Abstract
A review of numerous case reports was made, in order to demonstrate the possibilities for treatment of dental disorders in patients with Cleidocranial dysplasia (CCD). In this paper, our own report, including a diagnosis of the effect on the auditory system, is presented. In addition to the triad of CCD symptoms that include hypoplastic or aplastic clavicles, impacted and supernumerary teeth, delayed closure of fontanelles and cranial sutures, impairment of the hearing system resulting in conductive hearing loss also occurs. Our own report is based on the case of a 12-year-old CCD patient, in whom Cone Beam Computed Tomography (CBCT) revealed the presence of 12 supernumerary teeth. Furthermore, a clinical examination pointed to the presence of retained deciduous teeth and a delayed eruption of permanent teeth. Orthodontic-surgical procedures were implemented, in accordance with the literature. During the course of the orthodontic treatment, a decrease in auditory sensitivity was observed, for which reason hearing tests were also performed. Conductive hearing loss was detected. As such, it is important to remember that in such cases, auditory check-ups need to be performed between the many surgical and orthodontic interventions, which usually last a few years.
Keywords: cleidocranial dysplasia, hearing loss, orthodontic-surgical treatment
1. Introduction
Cleidocranial dysplasia (CCD), is a rare, hereditary, autosomal, dominant disease, with an incidence rate of one in a million live births. The appearance of people with CCD is usually pathognomonic. People suffering from this condition are relatively short. The main symptoms reported in the literature are: bilateral or one-sided hypoplastic or aplastic clavicles (affecting 10%), resulting in hypermobility of the arms; supernumerary teeth; brachycephalic skull; delayed anterior fontanelle closure; delayed sagittal and frontal suture closure; numerous Wormian bones; a hypoplastic jaw and zygomatic bone (making the face seem smaller than usual); a wide based nose with a collapsed ridge, as well as many other skeletal deformities [1,2,3,4]. Hearing problems are most often a result of abnormalities in the development of the facial skeleton, a high, arched palate, reduced paranasal sinuses and mastoid cells (or a lack thereof), dysfunction of the auditory tube and frequent inflammation of the middle ear [5,6]. However, there are no mental abnormalities in CCD. Therapy focuses mainly on the surgical-orthodontic aspect: removal of persistent deciduous teeth and supernumerary teeth [7], with the inclusion of solid teeth to the arch [8,9,10,11]. An important element of the established therapy is to take the patient along the diagnostic and audiological pathway – the authors of this paper indicate that diagnosis of hearing loss can be crucial in CCD diagnosis [4,12]. Among the testing that it is necessary to perform are: tone and speech audiometry, tympanometry (tympanograms and stapedius reflexes), and otoacoustic emission recording [2,12]. This paper is aimed at presenting a case-by-case study of CCD patients treated with surgical-orthodontic treatment in the past five years, as well as the specific case of a 12-year-old CCD girl treated orthodontically and tested audiologically.
2. Methodology and case description
The PubMed literature database was searched using the following keywords: ‘cleidocranial dysplasia’, ‘CCD’, and ‘case report.’ From this, 458 reports were obtained, and 9 articles from the last 5 years on CCD cases in 8-16-year-old patients were selected. Publications where orthodontic treatment was planned, but no active orthodontic therapy was shown were excluded. 4 articles including descriptions of their own CCD cases were selected.
Table 1 below summarizes the case reports in literature that we reference in this article.
Table 1.
| Author and year of publication | Number of patients studied | Age and sex | Diagnostics | Surgical-orthodontic treatment |
|---|---|---|---|---|
| Nagarathna et al., 2012 | 1 | 15, F |
|
|
| Park et al., 2013 | 2 | 12, M |
|
|
| 14, F |
|
|
||
| Bechtold et al., 2014 | 1 | 9, M |
|
|
| Zhang et al., 2015 | 2 | 16, F |
|
|
| 15, M |
|
|
||
Nagarathna et al. [13] described a 15-year-old CCD patient. In the course of treatment, all front deciduous teeth of the mandible and supernumerary teeth were removed, retained front teeth of the mandible were uncovered, orthodontic brackets were attached to them and therapy was started. After 2 months, the same procedure was performed in the maxilla. As a result of treatment, after 6 months, the front permanent teeth underwent eruption.
