Abstract
To a great extent, research on geographic accessibility to mammography facilities has focused on urban–rural differences. Spatial accessibility within urban areas can nonetheless pose a challenge, especially for minorities and low-income urban residents who are more likely to depend on public transportation. To examine spatial and temporal accessibility to mammography facilities in the Atlanta metropolitan area by public and private transportation, we built a multimodal transportation network model including bus and rail routes, bus and rail stops, transfers, walk times, and wait times. Our analysis of travel times from the population-weighted centroids of the 282 census tracts in the 2-county area to the nearest facility found that the median public transportation time was almost 51 minutes. We further examined public transportation travel times by levels of household access to a private vehicle. Residents in tracts with the lowest household access to a private vehicle had the shortest travel times, suggesting that facilities were favorably located for women who have to use public transportation. However, census tracts with majority non-Hispanic black populations had the longest travel times for all levels of vehicle availability. Time to the nearest mammography facility would not pose a barrier to women who had access to a private vehicle. This study adds to the literature demonstrating differences in spatial accessibility to health services by race/ethnicity and socioeconomic characteristics. Ameliorating spatial inaccessibility represents an opportunity for intervention that operates at the population level.
Keywords: Breast cancer, Mammography, Geographic information systems (GIS), Social disadvantage, Healthcare access
Introduction
Screening by mammography is currently the most effective method of detecting early breast cancer and reducing breast cancer mortality with current estimates of the magnitude of mortality reduction ranging from 10 to 25%. [1–3] The most recent guidelines from the U.S. Preventive Services Task Force (USPSTF) recommend that women undergo biennial mammography screening beginning at age 50. Decisions to start screening at an earlier age should be made on an individual basis [4]. Earlier USPSTF recommendations and the current recommendations of the American Cancer Society, and the American College of Radiology, and the Society of Breast Imaging recommend annual mammography screening every 1 to 2 years beginning at age 40. [5–7]
Despite increases in mammography use over the past 2 decades, population-based surveys have consistently demonstrated that a substantial proportion of women were not up-to-date on screening [8, 9]. Factors associated with mammography utilization have been explored in a large number of studies and reviews that have focused on characteristics related to socioeconomic status and health systems that may be barriers to or facilitators of screening. Among the often-cited factors are income, insurance status, usual source of care, out-of-pocket expenses, client reminders, and recommendations for screening by health care providers [10–18].
Access to care has also been described in terms of number of services available and transportation to those services [19]. Mammography capacity, or the availability of machines, shows considerable geographic variability at the county level and has been shown to be an important factor in mammography usage and in late stage breast cancer diagnosis [20, 21]. Geographic accessibility is also commonly measured as distance to services. It is intuitively apparent that more sparsely populated locations may be at a spatial disadvantage with respect to access to medical care; and geographical distance as a barrier to breast cancer screening and treatment has been described for several rural areas [22–30]. In contrast with rural areas, distances to facilities in urban areas are shorter and multiple means of transportation are often available for residents. Spatial accessibility in urban areas can nonetheless pose a challenge, especially for historically disadvantaged populations that are more likely to depend on public transportation. For example, among black households in Atlanta, more than 15% do not have access to a private vehicle. Among whites, fewer than 4% do not have access to a private vehicle. [31]
Accessibility to mammography facilities in urban areas is receiving increasing attention in studies that have focused on disadvantaged populations. A study of the spatial distribution of Chicago’s low- or no-cost mammography screening facilities showed overall shorter travel time for low-income residents. However, longer travel time and distances were shown for low-income black neighborhoods than for other low-income neighborhoods [32]. A study in Los Angeles County showed that mammography use was higher in neighborhoods with a greater density of facilities [33]. Distance to mammography facilities was also associated with late-stage breast cancer diagnosis among Latinas in Los Angeles County and among blacks in segregated areas in Detroit, Michigan as defined by zip codes [34, 35]. A J-shaped curve for late-stage breast cancer risk was described for women in Illinois with the most highly urbanized area (Chicago) and most isolated rural areas having the highest risk [36].
Economic research has demonstrated a spatial mismatch between dispersed urban employment opportunities and residential locations that is exacerbated by public transportation systems that fail to connect these areas [37]. Our objective was to assess whether there is a comparable spatial mismatch between mammography facilities and women 40 years old and older who rely on public transportation in one major urban center, Atlanta. We further investigated whether spatial accessibility to mammography facilities differed by the proportion of non-Hispanic black and other minority residents in the census tracts. This was accomplished through the construction of a multi-modal transportation network that enabled us to calculate direct travel time and distance from all census tracts to the closest mammography facility in the Atlanta metropolitan area.
