Abstract
Background
Pulmonary embolism (PE) during pregnancy remains one of the leading causes of maternal morbidity and mortality in the developed world. However, there is a paucity of high-quality evidence resulting in a lack of consensus in managing this group of patients. The aims of the study were to address the diagnostic utility of D-dimer for suspected PE in pregnant and post-partum patients and to identify any clinical presentation variables that are predictors of PE in this group of patients.
Methods
A retrospective case note review of 152 pregnant and post-partum patients who underwent diagnostic imaging (ventilation/perfusion (V/Q) or computed tomographic pulmonary angiography (CTPA)) for suspected PE at a tertiary teaching hospital from 2007 to 2011 was conducted. The reference range for D-dimer was less than 0.5 mg/L as being normal. The following variables were also assessed in terms of their predictive capability for PE diagnosis in pregnancy: heart rate (HR), mean arterial pressure (MAP), shock index (SI) and A-a gradient.
Results
The application of D-dimer testing for suspected PE in this study population had a sensitivity of 100% (95% CI, 73–100%), specificity of 42% (95% CI, 31–53%) and a likelihood negative ratio of 0. None of the clinical variables were significant predictors of PE according to regression analyses.
Conclusions
There is supportive evidence that a negative D-dimer result is useful as a means of ruling out PE in pregnant and post-partum patients. However, we need a larger prospective observational study to collaborate the findings.
Keywords: Pulmonary embolism, Pregnancy, Post-partum, D-dimer
Background
Pregnancy-related pulmonary embolism (PE) remains one of the leading causes of maternal morbidity and mortality in the developed world [1]. The risk of antenatal venous thromboembolism (VTE) is four- to fivefold higher in pregnant women than non-pregnant women of the same age [2]. Venous thromboembolism can occur at any stage of pregnancy, but the puerperium remains the time of highest risk with an estimated 20-fold increase in relative risk [3]. This is because each component of Virchow’s triad (venous stasis, hypercoagulable state and tissue trauma) is present at some stage during pregnancy [4].
The Confidential Enquiry into Maternal and Child Health (2004) in the UK identified areas of substandard care in two thirds of the cases, including failures in obtaining objective diagnoses and acting promptly in providing necessary treatment in suspected cases of VTE [1].
PE amongst pregnant and post-partum patients remains arguably one of the most difficult diagnostic challenges for clinicians. Many of the signs and symptoms of PE are similar to the manifestation of physiological changes that occur during the course of pregnancy. Radiation exposure is also a particular concern with consequent implications of carcinogenesis and teratogenesis and interruptions of breastfeeding for post-partum lactating women. Historically, the diagnosis of PE has relied on validated diagnostic algorithms, such as the Wells rule [5], for constructing the pre-test probability of the disease. The Wells rule [5] includes the clinicians’ subjective judgement of whether PE is more likely than an alternative diagnosis. New rules, such as the Geneva [6], Pisa [7], Charlotte [8] and pulmonary embolism rule-out criteria (PERC) [9] rules, contain objective items only. However, none of these diagnostic tools have been validated on pregnant patients.
Our knowledge of the risk assessment of PE is largely derived from two large prospective multi-centre trials, PIOPED I and PIOPED II, conducted in the last 20 years [10, 11]. The most widely used clinical model for PE, Wells rule [5], was extracted from relevant clinical presentation characteristics detected in PIOPED trials. However, pregnant and post-partum patients were excluded from these trials. Hence, the same clinical prediction rules do not apply to this group of patients.
The diagnostic utility of D-dimer for PE is well established in non-pregnant, low-risk patients [5]. However, its role in pregnancy is uncertain because of the substantial increase of D-dimer throughout gestational age [12, 13]. This increase is thought to be related to the rising levels of circulating fibrinogen in pregnancy, rather than due to an increase in levels of fibrin degradation products [12].
A simple management strategy is urgently required for pregnant and post-partum patients with suspected PE in order to provide a rapid and reliable diagnosis while avoiding unnecessary anticoagulation treatment and radiation exposure.
