Abstract
Access to screening mammography may be limited by the availability of facilities and machines, and nationwide mammography capacity has been declining. We assessed nationwide capacity at state and county levels from 2003 to 2009, the most recent year for which complete data were available. Using mammography facility certification and inspection data from the Food and Drug Administration, we geocoded all mammography facilities in the United States and determined the total number of fully accredited mammography machines in each US County. We categorized mammography capacity as counties with zero capacity (i.e., 0 machines) or counties with capacity (i.e.,≥1 machines), and then compared those two categories by sociodemographic, health care, and geographic characteristics. We found that mammography capacity was not distributed equally across counties within states and that more than 27 % of counties had zero capacity. Although the number of mammography facilities and machines decreased slightly from 2003 to 2009, the percentage of counties with zero capacity changed little. In adjusted analyses, having zero mammography capacity was most strongly associated with low population density (OR = 11.0; 95 % CI 7.7–15.9), low primary care physician density (OR = 8.9; 95 % CI 6.8–11.7), and a low percentage of insured residents (OR = 3.3; 95 % CI 2.5–4.3) when compared with counties having at least one mammography machine. Mammography capacity has been and remains a concern for a portion of the US population—a population that is mostly but not entirely rural.
Keywords: Mammography, Access, Breast cancer, Screening
Introduction
Screening mammography is currently the most effective way to detect breast abnormalities and has led to an estimated 10–25 % mortality reduction from breast cancer [1, 2]. Even as mammography use has reached a plateau in recent years [3], mammography usage varies by state [4] and a significant proportion of women are not up-to-date with screening, especially low-income women, those who are uninsured [5, 6] and those without usual source of care [7]. In November 2009, the US Preventive Services Task Force (USPSTF) recommended that women aged 50 and older undergo routine screening mammography every 2 years [8]. Earlier USPSTF recommendations and those of the American Cancer Society and the American College of Radiology recommended beginning annual screening for women 40 years of age and older [9, 10].
Among the barriers to screening that have been detailed in the literature is access to mammography facilities [11–15]. The conceptual framework describing access to medical services includes a number of related characteristics: availability or supply of services, accessibility or distance to those services, how accommodating and acceptable the services are to individuals, and the affordability of the services [16]. The availability of mammography machines, defined as mammography capacity, is a key component of access. In 2006, the US Government Accountability Office (GAO) issued a report regarding nationwide capacity for mammography from 2001 to 2004 indicating that mammography capacity decreased by 6 %. Although the capacity was judged to be nationally adequate, one-fourth of counties had no mammography capacity [17]. Additional research has shown that the lack of imaging resources in the US may be a barrier to screening [18] as well as being associated with a later breast cancer stage at diagnosis [19].
For this analysis, we updated the GAO 2006 report and provided a more detailed examination of state- and county-level mammography capacity from 2003 to 2009, the most recent years for which complete data were available. Because a relatively large proportion of counties have no capacity, we further sought to describe and compare the sociodemographic and geographic characteristics of counties with zero mammography capacity (no machines) with those counties having capacity (at least one machine) in order to better understand the factors that underlie disparities in access to mammography.
Methods
Mammography Facilities
To determine the location of all certified mammography facilities in US counties during 2003–2009, we obtained data from the mammography program reporting and information system (MPRIS), which is managed by the Food and Drug Administration (FDA) [20]. The FDA requires all US mammography facilities (including those in US territories and overseas military facilities) to undergo annual inspections and triennial accreditation and certification in order to comply with the Mammography Quality Standards Act (MQSA) of 1992 (42 U.S.C. 263b, reauthorized 1998 and 2004). For each year in our study interval, we identified all facilities certified on October 1st of that year. Using the facility ID codes, we linked each certification record to the corresponding annual inspection record, which contained the address data used for the on-site inspections and findings from those inspections.
After excluding facilities with an address in a US territory or an overseas location, we used all available street address, city, state and ZIP code data to determine the county where the facility was located. Using a variety of geocoding resources [ESRI Street Map Premium, 2008 NAVTEQ streets, Caliper TransCAD, and ESRI Data DVD 9.3 with ArcGIS software (Version 9.3, ESRI, Redlands, CA)], we geocoded 97 % of the facilities to the street level and the remaining 3 % to the zip code level. In most instances in which facilities were geocoded only to the zip code level, the entire zip code area fell within a county boundary. If the zip code spanned more than one county, but 95 % of the population in that zip code resided in one county, we assigned the facility to that county. We also used web mapping tools (Superpages.com and Google Maps) or information from facility staff to determine the county in which a facility was located. County boundaries in all states were based on 2007 data.
To estimate annual county-level mammography capacity, we aggregated inspection record data across all county facilities to determine the total number of available fully accredited mammography units in each county, including all full field digital, computed radiography, film screen and mobile units. We then classified counties as either having or not having at least one mammography unit. Next, we derived year-specific mammography capacity ratios for each county by dividing the number of mammograms that theoretically could be performed in the county by the number of women in the county 40 years of age and older. We estimated the number of mammograms that theoretically could be performed by multiplying the number of mammography machines in the county by 6,000 (the number of mammograms that the GAO estimated that a single mammography machine can perform per year) [17]. A capacity to population ratio ≥1 indicates that capacity fully meets the population needs for that year. Ratios below 1.0 suggest the county would not be able to provide a mammogram to all female county residents 40 years of age and older in that year. We used an age cutoff of 40 for our analyses because most screening guidelines during the study period recommended that mammography screening begin at age 40, and results of a 2006–2007 survey of US primary care physicians showed that virtually all were recommending that their patients begin annual mammography screening at age 40 [21].
