technology suggests that mobile applications will become an increasingly important method to improve and maintain professional standards in health care.40
Physician interaction with patients
The active participation of patients in health care consultations and development of patient autonomy is a principle common to professional standards across the world.41 This includes the Physician Charter,42 adopted by the European Federation of Internal Medicine, the American Board of Internal Medicine, and the American College of Physicians, as well as standards of the UK General Medical Council.39 The CanMEDS code of the Royal College of Physicians and Surgeons of Canada puts a responsibility on physicians to facilitate patient learning, not only by educating patients but also by promoting health literacy for the purposes of ‘establishing rapport and trust, formulating a diagnosis, delivering information, striving for mutual understanding, and facilitating a shared plan of care’.43 Similarly, the Core Curriculum for General Cardiologists of the ESC and the Core Curriculum for Nurses of the ESC Council for Cardiovascular Nursing and Allied Professions recognize the importance of patient education in all areas of cardiac care.44,45
Design
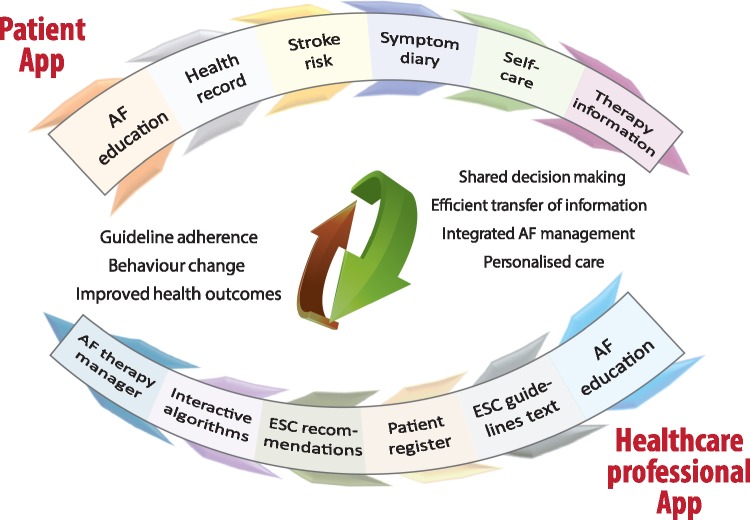
App design was led by a core group (see Supplementary material online, Appendix 1) comprising of representatives from the Characterizing Atrial fibrillation by Translating its Causes into Health Modifiers in the Elderly (CATCH ME) Consortium, the ESC Guidelines Task Force on AF, and the European Heart Rhythm Association (EHRA). Börm Bruckmeier Publishing (Germany) was commissioned to produce the apps. The main components and objectives of the app development programme are displayed in Figure 3.
Figure 3.
Components and objectives of the app development programme. AF, atrial fibrillation; ESC, European Society of Cardiology.
In brief, we developed the apps in tandem with the writing of the 2016 ESC Guidelines on AF while maintaining the confidentiality of the guidelines. The Task Force writing the guidelines were instrumental in defining the content of the apps. The guideline flowcharts for different sections of AF management determined the design of the apps. This process began in October 2014, an outline of the app functionalities was completed in October 2015, and the final guideline structure was incorporated into the Apps Software Requirements Specification by February 2016. Model View Presenter Framework (Android) and Model View Controller (iOS) were used, with the overall product based on Client Server Architecture. The apps were publicly released at the ESC Congress in Barcelona (August 2017). As the Healthcare Professional app determines patient treatment, a CE (Conformité Européene) certification application has been submitted to conform with European Commission Directives (Class IIa medical device).