In 2013, Park et al. [14] described two CCD cases: a 12 year-old boy and a 14 year-old girl. The children had been assessed with pantomograms (panoramic radiograph) and cephalograms. The boy’s treatment plan included restorative treatment, removal of nine persistent deciduous teeth, surgical removal of seven supernumerary teeth, and removal of all permanent retained canines as their presence prevented the eruption of other retained, permanent teeth. The permanent teeth were observed for spontaneous eruption over the next 9 months. The lateral incisors of the mandible and upper right lateral incisor of the jaw did not erupt spontaneously, but were exposed surgically and attached to a gold chain joined to the jaw and mandible arches, for controlled eruption. A full upper and lower appliance was set up to align the arches. After achieving skeletal maturity at the age of 19, an osteotomy of the jaw was performed, to correct 6 mm in the sagittal dimension and a vertical jaw deficit. Treatment ended at the age of 24 with the infixing of crowns and bridges on implants. Analysis of superimposed, lateral cephalometric images before and after treatment showed a significant improvement in the sagittal relation, mainly in the ANB angle of overbite and overjet.
The girl’s treatment plan included extension of the jaw; Hyrax was fixed for 2 months and an 11 mm extension was achieved. Her persistent deciduous teeth were removed. Retained permanent teeth were surgically exposed, combined with a gold chain to provide controlled eruption. As a result, all of the teeth erupted after 11 months. Tooth 21 was removed due to having a very short root. Orthodontic treatment was completed after 14 months. A LeFort I osteotomy was performed at the age of eighteen. A tooth 21 was prosthodontically implanted. Comparison of the ANB angle of overbite and overjet before and after treatment showed a significant improvement in the sagittal relation.
In 2014, Bechtold et al. [15] described a 9 year-old boy with nineteen supernumerary teeth, a third skeletal class, and persistent deciduous teeth. A pantomogram, orthopantomogram, cephalometric scans in the lateral projection and CBCT were all performed. Treatment was begun with surgical exposure of the upper incisors at the age of nine and six months. One week after surgery, an orthodontic appliance with an extra rigid arch was fixed from the side of the vestibule. The appliance was attached to the exposed teeth. The orthodontic arch was attached to locks on the molars and canines. The seven hooks were fitted to the anterior vestibule segment of the orthodontic appliance to provide selective differentiation of direction of orthodontic forces along the arch. After 8 months, 4 incisors in the jaw erupted to a level at which the appliance could be removed.
Zhang et al., [16] described 2 cases of CCD: a 16 year-old girl and a 15 year-old boy, whose primary complaints were non-eruption of permanent incisor teeth. They shared similar features, including facial-cranial and dental abnormalities. The 16 year-old girl was given a cephalometric x-ray and a pantomogram, which showed five supernumerary teeth in the jaw and mandible, and root curvature in some teeth. The presence of a constricted arch of the jaw, and lateral and anterior cross-bite of a Class III occlusion, were found intraorally. Treatment was begun with surgical exposition of the crowns of the central incisors and the left lateral incisor of the jaw. Brackets were then fixed to the crowns and elastic traction was fitted. In the closed eruption technique, the elastic traction protruded through the mucous membrane and was connected to a removable hooking device. Orthodontic traction with alignment of the front teeth lasted 12 months. After 12 months, all of the front teeth had erupted; lateral cross-bite remained due to jaw hypoplasia. Continuation of orthodontic treatment assumed correction of the Class III occlusion.
The 15-year-old boy was found to have two supernumerary teeth, and so surgical removal of the retained teeth with removal of the supernumerary teeth was performed. After attaching orthodontic brackets to the surgically exposed retained teeth, orthodontic traction was begun immediately after the surgery. After 4 months, the incisor teeth of the jaw had erupted. Comparison of intraoral x-rays before and after treatment revealed a significant improvement in occlusion in the anterior segment. Continuation of orthodontic treatment included correction of the Class III occlusion.