County Characteristics
We used the most recent county-level sociodemographic data available from a number of sources. We obtained annual population data from the US Bureau of the Census [22]; county-level estimates of the number of residents in poverty from the Bureau of the Census’ Small Area Income Poverty Estimates (SAIPE) 2009 file [23]; the percentage of residents in each county who had health insurance from 2007 Small Health Area Insurance Estimates (SAHIE) data; and the percentage of the employed civilian labor force, aged 16 years or older, who were in management, professional, and related occupations, and the percentage who were in sales and office occupations from the 2000 Census of Population and Housing Demographic Profile, included in the Health Resources and Services Administration 2009–2010 Area Resource File (ARF) [24]. In addition, we used data from Census 2000 Summary File 3 to calculate the household income inequality ratio for each county. The household income inequality ratio is the ratio of the number of households with high household income in 1999 (the upper fifth or ≥$75,000) divided by the number of households with low household income (lowest fifth or ≤$19,000 or less). Census 2000 Summary File 3 provided the number of households in 16 county-level household income categories. The total household income for each category was estimated by multiplying the number of households in each category by the mid-point of the range of income for each category.
We also used data from the 2009–2010 ARF to determine county-level numbers of non-federal primary care physicians (i.e., physicians specializing in family medicine, general practice, general internal medicine, and general obstetrics-gynecology). We then calculated the primary care physician density per 100,000 county residents by dividing the number of primary care physicians in each county by that county’s population estimate and multiplying by 100,000.
Rural/Urban Classification of Counties
We divided counties into three population categories based on rural/urban continuum (RUCC) codes developed in 2003 by the US Department of Agriculture [25]. The RUCC codes divide counties into nine groups based on their population and their adjacency to a metropolitan county. We distinguished between metropolitan counties (codes 1–3), suburban/small town counties (codes 4–7) and rural counties (codes 8–9) in our analyses.
Statistical Analyses
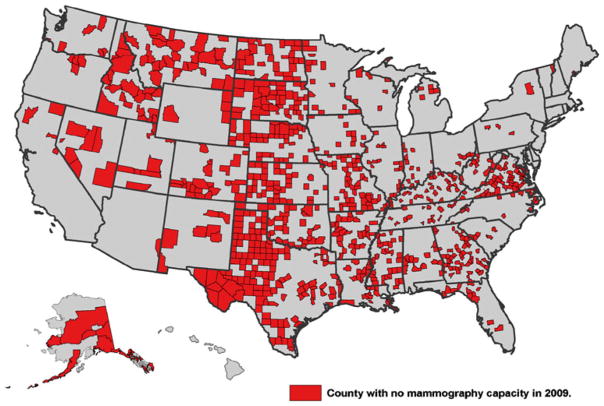
We used SAS version 9.2 (SAS Institute Inc., Cary, North Carolina) to compare zero capacity counties to counties with at least one mammography machine by their urban–rural classification and by the selected socio-demographic characteristics and health care variables described above. Using ArcGIS 10 software (ESRI, Redlands WA), we constructed a map showing the location of counties with no mammography capacity.
We then examined the relationship between mammography capacity (zero capacity vs. any capacity) and total population density, percent insured, percent poverty, household income inequality ratio, and primary care physician density using multivariate logistic regression to calculate adjusted odds ratios (ORs) and 95 % confidence intervals (CIs). The values of each of the independent variables were divided into tertiles. Regression analyses were performed using SAS software version 9.2 (SAS Institute Inc., Cary, North Carolina).
Results
From 2003 to 2009, the number of US, mammography facilities decreased by roughly 5 % (from 8,936 to 8,505) and the number of mammography machines decreased by roughly 10 % (from 13,400 to 12,098) (Table 1). If one assumes that each machine has the potential to perform 6,000 mammograms per year, this means that the maximum annual number of mammograms that could be performed in the United States decreased by 7.8 million during this period. The number of digital machines increased almost 19-fold (from 350 to 6,572), and the proportion of all machines that were digital increased from 2.6 to 54.3 %. The number of counties with no machines, or zero capacity, remained between 27 and 28 % throughout the study period. In 2009, 3.4 % of US women aged 40 years or older, or slightly more than 2.5 million women, resided in counties with no mammography capacity. However, the proportion of women in zero-capacity counties varied substantially by region: 0.2 % in the Northeast region, 1.2 % in the West region, 3.9 % in the Midwest region, and 6.1 % in the South region (data not shown). As shown in Fig. 1, zero-capacity counties were concentrated in a wide swath from west Texas–North Dakota as well as in several southern states.
Table 1.
