Abstract
Background
The Sewol ferry disaster caused national shock and grief in Korea. The present study examined the prevalence and associated factors of post-traumatic stress disorder (PTSD) symptoms among the surviving students 20 months after that disaster.
Methods
This study was conducted using a cross-sectional design and a sample of 57 students (29 boys and 28 girls) who survived the Sewol ferry disaster. Data were collected using a questionnaire, including instruments that assessed psychological status. A generalized linear model using a log link and Poisson distribution was performed to identify factors associated with PTSD symptoms.
Results
The results showed that 26.3% of participants were classified in the clinical group by the Child Report of Post-traumatic Symptoms score. Based on a generalized linear model, Poisson distribution, and log link analyses, PTSD symptoms were positively correlated with the number of exposed traumatic events, peers and social support, peri-traumatic dissociation and post-traumatic negative beliefs, and emotional difficulties. On the other hand, PTSD symptoms were negatively correlated with psychological well-being, family cohesion, post-traumatic social support, receiving care at a psychiatry clinic, and female gender.
Conclusion
This study uncovered risk and protective factors of PTSD in disaster-exposed adolescents. The implications of these findings are considered in relation to determining assessment and interventional strategies aimed at helping survivors following similar traumatic experiences.
Keywords: Sewol Ferry Disaster, Surviving Students, Post-traumatic Stress Disorder, Associated Factors
Graphical Abstract
INTRODUCTION
The Sewol ferry was carrying 476 people when it sank off the southwestern coast of Korea in April 2014, resulting in a loss of 304 lives. Of the 325 Danwon High School students on a class trip, only 75 were rescued and 250 died in the disaster. The ferry tragedy shocked and enraged the whole country as it became clear that it was almost entirely man-made, the result of an illegal redesign, an overloaded cargo bay, an inexperienced crew, and an unhealthy nexus between operators and state regulators.
One of the surviving passengers, who saved 20 students from the sinking ferry, attempted suicide 1 month after the accident. He slashed his wrist with a knife, but was found by his family and sent to a nearby hospital. His injury was not life threatening, but he has had to undergo post-traumatic stress disorder (PTSD) treatment. Another survivor developed PTSD much later. The tragic memories of the day suddenly started to disturb his life, which led him eventually to be fired from his job due to frequent absences.
The body of research conducted after disasters in the past three decades suggests that the burden of PTSD among persons exposed to disasters is substantial.1,2 The highest prevalence of PTSD is found among survivors and first responders.3 For example, 1 month after exposure, PTSD prevalence ranged from 20.3% among survivors of the 1993 Sivas religious uprisings in Turkey1 to 29% among survivors of the 1991 mass shooting episode in Killeen, Texas.2
Post-disaster PTSD is associated with a range of correlates, including sociodemographic and background factors, event exposure characteristics, social support factors, and personality traits.3 Peri-traumatic dissociation, a term used to describe a complex array of reactions to trauma, including depersonalization, derealization, and emotional numbness, has been associated with PTSD symptoms across a number of studies.4 Additionally, post-traumatic stress reactions are strongly related to quality of life. Children who are exposed to trauma report a lower quality of life than unexposed children.5 Veterans who screen positive for PTSD report greater difficulties in their relationships with romantic partners, less cohesion in their families, less social support, poorer social functioning, and lower life satisfaction compared with other treatment-seeking veterans.6 Many influential models of trauma-related psychological sequelae highlight the importance of individual negative beliefs about self, others, and the world.7
However, few studies are available on PTSD and related factors among survivors after the ferry disaster in Korea. Understanding factors associated with PTSD is important to identify disaster-exposed individuals who are at high risk and to provide targeted interventions and treatments.
The aim of this study was to identify the factors associated with symptoms of PTSD among the surviving students 20 months after that disaster. We hypothesized that the symptoms of PTSD among the surviving students would be severe and that demographic characteristics and psychological and interventional variables would be associated with symptoms of PTSD in this population. Thus, the aims of this study were to investigate symptoms of PTSD in surviving students 20 months after the Sewol ferry disaster and identify factors (demographic characteristics and psychological and interventional variables) associated with symptoms of PTSD.
