Abstract
Background
To investigate the repeatability and accuracy of quantitative CT (QCT) measurement of bone mineral density (BMD) by low-mAs using iterative model reconstruction (IMR) technique based on phantom model.
Methods
European spine phantom (ESP) was selected and measured on the Philips Brilliance iCT Elite FHD machine for 10 times. Data were transmitted to the QCT PRO workstation to measure BMD (mg/cm3) of the ESP (L1, L2, L3). Scanning method: the voltage of X-ray tube is 120 kV, the electric current of X-ray tube output in five respective groups A–E were: 20, 30, 40, 50 and 60 mAs. Reconstruction: all data were reconstructed using filtered back projection (FBP), IR levels of hybrid iterative reconstruction (iDose4, levels 1, 2, 3, 4, 5, 6 were used) and IMR (levels 1, 2, 3 were used). ROIs were placed in the middle of L1, L2 and L3 spine phantom in each group. CT values, noise and contrast-to-noise ratio (CNR) were measured and calculated. One-way analysis of variance (ANOVA) was used to compare BMD values of different mAs and different IMR.
Results
Radiation dose [volume CT dose index (CTDIvol) and dose length product (DLP)] was positively correlated with tube current. In L1 with low BMD, different mAs in FBP showed P<0.05, indicating statistically significant BMD in ESP. In other iterative algorithms, different mAs under same iterative algorithms showed P>0.05, indicating no difference in BMD. And P>0.05 was observed among BMD of spine phantom in L1, L2 and L3 under same mAs joined with varied iterative reconstruction. The BMD in L1 varied greatly during FBP reconstruction, and less variation was observed in reconstruction of IMR [1] and IMR [2]. The BMD of L2 changed more during FBP reconstruction, where less was observed in IMR [2]. The BMD of L3 varied greatly during FBP reconstruction, and was less varied in all levels of iDose4 and reconstruction of IMR [2]. In addition, along with continuous mAs incensement, the CNRs in various algorithms continued to increase. Among them, CNR with the FBP algorithm is the lowest, and CNR of the IMR [3] algorithm is the highest.
Conclusions
Repeated measurements of BMD with QCT in the ESP multicenter showed that BMD changes in L1–L3 are the least varied at IMR [2] algorithm. It is recommended to scan at 120 kV with 20 mAs combined with IMR [2] algorithm. In this way, the BMD of spine by QCT could be accurately measured, while radiation dosage significantly reduced and imaging quality improved at the same time.
Keywords: Quantitative CT (QCT), bone mineral density (BMD), European spine phantom (ESP), X-ray computer, radiation dosage, iterative model reconstruction (IMR)
Introduction
Osteoporosis can be diagnosed by noninvasive bone mineral density (BMD) test, and BMD usually reflect more than 75% of bone strength (1). Recent studies have shown that the proportion of osteoporosis in men and women over the age of 50 in China is 10.4% and 31.2% respectively (2), indicating an increasing demand for BMD measurement. Nowadays, it is of great research interest to use reasonable low-dose in BMD measurement combined with low-dose CT scan under the premise of meeting clinical diagnostic imaging quality. The objective of this study was to repeatedly measure BMD of a known internal “real-density” European spine phantom (ESP) using multicenter lumbar quantitative CT (QCT) (3). The accuracy of different mAs and different iterative algorithms was evaluated and the deviation in the repeatability and accuracy of QCT BMD measurement with low mAs joint iterative algorithms was explored under the premise of not affecting the BMD accuracy.