US mammography capacity by year, 2003–2009
| Year | Facilities | Mammography machines, totala | Counties with no machines | Digital machinesc | Mobile units | Counties with at least 1 mobile unit |
|---|---|---|---|---|---|---|
| N | N | N (%b) | N (% total) | N | % | |
| 2003 | 8,936 | 13,400 | 866 (27.6) | 350 (2.6) | 305 | 6.2 |
| 2004 | 8,827 | 13,408 | 852 (27.1) | 544 (4.1) | 262 | 5.6 |
| 2005 | 8,704 | 13,394 | 852 (27.2) | 860 (6.4) | 215 | 4.4 |
| 2006 | 8,655 | 13,314 | 860 (27.4) | 1,437 (10.8) | 180 | 3.5 |
| 2007 | 8,647 | 12,993 | 857 (27.3) | 2,595 (20.0 | 155 | 3.1 |
| 2008 | 8,616 | 12,548 | 856 (27.3) | 4,662 (37.2) | 160 | 3.0 |
| 2009 | 8,505 | 12,098 | 870 (27.7) | 6,572 (54.3) | 225 | 4.7 |
Sum of number of film screen units, full field digital units, and computed radiology units
Percentage of all 3,141 US counties
Full field digital units or computed radiology units
Fig. 1.
Counties with no mammography capacity (n = 870), Mammography Program Reporting and Information System Data, 2009
At the state level (Table 2), the capacity to population ratio ranged from 0.78 in Maryland to 2.14 in North Dakota. Although most states had an adequate number of mammography machines overall, 84 % of states had one or more counties with no machines. In 2009, Texas, Virginia, Georgia, Missouri, and Nebraska had the largest number of zero-capacity counties, and South Dakota, North Dakota, Texas, Alaska, and Idaho had the highest percentage of zero-capacity counties. All but 8 states had fewer machines in 2009 than in 2003, with the largest decreases occurring in New York, Pennsylvania, Indiana, Texas, and Illinois.
Table 2.
Ratio of mammography capacitya to population, percentage of mammography machines that were digital, and percentage of counties with no machines, by state, 2009
| State | Women age ≥40 in state n | Mammography machines, total n | Ratio of mammography capacity to population | Digital machines % total | Counties total n | Counties with no machines, n |
|---|---|---|---|---|---|---|
| Alabama | 1,176,528 | 182 | 0.93 | 49.5 | 67 | 13 |
| Alaska | 140,231 | 41 | 1.75 | 46.3 | 27 | 13 |
| Arizona | 1,483,090 | 228 | 0.92 | 57.0 | 15 | 1 |
| Arkansas | 708,169 | 121 | 1.03 | 37.2 | 75 | 27 |
| California | 8,216,521 | 1,153 | 0.84 | 48.8 | 58 | 4 |
| Colorado | 1,131,576 | 174 | 0.92 | 57.5 | 64 | 24 |
| Connecticut | 922,806 | 175 | 1.14 | 77.1 | 8 | 0 |
| Delaware | 226,121 | 39 | 1.03 | 79.5 | 3 | 0 |
| District of Columbia | 139,335 | 31 | 1.33 | 54.8 | 1 | 0 |
| Florida | 4,909,256 | 706 | 0.86 | 59.1 | 67 | 12 |
| Georgia | 2,207,221 | 380 | 1.03 | 46.3 | 159 | 54 |
| Hawaii | 315,686 | 54 | 1.03 | 46.3 | 5 | 1 |
| Idaho | 337,673 | 58 | 1.03 | 55.2 | 44 | 21 |
| Illinois | 3,054,825 | 542 | 1.06 | 48.7 | 102 | 20 |
| Indiana | 1,544,152 | 266 | 1.03 | 62.8 | 92 | 14 |
| Iowa | 749,565 | 165 | 1.32 | 50.3 | 99 | 12 |
| Kansas | 663,398 | 144 | 1.30 | 44.4 | 105 | 40 |
| Kentucky | 1,069,830 | 213 | 1.19 | 45.5 | 120 | 36 |
| Louisiana | 1,068,133 | 191 | 1.07 | 63.9 | 64 | 20 |
| Maine | 368,684 | 71 | 1.16 | 71.8 | 16 | 1 |
| Maryland | 1,430,231 | 186 | 0.78 | 54.8 | 24 | 0 |
| Massachusetts | 1,704,729 | 280 | 0.99 | 75.4 | 14 | 0 |
| Michigan | 2,511,989 | 442 | 1.06 | 51.8 | 83 | 6 |
| Minnesota | 1,265,852 | 254 | 1.20 | 53.9 | 87 | 15 |
| Mississippi | 699,601 | 116 | 0.99 | 39.7 | 82 | 32 |
| Missouri | 1,488,323 | 256 | 1.03 | 51.2 | 115 | 49 |
| Montana | 245,333 | 48 | 1.17 | 72.9 | 56 | 26 |
| Nebraska | 422,397 | 100 | 1.42 | 48.0 | 93 | 41 |
| Nevada | 577,862 | 84 | 0.87 | 40.5 | 17 | 7 |
| New Hampshire | 348,651 | 61 | 1.05 | 73.8 | 10 | 0 |
| New Jersey | 2,234,204 | 312 | 0.84 | 63.1 | 21 | 0 |
| New Mexico | 472,167 | 66 | 0.84 | 39.4 | 33 | 7 |
| New York | 4,953,347 | 782 | 0.95 | 60.1 | 62 | 1 |
| North Carolina | 2,278,237 | 332 | 0.87 | 59.6 | 100 | 14 |
| North Dakota | 154,521 | 55 | 2.14 | 32.7 | 53 | 29 |
| Ohio | 2,938,639 | 554 | 1.13 | 33.8 | 88 | 5 |
| Oklahoma | 873,491 | 140 | 0.96 | 58.6 | 77 | 29 |
| Oregon | 941,112 | 141 | 0.90 | 63.8 | 36 | 4 |
| Pennsylvania | 3,354,948 | 537 | 0.96 | 52.1 | 67 | 3 |
| Rhode Island | 276,735 | 57 | 1.24 | 66.7 | 5 | 0 |
| South Carolina | 1,143,013 | 175 | 0.92 | 62.9 | 46 | 5 |
| South Dakota | 195,378 | 57 | 1.75 | 47.4 | 66 | 39 |
| Tennessee | 1,566,259 | 260 | 1.00 | 50.0 | 95 | 19 |
| Texas | 5,197,900 | 776 | 0.90 | 62.1 | 254 | 126 |
| Utah | 488,381 | 67 | 0.82 | 53.7 | 29 | 8 |
