Abstract
Since the use of antibiotics, bladder necrosis has become a rare condition. We report a case of bladder necrosis in a 90-year-old man following urinary retention. After insertion of a transurethral catheter (TUC), 2 L of urine was evacuated. In the following days, the TUC became intermittently blocked. Adequate bladder drainage could not be obtained despite intensive rinsing and placement of a suprapubic catheter. On surgical exploration necrosis of almost the entire bladder wall, except for the trigone, was encountered. Surgical debridement of the non-viable bladder wall without opening the abdominal cavity was conducted, and a TUC was placed in the Retzius cavity to ensure evacuation of urine. Since the patient was haemodynamically unstable, construction of a urinary diversion was waived and urinary drainage of the Retzius cavity by the TUC was accepted, resulting in adequate urinary drainage without compromising renal function.
Keywords: urology, urinary tract infections, urological surgery, hematuria, infections
Background
Necrosis of the bladder is a rare condition that varies from partial necrosis (mucosa and/or submucosa) to necrosis of the entire detrusor wall. In the literature it is mostly described as vesical necrosis, bladder necrosis and gangrenous cystitis.1–3 Factors that may contribute to bladder necrosis can be divided into indirect and direct factors.4 Indirect factors lead to impaired blood supply, such as pressure from the outside of the bladder (eg, pregnancy, prolonged labour), inside (overdistention of the bladder due to urinary retention), or blockage of the venous or arterial vessels (eg, emboli). Direct factors cause direct damage to the bladder wall, such as instillations with chemotherapeutic agents for the treatment of bladder cancer, radiation therapy and infections.
Although already rare in the past, to date, the incidence has decreased even more due to improved obstetrical care and better and earlier antibiotic treatment. The largest documented series originate from the 1930s and 1940s.5 After the 1980s only occasional cases have been reported.1–3 6–8 The symptoms of bladder necrosis are non-specific, such as pain in the lower abdomen, frequency, urgency, haematuria and pyuria, which hampers early diagnosis.
We report the case of a 90-year-old man with a massive chronic urinary retention in whom, after bladder drainage, recurrent blockade of the transurethral catheter (TUC) turned out to be caused by bladder necrosis. Additionally, we demonstrate that transurethral drainage of the Retzius cavity in a patient without a bladder, except for the trigone, can serve as a temporary solution in a fragile patient. Without performing a urinary diversion (Bricker deviation), the kidney function was preserved and no infectious complications occurred.
Case presentation
A 90-year-old man presented to the emergency room with progressive pain in the lower abdomen after constipation for 1 week and a period of frequency, urgency and urge incontinence. Three days before presentation, his urine became haemorrhagic.
His medical history included an ischaemic cerebrovascular accident, atrial fibrillation, intermittent claudication and lower urinary tract symptoms. Medication included acenocoumarol, verapamil and tamsulosin.
Physical examination revealed a painful lower abdomen and a full bladder, which was palpated up until the umbilicus. The patient did not have fever, and on digital rectal examination a small, firm prostate was palpated.
Serum creatinine was slightly elevated (152 µmol/L; normal 64–104 µmol/L), and serological infection parameters were high with a C reactive protein level of 459 mg/L (normal <8 mg/L) and a leucocyte count of 34.1×109/L (normal 4–10×109/L). A bladder scan revealed urinary retention, after which a TUC was inserted and 2 L of haemorrhagic urine was drained. The patient was then admitted to the hospital and a CT scan was performed. It is noteworthy that the initial bladder drainage did not relieve the abdominal pain.
Investigations
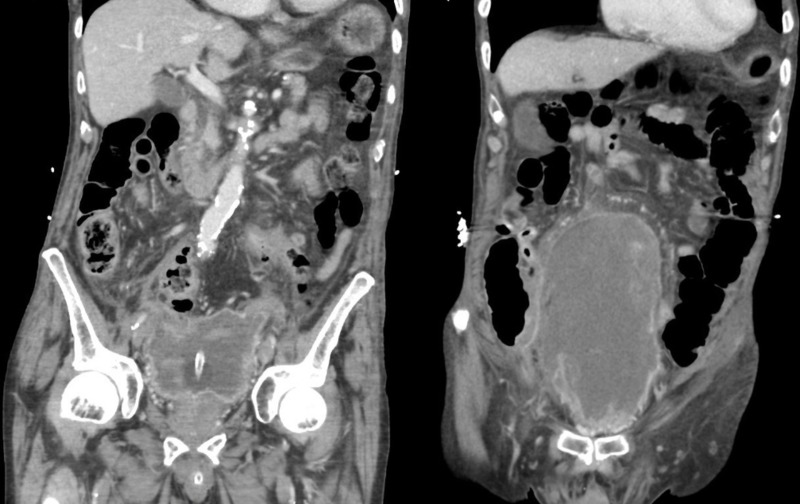
CT scan of the abdomen showed an abnormal layered aspect of the bladder wall (figure 1). The content of the bladder was inhomogeneous, suspicious for blood clots. At this point, failure to adequately drain the bladder was attributed to blockage of the TUC with debris and blood clots.