Methods
Research subjects
This study measured and analyzed the same ESP (No.145, Germany ORM company). The ESP adopted for QCT examination is a phantom that simulates spine of the human body and was used to standardize and calibrate BMD measuring instruments, applied both for dual X-ray absorptiometry (DXA) and QCT. It could be used for routine quality control (4). ESP is composed of plastic made of epoxy resin plus a variety of other ingredients which is equivalent to water and bone solid material composition, including three trabecular of unequal BMD. The hydroxyapatite density of three trabecular were L1 (50 mg/cm3), L2 (100 mg/cm3) and L3 (200 mg/cm3) (3). BMD of the ESP was measured on a Philips Brilliance iCT Elite FHD machine. CT was performed according to the set conventional spine scanning conditions: scanning method: tube voltages were all set as 120 kV and the tube currents were respectively set as A–E (20, 30, 40, 50, 60 mAs). Reconstruction: both filtered back projection (FBP), iDose4 (levels 1, 2, 3, 4, 5, 6) and iterative model reconstruction (IMR) (levels 1, 2, 3) data reconstruction were conducted. When using traditional filtered-back projection (FBP) reconstruction, there usually inevitably exist many artifacts. Different from traditional FBP, IMR technique adopted the matrix algebra to selectively distinguish and remove image noise through mathematic model. iDose4 is the 4th generation reconstruction algorithm, which combined both FBP and IMR. IMR is a new iterative algorithm without FBP part, showing significant benefit in removing image noise towards low dosage CT scanning. Screw pitch was set as 0.914. Scanning layer thickness, interlayer spacing were set as 5 mm. Recombination layer thickness, layer spacing were set as 1 mm. X-ray tube rotation speed was 0.5 s/r; matrix as 512×512, DFOV 500 mm. Bed height and initial bed height were set as 146 mm. The same examiner performed 10 scans without reposition. Scan data were uploaded to the BMD workstation (Mindways QCT PRO workstation) for analysis, BMD of each ESP cancellous (measured in mg/cm3) was calculated. During above measurements, unless obvious errors occurred in the operation, workstation softwares were adopted for automatic analysis, such as automatic functions, automatic detection of boundaries, and automatic generation of ROIs.
Objective assessment of ESP phantom images
The following indicators were jointly measured by two radiologists. The middle of L1, L2 and L3 was marked on the coronal images and correlated to the corresponding axial images. The ROIs were set at L1, L2 and L3. The circular area was about 2/3 of the entire lumbar axial image. CT value was recorded as CT1; At the same time, ROI was placed at a position 2/3 from anterior margin of lumbar spine to ventral front of corresponding lumbar vertebra (water as material). CT value was measured and recorded as CT2. The standard deviation (SD) was set as image background noise. Contrast-to-noise ratio (CNR) was calculated, CNR = (CT1 − CT2)/SD.
Dose volume
Volume CT dose index (CTDIvol) and dose length product (DLP) were automatically calculated by computer.
Statistics
SPSS 21.0 software was used for statistical analysis. One-way analysis of variance (ANOVA) was used to compare BMD values of different mAs and different iterative algorithms. P<0.05 was defined as statistically significant.
Results
Radiation dose of ESP under different mAs scanning and 120 kV tube voltage
The blue line in Figure 1 above indicated that CTDIvol showed a linear increase trend under different mAs. The red indicated that DLP shows a linear increase trend using different mAs. Radiation dose was positively correlated to tube current output.
Figure 1.
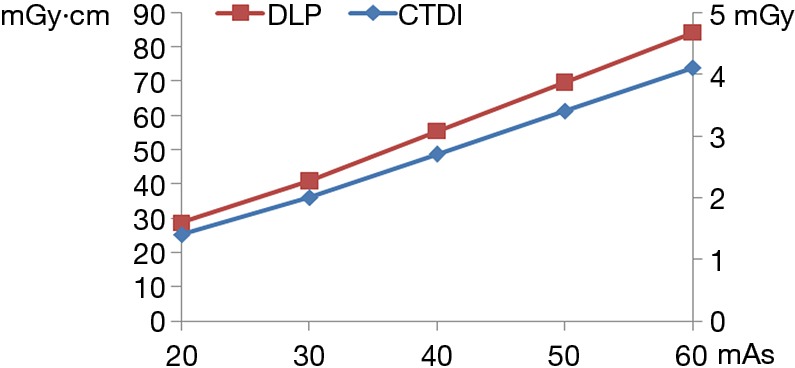
Comparison of ESP scanning dose at different mAs but same 120 Kv. ESP, European spine phantom; DLP, dose length product; CTDI, CT dose index.