Methods
Overview
We used a geographic information system (GIS) and network analysis to quantify spatial and temporal accessibility to mammography facilities in the Atlanta metropolitan area. We built a multimodal transportation network model that included all bus and rail routes, bus and rail stops, and transfers and that provided for the capture of walk and wait times experienced by public transportation system travelers. Using this network, we then calculated travel time to mammography facilities using public and private transportation from a study-specific population-weighted center of all census tracts located within the 2-county area served by the Metropolitan Atlanta Rapid Transit Authority (MARTA). We also compared travel times and distances to all mammography facilities and to the Georgia Cancer Screening Program facilities which provide breast and cancer screening to uninsured and underinsured women. To highlight transportation barriers for those census tracts where the population was most likely to use public transportation, we broadly grouped the tracts by levels of household access to a private vehicle when calculating time and distance.
Data Sources
The following preexisting datasets were used for the analysis: U.S. Census data from 2000, Tele Atlas boundary files (Tele Atlas, Lebanon, New Hampshire), transportation network files from MARTA, locations of FDA certified mammography facilities, and locations of Georgia Cancer Screening Program facilities.
U.S. Census data from 2000 were used to identify women 40 years of age and older in each of the 282 census tracts of Fulton and DeKalb counties within the Atlanta metropolitan area serviced by MARTA. In addition, two variables available at the census tract level were used to classify census tracts. The first, vehicle access, is defined by the number of private vehicles (none vs. 1, 2, 3, 4, and 5 or more automobile, van, or small truck) available for use by members of a household. We dichotomized access to a private vehicle as none vs. 1 or more vehicles available to a household. The second is race. Race categories included non-Hispanic black (identified in the US Census as such, or as African American), non-Hispanic white, and all other races (Asian, American Indian and Alaska Native, Native Hawaiian and Pacific Islander and those noting 2 or more races). Ethnic variables are limited to Hispanic ethnicity as Hispanics can be of any race. This study focused primarily on non-Hispanic blacks and whites.
Tele Atlas data boundary files were used to identify uninhabited areas such as parks, shopping centers, industrial parks, and bodies of water at the census block level. These data, along with the number of women 40 years of age and older within each census block were used to locate a population-weighted centroid for each census tract.
Mammography screening facilities were identified from a regularly updated list of Food and Drug Administration (FDA) accredited facilities (http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfMQSA/mqsa.cfm). These facilities meet baseline quality standards for equipment, personnel, and practices under the Mammography Quality Standards Act of 1992 and the subsequent amendments of 1998 and 2004 in the Mammography Quality Standards Reauthorization Act. Mammography facility address information for the 47 facilities in Fulton and DeKalb counties obtained from FDA certified list for 2008 were successfully geocoded to the street address level of precision using Centrus geocoding software (Pitney Bowes Business Insight, Troy, New York). One facility offering only diagnostic mammography services and another facility providing access only to military families were excluded from analyses. The Georgia Cancer Screening Program provided names and addresses of 9 facilities to which their providers refer their patients. These facilities are a subset of all facilities in the study area.
Collaborations with MARTA provided an extensive route network containing all of the bus stops, bus routes, rail routes, and rail stops as of October 2008. MARTA runs hundreds of buses over 138 routes covering over 1,000 route-miles. The train system includes 59 miles of rail lines and 38 stations. The train network is largely limited to the intown portion of Atlanta with northern and southwestern Fulton County and southeastern DeKalb County being comparatively underserved.
Construction of the Private and Multimodal Public Transportation Network Models
The multimodal public transportation model was based on a spatial database provided by MARTA. The database contained many spatial layers, including streets, rail lines, rail stops, station entrances, bus routes, and bus stops. The private transportation model was based on the street-level layers provided by MARTA. Both public and private transportation models were built using ArcGIS Network Analyst® (ESRI, Redlands, California).
In an urban environment, the rate of travel depends on a number of factors including traffic volume, weather conditions, time of day, day of week, the number of commuters using the system, and individual driving and/or walking speeds. We did not attempt to model the significant variability encountered in day-to-day commutes. To simplify our model, we used constant rates of travel that varied only according to the mode of transportation:
Walking rate = 4.3 km per hour (2.7 miles per hour or 4 feet per second)
Bus rate = 24.2 km per hour (15 miles per hour)
Train rate = 48.3 km per hour (30 miles per hour)
Automobile rate = travel speeds were assigned to each road segment based on the TIGER/Line File Census Feature Class Codes for the road type[38].
The constants were chosen as a reasonable approximation of travel speeds during average conditions. The walking rate (4 feet per second) is based on the value used by the Manual of Uniform Traffic Control Devices[39]. Using bus travel estimates by the Transit Cooperative Research Program[40], we averaged bus speeds for central city, city and suburbs to arrive at 15 miles per hour. The train speed constant was based on MARTA’s published train schedules from which an average train speed for the two lines was calculated [41] (http://www.itsmarta.com/ne-nor.aspx).