3. Description of the orthodontic therapy of this author’s CCD case
The patient is a 12-year-old ZJ girl with CCD, diagnosed at age 6 from a clinical picture and radiological scans. According to the interview, she was born naturally in the 32nd week of pregnancy. The CCD was confirmed on the basis of genetic testing. The clinical picture of the patient is typical of CCD, with hypermobility of the arms (Figure 1), and a brachycephalic skull with prominent frontal bone (Figure 2).
Figure 1.

The patient’s arms hypermobility
Figure 2.

The patient’s brachycephalic skull.
There was no genetic history of the disease in the family. At the age of 12, Cone Beam Computed Tomography (CBCT) was performed (Figure 3) to determine the state of dentition, supernumerary teeth, their position, as well as the surgical plan for removal of the deciduous and supernumerary teeth.
Figure 3.

X-ray of the patient’s mouth.
Figure 4.

Close-up of the surgical treatment and corrective apparatus
12 supernumerary teeth were found: 6 in the jaw and 6 in the mandible. Surgical treatment began with the removal of the two upper deciduous incisors and two supernumerary teeth. Retained permanent incisors had orthodontic brackets fixed from the lip side, and orthodontic elastic traction was fitted. A closed eruption technique was used, the gingival patch was repositioned and stapled in such a way that the crowns with the brackets were not exposed, leaving the elastic traction to protrude through the mucous membrane. The removable loop apparatus was developed pre-operatively, the protruding elastic traction was fitted by the patient onto the loops. The appliance was used to bring the retained incisors to the correct position in the oral cavity, with the orthodontic traction initiated the same day.
While the retained teeth moved downward, the elastic traction was cut short to provide effective tooth eruption. Three months later, two supernumerary upper incisors, placed palatally from the extruded jaw incisors that had already been partially erupted, were removed. At present, the patient is in the active phase of bringing further teeth into the arch. However, during orthodontic therapy, clinically lowered sensitivity of the hearing was found, so the girl was referred for a hearing diagnostic to the Poznan University of Medical Sciences’ Department of Hearing Prosthetics.
An audiological interview revealed a problem with chronic inflammation of the middle ear and asymmetry of the paranasal sinuses. Following prior otoscopy and exclusion of inflammation of the middle ear, a full audiological diagnostic pathway was performed. In view of the age of the patient, a full range of objective audiometry was also performed: the recording of Auditory Brainstem Response (ABR) triggered by clicks; Distortion Product Otoacoustic Emissions testing (DPOAE); classical tympanometry (226 Hz); stapedius reflex measurements; wideband tympanometry in a range from 250 Hz to 8000 Hz, and pure tone audiometry 125-14,000 Hz.
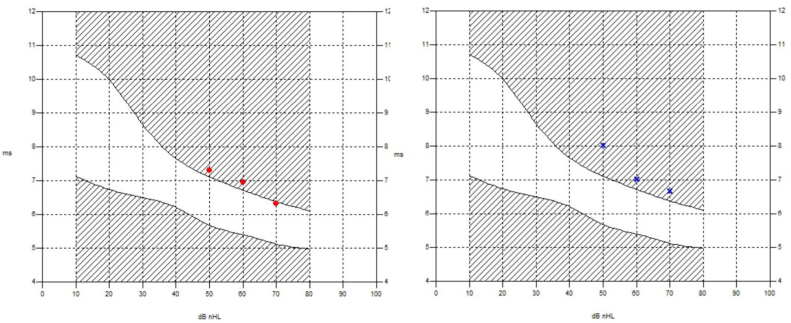
Analysis of ABR results indicated bilateral hearing loss at 50 dB nHL, with the wave V latency times indicating the coexistence of a conductive component (Figure 5).
Figure 5.
Wave V latency times, right and left ear.