METHODS
Participants and procedure
This study was conducted with survivors of the Korean Sewol ferry disaster from Danwon High School in December of 2015 (20 months after the disaster). During their last winter vacation as high school students, students were enrolled in the Disaster Cohort Study and were invited to participate in the present study. The invitation was offered in person by a school psychiatrist or psychologist, and all respondents had the opportunity to decline. Questionnaires were distributed to all 75 surviving students, and completed questionnaires were obtained from 62 students. In total, 57 questionnaires were included in the final analysis, after excluding five questionnaires with incomplete responses.
Variables and measurements
Variables to be evaluated were selected based on previous studies exploring factors related to PTSD after disasters.3,4,5,6,7 Socioeconomic variables including gender and birth year were collected. Students also completed the Strengths and Difficulties Questionnaire (SDQ), Peri-traumatic Dissociation–Post-traumatic Negative Beliefs–Post-traumatic Social Support (PTD-PTNB-PTSS) scale, Lifetime Incidence of Traumatic Events-Child (LITE-C), KIDSCREEN-27, Child Report of Post-traumatic Symptoms (CROPS), and the Family Adaptability and Cohesion Evaluation Scale (FACES)-III. Year of birth was categorized as 1997, 1998, and 1999.
The dependent variable of CROPS was used as a screening tool for determining post-traumatic symptoms in individuals who may or may not have had a traumatic childhood event.8 CROPS constitutes 26 items which assess post-traumatic symptoms during the previous 7 days, rated on a 3-point Likert scale (0 = “none”, 1 = “some”, 2 = “a lot”). The score is calculated by adding all item responses, and higher scores represent more post-traumatic symptoms. The cutoff identifies what is considered a clinical concern. Presently, the cutoff number for CROPS score is 19.8 Lee et al.9 translated CROPS into Korean, and assured its validity and reliability.
LITE-C is a checklist that assesses losses or trauma experienced by children and also evaluates how many times the trauma occurred, how the child felt at the time, and determined the age at which the trauma occurred.10 The items on the LITE-C include: house fires, death of a family member, witness to violence, sexual assault, exposure to threats, car accidents, and other distressing events. The LITE has a test-retest reliability of the r value of 0.80 (P < 0.001). The score is calculated by adding the number of “yes (experienced)” responses.
The KIDSCREEN (KIDSCREEN-52) considers the well-being (health-related quality of life) and the subjective health of children and adolescents.11 The instrument is a self-report measure developed for chronically ill and healthy children and adolescents 8–18 years old. The KIDSCREEN-27 is a shorter version of the KIDSCREEN-52, with good psychometric properties and minimum information loss.11 All five dimensions of the subsequent KIDSCREEN-52 are Rasch scales: physical well-being (five items), psychological well-being (seven items), autonomy & parents (seven items), peers & social support (four items), and school environment (four items).
FACES III assesses two major dimensions on the circumflex model: cohesion of the family and adaptation.12 This measure is applicable to families across the life-cycle, from young couples with no children to retired couples. The authors stated that children > 12 years old can complete the FACES III to enable comparisons between family members. There are four levels of adaptability ranging from low adaptability, to high adaptability: rigid, structured, flexible, and chaotic. Comparably, there are four levels of family cohesion: disengaged, separated, connected, and enmeshed. Family members estimate the relative truth of 20 statements (e.g., it is hard to identify the leaders in our family; family members ask each other for help). A second scale assesses what a family member would like in an ideal setting (e.g., we want to know the leader of our family; family members ask each other for help).
The PTD-PTNB-PTSS is a shortened version of the Post-trauma Risk checklist (PRC),13 and is a validated and valuable Korean instrument that measures risk factors for PTSD. Consisting of 57 items, it evaluates PTD, PTNB, and PTSS. The PTD-PTNB-PTSS consists of eight items selected from the PRC (three PTD items, 10 PTNB items, and five PTSS items) that were changed from yes or no questions to a 5-point Likert scale.