Lumbar BMD at 120 kV tube voltage, varying mAs and iterative algorithms
As shown in the following Tables 1, 2 and 3, in L1 with low BMD, different mAs in FBP showed P<0.05, indicating statistically significant BMD in ESP. In other iterative algorithms, different mAs under same iterative algorithms showed P>0.05, indicating no difference in BMD. In L2 and L3, P>0.05 were observed under the same iterative algorithms but different mAs, indicating there was no statistical difference in ESP BMD. L1, L2 and L3 showed statistically same BMD in ESP in same mAs and different iterative algorithms, with P>0.05. BMD of L1 varied greatly during FBP reconstruction, and was less changed in IMR [1] and IMR [2] reconstruction. BMD of L2 changed more during FBP reconstruction, while changed less during IRM [2] reconstruction. BMD of L3 varied greatly during FBP reconstruction, and they varied less in all levels of iDose4 and IMR [2] reconstruction. In addition, along the increase of mAs, CNRs increased despite various reconstruction algorithms. Among them, CNR of the FBP reconstruction algorithm was the lowest, and CNR of the IMR [3] reconstruction was the highest.
Table 1. L1 bone mineral density and their statistics under different mAs and different iterative algorithms.
| Algorithms | 20 mAs | 30 mAs | 40 mAs | 50 mAs | 60 mAs | P |
|---|---|---|---|---|---|---|
| FBP | 45.86 | 45.70 | 46.60 | 48.69 | 46.80 | 0.035 |
| iDose4 [1] | 47.69 | 47.63 | 48.32 | 47.98 | 47.70 | 0.552 |
| iDose4 [2] | 47.63 | 47.54 | 48.13 | 48.31 | 46.87 | 0.326 |
| iDose4 [3] | 47.28 | 47.87 | 48.36 | 48.01 | 47.82 | 0.103 |
| iDose4 [4] | 47.42 | 47.62 | 48.29 | 48.31 | 47.23 | 0.301 |
| iDose4 [5] | 47.78 | 47.79 | 48.54 | 48.12 | 47.70 | 0.252 |
| iDose4 [6] | 47.30 | 47.05 | 48.92 | 48.32 | 47.58 | 0.058 |
| IMR [1] | 46.22 | 46.36 | 47.18 | 47.43 | 46.86 | 0.623 |
| IMR [2] | 46.08 | 45.82 | 47.66 | 46.84 | 46.99 | 0.26 |
| IMR [3] | 46.35 | 46.27 | 47.50 | 46.63 | 47.07 | 0.35 |
| P | 0.052 | 0.056 | 0.466 | 0.405 | 0.963 | – |
FBP, filtered back projection; IMR, iterative model reconstruction.
Table 2. L2 bone mineral density and their statistics under different mAs and different iterative algorithms.
| Algorithms | 20 mAs | 30 mAs | 40 mAs | 50 mAs | 60 mAs | P |
|---|---|---|---|---|---|---|
| FBP | 97.94 | 98.29 | 98.23 | 98.57 | 98.08 | 0.146 |
| iDose4 [1] | 101.83 | 100.4 | 100.27 | 100.13 | 99.51 | 0.137 |
| iDose4 [2] | 101.44 | 101.12 | 100.4 | 99.88 | 99.75 | 0.37 |
| iDose4 [3] | 101.77 | 100.87 | 99.81 | 100.39 | 100.04 | 0.163 |
| iDose4 [4] | 101.42 | 100.45 | 100.05 | 100.49 | 100.28 | 0.12 |
| iDose4 [5] | 101.62 | 101.25 | 99.85 | 100.68 | 99.71 | 0.129 |
| iDose4 [6] | 101.84 | 101.21 | 100.45 | 99.92 | 99.45 | 0.064 |
| IMR [1] | 100.85 | 99.49 | 99.19 | 99.15 | 99.13 | 0.229 |
| IMR [2] | 100.8 | 99.91 | 99.21 | 98.81 | 98.98 | 0.08 |
| IMR [3] | 100.15 | 99.23 | 98.75 | 98.77 | 98.65 | 0.194 |
| P | 0.051 | 0.061 | 0.076 | 0.079 | 0.075 | – |
FBP, filtered back projection; IMR, iterative model reconstruction.
