Abstract
Purpose
The aim of this study is to generate reference values for anterior chamber morphometrics to facilitate the interpretation of anterior chamber images acquired with swept-source optical coherence tomography (SS-OCT) in a Caucasian population.
Materials and methods
Non-glaucomatous Caucasian subjects, who were newly referred to the outpatient department of the University Eye Clinic Maastricht UMC+, were asked to undergo anterior segment assessment with SS-OCT imaging prior to routine eye examination (including visual acuity and refractive error measurements, Goldmann applanation tonometry, slit lamp examination and funduscopy).
Results
A total of 647 Caucasian subjects, aged 40–80 years, were included. Mean age (± standard deviation) was 61.7±10.3 years, and 294 were male (45%). Mean refractive error was −0.63±3.17 D. OCT images and measurements were obtained in all cases. The mean temporal trabecular iris angle at 500 µm (TIA500) was 27.04°±12.04°, the mean nasal TIA500 was 27.43°±11.75°, the mean anterior chamber depth (ACD) was 2.75±0.39 mm and the mean lens vault (LV) was 0.44±0.30 mm. A smaller temporal TIA500, shallower ACD and higher LV were found in female and hyperopic subjects.
Conclusion
Reference values for anterior chamber morphometrics in Caucasians were generated, quantified and presented. These values offer tools for the interpretation of anterior segment images of Caucasians and differentiation between presumed mechanisms of angle closure.
Keywords: reference value, anterior chamber, optical coherence tomography, Caucasian
Introduction
An important goal in the prevention of primary angle closure and primary angle closure glaucoma (PACG) is early detection and monitoring of angle closure. The degree of angle closure can be detected by visualizing the anterior chamber angle, which is crucial for the correct diagnosis, prevention and timely treatment of PACG.1–5
Imaging techniques as tools to visualize the anterior chamber and detect angle closure are still relatively new. However, they are rapidly gaining popularity. In contrast to gonioscopy, anterior segment optical coherence tomography (AS-OCT) is a noncontact imaging technique. Anterior segment imaging offers the opportunity of detailed visualization of anterior segment structures together with tools for quantitative measurements of the anterior chamber angle and anterior chamber depth (ACD), that can be used for screening purposes to detect (the degree of) angle closure and also identify those who need further diagnostics with gonioscopy.6,7
Swept-source optical coherence tomography (SS-OCT), the second-generation AS-OCT, offers very detailed images of the anterior segment and anterior chamber angle, with almost no burden for the patient. Obtaining images is easy. However, reference values for Caucasians which would facilitate standardization of interpreting results are currently unavailable.
The purpose of this study was to generate reference values for SS-OCT anterior chamber morphometrics in a Caucasian population, to offer tools for the interpretation of anterior segment images in daily practice and that can be used as a basis for further use in research.
Materials and methods
This prospective study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the Maastricht University Medical Center+ (Maastricht, the Netherlands) institutional review board. Examinations of individuals participating in this study were carried out from April 2014 to April 2015.
Subjects
The Detection of Angle Closure (DTAC) study is a hospital-based study carried out in the outpatient clinic of the University Eye Clinic Maastricht UMC+ (the Netherlands), to detect the presence of angle closure in Caucasian patients with the use of SS-OCT.
Eligible subjects were consecutive new patients presenting at the outpatient clinic, meeting the following inclusion criteria: no history of eye disease(s), Caucasian race, age 40–80 years and willing and able to comply with scheduled visits and other study procedures. The principal investigator identified the origin of the subjects by self-reported Caucasian ancestry for both parents. For purposes of this study, the term Caucasian included only European-derived white people. If there was any doubt about the patient’s eligibility in regard to ancestry or if the questions could not be answered, the patients were not included in the study. After explaining the nature of the study (acquiring SS-OCT images), all subjects gave their signed written informed consent. A subject was excluded if there was a history of eye disease (ie, glaucoma, or any other significant eye disease) or any condition (ie, previous intraocular laser/incisional surgery or ophthalmological procedure or treatment), or an eye condition/abnormality that could affect the acquisition/reliability of measurements (eg, vitreous hemorrhage, uveitis, intraocular trauma, significant corneal opacity) or if the participant was unable to communicate properly or to understand instructions.