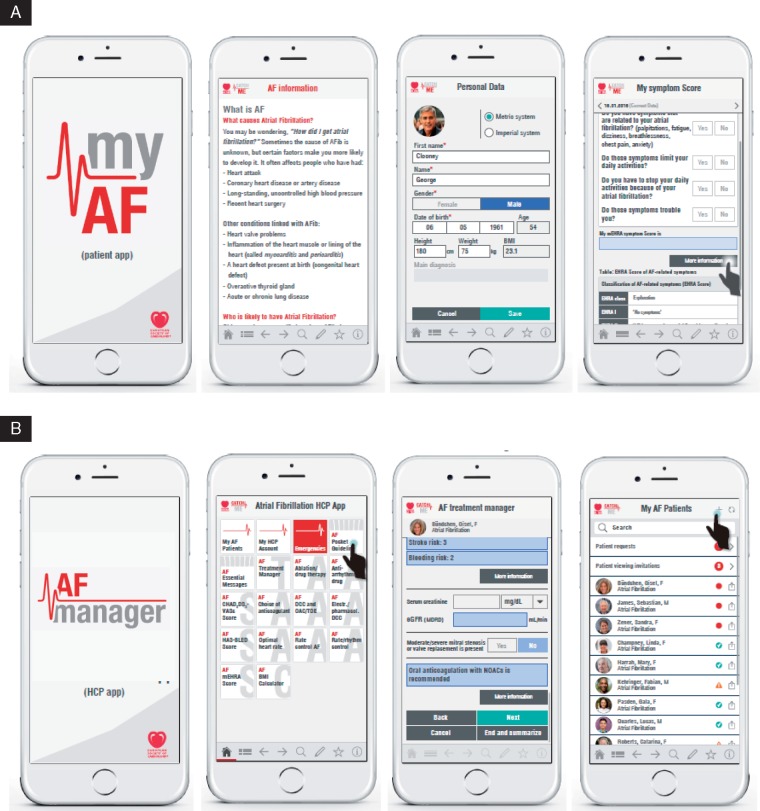
Patient app
The patient app provides education on AF, including sections describing the pathology, symptoms, prognosis, associated comorbidities, management strategies, and practical tips for self-care (Figure 4A). Information was derived from existing patient documentation developed by the British Heart Foundation (https://www.bhf.org.uk/), the German National Network of Competence in Atrial Fibrillation (AFNET; http://www.kompetenznetz-vorhofflimmern.de/), and a patient booklet on AF developed in the Netherlands.46 The text was then edited by a team of patient representatives with AF (funded through a UK National Institute of Health Research grant on improving patient outcomes in AF).47 The patient app will also present information on individual stroke risk and provide a personal health record and symptom diary. Patients are asked to fill in sections about relevant previous health issues, which can facilitate consultation when shared with their health care professional(s).
Figure 4.
Screenshots of the patient app (A) and the health care professional app (B). Both apps available free of charge for Android and iOS through the Google Play, Amazon, and Apple stores. The standalone AF treatment manager can also be accessed through the ESC Pocket Guidelines app (AF section). All names displayed in the figure are fictitious.
Healthcare Professional app
The Healthcare Professional app is a more complex tool, allowing both conventional viewing of guideline text and recommendations and interactive treatment algorithms (Figure 4B). The app is also designed to improve consultation efficiency, with the provision of a patient register, pre-filled with data supplied by the patient. A tablet version of the app will also be available, allowing overview of multiple patients (e.g. in an outpatient clinic setting). Users are able to launch the AF Treatment Manager directly through the existing ESC Pocket Guidelines app, also available free of charge for iOS and Android devices through their respective stores.
Patient to doctor communication, security, and privacy
A key feature of the apps is communication between consenting patients and their health care professional(s). Patients will be able to securely share their data through a cloud server, permitting health care professionals to import relevant information into the Healthcare Professional app (such as symptoms, stroke risk factors, and medications). The patient can disable this access at any time. All shared information is encrypted and password protected. Reciprocally, the health care professional can also share collated information with the patient, in the form of an automated email.
Potential for observational research
For patients who specifically consent to the use of data for research purposes, anonymized data will be saved for future exploration of symptomatology, treatment patterns, and guideline adherence. This is an unparalleled capability, allowing us to collate information on patients with AF across all communities, including primary practice and hospital clinics. Understanding the barriers to effective guideline implementation will help to improve future guidelines on AF and make them more relevant to patient care.
Evaluation
Evaluation of the apps is essential to determine their ability to provide knowledge to patients and health care professionals and their impact on guideline adherence. This is an ongoing process, and feedback will drive the further development of these tools.
The process of initial testing and evaluation was as follows:
Appraisal by members of the ESC AF Guidelines Task Force to ensure that content for both patient and health care apps followed guideline recommendations.