Table 3. L3 bone mineral density and their statistics under different mAs and different iterative algorithms.
| Algorithms | 20 mAs | 30 mAs | 40 mAs | 50 mAs | 60 mAs | P |
|---|---|---|---|---|---|---|
| FBP | 191.56 | 191.19 | 190.45 | 193.3 | 191.82 | 0.215 |
| iDose4 [1] | 193.95 | 193.97 | 193.16 | 193.24 | 192.62 | 0.087 |
| iDose4 [2] | 194.26 | 193.04 | 192.8 | 194.82 | 193.00 | 0.078 |
| iDose4 [3] | 195.07 | 193.75 | 193.07 | 194.07 | 192.42 | 0.266 |
| iDose4 [4] | 193.11 | 193.1 | 192.98 | 194.98 | 193.23 | 0.15 |
| iDose4 [5] | 194.02 | 193.09 | 192.5 | 195.09 | 193.05 | 0.078 |
| iDose4 [6] | 193.96 | 193.61 | 192.2 | 194.28 | 192.38 | 0.096 |
| IMR [1] | 192.71 | 191.1 | 191.07 | 192.05 | 191.61 | 0.242 |
| IMR [2] | 192.70 | 190.72 | 191.78 | 191.86 | 191.11 | 0.086 |
| IMR [3] | 192.01 | 190.17 | 191.58 | 191.31 | 191.16 | 0.059 |
| P | 0.053 | 0.051 | 0.165 | 0.052 | 0.08 | – |
FBP, filtered back projection; IMR, iterative model reconstruction.
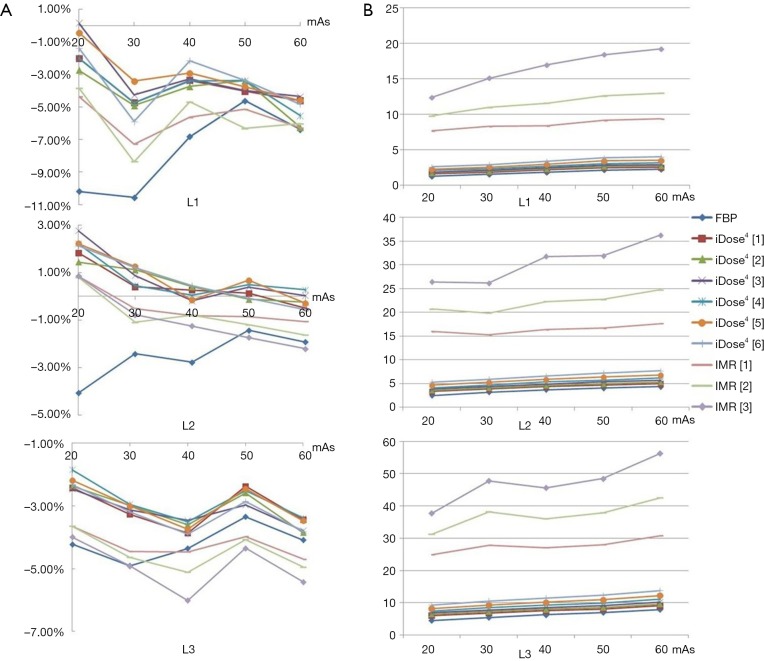
Deviation in BMD accuracy
The accuracy deviation of BMD in each lumbar was measured under different iterative algorithms and different mAs. Results were shown in Figure 2 below on the left. The objective evaluation of CNR images was shown in Figure 2 below on the right. The L1 BMD showed a larger change under FBP reconstruction as indicated in Figure 2. Among them, when measuring iDose4 [1] of L1, the image noise is getting lower with the increase of mAs, and CNR at 60 mAs is 70% higher than that at 20 mAs. With the proportion of different iterative algorithms increased at 20 mAs, image noise reduced significantly, with a 69.6% CNR increase in IMR [3] over FBP reconstruction. In addition, the maximum accuracy deviation of L1 is 11%, the maximum accuracy deviation in L2 is 4%, and the maximum accuracy deviation in L3 is 6%.
Figure 2.
Accuracy deviation in ESP bone mineral density and CNR comparison. (A) Indicated accuracy deviation among L1, L2 and L3; (B) indicated CNR comparison among L1, L2 and L3. ESP, European spine phantom; CNR, contrast-to-noise ratio.
