Abstract
OBJECTIVES
To identify facility- and individual-level predictors of nursing home safety culture.
DESIGN
Cross-sectional survey of individuals within facilities.
SETTING
Nursing homes participating in the national Agency for Healthcare Research and Quality Safety Program for Long-Term Care: Healthcare-Associated Infections/Catheter-Associated Urinary Tract Infections Project.
PARTICIPANTS
Responding nursing home staff (N = 14,177) from 170 (81%) of 210 participating facilities.
MEASUREMENTS
Staff responses to the Nursing Home Survey on Patient Safety Culture (NHSOPS), focused on five domains (teamwork, training and skills, communication openness, supervisor expectations, organizational learning) and individual respondent characteristics (occupation, tenure, hours worked), were merged with data on facility characteristics (from the Certification and Survey Provider Enhanced Reporting): ownership, chain membership, percentage residents on Medicare, bed size. Data were analyzed using multivariate hierarchical models.
RESULTS
Nursing assistants rated all domains worse than administrators did (P < .001), with the largest differences for communication openness (24.3 points), teamwork (17.4 points), and supervisor expectations (16.1 points). Clinical staff rated all domains worse than administrators. Nonprofit ownership was associated with worse training and skills (by 6.0 points, P =.04) and communication openness (7.3 points, P =.004), and nonprofit and chain ownership were associated with worse supervisor expectations (5.2 points, P =.001 and 3.2 points, P =.03, respectively) and organizational learning (5.6 points, P =.009 and 4.2 points, P = .03). The percentage of variation in safety culture attributable to facility characteristics was less than 22%, with ownership having the strongest effect.
CONCLUSION
Perceptions of safety culture vary widely among nursing home staff, with administrators consistently perceiving better safety culture than clinical staff who spend more time with residents. Reporting safety culture scores according to occupation may be more important than facility-level scores alone to describe and assess barriers, facilitators, and changes in safety culture.
Keywords: nursing home, patient safety, safety culture
Developing nursing home environments that promote resident safety can improve outcomes, with some evidence linking better safety culture to fewer falls and pressure ulcers, less restraint use, and other quality-of-care measures.1–3 Safety culture is measured through individual staff expectations for common behaviors and processes regarding safety within a facility, and the Nursing Home Survey on Patient Safety Culture (NHSOPS) tool and its predecessor the Patient Safety Culture (PSC) instrument have been widely used to assess safety culture through surveying multiple individuals working in a nursing home, including those in different clinical, support, and administrative roles.1 Previous studies have found that individual-level characteristics,4,5 including job role and turnover, and facility-level characteristics,1,6 such as ownership, size, and resident case-mix, predict ratings for safety culture. However, the relative importance of these factors on safety culture has not been assessed and could help inform what is most critical for the development of a facility’s safety culture.7
Using data collected within a resident safety collaborative, sponsored by the Agency for Healthcare Research and Quality (AHRQ), we studied how NHSOPS safety culture scores varied by individual- and facility-level characteristics. Based on previous research, it was hypothesized that nonprofit and smaller facilities and facilities with a greater proportion of residents on Medicare would have higher safety culture ratings.3,8 It was also expected that healthcare staff with the most resident contact, including certified nursing assistants and licensed practice nurses would rate safety the poorest, because they more frequently confront complications in resident care.9–11
METHODS
Study Design and Data Sources
This cross-sectional study examined predictors of individual safety culture ratings from the first two cohorts of the AHRQ Safety Program for Long-term Care: Healthcare-Associated Infections (HAIs)/Catheter-Associated Urinary Tract Infections (CAUTI) Project.12 This collaborative was focused on improving safety knowledge and infection prevention practices to reduce HAIs, with a strong focus on CAUTIs. Staff in a range of roles in the nursing homes participating in the collaborative reported on safety culture; these roles included clinicians, nursing professionals and support, and administrative personnel.12
Methods for recruiting facilities and collecting survey data have been described previously.12,13 Facilities were encouraged to have as many staff as possible, regardless of occupation or role, complete the survey, and the national project set a goal of 60% response rate within facilities.14 This analysis included non-federal nursing homes from Florida, Michigan, New Hampshire, New York, South Carolina, and South Dakota (from Cohort 1) and from Arkansas, Connecticut, Massachusetts, Missouri, Pennsylvania, Oklahoma, Oregon, Rhode Island, and Tennessee (from Cohort 2). The University of Michigan Institutional Review Board reviewed this study and determined it to be non-regulated quality improvement activity. Subsequent cohorts also added nursing homes from the Department of Veterans Affairs and remaining states, but those data were not available at the time analyses were completed. Finally, facilities with fewer than five respondents were dropped from this analysis because AHRQ discourages the use of NHSOPS data from fewer than five individuals.