In-house testing of individual components by the app development team, including at least fortnightly confidential teleconferencing updates during the finalization of the 2016 ESC AF Guidelines.
Initial evaluation was centred around interface design, technology, and acceptability, using published scales that help evaluate health care smartphone applications (see Supplementary material online, Appendix 2).48,49
Discussions and protocol development for patient data protection, data storage, and security.
Patient-facing materials (educational text and images) were designed and reviewed by a patient involvement team and representatives of the British Heart Foundation.
Testing of each app in entirety by the app development team to identify programming errors and inconsistencies.
Confidential testing and design enhancement by the wider ESC AF Guidelines Task Force, members of the CATCH ME consortium and EHRA to improve app functionality.
Beta-testing using self-contained devices within user cohorts to ensure acceptable language, ease of use, and clinical utility. The apps were tested by a group of CATCH ME investigators and junior and senior clinicians at the CATCH ME clinical centres on three occasions throughout 2016. Further testing regarding content and usability was carried out during the AFNET/EHRA Consensus Conference (January 2017) by AF clinicians and specialists.
Updates following beta-testing and finalization of app design. Beta-testing was performed by 67 persons (iOS and Android, both patient and health care professional apps), with feedback leading to new test versions. In total, there were 50 test versions of the apps, with step-wise iterations leading to better functionality.
Post-publication feedback
As surveying users can often be biased, the apps will include an anonymous feedback option for comment on features that work or do not work well. Although web-based surveys also suffer from sampling biases, they do allow more self-disclosure50 and are likely to be a more useful tool for evaluation and subsequent app modification.
Discussion
The development of smartphone and tablet apps for patients and health care professionals is an exciting opportunity to increase active patient involvement in the management of their AF, provide education to patients and health care professionals, and potentially improve clinical outcomes through the pursuit of guideline-adherent care. This approach is well suited to provide structured and integrated management of AF, as recommended in the 2016 ESC AF Guidelines.7
As discussed above, there is a good rationale behind the development of apps in AF, including evidence from other health care applications showing improvement in patient management.51 The apps also provide a new method to support patient empowerment through education as well as easily accessible ‘on-the-job’ health care professional training. The ability of the apps to enhance learning is based on a number of educational theories that offer users not only knowledge from evidence-based guidelines but also the application and reinforcement of this information within a digital platform. The health care professional app also addresses a number of key professional standards for the development of good clinical practice with regard to continued professional development and establishing an integrated, patient-centred approach to care. The long-term management of chronic conditions like AF is likely to benefit from informed and autonomous patients,52,53 potentially leading to better outcomes through shared decision-making.8,54,55 Although patient information is now widely available through written and verbal information, there remains a lack of specific knowledge related to AF.56–58 Currently available education tools are almost entirely focused on anticoagulation therapy,10,59–61 and although of clear clinical importance, this may not match what patients want and need to know about AF in general.62,63 The huge advantage of our app-based tools are the dynamic nature of the technology, allowing us to add and modify features or information sources in response to user feedback and reflecting future updates of the ESC AF guidelines.
App-based interventions are a relatively new method of education in health care; however, there is a large body of evidence for online learning in the teaching profession. In a systematic review of 99 studies, face-to-face and online learning methods were examined in a variety of topics for undergraduate and postgraduate learners. Effect sizes were largest for the combination of face-to-face and online instruction compared with either separately, and online working was more efficient if directed or collaborative rather than independent student learning.64 To extrapolate to the use of medical apps, this reinforces the need for the patient app to be part of the clinical experience, underpinned by the standard educational approach from health care professionals. Similarly, the Healthcare Professional app should be used in the context of ongoing professional development to achieve improvements in clinical management. New innovations usually go through a peak and trough of usage (the so-called ‘hype cycle’), and the design group were therefore keen to ensure that the apps retain relevance and functionality over time by including the means for continual update and improvement. The rapid rate of change in technology itself creates a number of issues related to access, ethical process, and privacy. However, as the general public move towards greater acceptance (and reliance) on mobile platforms, the medical community have an opportunity to use these advances to improve patient care.