Included participants underwent a routine ophthalmic examination, including visual acuity and refractive error measurements, slit lamp examination, Goldmann applanation tonometry and funduscopy. Quantification of morphometric details of the anterior chamber was performed by SS-OCT (Casia SS-1000 OCT; Tomey, Nagoya, Japan).
Anterior chamber angle data recording and analysis
Anterior chamber data recording was carried out with SS-OCT. One image was taken of both eyes, with undilated pupils, in a darkened room, while subjects looked at the internal fixation light. SS-OCT was performed under standard dark room (<10 lux illumination) conditions for all image acquisitions. Images were acquired in the angle analysis mode. This scan mode consists of 128 radial B-scans, 16 mm long, automatically aligned on the corneal center. Each B-scan includes 512 A-scans. The measurement time in this scan mode is 2.4 seconds.
The anterior chamber and angle parameters were analyzed using the available software for SS-OCT (Version 6; Tomey). Image analysis was performed by a single investigator (HR) through manual placement of the iridocorneal angle tool at the scleral spur (reference point for the relative position of the trabecular meshwork) in the temporal and nasal angle (0°–180° meridian), after which the intrinsic software of the SS-OCT automatically calculated the trabecular iris angle at 500 µm (TIA500) and 750 µm, ACD and lens vault (LV) (Figure 1). The nasal and temporal angle values were used for anterior chamber angle analysis.
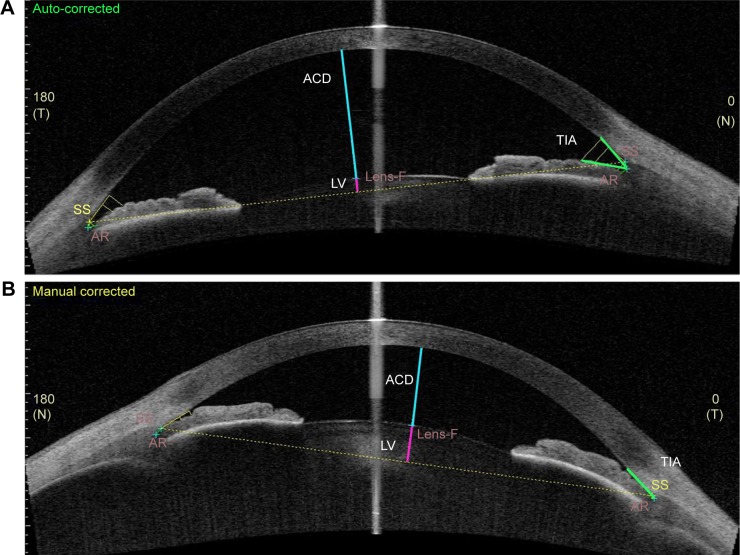
Figure 1.
Location of TIA, ACD and LV is shown in an SS-OCT image. The ICA tool is shown which had to be placed manually on the scleral spur by the operator which then displayed the lines measuring the anterior chamber morphometric data displayed in the tables. (A) An open anterior chamber. (B) Angle closure with shallow ACD. In both images, TIA is displayed in green, ACD in blue and LV in pink.
Abbreviations: TIA, trabecular iris angle; ACD, anterior chamber depth; LV, lens vault; SS-OCT, swept-source optical coherence tomography; ICA, iridocorneal angle; SS, scleral spur; AR, angle recess; N, nasal; T, temporal.