Figure 1.
CT scan with signs of white shreds in the bladder, in retrospect caused by necrotic fragments of the bladder wall.
On cystoscopy, which was performed to determine the cause of bleeding, the patient experienced severe urgency after instillation of 100 mL of saline. Visibility was poor due to debris and haematuria, and neither the bladder wall nor the ureteral orifices could be identified. The procedure was ceased, and an indwelling catheter was placed.
Treatment
Treatment consisted of continuous irrigation of the bladder and empirical broad-spectrum antibiotics pending urine cultures. During the admittance, the patient developed diarrhoea due to Clostridium infection, for which antibiotics (vancomycin) were administered. Thereafter, his clinical condition improved, leucocyte counts decreased and the urine became clear. On day 17 he was discharged with an indwelling catheter and normalised serology levels. Further examinations including a cystoscopy were planned at the outpatient clinic, but prior to the cystoscopy he had to be readmitted because of a blocked TUC. Even after several replacements, both transurethral and suprapubic bladder drainage remained inadequate. Saline could be instilled but could not be drained. Ultrasound revealed a floating white-grey shred that seemed to divide the supposed bladder in several compartments, and the TUC was visible in one of the compartments.
Because of the unexplained inadequate urinary drainage and clinical deterioration, surgical exploration was performed. Cavum Retzius space was opened without opening the abdominal cavity. A full-thickness necrosis of the entire bladder, except for the trigone, was encountered and the necrotic bladder was removed manually (figure 2). Since the patient was haemodynamically unstable, it was decided to end the surgery without performing a urinary diversion. A TUC and a suprapubic drain were placed to drain the Retzius cavity and two ureteral stents were inserted.
Figure 2.
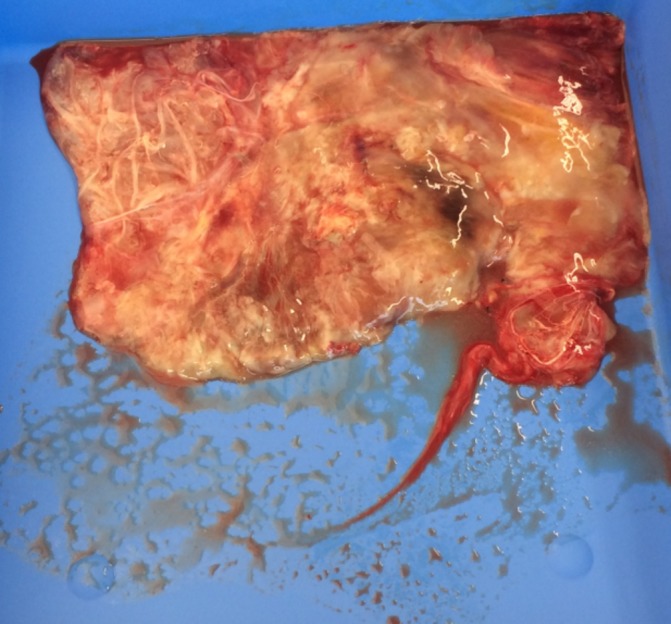
Removed necrotic bladder tissue.
Postoperatively, the patient was transferred to the intensive care unit because of haemodynamic instability and the need for respiratory support for a total of 2 days. He recovered quickly, and was discharged with an indwelling TUC in the Retzius cavity and normalised creatinine levels after 21 days.
Although an indwelling catheter in the cavum Retzius was initially considered a temporarily solution, it was eventually accepted as a definitive solution because the patient has no desire to undergo major surgery whatsoever.
Outcome and follow-up
After 6 months of follow-up, one complication occurred. The TUC got blocked, causing inflammation of the suprapubic region. Treatment consisted of replacement of the TUC and antibiotics during a few days of admission.
