Abstract
Objective
To describe how a community-academic partnership between Taller Salud Inc., a community-based organization, and the Puerto Rico Community Cancer Control Outreach Program of the University of Puerto Rico was crucial in the adaptation and implementation of Cultivando La Salud (CLS), an evidence-based educational outreach program designed to increase breast and cervical cancer screening among Hispanic women living in Puerto Rico. This collaboration facilitated the review and adaptation of the CLS intervention to improve cultural appropriateness, relevance, and acceptability for Puerto Rican women.
Methods
A total of 25 interviewers and 12 Lay Health Workers (LHWs) were recruited and trained to deliver the program. The interviewers recruited women who were non-adherent to recommended screening guidelines for both breast and cervical cancer. LHWs then provided one-on-one education using the adapted CLS materials.
Results
A total of 444 women were recruited and 48% of them were educated through this collaborative effort.
Conclusions
Our main accomplishment was establishing the academic-community partnership to implement the CLS program. Nevertheless, in order to promote better collaborations with our community partners, it is important to carefully delineate and establish clear roles and shared responsibilities for each partner for the successful execution of research activities, taking into consideration the community’s needs.
Indexing Terms: Lay Health Worker (LHW), evidence-based intervention, community-based participatory research (CBPR), Puerto Rico, Breast and Cervical Cancer
INTRODUCTION
Despite the advances in cancer screening and treatment, breast and cervical cancer remain a public health problem for Puerto Rican women. Breast canceris the most prevalent cancer in Puerto Rico (PR)and accounts for 29.8% of all female cancers and 18.1% of all female cancer deaths [1]. Most recent data available from the PR Central Cancer Registry indicates that between 2008 and 2012, 9,855 new breast cancer cases were reported [1]. The incidence rate of invasive breast cancer among females in PR increased significantly by an average of 1.5% each year during 1987–2012, while the mortality rates decreased at a significant rate by an average of 0.1% during 1987–2012 [1]. In addition, cervical cancer is the seventh most commonly diagnosed cancer in Puerto Rican women and represents 3.9% of all female cancer diagnoses and 2.3% of cancer deaths in women [1]. From 1987 to 2004, the incidence in cervical cancer showed a decrease while, for 2004 to 2011 the incidence trends increased significantly [conference abstract]. Racial and ethnic disparities have also been reported when comparing the incidence of cervical cancer with other racial/ethnic groups in the United States of America (US), in which higher incidence rates are observed for PR women than for US non-Hispanics whites [2].
Furthermore, during 1996, 59.7% of Puerto Rican women aged 40+ had a mammogram within the past two years [3]. This percent increased to 77.5% in 2012 [3], which is higher in comparison to US women in general (74.0%) and US Hispanic women (69.0%). Despite this, recent estimates are still lower than the 81.1% target established by Healthy People 2020 [4]. Data from the BRFSS 2012 for Pap test screening reports that 71.0% of Puerto Rican women aged 18 or more had a Pap test in the past three years [3]. Poor adherence to screening can result in later stages of diagnosis of cervical cancer and increased morbidity and mortality. In fact, 50% of cervical cancer cases occur in females who never had a Pap test until they developed cervical cancer and an additional 10% of cases occur in females who have not been screened in the previous 5 years [5]. For breast cancer, the vast majority of deaths due to this cancer (71%) occur among women not regularly screened with mammography [6].
Community Based Participatory Research (CBPR) has been identified as a collaborative approach in creating interventions and prevention strategies to reduce health disparities [7]. Within cancer prevention, CBPR provides strategies for contextualizing interventions to promote external validity across diverse communities and incorporates cultural norms and community knowledge with evidence-based socio-behavioral theory for the implementation of comprehensive interventions [8]. CBPR generates opportunities and challenges for researchers and communities in addressing health disparities [9–11].
The Community Preventive Services Task Force recommends the use of one-on-one education on the basis of strong evidence of effectiveness in increasing screening for breast and cervical cancer [12]. One-on-one education has resulted in positive outcomes in cervical and breast screening behaviors in the Hispanic community [13] and other ethnicities living in the US [14–18]. An educational outreach program that proved to be effective at increasing breast and cervical screening among Hispanic women is Cultivando La Salud (CLS) [19]. This evidence-based program used principles of CBPR during the development throughout its dissemination to new settings.