Analysis
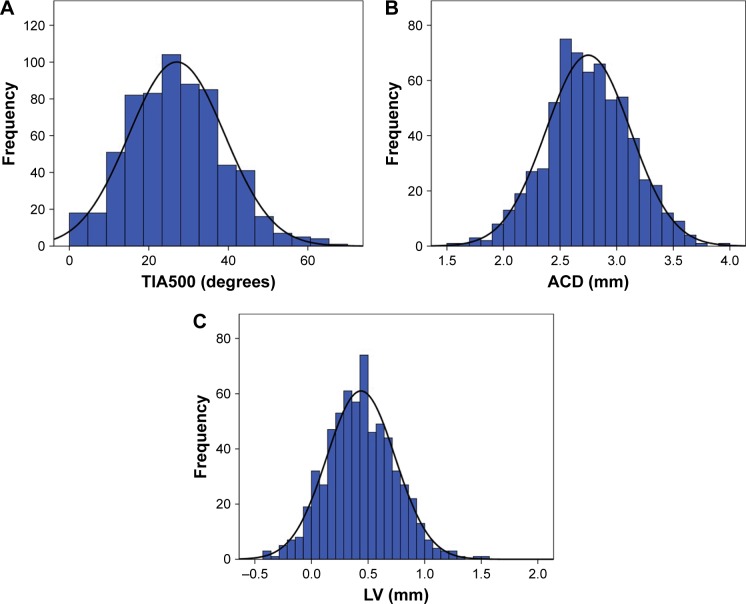
All data were analyzed using a statistical software package (SPSS version 23; IBM, Armonk, NY, USA). All available data were extracted from the analyses performed with SS-OCT. First, histograms were constructed and frequency analysis was performed to obtain information on distribution of the data (Figure 2). Descriptive statistical results were described as the mean ± standard deviation (SD) with the range and the lower 5th, 10th, 20th and 90th percentiles for TIA500 and ACD and with the 10th and higher 80th, 90th and 95th percentiles for LV.
Figure 2.
Distribution of the (A) TIA500, (B) ACD and (C) LV on the right phakic eyes.
Abbreviations: TIA, trabecular iris angle at 500 µm; ACD, anterior chamber depth; LV, lens vault.
All data are presented for the right phakic eyes. Because the TIA500, ACD and LV data all displayed a near-normal distribution, we used analysis of variance to show possible differences with age, gender and refractive error. The refractive error was divided in three groups to explore the anterior chamber data. The groups were defined as follows: myopia as mean spherical equivalent (SE) ≤−1 D, emmetropia as mean SE ≤1 D and >−1 D and hyperopia as mean SE >1 D.
Results
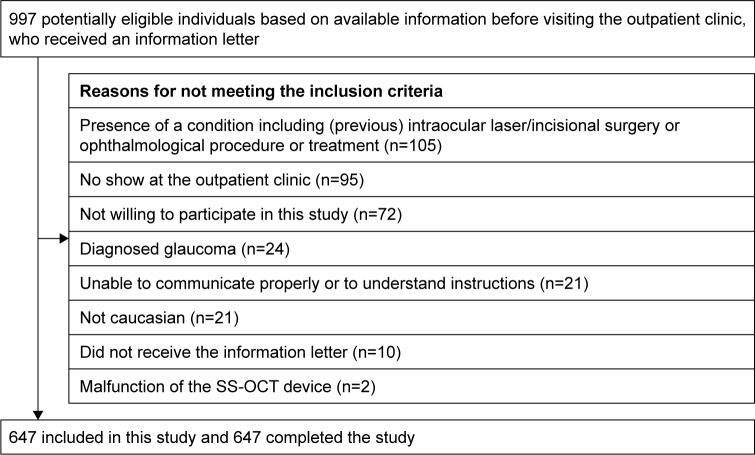
Since it was their first visit to our clinic, participating individuals were screened for eligibility based on information in the referral letter from the general practitioner, when available. There were 997 eligible individuals, who were invited to participate by an explanatory letter. When individuals visited the outpatient clinic for their scheduled appointment, inclusion and exclusion criteria were checked, and from these 997 individuals, 647 subjects were consecutively enrolled in this study; 350 individuals were excluded since they did not meet the inclusion criteria or did not want to participate (Figure 3). SS-OCT measurements were obtained for all 647 included individuals. The scleral spur and the anterior chamber angle were assessed and needed to be visible to meet the quality standards for further analysis. The scleral spur was identifiable in all SS-OCT images. No images had to be excluded for the reason of inadequate image quality or any other reason. A total of 647 SS-OCT images were used, in which the scleral spur was correctly marked.
