Abstract
Depression and Obstructive sleep apnea (OSA) are the major associated comorbidities. OSA is a rapidly growing problem in the society that is connected to the rising rates of obesity; at the same time, the depression rate is also increasing day by day. Patients with OSA present with sleep problems, anxiety, and depressive symptoms, depressive patients can also present with the same symptoms. The quality of an individual's health can be improved by the early detection of the symptoms of overlapping OSA and depression. By addressing these issues early, the associated healthcare costs and burden can be reduced simultaneously.
Keywords: CPAP, Depression, OSA, Psychosocial, Sleep, Natriuretic peptide
Introduction
Many symptoms of depression and obstructive sleep apnea overlap, causing under-diagnosis of obstructive sleep apnea (OSA) in depressed patients. OSA patients can present with major depressive symptoms, but it is highly recommended that the primary care physician should determine the underlying cause of depression rather than simply diagnosing the patient as depressed. Patients with OSA have a higher prevalence of depression than the general population [1]. Major depressive disorder can be ruled out by presenting patients with different questionnaires e.g., the Beck depression inventory (BDI) [2] or the patient health questionnaire (PHQ-9) during primary health care services. The answers to these questionnaires should be analyzed along with the symptoms of patients and clinical evaluation [3]. The patient health questionnaire (PHQ-9) is a useful tool for the screening of depression. It is very easily implemented and can offer diagnostic results very quickly in the primary healthcare setting [4].
Depression and Clinical Outcomes
Depression is a risk factor for coronary artery disease [5]. Coronary artery disease (CAD) when it occurs simultaneously with depression has a greater morbidity and mortality risk in cardiac patients compared to patients with no depression [6]. Because depression is a risk factor for cardiac disease, controlling depression symptoms in patients diagnosed with mild depression can improve cardiac function; in severe depression, however, it has a worse prognosis [7]. In major depressive disorder (MDD), MRI results show that the volume of a patient's hippocampus decreases with chronic illness, not in the beginning of the depression, but significant decrease occurs after the onset of the disease [8]. In MDD, a negative emotional stimulus shows a more significantly negative response in depressed patients in regions of the brain that are involved in the processing of stimuli related to emotions compared to happy stimuli [9].
Depression and Obstructive Sleep Apnea
MDD carries with it an 18% prevalence of associated OSA; OSA has a 17.6% prevalence of MDD. There is a co-linear relationship between OSA and MDD. Both conditions present with common mood symptoms, anxiety, restlessness, fatigue, and poor concentration. In OSA patients, MDD must be ruled out before a treatment regimen can be implemented [10]. These co-related problems must be diagnosed properly to be treated effectively [11]. Some OSA patients present with the symptoms of depression, and these symptoms get better with the implementation of CPAP therapy [12]. Some OSA patients present with both OSA and depression symptoms; in these patients, both conditions need to be treated [13]. Older women with OSA present with greater decline in cognitive function than without OSA [14]. Patients with major symptoms of depression along with OSA respond to CPAP therapy and their depression symptoms gradually resolve; the patient's quality of life improves [15]. Many patients present with both OSA and major depression together [11]. The most common symptoms of OSA and depression are fatigue and sleep disturbance. Both of these problems can disguise each other because of their similar symptoms, but it is the responsibility of a clinician to treat the symptoms of a specific disease and determine the underlying cause [16]. Table 1 shows common sharing symptoms of MDD and OSA. Patients with OSA have a higher depression rate and thus have poor concentration and alertness during the day which can lead to traffic accidents and workplace accidents [17]. Figure 1 shows OSA causes sleep disturbance and could be the cause of depression, impaired psychosocial health and road traffic accidents due to sleepiness and improper judgment.
Table 1.
