Abstract
Background
Assessing athletes’ readiness is a key component for successful outcomes after ACL reconstruction (ACLR).
Objectives
To investigate whether return-to-activity criteria, individually or in combination, at 6 months after ACLR can predict return to participation in the same preinjury activity level at 12 and 24 months after ACLR.
Methods
Ninety-five level I/II participants completed return-to-activity criteria testing (isometric quadriceps index, single-legged hop tests, Knee Outcome Survey-Activities of Daily Living Scale (KOS-ADLS) and Global Rating Score (GRS)) at 6 months after ACLR. The PASS group was defined as scoring ≥90% on all criteria and the FAIL group as scoring <90% on any criteria. At 12 and 24 months after ACLR, participants were asked if they had returned to participate in the same preinjury activity level or not. All return-to-activity criteria, except quadriceps index, were entered into the logistic regression model.
Results
Eighty-one percent and 84.4% of the PASS group returned to participation in the same preinjury activity level, while only 44.2% and 46.4% of the FAIL group returned at 12 and 24 months, respectively, after ACLR. The 6-meter timed hop, single hop and triple hop limb symmetry indexes; GRS; and KOS-ADLS individually predicted the outcome of interest at 12 months after ACLR (range: R2: 0.12–0.22, p≤0.024). In combination, they explained 27% of the variance (p=0.035). All hop tests, individually, predicted the outcome of interest at 24 months after ACLR (range: R2: 0.26–0.37; p≤0.007); in combination they explained 45% of the variance (p≤0.001).
Conclusion
Return to participation in the same preinjury activity level at 12 and 24 months after ACLR was higher in those who passed the criteria compared with those who failed. Individual and combined return-to-activity criteria predicted the outcomes of interest, with the hop tests as consistent predictors at 12 and 24 months after ACLR.
INTRODUCTION
Rupturing the ACL is a common sport injury resulting in physical and functional impairments that prevent athletes from participating in both daily living and high-level physical activities.1–6 Early ACL reconstruction (ACLR) is the standard of care for athletes who are intending to return to high-level physical activities.2 However, the rate of return to preinjury activity level continues to be low after ACLR,3–6 with only one-third of athletes returning to full competition at 1 year after ACLR.3 This low rate might be due to the persistence of knee impairments and functional deficits that are commonly reported after ACLR.1,7–11 Additionally, the lack of consensus in the criteria that are used to determine patients’ physical readiness to return to the preinjury activity level may account for the low rate of return to preinjury activity levels after surgery.
Multiple factors have been reported to be associated with the low rate of return to preinjury activities; however, some of them are non-modifiable by rehabilitation.12–15 Other factors are modifiable ie, quadriceps strength deficit, knee range of motion limitation, psychological unreadiness,16 neuromuscular dysfunction and aberrant biomechanical patterns17 and can promote patients’ functional recovery and maximise their functional capacities. This, in turn, may allow patients to meet the physical demands of their high-level physical activities.16 After ACLR, determining the patient’s readiness is still challenging clinicians, as there is no standardised objective measures to determine patients’ physical readiness. Identifying a set of measures that can effectively evaluate patients’ physical capacity and ultimately contribute to the return to the preinjury activity level is important during the decision-making process to determine patient’s physical readiness. Additionally, determining the prediction ability of these measures may help clinicians to identify those patients who may return to the preinjury activity level after surgery.
Our physical therapy clinic uses a battery of objective return-to-activity criteria that provides a comprehensive assessment of the patients’ physical performance and knee function. These criteria emphasise limb-to-limb symmetry and normal knee function.9,18,19 Additionally, these criteria can capture multiple aspects of functional deficits and impairments, which may help clinicians to modify the rehabilitation programme to address patients’ functional deficits and impairments before returning to high-level physical activity.19–24 To this end, it is unknown whether an individual or a combination of return-to-activity criteria can predict return to preinjury activity level after ACLR. Therefore, the purpose of this study was to (1) investigate whether return-to-activity criteria predict return to participation in the same preinjury activity level at 12 and 24 months after ACLR and (2) determine which individual and combination of return-to-activity criteria 6 months after ACLR predicts return to participation in the same preinjury activity level 12 and 24 months after ACLR.
METHODS
One-hundred and seven participants with an ACLR from an ongoing, prospective, longitudinal cohort study participated in this study. The rest of the cohort study’s participants were not included in this analysis because they opted for non-surgical management (n=43 participants). All participants were between the ages of 15 and 55 years and were regular participants in level I or II sport activities that involve jumping, cutting, pivoting and lateral movements (soccer, football, rugby, tennis, ice hockey) for at least 50 hours per year prior to the injury.1 Participants with concomitant grade III ligamentous injury, repairable meniscal injury, full-thickness articular cartilage damage or a history of serious lower extremity injury (eg, fracture) were not enrolled into the cohort study. All participants received a presurgical rehabilitation training that included progressive strengthening and perturbation training as described by Fitzgerald et al.25 All participants received a reconstruction surgery and a progressive postsurgical rehabilitation training that included early resolution of joint effusion, range of motion deficits, strength impairments and activity limitations. Neuromuscular and weight-bearing training activities were integrated early in the postsurgical rehabilitation process.18 Participants were progressed through the rehabilitation programme as they met clinical milestones described by Adams et al.18 The study was approved by the University of Delaware’s Institutional Human Subjects Review Board. All participants were provided with a written informed consent for participation in this study. Majority of the participants were recruited from the University of Delaware’s physical therapy clinic. Data were collected from participants at 6 months (mean: 6.26±0.81 months), 12 months (mean: 12.44±1.13 months) and 24 months (mean: 25.1±4.16 months) after ACLR. Number of participants and reasons for missing data are illustrated in figure 1.