Limitations
There are limitations to our approach, most notably that not all patients and health care professionals will have access to smartphones or tablets. However, recent data from the USA suggest that even in adults over the age of 65, internet use is increasing exponentially and that around 70% now own a mobile phone (although smartphones in this age group are still less common).65 The main barriers to smartphone use in older patients appears to be related to lack of perceived knowledge around the technology and visual impairment.66 Both of these issues were considered during the design phase of the apps, with the use of ‘patient-approved’ education materials, simple functionality, straightforward layout, and readable font size.
Finally, although digital forms of learning are increasing and may provide benefit,67 there is a tendency to overvalue the use of technology.68 Put simply, we should ensure that the time spent in learning and using a new resource is time and cost-efficient, with sustained value over any short-term (or gimmick) objectives. Our aim was to achieve good productivity of both the patient and health care professional apps, and for usage to increase over time, while accepting that our initial designs are likely to need ongoing improvements in response to the changing requirements of patients with AF and their health care providers.
Conclusions and clinical perspective
We have outlined the rationale for new smartphone and tablet applications for patients with AF and their health care professionals, reviewing the evidence for improving patient outcomes, enhancing professional standards, and supporting the use of digital learning. Our clinical aim is to increase patient engagement and guideline adherence with AF management and, ultimately, improve patient well-being and long-term prognosis. The apps are freely available for Android and iOS devices.
Supplementary material
Supplementary material is available at Europace online.
Supplementary Material
Acknowledgements
We would like to thank Marios Hadjianastasis for guidance on digital learning (Centre for Learning and Academic Development, University of Birmingham) and the British Heart Foundation for assistance with the patient education material.
Conflict of interest: D.K. reports non-financial support from Daiichi Sankyo, grants from Menarini, lecture fees from AtriCure, all outside the submitted work; and Lead for the Beta-blockers in Heart Failure Collaborative Group (BB-meta-HF) and RAte control Therapy Evaluation in Atrial Fibrillation (RATE-AF) Trial. L.F. reports grants from EU Horizon 2020 (CATCH ME) during the conduct of the study; grants from DFG (Deutsche Forschungsgemeinschaft), grants from Medical Research Council, grants from British Heart Foundation, grants from Gilead, all outside the submitted work; in addition, L.F. has a patent for Personalised AF Therapy (GB1404998.5) and Markers for AF (GB1413081.9) issued to the University of Birmingham. B.C. reports a grant from EU Horizon 2020 (CATCH ME) during the conduct of the study; grants from British Heart Foundation and one un-restricted grant from Astra-Zeneca, outside the submitted work. U.S. reports grants from the European Union, during the conduct of the study; personal fees from Roche Diagnostics, non-financial support from Bayer Healthcare, grants and non-financial support from Medtronic, grants from Netherlands Heart Foundation, grants from Netherlands Genomics Initiative, all outside the submitted work; in addition, U.S. has a patent for Non-invasive Classification of AF issued. P.K. reports consulting fees, honoraria and research grants from 3M Medica, MEDA Pharma, AstraZeneca, Bayer Healthcare, Biosense Webster, Boehringer Ingelheim, Bristol-Myers Squibb, Cardiovascular Therapeutics, Daiichi-Sankyo, German Cardiac Society – Akademie, Johnson & Johnson, Medtronic, Merck, MSD, OMRON, Otsuka Pharma, Pfizer, Sanofi, St. Jude Medical, Servier, Siemens, TAKEDA, German Federal Ministry for Education and Research (BMBF), Fondation Leducq, German Research Foundation (DFG), British Heart Foundation, Medical Research Council UK, all outside the submitted work; grants from EU Horizon 2020 (CATCH ME) during the conduct of the study; in addition, P.K. is listed as an inventor on two patent applications submitted by University of Birmingham on Atrial Fibrillation Therapy (GB1404998.5) and Markers for AF (GB1413081.9). P.V. reports research grants from Parexel International, speaker fees from Menarini and Servier, and consultancy fees from AFEA and Dean Medicus. H.H. has received lecture and consultancy fees from Daiichi-Sankyo, Bayer, Boehringer-Ingelheim, BMS, Pfizer, CMGRP Ltd, Downtown Europe, the Flemish Organisation of Sports Physicians and PSL Group Educational Services; research grants from Bayer (through Hasselt University) and Bracco Imaging, Medtronic and Boston Scientific (through the University of Antwerp). W.C., J.H., and V.D. have nothing to declare.