The SDQ is a concise behavioral questionnaire developed for the 3–16 years old age group.14 The SDQ inquires about 25 attributes, both positive and negative. There are many versions, to meet the needs of educators, researchers, and clinicians. The 25 items are separated among five scales: 1 = emotional symptoms; 2 = conduct problems; 3 = hyperactivity/inattention; 4 = peer relationship problems; 5 = prosocial behavior; scales 1–4 can be added together to create a total difficulties score. This self-report version is compatible with youths aged 11–16 years old, depending on their level of literacy and understanding.
Health and Therapeutics assess whether an individual is receiving outpatient treatment, attending pre-accident psychiatric treatment, or receiving psychotherapy. It also detects post-disaster use of help or services, including any kind of counseling, religious practices, care at a psychiatry clinic, or talking with a close friend. This includes any possible strategy that an individual might use to obtain support from others, both professional and non-professional. This information was obtained by asking “Yes or No” questions.
Statistical analysis
The subjects' general characteristics were determined through descriptive analyses of the data, and means, standard deviations, percentages and frequencies were all calculated. As the dependent variable, CROPS scores are count data that violate the distributional assumption of normality, and linear regression was inappropriate. Therefore, a generalized linear model, Poisson distribution, and a log link were conducted.15 No significant multicollinearity was detected when the variance inflation factor was evaluated. Stata/MP 14.2 software (StataCorp, College Station, TX, USA) was used for all statistical procedures, and the threshold for significance was P < 0.05 (two sided).
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of National Medical Center (IRB No. H-1505-054-002). Informed consent was submitted by all subjects when they were enrolled.
RESULTS
Table 1 summarizes the sociodemographic and health-related characteristics of the study participants. Twenty-nine of the 57 participants were male, and 28 were female. The majority of the participants were born in the year 1997 (82.5%). Health and Therapeutics determined that 75% of participants received outpatient treatment, and 26% of participants attended psychiatric therapy or received psychotherapy prior to the accident. The post-disaster use of services found that 50% of participants attended counseling, 10% participated in religious practices, 71% received care at a psychiatric department, and 52% talked with a close friend.
Table 1. Sociodemographic and health-related characteristics of the study population.
| Variables | Subcategory | No. or mean | % or SD |
|---|---|---|---|
| Gender | Male | 29 | 50.9 |
| Female | 28 | 49.1 | |
| Birth year | 1997 | 47 | 82.5 |
| 1998 | 9 | 15.8 | |
| 1999 | 1 | 1.8 | |
| LITE-C | (min = 0, max = 17) | 3.65 | 2.9 |
| KIDSCREEN-27 | Total score (min = 64, max = 135) | 93.36 | 19.5 |
| Physical well-being (min = 8, max = 25) | 16.21 | 4.2 | |