Figure 1.
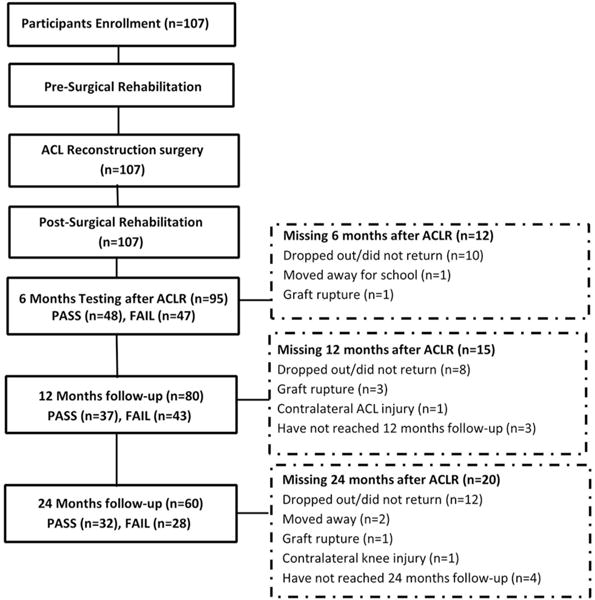
Flow diagram for participant’s participation at 6, 12 and 24 months follow-up testing after ACLR.
Testing
Participants completed a battery of return-to-activity criteria testing (performance-based tests and patient-reported measures of knee function) at 6 months after ACLR.9,18,26 At 12 and 24 months follow-up after ACLR, participants answered a single yes or no question that asks whether they have returned to participate in the same level of sport or recreational activities as before their injury or not. Participants were instructed at the time of follow-ups to indicate whether their current level of participation in jumping, cutting, pivoting and lateral movements activities is the same as their level before the injury.
Performance-based measures
Isometric quadriceps strength was measured 6 months after ACLR using a maximal voluntary isometric contraction (MVIC) of the quadriceps muscles27 on an electromechanical dynamometer (Kin-Com, Chattanooga, Chattanooga, Tennessee, USA). The MVIC testing was described in a previous published study.19 Quadriceps strength was reported as quadriceps index (force of involved limb by the force of uninvolved limb multiplied by 100). One participant did not complete the strength testing at 6 months after ACLR due to patellofemoral pain.
Single-legged hop performance was measured 6 months after ACLR using a series of single-legged hop tests28: single hop, triple cross-over hop and triple hop for distance and 6-meter timed hop. All hop test data were collected with participants wearing a functional knee brace. Hop performance was reported as limb symmetry indexes (LSIs). Hop tests were described in a previous study.19 Five participants did not complete single-legged hop tests at 6 months after ACLR due to increased knee effusion,29 quadriceps index <80% and patellofemoral and foot pain.
Patient-reported outcome measures
At 6 months after ACLR, participants filled out patient-reported questionnaires (Knee Outcome Survey-Activities of Daily Living Scale (KOS-ADLS) and Global Rating Score (GRS)) after performance-based testing was completed. KOS-ADLS is a patient-reported measure consisting of 14 items regarding the participants’ perception of postsurgical symptoms and functional limitations and how they affect the ability to perform ADLs (walking, ascending and descending stairs, kneeling, sitting and squatting).30 KOS-ADLS has been shown to be a reliable, valid and responsive measure for assessing functional limitations of the knee, with high intraclass coefficients of 0.97 and test–retest reliability.31 KOS-ADLS’s scores were reported as a percentage of the participant’s points divided by the total possible points multiplied by 100. The GRS is a one-item question that assesses participants’ current knee functional performance. Participants rated their current knee function on a scale from 0% to 100%, with 0% being the inability to perform any activity and 100% being their level of knee function prior to injury, including sports activities. It has been reported that analogue GRS has a high test–retest intraclass coefficients of 0.96.32
Return-to-activity criteria
Participants who scored ≥90% on all the criteria at 6 months were categorised as the PASS group and those who scored <90% on any of the criteria were categorised as the FAIL group. Participants who did not complete the hop tests due to quadriceps weakness (quadriceps index <80%) or pain or who reported having instability or were apprehensive to hop were also classified as FAIL. Return-to-activity criteria were only used to classify participants as PASS or FAIL 6 months after ACLR. Participants’ classification on return-to-activity criteria was previously described by Nawasreh et al.19
Statistical analysis
At 6 months after ACLR, independent Student’s t-test was used to determine differences between PASS and FAIL groups for participant’s demographics and return-to-activity criteria variables, χ2 test was used to determine whether women to men ratios were different between groups and Mann-Whitney U test was used as a post hoc test.
At 12 and 24 months after ACLR, likelihood ratios were used to determine the relationship between participants who did and did not return to preinjury activity level between PASS and FAIL groups. Sensitivity was computed as the percentage of participants who passed the criteria and returned to preinjury activity level divided by the total number of participants who did return. Specificity was computed as the percentage of participants who failed the criteria and did not return to preinjury activity level divided by the total number of participants who did not return. Positive likelihood ratios are the probability of a participant who returned to preinjury activity level and passed the criteria divided by the probability of a participant who did not return and passed the criteria, whereas negative likelihood ratios are the probability of a participant who did not return to preinjury activity level and failed the criteria divided by the probability of a participant who did return and failed the criteria.