For commuters using public transit, the time spent waiting for a bus or train is another factor influencing total trip time. Wait times for buses and trains vary depending on bus or train frequency (level of service) and, for buses, on traffic conditions. Again, we chose to incorporate wait times into the model as constant values approximating average wait times:
Wait time for bus = 16 minutes
Wait time for train = 6 minutes
These times are based on MARTA’s published bus and train schedules. We averaged the trip frequency time for hundreds of scheduled trips. Our constant wait time values represent approximately half the average trip frequency. This is the midpoint between a full wait time (just missing a bus or train) and no wait (boarding a bus or train immediately upon arrival).
Analysis and Mapping
A dasymetric mapping methodology was used to locate a population-weighted centroid for each census tract. Compared with using a simple geometric centroid which assumes an even population distribution, dasymetric mapping provides a more realistic representation of the actual distribution of the population within a census tract [42]. To accomplish this, ancillary data (From TeleAtlas, in this instance) were used to identify uninhabited areas such as parks, shopping centers, industrial parks and bodies of water. Block level counts of women 40 years of age and older were obtained from the US 2000 Census. The mean center algorithm provided with ArcGIS 9.3 software (ESRI, Redlands, California) was applied to locate the population-weighted centroid within each census tract. This centroid was calculated as an average of the x and y geometric center values of the zero-population areas and the census blocks within each tract using population counts as weights. Because zero population areas have no weight, and the inhabited blocks have varying size populations, the tract centroid was ‘pulled’ toward those blocks with the highest population counts.
Travel times and distances were modeled from the population-weighted centroids of each of the tracts to the closest mammography facility (by time) via both public transportation and private transportation. ArcGIS Network Analyst® evaluates models by selecting the minimal time or distance as travel pathways are traversed. Travel time was calculated by the formula T = L/R where T is the travel time through a line segment, L is the length of the line segment, and R is the rate of travel. Travel time was calculated for every line segment (bus, rail and walking) and stored as an attribute of that segment.
Thus, each census tract in the data set was associated with a travel time by public transportation and a travel time by private transportation. We first calculated summary measures of travel time (means, medians, and interquartile ranges) by levels of household access to a private vehicle categorized roughly into tertiles defined as: low vehicle access = more than 20% of the population had no access to a private vehicle, medium vehicle access = 5%–20% of the population had no access to a private vehicle, and high vehicle access = less than 5% of the population had no access to a private vehicle. We then stratified vehicle access travel times (means, medians, and interquartile ranges) by majority non-Hispanic white women, majority non-His-panic black women, and neither majority to illuminate potential disparities [43]. Majority was defined as ≥50%.
All summary travel time measures were calculated by weighting the travel time for each tract by the number of women 40 years of age and older in that tract. Rather than adding travel time for each tract and dividing by the number of tracts in a particular vehicle access category, we multiplied travel times by the number of women 40 years and older in each census tract, added these across the category, and divided by the total population of women 40 years and older in that category.
Results
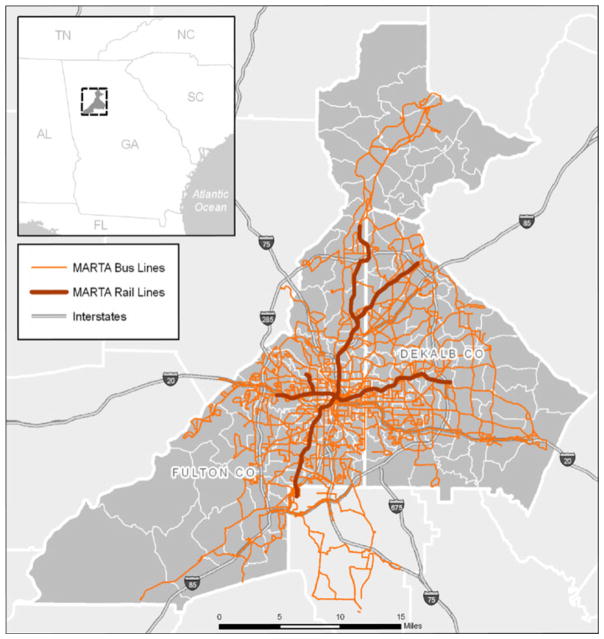
Figure 1 displays the transportation network for the Fulton-and DeKalb-county study area. The network includes the MARTA rail lines, bus lines, and interstate highways. As shown in this map, there are areas in northern and southwestern Fulton County and in eastern and southern DeKalb County that have limited or no public transportation services compared to the well-serviced central city areas.
Fig. 1.
Transportation network, Fulton and DeKalb counties
Table 1 presents a description of the 282 census tracts in Fulton and DeKalb counties. Across all census tracts, the median public transportation travel time to the nearest mammography facility was almost 51 minutes and to the nearest Georgia Cancer Screening Program facility was 68 minutes. By car, the travel times were approximately 6 minutes and 8 minutes, respectively. The distances to the nearest mammography facility were similar regardless of whether women travelled by car or by public transportation. On average, 12% of households in this 2-county area had no access to a private vehicle and more than 27% were below the 200% poverty level. There was a strong correlation (r = 0.91) between lack of access to a private vehicle and poverty.
Table 1.