| Psychological well-being (min = 12, max = 35) | 24.91 | 5.6 | |
| Peers & social support (min = 6, max = 20) | 14.12 | 3.4 | |
| Autonomy & parents (min = 14, max = 35) | 23.91 | 5.8 | |
| School environment (min = 4, max = 20) | 12.88 | 3.9 | |
| FACES | Total score (min = 35, max = 100) | 67.98 | 15.9 |
| Cohesion (min = 10, max = 50) | 33.37 | 8.6 | |
| Adaptability (min = 10, max = 50) | 33.14 | 8.3 | |
| PTD-PTNB-PTSS | Total score (min = 15, max = 56) | 22.96 | 9.0 |
| Peri-traumatic dissociation (min = 3, max = 15) | 5.51 | 2.9 | |
| Post-traumatic negative beliefs (min = 10, max = 33) | 16.54 | 6.3 | |
| Post-traumatic social support (min = 5, max = 15) | 6.18 | 2.3 | |
| SDQ | Difficulties | 11.39 | 5.7 |
| Strengths | 6.63 | 1.9 | |
| Receiving outpatient treatment | No | 43 | 75.4 |
| Yes | 14 | 24.6 | |
| Attending pre-accident psychiatric therapy, or receiving psychotherapy | No | 42 | 73.7 |
| Yes | 15 | 26.3 | |
| Counseling | No | 28 | 49.1 |
| Yes | 29 | 50.9 | |
| Religious practices | No | 51 | 89.5 |
| Yes | 6 | 10.5 | |
| Receiving care at the psychiatry clinic | No | 16 | 28.1 |
| Yes | 41 | 71.9 | |
| Talking with close friend | No | 27 | 47.4 |
| Yes | 30 | 52.6 | |
| CROPS | (min = 0, max = 37) | 12.51 | 9.5 |
SD = standard deviation, LITE-C = Lifetime Incidence of Traumatic Events-Child, FACES = Family Adaptability and Cohesion Evaluation Scale, PTD-PTNB-PTSS = Peri-traumatic Dissociation–Post-traumatic Negative Beliefs–Post-traumatic Social Support, SDQ = strengths and difficulties questionnaire, CROPS = Child Report of Post-traumatic Symptoms, min = minimum, max = maximum.
Table 2 summarizes the clinical classification of the study population. The participants were classified into the KIDSCREEN-27 clinical groups as follows: 16.0% (autonomy & parents dimension), 43.8% (psychological well-being, peers & social support, and autonomy & parents dimension), and 21.0% (school environment dimension). The participants were classified into the following SDQ clinical groups: 12.0% (prosocial behavior dimension), 5.3% (emotional symptoms dimension), 14.0% (conduct problems dimension), 8.8% (hyperactivity/inattention dimension), and 8.8% (peer relationship problems dimension). About 26.3% of participants were classified into the clinical group by the CROPS score.
Table 2. Clinical classification of study population.
| Variables | Subcategory | Normal group | Clinical group |
|---|---|---|---|
| KIDSCREEN-27 | Physical well-being | 48 (84.2) | 9 (15.8) |
| Psychological well-being | 32 (56.1) | 25 (43.8) | |
| Peers & social support | 32 (56.1) | 25 (43.8) | |
| Autonomy & parents | 32 (56.1) | 25 (43.8) | |
| School environment | 45 (78.9) | 12 (21.0) | |
| SDQ | Prosocial behavior | 50 (87.7) | 7 (12.3) |
| Emotional symptoms | 54 (94.7) | 3 (5.3) | |
| Conduct problems | 49 (86.0) | 8 (14.0) | |
| Hyperactivity/inattention | 52 (91.2) | 5 (8.8) | |
| Peer relationship problems | 52 (91.2) | 5 (8.8) | |
| CROPS | 42 (73.7) | 15 (26.3) |
Values are presented as number (%).
SDQ = Strengths and Difficulties Questionnaire, CROPS = Child Report of Post-traumatic Symptoms.