The objectives of our study were largely twofold. First of all, we attempted to address the diagnostic utility of D-dimer for PE in pregnant patients and those within 6 weeks post-partum. Secondly, we attempted to identify any clinical presentation variables that were predictors of PE during pregnancy and post-partum periods. In particular, we looked at the association between the diagnosis of PE and the median heart rate (HR), mean arterial pressure (MAP), shock index (SI) and A-a gradient.
Methods
Consecutive pregnant and post-partum patients presenting to the emergency department (ED) or antenatal clinics with clinically suspected acute PE between January 2007 to January 2011 at a tertiary teaching hospital in London, who underwent V/Q scans, CTPAs or pulmonary angiography were retrospectively selected for data review. The post-partum period lasted for 6 weeks after the delivery of the foetus or termination of the pregnancy. Patients were identified electronically from all V/Q scans, CTPA and pulmonary angiography previously performed for suspected PE during the study period. The selected patients’ case records were then examined for the recording of their clinical presentation, D-dimer results and outcomes.
A radiological diagnosis of PE was defined by the PIOPED criteria [10, 11]—a high-probability ventilation/perfusion (V/Q) scan with no previous history of PE, i.e. ≥ 2 segmental perfusion defects (V/Q mismatch), a positive CTPA scan or pulmonary angiography.
D-dimer was measured by MDA Auto-Dimer, an immunoturbidimetric assay that utilises antibody coated latex particles. The reference range for D-dimer was less than 0.5 mg/L as being normal.
A-a gradient (kPa) was calculated from the following equation: [(FiO2) × (atmospheric pressure − H2O pressure) − (PaCO2/0.8)] − PaO2 [14].
Shock index was calculated as HR/systolic BP.
The sensitivity and specificity with 95% confidence intervals (95% CI) were calculated to assess the diagnostic performance of D-dimer for PE in pregnant and post-partum patients. Positive and negative predictive values (PPVs, NPVs) were also reported with 95% CIs.
The D-dimer levels and gestation of the pregnancy at presentation were noted and compared between the two groups (non-PE and PE) using the Mann-Whitney U test. The clinical presentation parameters, namely heart rate (HR), mean arterial pressure (MAP), shock index (SI) and A-a gradient, were also compared between non-PE and PE groups, using the two-tailed t test or the Mann-Whitney U test (on condition of non-normal distributions).
To assess the predictive capability of the aforementioned clinical parameters for PE diagnosis in pregnancy, the univariate regression analyses were performed using Student’s t test. Significance was fixed at p value < 0.05.
All statistical analyses were performed using spreadsheet-based statistical software (StatsDirect, release 2.3.8; CamCode, Herts, England).
The study was discussed with the local research and development department who advised that formal ethics committee approval was not required for this project due to its observational nature. All data were anonymised.
Results
Overall, 152 pregnant and post-partum patients within 6 weeks of delivery or termination of pregnancy underwent V/Q scans or CTPAs as part of their assessment for suspected PE over a 4-year period between 2007 and 2011. No pulmonary angiogram was performed on any of these patients.
Patient demographics for the study population are given in Table 1.
Table 1.
Characteristics of the study population
| Total number of women, n | 152 |
| Weeks of gestation at presentation, n (%) | |
| < 12 | 23 (15.1) |
| 12–28 | 42 (27.6) |
| > 28 | 59 (38.8) |
| Post-partum | 28 (18.4) |
| Age, mean (SD), years | 31.4 (5.1) |
| Nulliparous, n (%) | 35 (23.0) |
| Gravity, mean (SD) | 2.9 (2.1) |
| Twin pregnancy, n (%) | 3 (2.0) |
| Termination of pregnancy, n (%) | 1 (0.7) |
| Outcomes | |
| In-hospital mortality, n (%) | 0 |
| 28-day mortality, n (%) | 0 |
| ICU/HDU/CCU admissions, n (%) | 8 (5.3) |
| Reasons for ICU/HDU/CCU admission | |
| Intra-abdominal bleeding following anticoagulation | 1 |
| Asthma exacerbation | 1 |
| H1N1 | 1 |
| Other URTI/LRTI | 2 |
| Thrombolysis for saddle pulmonary embolus | 1 |
| Eclampsia | 1 |
| PCI following MI (CCU) | 1 |
Data are presented as number (percentage) of women, unless otherwise indicated
CCU coronary care unit, ICU intensive care unit, MI myocardial infarction, URTI upper respiratory tract infection, LRTI lower respiratory tract infection, PCI percutaneous coronary intervention
Of 152 patients, 93 had the D-dimer assay performed as part of their assessment for PE. One hundred thirty had the HR and MAP documented in their case notes, and 110 patients had the blood gas measurements documented.