Association of OSA and Depression.
| Associated Disease | Symptoms | Diagnostic Criteria | Treatment |
|---|---|---|---|
| OSA | Disturbed sleep, obesity, snoring, anxiety. | Symptoms + PSG | Weight loss, CPAP |
| Depression | Disturbed sleep, weight gain/weight loss, sadness, impaired concentration, anhedonia, recurrent thoughts of death. (DSM-5) | Clinical Diagnosis | Antidepressants, ECT |
| OSA and Depression | Disturbed sleep, restlessness, anxiety, weight gain, tiredness, traffic accidents, impaired psychosocial health |
a) Electroconvulsive therapy (ECT).
b) Polysomnography (PSG).
c) Continuous Positive Airway Pressure (CPAP).
Figure 1.
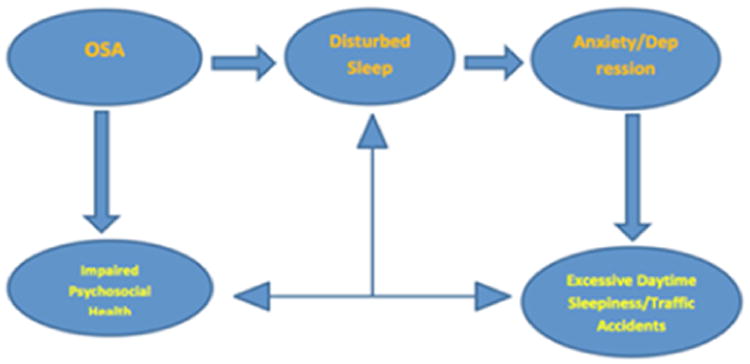
OSA and Its associated pathology.
There is more cognitive dysfunction noted in OSA and obese patients compared to the general population [18]. Patients who have been diagnosed with MDD who still show some residual symptoms of depression after treatment and who show some risk factors of OSA must be screened for OSA by using polysomnography (PSG). Patients who do not improve after taking antidepressant therapy and have symptoms of OSA should be screened for OSA and be treated with CPAP if OSA is diagnosed [19-21]. Patients who were diagnosed with MDD and treated by antidepressants but saw no improvement started to see their depression symptoms resolved when they began taking CPAP therapy [12]. Mood disorder and depressive symptoms associated with OSA can be improved by CPAP therapy, but the effect of treatment can take longer depending on the variations and severity of the mood symptoms. OSA patients need follow-up visits with their primary care physician to see the beneficial effects of CPAP therapy [22]. Depressive symptoms in OSA greatly improve after CPAP treatment. In OSA patients, hypoxemia treatment relieves sleep disturbance as well as psychological stress related to sleep apnea [23]. In MDD, CPAP therapy plays a vital role in treating residual symptoms of major depression if the patient has associated OSA as well [20]. In addition to CPAP therapy, reduction in BMI has a very beneficial effect on OSA and depressive symptoms [24]. In OSA patients neural injuries are noted in different parts of the brain compared to non-OSA patients. Depressed patients also show a loss of gray matter. Depression exacerbates the neural injuries more associated with OSA [25]. Depression and OSA are both conditions that decrease the quality of life of a patient compared to normal people [26].
