Abstract
The purpose of this study is to estimate the national prevalence of parent-reported attention deficit/hyperactivity disorder (ADHD) diagnosis and treatment among U.S. children 2–17 years of age using the 2016 National Survey of Children’s Health (NSCH). The NSCH is a nationally representative, cross-sectional survey of parents regarding their children’s health that underwent a redesign before the 2016 data collection. It included indicators of lifetime receipt of an ADHD diagnosis by a health care provider, whether the child currently had ADHD, and receipt of medication and behavioral treatment for ADHD. Weighted prevalence estimates were calculated overall and by demographic and clinical subgroups (n = 45,736). In 2016, an estimated 6.1 million U.S. children 2–17 years of age (9.4%) had ever received an ADHD diagnosis. Of these, 5.4 million currently had ADHD, which was 89.4% of children ever diagnosed with ADHD and 8.4% of all U.S. children 2–17 years of age. Of children with current ADHD, almost two thirds (62.0%) were taking medication and slightly less than half (46.7%) had received behavioral treatment for ADHD in the past year; nearly one fourth (23.0%) had received neither treatment. Similar to estimates from previous surveys, there is a large population of U.S. children and adolescents who have been diagnosed with ADHD by a health care provider. Many, but not all, of these children received treatment that appears to be consistent with professional guidelines, though the survey questions are limited in detail about specific treatment types received. The redesigned NSCH can be used to annually monitor diagnosis and treatment patterns for this highly prevalent and high-impact neurodevelopmental disorder.
INTRODUCTION
Attention deficit/hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder diagnosed in childhood (Perou et al., 2013), and it is characterized by chronic symptoms of inattention, impulsivity, and/or hyperactivity that lead to functional impairment experienced in multiple settings (American Psychiatric Association, 2013). Children and adolescents with ADHD are more likely to experience a variety of negative outcomes compared to their peers without the disorder, including lower academic attainment, impaired social functioning, increased risk of hospital admissions and injuries, increased substance use and risk of substance use disorder, and reduced income and participation in labor markets as adults (Fleming et al., 2017; Fletcher, 2014; Groenman, Janssen, & Oosterlaan, 2017; Molina et al., 2013; Ros & Graziano, 2017). In 2013, U.S. health care expenditures for ADHD totaled $23 billion (Dieleman et al., 2016), and the annual societal costs including health care, education, and reduced family productivity associated with childhood ADHD in the United States have been estimated to range from $38 billion to $72 billion (Doshi et al., 2012).
Criteria for the diagnosis of ADHD are laid out in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and were revised for the fifth edition published in 2013 (American Psychiatric Association, 2013). These changes included shifting the age of onset requirement from the presence of symptoms and impairment by age 7 years to the presence of some symptoms by age 12 years, reducing the number of symptoms required for a diagnosis for individuals 17 years of age and older, and providing clinical examples of symptoms that are more age appropriate for older adolescents and adults (Matte et al., 2015; Sibley, Waxmonsky, Robb, & Pelham, 2013). Children with ADHD are most commonly diagnosed by pediatricians or other primary care physicians (53%); approximately 14% of children with ADHD received their diagnosis from a psychologist (Visser, Zablotsky, Holbrook, Danielson, & Bitsko, 2015b). Similarly, approximately one in eight children with ADHD received treatment services from a psychologist, whereas the majority of children with ADHD receive their treatment from a physician (Olfson, Gameroff, Marcus, & Jensen, 2003).
Clinical guidelines for the diagnosis and treatment of ADHD have been published for pediatricians and child and adolescent psychiatrists (American Academy of Child and Adolescent Psychiatry, 2007; American Academy of Pediatrics [AAP], 2011). In 2011, the AAP published updated clinical practice guidelines for ADHD, and this update included age-specific treatment recommendations for preschool-age children (4–5 years of age), elementary-school-age children (6–11 years), and adolescents (12–18 years; AAP, 2011). For preschool-age children diagnosed with ADHD, the AAP recommends parent-or teacher-administered behavior therapy as the first-line treatment, with medication prescribed only if impairment remains after an adequate trial of behavior therapy. For children 6–11 years of age, the AAP recommends prescribing medication and/or behavior therapy, with a preference for both treatments in combination, and for adolescents 12–18 years of age, medication is recommended with a preference for it to be prescribed in combination with behavior therapy. Combination therapy is also supported in practice parameters for child and adolescent psychiatrists, particularly for children who still have functional impairment while being treated with medication alone or for children who have ADHD and a co-occurring disorder (American Academy of Child and Adolescent Psychiatry, 2007). Clinical guidance published for child and adolescent psychiatrists also recommends the use of psychotherapy to treat very young children with ADHD before initiating medication treatment (Gleason et al., 2007). Receipt of recommended treatment for children and adolescents with ADHD has been identified as a developmental objective for the improvement of the nation’s health in Healthy People 2020, with the goal of increasing the proportion of children 4–5 years of age with ADHD who receive recommended behavioral treatment and increasing the proportion of children and adolescents 6–17 years of age who receive recommended behavioral treatment, medication treatment, or a combination of the two (United States Department of Health & Human Services, 2010).
National surveys are commonly used to monitor trends in the prevalence of ADHD diagnosis and treatment, and this information can be used to characterize service needs of children with ADHD and for identification of service gaps. A previous study using nationally representative data has shown that in 2011–2012 approximately 11% of children and adolescents 4–17 years of age had ever received an ADHD diagnosis from a health care provider (Visser et al., 2014). Data from two periodically administered national surveys have tracked an increase in diagnosed ADHD since the late 1990s and early 2000s (Akinbami, Liu, Pastor, & Reuben, 2011; Visser et al., 2014), with another study documenting an increase specifically in the population of children 2–5 years of age from 2007–2008 to 2011–2012 (Danielson et al., 2017b). There was also a noted increase in the percentage of U.S. children taking ADHD medication during the same period; an estimated 4.8% of children 4–17 years of age had current ADHD and were taking ADHD medication in 2007–2008 compared to 6.1% in 2011–2012 (Visser et al., 2014). Approximately 30%–40% of children and adolescents with current ADHD were reported to have been receiving behavioral or psychosocial treatments for their ADHD based on parent-reported national survey data (Danielson, Visser, Chronis-Tuscano, & DuPaul, 2017a; Visser et al., 2015a).
The purpose of the present study is to provide updated national prevalence estimates of ADHD diagnosis and treatment for children 2–17 years of age living in the United States based on National Survey of Children’s Health (NSCH) data collected in 2016. This iteration of the NSCH is the first after a major survey redesign and will provide baseline estimates for diagnosed ADHD prevalence and treatment indicators that can be used for trend analyses with future annual administrations of the NSCH.
METHODS
The NSCH is a population-based, cross-sectional survey designed to monitor the health and well-being of noninstitutionalized children 0–17 years of age living in the United States. The survey is sponsored by the Health Resources and Services Administration’s Maternal and Child Health Bureau, and the U.S. Census Bureau started conducting this survey annually in 2016. Previous versions of this survey had been conducted every 4 years as a telephone survey, but due to decreasing response rates and increasing costs for survey implementation, the NSCH was transitioned to an online/mail-based survey beginning with the 2016 data collection period (United States Census Bureau, 2017). Households were randomly selected for participation and mailed an invitation to complete a household screener and, if children were present, a child-specific questionnaire regarding the health and well-being of one randomly selected child living in the household. These survey components could be completed either online using a secure, confidential website or with a mailed paper version of the questionnaire. A full description of the survey methods has been published elsewhere (United States Census Bureau, 2017). There were 50,212 completed interviews for the 2016 NSCH, with an overall weighted response rate of 40.7%; the proportion of screened households known to contain a child that completed the child-specific questionnaire was 69.7%. This study included data on children 2–17 years of age and a valid response to the lifetime ADHD diagnosis question described next (n = 45,736).
This study focused on survey questions related to ADHD. The household respondent (generally a parent, and hereafter referred to as the parent) was asked if “a doctor or other health care provider ever told you that this child has attention deficit disorder or attention-deficit/hyper-activity disorder, that is, ADD or ADHD.” If the parent responded affirmatively, he or she was directed to answer two follow-up questions: if the child currently has ADHD, and, if so, whether the child’s ADHD was mild, moderate, or severe. Parents were also asked if their child was “currently taking medication for ADD or ADHD,” if their child received “behavioral treatment for ADD or ADHD such as training or an intervention that you or this child received to help with his or her behavior” in the past 12 months, and if their child “received any treatment or counseling from a mental health professional … [including] psychiatrists, psychologists, psychiatric nurses, or clinical social workers” in the past 12 months.