The analyses used two sources of data: baseline individual surveys of safety culture collected at the time each facility enrolled in the collaborative using AHRQ’s NHSOPS instrument15 and structural information on facilities from the most proximate state inspection report in the Centers for Medicare and Medicaid Services Certification and Survey Provider Enhanced Reporting (CASPER) system in 2012 or 2013. Structural characteristics of facilities were compared with those of all U.S. nursing homes in 2013 using the 2013 CASPER data (on 15,579 facilities). The NHSOPS instrument used for this study was developed from frequently used safety culture tools, informed by expert opinion and an extensive literature review, and has been used to report on patient safety culture in hundreds of facilities, in which the instrument’s reliability proved strong.16 CASPER data used here were from the annual inspection closest in time to the survey date, retrieved from LTCFocus.org and accessed on September 10, 2015.17 Facilities that could not be matched to the CASPER data were dropped from analyses.
Measures of Safety Culture
The survey instrument included all 43 NHSOPS items within the 13 domains; a full description of all the items in the NHSOPS is available in Table S1. Previous AHRQ reports in 2011 and 2014 have demonstrated high consistency and reliability in the NHSOPS domains for nursing homes across the country that voluntarily shared data.16,18 The current study data are consistent and reliable in comparison with statistics that AHRQ has reported.
We focused on the five NHSOPS domains closely related to the collaborative’s subsequent work. These domains included: teamwork, training and skills provided in patient safety, communication openness, supervisor expectations, and organizational learning. These domains were key to the types of culture change that the collaborative promoted, including increasing teamwork, improving communication skills, and building teams in nursing homes that encourage changes in work practices. Each of these safety culture domains was measured using three to four statements for which respondents indicated how accurately the statement described their facility using a 5-point Likert scale from strongly disagree (1) to strongly agree (5). The teamwork domain evaluated staff perceptions of aspects of collaboration with colleagues for patient safety, the training and skills domain evaluated adequacy of safety training, and the communication openness domain evaluated the extent to which others listen to staff comments. There were three statements on the extent to which staff and supervisors communicate regarding safety and four statements on the extent to which the facility routinely makes changes and responds to safety issues.
Responses of “strongly agree” and “agree” were coded as positive. Negatively worded items were reverse coded, such that “strongly disagree” and “disagree” were coded as positive. Percentage positive scores were then computed for each domain as the number of items with positive responses divided by the number of items with nonmissing responses in the domain. Table S2 reports the percentage positive and Cronbach’s alpha, a statistical measure of reliability, for all the NHSOPS cultural domain scales and a comparison with reliability of AHRQ self-reported data from 2011.16 The data indicate that a high percentage of nursing home staff rated safety culture domains positively; the domains that received the lowest percentage positive from staff were staffing in safety and nonpunitive responses to mistakes. The data were generally consistent and reliable, using a Cronbach’s alpha of 0.70 or higher, which is similar to what is reported from AHRQ-reported safety culture data. The domains with the lowest level of consistency (<0.70), which includes nonpunitive responses to mistakes, compliance with procedures, and staffing in safety, were not used in the main analyses for this article; among the domains included in the analyses, organizational learning had the lowest reliability score (0.72).