Obstructive Sleep Apnea and Clinical Outcomes
OSA is a globally growing epidemic around the world. Apnea and hypoxemia episodes caused by the collapse of the upper respiratory tract occur during sleep and result in sleep disturbances [27]. Due to excessive daytime sleep, most OSA patients are not alert and demonstrate poor concentration, factors which could be the cause of severe mood disorders [17]. OSA is a major risk factor for CAD mortality and morbidity, especially in men 40 to 60 years of age [28]. OSA is also a major risk factor for CVD and stroke [29]. Moreover, OSA is highly associated with psychiatric disorders, predominantly MDD. Patients with psychiatric disorders, who are also showing symptoms of sleep disordered breathing, must be screened for OSA [30]. In OSA patients, neurocognitive function greatly improves after the treatment through continuous CPAP therapy, because sleep deprivation improves and the patient feels more rejuvenated and energetic, ultimately improving their quality of life [31]. OSA is an independent risk factor of CVD, hypertension, stroke, and EDS, obesity is a major cause of OSA; controlling obesity is the primary strategy to overcome and prevent OSA [32]. Severe OSA is related to a higher mortality [33]. OSA is related with excessive daytime sleepiness (EDS), which can cause preventable traffic accidents and injury [34]. CPAP therapy along with pharmacotherapy more effectively reduces hypertension compared to pharmacological treatment alone [35]. OSA causes severe morbidity and mortality. CPAP therapy greatly reduces these risks [36]. In OSA patients, treatment with CPAP therapy improves EDS and mood disorders; additionally, the traffic accident rate can be reduced [37]. Even the most seemingly insignificant single component of OSA, snoring, can play a significant part in causing CVD, hypertension, and cerebral infarction due to hypoxic episodes; treatment with CPAP can improve these associated conditions [38]. In older depressed patients, OSA should be ruled out before antidepressant pharmacotherapy is implemented because antidepressant medications do not help to treat the depressive symptoms that are produced by OSA. There is an additional need for CPAP therapy to follow up with response to the depressive symptoms of OSA [39]. OSA and depression must be diagnosed accurately so that their treatment strategy is not compromised. Undiagnosed sleep apnea can interfere with the proper treatment of a patient, and patient depressive symptoms cannot be addressed properly by using antidepressant pharmacotherapy [40]. Therefore, to effectively treat all facets of OSA, a comprehensive diagnosis should be sought.
Depression, Coronary Artery Disease and Obstructive Sleep Apnea
People who are depressed have a high risk of developing CAD [41,42]. MDD is a major risk factor of CAD [43]. MDD is also a major risk factor of persistent angina [44]. Depression is a major risk factor of angina, and depressive patients can show a poor prognosis even after revascularization surgery if the depression is not treated [45]. There is a release of inflammatory markers both in depression and CAD. These inflammatory makers are IL-1, IL-2, IL- 4, IL-6, IL-10, TNF-α [46-48]. This inflammatory process can lead to fibrinolysis and thrombolysis, which can also increase the risk of CAD [49]. Studies show that women who are depressed have an increased risk of CAD, and there should be a screening-as well as a treatment plan-for the patients that should be implemented by the health care providers and the government officials, even in the most remote areas of the country [50]. MDD is a major risk factor of CAD and should be screened at the earliest possible time, because without treatment of the depression, the prognosis of CAD would be poor. The screening of depression could be accomplished using Patient Health Questionare-9 (PHQ-9) after myocardial infarction [51]. CAD associated with OSA has better clinical outcomes after CPAP therapy. CPAP therapy greatly reduces N- Terminal Pro-brain Natriuretic Peptide (NT-pro BNP) and high levels of sensitive troponin T (hs-TropT) [52,53]. In MDD, patients sleep disturbance is greatly reduced by regular exercise, along with pharmacological treatment [54]. Regular exercise produces better clinical outcomes in both MDD and CAD [55].
Pharmacological Treatment of Depression: An Overview
Drugs designed to treat MDD are mainly MAO Inhibitors, SSRI, and tricyclic antidepressants [56]. Antidepressants are significantly used to treat MDD [57]. SSRI such as Vortioxetine improves cognitive unctioning in MDD Patients [58,59]. Monoamine oxidase inhibitors (MAO) are also used to treat MDD [60]. In MDD, SNRI-such as duloxetine can also be safely used, along with associated CVD [61]. For MDD associated with CVD, selective and reversible monoamine inhibitors are also commonly used drugs for treatment [62] SRI and serotonin reuptake inhibitors (SNRI) are also commonly used drugs for the treatment of MDD [63].