Funding
The smartphone and tablet applications have been funded by the CATCH ME Consortium (EU Horizon 2020 Grant 633196) and the European Society of Cardiology. D.K. is supported by a National Institute of Health Research (NIHR) Career Development Fellowship (CDF-2015-08-074). L.F. has received institutional support from DFG, MRC, the EU, and Gilead. J.H. is supported by a Post-Doctoral Fellowship from the Heart Foundation of Australia. U.S. is supported by a grant from the Netherlands Heart Foundation (CVON2014–09, RACE V). B.C. research is supported by the British Heart Foundation and the European Union. The opinions expressed in this paper are those of the authors and do not represent any of these funders.
References
- 1. Eng TR, Gustafson DH, Henderson J, Jimison H, Patrick K.. Introduction to evaluation of interactive health communication applications. Science Panel on Interactive Communication and Health. Am J Prev Med 1999;16:10–5. [DOI] [PubMed] [Google Scholar]
- 2. Adams RJ. Improving health outcomes with better patient understanding and education. Risk Manag Healthc Policy 2010;3:61–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sheridan SL, Viera AJ, Krantz MJ, Ice CL, Steinman LE, Peters KE. et al. The effect of giving global coronary risk information to adults: a systematic review. Arch Intern Med 2010;170:230–9. [DOI] [PubMed] [Google Scholar]
- 4. Murray E, Burns J, See TS, Lai R, Nazareth I.. Interactive Health Communication Applications for people with chronic disease. Cochrane Database Syst Rev 2005;CD004274. [DOI] [PubMed] [Google Scholar]
- 5. Edlin JC, Deshpande RP.. Caveats of smartphone applications for the cardiothoracic trainee. J Thorac Cardiovasc Surg 2013;146:1321–6. [DOI] [PubMed] [Google Scholar]
- 6. Lane DA, Skjoth F, Lip GYH, Larsen TB, Kotecha D.. Temporal trends in incidence, prevalence, and mortality of atrial fibrillation in primary care. J Am Heart Assoc 2017;6:e005155.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B. et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace 2016;18:1609–78. [DOI] [PubMed] [Google Scholar]
- 8. Seaburg L, Hess EP, Coylewright M, Ting HH, McLeod CJ, Montori VM.. Shared decision making in atrial fibrillation: where we are and where we should be going. Circulation 2014;129:704–10. [DOI] [PubMed] [Google Scholar]
- 9. Lane DA, Aguinaga L, Blomstrom-Lundqvist C, Boriani G, Dan GA, Hills MT. et al. Cardiac tachyarrhythmias and patient values and preferences for their management: the European Heart Rhythm Association (EHRA) consensus document endorsed by the Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulacion Cardiaca y Electrofisiologia (SOLEACE). Europace 2015;17:1747–69. [DOI] [PubMed] [Google Scholar]
- 10. Clarkesmith DE, Pattison HM, Lip GYH, Lane DA, ten Cate H.. Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS One 2013;8:e74037.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hendriks JML, de Wit R, Crijns HJGM, Vrijhoef HJM, Prins MH, Pisters R. et al. Nurse-led care vs. usual care for patients with atrial fibrillation: results of a randomized trial of integrated chronic care vs. routine clinical care in ambulatory patients with atrial fibrillation. Eur Heart J 2012;33:2692–9. [DOI] [PubMed] [Google Scholar]
- 12. Hendriks J, Tomini F, van Asselt T, Crijns H, Vrijhoef H.. Cost-effectiveness of a specialized atrial fibrillation clinic vs. usual care in patients with atrial fibrillation. Europace 2013;15:1128–35. [DOI] [PubMed] [Google Scholar]
- 13. Nieuwlaat R, Olsson SB, Lip GY, Camm AJ, Breithardt G, Capucci A. et al. Guideline-adherent antithrombotic treatment is associated with improved outcomes compared with undertreatment in high-risk patients with atrial fibrillation. The Euro Heart Survey on Atrial Fibrillation. Am Heart J 2007;153:1006–12. [DOI] [PubMed] [Google Scholar]