Descriptive statistics of Atlanta (Fulton and DeKalb counties) census tracts (n = 282)
| Mean | Median | Minimum | Maximum | |
|---|---|---|---|---|
| Percentage of residents below 100% poverty level | 17.5% | 12.3% | 0.0% | 75.7% |
| Percentage of residents below 200% poverty level | 27.4% | 21.9% | 0.0% | 92.9% |
| Percentage of residents with no vehicle access | 12.2% | 7.5% | 0.0% | 80.2% |
| Percentage of non-Hispanic black residents | 53.5% | 66.1% | 0.1% | 100.0% |
| Percentage of white residents | 35.8% | 19.8% | 0.0% | 95.7% |
| Percentage of Hispanic residents | 5.9% | 2.7% | 0.0% | 71.2% |
| Percentage of other race residents | 4.8% | 3.1% | 0.0% | 25.6% |
| Public transportation time to nearest facility (minutes) | 55.4 | 50.6 | 6.3 | 205.6 |
| Public transportation time to nearest Georgia Cancer | ||||
| Screening Program facility (minutes) | 75.4 | 68.2 | 6.3 | 205.6 |
| Private transportation time to nearest facility (minutes) | 6.6 | 6.0 | 0.1 | 28.0 |
| Private transportation time to nearest Georgia Cancer Screening Program facility (minutes) | 9.9 | 8.3 | 0.7 | 28.5 |
| Public transportation distance to nearest facility (miles) | 4.6 | 4.0 | 0.3 | 19.2 |
| Public transportation distance to nearest Georgia Cancer Screening Program facility (miles) | 6.8 | 5.6 | 0.3 | 20.2 |
| Private transportation distance to nearest facility (miles) | 4.1 | 3.6 | 0.1 | 21.3 |
| Private transportation distance to nearest Georgia Cancer Screening facility (miles) | 5.2 | 4.3 | 0.3 | 15.3 |
Table 2 shows that as the proportion of the population with access to a private vehicle increases, travel time increases. Median public transportation travel times for areas with high vehicle access were 60% longer than areas with low vehicle access. Median public transportation travel times to GA CSP facilities were 8, 15, and 38 minutes longer across low, medium, and high vehicle access categories. Private transportation travel time to the nearest Georgia Cancer Screening Program facilities also increased as access to a private vehicle increased. We further stratified vehicle access by race/ethnicity. One hundred and fifteen tracts were classified as majority non-Hispanic white (≥50% white); 154 tracts were majority black (≥50% non-Hispanic black). Only 13 of the 282 census tracts (5%) in Fulton and DeKalb counties could not be classified as majority white or majority black and of those, only 3 tracts were majority Hispanic. We present only travel times for census tracts with majority black and majority white women 40 years of age and older.
Table 2.
Public and private transportation times to the nearest mammography facility for Fulton and DeKalb counties by household availability of a private vehicle
| Mean | Median | 25% | 75% | |
|---|---|---|---|---|
| All access categories | ||||
| Public transportation time | 55.4 | 50.6 | 36.2 | 67.7 |
| Private transportation time | 6.6 | 6.0 | 4.2 | 8.4 |
| Georgia Cancer Screening Program public transportation time | 75.4 | 68.2 | 47.2 | 98.0 |
| Georgia Cancer Screening Program private transportation time | 9.9 | 8.3 | 5.5 | 13.5 |
| Low vehicle access (NVA > 20%) | ||||
| Public transportation time | 39.1 | 38.8 | 26.6 | 49.3 |
| Private transportation time | 5.0 | 5.2 | 3.5 | 6.3 |
| Georgia Cancer Screening Program public transportation time | 44.9 | 47.2 | 33.2 | 53.8 |
| Georgia Cancer Screening Program private transportation time | 5.5 | 5.4 | 4.2 | 7.0 |
| Medium vehicle access (NVA 5–20%) | ||||
| Public transportation time | 51.9 | 48.4 | 35.6 | 65.3 |
| Private transportation time | 6.6 | 5.9 | 3.6 | 8.1 |
| Georgia Cancer Screening Program public transportation time | 64.6 | 63.6 | 43.8 | 83.5 |
| Georgia Cancer Screening Program private transportation time | 8.7 | 8.1 | 5.3 | 10.6 |
| High vehicle access (NVA < 5%) | ||||
| Public transportation time | 69.6 | 63.9 | 48.8 | 86.1 |
| Private transportation time | 7.5 | 6.6 | 5.4 | 9.5 |
| Georgia Cancer Screening Program public transportation time | 108.1 | 101.9 | 80.6 | 128.4 |
| Georgia Cancer Screening Program private transportation time | 14.1 | 14.1 | 8.6 | 18.4 |
NVA No vehicle access
The same pattern of increasing travel time with increasing vehicle access holds for whites and blacks (Table 3). As vehicle availability decreased, median transportation travel time to the nearest facility decreased. However, for every category of vehicle access, whites had the shortest travel time to any mammography facility. This was also true for travel times to the Georgia Cancer Screening Program facilities, except for the category of high vehicle access where white majority tracts had a slightly longer median travel time (104.6 vs. 98.0 minutes). For the low vehicle access tracts, median public transportation trip times from majority black census tracts were 3 times those of whites. However, there were very few tracts that were majority white with low vehicle availability (n = 2). Private transportation time to the nearest facility ranged from under 1 minute to just over 15 minutes (in 1 of these tracts, the centroid of the tract was adjacent to the facility). For all categories of vehicle access, travel time by private vehicle increased with increasing access. Also, as with public transportation travel time, blacks experienced longer private transportation time across the 3 categories of vehicle access. The differences between public transportation times to the nearest facility compared to public transportation times to the nearest Georgia Cancer Screening Program facility were shortest for the tracts with lowest vehicle access and for tracts that were majority black when compared with majority white. Median public transportation travel times in the 13 census tracts having no majority population typically fell between travel times of the majority black and majority white tracts. Almost all of these tracts (12 out of 13) had low or medium vehicle access. Only 1 tract had high vehicle access.