Analytic Methods
Respondents’ percentage positive scores for each of the five domains were used as outcomes in models that included facility-level predictors of ownership, chain membership, percentage of residents on Medicare, and bed size (from CASPER) and the respondent-level predictors of role, tenure, and hours worked (from NHSOPS). Hierarchical linear regression models were used to account for respondent clustering within facilities. A series of multivariate models was used for each patient safety domain, beginning with a null model that included no covariates, a second model including just individual-level characteristics, and a full model including individual and facility characteristics. The intraclass correlation coefficient was calculated from the null model and indicates the percentage of the variance in the dependent variable that is attributable to organizational rather than individual factors. Estimates of the variance explained across models, which identifies how much the factors in the models explain variation at the individual and facility level, are also reported.
RESULTS
Survey responses from 170 facilities (81%) of the 210 enrolled in these two collaborative cohorts were included in the analyses. Twelve facilities were excluded because fewer than five employees responded to the culture survey, and another 28 were excluded because they were missing CASPER data. Table 1 provides descriptive statistics for the 170 facilities and the 14,177 respondents in the sample. The characteristics of the nursing homes in the study were similar to those of the national population of nursing homes. Approximately 31.2% were nonprofit, compared with 30.7% nationally, and 49.4% belonged to a corporate chain, compared with 55% nationally. Facilities participating in the collaborative were slightly larger on average in bed size than nursing homes nationally, with approximately 125 beds on average (vs 106 nationally) and 14.4% of residents were Medicare beneficiaries (vs 15.7% nationally).
Table 1.
Facility and Employee Characteristics
| Characteristic | Value |
|---|---|
| Facility structural measures (N = 170) | |
| Government or nonprofit ownership, n (%) | 53 (31.2) |
| Facility part of a chain, n (%) | 84 (49.4) |
| Number of beds, mean ± SD | 125.3 ± 69.0 |
| Percentage of residents on Medicare, mean ± SD | 14.4 ± 12.4 |
| Employee measures, n (%) (N = 14,177) | |
| Role in facility | |
| Administrator, manager | 1,123 (7.9) |
| Physician, other provider | 116 (0.8) |
| Licensed nurse | 2,991 (21.1) |
| Certified nurse assistant | 5,109 (36.1) |
| Support | 4,398 (31.0) |
| Not specified | 440 (3.1) |
| Tenure in facility | |
| <2 months | 623 (4.4) |
| 2-11 months | 2,284 (16.1) |
| 1-2 years | 2,783 (19.6) |
| 3-5 years | 3,057 (21.6) |
| 6-10 years | 2,682 (18.9) |
| ≥11 years | 2,382 (16.8) |
| Not specified | 366 (2.6) |
| Hours per week worked in facility | |
| <16 | 420 (3.0) |
| 16-24 | 1,219 (8.6) |
| 25-40 | 9,430 (66.5) |
| >40 | 2,762 (19.5) |
| Not specified | 346 (2.4) |
SD = standard deviation.
Data were not available on individual response rates within facilities, although the mean number of staff responses per facility was 83 (range 5–336, median 72). Of individual respondents, 36% were nursing assistants, 31% were support personnel, 21% were licensed nurses (licensed practical nurses or registered nurses), nearly 8% of respondents were administrators or managers, and fewer than 1% of respondents were physicians. Although there were too few physicians to generalize to this population, they were differentiated as a group in analyses because they have a unique role in this setting. For individual respondents, the median tenure in a nursing home was approximately 3–5 years, and 20% reported working in the facility for less than 1 year. Most respondents reported working 25–40 hours per week (Table 1). Respondents’ tenure was similar to that reported in AHRQ’s database of self-reported culture data, for which the median tenure of respondents across job categories was 3–5 years.18
Parameter estimates from the multivariate model results describing the association between the NHSOPS domain culture scores and facility and employee characteristics are shown in Table 2. For training and skills, communication openness, supervisor expectations, and organizational learning domains, the strongest facility-level predictor was ownership, although not in the direction predicted. Nonprofit and government facilities had significantly lower scores for training and skills (6.0 points), communication openness (7.3 points), supervisor expectations (5.2 points), and organizational learning (5.6 points). Supervisor expectations (3.2 points) and organizational learning (4.2 points) were also lower in chain-owned facilities. Percentage positive scores for communication openness (3.8 points) and organizational learning (2.8 points) were also significantly lower for larger facilities, measured in total beds (×100s). Individual-level respondent characteristics, including occupational role, tenure at the facility (vs new hires), and hours worked per week, were all highly statistically significant as predicted.