Figure 3.
Flowchart of inclusion and exclusion of study participants.
Abbreviation: SS-OCT, swept-source optical coherence tomography.
Mean age was 62±10 years, 294 (45%) were male and mean refractive error (SE) was −0.63±3.17 D. For all participants, mean temporal TIA500 was 27.04°±12.04°, mean nasal TIA500 was 27.43°±11.75°, mean ACD was 2.75±0.37 mm and mean LV was 0.44±0.30 mm.
Tables 1 and 2 display the mean temporal and nasal TIA500, respectively, along with the SD, range and the lower limits (mm), that is, 5th, 10th, 20th and 90th percentile values, for the total population and separately for male and female subjects, different age groups and refractive error groups. The same parameters are displayed in Table 3 for ACD (mm). Table 4 displays the mean LV (mm), SD, range and 10th, 80th, 90th and 95th percentiles, since for LV the higher limits are of importance.
Table 1.
Temporal TIA500 in the right phakic eyes (SS-OCT)
| N (%) | TIA500 (degrees)
|
P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Range | 5th percentile | 10th percentile | 20th percentile | 90th percentile | |||
| Gender | 0.015 | ||||||||
| Male | 294 (45.4) | 28.30 | 11.40 | 0.0–62.6 | 10.3 | 14.0 | 17.8 | 43.6 | |
| Female | 353 (54.6) | 25.98 | 12.46 | 0.0–67.8 | 5.8 | 11.0 | 14.9 | 43.1 | |
| Age group (years) | 0.81 | ||||||||
| 40–49 | 102 (15.8) | 27.60 | 12.20 | 0.0–62.1 | 8.8 | 13.1 | 17.1 | 43.2 | |
| 50–59 | 160 (24.7) | 27.18 | 12.33 | 0.0–63.1 | 4.9 | 11.2 | 17.0 | 42.9 | |
| 60–69 | 213 (32.9) | 27.27 | 11.32 | 0.0–67.8 | 10.8 | 14.0 | 17.0 | 44.3 | |
| 70–79 | 172 (26.6) | 26.30 | 12.58 | 0.0–62.6 | 5.2 | 10.3 | 15.2 | 42.7 | |
| Refractive error | <0.01 | ||||||||
| Myopia | 182 (28.1) | 32.17 | 11.34 | 2.7–67.8 | 13.2 | 17.4 | 23.7 | 45.6 | |
| Emmetropia | 228 (35.2) | 25.92 | 11.98 | 0.0–63.1 | 6.4 | 11.6 | 16.6 | 41.7 | |
| Hyperopia | 154 (23.8) | 22.71 | 10.69 | 0.0–55.7 | 4.9 | 10.7 | 13.9 | 37.6 | |
| Total | 647 (100) | 27.04 | 12.04 | 0.0–67.8 | 8.8 | 12.5 | 16.8 | 43.8 | |
Note: Refractive error (SE) was defined as follows: myopia as mean SE ≤−1 D, emmetropia as mean SE ≤1 D and >−1 D and hyperopia as mean SE >1 D.
Abbreviations: TIA500, trabecular iris angle at 500 µm; SS-OCT, swept-source optical coherence tomography; SD, standard deviation; SE, spherical equivalent.
Table 2.