Table 2 shows a 2 × 2 table for the binary variable ‘PE diagnosis’ and the dichotomised variable ‘D-dimer test’ using a cut-off point of 0.5 mg/L that distinguished between a positive (> 0.5 mg/L) and negative (< 0.5 mg/L) test result.
Sensitivity = 100% (95% CI, 73–100%)
Specificity = 42% (95% CI, 31–53%)
Positive predictive value (PPV) = 23% (95% CI, 14–36%)
Negative predictive value (NPV) = 100% (95% CI, 87–100%)
Likelihood ratio positive (LR+) = sensitivity/(1 − specificity) = 1/(1–0.42) = 1.72 (95% CI, 1.42–2.07)
Likelihood ratio negative (LR−) = (1 − sensitivity)/specificity) = 0/0.42 = 0
Table 2.
Performance of D-dimer for detecting PE in pregnant and post-partum patients
| PE diagnosis | ||||
|---|---|---|---|---|
| Negative (0) | Positive (1) | Total | ||
| D-dimer test | Negative (0) | 33 | 0 | 33 |
| Positive (1) | 46 | 14 | 60 | |
| Total | 79 | 14 | 93 | |
In both groups, the spread of D-dimers was not normally distributed for either set of patients (non-PE and PE) across all stages of gestation.
A box plot of D-dimer for the two groups is shown in Fig. 1, and the D-dimers were compared using the non-parametric Mann-Whitney U test. There was a significant difference in the median values between the two groups (p = 0.0061).
Fig. 1.
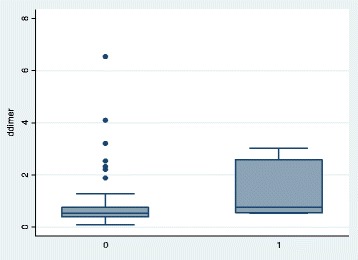
Box plot of D-dimer for patients without (0) and with PE (1)
The null hypothesis that the D-dimer variable is the same between non-PE and PE pregnant and post-partum patients was rejected.
Figure 2 illustrates D-dimer levels against week gestation for non-PE and PE groups respectively.
Fig. 2.
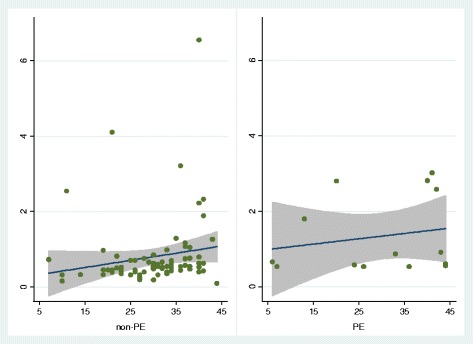
D-dimer against number of weeks of gestation and post-partum
Despite the fact that Fig. 2 appears to show increasing linear trends throughout gestation for both non-PE and PE groups, these trends are not significant in a regression analysis.
| Regression results from non-PE group (79 patients): | ||||
| D-dimer | Coefficient | p value | 95% CI | |
| Constant | 0.236455 | 0.534 | − 0.51644 | 0.989347 |
| Weeks | 0.018921 | 0.124 | − 0.00529 | 0.043131 |
| Regression results for PE group (14 patients): | ||||
| D-dimer | Coefficient | p value | 95% CI | |
| Constant | 0.920815 | 0.2 | − 0.55866 | 2.400287 |
| Weeks | 0.014102 | 0.509 | − 0.03101 | 0.059215 |
Table 3 illustrates the median values for non-PE and PE patients and the p values obtained when comparing the clinical presentation variables for the two groups. None of the presentation variables were significant at the 95% level. Only the A-a gradient was close to being significant for these data.
Table 3.