Community-based interventions designed to increase behavioral screening practices for cancer prevention and control have been scarce. With the purpose of improving cancer prevention and control in Puerto Rico, we initiated a community-academic partnership between Taller Salud, Inc. (TS)-a feminist community-based organization- and the Puerto Rico Community Cancer Control Outreach Program (PRCCCOP). The PRCCCOP is one of the core programs of the University of Puerto Rico (UPR) and MD Anderson Cancer Center (MDACC) Partnership for Excellence in Cancer Research, funded by the National Cancer Institute.
In this article, we describe the process of building the collaboration, the implementation of the intervention and how this community-academic partnership was critical in the planning, delivery, and effectiveness of the intervention. Lessons learned and recommendations for future community-academic cancer prevention and control efforts are delineated. The Institutional Review Board of the UPR Medical Sciences Campus (A1250312) approved study protocol.
BUILDING PARTNERSHIPS
The PRCCCOP started as a pilot project in 2006 with the objective of identifying community-based organizations and agencies from the private and public sector for delineating and strengthened efforts for tobacco control in PR. The PRCCCOP evolved and created a network of community members and cancer control planners with the main goal of identifying and prioritizing cancer control issues in the community (e.g., access to breast cancer and Pap screening, HPV vaccination, tobacco cessation programs) and developing strategies to address those problems [20]. One of PRCCCOP early goals was to increase breast and cervical cancer screening and evaluate whether a minimally adapted evidence-based intervention could increase screening. With added collaboration from the Office of Community Research & Engagement (OCRE) of the Puerto Rico Clinical and Translational Research Consortium at the UPR Medical Sciences Campus, we formed an alliance with TS based on the common interest in women’s health and an identified high-need service area: Canóvanas (Figure 1). Canóvanas is a municipality of PR located in the northeastern region with a high incidence and mortality from breast cancer (91.2 and 21.3 per 100,000 women, respectively) and moderate incidence of cervical cancer (11.7 per 100,000 women) [1].
Figure 1.
Puerto Rico and Canóvanas Municipality geographical areas
Source: U.S. Census Bureau. 2000 Census of Population and Housing. [Population and Housing Unit Counts PHC-3–53, Puerto Rico Web site]. Washington, 2003. Retrieved from: http://www.census.gov/prod/cen2000/phc-3-53-sp.pdf28
TS works for the well-being of girls, young and adult women, primarily focusing on low-income communities [21] (at Loiza and other several municipalities at the northeastern region) to provide women with greater knowledge and empowerment about their health and well-being. TS had previous experience delivering health education interventions using Lay Health Workers (LHWs). Meetings with TS also identified Canóvanasas a municipality in need.
CULTIVANDO LA SALUD
Because of limited funds to develop a new program and after conducting qualitative studies to better understand factors influencing breast and cervical cancer in PR, we collectively decided to implement in Puerto Rico Cultivando la Salud (CLS). This program was originally developed by the National Center for Farmworker Health (located in Buda, Texas) with a focus on low-income Hispanic women living in the US (on the US-Mexico border and California). The program was designed to be delivered by LHWs conducting one-on-one or group education with women in the community. In the original intervention trial, CLS was found to be effective in increasing breast and cervical cancer screening among women over 50 years of age [19]. The program was updated and adapted to be appropriate for women and was implemented in Hays County and Houston, Texas. The program was again effective in significantly increasing breast and cervical cancer screening in these populations [19, 22–23]. Intervention mapping (IM), a planning process for development of theory and evidence-informed program, was used to develop the original program and was also used to guide adaptation decisions for the PR pilot intervention [24].
ADAPTING THEINTERVENTION
In collaboration with research partners, we used IM in the following way: first, through a series of focus groups, we sought to clearly understand the factors influencing breast and cervical cancer screening in our priority population of low income Puerto Rican women. We then created a logic model of change indicating what behaviors and environmental conditions influence breast and cervical cancer screening in PR and what determinants were the most salient. We compared the model to the original program, noted differences, and made adaptation decisions, such as language acculturation of educational materials [24].