- 14. Qin D, Leef G, Alam MB, Rattan R, Munir MB, Patel D. et al. Patient outcomes according to adherence to treatment guidelines for rhythm control of atrial fibrillation. J Am Heart Assoc 2015;4:e001793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lip GY, Laroche C, Popescu MI, Rasmussen LH, Vitali-Serdoz L, Dan GA. et al. Improved outcomes with European Society of Cardiology guideline-adherent antithrombotic treatment in high-risk patients with atrial fibrillation: a report from the EORP-AF General Pilot Registry. Europace 2015;17:1777–86. [DOI] [PubMed] [Google Scholar]
- 16. Birney AJ, Gunn R, Russell JK, Ary DV.. MoodHacker mobile web app with email for adults to self-manage mild-to-moderate depression: randomized controlled trial. JMIR Mhealth Uhealth 2016;4:e8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Irvine AB, Russell H, Manocchia M, Mino DE, Cox Glassen T, Morgan R. et al. Mobile-Web app to self-manage low back pain: randomized controlled trial. J Med Internet Res 2015;17:e1.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Safran Naimark J, Madar Z, Shahar DR.. The impact of a Web-based app (eBalance) in promoting healthy lifestyles: randomized controlled trial. J Med Internet Res 2015;17:e56.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maher C, Ferguson M, Vandelanotte C, Plotnikoff R, De Bourdeaudhuij I, Thomas S. et al. A web-based, social networking physical activity intervention for insufficiently active adults delivered via facebook app: randomized controlled trial. J Med Internet Res 2015;17:e174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fukuoka Y, Gay CL, Joiner KL, Vittinghoff E.. A novel diabetes prevention intervention using a mobile app: a randomized controlled trial with overweight adults at risk. Am J Prev Med 2015;49:223–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Direito A, Jiang Y, Whittaker R, Maddison R.. Apps for IMproving FITness and Increasing Physical Activity Among Young People: the AIMFIT Pragmatic Randomized Controlled Trial. J Med Internet Res 2015;17:e210.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mira JJ, Navarro I, Botella F, Borras F, Nuno-Solinis R, Orozco D. et al. A Spanish pillbox app for elderly patients taking multiple medications: randomized controlled trial. J Med Internet Res 2014;16:e99.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P. et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med 2013;10:e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ertmer PA, Newby T.. Behaviorism, cognitivism, constructivism: comparing critical features from an instructional design perspective. Perform Improv Q 1993;6:50–72. [Google Scholar]
- 25. Doolittle PE, Camp WG.. Constructivism: the career and technical education perspective. J Vocat Tech Edu 1999;16:23–46. [Google Scholar]
- 26. Harasim L. Introduction to learning theory and technology, Chapter 1 Learning Theory and Online Technologies. New York: Routledge; 2012. [Google Scholar]
- 27. Attwell G, Hughes J. Pedagogic approaches to using technology for learning—literature review. Lifelong Learning UK 2010. http://dera.ioe.ac.uk/id/eprint/2021 (05 January 2016, date last accessed)
- 28. Kirkwood A. E‐learning: you don't always get what you hope for. Technol Pedag Educ 2009;18:107–21. [Google Scholar]
- 29. Aldridge MD. Writing and designing readable patient education materials. Nephrol Nurs J 2004;31:373–7. [PubMed] [Google Scholar]
- 30. Hoffmann T, McKenna K.. Analysis of stroke patients' and carers' reading ability and the content and design of written materials: recommendations for improving written stroke information. Patient Educ Couns 2006;60:286–93. [DOI] [PubMed] [Google Scholar]
- 31. Weih M, Reinhold A, Richter-Schmidinger T, Sulimma AK, Klein H, Kornhuber J.. Unsuitable readability levels of patient information pertaining to dementia and related diseases: a comparative analysis. Int Psychogeriatr 2008;20:1116–23. [DOI] [PubMed] [Google Scholar]
- 32. Salmon G, E-tivities: The Key to Active Online Learning. New York: Routledge, Taylor & Francis Group; 2013. [Google Scholar]