Comparing clinical presentation variables in PE and non-PE groups
| Characteristic | Median [IQR] | p value | Significant? | |
|---|---|---|---|---|
| Non-PE | PE | |||
| Heart rate (HR) | 97 [82, 110] | 95 [80, 119] | 0.9121 | No |
| Mean arterial pressure (MAP) | 85 [77.67, 92.67] | 92 [79.33, 98.33] | 0.2975 | No |
| Shock index (SI) | 0.81 [0.70, 0.95] | 0.84 [0.54, 0.89] | 0.6195 | No |
| A-a gradient | 1.3 [0.5, 3.1] | 3.3 [2.4, 4.2] | 0.0739 | No |
Table 4 summarises the results of the clinical presentation characteristics as predictors of PE after univariate regression analyses. None of the variables were significant predictors of PE diagnosis. However, the A-a gradient was borderline significant.
Table 4.
Patient presentation characteristics and their association with PE diagnosis in pregnancy and the puerperium (univariate analysis)
| Presentation characteristics | Odds ratio | 95% CI | p value |
|---|---|---|---|
| D-dimer | 1.52 | [0.95, 2.42] | 0.14 |
| Heart rate (HR) | 1.02 | [0.56, 1.85] | 0.65 |
| Mean arterial pressure (MAP) | 1.54 | [0.89, 2.66] | 0.15 |
| Shock index (SI) | 0.70 | [0.33, 1.51] | 0.47 |
| A-a gradient | 2.08 | [0.93, 4.62] | 0.081 |
Discussion
Currently, there is a paucity of data that addresses the diagnostic utility of D-dimer in pregnant and post-partum populations with suspected PE. Not surprisingly, there is no clear guidance on the management of this specific cohort of patients due to the lack of evidence available.
Before our study, the only available data that directly addressed the above clinical dilemma was by Damodaram et al. [15], a retrospective case study comprising 37 women with suspected PE that underwent ventilation/perfusion diagnostic scanning. There is also a case report based on a single pregnant patient with PE [16]. Hence, our retrospective study comprising 93 pregnant and post-partum patients with recorded D-dimer levels represents the largest study sample to date.
Our study data showed that the sensitivity and specificity of D-dimer as a screening test for suspected PE in pregnant and post-partum patients undergoing emergency diagnostic imaging was 100 and 42%, respectively, while the negative likelihood ratio was 0 (Table 2). These results appear to be principally dictated by the lack of a single positive PE diagnosis when the D-dimer measure was below the 0.5 mg/L cut-off.
By contrast, Damodaram et al. [15] showed the sensitivity of 73% and specificity of 15%, respectively, while the negative likelihood ratio was 1.8. Their D-dimer cut-off point was also 0.5 mg/L. However, a moderate probability V/Q was also considered as a positive diagnostic test for PE. This is against the current guidelines [10, 11, 17]. A single case report by To et al. [16] illustrated a case of a pregnant patient with objectively diagnosed PE, but with a negative D-dimer.
Clearly, we need a larger prospective study to determine with confidence if a negative D-dimer result can safely rule out the diagnosis of PE in pregnancy as our study findings contradict those of the existing smaller retrospective study [15] and of the case report [16].
In the non-pregnant woman, a negative MDA latex agglutination D-dimer test helped to rule out VTE (both DVT and PE) in those with both intermediate and low clinical probability with the pooled sensitivity 97%, specificity 46%, +LR 1.8 and −LR 0.07 [18]. It is likely that the same D-dimer assay, as utilised in our study, could be potentially useful as a means of ruling out PE in pregnant and post-partum patients.
Our D-dimer data appeared to show increasing linear trends throughout gestation for both non-PE and PE groups (Fig. 2), but these trends were not significant in a regression analysis. This lack of significance could be due to the impact of outlying values and a lack of power attributable to the small sample size. Unfortunately, we had insufficient data to apply the results to patients in the individual stages of gestation (trimesters and post-partum).
Our data did not show any significant differences in median HR, MAP, SI and A-a gradient amongst pregnant and post-partum patients between non-PE and PE groups (Table 3). Only the A-a gradient was close to being statistically significant. None of these clinical presentation variables were significant predictors of PE during pregnancy and post-partum periods.
There is no published data that addresses the relationship between the A-a gradient and PE in pregnant and post-partum populations.