We compared the specific behaviors required for screening, the environmental conditions that influence screening, and the psychosocial determinants of screening of the original program with the logic model of change we had developed for our new population and setting. Focus group findings indicated that many of the psychosocial factors influencing breast and cervical cancer screening among Puerto Rican women were similar to those addressed in the original CLS program. However, access factors were different since almost all of our Puerto Rican population (91.7%) had health care coverage [25]. Upon evaluation, we determined that only a minimal adaptation of the program content would be required since the actions that individuals needed to take and the determinants influencing breast and cervical cancer screening were very similar. Consequently, the recommended CLS intervention for Canóvanasconsisted of the following elements: 1) LHW training curriculum to prepare LHWs for implementation, 2) Flipchart for one-on-one education, 3) a breast model to facilitate LHWs discussion of “breast health awareness”, including noticing breast changes and emphasizing the importance of mammography, and 4) an information sheet about local providers delivering low-cost or free breast and cervical cancer screening services.
TRAINING AND PREPAREDNESS OF LHWs
The active participation of our community partner was fundamental in the delivery of the training of the LHWs. Initially, TS recruited four LHWs (all women) to deliver educational sessions focusing on increasing breast and cervical cancer screening practices among non-adherent women. LHWs attended a two-day training session offered by the National Center for Farmworker Health on the role of LHW, strategies for reaching women, breast and cervical cancer epidemiology and screening, teaching methods, and practices sessions. A Train the Trainer session was provided to facilitate reinforcement of CLS and/or train new LHWs. The LHWs model is based on health education in which respected community members educate peers in a culturally appropriate manner [24]. For this training most of LHWs were not residents of Canóvanas (lived in the surrounding municipalities) but were trained to approach and deliver program following LHWs model.
STUDY PROTOCOL
Women recruited were randomly assigned to a study group (intervention or control), and then interviewed. Women in the intervention group received an individualized educational intervention visit and a follow-up interview approximately 4 months after the program. Meanwhile, the women in the control group were interviewed at baseline and at follow-up 4 months after being recruited. CLS was conducted from 2012–2014.
RECRUITING
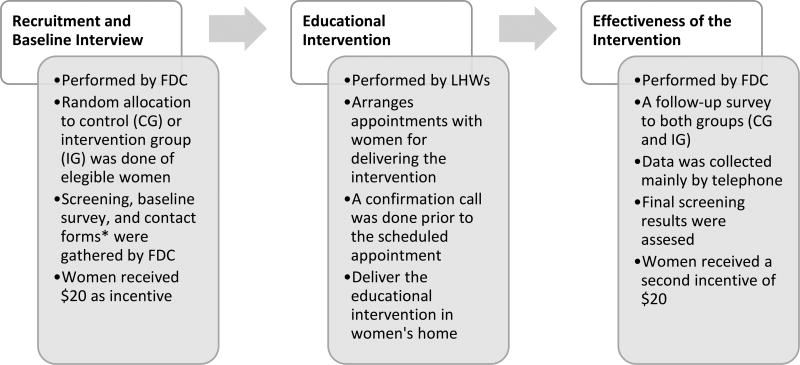
All collaborators assisted in recruitment and delivery of educational intervention. The academic and community research staff included a study coordinator, field data collectors (FDCs), and LHWs. FDCs recruited participants for this program who were: (a) women 21+years old with no Pap test in the last 3 years, or (b) women 40+years old who had not had a mammogram in the previous 12 months, (c) no current or previous cancer diagnosis, (d) no hysterectomy history, and (e) not pregnant. FDCs used screening forms to gather inclusion criteria and identified potential candidates. After inclusion criteria were confirmed, FDCs informed eligible participants of the study purpose, procedures, benefits, risks and incentives. The procedure consisted of an informed consent, a baseline interview, an educational session and a follow-up interview. LHWs contacted women to set up a face-to-face session at the participant’s home. Each educational session lasted between 45–90 minutes (Figure 2).
Figure 2.
Process flow of the Intervention using LHWs to encourage breast and cervical cancer screening in Puerto Rico
*Contact forms were given to LWHs to contact women assigned to the IG.