| Vermont | 167,611 | 26 | 0.93 | 80.8 | 14 | 2 |
| Virginia | 1,908,689 | 309 | 0.97 | 61.5 | 134 | 60 |
| Washington | 1,577,522 | 219 | 0.83 | 64.8 | 39 | 6 |
| West Virginia | 486,822 | 90 | 1.11 | 37.8 | 55 | 13 |
| Wisconsin | 1,398,103 | 353 | 1.51 | 45.0 | 72 | 7 |
| Wyoming | 124,265 | 29 | 1.40 | 31.0 | 23 | 4 |
| US total | 73,859,112 | 12,098 | 0.98 | 54.3 | 3,141 | 870 |
Ratio of capacity to population = 6000
Number of machines/number of women 40 years of age or older
In 2009, the proportion of mammography machines that were digital ranged from 31 % in Wyoming to 81 % in Vermont; California, Texas, New York, Florida, and Pennsylvania had the largest number of digital machines (together accounting for 34 % of the national total) (Table 2). Of all digital machines, 86.1 % were in metropolitan counties, 13.3 % in suburban/small town counties, and 0.6 % in rural counties (data not shown).
Of the 12,098 mammography machines reported for 2009, 225 were mobile machines. Furthermore, 86 % (194/225) of the mobile machines were in metro counties. Only 3 mobile mammography machines were in completely rural counties (RUCC codes 8–9) (data not shown).
Most zero-capacity counties were classified as “rural” (Table 3). Rural counties were eight times more likely to have zero capacity than were counties classified as “metropolitan” (data not shown). Among women 40 years of age and older who resided in rural counties, more than half of the women resided in counties with no mammography machines whereas only around 2 % of those in metropolitan counties had no such access. In addition, the 2009 population density in zero-capacity counties was less than that in counties with at least one mammography machine even among counties with the same urban–rural classification. However, the mean population density in both suburban/small town and rural zero-capacity counties was considerably less than that in metropolitan zero-capacity counties, which suggests that population density does not, by itself, account for the number of mammography machines. Overall, there was about 6 % difference in the percent insured among the various rural–urban categories, with the lowest percent insured seen in zero capacity non-metropolitan rural counties.
Table 3.
Selected characteristics of residents in US counties by rural–urban categoriesa and by mammography capacity (0 machines vs.≥1 machine) in 2009
| County rural–urban category and number | Counties | Women age ≥40 years 2009 | Population density, 2009b | Percent white collar, 2000 | Percent insured, 2007 | Percent below poverty level, 2007 | Household income inequality ratio, 2000c | Primary care physician density, 2008d | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|||||||||
| Mammography machines | n | n | Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE |
| Metropolitan | ||||||||||||||
| 0 machines | 195 | 1,034,399 | 137.3 | 39.4 | 49.7 | 0.5 | 79.7 | 0.4 | 15.2 | 0.4 | 8.5 | 0.7 | 25.7 | 2.9 |
| ≥1 machine | 895 | 59,749,194 | 746 | 97.5 | 57.5 | 0.3 | 83.3 | 0.2 | 13.6 | 0.2 | 15.4 | 0.6 | 67.4 | 1.3 |
| Suburban/small town | ||||||||||||||
| 0 machines | 198 | 651,460 | 47.3 | 11.8 | 46.5 | 0.4 | 79.3 | 0.5 | 20.3 | 0.5 | 3.9 | 0.2 | 37.5 | 2.5 |
| ≥1 machine | 1,183 | 10,981,934 | 60 | 3.2 | 49.4 | 0.2 | 82.8 | 0.2 | 17.3 | 0.2 | 5.7 | 0.2 | 53.9 | 0.9 |
| Rural | ||||||||||||||
| 0 machines | 477 | 824,823 | 12.5 | 0.7 | 50.2 | 0.3 | 77.8 | 0.3 | 17.8 | 0.3 | 4.1 | 0.1 | 27.6 | 1.6 |
| ≥1 machine | 193 | 617,302 | 21.4 | 1.4 | 49.6 | 0.4 | 81.3 | 0.3 | 16.6 | 0.4 | 4.2 | 0.2 | 55.3 | 3.3 |
| All counties by mammography machine status | ||||||||||||||
| 0 machines | 870 | 2,510,682 | 48.4 | 9.4 | 49.2 | 0.2 | 78.6 | 0.2 | 17.8 | 0.2 | 5.0 | 0.2 | 29.4 | 1.3 |
| ≥1 machine | 2,271 | 71,348,430 | 327.1 | 39.1 | 52.6 | 0.2 | 82.9 | 0.1 | 15.8 | 0.1 | 9.4 | 0.3 | 59.3 | 0.8 |
| All counties by population category | ||||||||||||||
| Metropolitan | 1,090 | 60,783,593 | 637.1 | 80.6 | 56.1 | 0.3 | 82.7 | 0.2 | 13.9 | 0.2 | 14.2 | 0.5 | 59.9 | 1.3 |
| Suburban/small town | 1,381 | 11,633,394 | 58.2 | 3.2 | 49.0 | 0.2 | 82.3 | 0.2 | 17.7 | 0.2 | 5.4 | 0.1 | 51.5 | 0.8 |
| Rural | 670 | 1,442,125 | 15.1 | 0.7 | 50.0 | 0.3 | 78.8 | 0.2 | 17.4 | 0.3 | 4.1 | 0.1 | 35.6 | 1.6 |
RUCC codes are the US Department of Agriculture 2003 Rural–Urban Continuum Codes [1–9] where Metropolitan counties are RUCC 1–3; suburban/small town (excluding rural) counties are RUCC 4–7; and Rural counties are RUCC 8–9