Stein et al. examined the data derived from PIOPED I for any potential diagnostic utility of an A-a gradient for PE in non-pregnant patients [19]. They found that normal values of the A-a gradient did not exclude the diagnosis of acute PE.
One needs to recognise a fundamental physiological difference in the population characteristics between those in PIOPED I and II trials [10, 11]—generally older patients with variable baseline cardio-pulmonary function vs. pregnant and post-partum patients and younger patients with healthy baseline cardio-pulmonary function. Hence, an abnormal A-a gradient could prove to be a more significant predictor of PE amongst our study cohort, compared to that of the PIOPED cohorts. Further investigation and more data are needed to assess this relationship further.
Limitations
The study relied on the retrospective data collection with subsequent absence of some data. It is also a single-centred study with a relatively small number of participants. Nonetheless, it is still the biggest study to address the utility of D-dimer in the diagnosis of pregnancy-associated PE.
The study identified only those patients with suspected PE who underwent emergency diagnostic imaging. It is possible that some patients were discharged home from the emergency department or antenatal clinics with a normal D-dimer and no imaging but had subsequently developed PE. Such patients would not have been captured in our data if they had sought health care services elsewhere for treatment.
Finally, it is possible that CTPA or V/Q imaging were considered unnecessary in some patients but still treated for presumed PE, i.e. positive bilateral leg DVT scans or echocardiography findings suggestive of PE. The study focused on CTPAs and V/Q scans as the diagnostic imaging of choice, as this is the accepted practice in the authors’ hospital. However, it is likely that there are other accepted modes of investigation across different healthcare settings. This lack of agreement is due to the absence of consensus in the national or international guidelines.
Conclusions
None of the patients with PE had a D-dimer below the 0.5 mg/L cut-off level, making it a potentially useful screening tool for ruling out PE with a negative D-dimer.
An A-a gradient performed better than D-dimer in predicting PE in our study cohort. However, neither of them were significant predictors of PE diagnosis in pregnancy. We need a larger prospective observational study to collaborate these findings amongst pregnant and post-partum patients.
Authors’ contributions
HC conceived the study, collected the data, did the analysis and drafted the manuscript. DK collected the data, assisted with the analysis and drafted the manuscript. HC takes responsibility for the paper as a whole. Both authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was discussed with the local research and development department who advised that formal ethics committee approval was not required for this project due to its observational nature. All data were anonymised.
Competing interests
Both authors declare they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hyun Choi, Email: hchoi@doctors.org.uk.
Dinesh Krishnamoorthy, Email: kdinesh60@gmail.com.
References
- 1.Lewis G, Drife J. Why mothers die 2000–2002: the sixth report of the confidential enquiries into maternal deaths in the United Kingdom. London: RCOG Press; 2004. [Google Scholar]
- 2.Heit J, Kobbervig C, James A, Patternson T, Bailey KR, Melton LJ. Trends in the incidence of deep vein thrombosis and pulmonary embolism during pregnancy or the puerperium: a 30-year population-based study. Ann Int Med. 2005;143:697–706. doi: 10.7326/0003-4819-143-10-200511150-00006. [DOI] [PubMed] [Google Scholar]
- 3.Reducing the risk of venous thromboembolism during pregnancy and the puerperium (Green-top Guideline No. 37a). R Coll Obstet Gynaecol. [cited 29 Jan 2018]. Available from: https://www.rcog.org.uk/globalassets/documents/guidelines/gtg-37a.pdf