Table 3.
Public and private transportation time to mammography facilities by household availability of a private vehicle and by race/ethnicity, Fulton and DeKalb counties
| # Tracts | Majority black women 40 years of age and older | # Tracts | Majority white women 40 years of age and older | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Mean | Median | 25% | 75% | Mean | Median | 25% | 75% | |||
| Public transportation time (minutes) | 154 | 115 | ||||||||
| Low vehicle access (NVA > 20%) | 80 | 39.4 | 39.5 | 26.6 | 49.3 | 2 | 18.5 | 13.1 | 13.1 | 31.9 |
| Medium vehicle access (NVA 5–20%) | 56 | 60.5 | 57.6 | 48.4 | 71.6 | 62 | 43.6 | 38.7 | 29.1 | 49.5 |
| High vehicle access (NVA < 5%) | 18 | 80.0 | 70.2 | 59.4 | 94.5 | 51 | 66.3 | 59.0 | 45.2 | 76.3 |
| Georgia Cancer Screening Program public transportation time (minutes) | 154 | 115 | ||||||||
| Low vehicle access (NVA > 20%) | 80 | 45.1 | 47.2 | 34.6 | 53.8 | 2 | 34.6 | 35.7 | 31.9 | 35.7 |
| Medium vehicle access (NVA 5–20%) | 56 | 70.4 | 69.8 | 50.6 | 87.9 | 62 | 59.0 | 53.2 | 39.6 | 76.1 |
| High vehicle access (NVA < 5%) | 18 | 106.9 | 98.0 | 86.2 | 131.5 | 51 | 108.5 | 104.6 | 74.4 | 128.4 |
| Private transportation time (minutes) | 154 | 115 | ||||||||
| Low vehicle access (NVA > 20%) | 80 | 5.1 | 5.4 | 3.5 | 6.4 | 2 | 1.5 | 0.8 | 0.8 | 3.1 |
| Medium vehicle access (NVA 5–20%) | 56 | 7.8 | 7.6 | 5.5 | 9.2 | 62 | 5.5 | 4.7 | 3.0 | 6.5 |
| High vehicle access (NVA < 5%) | 18 | 9.5 | 9.5 | 8.0 | 10.2 | 51 | 6.9 | 6.2 | 4.9 | 8.9 |
| Georgia Cancer Screening Program private transportation time (minutes) | 154 | 115 | ||||||||
| Low vehicle access (NVA > 20%) | 80 | 5.5 | 5.4 | 3.9 | 7.0 | 2 | 4.7 | 5.3 | 3.1 | 5.3 |
| Medium vehicle access (NVA 5–20%) | 56 | 10.1 | 9.9 | 6.4 | 13.4 | 62 | 7.5 | 6.5 | 4.3 | 9.6 |
| High vehicle access (NVA < 5%) | 18 | 15.3 | 15.2 | 13.2 | 18.4 | 51 | 13.8 | 13.5 | 7.1 | 20.0 |
NVA No vehicle access
Discussion and Conclusions
Overall, our analysis found that the median public transportation time to the nearest mammography facility in the 2-county study area is almost 51 minutes. This compares with 23 minutes average travel time by public transportation in Chicago, Illinois. [32] Inasmuch as Chicago is both smaller in area and more densely populated, this is not an unexpected finding. We found that as private transportation availability decreased, time to facilities decreased, and residents in the tracts with lowest access to a private vehicle had the shortest travel times. This demonstrated that, in general, facilities are advantageously located for women who have to use public transportation. However, census tracts with majority African American populations had the longest travel times for all levels of vehicle availability. Despite the differences in area and population density between Chicago and Atlanta, and the use of vehicle access to classify census tracts, these findings corroborate those of Zenk et al. (2006) who demonstrated longer public transportation times and distances to mammography facilities for black neighborhoods than for neighborhoods with proportionately fewer black residents. We also found that time to the nearest mammography facility did not appear to pose a barrier to women who had access to a private vehicle. Median travel times ranged from less than 5 minutes to just over 15 minutes by car (Table 3). However, as with public transportation time, private transportation times were longer for tracts with majority black women. Atlanta illustrates many of the urban planning challenges encountered in U.S. metropolitan areas. Atlanta is the 8th largest and the 2nd fastest growing metropolitan area in the U.S. since 2000. [44]
Some limitations are important to mention. Estimating transportation times required a number of assumptions that may not be generalizable to all times and all days. We calculated average and median travel times not accounting for rush hour or other delays. Also, we based our estimates on scheduled times though we recognize that on-time performance of rail and bus services may vary by census tract. We made assumptions for walking times and wait times at stops. In addition, we did not include an estimation of travel time over the weekend since very few facilities were open on Saturdays. Finally we did not account for mammography clinics in surrounding counties which may provide services to residents near county borders. However, train lines do not extend beyond Fulton and DeKalb counties and bus lines are limited in outlying counties. Another consideration was our categorization of vehicle access. We conservatively based our classification of census tracts on access to 1 vehicle per household. It may be that 1 vehicle in a large household may not provide everyone in the household with equal access.