Per square mile
Average annual income among households in highest income quintile/average annual income among households in lowest income quintile
Per 100,000 population
The proportion of residents with incomes below the poverty level averaged 13.9 % in urban counties, 17.7 % in suburban/small town counties, and 17.4 % in rural counties (Table 3). The highest percentage of poverty (20.3 %) was in zero-capacity suburban/small town counties. Overall, the household income inequality ratio in metropolitan counties was about 2.5 times higher than that in suburban/small town counties and about 3.0 times higher than that in rural counties. Although the income inequality ratios for metropolitan and suburban/small town counties were substantially higher in counties with mammography capacity than in counties with no capacity (15.4 vs. 8.5 and 5.7 vs. 3.9, respectively), the ratios for rural counties differed little by mammography capacity status (4.2 vs. 4.1). Among counties with mammography capacity, primary care physician density was higher in those classified as metropolitan than in those classified as suburban/small town or rural. Among zero-capacity counties, physician density was highest in those classified as suburban/small town, and physician density in counties classified as rural was similar to that in counties classified as metropolitan.
Results of our unadjusted analysis of the relationship between the absence of mammography machines and county characteristics showed that the likelihood of a county having zero capacity was positively associated with the percentage of the population below the poverty level and negatively associated with population density, percentage of the population with health insurance, household income inequality ratio, and primary care physician density (Table 4). Although each of these associations remained significant in our adjusted analyses, zero capacity was most strongly associated with low population density (OR = 11.0; 95 % CI 7.7, 15.9), low primary care physician density (OR = 8.9; 95 % CI 6.8, 11.7), and a low percentage of insured residents (OR = 3.3; 95 % CI 2.5, 4.3).
Table 4.
Relationship between county sociodemographic characteristics and absence of mammography machines, 2009
| Unadjusted | Adjusteda | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Odds ratio | 95 % CI | p value | Odds ratio | 95 % CI | p value | |
| Population density | ||||||
| Highest | 1.0 | 1.0 | ||||
| Middle | 5.6 | (4.1, 7.6) | < .0001 | 2.9 | (2.1, 4.1) | < .0001 |
| Lowest | 21.2 | (15.9, 28.9) | < .0001 | 11.0 | (7.7, 15.9) | < .0001 |
| Percent insured | ||||||
| Highest | 1.0 | 1.0 | ||||
| Middle | 2.6 | (2.1, 1.3) | < .0001 | 1.7 | (1.3, 2.3) | < .0001 |
| Lowest | 5.7 | (4.6, 7.1) | < .0001 | 3.3 | (2.5, 4.3) | < .0001 |
| Percent in poverty | ||||||
| Highest | 1.0 | 1.0 | ||||
| Middle | 0.6 | (0.5, 0.7) | < .0001 | 1.0 | (0.8, 1.3) | NS |
| Lowest | 0.6 | (0.5, 0.7) | < .0001 | 1.3 | (1.0, 1.8) | NS |
| Household income inequality | ||||||
| Highest | 1.0 | 1.0 | ||||
| Middle | 2.6 | (2.0, 3.2) | < .0001 | 1.0 | (0.7, 1.4) | NS |
| Lowest | 6.1 | (4.9, 7.7) | < .0001 | 1.6 | (1.1, 2.3) | 0.01 |
| Primary care physician density | ||||||
| Highest | 1.0 | 1.0 | ||||
| Middle | 1.9 | (1.4, 2.4) | < .0001 | 1.8 | (1.3, 2.4) | < .0001 |
| Lowest | 11.5 | (9.1, 14.6) | < .0001 | 8.9 | (6.8, 11.7) | < .0001 |
Values for each variable adjusted for all other variables in table
Discussion and Conclusions
For the majority of states in the US, the number of mammography machines appears adequate for the population as a whole, but analyses by state do not capture geographic disparities within the state. Similar to an earlier examination of national mammography capacity, our findings indicate that capacity is not distributed equally across counties [18] and that 870 (27.7 %) counties have zero capacity. Although the number of mammography facilities and machines decreased slightly between 2003 and 2009, the percentage of zero-capacity counties remained fairly consistent. According to 2009 census data, almost 2.5 million women 40 years of age and older lived in these zero-capacity counties. In general, zero-capacity counties had a lower population density, a higher percentage of residents in poverty, a lower prevalence of insurance coverage, and a lower primary care physician density than did counties with at least one mammography machine.