Antidepressants Overdose Effect on Cardiac Function
Overdoses of tricyclic antidepressants (Amitriptyline, Nortriptyline) have severe toxic side effects related to cardiac function, toxicity, seizures, hypotension, arrhythmias and refractory QRS complex widening [64-66]. Overdose of Serotonin reuptake inhibitors (SNRI) including venlafaxine, fluoxetine, fluvoxamine, paroxetine, and citalopram, can cause seizures, drowsiness, and hypotension. Overdose toxicity is also higher, with citalopram EKG findings showing a prolongation of the QT interval and a widening of QRS [67-71].
Psychosocial Health
In OSA patients, sleep disturbance causes significant psychological health impairment [72]. Studies have shown that female caregivers with OSA have more severe problems compared to non-caregivers, such as EDS, fatigue, and poor concentration [73]. In OSA and MDD, when sleep is disturbed, the patient's psychosocial health is also significantly disturbed. Due to EDS, fatigue and poor concentration, the individual cannot enjoy the time socially and feel abandoned and isolated from the society. To resolve these issues, the quality of sleep must be addressed properly in the health care system [74]. In older people, the incidence of OSA and depression are both higher. Advanced age, high BMI and EDS have increased risk factors for OSA and MDD in older people, and these patients present with poorer psychosocial health [75]. Individuals with eating disorders, especially binge eating disorder (BED), are more prone to obesity and OSA. Additionally, the depressive symptoms are higher in patients with associated BED and OSA compared to patients diagnosed with OSA alone. Patients with OSA and BED have poorer physical and mental health and their quality of life is decreased compared to patients without OSA or BED [76]. OSA patients have an impaired quality of life, poor participation in social life, more problems at work, poor concentration, and disturbed sleep. Not only is their mental health impaired, but they are also at higher risk for CVD [77]. OSA and impaired mental health are highly associated conditions [78]. OSA has a high comorbidity with MDD and both are more common in patients with poor family support, who live alone, and have a lack of social support [79]. In OSA patients, quality of life is low compared to that of the general population. However, the accurate diagnosis of OSA and proper treatment can improve each patient's quality of life by treating their depressive symptoms related to OSA [80].
OSA patients not only show impaired mental health but their physical health is also compromised compared to people without any sleep problems [81]. Patients with OSA have work related problems, especially in terms of executive tasks. The cognitive symptoms in OSA interfere significantly with a patient's work performance and daily life [82]. The quality of life in OSA patients is greatly compromised when cognitive symptoms are severe and predominant [83]. When a patient is diagnosed with OSA, associated anxiety and depressive symptoms are often also present. It is the responsibility of healthcare professionals to treat the psychological symptoms and to give complete and comprehensive treatment guidelines to patients. Adherence to the CPAP therapy can offer significant results and improve a patient's psychosocial health [84]. In OSA patients, cognitive symptoms especially mood symptoms greatly improve after treatment with CPAP therapy [13]. In OSA patients, treatment adherence is very important. If the underlying cause of the patient's OSA is obesity, then that patient should be educated and encouraged to lose weight, exercise, and work on diet control. If all other treatment measures fail, then surgical procedures should be performed. Patient self-motivation and family support are very necessary to improve each patient's physical and psychosocial health [85].
Discussion
It has been well established through various studies that there is as the association between OSA and depression. In order to effectively treat either related condition, primary care physicians must offer treatment solutions for both. Some of the manifestations of depression, including difficulty concentrating, feeling tired, decreased energy, and the feeling of not having had a restful sleep may also overlap with the features of OSA. It is fathomable that patients with OSA might wake up with an irritable or a depressed mood. These issues make it hard to separate the two conditions in terms of diagnosis and treatment. Using sedation, antidepressants, or hypnotics to treat insomnia related to depression may exacerbate OSA, which in turn may worsen the patient's mood. It makes a lot of clinical sense to screen patients with OSA for depression and reciprocally to evaluate patients who are depressed for OSA. Early detection of each disease and the development of prevention/treatment strategies can help reduce the risks associated with both diseases.