- 33. Fumagalli LP, Radaelli G, Lettieri E, Bertele P, Masella C.. Patient empowerment and its neighbours: clarifying the boundaries and their mutual relationships. Health Policy 2015;119:384–94. [DOI] [PubMed] [Google Scholar]
- 34. Vygotsky LS, Interaction between learning and development, Chapter 6 In Cole M, John-Steiner V, Scribner S, Souberman E (eds). Mind in Society: The Development of Higher Psychological Processes. Cambridge, MA: Harvard University Press; 1978. p79–91. [Google Scholar]
- 35. Anderson LW, Krathwohl DR, Airasian PW, Cruikshank KA, Mayer RE, Pintrich PR. et al. A Taxonomy for Learning, Teaching, and Assessing: A Revision of Bloom's Taxonomy of Educational Objectives. New York: Pearson, Allyn & Bacon; 2001. [Google Scholar]
- 36. European Commission Directorate-General for Education and Culture. Common European principles for teacher competences and qualifications 2005. http://www.atee1.org/uploads/EUpolicies/common_eur_principles_en.pdf (05 June 2016, date last accessed)
- 37. Council of the European Union. Council conclusions of 12 May 2009 on a strategic framework for European cooperation in education and training (‘ET 2020’). Official J 2009; C 199/2 http://www.atee2011.org/uploads/EUpolicies/updated_strategic_framework_for_eucooperation_council_et2020.pdf (22 June 2016, date last accessed)
- 38. The Higher Education Academy. The UK Professional Standards Framework for teaching and supporting learning in higher education. 2011. https://www.heacademy.ac.uk/sites/default/files/downloads/UKPSF_2011_English.pdf (01 November 2015, date last accessed)
- 39. General Medical Council. Standards for curricula and assessment systems. 2010.http://www.gmc-uk.org/Standards_for_curricula_and_assessment_systems_1114.pdf_48904896.pdf (16 December 2015, date last accessed)
- 40. Payne KB, Wharrad H, Watts K.. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak 2012;12:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chisholm A, Askham J.. A Review of Professional Codes and Standards for Doctors in the UK, USA and Canada. Oxford: Picker Institute Europe; 2006. [Google Scholar]
- 42. Medical professionalism in the new millennium: a physicians' charter. Lancet 2002;359:520–2. [DOI] [PubMed] [Google Scholar]
- 43. The CanMEDS 2005 Physician Competency Framework. Better Standards. Better Physicians. Better Care. Ottawa: The Royal College of Physicians and Surgeons of Canada; 2005. [Google Scholar]
- 44. Gillebert TC, Brooks N, Fontes-Carvalho R, Fras Z, Gueret P, Lopez-Sendon J. et al. ESC core curriculum for the general cardiologist (2013). Eur Heart J 2013;34:2381–411. [DOI] [PubMed] [Google Scholar]
- 45. Astin F, Carroll D, De Geest S, Fernandez-Oliver AL, Holt J, Hinterbuchner L. et al. A Core Curriculum for the Continuing Professional Development of Nurses Working in Cardiovascular Settings: Developed by the Education Committee of the Council on Cardiovascular Nursing and Allied Professions (CCNAP) on behalf of the European Society of Cardiology. Eur J Cardiovasc Nurs 2015;14:S1–17. [DOI] [PubMed] [Google Scholar]
- 46. Hendriks JM, Luermans JG, De diagnose boezemfibrilleren – wat kan ik zelf doen? [The Diagnosis of Atrial Fibrillation - What Can I Do?]. The Hague: Academic Pharmaceutical Productions BV; 2014. [Google Scholar]
- 47. Kotecha D, Calvert M, Deeks JJ, Griffith M, Kirchhof P, Lip GYH. et al. A review of rate control in atrial fibrillation, and the rationale and protocol for the RATE-AF trial. BMJ Open 2017;7:e015099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jin M, Kim J.. Development and evaluation of an evaluation tool for healthcare smartphone applications. Telemed J E Health 2015;21:831–7. [DOI] [PubMed] [Google Scholar]
- 49. Wyatt JC, Thimbleby H, Rastall P, Hoogewerf J, Wooldridge D, Williams J.. What makes a good clinical app? Introducing the RCP Health Informatics Unit checklist. Clin Med 2015;15:519–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Grandcolasa U, Rettiea R, Marusenkoa K.. Web survey bias: sample or mode effect? J Market Manag 2003;19:541–61. [Google Scholar]