We also found that, in metropolitan and suburban/small town counties, the likelihood of having a least one mammography machine was positively associated with income inequality. The magnitude of differences across the income spectrum and concentrated wealth or poverty represent different kinds of inequalities that can operate differently at individual, community or larger geographic levels [26]. Income inequality has been associated with health disparities [27] but the pathways through which inequality operates are not fully understood [28] [29]. A higher income inequality ratio indicates a wider range of incomes and higher incomes suggest higher demand and ability to pay for services requiring more resources to meet that demand [30]. This may be especially true for the growth of a new technology such as digital mammography. Higher income inequalities were seen in metropolitan and suburban/small town counties compared with rural counties and in metropolitan capacity versus metropolitan zero-capacity counties. Income inequality, mammography capacity, and the proportion of digital machines were largest for the metropolitan counties. While services may be present in metropolitan counties with high income inequalities as demanded by high income groups, these services may not be accessible to the lowest income groups within that county whose dependence on public transportation may limit access [31]. Household income inequality ratio was the same for rural capacity and zero-capacity counties. Rural counties with capacity have higher population density, lower poverty and higher physician density than rural counties with zero capacity.
The results of our multivariate regression analysis showed that population density, primary care physician density, and insurance prevalence were the factors most strongly associated with a county’s mammography capacity status. Within all three of our urban–rural categories, zero-capacity counties had a lower primary care physician density than did counties with at least one mammography machine. The metropolitan zero capacity counties had a physician density almost equal to the zero capacity rural areas despite the higher population density of the metropolitan area counties. Although most of these counties were classified as metropolitan due in some degree to their adjacency to large metropolitan counties, they are not rural. Clearly medical service shortage is not strictly a phenomenon of rural areas.
Technology is an important consideration with respect to the geographic allocation of medical resources. More advanced technology would typically be seen in locations that can support such technology, both in terms of trained personnel, specialized facilities or other resources, and this is true for digital mammography capacity located primarily in metropolitan areas. While the percent of digital mammography machines has increased substantially over this time period, the vast majority are located in metropolitan areas (86 % in metropolitan counties vs. 0.6 % in rural counties (data not shown). These areas are also areas of greatest income inequality and of demand and ability to pay for new technologies. However, because digital mammography machines produce images that can be transmitted electronically to off-site locations for interpretation, digital machines may be especially appropriate technology for rural areas, the areas least likely to have them. A potential barrier is the increased cost associated with digital mammography [32]. Even as digital machines allow facilities to increase exam workload [33] and produce records that are easily accessible thereby improving efficiency and productivity, savings may be offset by the cost of the equipment as well as costs associated with image archiving and printing [34].
Our facility numbers do not exactly match those found on the FDA Website Scorecard Statistics which presents commonly requested national statistics on the MQSA program [35]. This is due to several factors. First, the FDA counts all facilities that are certified, including military facilities outside the US We included only facilities within US counties. Second, the FDA summary statistics are based upon certification records where addresses may not be actual facility addresses but may refer to administrative offices. In contrast, we merged certification information with inspection records in order to obtain the actual addresses used by inspectors when they go onsite to inspect the facilities. Despite these differences, we obtained an overall facility percentage match of 97–98 % for the years 2003–2009.
One limitation is that capacity assessments at the state or county levels do not indicate whether people in a specific area within a state or county have access to mammography services within that area. For example, we found that North Dakota had a large number of zero-capacity counties even though it had an overall capacity to population ratio >1, indicating adequate capacity at the state level. Similarly, the assignment of uniform sociodemographic characteristics at the county level can conceal considerable variation in the distribution of these characteristics at the community level, a variation which our results do not reflect. Furthermore, US counties differ substantially in size and population density, and county residents are not distributed evenly within counties. We took population density into account in our assessment of the relationship between county sociodemographic characteristics and absence of mammography machines. Another potential limitation is that women in zero capacity counties may have obtained mammograms from a neighboring county or from a mobile mammography machine from an adjacent county. Since the locations of mobile mammography machines were assigned to the county of its home facility, their areas of service were unknown. Although the number of mobile machines is low, resulting in little impact on overall capacity, some zero capacity counties may be served by these mobile machines from another county. Another limitation is that we almost certainly overestimated mammography capacity because we assumed that all machines were fully functional at all times.
Several studies comparing screening prevalence to availability of mammography facilities using data from the Behavioral Risk Factor Surveillance System (BRFSS) found that unavailability of mammography facilities may be a barrier to screening [18, 36]. We could not provide a direct assessment of the relationship between screening utilization as reported in the BRFSS and the availability of screening facilities from the FDA because of BRFSS data limitations. BRFSS samples are designed to provide reliable national and state-level estimates on risk factors and health-related behavior. Many of our zero capacity counties had relatively small populations, and the number of BRFSS respondents in those counties was too small to provide a reliable county level estimate.
Our results show that mammography capacity has been and remains a concern for a portion of the US population—a population that is mostly but not entirely rural. Increasing the age at which mammography is initiated from 40 to 50 years of age would reduce the total number of mammography machines needed on a national basis, would have no effect on zero capacity counties. In the current economic environment, the efficient allocation of resources where need is greatest assumes an even greater importance. This investigation of capacity is one step in assessing that need. Also suggested by this research is the need to allocate resources where the need is greatest or likely to increase. Digital mammography can facilitate remote screening services which may help to address chronic deficits in medical services, despite increased cost. Furthermore, changes in the age distribution of the population and changes in insurance coverage that would decrease cost-sharing would be expected to create greater demand in certain locations [37]. A countervailing trend however, is a potential for decline in capacity due to financial constraints brought on by the recent economic downturn. These changes suggest a need to monitor capacity in the future. A focus on the distribution of mammography services and on the effects of technological advances may inform our efforts to address disparities in access to mammography.