DELIVERING “CULTIVANDO LA SALUD”
The educational sessions for the intervention group consisted of an individualized presentation and discussion of educational material using CLS flipchart and breast model, if applicable. The CLS flipchart allowed LHWs cover the following topics: cancer, breast/cervical cancer, risk factors, early cancer detection relevancy and HPV vaccination, mammography/Pap test, clinical breast exam, and communication with physician. The flipchart included testimonials of women who underwent breast/cervical cancer screening and to identify and address barriers against screening test. LHWs delivered sessions according to non-adherence cancer screening status of the women (women who were non-adherent for both mammography and Pap test screening received both). At the end of each session, LHWs provided women with information about local low–cost or free breast and cervical cancer screening services.
OUR EFFORT IN THE FIELD
Our efforts resulted in a total of 3,665 households visited and 2,019 women were approached. Overall, after screening evaluations were performed, 501 (25%) were eligible women. Most eligible women (444, 89%) were enrolled and interviewed as part of the baseline survey. Of those, 177 (40%) were non-adherent to breast cancer screening, 142 (32%) non-adherent to cervical cancer, and 125 (28%) were non-adherent to both cancer screening tests recommendations. Overall, respondents had a mean age of 49.9 years (SD = 14.1), and had health care coverage (90.5%). Forty eight percent reported having >12 years of education; 58.3% were married or living together, and 30.2% had an annual family income of ≥$15,000 (Table 1).
Table 1.
Demographic characteristics of study participants.
| Frequency | Percent | |
|---|---|---|
| Age (years) | ||
| 21–29 | 38 | 8.6 |
| 30–39 | 63 | 14.2 |
| 40–49 | 123 | 27.7 |
| 50–59 | 108 | 24.3 |
| ≥ 60 | 112 | 25.2 |
| Age (mean ± SD) 49.88 ± 14.07 | ||
| Education (years)* | ||
| ≤ 12 | 230 | 52.0 |
| > 12 | 213 | 48.0 |
| Marital status | ||
| Never married | 82 | 18.5 |
| Married or living together | 259 | 58.3 |
| Divorced or separated | 63 | 14.2 |
| Widowed | 40 | 9.0 |
| Income* | ||
| < $15,000 | 293 | 69.8 |
| ≥ $15,000 | 127 | 30.2 |
| Health insurance coverage* | ||
| Private | 182 | 41.3 |
| Public | 217 | 49.2 |
| None | 42 | 9.5 |
Counts differed due to missing values.
CHALLENGES
We encountered a series of challenges in the implementation of the CLS educational intervention. The most salient challenges were: a) LHW turnover, b) neighborhood identification and access, and c) higher than planned efforts to contact participants.
LHW turnover
We faced a high LHW turnover during the intervention delivery period from August 2012 to October 2013. A total of 14 LHWs were trained to deliver intervention, with an average of 4 active LHWs at a time. We had a 4-month period with no LHWs. PRCCCOP members assisted in the delivery of the intervention. LHWs had different backgrounds: undergraduate (6) and graduate (3) students, healthcare professionals, (3) and community health workers (2); eight of them were from TS and the rest were members of PRCCCOP.
Neighborhood identification and access
Canóvanas’ geographic area itself presented a challenge. This area had hard-to-access areas as well as streets lacking identification or newly assigned names, making the task of reaching homes very challenging and the recruitment became very intense and time consuming. Nonetheless, we used technology tools (e.g. Google Earth/Maps), which contributed to the achievement of the task.
Efforts to contact participants
TS and PRCCCOP carried out intensive efforts to implement the intervention and follow-ups. Several contact tactics were implemented to reach participants since some women had moved, changed or disconnected their phones or did not call back. Primary contact consisted of LHWs coordinating a home visit with participants via phone calls. If women could not be reached, second contact attempts included home visits to locate women and arrange an appointment. If participants were not home, LHWs left postcards that included LHWs Coordinator and/or LHWs telephone number for rescheduling. LHWs completed at least three home visits at different days and hours for those unreachable participants.