Nasal TIA500 in the right phakic eyes (SS-OCT)
| N (%) | TIA500 (degrees)
|
P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Range | 5th percentile | 10th percentile | 20th percentile | 90th percentile | |||
| Gender | 0.14 | ||||||||
| Male | 294 (45.4) | 28.17 | 11.62 | 0.0–60.2 | 9.9 | 13.3 | 18.0 | 43.3 | |
| Female | 353 (54.6) | 26.80 | 11.84 | 0.0–62.0 | 8.3 | 12.2 | 16.2 | 40.8 | |
| Age group (years) | 0.20 | ||||||||
| 40–49 | 102 (15.8) | 28.24 | 11.18 | 0.0–52.5 | 12.6 | 14.5 | 17.7 | 42.4 | |
| 50–59 | 160 (24.7) | 27.95 | 12.14 | 0.0–62.0 | 7.7 | 13.4 | 18.7 | 43.2 | |
| 60–69 | 213 (32.9) | 27.97 | 11.46 | 0.0–60.2 | 10.6 | 13.1 | 17.3 | 43.2 | |
| 70–79 | 172 (26.6) | 25.79 | 12.02 | 0.0–62.0 | 5.9 | 10.3 | 15.2 | 39.5 | |
| Refractive error | <0.01 | ||||||||
| Myopia | 182 (28.1) | 32.47 | 11.18 | 1.5–60.2 | 14.0 | 18.4 | 23.4 | 47.3 | |
| Emmetropia | 228 (35.2) | 26.54 | 11.36 | 0.0–62.0 | 7.7 | 11.7 | 16.3 | 40.0 | |
| Hyperopia | 154 (23.8) | 22.90 | 10.59 | 0.0–58.5 | 7.0 | 10.1 | 13.3 | 36.9 | |
| Total | 647 (100) | 27.43 | 11.75 | 0.0–62.0 | 9.0 | 12.7 | 17.3 | 42.7 | |
Note: Refractive error (SE) was defined as follows: myopia as mean SE ≤−1 D, emmetropia as mean SE ≤1 D and >−1 D and hyperopia as mean SE >1 D.
Abbreviations: TIA500, trabecular iris angle at 500 µm; SS-OCT, swept-source optical coherence tomography; SD, standard deviation; SE, spherical equivalent.
Table 3.
ACD in the right phakic eyes (SS-OCT)
| N (%) | ACD (mm)
|
P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Range | 5th percentile | 10th percentile | 20th percentile | 90th percentile | |||
| Gender | <0.01 | ||||||||
| Male | 294 (45.4) | 2.80 | 0.37 | 1.63–3.93 | 2.13 | 2.30 | 2.50 | 3.25 | |
| Female | 353 (54.6) | 2.70 | 0.37 | 1.58–3.70 | 2.10 | 2.23 | 2.42 | 3.20 | |
| Age group (years) | 0.01 | ||||||||
| 40–49 | 102 (15.8) | 2.83 | 0.34 | 1.92–3.55 | 2.29 | 2.41 | 2.52 | 3.29 | |
| 50–59 | 160 (24.7) | 2.79 | 0.30 | 1.73–3.68 | 2.17 | 2.31 | 2.47 | 3.30 | |
| 60–69 | 213 (32.9) | 2.76 | 0.37 | 1.81–3.70 | 2.15 | 2.27 | 2.45 | 3.23 | |
| 70–79 | 172 (26.6) | 2.65 | 0.38 | 1.58–3.93 | 2.03 | 2.14 | 2.34 | 3.10 | |
| Refractive error | 0.01 | ||||||||
| Myopia | 182 (28.1) | 2.92 | 0.34 | 1.98–3.93 | 2.40 | 2.45 | 2.62 | 3.33 | |
| Emmetropia | 228 (35.2) | 2.72 | 0.36 | 1.58–3.70 | 2.08 | 2.27 | 2.47 | 3.21 | |
| Hyperopia | 154 (23.8) | 2.59 | 0.35 | 1.63–3.57 | 2.02 | 2.15 | 2.26 | 3.03 | |
| Total | 647 (100) | 2.75 | 0.37 | 1.58–3.93 | 2.13 | 2.27 | 2.45 | 3.23 | |
Note: Refractive error (SE) was defined as follows: myopia as mean SE ≤−1 D, emmetropia as mean SE ≤1 D and >−1 D and hyperopia as mean SE >1 D.