Table 2.
| (95% Confidence Interval) | |||||
|---|---|---|---|---|---|
| Teamwork | Training and Skills | Communication Openness | Supervisor Expectations | Organizational Learning | |
| Facility characteristics | |||||
| Non-profit or Govtc | −6.0 (−12.2, 0.1) | −6.0 (−11.8, −0.2)* | −7.3 (−12.3, −2.4)** | −5.2 (−8.4, −2.0)** | −5.6 (−9.7, −1.4)** |
| Chain-ownedd | −2.2 (−7.9, 3.5) | −2.7 (−8.0, 2.6) | −3.2 (−7.8, 1.4) | −3.2 (−6.1, −0.2)* | −4.2 (−8.1, −0.4)* |
| % on Medicare | 0.1 (−0.1, 0.3) | 0.1 (−0.2, 0.3) | 0.1 (−0.1, 0.3) | 0.1 (−0.1, 0.2) | 0.1 (−0.1, 0.3) |
| Total beds (100s) | 0.1 (−4.0, 4.1) | 1.6 (−2.2, 5.4) | −3.8 (−7.0, −0.5)* | −0.9 (−3.0, 1.1) | −2.8 (−5.5, −0.1)* |
| Respondent Characteristics | |||||
| Rolee | |||||
| Physician/Other provider | −7.7 (−14.6, −0.9)* | −8.4 (−15.0, −1.9)* | −14.2 (−21.7, −6.6)*** | −7.2 (−13.7, −0.6)* | −11.6 (−17.8, −5.3)*** |
| Licensed nurse | −9.7 (−12.2, −7.1)*** | −4.2 (−6.6, −1.8)*** | −15.2 (−18.0, −12.4)*** | −8.4 (−10.7, −6.1)*** | −5.6 (−8.0, −3.3)*** |
| Certified nurse assistant | −17.4 (−19.8, −15.0)*** | −3.8 (−6.1, −1.5)** | −24.3 (−26.9, −21.6)*** | −16.1 (−18.3, −13.9)*** | −10.1 (−12.3, −7.9)*** |
| Support | −11.9 (−14.4, −9.5)*** | −5.3 (−7.7, −3.0)*** | −16.8 (−19.4, −14.1)*** | −7.2 (−9.4, −5.0)*** | −10.5 (−12.7, −8.2)*** |
| Tenure at current facilityf | |||||
| 2-11 months | −12.0 (−15.2, −8.9)*** | −7.4 (−10.4, −4.4)*** | −9.4 (−12.9, −6.0)*** | −7.6 (−10.6, −4.7)*** | −5.3 (−8.2, −2.4)*** |
| 1-2 years | −12.7 (−15.8, −9.5)*** | −9.1 (−12.0, −6.1)*** | −12.4 (−15.8, −9.0)*** | −9.0 (−11.9, −6.1)*** | −5.3 (−8.1, −2.4)*** |
| 3-5 years | −13.9 (−17.0, −10.8)*** | −9.2 (−12.2, −6.2)*** | −13.3 (−16.7, −9.8)*** | −9.5 (−12.4, −6.7)*** | −5.9 (−8.7, −3.0)*** |
| 6-10 years | −13.3 (−16.5, −10.1)*** | −8.4 (−11.4, −5.4)*** | −12.9 (−16.4, −9.4)*** | −9.2 (−12.1, −6.2)*** | −3.7 (−6.6, −0.8)* |
| 11+ years | −11.4 (−14.6, −8.1)*** | −6.8 (−9.9, −3.7)*** | −11.4 (−14.9, −7.9)*** | −7.2 (−10.2, −4.2)*** | −0.5 (−3.5, 2.5) |
| Hours worked per weekg | |||||
| 16-24 hours | −6.1 (−10.1, −2.1)** | −3.8 (−7.6, 0.1) | −4.3 (−8.7, 0.0) | −5.1 (−8.8, −1.4)** | −2.9 (−6.5, 0.8) |
| 25-40 hours | −7.5 (−11.0, −3.9)*** | −3.8 (−7.2, −0.4)* | −4.2 (−8.1, −0.4)* | −2.5 (−5.8, 0.8) | −1.1 (−4.3, 2.2) |
| >40 hours | −7.4 (−11.2, −3.7)*** | −5.0 (−8.6, −1.4)** | −2.3 (−6.4, 1.8) | −3.3 (−6.9, 0.2) | −0.6 (−4.1, 2.8) |
| Intercept | 98.5 (89.4, 107.6)*** | 86.1 (77.6, 94.7)*** | 96.9 (88.8, 105.1)*** | 105.7 (99.7, 111.7)*** | 91.4 (84.6, 98.2)*** |
Percent positive is defined as the percent of all domain items coded by the respondent as “Agree” or “Strongly Agree”. Negatively worded items were reverse coded.
NHSOPS is the Nursing Home Survey on Patient Safety Culture and within this table, levels of significance are:
P < .05,
P < .01,
P < .001. See Supplementary Table S1 for NHSOPS items and domains.
Facility Characteristics:
Reference group is Non-government, for-profit ownership.
Reference group is Facility is not part of a chain.
Respondent characteristics:
Reference group is Administrator.
