Abstract
Introduction
Extracranial vertebral artery aneurysm (EVAA) and extrapleural haematoma (EH) are rare clinical findings most often associated with blunt or penetrating trauma. However, EVAA rupture can be complicated by development of a large EH.
Report
A 50 year old man underwent an emergency thrombectomy followed by graft reconstruction of an aorto-bi-femoral bypass. The post-operative course was complicated by respiratory failure and severe anaemia. Computed tomography revealed EVAA rupture and EH, so ligation of EVAA was performed with thoracotomy.
Discussion
In a patient with extensive peripheral vascular disease and rapid development of EH, the rupture of a supra-aortic vessel aneurysm might be considered.
Keywords: Extracranial vertebral artery, Aneurysm, Rupture, Extrapleural haematoma
Highlights
-
•
Extracranial vertebral artery aneurysm is a rare clinical finding, representing less than 0.5% of all reported aneurysms.
-
•
Extrapleural haematoma is a rare complication of vertebral artery aneurysm rupture.
-
•
Extrapleural haematoma is a diagnostic challenge and can be life threatening.
Introduction
Vertebral artery aneurysms are rare clinical findings, representing 1% of supra-aortic aneurysms.1 The most common cause of extracranial vertebral artery aneurysms (EVAA) is penetrating neck trauma, but they can also occur secondary to dissection, atherosclerosis, infection, connective tissue disease, and inherited disorders. The rupture of an EVAA can lead to catastrophic bleeding and pose a diagnostic and therapeutic challenge. Extrapleural haematoma (EH) is also a rare entity usually caused by blunt or penetrating trauma, and is often misdiagnosed as a haemothorax. To the authors' knowledge, this is the first report describing intra-operative rupture of an atherosclerotic EVAA complicated by a large EH.
Report
A 50 year old man presented for an emergency thrombectomy followed by reconstruction of an aorto-bi-femoral graft. His past medical history included above knee femoropopliteal and aorto-bi-femoral bypass surgery, hypertension, hypercholesterolaemia, and non-insulin dependent diabetes mellitus. There was no history of previous head or neck injury and neurological examination was unremarkable. Immediately after endotracheal intubation he had a severe hypertensive episode with a blood pressure of 240/130 mmHg. This was successfully treated by boluses of labetalol and remifentanil. Surgery was uneventful, the patient was extubated on the table and transferred to the intensive care unit. Six hours after surgery the patient developed Type 2 respiratory failure and severe anaemia. Chest Xray revealed an almost complete white out of the left hemithorax. A left sided chest drain was inserted, draining only 20 mL of blood. An urgent CT of the chest and supra-aortic vessels was performed demonstrating a left vertebral artery (VA) V1 segment aneurysm with suspected rupture (Fig. 1). A large EH was present in the left hemithorax with a pathognomonic “displaced extrapleural fat” sign.2 This haematoma was expanding from the supraclavicular fossa, along the para-vertebral space and into the extrapleural space of the left hemithorax (Fig. 2). Despite fluid resuscitation, the patient became haemodynamically unstable so it was decided to perform an urgent ligation of the ruptured aneurysm and posterolateral thoracotomy for haematoma evacuation. A double lumen endotracheal tube was used for intubation and the patient was placed in the supine position. Exposure of the V1 segment was obtained through a modified Henry's approach,3 and the VA was ligated proximal and distal to the aneurysm. The patient was then placed in the right lateral position, one lung ventilation initiated and posterolateral thoracotomy was performed. Blood was evacuated (2500 mL) from the extrapleural space. The patient woke up with a Horner's syndrome (miosis, ptosis, enophthalmos) that completely resolved after 1 month. The rest of his post-operative course was uneventful and he was discharged home on the 10th post-operative day. After 1 year the patient was doing well with normal neurological and chest findings.
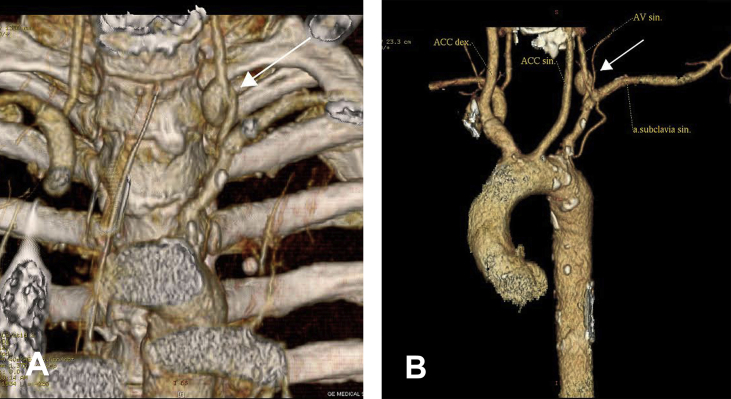
Figure 1.
(A and B), 3D reconstruction computed tomography scan showing a left vertebral artery aneurysm (arrow). (B), vertebral artery (VA), common carotid artery (ACC).