Abbreviations: ACD, anterior chamber depth; SS-OCT, swept-source optical coherence tomography; SD, standard deviation; SE, spherical equivalent.
Table 4.
LV in the right phakic eyes (SS-OCT)
| N (%) | LV (mm)
|
P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Range | 10th percentile | 80th percentile | 90th percentile | 95th percentile | |||
| Gender | 0.02 | ||||||||
| Male | 294 (45.4) | 0.41 | 0.31 | −0.43 to 1.49 | 0.02 | 0.65 | 0.80 | 0.90 | |
| Female | 353 (54.6) | 0.46 | 0.30 | −0.20 to 1.52 | 0.06 | 0.71 | 0.87 | 0.95 | |
| Age group (years) | <0.01 | ||||||||
| 40–49 | 102 (15.8) | 0.34 | 0.27 | −0.43 to 1.03 | −0.01 | 0.61 | 0.71 | 0.74 | |
| 50–59 | 160 (24.7) | 0.39 | 0.30 | −0.42 to 1.24 | 0.02 | 0.62 | 0.81 | 0.90 | |
| 60–69 | 213 (32.9) | 0.43 | 0.29 | −0.30 to 1.49 | 0.06 | 0.68 | 0.80 | 0.90 | |
| 70–79 | 172 (26.6) | 0.54 | 0.30 | −0.23 to 1.52 | 0.21 | 0.80 | 0.93 | 1.03 | |
| Refractive error | <0.01 | ||||||||
| Myopia | 182 (28.1) | 0.30 | 0.28 | −0.43 to 1.15 | −0.06 | 0.52 | 0.69 | 0.76 | |
| Emmetropia | 228 (35.2) | 0.45 | 0.30 | −0.42 to 1.52 | 0.07 | 0.69 | 0.83 | 0.93 | |
| Hyperopia | 154 (23.8) | 0.58 | 0.27 | −0.23 to 1.31 | 0.24 | 0.80 | 0.92 | 0.99 | |
| Total | 647 (100) | 0.44 | 0.30 | −0.43 to 1.52 | 0.05 | 0.69 | 0.83 | 0.93 | |
Note: Refractive error (SE) was defined as follows: myopia as mean SE ≤−1 D, emmetropia as mean SE ≤1 D and >−1 D and hyperopia as mean SE >1 D.
Abbreviations: LV, lens vault; SS-OCT, swept-source optical coherence tomography; SD, standard deviation; SE, spherical equivalent.
The temporal TIA500 and ACD were smaller, whereas the LV was larger in female compared to male (P<0.05). In participants with hyperopia compared to those with emmetropia and myopia, temporal and nasal TIA500 and ACD were smaller and the LV was larger (P<0.01). With aging, ACD decreased and LV increased (P<0.01), although this result was not statistically significant for temporal and nasal TIA500 (Tables 1–4).
Discussion
To our knowledge, the DTAC study is the first to report reference values for anterior segment morphometrics assessed with SS-OCT in a large Caucasian population, solely from Dutch origin. Therefore, the study comprises a native homogenous population.
The University Eye Clinic Maastricht UMC+ is the largest eye hospital in the region and provides both academic eye care and basic regional eye care. The findings of our study may therefore reflect the real population and not only a subset of academic referrals.