Reference group is <2 months.
Reference group is <=15 hours.
The percentage of variance in safety culture scores that individual and facility characteristics explained is presented in Table 3. The intraclass correlation coefficient ranged from 7% for supervisor expectations to 21% for teamwork and training and skills. The various individual characteristics added to the model explained a minimal amount of variance (2.5% for teamwork, 3.4% for communication openness, 2.7% for supervisor expectations, 1.4% for organizational learning domains) and less than 1% of variance (0.5%) for the training and skills domain. Facility-level predictors added to the models explained 2.4% of variance for teamwork, 2.6 for training and skills, and as much as 11.2% for communication openness and organizational learning (reported in column 3). At the facility level, the predictors did well in explaining the variance between facilities in communication openness, supervisor expectations, and organizational learning but were less able to explain variance in training and skills and teamwork. At the individual level, the predictors were highly significant but explained little of the variation within facilities.
Table 3.
Variance Explained in Multivariate Models Predicting Percentage Positive Scores (N = 170 facilities)
| Domain | Null Model | +Individual Characteristicsa | +Facility Characteristicsb |
|---|---|---|---|
| Teamwork (N = 13,398) | |||
| Variance within facilities | 1,249.4 | 1,217.7 | 1,217.7 |
| Variance between facilities | 327.3 | 328.1 | 319.4 |
| Intraclass correlation | 0.21 | ||
| Variance explained within facilities, % | 2.5 | ||
| Variance explained between facilities, % | 2.4 | ||
| Training and skills (N = 13,317) | |||
| Variance within facilities | 1,094.5 | 1,088.5 | 1,088.5 |
| Variance between facilities | 286.4 | 288.0 | 278.9 |
| Intraclass correlation | 0.21 | ||
| Variance explained within facilities, % | 0.5 | ||
| Variance explained between facilities, % | 2.6 | ||
| Communication openness (N = 13,426) | |||
| Variance within facilities | 1,512.0 | 1,460.8 | 1,460.8 |
| Variance between facilities | 218.7 | 214.7 | 194.0 |
| Intraclass correlation | 0.13 | ||
| Variance explained within facilities, % | 3.4 | ||
| Variance explained between facilities, % | 11.2 | ||
| Supervisor expectations (N = 13,173) | |||
| Variance within facilities | 1,028.7 | 1,001.0 | 1,000.8 |
| Variance between facilities | 81.5 | 79.7 | 72.9 |
| Intraclass correlation | 0.07 | ||
| Variance explained within facilities, % | 2.7 | ||
| Variance explained between facilities, % | 10.6 | ||
| Organizational learning (N = 13,422) | |||
| Variance within facilities | 1,040.1 | 1,025.1 | 1,025.1 |
| Variance between facilities | 154.1 | 151.1 | 136.7 |
| Intra-class correlation | 0.13 | ||
| Variance explained within facilities, % | 1.4 | ||
| Variance explained between facilities, % | 11.3 |
Percentage positive is defined as the percentage of all domain items that the respondent coded as “agree” or “strongly agree.” Negatively worded items were reverse coded.