ACCEPTABILITY OF THE INTERVENTION
Because the program was an adapted intervention, we assessed acceptability of the intervention at follow-up. The vast majority of participants reported that the intervention was helpful (94% among women needing Pap test and 96% among women needing mammography). Additionally,84% of the mammography and 90% of the Pap cohorts indicated that the element they liked the most was the conversation with the LHWs at the educational session.
Participants were also asked to indicate the information (or topics) discussed during the intervention by the LHWs. Participants reported receiving information about cancer (82%–90%), mammography (63%), breast self-exam (46%), and Pap test (74%).
LESSONS LEARNED
This collaborative effort for the implementation of a LHW program was successful and addressed priorities identified by CBPR process. Nevertheless, it was not without challenges. Although some specific principles of CBPR were not followed, since the program was only adapted to be appropriate for our community, an effort to understand how future efforts can include members from the community since the initial stages, among other topics were discussed in a round table discussion with all collaborators, community leaders and all staff. The main objectives of round table were to: (1) present the preliminary results of CLS, (2) discuss different phases of the study, (3) gather feedback, (4) obtain recommendations about future community studies, and (5) discuss challenges presented during the project.
During group discussions, several topics emerged. Regarding the educational materials, the group indicated that the flipchart’s images used did not represent the target community culture and which could affect participant’s identification with program models and influencing message processing. Another suggestion was hiring community leaders to facilitate the recruitment and ensure the success of initial research stages. Despite the effectiveness of the program in increasing Pap test screening, these observations indicate the preference for educational material that includes images and characters that resemble target population.
During the round table, the group also discussed that a Google Earth workshop should be included as part of the training curriculum. This would be important to include as part of the training prior to the field activities, because Canóvanas (as most rural municipalities in PR), have roads that are not identified or developed [26]. Also, one of the most significant challenges during this implementation was the frequent cancellation of appointments by study’s participants. This issue draws attention to improving timely implementation and diligence in follow-up in future projects. Finally, management turnover in both the academic-research and the community-based organization occurred during the same period, which affected the logistics of the project. Both events interrupted the continuous availability of personnel, adequate supervision and delivering of timely interventions to participants. In the field, LHW encountered difficulties to deliver educational sessions in scheduled time (it varied from a few weeks to up to 2 months). From the round table, all members strongly suggested that LHWs should be active members of the target community and an increase in compensation should be highly considered. This is a very important issue for future studies and budget preparation in order to decrease staff turnover and to maintain group effort in completing the interventions and the timeline established.
RECOMMENDATIONS FOR FUTURE COMMUNITY-ACADEMIC EFFORTS IN CANCER PREVENTION AND CONTROL
As presented, in this 45-month initiative (from the development of the focus groups in 2010to the completion of the program in 2014), developing a strong collaboration between academic and community partners is key to successfully executing behavioral interventions in the future. Overall, and following CBPR spirit [27–28], it is vitally important to include the community and the organization during early stages of the activity. Academic partners need to be sensitive and aware of the efforts of the community organizations in the field in other outreach activities and the limitations regarding small staff and limited budget. In order to promote better collaborations with our community partners, it is important to carefully delineate and establish clear roles and shared responsibilities for each partner. However, although most of these can be establisheda priori, the roles and shared responsibilities will keep evolving in response to the dynamics of the community and research. Understanding the community and the community leader’s expectations is critical during all phases of the research and it is the responsibility of the academic partners to carefully and regularly discuss the project with the community team.
In order to enhance the alliance to become meaningful and sustainable and to strengthen our research efforts[27–28], TS developed a workshop for academia and our clinical partners describing different strategies to maintain and strengthen participant recruitment in research studies. Future efforts to maintain and extend this workshop from the community partners are expected to continue with the ultimate goal of discussing and delineating future opportunities for cancer prevention and promotion and to inform future research and/or intervention proposal development.
In summary, this is PRCCCOP’s first effort in adapting an intervention aimed at increasing breast and cervical cancer screening in PR. This study helped build trust and engagement with the community. Future efforts in cancer prevention and behavioral intervention are expected in the island, given the documented cancer burden, primarily in cancers where screening tests are available and screening rates continue to be low.