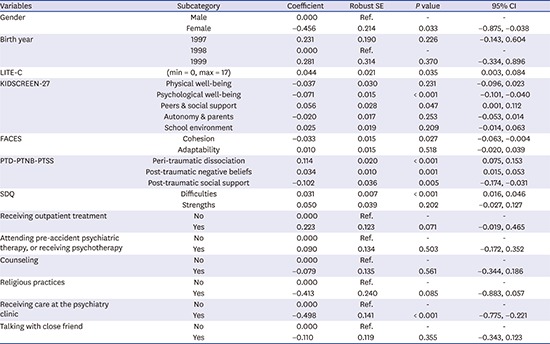
Table 3 summarizes the results from the generalized linear model identifying factors related to CROPS after controlling for sociodemographic and psychological factors. After adjusting for birth year and gender covariates, CROPS was significantly associated with gender, LITE-C, psychological well-being, and the peer and the social support dimension of KIDSCREEN-27, the cohesion dimension of FACES, peri-traumatic dissociation, post-traumatic negative beliefs, post-traumatic social support dimensions of PTD-PTNB-PTSS, difficulties dimension of SDQ, and receiving care at the psychiatry clinic for the post-disaster use of service. Higher scores on the LITE-C (coefficient [coef.] = 0.044; P = 0.035; 95% confidence interval [CI], 0.003–0.084), peers and social support dimension of KIDSCREEN-27 (coef. = 0.056; P = 0.047; 95% CI, 0.001–0.112), peri-traumatic dissociation (coef. = 0.114; P < 0.001; 95% CI, 0.075–0.153), and post-traumatic negative beliefs (coef. = 0.034; P < 0.001; 95% CI, 0.015–0.053), dimensions of PTD-PTNB-PTSS, and the difficulties dimension of SDQ (coef. = 0.031; P < 0.001; 95% CI, 0.016–0.046) were all variables significantly associated with higher CROPS scores. On the other hand, higher scores of the psychological well-being (coef. = −0.071; P < 0.001; 95% CI, −0.101, −0.040) dimension of KIDSCREEN-27, the cohesion dimension of FACES (coef. = −0.033; P = 0.027; 95% CI, −0.063, −0.004), the post-traumatic social support dimension of PTD-PTNB-PTSS (coef. = −0.102; P = 0.005; 95% CI, −0.174, −0.031), individuals receiving care at a psychiatry clinic (coef. = −0.498; P < 0.001; 95% CI, −0.775, −0.221), and female gender (coef. = −0.456; P = 0.033; 95% CI, −0.875, −0.038) were all variables significantly associated with lower CROPS scores.
Table 3. Results from generalized linear models evaluating the factors associated with CROPS.
| Variables | Subcategory | Coefficient | Robust SE | P value | 95% CI |
|---|---|---|---|---|---|
| Gender | Male | 0.000 | Ref. | - | - |
| Female | −0.456 | 0.214 | 0.033 | −0.875, −0.038 | |
| Birth year | 1997 | 0.231 | 0.190 | 0.226 | −0.143, 0.604 |
| 1998 | 0.000 | Ref. | - | - | |
| 1999 | 0.281 | 0.314 | 0.370 | −0.334, 0.896 | |
| LITE-C | (min = 0, max = 17) | 0.044 | 0.021 | 0.035 | 0.003, 0.084 |
| KIDSCREEN-27 | Physical well-being | −0.037 | 0.030 | 0.231 | −0.096, 0.023 |
| Psychological well-being | −0.071 | 0.015 | < 0.001 | −0.101, −0.040 | |
| Peers & social support | 0.056 | 0.028 | 0.047 | 0.001, 0.112 | |
| Autonomy & parents | −0.020 | 0.017 | 0.253 | −0.053, 0.014 | |
| School environment | 0.025 | 0.019 | 0.209 | −0.014, 0.063 | |
| FACES | Cohesion | −0.033 | 0.015 | 0.027 | −0.063, −0.004 |
| Adaptability | 0.010 | 0.015 | 0.518 | −0.020, 0.039 | |
| PTD-PTNB-PTSS | Peri-traumatic dissociation | 0.114 | 0.020 | < 0.001 | 0.075, 0.153 |
| Post-traumatic negative beliefs | 0.034 | 0.010 | 0.001 | 0.015, 0.053 | |
| Post-traumatic social support | −0.102 | 0.036 | 0.005 | −0.174, −0.031 | |
| SDQ | Difficulties | 0.031 | 0.007 | < 0.001 | 0.016, 0.046 |
| Strengths | 0.050 | 0.039 | 0.202 | −0.027, 0.127 | |
| Receiving outpatient treatment | No | 0.000 | Ref. | - | - |
| Yes | 0.223 | 0.123 | 0.071 | −0.019, 0.465 | |
| Attending pre-accident psychiatric therapy, or receiving psychotherapy | No | 0.000 | Ref. | - | - |
| Yes | 0.090 | 0.134 | 0.503 | −0.172, 0.352 | |
| Counseling | No | 0.000 | Ref. | - | - |
| Yes | −0.079 | 0.135 | 0.561 | −0.344, 0.186 | |
| Religious practices | No | 0.000 | Ref. | - | - |
| Yes | −0.413 | 0.240 | 0.085 | −0.883, 0.057 | |
| Receiving care at the psychiatry clinic | No | 0.000 | Ref. | - | - |
| Yes | −0.498 | 0.141 | < 0.001 | −0.775, −0.221 | |
| Talking with close friend | No | 0.000 | Ref. | - | - |
| Yes | −0.110 | 0.119 | 0.355 | −0.343, 0.123 |
CROPS = Child Report of Post-traumatic Symptoms, SE = standard error, CI = confidence interval, LITE-C = Lifetime Incidence of Traumatic Events-Child, FACES = Family Adaptability and Cohesion Evaluation Scale, PTD-PTNB-PTSS = Peri-traumatic Dissociation–Post-traumatic Negative Beliefs–Post-traumatic Social Support, SDQ = Strengths and Difficulties Questionnaire.