At 12 and 24 months after ACLR, an initial binary logistic regression model (univariate) was used to evaluate whether classifying participants into PASS and FAIL groups and individual return-to-activity criteria variables (independent variables) at 6 months after ACLR can predict return to participate in the same preinjury activity level at 12 and 24 months after ACLR (dependent variable) and to evaluate the proportion that each variable can predict the outcome of interest. Participants’ age and sex were used as covariates in the univariate and multivariable logistic regression models. Only those significant univariate predictors were entered into the multivariable logistic regression model; the variables were entered based on their predictability from the most to the least (R2: Nagelkerke R square, ORs and 95% CI). Data from both groups were used in the logistic regression analysis. The quadriceps index variable was not used in the prediction model of this study because it was used as an assessment measure to determine participants’ eligibility to perform the single-legged hop tests (participants were not allowed to perform the single-legged hop tests unless they demonstrated 80% or more on quadriceps index). Therefore, this may have an effect on the predictability of the quadriceps index. Additionally, quadriceps index was excluded from the prediction model as the patients’ performance on the quadriceps strength test most likely corresponds with the scores of the hop tests.33–35 All data were analysed with SPSS V.20.0 (IBM) with a significance level of 0.05 set a priori.
RESULTS
The only participants’ demographic difference between PASS and FAIL groups at 6 months after ACLR was the women to men ratios (p<0.03); post hoc test showed that the number of women was significantly higher in the FAIL group than in the PASS group (p=0.01). Additionally, the number of men was significantly higher than women in the PASS group and in the overall study (p<0.001) (table 1). All return-to-activity criteria variables were significantly different between groups at 6 months after ACLR (p<0.05) except for KOS-ADLS (p=0.13) (table 1). Quadriceps strength deficits (<90%), poor functional performance on single-legged hop tests (<90%) and scoring lower on patient-reported outcome measures (<90%) accounted for failing the criteria. In addition, some participants complained of knee pain and knee effusion that prevented them from completing the single-legged hop testing.
Table 1.
Participants’ demographics and return-to-activity criteria variables of the PASS and FAIL groups at 6 months after ACLR (mean (SD))
| Variables | PASS group | FAIL group | p Value |
|---|---|---|---|
| Participants (n) (women/men) | 48 (11/37) | 47 (21/26) | 0.03 |
| Age (year) | 25.8 (9.4) | 29.4 (11.4) | 0.133 |
| BMI (kg/m2) | 24.4 (2.7) | 25.4 (4.4) | 0.40 |
| Graft type (autograft/allograft) | 19/29 | 17/30 | 0.60 |
| Quadriceps index (%) | 103.3 (10.3) | 91.7 (11.8) | <0.001 |
| Single hop LSI (%) | 97.3 (5.2) | 89.1 (12.0) | <0.001 |
| Cross-over hop LSI (%) | 97.9 (4.4) | 93.9 (9.7) | 0.008 |
| Triple hop LSI (%) | 97.2 (4.4) | 92.8 (7.4) | 0.003 |
| 6-meter timed hop LSI (%) | 99.6 (5.4) | 92.8 (8.6) | <0.001 |
| KOS-ADLS (%) | 97.3 (2.5) | 96. (4.4) | 0.13 |
| GRS (%) | 95.3 (4.0) | 87.4 (11.7) | <0.001 |
BMI, body mass index; GRS, Global Rating Score; KOS-ADLS, Knee Outcome Survey-Activities of Daily Living Scale; LSI, limb symmetry index.
Follow-up at 12 months after ACLR
The rates of return to participation in the same preinjury activity level at 12 months after ACLR were 81.1% for the PASS group and 44.2% for the FAIL group; the overall rate was 61.3% (table 2). Testing participants on return-to-activity criteria at 6 months after ACLR had a sensitivity of 61.2%, specificity of 77.4%, positive likelihood ratio of 2.71 and negative likelihood ratio of 1.99 to returning to participation in the same preinjury activity level at 12 months after ACLR (p<0.001).
Table 2.
Number of participants who returned and did not return to participate in the same preinjury activity level at 12 months after ACLR among PASS and FAIL groups
| Returned at 12 months, n (%) | Did not return at 12 months, n (%) | Total | |
|---|---|---|---|
| PASS group | 30 (81) | 7 (19) | 37 |
| FAIL group | 19 (44.2) | 24 (55.8) | 43 |
| Total | 49 (61.25) | 31 (38.75) | 80 |
Classifying participants into PASS or FAIL at 6 months after ACLR explained 9.5% of the outcome’s variance at 12 months after ACLR (p=0.002). Participants’ age and sex (p≥0.43) were not predictors of the outcome measure of interest at 12 months after ACLR. After adjusting for participants’ age and sex, all of 6-meter timed hop, triple hop and single hop LSIs, GRS and KOS-ADLS at 6 months after ACLR were significant predictors of returning to participate in the same preinjury activity level at 12 months after ACLR (p<0.05). The 6 m timed hop LSI and GRS were the strongest predictor variables (table 3).
Table 3.