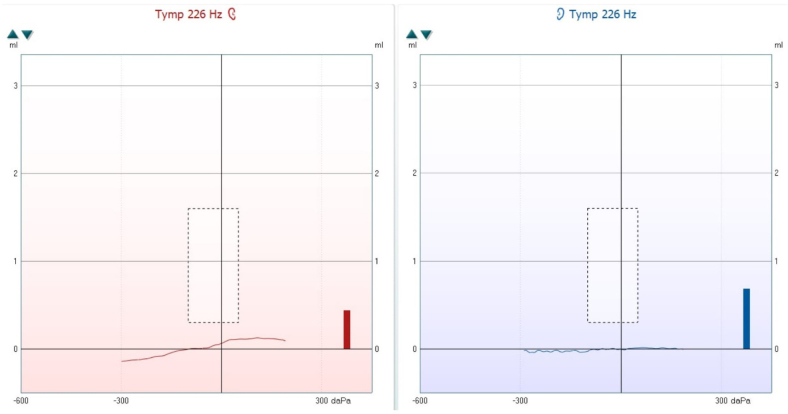
The impedance audiometry showed a decrease of eardrum mobility, with the impedance curves classified as Type B. This was confirmed by two clinical tests using a MADSEN Zodiac 901 and Interacoustics Titan. Stapedius reflexes were recorded in the right ear at 500 Hz 90 dB HL, 1 kHz at 95 dB HL, and 2 kHz at 90 dB HL. The reflex for the left ear was recorded classified as Type B (Figure 6).
Figure 6.
Results of classical tympanometry for 226 Hz, right and left ear.
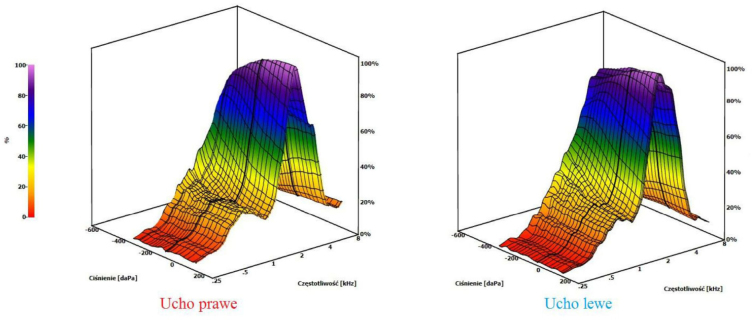
In addition to classical tympanometry, the patient was also screened for wideband tympanometry, which confirmed the previous results. Flat curves were obtained throughout the frequency range (Figure 7).
Figure 7.
Results of wideband tympanometry, right and left ear.
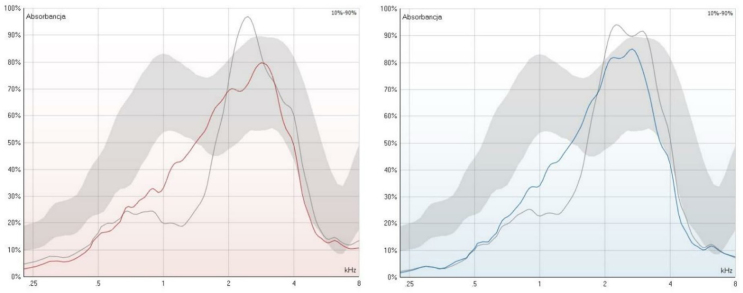
Absorbance, i.e. the ability of the hearing system to absorb sounds through the hearing system, is here seen to be lowered for low frequencies, and deviates from the norm (Figure 8).
Figure 8.
Results of absorbance measurement, right and left ear.
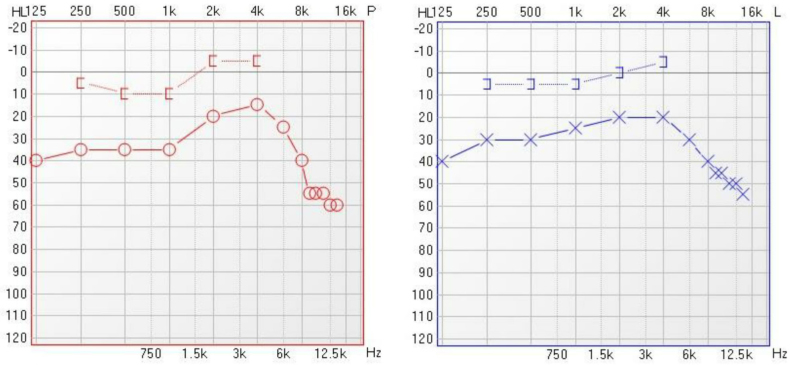
Distortion product otoacoustic emissions were recorded in the left ear only for high frequencies, i.e., above 2000 Hz, and in the right ear for both lower frequencies - 996 Hz and 1191 Hz, and for high frequencies of 2832 Hz. Pure tone audiometry confirmed the results of the objective testing, with a clear cochlear reserve in the range of 250-4000 Hz indicating conductive hearing loss. For frequencies above 8000 Hz, a noticeable drop in the auditory threshold was observed, reaching up to 60 dB HL for 14000 Hz (Figure 9).