AS-OCT seems a suitable technique to screen for angle closure and thus identify those who need further diagnostics with gonioscopy, thereby relieving the burden of performing gonioscopy in all glaucoma suspects.6,7 AS-OCT has been available since the last decade. SS-OCT is the second-generation OCT, with significant improvements over the first-generation AS-OCT (Visante; Carl Zeiss Meditec), which is a time-domain OCT (TD-OCT). Compared to TD-OCT, SS-OCT has a higher scanning speed (30,000 A-scans/s vs 2,000 A-scans/s) and a higher axial resolution (<10 µm vs 18 µm). The superior ease of use, low variability and possibility of quantification of the results of OCT devices compared to gonioscopy and higher resolution compared to TD-OCT promotes SS-OCT as a screening tool for anterior segment and angle assessment in daily ophthalmic practice. It must be noted that SS-OCT cannot replace gonioscopy as both methods have their own merits. Gonioscopy permits dynamic visualization and allows indentation testing, to differentiate appositional from synechial angle closure.8 These features are crucial for a correct diagnosis and cannot be offered by SS-OCT. But gonioscopy is rather difficult to perform, it requires contact with the eye and there is a learning curve for correct interpretation. Reproducibility and test–retest reliability of gonioscopy are low.9 All this makes gonioscopy an unpopular tool for angle assessment. Ophthalmologists do not perform gonioscopy on all (new) patients in current daily practice, and this may possibly lead to underdiagnosing angle closure.10,11 OCT seems a suitable technique to first screen for angle closure in new patients and thus identify those who will need further diagnostics with gonioscopy, thereby relieving the burden of performing gonioscopy in all new patients visiting the outpatient clinic.6,7 This study offers the first reference values for a Caucasian population. In a previous study by our group, SS-OCT demonstrated high intra- and interobserver reproducibility of angle analysis in Caucasian subjects.7 Park et al reported that AS-OCT has an excellent capability to discriminate between angle closure and open angles determined with gonioscopy (area under the curve: temporal angle opening distance at 500 µm [AOD500] =0.96, nasal AOD500 =0.99). This means that AS-OCT values could discriminate between angle closure and open angle, which was detected by gonioscopy. Park et al concluded that AS-OCT could be used as a screening method to detect angle closure.9
In recent studies that compared the angle landmarks obtained by TD-OCT and SS-OCT, a visualization of the scleral spur between 70% and 78.9% for TD-OCT12,13 and between 95% and 100% for SS-OCT14 was found. Cumba et al could not identify the scleral spur in 17 of 124 angles. However, it must be noted that 16 of these angles concerned the superior and inferior quadrants, which we did not assess in the present study.15 SS-OCT images were only assessed in the 0°–180° meridian. However, these nasal and temporal angles are the same angles as assessed with the Van Herick method that is commonly used as a quick screening tool for angle closure in daily practice. Measuring the anterior chamber angle in the superior and inferior quadrants is considered challenging, since it requires opening the eyelids without exerting inadvertent pressure on the eyeball (which would change the anterior segment anatomy). This was also confirmed by Cumba et al.15 Since our aim was to generate reference values for clinical use, we presented 5th, 10th and 20th percentile values for ACD and TIA, and 80th, 90th and 95th percentile values for LV. Our study used standardized protocols to obtain biometric measurements and refractive error, allowing comparison of our data with other populations.
Further research will be conducted (by our group) to analyze the correlation between proven risk factors for angle closure in Asians (ie, age), which are still unclear in the Caucasian population.