Weighted prevalence estimates and 95% Wald confidence intervals were calculated overall for ADHD diagnosis (ever received an ADHD diagnosis and reported to have current ADHD) and for each treatment type (receipt of ADHD medication, receipt of behavioral treatment for ADHD, receipt of behavioral treatment for ADHD and/or any treatment or counseling from a mental health professional) among children 2–17 years of age with current ADHD. Combinations of treatment specific to ADHD were considered by four mutually exclusive treatment groups: (a) medication and behavioral treatment for ADHD, (b) medication only, (c) behavioral treatment only, and (d) neither medication nor behavioral treatment. Receipt of any treatment or counseling from a mental health professional was not considered in the analysis of the mutually exclusive treatment groups. Weighted prevalence estimates were also calculated and compared using prevalence ratios (PRs) and 95% confidence intervals (CIs) by the following demographic subgroups: child sex (male, female), age (2–5 years, 6–11 years, 12–17 years), race (White, Black, other), ethnicity (Hispanic, non-Hispanic), primary language in the home (English, Spanish, other language), highest education level in the household (less than high school, high school graduate, more than high school), poverty status (< 100% of federal poverty level, 100%–199% of federal poverty level, ≥ 200% of federal poverty level), type of health care coverage (public only, private only, private and public, insurance type unspecified, none), region of residence (Northeast, Midwest, South, West), and urban/rural status (lived in a Metropolitan Statistical Area [hereafter referred to as urban/suburban], did not live in a Metropolitan Statistical Area [hereafter referred to as rural]). For treatment type, comparisons were also made by parent-reported ADHD severity (mild, moderate, severe) and presence of a current co-occurring mental, emotional, or behavioral condition (yes, no; hereafter referred to as a co-occurring condition). Current co-occurring conditions were identified with questions similar to those for ADHD (parent reported whether a health care provider had ever told them their child had the condition and whether the child currently has the condition). The conditions considered in this analysis included behavioral or conduct problems, anxiety problems, depression, autism spectrum disorder, Tourette syndrome, and substance use disorder.1
Among all children included in the analytic sample, there was a small percentage of missing data for each of the ADHD-related variables of interest. Of children with a reported lifetime ADHD diagnosis, 2.0% were missing for the current ADHD question; these children were considered in the analysis not to have current ADHD. Of children with current ADHD, 0.5% were missing for the medication variable, 0.4% were missing for behavioral treatment, and 0.4% were missing for any treatment or counseling from a mental health professional. Respondents with missing data for one of these variables were excluded from the respective analyses on that treatment indicator. Missing data for five socio-demographic variables were imputed (United States Census Bureau, 2017). Child’s age (missing for 0.1% of the analytic sample), race (0.3%), and ethnicity (0.6%) were imputed using hot-deck imputation and the single imputed values were included in all relevant subgroup analyses. Household poverty ratio (missing for 18.7% of the analytic sample) and household educational attainment (3.0%) were multiply imputed using regression methods and analyses using these variables were conducted separately then merged using standard procedures for combining multiple imputation analyses (Little & Rubin, 2002). Children with missing data for any of the other demographic or clinical indicators were excluded from those subgroup comparisons. All analyses were conducted in SAS-callable SUDAAN version 11.0.1 (RTI International; Cary, NC) in order to account for the complex survey design and to apply sample weights that adjust for probability of selection, nonresponse, and the underlying demographic distribution of the target population.
RESULTS
In 2016, a weighted estimate of 6.1 million U.S. children 2–17 years of age (9.4%) had ever received an ADHD diagnosis by a doctor or other health care provider based on parent report. Of these, 5.4 million currently had ADHD, which was 89.4% of children who had ever been diagnosed with ADHD and 8.4% of all U.S. children 2–17 years of age.
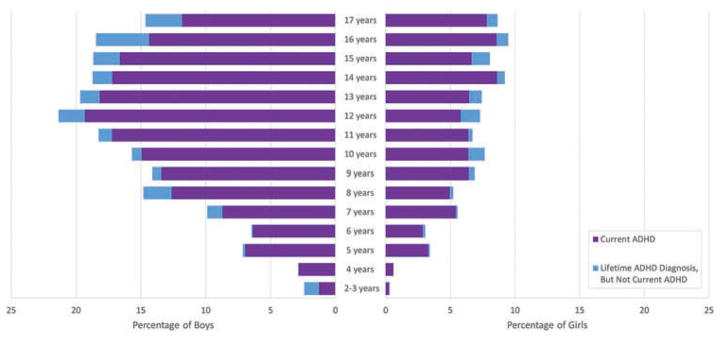
The prevalence of having ever received an ADHD diagnosis and currently having ADHD by parent report was significantly different by each set of demographic groups compared (Table 1). Boys, adolescents 12–17 years of age, Black children, non-Hispanic children, children living in households with English as the primary language, children in the lowest income bracket (i.e., living in households with income less than 100% of the federal poverty level), children with public insurance only or both public and private insurance, children living in the Midwest or South, and children living in rural areas were more likely to have ever received an ADHD diagnosis and to currently have ADHD than their respective counterparts. The weighted percentage of children ever diagnosed with ADHD increased with age, with 2.4% of young children (2–5 years; approximately 388,000 children), 9.6% of school-age children (6–11 years; 2.4 million), and 13.6% of adolescents (12–17 years; 3.3 million) having ever received an ADHD diagnosis. The prevalence of current ADHD also increased with age, as 2.1% of young children (an estimated 335,000 children), 8.9% of school-age children (2.2 million), and 11.9% of adolescents (2.9 million) were reported to currently have ADHD. For boys, the prevalence of ever-diagnosed and current ADHD was highest at age 12, whereas the prevalence for girls for ever having received an ADHD diagnosis was highest at age 16 (Figure 1).
TABLE 1.
Weighted Prevalence Estimates of Parent-Reported ADHD Diagnosis by a Health Care Provider in Children 2–17 Years of Age by Demographic Subgroups, National Survey of Children’s Health, 2016