Individual return-to-activity criteria variables at 6 months after ACLR prediction of return to participation in the same preinjury activity level at 12 and 24 months after ACLR (R2: Nagelkerke R2, OR and 95% CI)
| Return at 12 months after ACLR (R2 (p value)) OR (95% CI) |
Return at 24 months after ACLR (R2 (p value)) OR (95% CI) |
|
|---|---|---|
| Classifying PASS vs FAIL |
0.095 (0.037) 0.36 (0.13 to 0.94) |
0.21 (0.013) 0.21 (0.06 to 0.72) |
| Single hop LSI* |
0.133 (0.024) 1.07 (1.01 to 1.14) |
0.372 (0.003) 1.15 (1.05 to 1.26) |
| Cross-over hop LSI* | 0.101 (0.058) 1.06 (0.99 to 1.15) |
0.260 (0.007) 1.12 (1.03 to 1.21) |
| Triple hop LSI* |
0.138 (0.02) 1.11 (1.02 to 1.20) |
0.294 (0.004) 1.17 (1.05 to 1.31) |
| 6-meter timed hop LSI* |
0.216 (0.004) 1.13 (1.04 to 1.22) |
0.374 (0.002) 1.18 (1.06 to 1.31) |
| KOS-ADLS* |
0.116 (0.024) 1.18 (1.02 to 1.35) |
0.075 (0.456) 1.07 (0.89 to 1.31) |
| GRS* |
0.191 (0.007) 1.11 (1.03 to 1.20) |
0.092 (0.161) 1.06 (0.98 to 1.15) |
Patients’ age and sex were adjusted for in the univariate logistic regression model. GRS, Global Rating Score; KOS-ADLS, Knee Outcome Survey-Activities of Daily Living Scale; LSI, limb symmetry index.
The combination of 6-meter timed hop LSI and GRS explained 26.4% of the outcome’s variance at 12 months after ACLR (p=0.001) (table 4). Adding the single hop LSI, triple hop LSI and KOS-ADLS to the regression model did not improve the ability of the model to explain the outcome’s variance significantly (step p value>0.05), as they explained only an additional 0.2% of the outcome’s variance (table 4).
Table 4.
Combination of return-to-activity criteria variables at 6 months after ACLR prediction of return to the participation in the same preinjury activity level at 12 months after ACLR (R2: Nagelkerke R2, OR and 95% CI)
| Model | Variable in the model | 12 months after ACLR (R2) | OR (95% CI) | Model (p value) | step (p value) |
|---|---|---|---|---|---|
| Step 1 | Age Sex 6meter timed hop LSI |
0.192 | 0.98 (0.93 to 1.04) 0.76 (0.25 to 2.31) 1.12 (1.04 to 1.22) |
0.015 | 0.015 |
| Step 2 | Age Sex 6-meter timed hop LSI GRS |
0.264 | 0.98 (0.92 to 1.04) 0.94 (0.26 to 2.67) 1.10 (1.01 to 1.19) 1.10 (0.99 to 1.21) |
0.035 | 0.035 |
| Step 3 | Age Sex 6-meter timed hop LSI GRS Triple hop LSI |
0.264 | 0.98 (0.93 to 1.04) 0.83 (0.26 to 2.67) 1.09 (0.99 to 1.20) 1.10 (0.99 to 1.21) 1.01 (0.90 to 1.12) |
0.011 | 0.93 |
| Step 4 | Age Sex 6-meter timed hop LSI GRS Triple hop LSI Single hop LSI |
0.264 | 0.98 (0.93 to 1.04) 0.83 (0.26 to 2.71) 1.09 (0.99 to 1.21) 1.10 (0.99 to 1.21) 1.01 (0.87 to 1.16) 0.99 (0.89 to 1.12) |
0.021 | 098 |
| Step 5 | Age Sex 6-meter timed hop LSI GRS Triple hop LSI Single hop LSI KOS-ADLS |
0.266 | 0.98 (0.93 to 1.04) 0.84 (0.26 to 2.71) 1.09 (0.98 to 1.21) 1.08 (0.97 to 1.21) 1.01 (0.87 to 1.16) 1.02 (0.89 to 1.12) 1.04 (0.85 to 1.28) |
0.035 | 0.711 |
GRS, Global Rating Score; KOS-ADLS, Knee Outcome Survey-Activities of Daily Living Scale; LSI, limb symmetry index.
Follow-up at 24 months after ACLR
The rates of return to participation in the same preinjury activity level were 84.4% for the PASS group and 46.4% for the FAIL group; the overall rate was 66.7% (table 5). Testing participants on return-to-activity criteria at 6 months after ACLR had a sensitivity of 67.5%, specificity of 75%, positive likelihood ratio of 2.70 and negative likelihood ratio of 2.31 to return to participation in the same preinjury activity level at 24 months after ACLR (p<0.009).
Table 5.
Number of participants who returned and did not return to participate in the same preinjury activity level at 24 months after ACLR among PASS and FAIL groups
| Returned at 24 months, n (%) | Did not return at 24 months, n (%) | Total | |
|---|---|---|---|
| PASS group | 27 (84.4) | 5 (15.6) | 32 |
| FAIL group | 13 (46.4) | 15 (53.6) | 28 |
| Total | 40 (66.7) | 20 (33.3) | 60 |
Classifying participants into PASS or FAIL at 6 months after ACLR explained 21% of the outcome’s variance at 24 months after ACLR (p=0.013). Participants’ age and sex (p≥0.33) were not predictors of the outcome measure of interest at 24 months after ACLR. After adjusting for participants’ age and sex, only the single-legged hop LSIs were significant predictors of return to participation in the same preinjury activity level at 24 months after ACLR. Six-meter timed hop and single hop LSIs were the strongest predictor variables of the outcome’s variance at 24 months after ACLR (table 3). The combination of 6 m timed hop and single hop LSIs explained 43.6% of the outcome’s variance (p<0.001) (table 6). Adding triple hop and cross-over LSIs to the regression model did not improve the predictability of model significantly (step p value>0.05) as they explained only an additional 1.8% of the outcome’s variance at 24 months after ACLR (table 6).
Table 6.