Acknowledgments
Funding source: The project described was supported by National Cancer Institute/National Institute of Health (NCI/NIH) grant number U54CA096297/CA096300 for the University of Puerto Rico / MD Anderson Cancer Center, Partnership for Excellence in Cancer Research. This project was also supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under the Award number 2U54MD007587. W.A.C. was supported by NCI-sponsored pre- and postdoctoral cancer training programs R25CA057712 and R25CA116339. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
We wish to express our gratitude to our study participants and all the LHWs, FDCs and the undergraduate and graduate students from the UPR who participated as part of their community-based research experience. Finally, we thank Dr. Elba C. Díaz-Toro, Mrs. Mirza Rivera-Lugo, Ms. Lizbeth Medina-Cortés, Dr. Edna Acosta Pérez and Dr. Héctor Colón, all from the UPR Medical Sciences Campus, for their assistance in the adaptation and implementation of the CLS intervention.
Footnotes
The authors have no conflict of interest to disclose.
References
- 1.Zavala-Zegarra D, Tortolero-Luna G, Torres-Cintrón CR, et al. Cancer in Puerto Rico, 2008–2012. Puerto Rico Central Cancer Registry; San Juan, PR: 2015. [Google Scholar]
- 2.Torres-Cintrón M, Ortiz AP, Pérez-Irizarry J, et al. Incidence and mortality of the leading cancer types in Puerto Rico: 1987–2004. PR Health Sci J. 2010;29:317–329. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. [accessed Dec 07, 2015];BRFSS Prevalence & Trends Data. 2015 [Internet]. Available from: http://www.cdc.gov/brfss/brfssprevalence/
- 4.Healthy People 2020. Washington, DC: U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion; [accessed Dec 7, 2015]. [Internet]. Available from: http://www.healthypeople.gov/2020/topics-objectives/topic/cancer/objectives. [Google Scholar]
- 5.Saslow D, Lawson HW, Killackey M, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology Screening Guidelines for the Prevention and Early Detection of Cervical Cancer. J Low Genit Tract Dis. 2012;16:175–204. doi: 10.1097/LGT.0b013e31824ca9d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Webb ML, Cady B, Michaelson JS, et al. A failure analysis of invasive breast cancer: most deaths from disease occur in women not regularly screened. Cancer. 2014;120:2839–2846. doi: 10.1002/cncr.28199. [DOI] [PubMed] [Google Scholar]
- 7.Minkler M, Wallerstein . N’s Community-based participatory research for health. 2. San Francisco (CA): Jossey-Bass; 2008. p. 6. [Google Scholar]
- 8.Meade CD, Menard JM, Luque JS, Martinez-Tyson D, Gwede CK. Creating community-academic partnerships for cancer disparities research and health promotion. Health Promot Pract. 2011;12:456–462. doi: 10.1177/1524839909341035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Green BL, Rivers DA, Kumar N, et al. Establishing the Infrastructure to Comprehensively Address Cancer Disparities: A Model for Transdisciplinary Approaches. J Health Care Poor Underserved. 2013;24:1614–1623. doi: 10.1353/hpu.2013.0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Israel B, Schulz A, Parker E, Becker A. Review of community-based participatory research: Assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 11.Israel B, Krieger J, Vlahov D, et al. Challenges and facilitating factors in sustaining community-based participatory research partnerships: Lessons learned from the Detroit, New York City and Seattle urban research centers. J Urban Health. 2006;83:1022–1040. doi: 10.1007/s11524-006-9110-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sabatino SA, Lawrence B, Elder R, et al. Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for The Guide to Community Preventive Services. Am J Prev Med. 2012;43:765–786. doi: 10.1016/j.amepre.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 13.Nuño T, Martinez ME, Harris R, García F. A Promotora-administered group education intervention to promote breast and cervical cancer screening in a rural community along the U.S.-Mexico border: a randomized controlled trial. Cancer Causes Control. 2011;22:367–374. doi: 10.1007/s10552-010-9705-4. [DOI] [PubMed] [Google Scholar]