| Unweighted Sample Size | Ever Received ADHD Diagnosis | Has Current ADHD | |||
|---|---|---|---|---|---|
|
|
|
||||
| Weighted % [95% CI] | PR [95% CI] | Weighted % [95% CI] | PR [95% CI] | ||
| Overall (2–17 Years) | 45,736 | 9.4 [8.8, 9.9] | 8.4 [7.9, 8.9] | ||
| 3–17 Years | 42,935 | 9.9 [9.4, 10.5] | 8.9 [8.4, 9.4] | ||
| 4–17 Years | 40,422 | 10.5 [9.9, 11.1] | 9.4 [8.9, 10.0] | ||
| Sex | |||||
| Male | 23,400 | 12.9 [12.0, 13.8] | 2.29 [2.04, 2.58] | 11.5 [10.7, 12.4] | 2.27 [2.01, 2.56] |
| Female | 22,336 | 5.6 [5.1, 6.2] | Ref. | 5.1 [4.6, 5.6] | Ref. |
| Age | |||||
| 2–5 Years | 10,320 | 2.4 [1.6, 3.7] | 0.25 [0.17, 0.39] | 2.1 [1.4, 3.2] | 0.24 [0.16, 0.36] |
| 6–11 Years | 14,873 | 9.6 [8.8, 10.5] | Ref. | 8.9 [8.2, 9.7] | Ref. |
| 12–17 Years | 20,543 | 13.6 [12.7, 14.6] | 1.41 [1.26, 1.58] | 11.9 [11.1, 12.8] | 1.34 [1.19, 1.50] |
| Race | |||||
| White | 35,470 | 9.4 [8.9, 10.0] | Ref. | 8.4 [7.9, 8.9] | Ref. |
| Black | 2,827 | 12.0 [10.1, 14.1] | 1.27 [1.06, 1.52] | 10.7 [9.0, 12.6] | 1.27 [1.06, 1.52] |
| Other | 7,439 | 7.1 [5.9, 8.6] | 0.76 [0.62, 0.92] | 6.6 [5.4, 8.0] | 0.78 [0.63, 0.96] |
| Ethnicity | |||||
| Hispanic/Latino | 4,990 | 6.7 [5.6, 8.0] | 0.65 [0.54, 0.79] | 6.0 [4.9, 7.3] | 0.66 [0.54, 0.80] |
| Non-Hispanic/Latino | 40,746 | 10.2 [9.7, 10.8] | Ref. | 9.1 [8.6, 9.7] | Ref. |
| Primary Language in Home | |||||
| English | 42,581 | 10.4 [9.8, 11.0] | Ref. | 9.3 [8.8, 9.8] | Ref. |
| Spanish | 1,256 | 3.8 [2.3, 6.2] | 0.36 [0.22, 0.60] | 3.4 [2.0, 5.8] | 0.37 [0.21, 0.63] |
| Other Language | 1,565 | 1.3 [0.9, 2.1] | 0.13 [0.08, 0.20] | 1.1 [0.7, 1.7] | 0.12 [0.07, 0.19] |
| Highest Education in Householda | |||||
| Less Than High School | 1,532 | 8.5 [6.6, 10.9] | 0.92 [0.71, 1.19] | 7.8 [6.0, 10.1] | 0.96 [0.73, 1.25] |
| 12 Years, High School Graduate | 7,602 | 10.2 [9.1, 11.5] | 1.11 [0.97, 1.27] | 9.5 [8.4, 10.7] | 1.17 [1.02, 1.34] |
| More Than High School | 36,602 | 9.2 [8.6, 9.8] | Ref. | 8.1 [7.6, 8.6] | Ref. |
| Poverty Statusa | |||||
| < 100% of Federal Poverty Level | 4,467 | 10.6 [9.2, 12.1] | 1.22 [1.04, 1.44] | 10.0 [8.7, 11.5] | 1.31 [1.12, 1.54] |
| 100%–199% of Federal Poverty Level | 7,311 | 10.0 [8.6, 11.5] | 1.15 [0.98, 1.36] | 8.7 [7.5, 10.2] | 1.15 [0.97, 1.36] |
| > 200% of Federal Poverty Level | 33,958 | 8.7 [8.1, 9.3] | Ref. | 7.6 [7.1, 8.2] | Ref. |
| Type of Health Insurance | |||||
| Public Only | 8,272 | 12.5 [11.2, 13.8] | 1.64 [1.45, 1.86] | 11.6 [10.4, 12.9] | 1.74 [1.54, 1.98] |
| Private Only | 33,519 | 7.6 [7.1, 8.1] | Ref. | 6.6 [6.2, 7.1] | Ref. |
| Public and Private | 1,643 | 16.0 [12.7, 20.1] | 2.11 [1.66, 2.68] | 12.9 [10.3, 16.0] | 1.94 [1.54, 2.45] |
| Unspecified | 505 | 7.5 [4.6, 12.0] | 0.99 [0.61, 1.61] | 7.4 [4.5, 11.9] | 1.11 [0.68, 1.82] |
| None | 1,640 | 6.1 [4.4, 8.3] | 0.80 [0.58, 1.10] | 5.4 [3.8, 7.6] | 0.82 [0.58, 1.16] |
| Region | |||||
| Northeast | 8,633 | 8.4 [7.3, 9.5] | 1.23 [0.99, 1.53] | 7.7 [6.7, 8.9] | 1.35 [1.08, 1.68] |
| Midwest | 12,012 | 10.1 [9.2, 11.0] | 1.49 [1.22, 1.80] | 9.3 [8.5, 10.2] | 1.63 [1.34, 1.98] |
| South | 13,438 | 11.0 [10.1, 12.0] | 1.63 [1.34, 1.97] | 9.8 [8.9, 10.7] | 1.71 [1.41, 2.08] |
| West | 11,653 | 6.8 [5.7, 8.0] | Ref. | 5.7 [4.8, 6.8] | Ref. |
| Urbanicity | |||||
| Rural | 8,442 | 11.8 [10.5, 13.2] | 1.30 [1.14, 1.49] | 10.9 [9.7, 12.3] | 1.36 [1.19, 1.56] |
| Urban/Suburban | 37,294 | 9.0 [8.5, 9.6] | Ref. | 8.0 [7.5, 8.6] | Ref. |
Note: PR in bold indicates statistically significant difference from reference group at the α = 0.05 level. ADHD = attention deficit hyperactivity disorder; CI = confidence interval; PR = prevalence ratio.
Multiple imputation was used to estimate values for respondents with missing data on indicators used to calculate poverty status (data were imputed for 18.7% of respondents represented in this table) and household educational attainment (3.0% imputed).
FIGURE 1.
Weighted prevalence estimates of parent-reported attention deficit/hyperactivity disorder (ADHD) diagnosis among children and adolescents by age, National Survey of Children’s Health, 2016.
Among children with current ADHD, 14.5% were reported to have severe ADHD, 43.7% had moderate ADHD, and 41.8% had mild ADHD. Nearly two thirds (63.8%) of children with current ADHD had at least one current co-occurring condition; behavioral or conduct problems were the most common type of co-occurring condition reported (51.5% of all children with current ADHD), followed by anxiety problems (32.7%), depression (16.8%), autism spectrum disorder (13.7%), and Tourette syndrome (1.2%). A small percentage (1.0%) of adolescents 12–17 years of age with current ADHD had a parent-reported current substance use disorder.
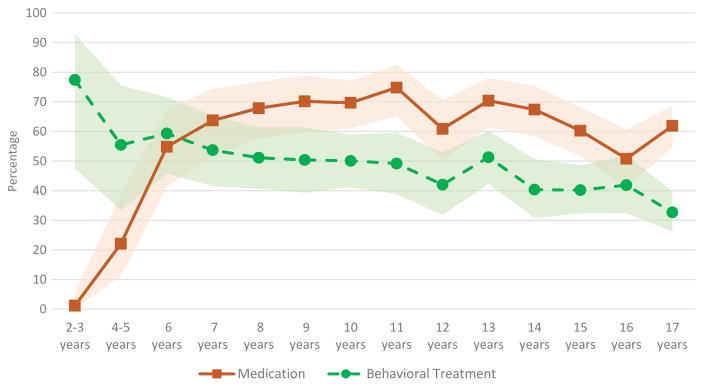
Of children with current ADHD, 62.0% were reported to be currently taking medication for their ADHD, representing 5.1% of all U.S. children 2–17 years of age (approximately 3.3 million children). There was not a statistically significant difference in the weighted estimates of ADHD medication use between boys and girls with current ADHD; however, non-Hispanic children, children living in homes where English was the primary language, and children living in the South were more likely to be taking medication than their counterparts (Table 2). There was also a statistically significant difference in medication rates by age group. Young children 2–5 years of age with current ADHD were less likely to be taking ADHD medication (18.2%; approximately 61,000 young children) than school-age children (68.6%, PR = 3.76, 1.5 million), 95% CI [2.05, 6.91], or adolescents (62.1%, PR = 3.41, 1.8 million), 95% CI [1.86–6.27]. The age at which the highest percentage of children with current ADHD were taking medication was 11 years (Figure 2). Children with mild ADHD (46.1%) were less likely to be taking medication than children with moderate ADHD (70.3%, PR = 1.53), 95% CI [1.36, 1.72], or severe ADHD (81.6%, PR = 1.77), 95% CI [1.56, 2.01] (Table 2). Children with current ADHD and a current co-occurring condition were more likely to be taking ADHD medication (66.6%, PR = 1.23), 95% CI [1.10, 1.38], than children without a reported co-occurring condition (54.0%).
TABLE 2.