Individual characteristics included in this model include occupational role, job tenure, and job hours per week.
Facility characteristics include whether nonprofit or government owned, whether chain owned, percentage of residents on Medicare, and total number of beds in facility.
Finally, Figure 1 depicts predicted mean safety culture scores across individual roles, giving an estimate of the range of safety culture scores expected within facilities. Administrators rated culture the highest, and nursing assistants and physicians rated it the lowest across domains. The percentage positive rating for safety culture scores was more than 60% for all domains except communication openness, which had a mean of 55%. Scores for supervisor expectations were the highest (mean 81%) (Table S2).
Figure 1.
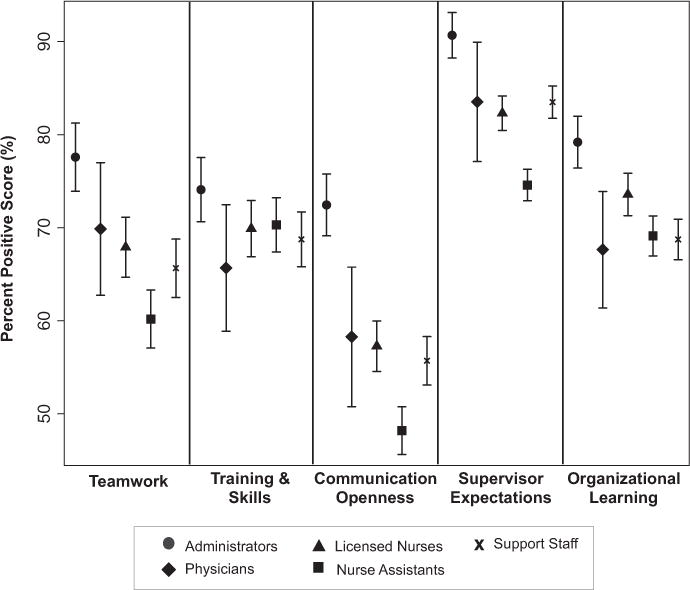
Marginal means and 95 percent confidence intervals for percentage positive scores according to domain and worker role.
DISCUSSION
Several important findings emerged from this study examining individual- and facility-level predictors of safety culture in nursing homes. First, relatively high average percentage positive ratings were observed across safety culture domains assessed in the NHSOPS. Second, bedside clinical staff generally had lower ratings of safety culture than administrators, highlighting the importance of surveying multiple individuals on safety culture to obtain more comprehensive ratings rather than relying on facility administrator reports, which often include the highest safety culture scores, to generate facility-level culture scores. Third, ratings of safety culture tended to be highest for employees with minimal tenure and lowest for those who were not new employees (with tenure of longer than 2 months). Fourth, although the results indicated that approximately 20% of variance in safety culture measures was attributable to facility-level variation, the set of facility variables explained at most 12% of that variation. The critical facility-level predictors of safety culture scores included ownership, with nonprofit and chain status unexpectedly associated with worse staff perceptions of safety.
The organizational predictors, which were based on previous studies of safety culture in nursing homes, did not explain fully the facility-level variance in teamwork or training and skills. Furthermore, across the five safety domains studied, 80% or more of the variance could be attributable to individual-level variation, although the individual-level predictors, including occupational role, explained less than 5% of the variation in safety culture scores. These results indicate that substantially more work is necessary on what motivates individuals’ perceptions of safety culture, a critical question if perceptions of safety culture within facilities are to be changed.