Acknowledgments
We would like thank Charles Finder, MD, and Timothy Haran at the Food and Drug Administration’s Division of Mammography Quality and Radiation Programs for their technical assistance. This manuscript was written in the course of employment by the United States Government and is not subject to copyright in the United States. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Funding support was provided by the Centers for Disease Control and Prevention (Contract No. 200-2002-00574, Task order 0015).
Contributor Information
Lucy A. Peipins, Division of Cancer Prevention and Control, Centers for Disease Prevention and Control, Atlanta, GA, USA. Epidemiology and Applied Research Branch, DCPC, CDC, 4770 Buford Highway, NE, Mailstop K55, Atlanta, GA 30341-3717, USA
Jacqueline Miller, Division of Cancer Prevention and Control, Centers for Disease Prevention and Control, Atlanta, GA, USA.
Thomas B. Richards, Division of Cancer Prevention and Control, Centers for Disease Prevention and Control, Atlanta, GA, USA
Janet Kay Bobo, Battelle Centers for Public Health Research and Evaluation, Seattle, WA, USA.
Ta Liu, Battelle Centers for Public Health Research and Evaluation, Seattle, WA, USA.
Mary C. White, Division of Cancer Prevention and Control, Centers for Disease Prevention and Control, Atlanta, GA, USA
Djenaba Joseph, Division of Cancer Prevention and Control, Centers for Disease Prevention and Control, Atlanta, GA, USA.
Florence Tangka, Division of Cancer Prevention and Control, Centers for Disease Prevention and Control, Atlanta, GA, USA.
Donatus U. Ekwueme, Division of Cancer Prevention and Control, Centers for Disease Prevention and Control, Atlanta, GA, USA
References
- 1.Kalager M, Zelen M, Langmark F, Adami HO. Effect of screening mammography on breast-cancer mortality in Norway. New England Journal of Medicine. 2010;363(13):1203–1210. doi: 10.1056/NEJMoa1000727. [DOI] [PubMed] [Google Scholar]
- 2.Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. New England Journal of Medicine. 2005;353(17):1784–1792. doi: 10.1056/NEJMoa050518. [DOI] [PubMed] [Google Scholar]
- 3.Richardson LC, Rim SH, Plescia M. Vital Signs: Breast cancer screening among women aged 50–74 years–United States, 2008. MMWR Morbidity and Mortality Weekly Report. 2010;59:6–9. [PubMed] [Google Scholar]
- 4.Miller JW, King JB, Ryerson AB, Eheman CR, White MC. Mammography use from 2000 to 2006: State-level trends with corresponding breast cancer incidence rates. American Journal of Roentgenology. 2009;192(2):352–360. doi: 10.2214/ajr.08.1757. [DOI] [PubMed] [Google Scholar]
- 5.Ryerson AB, Miller JW, Eheman CR, Leadbetter S, White MC. Recent trends in U.S. mammography use from 2000–2006: A population-based analysis. Preventive Medicine. 2008;47(5):477–482. doi: 10.1016/j.ypmed.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 6.Sabatino SA, Coates RJ, Uhler RJ, Breen N, Tangka F, Shaw KM. Disparities in mammography use among US women aged 40–64 years, by race, ethnicity, income, and health insurance status, 1993 and 2005. Medical Care. 2005;46(7):692–700. doi: 10.1097/MLR.0b013e31817893b1. [DOI] [PubMed] [Google Scholar]
- 7.Swan J, Breen N, Graubard BI, McNeel TS, Blackman D, Tangka FK, et al. Data and trends in cancer screening in the United States: Results from the 2005 national health interview survey. Cancer. 2010;116(20):4872–4881. doi: 10.1002/cncr.25215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine. 2009;151(10):716–726. W-236. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- 9.Smith RA, Cokkinides V, Brooks D, Saslow D, Brawley OW. Cancer Screening in the United States, 2010: A review of current American Cancer Society guidelines and issues in cancer screening. CA: A Cancer Journal for Clinicians. 2010;60(2):99–119. doi: 10.3322/caac.20063. [DOI] [PubMed] [Google Scholar]
- 10.Lee CH, Dershaw DD, Kopans D, Evans P, Monsees B, Monticciolo D, et al. Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol. 2010;7(1):18–27. doi: 10.1016/j.jacr.2009.09.022. [DOI] [PubMed] [Google Scholar]
- 11.Doescher MP, Jackson JE. Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. Journal of Public Health Management and Practice. 2009;15(3):200–209. doi: 10.1097/PHH.0b013e3181a117da. [DOI] [PubMed] [Google Scholar]
- 12.Engelman KK, Hawley DB, Gazaway R, Mosier MC, Ahluwalia JS, Ellerbeck EF. Impact of geographic barriers on the utilization of mammograms by older rural women. Journal of the American Geriatrics Society. 2002;50(1):62–68. doi: 10.1046/j.1532-5415.2002.50009.x. [DOI] [PubMed] [Google Scholar]
- 13.Hyndman JC, Holman CD, Dawes VP. Effect of distance and social disadvantage on the response to invitations to attend mammography screening. Journal of Medical Screening. 2000;7(3):141–145. doi: 10.1136/jms.7.3.141. [DOI] [PubMed] [Google Scholar]