Combination of return-to-activity criteria variables at 6 months after ACLR prediction of return to participation in the same preinjury activity level at 24 months after ACLR (R2: Nagelkerke R2, OR and 95% CI)
| Model | Variable in the model | 24 months after ACLR (R2) | OR (95% CI) | Model (p value) | Step (p value) |
|---|---|---|---|---|---|
| Step 1 | Age Sex 6-meter timed hop LSI |
0.374 | 0.95 (0.88 to 1.01) 1.01 (0.24 to 4.21) 1.18 (1.06 to 1.31) |
0.001 | 0.001 |
| Step 2 | Age Sex 6-meter timed hop LSI Single hop LSI |
0.435 | 0.95 (0.89 to 1.02) 1.21 (0.26 to 5.64) 1.11 (0.99 to 1.25) 1.10 (0.99 to 1.21) |
<0.001 | 0.066 |
| Step 3 | Age Sex 6-meter timed hop LSI Single hop LSI Triple hop LSI |
0.436 | 0.95 (0.89 to 1.02) 1.18 (0.25 to 5.63) 1.11 (0.98 to 1.26) 1.09 (0.97 to 1.23) 1.02 (0.87 to 1.19) |
0.001 | 0.84 |
| Step 4 | Age Sex 6-meter timed hop LSI Single hop LSI Triple hop LSI Cross-over hop LSI |
0.453 | 0.95 (0.89 to 1.02) 1.46 (0.28 to 7.55) 1.14 (0.99 to 1.33) 1.11 (0.98 to 1.25) 1.06 (0.89 to 1.26) 0.92 (0.79 to 1.09) |
0.001 | 0.32 |
LSI, limb symmetry index.
DISCUSSION
The rates of return to participation in the same preinjury activity level at both 12 and 24 months after ACLR were higher among participants who passed the return-to-activity criteria than those who failed at 6 months after ACLR. Return-to-activity criteria, individually and in combination, can predict return to participation in the same preinjury activity level at 12 and 24 months after ACLR. Single-legged hop tests were consistent predictors of the outcomes of interest at both 12 and 24 months, while patient-reported measures predicted the outcomes of interest only at 12 months after ACLR. Additionally, participants who demonstrated normal knee function and limb-to-limb movement symmetry during functional tasks at 6 months after ACLR are more likely to return to participation in the same preinjury activity level 12 and 24 months after ACLR.
Rates of return to preinjury activity level, sensitivity, specificity and likelihood ratios
The rates of return to participation in the same preinjury activity level at 12 and 24 months after ACLR among all participants were within similar ranges reported in others studies.5,36,37 However, the rates for those who passed the criteria were superior at both 12 and 24 months after ACLR compared with other studies.5,36,37 Four out of five participants who passed the criteria returned to the preinjury activity level at both 12 and 24 months after ACLR compared with only one out of two of those who failed the criteria. Participants who returned to participate in the same preinjury activity level at both 12 and 24 months after ACLR were almost three times more likely to pass the criteria at 6 months after ACLR than those who did not return, while participants who did not return at 12 and 24 months after ACLR were at or over two times more likely to fail the criteria, respectively, at 6 months after ACLR than those who did return. Moreover, our criteria demonstrated a high specificity and a moderate sensitivity. In addition to the fact that our physical therapy clinic provides a specialised, high-standard and comprehensive evidence-based rehabilitation programme,18 the high rate of return to preinjury activity level of the PASS group might have resulted from using a strict return-to-activity criteria that emphasise normal knee function, limb-to-limb movement symmetry and normal quadriceps strength and not favouring one of their lower limbs that make them capable of participating in high-level physical activities as uninjured healthy individuals.6,11
Performance-based measures predicting the outcomes of interests at 12 and 24 months after ACLR
The hop tests were consistent predictors of the outcomes of interest at both time points, with larger variance explanation at 24 months compared with 12 months after ACLR. This finding was not surprising as athletes returning to high-level physical activities need to perform movement-specific tasks involving take-off, pivoting and landing manoeuvres that are replicated by the single-legged hop tests. Previous studies reported that single-legged hop tests can predict patient-reported knee function after non-surgical ACL management38 and reconstruction surgery.39 Further, they have the potential to discriminate between patients with functional deficit after ACLR from normal healthy athletes.40 From the hop test, the timed hop test was used as part of the decision-making scheme to determine appropriate candidates to return to high-level activity without surgery after ACL rupture.41 While the data of this study do not explain why the 6 m timed hop test was the strongest predictor at both time points, it might be easier for participants to perform a series of consecutive hops over a 6 m distance as fast as possible without changing the direction, controlling their landing or stopping their body momentum as it is the case in hop tests for distance. In this study, we did not randomise the hop tests; therefore, there might have been an order effect as participants may have felt less anxiety and more confident during the 6 m timed hop test and after they have already had finished the hop tests for distance. Eastlack and colleagues suggested that the order of conducting the hop tests may determine which one of the hop tests is the predictive measure.42
Patient-reported measures predicting the outcomes of interests at 12 and 24 months after ACLR
Patient-reported variables predicted the outcome of interest only at 12 months after ACLR. This might be due to the fact that patient-reported measures ask questions about postsurgical symptoms, impairments and knee function. As a result, patients’ perception of the postsurgical symptoms, impairments and knee function may have improved and have less impact on the participants’ functional performance at 24 months after surgery. Additionally, participants may have become more confident and satisfied with their knee function at 24 months after ACLR. The results of this study suggest that participants might require highly functional skills to succeed while participating in their preinjury activity levels at 24 months after ACLR. Still, this finding highlights the importance of addressing postsurgical symptoms and impairments as they have an effect on the short-term functional recovery after surgery.