Discussion
Osteoporosis often occurs in the elderly and in postmenopausal middle-aged women, with over 60% incidence in elderly patients over the age of 60 (5). Primary manifestations include fractures, low back pain and loss of viability. DXA and QCT are the most commonly used examination methods for osteoporosis detection. DXA is a two-dimensional area density measurement and is more affected by patients’ position. Along with popularized CT examination, QCT is getting more common for BMD for its sensitivity, accuracy, repeatability and small impact by bone volume (6). Compared to DXA, QCT also exhibited shortage of large radiation dose in BMD measurement. Therefore, research on low-dose scanning without affecting BMD accuracy has become QCT focus in clinical popularization. In the premise of meeting the image quality need in clinical diagnosis, researches have focused on reducing subject’s radiation dose, or in the case when radiation dose could not be reduced, maximizing diagnostic imaging information to maximize the value of radiation dose (7,8). According to the principle of As Low As Reasonably Achievable (ALARA), the choice of CTDIvol needs to be made after comprehensive analysis of clinical diagnosis purposes and image quality requirements. Excessively high CTDIvol means over suppression in CT sectional imaging noise level. In this case, radiation dose needs to be increased for better image quality; Over large DLP means over large scanning range, which could result in significant increase in total scan length. Niu et al. (9) reported that CTDIvol of lumbar spine was 25 mGy, which is lower than 35 mGy provided by organizations such as IAEA, and is much lower than 70 mGy in EC vertebral trauma. In the present study, the ideal low mAs could be 20 mAs, corresponding to CTDIvol 1.4, with significantly reduced dose. Such mAs could meet BMD measurement needs in clinical diagnosis. The radiation dose in this ESP study was positively related to tube current, indicating that under the circumstance of unchanged tube voltage, reducing tube current could reduce radiation dose in BMD measurement, which is consistent with the study conducted by Hu et al. (10).
During low mAs scanning, image noise increased obviously, image quality decreased significantly, especially in spine. How to greatly decrease radiation dose exposed to patients, and at the same time meeting clinical diagnostic need, has become research focus. Different from traditional FBP algorithms, different iterative reconstructions use matrix algebra to selectively identify and remove image noise through a mathematical model that improves low-density resolution by reducing image noise. iDose4 is the 4th generation algorithm that combines both FBP and iterative reconstruction. There are 7 levels involved in iDose4 processing (6 levels were involved in the present study) (11). IMR is the latest iterative algorithms, which does not contain FBP reconstruction. The IMR showed significant noise reduction effect in low-dose CT, and can significantly increase CNR, thus ensuring high image quality in low dose conditions (12). In this study, it was found during the ESP scanning that lower BMD varied greatly in FBP and less varied in IMR [2]. Normal BMD varied greatly in FBP, and less varied at different IMR levels, with most significant BMD found in IMR [2]. After using different iterative reconstructions, CNRs of L1, L2 and L3 in each group all showed the same trend as: FBP < iDose4 [1] < iDose4 [2] < iDose4 [3] < iDose4 [4] < iDose4 [5] < iDose4 [6] < IMR [1] < IMR [2] < IMR [3]. Under different mAs and different iterative reconstructions, without impacting BMD accuracy (considering the BMD variability), low mAs combined IMR [2] reconstruction approach could be adopted in clinical patient scan.
Chen et al. (3) reported that QPC of lower BMD correlated to higher precision deviation and worse repeatability. Adams et al. (2) reported that cancellous dominated site varied more in BMD than in cortical bone dominated site, which was consistent with results in the present study. We demonstrated that maximum deviation for accuracy was 11% in L1, 4% in L2 and 6% in L3. The accuracy deviation of QCT on ESP were all within the previously reported range of 4–15% (13,14), meeting clinical BMD measurement needs.
Limitations of this study
The study did not compare data with the DXA model; ESP is surrounded with water. Without simulation of human body CT density, the subjective image could not be scored, which also gives us a prospective incentive for future human body phantom reference.
In summary, it is recommended to use 120 kV, 20 mAs combined with IMR [2] reconstruction method in repeat BMD measurement of ESP multicenter QCT, which could accurately measure QCT, significantly reduce radiation dose without affecting the BMD accuracy. Such scanning method could also be applied to other CT manufactures.