Acknowledgments
The authors received support from the following foundations: Glaucoomfonds, Oogfonds and Landelijke Stichting voor Blinden en Slechtzienden, which contributed through UitZicht. The funding organizations had no role in the design or conduct of this research. They provided unrestricted grants.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Wilensky JT, Kaufman PL, Frohlichstein D, et al. Follow-up of angle-closure glaucoma suspects. Am J Ophthalmol. 1993;115(3):338–346. doi: 10.1016/s0002-9394(14)73585-8. [DOI] [PubMed] [Google Scholar]
- 2.Thomas R, George R, Parikh R, Muliyil J, Jacob A. Five year risk of progression of primary angle closure suspects to primary angle closure: a population based study. Br J Ophthalmol. 2003;87(4):450–454. doi: 10.1136/bjo.87.4.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas R, Parikh R, Muliyil J, Kumar RS. Five-year risk of progression of primary angle closure to primary angle closure glaucoma: a population-based study. Acta Ophthalmol Scand. 2003;81(5):480–485. doi: 10.1034/j.1600-0420.2003.00135.x. [DOI] [PubMed] [Google Scholar]
- 4.Bonomi L, Marchini G, Marraffa M, et al. Epidemiology of angle-closure glaucoma: prevalence, clinical types, and association with peripheral anterior chamber depth in the Egna-Neumarket Glaucoma Study. Ophthalmology. 2000;107(5):998–1003. doi: 10.1016/s0161-6420(00)00022-1. [DOI] [PubMed] [Google Scholar]
- 5.Lowe RF. Primary angle-closure glaucoma. Prevention and early treatment. Isr J Med Sci. 1972;8(8):1362–1365. [PubMed] [Google Scholar]
- 6.Tan AN, Sauren LD, de Brabander J, et al. Reproducibility of anterior chamber angle measurements with anterior segment optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52(5):2095–2099. doi: 10.1167/iovs.10-5872. [DOI] [PubMed] [Google Scholar]
- 7.Römkens HC, Beckers HJ, Frusch M, Berendschot TT, de Brabander J, Webers CA. Reproducibility of anterior chamber angle analyses with the swept-source optical coherence tomography in young, healthy Caucasians. Invest Ophthalmol Vis Sci. 2014;55(6):3999–4004. doi: 10.1167/iovs.13-12904. [DOI] [PubMed] [Google Scholar]
- 8.Salim S. The role of anterior segment optical coherence tomography in glaucoma. J Ophthalmol. 2012;2012:476801. doi: 10.1155/2012/476801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park SB, Sung KR, Kang SY, Jo JW, Lee KS, Kook MS. Assessment of narrow angles by gonioscopy, Van Herick method and anterior segment optical coherence tomography. Jpn J Ophthalmol. 2011;55(4):343–350. doi: 10.1007/s10384-011-0036-0. [DOI] [PubMed] [Google Scholar]
- 10.Klein BE, Klein R, Sponsel WE, et al. Prevalence of glaucoma. The Beaver Dam Eye Study. Ophthalmology. 1992;99(10):1499–1504. doi: 10.1016/s0161-6420(92)31774-9. [DOI] [PubMed] [Google Scholar]
- 11.Wensor MD, McCarty CA, Stanislavsky YL, Livingston PM, Taylor HR. The prevalence of glaucoma in the Melbourne Visual Impairment Project. Ophthalmology. 1998;105(4):733–739. doi: 10.1016/S0161-6420(98)94031-3. [DOI] [PubMed] [Google Scholar]
- 12.Sakata LM, Lavanya R, Friedman DS, et al. Assessment of the scleral spur in anterior segment optical coherence tomography images. Arch Ophthalmol. 2008;126(2):181–185. doi: 10.1001/archophthalmol.2007.46. [DOI] [PubMed] [Google Scholar]
- 13.Wong HT, Lim MC, Sakata LM, et al. High-definition optical coherence tomography imaging of the iridocorneal angle of the eye. Arch Ophthalmology. 2009;127(3):256–260. doi: 10.1001/archophthalmol.2009.22. [DOI] [PubMed] [Google Scholar]
- 14.McKee H, Ye C, Yu M, Liu S, Lam DS, Leung CK. Anterior chamber angle imaging with swept-source optical coherence tomography: detecting the scleral spur, Schwalbe’s Line, and Schlemm’s Canal. J Glaucoma. 2013;22(6):468–472. doi: 10.1097/IJG.0b013e31824485fa. [DOI] [PubMed] [Google Scholar]
- 15.Cumba RJ, Radhakrishnan S, Bell NP, et al. Reproducibility of scleral spur identification and angle measurements using Fourier domain anterior segment optical coherence tomography. J Ophthalmol. 2012;2012:487309. doi: 10.1155/2012/487309. [DOI] [PMC free article] [PubMed] [Google Scholar]