The results of this study support similar findings reported in previous studies.25,41,43 A battery of functional tests and patients’ self-reported questionnaire measures, similar to our criteria, has the potential to differentiate between those patients with and without dynamic knee stability early after ACL injury.41 Additionally, Fitzgerald et al41 reported that these same measures can predict a short-term return to preinjury activity level in patients who were treated non-surgically. The findings of this and Fitzgerald et al’s41 studies suggest that using performance-based and patient-reported measures might be the ideal way for assessing patient’s physical readiness to return to activity after ACL rupture or ACLR.
After ACLR, patients continue to exhibit residual impairments including strength deficits and poor knee function and tend to rely more on the uninvolved limb during dynamic functional activities. This, in turn, might lead to a long-term deterioration of knee joint health.9,26,44 Using return-to-activity criteria may have significant implications on the clinical management of patients with ACLR surgery, as these criteria may help in identifying participants with functional deficits and limb-to-limb movement asymmetry before they begin participating in high-demanding activities. This, in result, can assist in modifying the rehabilitation programme to address patients’ deficits by implementing strengthening, neuromuscular, agility and plyometric training.45 Additionally, using these criteria may help in advising participants with functional deficits and limb-to-limb movement asymmetry to modify their activity level to a lower level by avoiding risky multidirectional high physical activities.
In this study, the return-to-activity criteria variables at 6 months after surgery were reported as groups’ means but not as individual participants’ score. While the FAIL group had mean scores above 90% on multiple return-to-activity criteria variables, this does not indicate that participants in the FAIL group passed the criteria, as each participant has to score 90% or more on all the seven criteria in attempt to be classified as a passed participant. This may highlight the importance of evaluating participants at an individual level but not at a group level. Further, this suggests that the decision to determine participants’ physical readiness should be based on participants’ performance on a set of objective measures instead of using only one individual measure.
Though the FAIL group demonstrated a decreased knee functional performance and limb-to-limb movement asymmetry, almost half of them returned to participate in the same preinjury activity level at 12 and 24 months after ACLR. This might be because most participants sustained their ACL rupture during sport participation and chose to undergo a reconstruction surgery with the intention to return to their preinjury activities. This finding may highlight how important is the return to preinjury activity level for athletes after the surgery. These participants may, however, possess a high risk for knee reinjury. A recent study by Kyritsis et al reported that athletes who returned to professional sports without meeting the discharge criteria had four times greater risk for ACL graft rupture compared with those who met the criteria.46 Another study that used the same return-to-activity criteria of this study reported that 38% of the athletes who returned to level I sport activities without passing the criteria sustained a knee injury compared with only 5.6% who passed the criteria.47
Previous studies reported that returning to a high level of activity at 2 years after surgery was associated with the type and level of activities prior to the injury, lower body mass index and having limb-to-limb hop symmetry.6,48 In this study, the return-to-activity criteria did not fully explain the variances of the outcomes of interest. Factors related to decreased confidence in the knee, change in lifestyle, scholastic transition, lower opportunity to participate in activities or socioeconomic status may have limited the ability of the criteria to fully explain the outcomes’ variances.48–52 The results of this study suggest that additional measures might be added to the prediction model to further explain the variances of the outcomes of interest at 12 and 24 months after ACLR. These might include, but not restricted to, the psychological and socioeconomic factors, demographic factors related to the level of preinjury activities, severity of injury, concomitant injuries and graft types.6,37,48,51,53
Limitations
This study was limited to athletes who participated in level I/II sport activities and who underwent ACLR. Another limitation of this study may be related to the rehabilitation training programme that the participants of this study have received, as our physical therapy clinic is using a specialised, high-standard and supervised evidence-based practice that focuses on early resolution of the postsurgical impairments and function limitation and integrating a return-to-activity training approach. This may, therefore, affect the generalisability of the study’s findings to other clinical sittings that do not use the same rehabilitation training practice. In this study, a group of participants passed return-to-activity criteria earlier after ACLR; however, the 6 months after ACLR was used as baseline testing for predicting the outcome at 12 and 24 months after ACLR instead of using the exact date of passing the criteria. Six month was chosen because most athletes typically complete their rehabilitation programme and start to be cleared to begin gradually participating in their preinjury activities around that time.36 Therefore, evaluating patients at 6 months after ACLR may help identifying those patients with functional limitations and physical deficits before being cleared to return to their preinjury activities. Another limitation is the inconsistency and decrease in the participants’ number for each group at 12 and 24 months follow-ups, which may have had an effect on the results of this study. While the participant’s recruitment is still ongoing, there are few participants who have not reached the 12 and 24 months follow-ups. Additionally, some of the participants sustained lower extremity injuries that prevented them from participating in their activities; these participants were not included in the analysis of this study, and they may have partially accounted for the decreased number of participants who came to the follow-ups. The predictive variables of this study were the same return-to-activity criteria that were used to clear patients to return to preinjury activity level, which may have affected the predictability of the regression model. Furthermore, a patient-reported variable related to activities of daily living (KOS-ADLS) was used in the regression model, instead of using variables that are related to sport activities, to predict return to participation in the same preinjury activity levels after ACLR. This may also have affected the predictability of the regression model. One more limitation is that our criteria do not take into account the psychological status to determine the patients’ readiness to return to preinjury activity levels. Further research might evaluate other outcome measures related to participation in sport activities and psychological readiness to predict the outcomes of interest used in this study.