Acknowledgements
Funding: This study was supported by the grants from the National Nature Science Foundation of China (U1504821).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Osteoporosis: review of the evidence for prevention, diagnosis and treatment and cost-effectiveness analysis. Executive summary. Osteoporos Int 1998;8 Suppl 4:S3-6. [PubMed] [Google Scholar]
- 2.Adams JE. Quantitative computed tomography. Eur J Radiol 2009;71:415-24. 10.1016/j.ejrad.2009.04.074 [DOI] [PubMed] [Google Scholar]
- 3.Chen X, Cheng X, Peng J, Li B, Su J, Dai C. Assessment of Precision and Accuracy of Spinal QCT in a Multi-centre Clinical Research with a European Spine Phantom. Chinese Journal of Medical Imagine 2011;19:912-7. [Google Scholar]
- 4.Kalender WA, Felsenberg D, Genant HK, Fischer M, Dequeker J, Reeve J. The European Spine Phantom--a tool for standardization and quality control in spinal bone mineral measurements by DXA and QCT. Eur J Radiol 1995;20:83-92. 10.1016/0720-048X(95)00631-Y [DOI] [PubMed] [Google Scholar]
- 5.Liang CG, Zhang GN, Wang J, Tang XZ, Chen HJ, Yu RH. An epidemiological investigation of patients with hip fracture over 50 years old in Changning district. Chin J Bone Joint Injury 2013;28:1122-4. [Google Scholar]
- 6.Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein ML, Felsenberg D, Ito M, Prevrhal S, Hans DB, Lewiecki EM. Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: the 2007 ISCD Official Positions. J Clin Densitom 2008;11:123-62. 10.1016/j.jocd.2007.12.010 [DOI] [PubMed] [Google Scholar]
- 7.Mulkens TH, Marchal P, Daineffe S, Salgado R, Bellinck P, te Rijdt B, Kegelaers B, Termote JL. Comparison of low-dose with standard-dose multidetector CT in cervical spine trauma. AJNR Am J Neuroradiol 2007;28:1444-50. 10.3174/ajnr.A0608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cody DD, Moxley DM, Krugh KT, O'Daniel JC, Wagner LK, Eftekhari F. Strategies for formulating appropriate MDCT techniques when imaging the chest, abdomen, and pelvis in pediatric patients. AJR Am J Roentgenol 2004;182:849-59. 10.2214/ajr.182.4.1820849 [DOI] [PubMed] [Google Scholar]
- 9.Niu Y, Zhang Y, Kang T, Xian J. Investigation of radiation dose and diagnostic reference levels in CT scanning for adult patients. Chinese Journal of Radiological Medicine and Protection 2016;36:862-7. [Google Scholar]
- 10.Hu M, Zhao X, Song J, Zhao H. Preliminary study of the optimization of abdominal CT scanning parameters on 64-slice spiral CT. Chinese Journal of Radiology 2011;45:264-9. [Google Scholar]
- 11.Funama Y, Taguchi K, Utsunomiya D, Oda S, Yanaga Y, Yamashita Y, Awai K. Combination of a low-tube-voltage technique with hybrid iterative reconstruction (iDose) algorithm at coronary computed tomographic angiography. J Comput Assist Tomogr 2011;35:480-5. 10.1097/RCT.0b013e31821fee94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang W, Lee JM, Lee K, Yoon JH, Yu MH, Han JK, Choi BI. Assessment of a model-based, iterative reconstruction algorithm (MBIR) regarding image quality and dose reduction in liver computed tomography. Invest Radiol 2013;48:598-606. 10.1097/RLI.0b013e3182899104 [DOI] [PubMed] [Google Scholar]
- 13.Glüer CC, Engelke K, Lang TF, Grampp S, Genant HK. Quantitative computed tomography (QCT) of the lumbar spine and appendicular skeleton. Eur J Radiol 1995;20:173-8. 10.1016/0720-048X(95)00651-6 [DOI] [PubMed] [Google Scholar]
- 14.Guglielmi G, Gluer CC, Majumdar S, Blunt BA, Genant HK. Current methods and advances in bone densitometry. Eur Radiol 1995;5:129-39. 10.1007/BF00957107 [DOI] [PubMed] [Google Scholar]