There are several limitations in data collection for this study. The sample design, which depended on voluntary recruitment of facilities and participants into the AHRQ Safety Program for Long-term Care: HAIs/CAUTI Project may have influenced the observed effects of facility and individual predictors on safety culture scores. The nursing homes participating in the collaborative were less likely to be chain-owned and had more beds than the general U.S. nursing home population.12 Sampling may have affected the observed and unexpected result that for-profit and chain-owned nursing homes had more positive scores across multiple domains of safety culture (communication openness, supervisor expectations, organizational learning), which may reflect unique cultural values within the select group of for-profit nursing homes participating in the collaborative. At the same time, the study had limited capacity to reach individuals within facilities because the facility lead distributed surveys within facilities, and no information was provided on how surveys were distributed. Facilities were encouraged to distribute the surveys to at least 60% of their staff to obtain broad individual representation. Although these methods may limit generalizability, they provided a simple and accessible way to reach a range of stakeholders within facilities.
Future efforts to improve facility safety practices should focus on reducing variation in perceptions of safety culture of employees and on better understanding of the reasons behind individual variation in safety culture ratings. Further qualitative, in-depth research is necessary to explore further the reasons behind individual differences in safety culture scores because it is unknown why demographic characteristics such as tenure affected staff perspectives on safety practices. There may be specific events or interactions that prompt the lower safety culture assessment of those with the most bedside interaction and longer tenure.19 Successful culture change should also engage nursing home administrators, who rated safety culture the highest, in spending more time at the bedside with clinicians to understand challenges, concerns, and resource needs that affect resident safety. Administrators often lead the challenge to improve safety culture scores, but to be successful in that, they must reconsider their overly positive views of culture. Facility leadership can also play an important role in addressing the safety culture items rated poorest across facilities, including nonpunitive responses to mistakes and communication openness.
Finally, to more effectively monitor and respond to safety culture, nursing homes must address the individual-level variation in safety culture ratings within facilities. New employee training could be used to make expectations clear regarding safety practices, which may address the notably higher safety culture ratings of staff with the shortest tenure. Reporting safety culture scores according to occupation may be more important than using facility-level scores alone to describe and assess barriers to, facilitators of, and changes in safety culture.
Supplementary Material
Table S1. AHRQ Nursing Home Survey on Patient Safety Culture (NHSOPS) Domains (43 items)
Table S2. Summary statistics for NHSOPS domains Please note: Wiley-Blackwell is not responsible for the content, accuracy, errors, or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
Acknowledgments
We thank Laura Petersen, MHSA, for assistance with references and manuscript editing. This work was supported by Contract HHSA 2902010000251 from the Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services. The findings and conclusions in this report are those of the authors and do not necessarily represent those of the sponsor.
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Author Contributions: Study concept and design: JBH, HR, MTG, LM, JM. Acquisition of subjects and data: HR, LM, JM, MTG. Analysis and interpretation of data, preparation of manuscript: all authors.