- 14.Thompson B, Vilchis H, Moran C, Copeland W, Holte S, Duggan C. Increasing cervical cancer screening in the United States-Mexico border region. J Rural Health. 2014;30:196–205. doi: 10.1111/jrh.12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Byrd TL, Wilson KM, Smith JL, et al. AMIGAS: A multicity, multicomponent cervical cancer prevention trial among Mexican American women. Cancer. 2013;119:1365–1372. doi: 10.1002/cncr.27926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Brien MJ, Halbert CH, Bixby R, Pimentel S, Shea JA. Community health worker intervention to decrease cervical cancer disparities in Hispanic women. J Gen Intern Med. 2010 Nov;25:1186–1192. doi: 10.1007/s11606-010-1434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nguyen TT, McPhee SJ, Bui-Tong N, et al. Community-based participatory research increases cervical cancer screening among Vietnamese-Americans. J Health Care Poor Underserved. 2006;17:31–54. doi: 10.1353/hpu.2006.0091. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen TT, Le G, Nguyen T, et al. Breast cancer screening among Vietnamese Americans: a randomized controlled trial of lay health worker outreach. Am J Prev Med. 2009;37:306–313. doi: 10.1016/j.amepre.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fernández ME, Gonzales A, Tortolero-Luna G, et al. Effectiveness of Cultivando la Salud: a breast and cervical cancer screening promotion program for low-income Hispanic women. Am J Public Health. 2009;99:936–943. doi: 10.2105/AJPH.2008.136713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Calo WA, Fernández ME, Rivera M, et al. Assessing Awareness and Use of Evidence-Based Programs for Cancer Control in Puerto Rico. J Cancer Education. 2012;27:486–493. doi: 10.1007/s13187-012-0348-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taller Salud, Inc. [accessed Apr 6, 2015];Reducción de Violencias. [Internet]. Available from: http://www.tallersalud.com/
- 22.Bartholomew LK, Parcel GS, Kok G, Gottlieb NH. Planning Health Promotion Programs: An Intervention Mapping Approach. 2. San Francisco: Jossey-Bass; 2006. [Google Scholar]
- 23.Fernández ME, Gonzales A, Tortolero-Luna G, Partida S, Bartholomew LK. Using Intervention Mapping to develop a breast and cervical cancer screening program for Hispanic farmworkers: Cultivando La Salud. Health Promot Pract. 2005;6:394–404. doi: 10.1177/1524839905278810. [DOI] [PubMed] [Google Scholar]
- 24.Bartholomew LK, Parcel GS, Kok G, Gottlieb NH, Fernández ME. Planning Health Promotion Programs: An Intervention Mapping Approach. 3. San Francisco: Jossey-Bass; 2011. [Google Scholar]
- 25.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. [accessed Dec 04, 2015];BRFSS Prevalence & Trends Data. 2015 [Internet]. Available from: https://nccd.cdc.gov/BRFSSPrevalence/rdPage.aspx?rdReport=DPH_BRFSS.ExploreByLocation&rdProcessAction=&SaveFileGenerated=1&irbLocationType=States&islLocation=72&islClass=CLASS07&islTopic=Topic29&islYear=2015&hidLocationType=States&hidLocation=72&hidClass=CLASS07&hidTopic=Topic29&hidTopicName=Health+Care+Coverage&hidYear=2015&irbShowFootnotes=Show&iclIndicators_rdExpandedCollapsedHistory=&iclIndicators=HLTHPLN1&hidPreviouslySelectedIndicators=&DashboardColumnCount=2&rdShowElementHistory=&rdScrollX=0&rdScrollY=171&rdRnd=28915.
- 26.Vázquez-Colón B. Tendrán su pedazo de tierra.Índice. Sect Ín News. 2014 Oct 23; Available from: http://www.indicepr.com/noticias/2014/10/23/news/29986/tendran-su-pedazo-de-tierra/29.
- 27.Israel B, Schulz A, Parker E, Becker A. Review of community-based participatory research: Assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 28.Israel B, Krieger J, Vlahov D, et al. Challenges and facilitating factors in sustaining community-based participatory research partnerships: Lessons learned from the Detroit, New York City and Seattle urban research centers. J Urban Health. 2006;83:1022–1040. doi: 10.1007/s11524-006-9110-1. [DOI] [PMC free article] [PubMed] [Google Scholar]