The indwelling catheter was replaced every 6–8 weeks, and 6 months after surgery our patient was still completely satisfied with this situation.
Discussion
Bladder necrosis is a rare condition, but is important to recognise as it may be life-threatening.9 Bladder necrosis may be difficult to diagnose due to its non-specific presentation. Yet, if there is an abnormal course of a common urological problem, uncommon diagnoses such as bladder necrosis should be kept in mind.
In the presented case, the most likely cause of bladder necrosis is chronic ischaemia due to overdistension of the bladder caused by urinary retention. It was initially not recognised, since symptoms of frequency, urgency and pain in the lower abdomen were attributed to chronic urinary retention. Furthermore, the slow recovery was attributed to the Clostridium infection, and it was assumed that the inadequate urinary drainage was caused by debris and blood clots. In retrospect, the bladder was probably already necrotic at that time.
In case of a full-thickness necrosis,7 which affects the entire bladder wall, necrotic fragments of the bladder wall may form a thickened floating mass in the Retzius cavity.8 10 Subsequently, saline can be instilled into the bladder but urinary drainage remains inadequate, as was the case in our patient. Hence, if there is unexplained inadequate drainage of urine by an indwelling catheter, the possibility of bladder necrosis should be kept in mind.
Treatment consists of extensive debridement and adequate urinary drainage. In the current case, we demonstrated that draining the Retzius cavity with a TUC may serve as a (temporary) solution in patients who are too frail to undergo major surgery. Furthermore, the clinical outcome without performing urinary diversion was acceptable for a longer period of time.
Learning points.
If there is unexplained inadequate drainage of urine by an indwelling catheter, uncommon diagnoses such as bladder necrosis should be kept in mind.
Treatment of bladder necrosis consists of thorough debridement and assuring urine drainage.
A closed Retzius cavity can function as a (temporary) urinary deviation without compromising renal function.
Footnotes
Contributors: JB: drafting of the manuscript. FHKO: acquisition of data and critical revision of the manuscript. EJHM: critical revision of the manuscript. JAN: critical revision of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ballas K, Rafailidis S, Pavlidis T, et al. Gangrenous cystitis. Int Urogynecol J Pelvic Floor Dysfunct 2007;18:1507–9. 10.1007/s00192-007-0430-9 [DOI] [PubMed] [Google Scholar]
- 2.Grossklaus DJ, Franke JJ. Vesical necrosis after hydrodistension of the urinary bladder in a patient with interstitial cystitis. BJU Int 2000;86:140–1. 10.1046/j.1464-410x.2000.01739.x [DOI] [PubMed] [Google Scholar]
- 3.Zabihi N, Allee T, Maher MG, et al. Bladder necrosis following hydrodistention in patients with interstitial cystitis. J Urol 2007;177:149–52. Discussion 52 10.1016/j.juro.2006.08.095 [DOI] [PubMed] [Google Scholar]
- 4.Cristol DS, Greene LF. Gangrenous cystitis. Surgery 1945;18:343–6. [Google Scholar]
- 5.Stirling WC, Hopkins G. Gangrene of the bladder. Review of two hundred seven cases; report of two personal cases1. The Journal of Urology 1934;31:517–25. [Google Scholar]
- 6.De Rosa A, Amer T, Waraich N, et al. Gangrenous cystitis in a 42-year-old male. BMJ Case Rep 2011;2011:bcr1120103526 10.1136/bcr.11.2010.3526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt SS. Gangrene of the bladder due to over distention. J Urol 1995;153:409–10. 10.1097/00005392-199502000-00037 [DOI] [PubMed] [Google Scholar]
- 8.Hinev A, Anakievski D, Krasnaliev I. Gangrenous cystitis: report of a case and review of the literature. Urol Int 2010;85:479–81. 10.1159/000321010 [DOI] [PubMed] [Google Scholar]
- 9.Devitt AT, Sethia KK. Gangrenous cystitis: case report and review of the literature. J Urol 1993;149:1544–5. 10.1016/S0022-5347(17)36442-X [DOI] [PubMed] [Google Scholar]
- 10.Tenenbaum J, Soifer S. Necrosis of the urinary bladder with report of three cases. The American Journal of Surgery 1937;38:378–83. 10.1016/S0002-9610(37)90452-5 [DOI] [Google Scholar]