Weighted Prevalence of Receipt of Nonmutually Exclusive Treatment Types for ADHD Among Children 2–17 Years of Age With Current ADHD by Demographic Subgroups, National Survey of Children’s Health, 2016
| Unweighted Sample Sizea | Currently Taking ADHD Medication | Received Behavioral Treatment for ADHD in Past 12 Months | Received Behavioral Treatment for ADHD or Any Treatment/Counseling From a Mental Health Provider in Past 12 Months | ||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| Weighted % [95% CI] | PR [95% CI] | Weighted % [95% CI] | PR [95% CI] | Weighted % [95% CI] | PR [95% CI] | ||
| Overall | 4,259 | 62.0 [58.9, 65.0] | 46.7 [43.7, 49.7] | 59.9 [57.0, 62.7] | |||
| Sex | |||||||
| Male | 2,930 | 63.6 [59.8, 67.2] | 1.09 [0.98, 1.22] | 48.6 [44.9, 52.4] | 1.16 [1.01, 1.33] | 59.7 [56.1, 63.1] | 0.99 [0.89, 1.09] |
| Female | 1,329 | 58.1 [52.9, 63.1] | Ref. | 42.0 [37.2, 47.0] | Ref. | 60.4 [55.3, 65.3] | Ref. |
| Age | |||||||
| 2–5 Years | 137 | 18.2b [9.6, 31.8] | 0.27 [0.14, 0.49] | 59.5 [40.2, 76.3] | 1.16 [0.83, 1.61] | 62.9 [43.3, 79.0] | 1.01 [0.75, 1.37] |
| 6–11 Years | 1,566 | 68.6 [64.3, 72.5] | Ref. | 51.4 [46.9, 55.9] | Ref. | 62.1 [57.7, 66.4] | Ref. |
| 12–17 Years | 2,556 | 62.1 [58.4, 65.8] | 0.91 [0.83, 0.99] | 41.7 [37.9, 45.6] | 0.81 [0.71, 0.92] | 57.9 [54.1, 61.5] | 0.93 [0.85, 1.02] |
| Race | |||||||
| White | 3,416 | 63.3 [60.1, 66.3] | Ref. | 43.1 [40.0, 46.2] | Ref. | 57.4 [54.3, 60.5] | Ref. |
| Black | 315 | 61.9 [53.2, 70.0] | 0.98 [0.85, 1.13] | 55.9 [47.2, 64.3] | 1.30 [1.09, 1.54] | 64.1 [55.2, 72.2] | 1.12 [0.97, 1.29] |
| Other | 528 | 55.9 [45.2, 66.0] | 0.88 [0.73, 1.07] | 52.3 [42.2, 62.2] | 1.21 [0.99, 1.49] | 66.2 [57.4, 74.0] | 1.15 [1.00, 1.32] |
| Ethnicity | |||||||
| Hispanic/Latino | 424 | 50.5 [40.8, 60.2] | 0.78 [0.64, 0.96] | 51.8 [42.2, 61.3] | 1.14 [0.93, 1.39] | 63.8 [54.5, 72.2] | 1.08 [0.93, 1.25] |
| Non-Hispanic/Latino | 3,835 | 64.4 [61.5, 67.3] | Ref. | 45.6 [42.6, 48.6] | Ref. | 59.0 [56.1, 61.9] | Ref. |
| Primary Language in Home | |||||||
| English | 4,133 | 63.0 [60.1, 65.9] | Ref. | 46.5 [43.5, 49.5] | Ref. | 59.5 [56.6, 62.4] | Ref. |
| Spanish | 62 | 32.3b [15.3, 55.7] | 0.51 [0.26, 0.99] | 49.1 [24.3, 74.4] | 1.06 [0.60, 1.86] | 67.4 [45.0, 84.0] | 1.13 [0.83, 1.54] |
| Other Language | 34 | 37.6 [19.9, 59.3] | 0.60 [0.34, 1.04] | 53.7 [31.7, 74.4] | 1.16 [0.75, 1.77] | 55.0 [32.7, 75.4] | 0.92 [0.61, 1.40] |
| Highest Education in Householdc | |||||||
| Less Than High School | 179 | 60.4 [46.0, 73.2] | 0.98 [0.77, 1.24] | 55.1 [42.4, 67.2] | 1.17 [0.92, 1.50] | 69.7 [57.9, 79.3] | 1.17 [0.99, 1.38] |
| 12 Years, High School Graduate | 805 | 63.6 [57.4, 69.4] | 1.03 [0.93, 1.15] | 42.2 [36.0, 48.7] | 0.90 [0.76, 1.07] | 56.3 [49.9, 62.4] | 0.95 [0.84, 1.07] |
| More Than High School | 3,276 | 61.6 [58.2, 64.9] | Ref. | 46.9 [43.6, 50.3] | Ref. | 59.5 [56.3, 62.7] | Ref. |
| Poverty Statusc | |||||||
| < 100% of Federal Poverty Level | 608 | 58.8 [52.1, 65.3] | 0.92 [0.82, 1.05] | 51.4 [44.4, 58.4] | 1.19 [1.00, 1.41] | 61.3 [54.3, 67.9] | 1.07 [0.93, 1.22] |
| 100%–199% of Federal Poverty Level | 779 | 61.6 [53.4, 69.2] | 0.97 [0.84, 1.12] | 49.2 [41.5, 56.9] | 1.14 [0.95, 1.36] | 63.8 [56.6, 70.4] | 1.11 [0.97, 1.27] |
| > 200% of Federal Poverty Level | 2,872 | 63.7 [60.0, 67.1] | Ref. | 43.3 [39.6, 47.0] | Ref. | 57.4 [53.6, 61.1] | Ref. |
| Type of Health Insurance | |||||||
| Public Only | 1,214 | 63.6 [58.0, 68.9] | 1.03 [0.93, 1.14] | 55.0 [49.6, 60.2] | 1.38 [1.21, 1.56] | 67.5 [62.6, 72.1] | 1.27 [1.15, 1.40] |
| Private Only | 2,577 | 62.0 [58.4, 65.4] | Ref. | 40.0 [36.7, 43.4] | Ref. | 53.3 [49.8, 56.8] | Ref. |
| Public and Private | 288 | 64.4 [53.4, 74.0] | 1.04 [0.87, 1.23] | 48.9 [37.8, 60.1] | 1.22 [0.96, 1.57] | 64.8 [53.4, 74.7] | 1.21 [1.02, 1.45] |
| Unspecified | 42 | 60.5 [38.0, 79.3] | 0.98 [0.68, 1.41] | 44.0 [23.1, 67.3] | 1.10 [0.64, 1.90] | 66.2 [41.6, 84.4] | 1.24 [0.88, 1.76] |
| None | 119 | 43.0 [28.3, 59.0] | 0.69 [0.48, 1.01] | 31.3 [19.5, 46.3] | 0.78 [0.50, 1.22] | 41.6 [27.0, 57.8] | 0.78 [0.53, 1.15] |
| Region | |||||||
| Northeast | 774 | 59.2 [52.1, 65.9] | 1.13 [0.92, 1.39] | 47.3 [40.2, 54.6] | 0.84 [0.68, 1.04] | 64.8 [57.9, 71.2] | 0.97 [0.84, 1.12] |
| Midwest | 1,087 | 62.4 [57.1, 67.3] | 1.19 [0.99, 1.43] | 45.9 [40.9, 50.9] | 0.82 [0.68, 0.98] | 61.9 [56.8, 66.7] | 0.92 [0.81, 1.05] |
| South | 1,509 | 66.3 [61.5, 70.7] | 1.26 [1.05, 1.52] | 43.5 [38.8, 48.2] | 0.78 [0.65, 0.93] | 54.6 [49.9, 59.2] | 0.81 [0.71, 0.93] |
| West | 889 | 52.4 [43.6, 61.0] | Ref. | 56.1 [47.8, 64.0] | Ref. | 67.0 [59.9, 73.4] | Ref. |
| Urbanicity | |||||||
| Rural | 823 | 61.1 [54.2, 67.6] | 0.98 [0.87, 1.11] | 39.0 [33.2, 45.1] | 0.81 [0.68, 0.96] | 49.0 [42.7, 55.4] | 0.79 [0.69, 0.91] |
| Urban/Suburban | 3,413 | 62.2 [58.7, 65.4] | Ref. | 48.1 [44.8, 51.6] | Ref. | 61.9 [58.7, 65.0] | Ref. |
| ADHD Severity | |||||||
| Mild | 1,871 | 46.0 [41.4, 50.7] | Ref. | 32.1 [27.4, 37.1] | Ref. | 47.0 [42.2, 51.8] | Ref. |
| Moderate | 1,870 | 70.3 [66.0, 74.3] | 1.53 [1.36, 1.72] | 52.4 [47.9, 56.8] | 1.63 [1.37, 1.94] | 64.5 [60.3, 68.6] | 1.37 [1.22, 1.55] |
| Severe | 471 | 81.6 [74.5, 87.0] | 1.77 [1.56, 2.01] | 71.2 [63.2, 78.0] | 2.22 [1.85, 2.67] | 82.7 [76.2, 87.7] | 1.76 [1.56, 1.99] |
| Current Co-Occurring | |||||||
| Disorder | |||||||
| Yes | 2,676 | 66.6 [63.0, 70.0] | 1.23 [1.10, 1.38] | 57.5 [53.8, 61.1] | 2.07 [1.67, 2.56] | 73.1 [69.7, 76.2] | 1.99 [1.70, 2.33] |
| No | 1,568 | 54.0 [48.6, 59.3] | Ref. | 27.8 [22.5, 33.9] | Ref. | 36.8 [31.4, 42.5] | Ref. |
Note: PR in bold indicates statistically significant difference from reference group at the α = 0.05 level. Children receiving more than one treatment type are represented in the percentages for each treatment as appropriate. ADHD = attention deficit hyperactivity disorder; CI = confidence interval; PR = prevalence ratio.
Includes all respondents reported to have current ADHD and with a valid response to at least one ADHD treatment indicator.
Estimate is unstable and may be unreliable. It has a relative standard error between 30% and 50% and should be interpreted with caution.
Multiple imputation was used to estimate values for respondents with missing data on indicators used to calculate poverty status (data were imputed for 19.3% of respondents represented in this table) and household educational attainment (3.6% imputed).
FIGURE 2.
Weighted prevalence estimates of nonmutually exclusive parent-reported treatment types among children and adolescents with current attention deficit/hyperactivity disorder by age, National Survey of Children’s Health, 2016. Note: Shaded area represents 95% confidence interval for treatment point estimates by age. Children receiving both medication and behavioral treatment are represented in both lines.
Slightly less than half of children with current ADHD had received a behavioral treatment for their ADHD in the past 12 months (46.7%; 2.5 million children). The overall patterns of demographic differences for behavioral treatment rates were different than for ADHD medication (Table 2). Adolescents were less likely to have received behavioral treatment than younger children, and boys were more likely than girls to have received behavioral treatment. Black children were more likely than White children, and children with public insurance alone were more likely than children with private insurance alone, to have received behavioral treatment. Children living in the South or Midwest and children living in a rural area were less likely to receive behavioral treatment than children living in the West or in an urban/suburban area, respectively. However, similar to medication rates, behavioral treatment rates were higher for those with more severe ADHD and for children with a current co-occurring condition. Children 2–3 years of age with current ADHD had the highest percentage of behavioral treatment receipt in the past year (77.4%), followed by children 6 years of age (59.3%) and children 4–5 years of age (55.4%; Figure 2).