DISCUSSION
The present study is the first to examine factors related to PTSD symptoms in Danwon High School survivors. The prevalence of PTSD observed in this study was comparable to that following man-made disaster.3 In the present study, 26.3% of participants screened positive as manifesting PTSD, even 20 months after the ferry disaster, which is higher than that of community volunteers16 and lower than that of bereaved parents who lost their children due to the ferry disaster.17 Previous studies following the Sewol ferry disaster in Korea reported that clinically relevant PTSD symptoms were observed in 19.7% of community volunteers16 and in 70.2% of bereaved parents.17 Those findings could be explained by the high risk of PTSD associated with severity of exposure to disaster across numerous studies. The prevalence of PTSD is higher among persons who are directly exposed to a disaster (often referred as the ‘victims’ of a disaster in disaster studies), and lower among rescue workers and first responder populations.3 A study that evaluated post-traumatic stress symptoms (PTSS) in Korean adolescents who lived in Jindo, a disaster-affected community, reported that directly witnessing the rescue scene was significantly associated with PTSS.18 In addition, a systematic review and meta-analysis revealed that the combined incidence of PTSD among survivors with bereavement after disasters was higher than that of survivors without bereavement.19
A well-established finding is that females are more likely to develop PTSD after disasters.19 However, the female gender was associated with lower PTSS scores in our study. This finding was not easy to explain but could linked to the following: Danwon High School established a Mental Health Center after the ferry sank, and a full-time school psychiatrist and several psychologists provided the students with regular mental health checkups and any necessary counseling, which might have reduced sex differences in coping styles between males and females after surviving a disaster. Moreover, males became old enough to perform inevitable duties of military service at the study point, which would have been felt by some of them as a distressful burden.
Third, we found that family cohesion was a protective factor for PTSS 20 months after the disaster. Our study did not aim to reveal causal relationships among the factors. Although the regression analyses did not support the predictive relationship between family phenomena and PTSS in youth exposed to various traumas, the prospective studies favored significant relationships between family phenomena and youth PTSS according to a systematic literature review.20 In addition, a study that assessed the longitudinal interrelationship between PTSS and family cohesion among combat veterans reported the bi-directional mutual effects of PTSS and family cohesion over time.21
Individuals receiving care at a psychiatry clinic and post-traumatic social support were variables significantly associated with lower PTSS in this study, which is similar to previous studies.22,23,24 Having a lower level of social support was a risk factor for long-term adverse psychological outcomes among flood survivors after the disaster.22 Whether young adults who survived a shipping disaster in adolescence received post-disaster support at school was a predictive factor for duration and severity of PTSD.23 Participants who received mental health support showed a lower level of complicated grief than those who did not receive it after the Sewol ferry accident.24 Thus, receiving psychiatric care and social support may be useful in PTSD intervention and prevention for adolescents with traumatic experiences in the early stage after disasters.