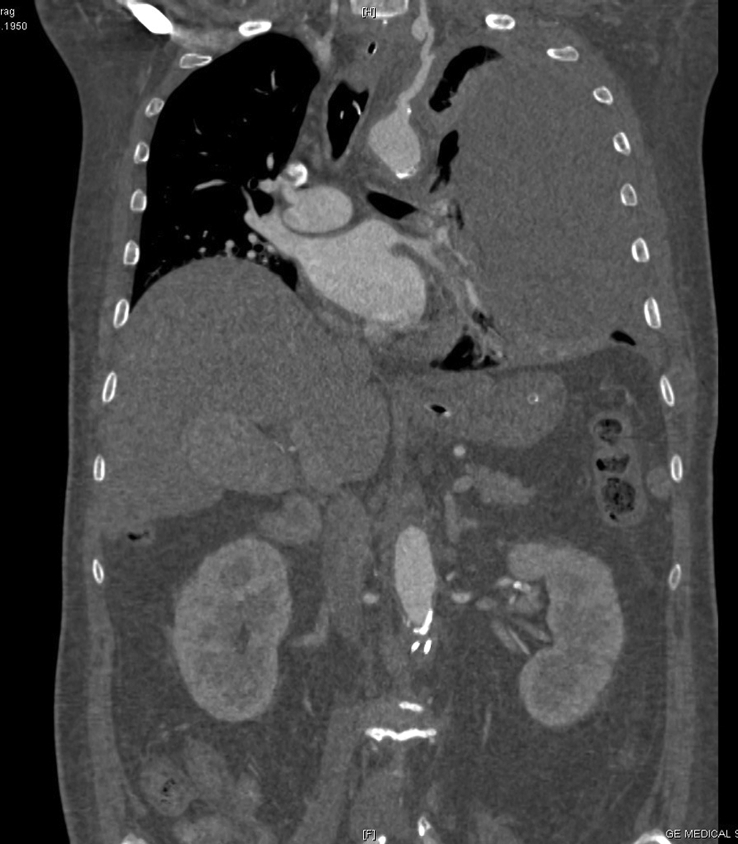
Figure 2.
Coronal computed tomography showing a large left extrapleural haematoma.
Discussion
EVAA can be congenital or acquired. The majority are located intracranially, and when they occur extracranially the most common cause is penetrating trauma, followed by blunt head and neck trauma.4 Non-traumatic EVAAs are less common, and potential causes include atherosclerosis, rheumatoid arthritis, infections, fibromuscular dysplasia, connective tissue and hereditary disorders including Ehlers Danlos syndrome, Marfan's syndrome, and neurofibromatosis type 1. Angiography is considered to be the gold standard for evaluating EVVA. Computed tomography angiography and magnetic resonance angiography are also important, especially when angiography provides insufficient information. Ruptured EVAA can be treated by endovascular procedures or by an open surgical approach. Endovascular therapies include embolisation of a small neck aneurysm with platinum coils, polyvinyl acetate foam particles, Onyx, and liquid n-butyl cyanoacrylate. Stent assisted coiling and the use of stent graft are alternative treatment methods.
The patient did not have signs or symptoms of connective tissue disease and denied a history of trauma. In view of his extensive peripheral vascular disease, it is thought that atherosclerosis was the main factor contributing to EVAA development and that the hypertensive crisis during induction of anaesthesia caused rupture. Ruptured EVAA can be treated by an endovascular or open surgical procedure. If a patient presents with haemodynamic instability and airway compromise resulting from expanding haematoma, open surgical approach is recommended. Extrapleural haematoma is defined as accumulation of blood between the parietal pleura and the endothoracic fascia and it is classified as spontaneous, traumatic, or iatrogenic.5 The most common cause is blunt chest trauma followed by penetrating trauma, aortic rupture, and iatrogenic injury. Diagnosis can be challenging and delayed especially when it is based solely on chest Xray. CT is recommended with a displaced extrapleural fat being pathognomonic. Based on CT findings, Chung et al.6 classified EH as bi-convex, commonly caused by arterial bleeding, and non-convex, a smaller volume associated with venous bleeding. Treatment options depend on the patient's clinical condition. Massive EH associated with haemodynamic instability and respiratory distress necessitates an urgent thoracotomy to control the bleeding and evacuate the clot.7
Conclusion
In a patient with complex vascular pathology, when a hypertensive crisis during surgery is associated with the rapid development of an extrapleural haematoma, although rare, rupture of a supra-aortic vessel aneurysm should be considered.
Conflict of interest
None.
Funding
None.
References
- 1.Cury M., Greenberg R.K., Morales J.P., Mohabbat W., Hernandez A.V. Supra-aortic vessels aneurysms: diagnosis and prompt intervention. J Vasc Surg. 2009;49:4–10. doi: 10.1016/j.jvs.2008.08.088. [DOI] [PubMed] [Google Scholar]
- 2.Aquino S.L., Chiles C., Oaks T. Displaced extrapleural fat as revealed by CT scanning: evidence of extrapleural hematoma. AJR Am J Roentgenol. 1997 Sep;169:687–689. doi: 10.2214/ajr.169.3.9275878. [DOI] [PubMed] [Google Scholar]
- 3.Henry A.K. 2nd ed. Churchill Livingstone; Edinburgh: 1973. Extensile exposure; pp. 58–74. [Google Scholar]
- 4.Morasch M.D., Phade S.V., Naughton P., Garcia-Toca M., Escobar G., Berguer R. Primary extracranial vertebral artery aneurysms. Ann Vasc Surg. 2013 May 31;27:418–423. doi: 10.1016/j.avsg.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Rashid M.A., Wikström T., Örtenwall P. Nomenclature, classification, and significance of traumatic extrapleural hematoma. J Trauma Acute Care Surg. 2000 Aug 1;49:286–290. doi: 10.1097/00005373-200008000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Chung J.H., Carr R.B., Stern E.J. Extrapleural hematomas: imaging appearance, classification, and clinical significance. J Thorac Imaging. 2011 Aug 1;26:218–223. doi: 10.1097/RTI.0b013e3181ebeaba. [DOI] [PubMed] [Google Scholar]
- 7.Poyraz A.S., Kilic D., Gultekin B., Ozulku M., Hatipoglu A. Extrapleural hematoma: when is surgery indicated? Monaldi Arch Chest Dis. 2005 Sep 30;63 doi: 10.4081/monaldi.2005.636. [DOI] [PubMed] [Google Scholar]