Among children who were reported not to have received behavioral treatment for their ADHD in the past 12 months (53.3% of children with current ADHD), nearly one fourth (24.4%) were reported to have received treatment or counseling from a mental health provider in the previous 12 months. Overall, 59.9% of children and adolescents with current ADHD had received behavioral treatment for their ADHD and/or any treatment or counseling from a mental health professional in the prior year. There were slight differences in the treatment patterns by demographic subgroups when receipt of any mental health treatment or counseling from a mental health professional is considered along with behavioral treatment specific to ADHD (Table 2). Of note, differences by sex, age, and race observed for receipt of behavioral treatment were narrowed or eliminated when the broader indicator of receipt of any mental health treatment (behavioral treatment for ADHD and/or treatment or counseling from a mental health professional) was examined in the analysis.
Considering combinations of current medication and behavioral treatment for ADHD in the past year, nearly one third of children with current ADHD had received both types of treatment (31.7%). More children had received medication alone (30.3%) than behavioral treatment alone (14.9%), and nearly one fourth (23.0%) had received neither treatment. There were significant differences in the combinations of medication and behavioral treatment by several demographic and clinical characteristics (Table 3). Young children 2–5 years of age with current ADHD were most likely to receive behavioral treatment alone (45.8%) or neither treatment (36.0%), whereas older children were more likely to receive medication with or without behavioral treatment. Black children were most likely to get both medication and behavioral treatment, whereas White children were the most likely to receive medication alone. Nearly half of children with current ADHD and no health insurance received neither treatment (49.1%), compared to 19.3% to 31.0% of children with the other types of health insurance. Children living in the West were more likely to get behavioral treatment alone and less likely to get medication alone than children living in other parts of the country. Children living in rural areas were more likely to get neither treatment than children living in urban/suburban areas. Children with severe ADHD and children with a current co-occurring condition were more likely to get medication and behavioral treatment together than children with mild or moderate ADHD and children with no co-occurring conditions, respectively; children with mild or moderate ADHD and children with no co-occurring conditions were more likely to receive neither treatment than children with severe ADHD or any co-occurring condition.
TABLE 3.
Mutually Exclusive Combinations of Treatment Types (Current ADHD Medication and past Year Behavioral Treatment for ADHD) Among Children 2–17 Years of Age With Current ADHD by Demographic Subgroups, National Survey of Children’s Health, 2016
| ADHD Medication and Behavioral Treatment for ADHD | ADHD Medication Only | Behavioral Treatment for ADHD Only | Neither ADHD Medication Nor Behavioral Treatment for ADHD | χ2 p | |
|---|---|---|---|---|---|
|
|
|
|
|
||
| Weighted % [95% CI] | Weighted % [95% CI] | Weighted % [95% CI] | Weighted % [95% CI] | ||
| Overall | 31.7 [29.0, 34.6] | 30.3 [27.8, 33.0] | 14.9 [12.5, 17.7] | 23.0 [20.6, 25.6] | |
| Sex | |||||
| Male | 33.3 [29.8, 36.9] | 30.4 [27.3, 33.7] | 15.3 [12.3, 19.0] | 21.0 [18.3, 24.0] | .0852 |
| Female | 28.0 [23.9, 32.6] | 30.2 [25.9, 35.0] | 13.9 [10.6, 17.9] | 28.0 [23.9, 32.6] | |
| Age | |||||
| 2–5 Years | 13.7a [6.4, 26.8] | 4.5a [1.9, 10.1] | 45.8 [26.3, 66.7] | 36.0 [20.3, 55.4] | < .0001 |
| 6–11 Years | 37.3 [33.0, 41.7] | 31.5 [27.3, 35.9] | 14.0 [11.4, 17.2] | 17.3 [14.1, 20.9] | |
| 12–17 Years | 29.7 [26.0, 33.6] | 32.5 [29.2, 36.0] | 12.0 [9.6, 14.8] | 25.8 [22.7, 29.2] | |
| Race | |||||
| White | 29.5 [26.8, 32.2] | 33.8 [30.9, 36.9] | 13.6 [11.3, 16.2] | 23.1 [20.6, 25.9] | .0203 |
| Black | 41.2 [32.6, 50.3] | 20.8 [15.1, 27.9] | 14.7 [10.1, 20.9] | 23.3 [16.4, 32.1] | |
| Other | 30.9 [22.3, 41.0] | 25.6 [19.0, 33.5] | 21.5 [12.1, 35.3] | 22.1 [16.0, 29.7] | |
| Ethnicity | |||||
| Hispanic/Latino | 30.0 [22.0, 39.4] | 20.9 [15.1, 28.3] | 21.9 [13.3, 33.8] | 27.2 [19.9, 36.0] | .0260 |
| Non-Hispanic/Latino | 32.1 [29.3, 35.0] | 32.3 [29.6, 35.2] | 13.4 [11.4, 15.7] | 22.1 [19.8, 24.7] | |
| Primary Language in Home | |||||
| English | 32.3 [29.5, 35.2] | 30.9 [28.3, 33.6] | 14.2 [12.2, 16.5] | 22.7 [20.3, 25.3] | .0314 |
| Spanish | 14.5a [6.1, 30.7] | 17.8a [6.5, 40.3] | 34.7a [11.2, 69.1] | 33.1a [16.3, 55.6] | |
| Other Language | 27.2a [12.6, 49.2] | 10.4a [3.9, 24.7] | 26.5a [10.3, 53.2] | 35.9a [17.4, 59.8] | |
| Highest Education in Householdb | |||||
| Less than High School | 40.5 [28.4, 53.9] | 20.6 [13.2, 30.7] | 14.7a [5.2, 35.0] | 24.2 [15.7, 35.4] | .1468 |
| 12 Years, High School Graduate | 30.5 [24.7, 36.8] | 33.1 [27.3, 39.5] | 11.7 [8.6, 15.8] | 24.7 [19.6, 30.7] | |
| More than High School | 30.6 [27.6, 33.8] | 31.0 [28.1, 34.1] | 16.2 [13.6, 19.3] | 22.1 [19.5, 25.0] | |
| Poverty Statusb | |||||
| < 100% of Federal Poverty Level | 35.5 [28.9, 42.7] | 23.4 [18.3, 29.5] | 16.1 [11.7, 21.6] | 25.0 [19.2, 31.9] | .0769 |
| 100–199% of Federal Poverty Level | 33.4 [26.4, 41.3] | 28.3 [22.5, 34.9] | 15.8 [9.4, 25.4] | 22.5 [17.2, 28.8] | |
| > 200% of Federal Poverty Level | 29.1 [26.1, 32.4] | 34.5 [31.2, 38.1] | 14.0 [11.4, 17.1] | 22.3 [19.4, 25.6] | |
| Type of Health Insurance | |||||
| Public Only | 38.0 [32.8, 43.5] | 25.6 [21.4, 30.2] | 17.1 [12.4, 22.9] | 19.3 [15.8, 23.4] | .0006 |
| Private Only | 25.7 [23.0, 28.6] | 36.3 [32.9, 39.8] | 14.1 [11.7, 16.9] | 23.9 [20.8, 27.3] | |
| Public and Private | 36.9 [26.4, 48.8] | 27.3 [18.3, 38.7] | 11.9 [7.1, 19.2] | 23.8 [15.7, 34.5] | |
| Unspecified | 35.5a [16.2, 61.1] | 25.0a [9.8, 50.5] | 8.5c [2.9, 22.6] | 31.0a [14.7, 54.0] | |
| None | 22.8 [13.3, 36.4] | 19.6 [11.2, 32.0] | 8.5a [3.6, 18.9] | 49.1 [32.4, 66.0] | |
| Region | |||||
| Northeast | 27.9 [21.6, 35.3] | 31.8 [25.5, 38.9] | 19.4 [14.4, 25.7] | 20.9 [16.1, 26.6] | .0038 |
| Midwest | 30.4 [26.1, 34.9] | 32.0 [27.5, 36.8] | 15.3 [11.7, 19.8] | 22.4 [18.2, 27.1] | |
| South | 33.3 [29.0, 38.0] | 32.9 [28.8, 37.3] | 10.1 [7.6, 13.4] | 23.6 [19.7, 28.0] | |
| West | 32.7 [25.4, 40.8] | 19.6 [14.6, 25.9] | 23.4 [14.8, 34.9] | 24.3 [19.1, 30.4] | |
| Urbanicity | |||||
| Rural | 28.7 [23.8, 34.2] | 32.5 [27.1, 38.4] | 10.0 [6.7, 14.8] | 28.8 [22.6, 35.9] | .0479 |
| Urban/Suburban | 32.3 [29.2, 35.6] | 29.9 [27.1, 32.9] | 15.8 [13.1, 19.0] | 21.9 [19.4, 24.7] | |
| ADHD Severity | |||||
| Mild | 14.7 [12.1, 17.8] | 31.5 [27.5, 35.7] | 17.2 [13.0, 22.5] | 36.6 [32.2, 41.3] | < .0001 |
| Moderate | 38.1 [33.8, 42.6] | 32.4 [28.5, 36.6] | 14.4 [11.3, 18.1] | 15.1 [12.3, 18.4] | |
| Severe | 59.5 [51.0, 67.4] | 22.0 [15.9, 29.6] | 11.6 [7.2, 18.2] | 6.9 [4.0, 11.6] | |
| Current Co-Occurring | |||||
| Disorder | |||||
| Yes | 41.0 [37.4, 44.7] | 25.7 [22.6, 29.1] | 16.6 [14.0, 19.6] | 16.7 [14.2, 19.5] | < .0001 |
| No | 15.5 [11.8, 20.2] | 38.5 [34.0, 43.3] | 12.1 [7.8, 18.3] | 33.9 [29.2, 38.9] | |
Note: ADHD = attention deficit hyperactivity disorder; CI = confidence interval; PR = prevalence ratio.