Figure 9.
Results of pure tone audiometry, right and left ear.
Ethical approval
The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance the tenets of the Helsinki Declaration, and has been approved by the authors‘ institutional review board or equivalent committee.
Informed consent
Informed consent has been obtained from all individuals included in this study.
4. Discussion
In any single case of CCD, the triad of symptoms includes the occurrence of supernumerary teeth. As such, one of the basic problems in orthodontic therapy of CCD is their correct diagnosis and removal. It is worth noting that of the five reports described above, only in one publication [13] did the researchers use Cone Beam Computed Tomography to plan treatment. In this author’s case, the CCD treatment plan and surgical-orthodontic therapy was preceded by CBCT. It appears then, based on our own experience and observation of patients treated for congenital defects of the facial part of the skull, that this radiological examination should be a standard procedure. The surgical exposure of permanent retained teeth, and fitting of orthodontic brackets with elastic traction on the exposed crowns of incisors using the closed technique, is part of currently-used therapeutic procedures in CCD [9]. The difference lies in the orthodontic appliances used to expose the retained teeth. The use of both fixed [13,14] and removable appliances were described [12,15], and a removable device was used in our own case. However, it is important to emphasize the fact that in such therapy, working directly with the patient is indispensable, as such cooperation strongly affects the final result – the lifespan of the appliance and the patient’s fixing of the elastic traction on their own significantly affects the outcome of the therapy. When using a fixed appliance, it is possible to eliminate this dependency. Our case, of the 12 year-old girl, was based on very close cooperation with full understanding and commitment to the treatment of both the child and the parents.
The analysis of surgical-orthodontic procedures described by other authors includes only one report on the completed treatment, of two CCD cases [13], but no information was found on the need to pay attention to hearing diagnosis. This is in spite of the fact that the literature does indicate that patients with CCD have otolaryngological problems, including conductive or sensory-neural hearing loss [2,6,8]. Even so, there is no information in the literature that during orthodontic treatment any activities aimed at assessing the functioning of the auditory system in CCD patients was undertaken – none of the studies analyzed herein included an interview for hearing impairment, and the patients were not instructed or required to have a hearing test. This suggests that most authors do not pay attention to the problem of hearing impairment in this disease.
In comparison, the audiological results in our case seem to be typical of CCD. The hearing loss in our patient was not great enough to affect her cognitive and communicative abilities, and the child’s intellectual development is correct.Still, it is disturbing that the parents of the child were unable to provide any earlier audiological findings, despite the diagnosis of CCD in the fifth year of life with a recommendation for a hearing check due to inflammation of the middle ear. Fast diagnosis should result in effective introduction of both orthodontic therapy, and if necessary, audiological treatment. Hearing loss in CCD can occur in a variety of forms and to varying degrees, so it is not always a diagnostic and therapeutic priority. The hearing of our patient should continue to be regularly checked by specialists.
5. Conclusions
Cleidocranial dysplasia requires interdisciplinary treatment. It is important to remember to perform auditory check-ups between the many surgical and orthodontic interventions, which usually last a few years.