Conclusion
Patients with OSA have impaired health and their psychosocial health and daily performance also decrease. Because disturbed sleep can cause poor concentration, mood problems, anxiety, and MDD, these factors are also the part of poor daytime performance [86]. The medical therapy of choice for OSA is CPAP, but proper education and patient adherence to treatment is important for treatment to be successful and offer measurable results [87]. CPAP treatment has been shown to improve the depressive symptoms associated with OSA [88]. CPAP therapy also improves the quality of life for OSA patients [89]. If OSA does not improve with CPAP treatment, then surgical procedures are also advised to overcome the physical and depressive symptoms of OSA [90].
Acknowledgments
Funding: This work is supported by the following funding agencies: R25-HL105444 and R25-HL116378 (NHLBI); R01-MD007716 (NIMHD) to GJL. However, the funders had no role in study design, data collection and analysis.
Abbrevations
- BDI
Beck Depression Inventory
- PHQ
Patient Health Questionnaire
- OSA
Obstructive Sleep Apnea
- CAD
Coronary Artery Disease
- MDD
Major Depressive Disorder
- NT-Pro BNP
N- Terminal Pro-Brain Natriuretic Peptide
- hs-Trop T
High Levels of Sensitive Troponin T
- MAO
Monoamine Oxidase Inhibitors
- SNRI
Serotonin Reuptake Inhibitors
- BED
Binge Eating Disorder
- PSG
Polysomnography
Footnotes
Conflicts of Interest: None.
References
- 1.Ejaz SM, Khawaja IS, Bhatia S, Hurwitz TD. Obstructive sleep apnea and depression: a review. Innov Clin Neurosci. 2011;8(8):17–25. [PMC free article] [PubMed] [Google Scholar]
- 2.Lewis G, Kounali DZ, Button KS, Duffy L, Wiles NJ, et al. Variation in the recall of socially rewarding information and depressive symptom severity: a prospective cohort study. Acta Psychiatr Scand. 2017;135(5):489–498. doi: 10.1111/acps.12729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balasubramanian BA, Cohen DJ, Jetelina KK, Dickinson LM, Davis M, et al. Outcomes of Integrated Behavioural Health with Primary Care. J Am Board Fam Med. 2017;30(2):130–139. doi: 10.3122/jabfm.2017.02.160234. [DOI] [PubMed] [Google Scholar]
- 4.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferketich AK, Schwartzbaum JA, Frid DJ, Moeschberger ML. Depression as an antecedent to heart disease among women and men in the NHANES I study. National Health and Nutrition Examination Survey. Arch Intern Med. 2000;160(9):1261–1268. doi: 10.1001/archinte.160.9.1261. [DOI] [PubMed] [Google Scholar]
- 6.Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, et al. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66(3):305–315. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- 7.Lespérance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation. 2002;105(9):1049–1053. doi: 10.1161/hc0902.104707. [DOI] [PubMed] [Google Scholar]
- 8.MacQueen GM, Campbell S, McEwen BS, Macdonald K, Amano S, et al. Course of illness, hippocampal function, and hippocampal volume in major depression. Proc Natl Acad Sci USA. 2003;100(3):1387–1392. doi: 10.1073/pnas.0337481100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Surguladze S, Brammer MJ, Keedwell P, Giampietro V, Young AW, et al. A differential pattern of neural response toward sad versus happy facial expressions in major depressive disorder. Biol Psychiatry. 2005;57(3):201–209. doi: 10.1016/j.biopsych.2004.10.028. [DOI] [PubMed] [Google Scholar]
- 10.Peppard PE, Szklo-Coxe M, Hla KM, Young T. Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med. 2006;166(16):1709–1715. doi: 10.1001/archinte.166.16.1709. [DOI] [PubMed] [Google Scholar]