- 4.Cerneca F, Ricci G, Simone R, Malisano M, Alberico S, Guaschino S. Coagulation and fibrinolysis changes in normal pregnancy. Increased levels of procoagulants and reduced levels of inhibitors during pregnancy induce a hypercoagulable state, combined with a reactive fibrinolysis. Eur J Obstet Gynecol Reprod Biol. 1997;73:31–36. doi: 10.1016/S0301-2115(97)02734-6. [DOI] [PubMed] [Google Scholar]
- 5.Wells PS, Ginsberg JS, Anderson DR, Kearon C, Gent M, Turpie AG, et al. Use of a clinical model for safe management of patients with suspected pulmonary embolism. Ann of Int Med. 1998;129:997–1005. doi: 10.7326/0003-4819-129-12-199812150-00002. [DOI] [PubMed] [Google Scholar]
- 6.Wicki J, Perneger TV, Junod A, Bounameaux H, Perrier A. Assessing clinical probability of pulmonary embolism in the emergency ward: a simple score. Arch Intern Med. 2001;161:92–97. doi: 10.1001/archinte.161.1.92. [DOI] [PubMed] [Google Scholar]
- 7.Miniati M, Bottai M, Monti S, Salvadori M, Serasini L, Passera M. Simple and accurate prediction of the clinical probability of pulmonary embolism. Am J Respir Crit Care Med. 2008;178:290–294. doi: 10.1164/rccm.200802-207OC. [DOI] [PubMed] [Google Scholar]
- 8.Kline JA, Wells PS. Methodology for a rapid protocol to rule out pulmonary embolism in the emergency department. Ann Emerg Med. 2003;42:266–275. doi: 10.1067/mem.2003.268. [DOI] [PubMed] [Google Scholar]
- 9.Kline JA, Mitchell AM, Kabrhell C, Richman PB, Courney DM. Clinical criteria to prevent unnecessary diagnostic testing in emergency department patients with suspected pulmonary embolism. J Tbromb Haemost. 2004;2:1247–1255. doi: 10.1111/j.1538-7836.2004.00790.x. [DOI] [PubMed] [Google Scholar]
- 10.PIOPED investigators Value of the ventilation/perfusion scan in acute pulmonary embolism. Results of the prospective investigation of pulmonary embolism diagnosis (PIOPED) JAMA. 1990;263:2753–2759. doi: 10.1001/jama.1990.03440200057023. [DOI] [PubMed] [Google Scholar]
- 11.Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, et al. Multidetector computed tomography for acute pulmonary embolism. N Engl J Med. 2006;354:2317–2327. doi: 10.1056/NEJMoa052367. [DOI] [PubMed] [Google Scholar]
- 12.Kline JA, Williams GW, Hernandez-Nino J. D-dimer concentrations in normal pregnancy: new diagnostic thresholds are needed. Clin Chem. 2005;51:825–829. doi: 10.1373/clinchem.2004.044883. [DOI] [PubMed] [Google Scholar]
- 13.Kovac M, Mikovic Z, Rakicevic L, Srzentic S, Mandic V, Djordjevic V, et al. The use of d-dimer with new cutoff can be useful in diagnosis of venous thromboembolism in pregnancy. Eur J Obstet Gynecol Reprod Biol. 2010;148:27–30. doi: 10.1016/j.ejogrb.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 14.Curran-Everett D. A classic learning opportunity from Fenn, Rahn, and Otis (1946): the alveolar gas equation. Adv Physiol Educ. 2006;30:58–62. doi: 10.1152/advan.00076.2005. [DOI] [PubMed] [Google Scholar]
- 15.Damodaram M, Kaladindi M, Luckit J, Yoong W. D-dimers as a screening test for venous thromboembolism in pregnancy: is it of any use? J Obstet Gynaecol. 2009;29:101–103. doi: 10.1080/01443610802649045. [DOI] [PubMed] [Google Scholar]
- 16.To MS, Hunt BJ, Nelson-Piercy C. A negative D-dimer does not exclude venous thromboembolism (VTE) in pregnancy. J Obstet Gynaecol. 2008;28:222–240. doi: 10.1080/01443610801915975. [DOI] [PubMed] [Google Scholar]
- 17.British Thoracic Society. British Thoracic Society guidelines for the management of suspected acute pulmonary embolism. Thorax. 2003;58:470–83. [DOI] [PMC free article] [PubMed]
- 18.Bates SM. A negative quantitative latex D-dimer assay helped to rule out venous thromboembolism. Evid Based Med. 2001;6:188. doi: 10.1136/ebm.6.6.188. [DOI] [Google Scholar]
- 19.Stein PD, Goldhaber SZ, Henry JW. Alveolar-arterial oxygen gradient in the assessment of acute pulmonary embolism. Chest. 1995;107:139–143. doi: 10.1378/chest.107.1.139. [DOI] [PubMed] [Google Scholar]