CONCLUSION
Return to participation in the same preinjury activity level at both 12 and 24 months after ACLR was higher among those who passed return-to-activity criteria than those who failed at 6 months after ACLR. Return-to-activity criteria variables, individually and in combination, predicted return to participation in the same preinjury activity level at both 12 and 24 months after ACLR. The combination of 6 m timed hop test LSI and GRS predicted one-fourth of the outcome’s variance at 12 months after ACLR, and the combination of 6 m timed hop and single hop test LSIs predicted almost one-half of the outcome’s variance at 24 months after ACLR.
What are the findings?
-
►
Passing a testing battery of performance-based and patient-reported measures was associated with high rate of return to participation in the same preinjury activity levels after reconstruction (ACLR).
-
►
Return-to-activity criteria variables, individually and in combination, can predict return to participation in the same preinjury activity level at 12 and 24 months after ACLR.
-
►
The combination of 6 m timed hop test and Global Rating Score predicted one-fourth of the variance of return to participation in the same preinjury activity level at 12 months after ACLR, and the combination of 6 m timed hop and single hop tests predicted almost one-half of the outcome’s variance at 24 months after ACLR.
How might it impact on clinical practice in the future?
-
►
Determining patients’ readiness to return to preinjury activity level should be based on patients’ performance on a battery of objective return-to-activity criteria that includes performance-based and patient-reported measures.
-
►
Patients’ performance on return-to-activity criteria might be used to differentiate between patients who may or may not return to participation in the same preinjury activity level after reconstruction (ACLR).
-
►
Utilising return-to-activity criteria may help in identifying those patients with poor knee functional performance and limb-to-limb asymmetry and help in modifying the rehabilitation protocol by providing additional training sessions to address their functional deficits and limb-to-limb asymmetry after ACLR.
Acknowledgments
We thank the University of Delaware Physical Therapy clinic (http://sites.udel.edu/ptclinic/) for assistance in this study’s patient management and data collection and Martha Callahan for research coordination.
Funding This ongoing prospective cohort study was funded by the National Institutes of Health (NIH R37HD37985, P30 GM103333) and Promotion of Doctoral Studies (PODS 1) Scholarship.
Footnotes
Contributors ZN, DL and LSM conceived the idea of this study. MA performed most of the surgeries. KC, DL and ZN collected the data from participants. ZN analysed the data.
Competing interests None declared.
Patient consent Obtained.
Ethics approval University of Delaware Institutional Human Subjects Review Board.
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.Daniel DM, Stone ML, Dobson BE, et al. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1993;22:632–44. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 2.Marx RG, Jones EC, Angel M, et al. Beliefs and attitudes of members of the American Academy of Anterior Cruciate Ligament Injury. Arthroscopy. 2003;19:762–70. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 3.Ardern CL, Webster KE, Taylor NF, et al. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 4.Lee DY, Karim SA, Chang HC. Return to sports after anterior cruciate ligament reconstruction - a review of patients with minimum 5-year follow-up. Ann Acad Med Singapore. 2008;37:273–8. [PubMed] [Google Scholar]
- 5.Nakayama Y, Shirai Y, Narita T, et al. Knee functions and a return to sports activity in competitive athletes following anterior cruciate ligament reconstruction. J Nippon Med Sch. 2000;67:172–6. doi: 10.1272/jnms.67.172. [DOI] [PubMed] [Google Scholar]
- 6.Ardern CL, Taylor NF, Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543–52. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 7.Lohmander LS, Ostenberg A, Englund M, et al. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145–52. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 8.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269–73. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40:141–54. doi: 10.2519/jospt.2010.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zwolski C, Schmitt LC, Quatman-Yates C, et al. The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:2242–9. doi: 10.1177/0363546515591258. [DOI] [PubMed] [Google Scholar]
- 11.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42:750–9. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paterno MV, Rauh MJ, Schmitt LC, et al. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22:116–21. doi: 10.1097/JSM.0b013e318246ef9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–51. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 14.Salmon L, Russell V, Musgrove T, et al. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:948–57. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 15.van Eck CF, Kropf EJ, Romanowski JR, et al. Factors that influence the intra-articular rupture pattern of the ACL graft following single-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1243–8. doi: 10.1007/s00167-011-1427-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ardern CL, Taylor NF, Feller JA, et al. A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med. 2013;47:1120–6. doi: 10.1136/bjsports-2012-091203. [DOI] [PubMed] [Google Scholar]
- 17.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968–78. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adams D, Logerstedt DS, Hunter-Giordano A, et al. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42:601–14. doi: 10.2519/jospt.2012.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nawasreh Z, Logerstedt D, Cummer K, et al. Do patients failing return-to-activity criteria at 6 months after anterior cruciate ligament reconstruction continue demonstrating deficits at 2 years? Am J Sports Med. 2017;45:1–12. doi: 10.1177/0363546516680619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bent NP, Wright CC, Rushton AB, et al. Selecting outcome measures in sports medicine: a guide for practitioners using the example of anterior cruciate ligament rehabilitation. Br J Sports Med. 2009;43:1006–12. doi: 10.1136/bjsm.2009.057356. [DOI] [PubMed] [Google Scholar]