Sponsor’s Role: None.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article:
References
- 1.Bonner AF, Castle NG, Perera S, et al. Patient safety culture: A review of the nursing home literature and recommendations for practice. Ann Longterm Care. 2008;16:18–22. [PMC free article] [PubMed] [Google Scholar]
- 2.Gruneir A, Mor V. Nursing home safety: Current issues and barriers to improvement. Annu Rev Public Health. 2008;29:369–382. doi: 10.1146/annurev.publhealth.29.020907.090912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas KS, Hyer K, Castle NG, et al. Patient safety culture and the association with safe resident care in nursing homes. Gerontologist. 2012;52:802–811. doi: 10.1093/geront/gns007. [DOI] [PubMed] [Google Scholar]
- 4.Castle NG, Wagner LM, Ferguson JC, et al. Safety culture of nursing homes: Opinions of top managers. Health Care Manage Rev. 2011;36:175–187. doi: 10.1097/HMR.0b013e3182080d5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hughes CM, Lapane KL. Nurses’ and nursing assistants’ perceptions of patient safety culture in nursing homes. Int J Qual Health Care. 2006;18:281–286. doi: 10.1093/intqhc/mzl020. [DOI] [PubMed] [Google Scholar]
- 6.Castle N, Sonon K. A culture of patient safety in nursing homes. Qual Saf Health Care. 2006;15:405–408. doi: 10.1136/qshc.2006.018424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singer SJ, Vogus TJ. Safety climate research: Taking stock and looking forward. BMJ Qual Saf. 2013;22:1–4. doi: 10.1136/bmjqs-2012-001572. [DOI] [PubMed] [Google Scholar]
- 8.Castle NG, Handler S, Engberg J, et al. Nursing home administrators’ opinions of the resident safety culture in nursing homes. Health Care Manage Rev. 2007;32:66–76. doi: 10.1097/00004010-200701000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Wisniewski AM, Erdley WS, Singh R, et al. Assessment of safety attitudes in a skilled nursing facility. Geriatr Nurs. 2007;28:126–136. doi: 10.1016/j.gerinurse.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Wagner LM, Capezuti E, Rice JC. Nurses’ perceptions of safety culture in long-term care settings. J Nurs Scholarsh. 2009;41:184–192. doi: 10.1111/j.1547-5069.2009.01270.x. [DOI] [PubMed] [Google Scholar]
- 11.Scott-Cawiezell J, Vogelsmeier A. Nursing home safety: A review of the literature. Annu Rev Nurs Res. 2006;24:179–215. [PubMed] [Google Scholar]
- 12.Mody L, Meddings J, Edson BS, et al. Enhancing resident safety by preventing healthcare-associated infection: A national initiative to reduce catheter-associated urinary tract infections in nursing homes. Clin Infect Dis. 2015;61:86–94. doi: 10.1093/cid/civ236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mody L, Greene MT, Meddings J, et al. A national implementation project to prevent catheter-associated urinary tract infection in nursing home residents. JAMA Intern Med. 2017 May 19; doi: 10.001/jamainternmed.2017.1689. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sorra J, Gray L, Streagle S, et al. AHRQ hospital survey on patient safety culture: user’s guide. Rockville, MD: Agency for Healthcare Research and Quality; 2016. [on-line]. Available at https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/patientsafetyculture/hospital/userguide/hospcult.pdf Accessed June 19, 2017. [Google Scholar]
- 15.Castle NG, Wagner LM, Perera S, et al. Assessing resident safety culture in nursing homes: Using the nursing home survey on resident safety. J Patient Saf. 2010;6:59–67. doi: 10.1097/PTS.0b013e3181bc05fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sorra J, Famolaro T, Dyer N, et al. Nursing home survey on patient safety culture: 2011 user comparative Database report. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [on-line]. Available at https://psnet.ahrq.gov/resources/resource/22968/nursing-home-survey-on-patient-safety-culture-2011-user-comparative-database-report Accessed February 10, 2017. [Google Scholar]
- 17.Centers for Medicare and Medicaid Services. Certification and Survey Provider Enhanced Reporting (CASPER) database [obn-line] Available at http://ltcfocus.org/ Accessed September 10, 2015.
- 18.Sorra J, Famolaro T, Yount N, et al. Nursing home survey on patient safety culture: 2014 user comparative Database report. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [on-line]. Available at http://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/patientsafetyculture/nursing-home/2014/nhsurv14-ptI.pdf Accessed June 20, 2017. [Google Scholar]
- 19.Weaver SJ, Lubomksi LH, Wilson RF, et al. Promoting a culture of safety as a patient safety strategy: A systematic review. Ann Intern Med. 2013;158:369–374. doi: 10.7326/0003-4819-158-5-201303051-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. AHRQ Nursing Home Survey on Patient Safety Culture (NHSOPS) Domains (43 items)
Table S2. Summary statistics for NHSOPS domains Please note: Wiley-Blackwell is not responsible for the content, accuracy, errors, or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.