Estimate is unstable and may be unreliable. It has a relative standard error between 30% and 50% and should be interpreted with caution.
Multiple imputation was used to estimate values for respondents with missing data on indicators used to calculate poverty status (data were imputed for 19.3% of respondents represented in this table) and household educational attainment (3.6% imputed).
Estimate is unreliable. It has a relative standard error larger than 50% and should not be used except for inferential statistics (e.g., comparisons with other estimates).
DISCUSSION
This study provides an updated epidemiological profile of ADHD diagnosis and treatment among noninstitutionalized children 2–17 years of age in the United States using national survey data collected in 2016. These results indicate that there were approximately 6.1 million children and adolescents in the United States who have ever received an ADHD diagnosis from a health care provider and 5.4 million children and adolescents who currently had ADHD. Approximately two thirds of children with current ADHD (62.0%) were currently taking medication for their ADHD, and slightly less than half (46.7%) had received behavioral treatment for ADHD during the previous 12 months.
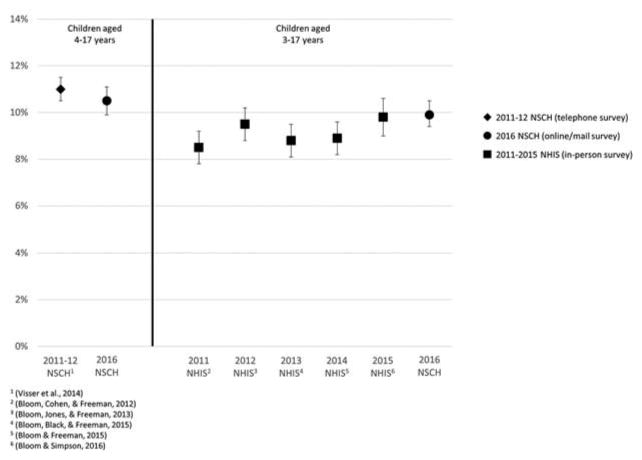
Due to significant methodological changes in the sampling and administration of the NSCH (United States Census Bureau, 2017), the 2016 data on ADHD prevalence and medication use and data from the same survey in previous years are not directly comparable statistically. However, the estimated prevalence of ever-diagnosed ADHD from the 2016 NSCH was consistent with published estimates from the National Health Interview Survey and previous administrations of the NSCH (Figure 3; Bloom, Black, & Freeman, 2015; Bloom, Cohen, & Freeman, 2012; Bloom & Freeman, 2015; Bloom, Jones, & Freeman, 2013; Bloom & Simpson, 2016; Visser et al., 2014). Results from administrative claims data over a similar period (2009–2015) have suggested that there may be subgroup differences in trends of diagnosed prevalence over time by type of insurance; there has been a steady increase in the prevalence of diagnosed ADHD among children 6–17 years of age with employer-sponsored insurance, whereas the proportion of children in Medicaid diagnosed with ADHD has plateaued from 2012 to 2015 (Nyarko et al., 2017). Detection of these types of subgroup differences over time may be used to identify differences in frequency of diagnosis for subpopulations of children and to recognize changes in the underlying population of children being diagnosed with ADHD. The 2016 NSCH estimates provide an important baseline from which to evaluate forthcoming annual NSCH data to identify the patterns in trends over time for these ADHD prevalence and treatment indicators overall and by demographic subgroups.
FIGURE 3.
Weighted prevalence estimates and 95% confidence intervals for children who have ever received an ADHD diagnosis from a health care provider, National Survey of Children’s Health (NSCH; 2011–2012–2016) and National Health Interview Survey (NHIS; 2011–2015).
Looking specifically at young children with ADHD, from 2007–2008 to 2011–2012, there was a 57% increase (from 1.0% to 1.5%) noted in the percentage of children 2–5 years of age with current ADHD (Danielson et al., 2017b). In the present study, an estimated 2.1% of children 2–5 years of age were reported to have current ADHD. This result provides additional evidence of an increasing trend in the prevalence of current ADHD in this age group, though there were differences in survey methodology for these sets of estimates. The higher prevalence observed for 2016 is consistent with a study of insurance claims data that showed an increase in the percentage of children 2–5 years of age receiving clinical care for ADHD from 2008 to 2014 (Visser et al., 2016) and a study of electronic health record data that showed an increase in the percentage of children 4–5 years of age with pediatric clinic visits associated with ADHD care from 2008 to 2014, though the rate of increase had slowed in this population after implementation of the AAP guidelines in 2011 (Fiks et al., 2016).
This report presents prevalence estimates for both ever-diagnosed ADHD and current ADHD. These prevalence estimates and their relationship to associated demographic and clinical characteristics are similar because nearly 90% of children who had ever received an ADHD diagnosis were reported to currently have the disorder. There is an increasing acknowledgment of ADHD as a chronic condition with symptoms and impairment that can persist into adolescence and adulthood for many individuals who were diagnosed during childhood (Agnew-Blais et al., 2016; Faraone, Biederman, & Mick, 2006; Holbrook et al., 2016). Changes made to the diagnostic criteria for ADHD in DSM-5 have broadened the definition of symptoms and impairment to be more applicable to older adolescents and adults, including changes to the minimum age of onset and symptom count, and use of symptom examples that relate to the expected behaviors of older adolescents and adults with ADHD. This combination of criteria changes may affect the number of adolescents and young adults who continue to meet diagnostic criteria for ADHD (Matte et al., 2015; McKeown et al., 2015) and shift the level of recognition on how ADHD-related symptoms and impairment persist beyond childhood.
The demographic patterns for report of a lifetime diagnosis of ADHD in children in 2016 were generally similar to estimates from 2011–2012 (Visser et al., 2014), where boys, non-Hispanic children, and children living in households with English as the primary language, in low-income households, with public insurance, or in the Midwest or South were more likely to have been diagnosed with ADHD than their counterparts. However, the pattern of diagnosed ADHD prevalence by race differed in 2016, where the proportion of Black children who have received an ADHD diagnosis was higher than for White children. Although it is possible that this difference is a function of the changes in NSCH survey methodology, this finding suggests that revisiting previously documented concerns about the underdiagnosis of ADHD in Black children (Coker et al., 2016; Morgan, Staff, Hillemeier, Farkas, & Maczuga, 2013) may be appropriate. Another demographic group with a higher prevalence of diagnosed ADHD is children living in rural areas, who were 30% more likely to have ever received an ADHD diagnosis than children living in urban or suburban areas. This disparity may be explained by the underlying distribution of demographic characteristics of children living in rural areas (Anderson, Neuwirth, Lenardson, & Hartley, 2013). With the limited availability of behavioral health services in rural settings, Kelleher and Gardner (2017) suggested that strategies to ensure that children with ADHD living in rural areas receive appropriate care may be helpful in addressing this disparity.