A particular strength of this study was the construction and use of a transportation network analysis which provided more accurate and realistic time and distance measurements than measurements based on simple Euclidean point-to-point distances. A recent study of time to mammography facilities in Los Angeles found an increasing likelihood of a recent mammogram as the number of facilities within a 2-mile buffer of the study respondent’s home increased, whereas the straight-line distance to the nearest facility showed no association [33]. We were also able to compare public vs. private transportation as well as to describe times and distances to the Georgia Cancer Screening Program facilities that offer free or low-cost mammograms to unemployed or underemployed women.
This study adds to the literature demonstrating differences in spatial accessibility to health services by race/ ethnicity and socioeconomic characteristics. In our data, poverty and household vehicle access were strongly correlated. Although general measures of economic deprivation such as poverty level or education are often used to classify or group geographic units, our analysis used household access to a private vehicle as a more direct measure of spatial accessibility. Using this measure and stratifying by race, we found that irrespective of the level of household vehicle availability, black women have longer travel times to mammography facilities than do white women. Furthermore, for those women who are most likely to need the services of the Georgia Cancer Screening Program facilities, public transportation travel times are longer. Additional geographic analyses should seek to pinpoint those areas where travel times are the longest and for which additional transportation services or mammography services would assure better accessibility. Among the wide range of characteristics that have been shown to affect screening, ameliorating spatial inaccessibility represents an opportunity for intervention that operates at the population level.
Acknowledgments
We thank Erin Justin, Senior Program Officer at the CDC Foundation, for project management assistance and Efomo Woghiren at the Agency for Toxic Substances and Disease Registry for assistance in building the transportation network model. This study was supported by a grant from Susan G. Komen for Cure through the CDC Foundation.
Footnotes
Disclaimer The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Lucy A. Peipins, Centers for Disease Control and Prevention, Division of Cancer Prevention and Control, 4770 Buford Hwy, NE, K-55, Atlanta, GA 30341, USA
Shannon Graham, Agency for Toxic Substances and Disease Registry, Geospatial Research, Analysis, and Services Program, Atlanta, GA, USA.
Randall Young, Agency for Toxic Substances and Disease Registry, Geospatial Research, Analysis, and Services Program, Atlanta, GA, USA.
Brian Lewis, Agency for Toxic Substances and Disease Registry, Geospatial Research, Analysis, and Services Program, Atlanta, GA, USA.
Stephanie Foster, Agency for Toxic Substances and Disease Registry, Geospatial Research, Analysis, and Services Program, Atlanta, GA, USA.
Barry Flanagan, Agency for Toxic Substances and Disease Registry, Geospatial Research, Analysis, and Services Program, Atlanta, GA, USA.
Andrew Dent, Agency for Toxic Substances and Disease Registry, Geospatial Research, Analysis, and Services Program, Atlanta, GA, USA.