- 21.Fitzgerald GK, Lephart SM, Hwang JH, et al. Hop tests as predictors of dynamic knee stability. J Orthop Sports Phys Ther. 2001;31:588–97. doi: 10.2519/jospt.2001.31.10.588. [DOI] [PubMed] [Google Scholar]
- 22.Flanigan DC, Everhart JS, Pedroza A, et al. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:1322–9. doi: 10.1016/j.arthro.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 23.Keskula DR, Duncan JB, Davis VL, et al. Functional outcome measures for knee dysfunction assessment. J Athl Train. 1996;31:105–10. [PMC free article] [PubMed] [Google Scholar]
- 24.Logerstedt D, Di Stasi S, Grindem H, et al. Self-reported knee function can identify athletes who fail return-to-activity criteria up to 1 year after anterior cruciate ligament reconstruction: a delaware-oslo ACL cohort study. J Orthop Sports Phys Ther. 2014;44:914–23. doi: 10.2519/jospt.2014.4852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physical active individuals. Phys Ther. 2000;80:128–40. [PubMed] [Google Scholar]
- 26.Logerstedt D, Lynch A, Axe MJ, et al. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:859–68. doi: 10.1007/s00167-012-1929-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Snyder-Mackler L, De Luca PF, Williams PR, et al. Reflex inhibition of the quadriceps femoris muscle after injury or reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1994;76:555–60. doi: 10.2106/00004623-199404000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–8. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 29.Sturgill LP, Snyder-Mackler L, Manal TJ, et al. Interrater reliability of a clinical scale to assess knee joint effusion. J Orthop Sports Phys Ther. 2009;39:845–9. doi: 10.2519/jospt.2009.3143. [DOI] [PubMed] [Google Scholar]
- 30.Irrgang JJ, Snyder-Mackler L, Wainner RS, et al. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80:1132–45. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Marx RG, Jones EC, Allen AA, et al. Reliability, validity, and responsiveness of four knee outcome scales for athletic patients. J Bone Joint Surg Am. 2001;83-A:1459–69. doi: 10.2106/00004623-200110000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Hopper DM, Goh SC, Wentworth LA, et al. Test–retest reliability of knee rating scales and functional hop tests one year following anterior cruciate ligament reconstruction. Physical Therapy in Sport. 2002;3:10–18. [Google Scholar]
- 33.Petschnig R, Baron R, Albrecht M, et al. The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1998;28:23–31. doi: 10.2519/jospt.1998.28.1.23. [DOI] [PubMed] [Google Scholar]
- 34.Sekiya I, Muneta T, Ogiuchi T, et al. Significance of the single-legged hop test to the anterior cruciate ligament-reconstructed knee in relation to muscle strength and anterior laxity. Am J Sports Med. 1998;26:384–8. doi: 10.1177/03635465980260030701. [DOI] [PubMed] [Google Scholar]
- 35.Baltaci G, Yilmaz G, Atay AO. The outcomes of anterior cruciate ligament reconstructed and rehabilitated knees versus healthy knees: a functional comparison. Acta Orthop Traumatol Turc. 2012;46:186–95. doi: 10.3944/aott.2012.2366. [DOI] [PubMed] [Google Scholar]
- 36.Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43:377–8. doi: 10.1136/bjsm.2007.044818. [DOI] [PubMed] [Google Scholar]
- 37.Lai CC, Ardern CL, Feller JA, et al. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2017;096836 doi: 10.1136/bjsports-2016-096836. [DOI] [PubMed] [Google Scholar]
- 38.Grindem H, Logerstedt D, Eitzen I, et al. Single-legged hop tests as predictors of self-reported knee function in nonoperatively treated individuals with anterior cruciate ligament injury. Am J Sports Med. 2011;39:2347–54. doi: 10.1177/0363546511417085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Logerstedt D, Grindem H, Lynch A, et al. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40:2348–56. doi: 10.1177/0363546512457551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41:377–87. doi: 10.2519/jospt.2011.3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2000;8:76–82. doi: 10.1007/s001670050190. [DOI] [PubMed] [Google Scholar]
- 42.Eastlack ME, Axe MJ, Snyder-Mackler L. Laxity, instability, and functional outcome after ACL injury: copers versus noncopers. Med Sci Sports Exerc. 1999;31:210–5. doi: 10.1097/00005768-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 43.Fitzgerald GK, Axe MJ, Snyder-Mackler L. Proposed practice guidelines for nonoperative anterior cruciate ligament rehabilitation of physically active individuals. J Orthop Sports Phys Ther. 2000;30:194–203. doi: 10.2519/jospt.2000.30.4.194. [DOI] [PubMed] [Google Scholar]
- 44.de Jong SN, van Caspel DR, van Haeff MJ, et al. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23:21.e1–21.e11. doi: 10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 45.Myer GD, Ford KR, Khoury J, et al. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med. 2011;45:245–52. doi: 10.1136/bjsm.2009.069351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kyritsis P, Bahr R, Landreau P, et al. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50:946–51. doi: 10.1136/bjsports-2015-095908. [DOI] [PubMed] [Google Scholar]
- 47.Grindem H, Snyder-Mackler L, Moksnes H, et al. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50:804–8. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dunn WR, Spindler KP, MOON Consortium Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38:2040–50. doi: 10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ardern CL, Österberg A, Tagesson S, et al. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48:1613–9. doi: 10.1136/bjsports-2014-093842. [DOI] [PubMed] [Google Scholar]
- 50.Ardern CL. Anterior cruciate ligament reconstruction—not exactly a one-way ticket back to the preinjury level: a review of contextual factors affecting return to sport after surgery. Sports Health. 2015;7:224–30. doi: 10.1177/1941738115578131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ardern CL, Taylor NF, Feller JA, et al. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41:1549–58. doi: 10.1177/0363546513489284. [DOI] [PubMed] [Google Scholar]
- 52.Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9:9–15. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 53.Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:2827–32. doi: 10.1177/0363546516651845. [DOI] [PubMed] [Google Scholar]