- 51. Silbernagel G, Spirk D, Hager A, Baumgartner I, Kucher N.. Electronic alert system for improving stroke prevention among hospitalized oral-anticoagulation-naive patients with atrial fibrillation: a randomized trial. J Am Heart Assoc 2016;5:e003776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Nuno R, Coleman K, Bengoa R, Sauto R.. Integrated care for chronic conditions: the contribution of the ICCC framework. Health Policy 2012;105:55–64. [DOI] [PubMed] [Google Scholar]
- 53. Bodenheimer T, Wagner EH, Grumbach K.. Improving primary care for patients with chronic illness. JAMA 2002;288:1775–9. [DOI] [PubMed] [Google Scholar]
- 54. Hibbard JH, Greene J.. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood) 2013;32:207–14. [DOI] [PubMed] [Google Scholar]
- 55. Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P. et al. Shared decision making: a model for clinical practice. J Gen Intern Med 2012;27:1361–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. McCabe PJ. Self-management of atrial fibrillation: a new frontier for nursing research. Prog Cardiovasc Nurs 2008;23:37–40. [DOI] [PubMed] [Google Scholar]
- 57. Thrall G, Lane D, Carroll D, Lip GYH.. Quality of life in patients with atrial fibrillation: a systematic review. Am J Med 2006;119:448.e441–19. [DOI] [PubMed] [Google Scholar]
- 58. Lip GY, Kamath S, Jafri M, Mohammed A, Bareford D.. Ethnic differences in patient perceptions of atrial fibrillation and anticoagulation therapy: the West Birmingham Atrial Fibrillation Project. Stroke 2002;33:238–42. [DOI] [PubMed] [Google Scholar]
- 59. Clarkesmith DE, Pattison HM, Lane DA.. Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Cochrane Database Syst Rev 2013;6:Cd008600. [DOI] [PubMed] [Google Scholar]
- 60. Smith DE, Xuereb CB, Pattison HM, Lip GY, Lane DA.. TRial of an Educational intervention on patients' knowledge of Atrial fibrillation and anticoagulant therapy, INR control, and outcome of Treatment with warfarin (TREAT). BMC Cardiovasc Disord 2010;10:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Smith MB, Christensen N, Wang S, Strohecker J, Day JD, Weiss JP. et al. Warfarin knowledge in patients with atrial fibrillation: implications for safety, efficacy, and education strategies. Cardiology 2010;116:61–9. [DOI] [PubMed] [Google Scholar]
- 62. Hendriks JM, Crijns HJ, Tieleman RG, Vrijhoef HJ.. The atrial fibrillation knowledge scale: development, validation and results. Int J Cardiol 2013;168:1422–8. [DOI] [PubMed] [Google Scholar]
- 63. McCabe PJ. What patients want and need to know about atrial fibrillation? J Multidiscip Healthc 2011;4:413–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. U.S. Department of Education Office of Planning Evaluation and Policy Development. Evaluation of Evidence-Based Practices in Online Learning: A Meta-analysis and Review of Online Learning Studies 2010. http://www2.ed.gov/rschstat/eval/tech/evidence-based-practices/finalreport.pdf (5 October 2015, date last accessed)
- 65. Pew Research Center. Older Adults and Technology Use 2014. http://www.pewinternet.org/2014/04/03/older-adults-and-technology-use/ (18 April 2016, date last accessed).
- 66. Mohadis HM, Ali NM, A study of smartphone usage and barriers among the elderly. In 2014 3rd International Conference on User Science and Engineering (i-USEr). 2014. DOI: 10.1109/IUSER.2014.7002686.
- 67. Rasmussen K, Belisario JM, Wark PA, Molina JA, Loong SL, Cotic Z. et al. Offline eLearning for undergraduates in health professions: a systematic review of the impact on knowledge, skills, attitudes and satisfaction. J Glob Health 2014;4:010405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Devitt P, Palmer E.. Computer-aided learning: an overvalued educational resource? Med Educ 1999;33:136–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.