References
- 1.Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, Mandelblatt JS, Yakovlev AY, Habbema JD, Feuer EJ, Cancer I Surveillance Modeling Network C. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353:1784–1792. doi: 10.1056/NEJMoa050518. [DOI] [PubMed] [Google Scholar]
- 2.Kalager M, Zelen M, Langmark F, Adami HO. Effect of screening mammography on breast-cancer mortality in Norway. New England Journal of Medicine. 2010;363:1203–1210. doi: 10.1056/NEJMoa1000727. [DOI] [PubMed] [Google Scholar]
- 3.Mandelblatt JS, Cronin KA, Bailey S, Berry DA, de Koning HJ, Draisma G, et al. Effects of mammography screening under different screening schedules: Model estimates of potential benefits and harms. Annals of Internal Medicine. 2009;151:738–747. doi: 10.1059/0003-4819-151-10-200911170-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine. 2009;151:716–726. W-236. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- 5.Lee CH, Dershaw DD, Kopans D, Evans P, Monsees B, Monticciolo D, et al. Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. Journal of the American College of Radiology. 2010;7:18–27. doi: 10.1016/j.jacr.2009.09.022. [DOI] [PubMed] [Google Scholar]
- 6.Smith RA, Cokkinides V, Brawley OW. Cancer screening in the United States, 2009: A review of current American Cancer Society guidelines and issues in cancer screening. CA: A Cancer Journal for Clinicians. 2009;59:27–41. doi: 10.3322/caac.20008. [DOI] [PubMed] [Google Scholar]
- 7.US Preventive Services Task Force. Screening for breast cancer: United States Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine. 2002;137(Part 1):344–346. [Google Scholar]
- 8.Ryerson AB, Miller JW, Eheman CR, Leadbetter S, White MC. Recent trends in U.S. mammography use from 2000–2006: A population-based analysis. Preventive Medicine. 2008;47:477–482. doi: 10.1016/j.ypmed.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Sabatino SA, Coates RJ, Uhler RJ, Breen N, Tangka F, Shaw KM. Disparities in mammography use among US women aged 40–64 years, by race, ethnicity, income, and health insurance status, 1993 and 2005. Medical Care. 2008;46:692–700. doi: 10.1097/MLR.0b013e31817893b1. [DOI] [PubMed] [Google Scholar]
- 10.Barr JK, Franks AL, Lee NC, Herther P, Schachter M. Factors associated with continued participation in mammography screening. Preventive Medicine. 2001;33:661–667. doi: 10.1006/pmed.2001.0942. [DOI] [PubMed] [Google Scholar]
- 11.Bobo JK, Shapiro JA, Schulman J, Wolters CL. On-schedule mammography rescreening in the National Breast and Cervical Cancer Early Detection Program. Cancer Epidemiology, Biomarkers and Prevention. 2004;13:620–630. [PubMed] [Google Scholar]
- 12.Coughlin SS, Leadbetter S, Richards T, Sabatino SA. Contextual analysis of breast and cervical cancer screening and factors associated with health care access among United States women, 2002. Social Science and Medicine. 2008;66:260–275. doi: 10.1016/j.socscimed.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 13.Levy-Storms L, Bastani R, Reuben DB. Predictors of varying levels of nonadherence to mammography screening in older women. Journal of the American Geriatrics Society. 2004;52:768–773. doi: 10.1111/j.1532-5415.2004.52216.x. [DOI] [PubMed] [Google Scholar]
- 14.Quinley J, Mahotiere T, Messina CR, Lee TK, Mikail C. Mammography-facility-based patient reminders and repeat mammograms for Medicare in New York State. Preventive Medicine. 2004;38:20–27. doi: 10.1016/j.ypmed.2003.09.024. [DOI] [PubMed] [Google Scholar]
- 15.Sambamoorthi U, McAlpine DD. Racial, ethnic, socioeconomic, and access disparities in the use of preventive services among women. Preventive Medicine. 2003;37:475–484. doi: 10.1016/s0091-7435(03)00172-5. [DOI] [PubMed] [Google Scholar]
- 16.Schueler KM, Chu PW, Smith-Bindman R. Factors associated with mammography utilization: A systematic quantitative review of the literature. J Womens Health (Larchmt) 2008;17:1477–1498. doi: 10.1089/jwh.2007.0603. [DOI] [PubMed] [Google Scholar]
- 17.Task Force on Community Preventive S. Recommendations for client- and provider-directed interventions to increase breast, cervical, and colorectal cancer screening. American Journal of Preventive Medicine. 2008;35:S21–S25. doi: 10.1016/j.amepre.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 18.Ward E, Halpern M, Schrag N, Cokkinides V, DeSantis C, Bandi P, et al. Association of insurance with cancer care utilization and outcomes. CA: A Cancer Journal for Clinicians. 2008;58:9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 19.Penchansky R, Thomas JW. The concept of access: Definition and relationship to consumer satisfaction. Medical Care. 1981;19:127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Elkin EB, Ishill NM, Snow JG, Panageas KS, Bach PB, Liberman L, et al. Geographic access and the use of screening mammography. Medical Care. 2010;48:349–356. doi: 10.1097/MLR.0b013e3181ca3ecb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elting LS, Cooksley CD, Bekele BN, Giordano SH, Shih YCT, Lovell KK, et al. Mammography capacity: Impact on screening rates and breast cancer stage at diagnosis. American Journal of Preventive Medicine. 2009;37:102–108. doi: 10.1016/j.amepre.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 22.Athas WF, Adams-Cameron M, Hunt WC, Amir-Fazli A, Key CR. Travel distance to radiation therapy and receipt of radiotherapy following breast-conserving surgery. Journal of the National Cancer Institute. 2000;92:269–271. doi: 10.1093/jnci/92.3.269. [DOI] [PubMed] [Google Scholar]