Several limitations of this study should be mentioned. First, the cross-sectional design made it difficult to identify causal relationships among factors. As a result, a longitudinal study is recommended. Second, some sampling bias may have occurred, as only 75% of the surviving students participated in the study. Therefore, it is unclear whether the findings of our study are generalizable to other survivors who suffered from the ferry disaster. Third, the prevalence of PTSD was measured using a self-report assessment tool rather than a structured clinical interview. Self-reporting does not always provide an accurate representation of PTSD symptomatology. However, the CROPS assessment tool used in this study was well validated for Korean children and adolescents.
In summary, this study indicated that PTSD symptoms were prevalent among the high school survivors, even 20 months after the ferry disaster in Korea. We found that the number of experienced traumatic events, peri-traumatic dissociation, post-traumatic negative beliefs, difficulties, and peers and social support were risk factors significantly related to PTSS in this population. Female gender, psychological well-being, family cohesion, post-traumatic social support, and receiving care at a psychiatry clinic were protective factors. More importantly, these findings may help those providing psychological health interventions to identify survivors who are at high risk of PTSD after similar disasters in Korea.
Footnotes
Funding: This study was supported by a grant from the Korean Mental Health Technology R & D Project, Ministry of Health & Welfare, Republic of Korea (HM15C1054).
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contributions: Conceptualization: Lee SH, Kim EJ. Investigation: Lee SH, Kim EJ, Chae JH. Data curation: Lee SH, Kim EJ, Noh JW. Formal analysis: Lee SH, Noh JH. Writing - original draft: Lee SH, Kim EJ, Noh JW, Chae JH. Writing - review & editing: Lee SH, Kim EJ, Noh JW, Chae JH.
References
- 1.Sungur M, Kaya B. The onset and longitudinal course of a man-made post-traumatic morbidity: survivors of the Sivas disaster. Int J Psychiatry Clin Pract. 2001;5(3):195–202. doi: 10.1080/136515001317021662. [DOI] [PubMed] [Google Scholar]
- 2.North CS, Smith EM, Spitznagel EL. Posttraumatic stress disorder in survivors of a mass shooting. Am J Psychiatry. 1994;151(1):82–88. doi: 10.1176/ajp.151.1.82. [DOI] [PubMed] [Google Scholar]
- 3.Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38(4):467–480. doi: 10.1017/S0033291707001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thompson-Hollands J, Jun JJ, Sloan DM. The association between peritraumatic dissociation and PTSD symptoms: the mediating role of negative beliefs about the self. J Trauma Stress. 2017;30(2):190–194. doi: 10.1002/jts.22179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alisic E, van der Schoot TA, van Ginkel JR, Kleber RJ. Looking beyond posttraumatic stress disorder in children: posttraumatic stress reactions, posttraumatic growth, and quality of life in a general population sample. J Clin Psychiatry. 2008;69(9):1455–1461. doi: 10.4088/jcp.v69n0913. [DOI] [PubMed] [Google Scholar]
- 6.Tsai J, Harpaz-Rotem I, Pietrzak RH, Southwick SM. The role of coping, resilience, and social support in mediating the relation between PTSD and social functioning in veterans returning from Iraq and Afghanistan. Psychiatry. 2012;75(2):135–149. doi: 10.1521/psyc.2012.75.2.135. [DOI] [PubMed] [Google Scholar]
- 7.Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther. 2000;38(4):319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- 8.Greenwald R, Rubin A. Assessment of posttraumatic symptoms in children: development and preliminary validation of parent and child scales. Res Soc Work Pract. 1999;9(1):61–75. [Google Scholar]