Footnotes
Conflict of interest
Conflict of interest statement: Authors state no conflict of interest
References
- [1].Hennekam R.C.M., Krantz I.D., Allanson J.E. Syndromes Affecting Bone: Skeletal Dysplasias with disproportionate short statuses in Gorlin’s Syndromes of the Head and Neck. Fifth. Oxford University Press; 2010. pp. 333–338. [Google Scholar]
- [2].Visosky A.M., Johnson J., Bingea B., Gurney T., Lalwani A.K.. Otolaryngological manifestations of cleidocranial dysplasia, concentrating on audiological findings. Laryngoscope. 2003;113:1508–1514. doi: 10.1097/00005537-200309000-00017. [DOI] [PubMed] [Google Scholar]
- [3].Bechtold T.E., Lee K., Park Y.C., Berneburg M., Göz G.R.. A Simultaneous Mobilization of Four Impacted Upper Incisors in a Case of an Adolescent Patient with Cleidocranial Dysplasia (CCD) Dentistry. 2014;4:2161–1122. doi: 10.4172/2161-1122.1000210. [DOI] [Google Scholar]
- [4].Cooper S.C., Flaitz C.M., Johnston D.A., Lee B., Hecht J.T.. A natural history of cleidocranial dysplasia. Am J Med Genet. 2001;104:1–6. doi: 10.1002/ajmg.10024. [DOI] [PubMed] [Google Scholar]
- [5].Segal N., Puterman M.. Cleidocranial dysplasia – Review with an emphasis on otological and audiological manifestations. Int J Pediatr Otorhinolaryngol. 2007;71:523–526. doi: 10.1016/j.ijporl.2006.11.021. http://dx.doi.org/10.1016/j.ijporl.2006.11.021 [DOI] [PubMed] [Google Scholar]
- [6].Candamourty R., Venkatachalam S., Yuvaraj V., Kumar G.S.. Cleidocranial dysplasia with hearing loss. J Nat Sci Biol Med. 2013;4:245–249. doi: 10.4103/0976-9668.107318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sękowska A., Dunin-Wilczyńska I., Chatas R.. Dysplazja obojczykowo-czaszkowa – wczesne postępowanie ortodontyczne. Dent Forum. 2012;20:119–123. [Google Scholar]
- [8].Kolokitha O.E., Ioannidou I.. A 13-year-old Caucasian boy with cleidocranial dysplasia: a case report. BMC Res Notes. 2013;6:6–8. doi: 10.1186/1756-0500-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Vij R., Batra P., Vij H.. Cleidocranial dysplasia: complete clinical, radiological and histological profiles. BMJ Case Rep. 2013;20 doi: 10.1136/bcr-2013-009015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lewandowski B., Martula-Gala K., Brodowski R., Zych B.. Multiple, supernumerary retained teeth in the course of cleidocranial dysplasia. A case report. Probl Med Wieku Rozwoj. 2015;19:503–507. [PubMed] [Google Scholar]
- [11].Verstrynge A., Carels C., Verdonck A., Mollemans W., Willems G., Schoenaers J.. Dentomaxillaire en-faciale problemen bij cleidocraniale dysplasie. Ned Tijdschr Tandheelkd. 2006;113:69–74. [PubMed] [Google Scholar]
- [12].Dhooge I., Lantsoght B., Lemmerling M., Vanzieleghem B., Mortier G.. Hearing loss as a presenting symptom of cleidocranial dysplasia. Otol Neurotol. 2001;22:855–857. doi: 10.1097/00129492-200111000-00024. [DOI] [PubMed] [Google Scholar]
- [13].Nagarathna C., Shakuntala B.S., Mathew S., Krishnamurthy N.H., Yumkham R.. Cleidocranial dysplasia presenting with retained deciduous teeth in a 15-year-old girl: a case report. J Med Case Rep. 2012;19:25. doi: 10.1186/1752-1947-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Park T.K., Vargervik K., Oberoi S.. Orthodontic and surgical management of cleidocranial dysplasia. Korean J Orthod. 2013;43:248–260. doi: 10.4041/kjod.2013.43.5.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bechtold T.E., Lee K.J., Park Y.C., Berneburg M., Göz G.R.. A simultaneous mobilization of four impacted upper incisors in a case of an adolescent patient with Cleidocranial Dysplasia (CCD) Dentistry. 2014;4(4):3. doi: 10.4172/2161-1122.1000210. [DOI] [Google Scholar]
- [16].Zhang C.Y., Si Y., Wang X.Z., Sun X.Y., Yan W.J., Zheng S.G.. Early dental treatments for patients with cleidocranial dysplasia. Chin J Dent Res. 2015;18:51–57. [PubMed] [Google Scholar]