- 23.Celaya MO, Rees JR, Gibson JJ, Riddle BL, Greenberg ER. Travel distance and season of diagnosis affect treatment choices for women with early-stage breast cancer in a predominantly rural population (United States) Cancer Causes and Control. 2006;17:851–856. doi: 10.1007/s10552-006-0025-7. [DOI] [PubMed] [Google Scholar]
- 24.Doescher MP, Jackson JE. Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. J Public Health Manag Pract. 2009;15:200–209. doi: 10.1097/PHH.0b013e3181a117da. [DOI] [PubMed] [Google Scholar]
- 25.Engelman KK, Hawley DB, Gazaway R, Mosier MC, Ahluwalia JS, Ellerbeck EF. Impact of geographic barriers on the utilization of mammograms by older rural women. Journal of the American Geriatrics Society. 2002;50:62–68. doi: 10.1046/j.1532-5415.2002.50009.x. [DOI] [PubMed] [Google Scholar]
- 26.Hyndman JC, Holman CD, Dawes VP. Effect of distance and social disadvantage on the response to invitations to attend mammography screening. Journal of Medical Screening. 2000;7:141–145. doi: 10.1136/jms.7.3.141. [DOI] [PubMed] [Google Scholar]
- 27.Larson S, Correa-de-Araujo R. Preventive health examinations: A comparison along the rural-urban continuum. Womens Health Issues. 2006;16:80–88. doi: 10.1016/j.whi.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 28.Meden T, St John-Larkin C, Hermes D, Sommerschield S. MSJAMA. Relationship between travel distance and utilization of breast cancer treatment in rural northern Michigan. JAMA. 2002;287:111. [PubMed] [Google Scholar]
- 29.Nattinger AB, Kneusel RT, Hoffmann RG, Gilligan MA. Relationship of distance from a radiotherapy facility and initial breast cancer treatment. Journal of the National Cancer Institute. 2001;93:1344–1346. doi: 10.1093/jnci/93.17.1344. [DOI] [PubMed] [Google Scholar]
- 30.Rushton G. Methods to evaluate geographic access to health services. Journal of Public Health Management and Practice. 1999;5:93–100. [PubMed] [Google Scholar]
- 31.U S Census Bureau. Census 2000 Summary File 3 (SF3)—United States. Sample data Technical Documentation. http://Factfinder.census.gov.
- 32.Zenk SN, Tarlov E, Sun J. Spatial equity in facilities providing low- or no-fee screening mammography in Chicago neighborhoods. J Urban Health. 2006;83:195–210. doi: 10.1007/s11524-005-9023-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meersman SC, Breen N, Pickle LW, Meissner HI, Simon P. Access to mammography screening in a large urban population: A multi-level analysis. Cancer Causes and Control. 2009;20:1469–1482. doi: 10.1007/s10552-009-9373-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gumpertz ML, Pickle LW, Miller BA, Bell BS. Geographic patterns of advanced breast cancer in Los Angeles: Associations with biological and sociodemographic factors (United States) Cancer Causes and Control. 2006;17:325–339. doi: 10.1007/s10552-005-0513-1. [DOI] [PubMed] [Google Scholar]
- 35.Dai D. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health & Place. 2010;16:1038–1052. doi: 10.1016/j.healthplace.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 36.McLafferty S, Wang F. Rural reversal? Cancer. 2009;115:2755–2764. doi: 10.1002/cncr.24306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sanchez KM. The connection between public transport and employment: The cases of Portland adn Atlanta. Journal of the American Planning Association. 1999;65:284–296. [Google Scholar]
- 38.Wang F. Quantitative methods and applications in GIS. Boca Raton: CRC Press, Taylor & Francis Group; 2006. [Google Scholar]
- 39.US Department of Transportation. Manual on uniform traffic control devices, 2009 edition. Washington, DC: Federal highway Administration; 2009. [Google Scholar]
- 40.StJacques K, Levinson HS. Operational Analysis of Bus Lanes on Arterials. Washington, DC: National Academy Press; 1997. [Google Scholar]
- 41.MARTA Metropolitan Atlanta Rapid Transit Authority. [Accessed 2 Nov 2010];Schedules and Maps. http://www.itsmarta.com/ne-nor.aspx.
- 42.Wright JK. A method of mapping densities of population: With Cape Cod as an example. The Geographical Review. 1936;26:103–110. [Google Scholar]
- 43.Lovett A, Haynes R, Sunnenberg G, Gale S. Car travel time and accessibility by bus to general practitioner services: A study using patient registers and GIS. Social Science and Medicine. 2002;55:97–111. doi: 10.1016/s0277-9536(01)00212-x. [DOI] [PubMed] [Google Scholar]
- 44.Atlanta Regional Commission. State of the Atlanta Region; By the Numbers. Regional Snapshot; Atlanta, GA: [Accessed 3 January 2011]. http://atlantaregional.com/info-center/arc-newsletters/regional-snapshots/Regional-Snapshots. [Google Scholar]