- 9.Lee KM, Jeong SH, Lee WK, Chung US. Reliability and validity of the Korean version of the child report of post-traumatic symptoms (CROPS) and the parent report of post-traumatic symptoms (PROPS) J Korean Acad Child Adolesc Psychiatry. 2011;22(3):169–181. [Google Scholar]
- 10.Prigerson HG, Maciejewski PK, Reynolds CF, 3rd, Bierhals AJ, Newsom JT, Fasiczka A, et al. Inventory of complicated grief: a scale to measure maladaptive symptoms of loss. Psychiatry Res. 1995;59(1-2):65–79. doi: 10.1016/0165-1781(95)02757-2. [DOI] [PubMed] [Google Scholar]
- 11.Ravens-Sieberer U, Auquier P, Erhart M, Gosch A, Rajmil L, Bruil J, et al. The KIDSCREEN-27 quality of life measure for children and adolescents: psychometric results from a cross-cultural survey in 13 European countries. Qual Life Res. 2007;16(8):1347–1356. doi: 10.1007/s11136-007-9240-2. [DOI] [PubMed] [Google Scholar]
- 12.Olson DH. FACES III (Family Adaptation and Cohesion Scales) St. Paul, MN: University of Minnesota; 1985. [Google Scholar]
- 13.Joo HS, Ahn HN. Development and validation of posttrauma risk checklist, Korean. Korean J Psychol Gen. 2008;27(1):235–257. [Google Scholar]
- 14.Kim MH, Ahn JS, Min S. Psychometric properties of the self-report version of the strengths and difficulties questionnaire in Korea. Psychiatry Investig. 2015;12(4):491–499. doi: 10.4306/pi.2015.12.4.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 16.Lee JY, Kim SW, Bae KY, Kim JM, Shin IS, Yoon JS. Factors associated with posttraumatic stress disorder symptoms among community volunteers during the Sewol ferry disaster in Korea. Compr Psychiatry. 2017;77(1):38–44. doi: 10.1016/j.comppsych.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Huh HJ, Huh S, Lee SH, Chae JH. Unresolved bereavement and other mental health problems in parents of the sewol ferry accident after 18 months. Psychiatry Investig. 2017;14(3):231–239. doi: 10.4306/pi.2017.14.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee JY, Kim SW, Bae KY, Kim JM, Shin IS, Yoon JS. Factors associated with post-traumatic stress symptoms among adolescents exposed to the Sewol ferry disaster in Korea. Psychiatry Res. 2017;256(1):391–395. doi: 10.1016/j.psychres.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 19.Dai W, Chen L, Lai Z, Li Y, Wang J, Liu A. The incidence of post-traumatic stress disorder among survivors after earthquakes:a systematic review and meta-analysis. BMC Psychiatry. 2016;16(1):188. doi: 10.1186/s12888-016-0891-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McDonald CC, Deatrick JA. The role of family phenomena in posttraumatic stress in youth. J Child Adolesc Psychiatr Nurs. 2011;24(1):38–50. doi: 10.1111/j.1744-6171.2010.00258.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zerach G, Solomon Z, Horesh D, Ein-Dor T. Family cohesion and posttraumatic intrusion and avoidance among war veterans: a 20-year longitudinal study. Soc Psychiatry Psychiatr Epidemiol. 2013;48(2):205–214. doi: 10.1007/s00127-012-0541-6. [DOI] [PubMed] [Google Scholar]
- 22.Dai W, Kaminga AC, Tan H, Wang J, Lai Z, Wu X, et al. Long-term psychological outcomes of flood survivors of hard-hit areas of the 1998 Dongting Lake flood in China: prevalence and risk factors. PLoS One. 2017;12(2):e0171557. doi: 10.1371/journal.pone.0171557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Udwin O, Boyle S, Yule W, Bolton D, O'Ryan D. Risk factors for long-term psychological effects of a disaster experienced in adolescence: predictors of post traumatic stress disorder. J Child Psychol Psychiatry. 2000;41(8):969–979. [PubMed] [Google Scholar]
- 24.Han H, Noh JW, Huh HJ, Huh S, Joo JY, Hong JH, et al. Effects of mental health support on the grief of bereaved people caused by sewol ferry accident. J Korean Med Sci. 2017;32(7):1173–1180. doi: 10.3346/jkms.2017.32.7.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]