- 14.Larson S, Correa-de-Araujo R. Preventive health examinations: A comparison along the rural-urban continuum. Womens Health Issues. 2006;16(2):80–88. doi: 10.1016/j.whi.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Meden T, John-Larkin C, Hermes D, Sommerschield S. Relationship between travel distance and utilization of breast cancer treatment in rural northern Michigan. JAMA. 2002;287(1):111. [PubMed] [Google Scholar]
- 16.Penchansky R, Thomas JW. The concept of access: Definition and relationship to consumer satisfaction. Medical Care. 1981;19(2):127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Unites States Government Accountability Office. Mammography: current nationwide capacity is adequate, but access problems may exist in certain locations. United States Government Accountability Office; Washington, DC: Jul, 2006. [Google Scholar]
- 18.Elkin EB, Ishill NM, Snow JG, Panageas KS, Bach PB, Liberman L, et al. Geographic access and the use of screening mammography. Medical Care. 2010;48(4):349–356. doi: 10.1097/MLR.0b013e3181ca3ecb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elting LS, Cooksley CD, Bekele BN, Giordano SH, Shih YCT, Lovell KK, et al. Mammography capacity: Impact on screening rates and breast cancer stage at diagnosis. American Journal of Preventive Medicine. 2009;37(2):102–108. doi: 10.1016/j.amepre.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 20.Center for Devices, Radiological Health. Mammography program reporting and information system (MPRIS), US Food and Drug Administration. MD: Silver Spring; 2007. [Google Scholar]
- 21.Meissner HI, Klabunde CN, Han PK, Benard VB, Breen N. Breast cancer screening beliefs, recommendations and practices: Primary care physicians in the United States. Cancer. 2011;117(14):3101–3111. doi: 10.1002/cncr.25873. [DOI] [PubMed] [Google Scholar]
- 22.U S Census Bureau. Census. Summary File 3 (SF3)—United States (2009) [Accessed April 8, 2007];Sample data technical documentation. 2000 Available at: http://Factfinder.census.gov.
- 23.U S Census Bureau. [Accessed Aug 12, 2011];Small Area Income Poverty Estimates. 2009 Available at: http://www.census.gov/did/www/saipe.
- 24.Health Resources and Service Administration. [Accessed Aug 12, 2011];Area Resource File (ARF) 2009 –2011. Available at: http://arf.hrsa.gov.
- 25.US Department of Agriculture. [Accessed Dec 6, 2010];Measuring rurality: Rural urban continuum codes. 2003 Available at: http://www.ers.usda/gov/briefing/rurality/ruralurbcon.
- 26.Wen M, Browning CR, Cagney KA. Poverty, affluence, and income inequality: Neighborhood economic structure and its implications for health. Social Science and Medicine. 2003;57(5):843–860. doi: 10.1016/s0277-9536(02)00457-4. [DOI] [PubMed] [Google Scholar]
- 27.Wilkinson RG, Pickett E. The spirit level: Why greater equality makes societies stronger. New York: Bloomsbury Press; 2009. [Google Scholar]
- 28.Lynch JW, Smith GD, Kaplan GA, House JS. Income inequality and mortality: Importance to health of individual income, psychosocial environment, or material conditions. British Medical Journal. 2000;320:1200–1204. doi: 10.1136/bmj.320.7243.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Maio FG. Income inequality measures. Journal of Epidemiology and Community Health. 2007;61:849–852. doi: 10.1136/jech.2006.052969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goldman DP, Lakdawalla DN. A theory of health disparities and medical technology. Contributions to Economic Analysis and Policy. 2005;4(1):1–30. [Google Scholar]
- 31.Peipins L, Graham S, Young R, Lewis B, Foster S, Flanagan B, et al. Time and distance barriers to mammography facilities in the Atlanta metropolitan area. Journal of Community Health. 2011;36(4):675–683. doi: 10.1007/s10900-011-9359-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tosteson AN, Stout NK, Fryback DG, Acharyya S, Herman BA, Hannah LG, et al. Cost-effectiveness of digital mammography breast cancer screening. Annals of Internal Medicine. 2008;148(1):1–10. doi: 10.7326/0003-4819-148-1-200801010-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spelic DC, Kaczmarek RV, Hilohi M, Belella A. United States radiological health activities: inspection results of mammography facilities. Biomedical Imaging and Intervention Journal. 2007;3(2):1–16. doi: 10.2349/biij.3.2.e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mullaney R, Burbage D, Evantash A, Penman E, Napoletano J, Grusenmeyer PA. Making the transition to digital mammography. Community Oncology. 2007;4:678–680. [Google Scholar]
- 35.U.S. Food and Drug Administration. [Accessed Feb 15, 2011];MQSA national statistics. 2011 Available at: http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardActandProgram/FacilityScorecard/ucm113858.htm.
- 36.Bennett KJ, Probst JC, Bellinger JD. Receipt of cancer screening services: Surprising results for some rural minorities. The Journal of Rural Health. 2012;28:63–72. doi: 10.1111/j.1748-0361.2011.00365.x. [DOI] [PubMed] [Google Scholar]
- 37.Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in medicare health plans. New England Journal of Medicine. 2008;358:375–383. doi: 10.1056/NEJMsa070929. [DOI] [PubMed] [Google Scholar]