This study also provides the first nationally representative estimates of the receipt of past-year nonpharmacologi-cal behavioral treatment for ADHD among all U.S. children with ADHD. A recently published study (Danielson et al., 2017a) analyzed data from a 2014 follow-back survey about children and adolescents with ADHD and showed that 62% of children with ADHD had received a psychosocial treatment during their lifetime, though this sample included only children who had the ADHD diagnosis for at least 2 years. Another study using 2009–2010 survey data on the subset of children with current ADHD who also had special health care needs showed that less than half of these children received behavioral treatment in the past year (Visser et al., 2015a), which is consistent with the results from the 2016 NSCH. Patterns of receipt of behavioral treatment for demographic and clinical subgroups were similar for these two populations by age, insurance status, ADHD severity, and presence of a co-occurring condition but differed from the previous study for region of residence such that, in 2016, children with ADHD living in the West had significantly higher rates of behavioral treatment than children living in in the South or Midwest, whereas the Northeast had the highest rates of behavioral treatment based on the 2009–2010 survey. These differences may reflect a change in receipt of behavioral treatment among these regional subgroups over time, though the differences in survey population, survey mode, and exact wording of the associated survey question may also have differentially affected how parents in different regions reported these types of treatments. In addition, patterns of estimates of the receipt of nonpharmacological treatments changed for some demographic subgroups when the receipt of any treatment or counseling from a mental health provider was considered. Although these children may have been receiving treatment for a co-occurring condition or other problems rather than treatment for their ADHD specifically, care from a mental health provider may have indirectly had an impact on the expression of ADHD symptoms and experience of functional impairment. A clinical care algorithm for pediatricians on diagnosing and treating ADHD recognizes the importance of identifying and treating co-occurring conditions among children diagnosed with ADHD, which may include coordinating care with specialists and prioritizing management of the co-occurring condition before addressing treatment for ADHD (Wolraich, Brown, & Brown, 2011).
Reported combinations of received ADHD treatment are of particular interest, as clinical guidelines recommend different treatment combinations based on the age of the child with ADHD. Specifically, behavior therapy is recommended as the first-line treatment for young children with ADHD (AAP, 2011; Gleason et al., 2007), and medication is recommended or preferred in combination with behavior therapy for older children with ADHD (AAP, 2011). The age-specific differences in treatment guidelines for ADHD reflect the differing levels of evidence of effectiveness for behavioral treatment in alleviating symptoms and impairment related to ADHD. A comparative effectiveness review has shown that behavior therapy has a higher strength of evidence for effectiveness than medication in children with ADHD younger than 6 years while also avoiding the potential risks of adverse events associated with ADHD medications (Charach et al., 2013). Psychosocial treatments such as peer intervention and organization training have been found to be effective in school-age children, but there remains a gap in the development of nonpharmacological treatments that have been evaluated and shown to be effective for adolescents (Evans, Owens, & Bunford, 2014).
The results from the 2016 NSCH suggest that the most common combinations of ADHD treatment by age group appear to be consistent with recommendations from clinical guidelines. For adolescents 12–17 years of age, the most common treatment type was medication alone (32.5%), followed by combined medication and behavioral treatment (29.7%), reflecting the recommendation for medication as the first-line treatment for ADHD in this age group, with a preference for the medication to be received in combination with behavior therapy. For children with ADHD 6–11 years of age, the recommended treatment is medication in combination with behavior therapy, and two thirds of children with ADHD in this age group were receiving medication, with slightly more receiving medication in combination with behavioral treatment (37.3%) than medication alone (31.5%). Among young children 2–5 years of age with ADHD, nearly half (45.8%) were receiving behavioral treatment alone, followed by approximately one third (36.0%) receiving neither treatment. Nearly one out of five (18.2%) young children with ADHD were receiving medication with or without behavioral treatment. These findings represent considerably higher estimates of behavioral treatment alone and lower estimates of medication use among this young age group compared to a previous study, where 33.7% received behavioral treatment alone and 44.0% had received medication, either with or without behavioral treatment (Danielson et al., 2017b). With regard to Healthy People 2020 objectives (United States Department of Health and Human Services, 2010), more than half (55.4%) of children 4–5 years of age with ADHD had received behavioral treatment for ADHD in the past year, and most children 6–17 years of age had received medication, behavioral treatment, or both (82.8% of children 6–11 years and 74.2% of adolescents 12–17 years). These results can serve as a baseline for the Healthy People 2020 objective to increase the proportion of children with ADHD who receive recommended treatments. However, it is important to note that these data provide only general indicators of types of treatment received and do not reflect the exact type, quality, duration, sequencing, or appropriateness of the medication or behavioral treatment received. Other national survey data from 2014 have shown that less than one third of children with ADHD have received evidence-based psychosocial treatments such as peer interventions or a parent who has received parent training (Danielson et al., 2017a), suggesting that there is likely a gap in the overall receipt of evidence-based nonpharmacological treatment.
This analysis is subject to several limitations. First, the data collected in this survey rely on parent report of diagnosis and treatment, and these indicators have not been validated against medical records or clinical judgment and may be subject to recall bias. However, previous work has shown that parent report of an ADHD diagnosis results in similar prevalence estimates to those attained through analysis of administrative claims data, suggesting convergent validity of estimated prevalence from both of these data sources (Visser, Danielson, Bitsko, Perou, & Blumberg, 2013). A second limitation is the lack of specificity for the question on receipt of behavioral treatment, as no examples were provided in the question and parents may have been unsure about which treatments should be reported in response to this question. This lack of specificity could potentially lead to an overestimate or underestimate of behavioral treatment receipt, depending on how parents interpret the question relative to the types of treatment and accommodations that their child has received for their ADHD. Relatedly, we were unable to distinguish the quality, type, or duration of the reported behavioral treatment, or specific types of medication, and therefore we cannot estimate the proportion of children with ADHD who were receiving recommended, evidence-based treatments. Finally, the overall response rate of 40.7% should be noted. This may have led to a biased sample; however, the development and application of sample weights to the analyses presented in this study were intended to attenuate bias resulting from nonresponse.
This study provides updated national estimates of the prevalence of diagnosed ADHD among children and adolescents living in the United States and presents population-based estimates of the types of treatment these children were receiving for their ADHD. Although the estimated prevalence of ADHD diagnosis does not appear to have increased in the time since previous nationally representative estimates were published, a sizeable proportion of U.S. children and adolescents have been diagnosed with the disorder, which justifies the continued monitoring of the treatment received and outcomes of this population. This study has also examined how the types of treatment this population received relate to clinical guidelines and Healthy People 2020 goals. These estimates indicate that many, but not all, children with ADHD are receiving treatment that appears to be generally consistent with clinical recommendations from the AAP, though there is limited detail available regarding the specific types of treatments reported in response to these survey questions. Future iterations of the NSCH can be used to continue to monitor the diagnosis and treatment patterns for this highly prevalent and high-impact neurodevelopmental disorder during childhood and adolescence. This information can help clinicians understand ongoing trends in the frequency of the diagnosis of ADHD in the community and the types of treatment received by children with ADHD. Recognition of these trends is particularly important for clinical and school psychologists, as they can play an integral role in the diagnosis and treatment of children with ADHD, particularly for the administration of evidence-based behavioral treatments that have been shown to be effective in improving symptoms and outcomes for children with ADHD.
Footnotes
The questions for the diagnosis of behavioral or conduct problems and substance use disorder also included educators (e.g., teachers and school nurses) along with doctors or other health care providers as providers who could have told parents that their child had these conditions.
DISCLAIMER
The views expressed in this article are those of the authors and do not necessarily reflect the official policies of the U.S. Department of Health and Human Services, the Centers for Disease Control and Prevention, or the Health Resources and Services Administration, nor does mention of the department or agency names imply endorsement by the U.S. government.
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/hcap.
Contributor Information
Melissa L. Danielson, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention
Rebecca H. Bitsko, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention
Reem M. Ghandour, Maternal and Child Health Bureau, Health Resources and Services Administration
Joseph R. Holbrook, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention
Michael D. Kogan, Maternal and Child Health Bureau, Health Resources and Services Administration
Stephen J. Blumberg, National Center for Health Statistics, Centers for Disease Control and Prevention
References
- Agnew-Blais JC, Polanczyk GV, Danese A, Wertz J, Moffitt TE, Arseneault L. Evaluation of the persistence, remission, and emergence of attention-deficit/hyperactivity disorder in young adulthood. JAMA Psychiatry. 2016;73(7):713–720. doi: 10.1001/jamapsychiatry.2016.0465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akinbami LJ, Liu X, Pastor PN, Reuben CA. Attention deficit hyperactivity disorder among children aged 5–17 years in the united states, 1998–2009. Nchs Data Brief. 2011;70:1–8. [PubMed] [Google Scholar]
- American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(7):894–921. doi: 10.1097/chi.0b013e318054e724. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Anderson NJ, Neuwirth SJ, Lenardson JD, Hartley D. Patterns of care for rural and urban children with mental health problems. 2013 Retrieved from https://www.ruralhealthresearch.org/publications/883.
- Bloom B, Black LI, Freeman G. Tables of summary health statistics for U.S. children: 2013 National Health Interview Survey. 2015 Retrieved from http://www.cdc.gov/nchs/nhis/SHS/tables.htm.
- Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey, 2011. Vital and Health Statistics. 2012;10(254):1–88. [PubMed] [Google Scholar]
- Bloom B, Freeman G. Tables of summary health statistics for U.S. children: 2014 National Health Interview Survey. 2015 Retrieved from http://www.cdc.gov/nchs/nhis/SHS/tables.htm.
- Bloom B, Jones LI, Freeman G. Summary health statistics for U.S. children: National health interview survey, 2012. Vital and Health Statistics. 2013;10(258):1–81. [PubMed] [Google Scholar]
- Bloom B, Simpson JL. Tables of summary health statistics for U.S. children: 2015 national health interview survey. 2016 Retrieved from http://www.cdc.gov/nchs/nhis/SHS/tables.htm.
- Charach A, Carson P, Fox S, Ali MU, Beckett J, Lim CG. Interventions for preschool children at high risk for ADHD: A comparative effectiveness review. Pediatrics. 2013;131(5):e1584–e1604. doi: 10.1542/peds.2012-0974. [DOI] [PubMed] [Google Scholar]
- Coker TR, Elliott MN, Toomey SL, Schwebel DC, Cuccaro P, Tortolero Emery S, … Schuster MA. Racial and ethnic disparities in ADHD diagnosis and treatment. Pediatrics. 2016;138(3) doi: 10.1542/peds.2016-0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson ML, Visser SN, Chronis-Tuscano A, DuPaul GJ. A national description of treatment among U.S. children and adolescents with ADHD. Journal of Pediatrics. 2017a doi: 10.1016/j.jpeds.2017.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson ML, Visser SN, Gleason MM, Peacock G, Claussen AH, Blumberg SJ. A national profile of attention-deficit hyperactivity disorder diagnosis and treatment among US children aged 2 to 5 years. Journal of Developmental and Behavioral Pediatrics. 2017b;38(7):455–464. doi: 10.1097/DBP.0000000000000477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dieleman JL, Baral R, Birger M, Bui AL, Bulchis A, Chapin A, … Murray CJ. US spending on personal health care and public health, 1996–2013. JAMA : the Journal of the American Medical Association. 2016;316(24):2627–2646. doi: 10.1001/jama.2016.16885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doshi JA, Hodgkins P, Kahle J, Sikirica V, Cangelosi MJ, Setyawan J, … Neumann PJ. Economic impact of childhood and adult attention-deficit/hyperactivity disorder in the United States. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(10):990–1002. e1002. doi: 10.1016/j.jaac.2012.07.008. [DOI] [PubMed] [Google Scholar]
- Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology. 2014;43(4):527–551. doi: 10.1080/15374416.2013.850700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychological Medicine. 2006;36(2):159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Fiks AG, Ross ME, Mayne SL, Song L, Liu W, Steffes J, Wasserman R. Preschool ADHD diagnosis and stimulant use before and after the 2011 aap practice guideline. Pediatrics. 2016;138(6):1–9. doi: 10.1542/peds.2016-2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming M, Fitton CA, Steiner MFC, McLay JS, Clark D, King A, … Pell JP. Educational and health outcomes of children treated for attention-deficit/hyperactivity disorder. JAMA Pediatrics. 2017;171(7) doi: 10.1001/jamapediatrics.2017.0691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher JM. The effects of childhood ADHD on adult labor market outcomes. Health Economics. 2014;23(2):159–181. doi: 10.1002/hec.2907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleason MM, Egger HL, Emslie GJ, Greenhill LL, Kowatch RA, Lieberman AF, … Zeanah CH. Psychopharmacological treatment for very young children: Contexts and guidelines. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(12):1532–1572. doi: 10.1097/chi.0b013e3181570d9e. [DOI] [PubMed] [Google Scholar]
- Groenman AP, Janssen TWP, Oosterlaan J. Childhood psychiatric disorders as risk factor for subsequent substance abuse: A meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry. 2017;56(7):556–569. doi: 10.1016/j.jaac.2017.05.004. [DOI] [PubMed] [Google Scholar]
- Holbrook JR, Cuffe SP, Cai B, Visser SN, Forthofer MS, Bottai M, … McKeown RE. Persistence of parent-reported ADHD symptoms from childhood through adolescence in a community sample. Journal of Attention Disorders. 2016;20(1):11–20. doi: 10.1177/1087054714539997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelleher KJ, Gardner W. Out of sight, out of mind–Behavioral and developmental care for rural children. New England Journal of Medicine. 2017;376(14):1301–1303. doi: 10.1056/NEJMp1700713. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. 2. Hoboken, NJ: Wiley; 2002. [Google Scholar]
- Matte B, Anselmi L, Salum GA, Kieling C, Goncalves H, Menezes A, … Rohde LA. ADHD in DSM-5: A field trial in a large, representative sample of 18- to 19-year-old adults. Psychological Medicine. 2015;45(2):361–373. doi: 10.1017/S0033291714001470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeown RE, Holbrook JR, Danielson ML, Cuffe SP, Wolraich ML, Visser SN. The impact of case definition on attention-deficit/hyperactivity disorder prevalence estimates in community-based samples of school-aged children. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54(1):53–61. doi: 10.1016/j.jaac.2014.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Arnold LE, Swanson JM, Pelham WE, Hechtman L, … Marcus S. Adolescent substance use in the Multimodal Treatment study of Attention-Deficit/Hyperactivity Disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(3):250–263. doi: 10.1016/j.jaac.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan PL, Staff J, Hillemeier MM, Farkas G, Maczuga S. Racial and ethnic disparities in ADHD diagnosis from kindergarten to eighth grade. Pediatrics. 2013;132(1):85–93. doi: 10.1542/peds.2012-2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyarko KA, Grosse SD, Danielson ML, Holbrook JR, Visser SN, Shapira SK. Treated prevalence of attention-deficit/hyperactivity disorder increased from 2009 to 2015 among school-aged children and adolescents in the United States. Journal of Child and Adolescent Pyschopharmacology. 2017;27(8):731–734. doi: 10.1089/cap.2016.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Gameroff MJ, Marcus SC, Jensen PS. National trends in the treatment of attention deficit hyperactivity disorder. American Journal of Psychiatry. 2003;160(6):1071–1077. doi: 10.1176/appi.ajp.160.6.1071. [DOI] [PubMed] [Google Scholar]
- Perou R, Bitsko RH, Blumberg SJ, Pastor P, Ghandour RM, Gfroerer JC, … Huang LN. Mental health surveillance among children–United States, 2005–2011. Morbidity and Mortality Weekly Report. 2013;62(Suppl 2):1–35. [PubMed] [Google Scholar]
- Ros R, Graziano PA. Social functioning in children with or at risk for attention deficit/hyperactivity disorder: A meta-analytic review. Journal of Clinical Child and Adolescent Psychology. 2017:1–23. doi: 10.1080/15374416.2016.1266644. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Waxmonsky JG, Robb JA, Pelham WE. Implications of changes for the field: ADHD. Journal of Learning Disabilities. 2013;46(1):34–42. doi: 10.1177/0022219412464350. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau, Associate Director of Demographic Programs, National Survey of Children’s Health. 2016 National Survey of Children’s Health frequently asked questions. 2017 Retrieved from https://mchb.hrsa.gov/data/national-surveys/data-user.
- United States Department of Health and Human Services. Healthy people 2020: Improving the health of Americans. 2010 Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/early-and-middle-childhood/objectives.
- Visser SN, Bitsko RH, Danielson ML, Ghandour RM, Blumberg SJ, Schieve LA, … Cuffe SP. Treatment of attention deficit/hyperactivity disorder among children with special health care needs. Journal of Pediatrics. 2015a;166(6):1423–1430. e1422. doi: 10.1016/j.jpeds.2015.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, … Blumberg SJ. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53(1):34–46. e32. doi: 10.1016/j.jaac.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Perou R, Blumberg SJ. Convergent validity of parent-reported attention-deficit/hyperactivity disorder diagnosis: A cross-study comparison. JAMA Pediatrics. 2013;167(7):674–675. doi: 10.1001/jamapediatrics.2013.2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Wolraich ML, Fox MH, Grosse SD, Valle LA, … Peacock G. Vital signs: National and state-specific patterns of attention deficit/hyperactivity disorder treatment among insured children aged 2–5 Years - United States, 2008–2014. Morbidity and Mortality Weekly Report. 2016;65(17):443–450. doi: 10.15585/mmwr.mm6517e1. [DOI] [PubMed] [Google Scholar]
- Visser SN, Zablotsky B, Holbrook JR, Danielson ML, Bitsko RH. Diagnostic experiences of children with attention-deficit/hyperactivity disorder. National Health Statistics Reports. 2015b;81:1–7. [PubMed] [Google Scholar]
- Wolraich M, Brown L, Brown R. Implementing the key action statements: An algorithm and explanation for process of care for the evaluation, diagnosis, treatment, and monitoring of ADHD in children and adolescents. Pediatrics. 2011;128(5):1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]