- 11.Ohayon MM. The effects of breathing-related sleep disorders on mood disturbances in the general population. J Clin Psychiatry. 2003;64(10):1195–200. doi: 10.4088/jcp.v64n1009. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz DJ, Kohler WC, Karatinos G. Symptoms of depression in individuals with obstructive sleep apnea may be amenable to treatment with continuous positive airway pressure. Chest. 2005;128(3):1304–1309. doi: 10.1378/chest.128.3.1304. [DOI] [PubMed] [Google Scholar]
- 13.Means MK, Lichstein KL, Edinger JD, Taylor DJ, Durrence HH, et al. Changes in depressive symptoms after continuous positive airway pressure treatment for obstructive sleep apnea. Sleep Breath. 2003;7(1):31–42. doi: 10.1007/s11325-003-0031-x. [DOI] [PubMed] [Google Scholar]
- 14.Yaffe K, Laffan AM, Harrison SL, Redline S, Spira AP, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011;306(6):613–619. doi: 10.1001/jama.2011.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sánchez AI, Buela-Casal G, Bermúdez MP, Casas-Maldonado F. The effects of continuous positive air pressure treatment on anxiety and depression levels in apnea patients. Psychiatry Clin Neurosci. 2001;55(6):641–646. doi: 10.1046/j.1440-1819.2001.00918.x. [DOI] [PubMed] [Google Scholar]
- 16.Harris M, Glozier N, Ratnavadivel R, Grunstein RR. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13(6):437–444. doi: 10.1016/j.smrv.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 17.Sforza E, de Saint Hilaire Z, Pelissolo A, Rochat T, Ibanez V. Personality, anxiety and mood traits in patients with sleep-related breathing disorders: effect of reduced daytime alertness. Sleep Med. 2002;3(2):139–145. doi: 10.1016/s1389-9457(01)00128-9. [DOI] [PubMed] [Google Scholar]
- 18.Aloia MS, Arnedt JT, Smith L, Skrekas J, Stanchina M, et al. Examining the construct of depression in obstructive sleep apnea syndrome. Sleep Med. 2005;6(2):115–121. doi: 10.1016/j.sleep.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Cai L, Xu L, Wei L, Sun Y, Chen W. Evaluation of the risk factors of depressive disorders comorbid with obstructive sleep apnea. Neuropsychiatr Dis Treat. 2017;13:155–159. doi: 10.2147/NDT.S122615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Habukawa M, Uchimura N, Kakuma T, Yamamoto K, Ogi K, et al. Effect of CPAP treatment on residual depressive symptoms in patients with major depression and coexisting sleep apnea: Contribution of daytime sleepiness to residual depressive symptoms. Sleep Med. 2010;11(6):552–557. doi: 10.1016/j.sleep.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 21.Hattori M, Kitajima T, Mekata T, Kanamori A, Imamura M, et al. Risk factors for obstructive sleep apnea syndrome screening in mood disorder patients. Psychiatry Clin Neurosci. 2009;63(3):385–391. doi: 10.1111/j.1440-1819.2009.01956.x. [DOI] [PubMed] [Google Scholar]
- 22.Saunamäki T, Jehkonen M. Depression and anxiety in obstructive sleep apnea syndrome: a review. Acta Neurol Scand. 2007;116(5):277–288. doi: 10.1111/j.1600-0404.2007.00901.x. [DOI] [PubMed] [Google Scholar]
- 23.Bardwell WA, Norman D, Ancoli-Israel S, Loredo JS, Lowery A, et al. Effects of 2-week nocturnal oxygen supplementation and continuous positive airway pressure treatment on psychological symptoms in patients with obstructive sleep apnea: a randomized placebo-controlled study. Behav Sleep Med. 2007;5(1):21–38. doi: 10.1207/s15402010bsm0501_2. [DOI] [PubMed] [Google Scholar]
- 24.Stubbs B, Vancampfort D, Veronese N, Solmi M, Gaughran F, et al. The prevalence and predictors of obstructive sleep apnea in major depressive disorder, bipolar disorder and schizophrenia: A systematic review and meta-analysis. J Affect Disord. 2016;197:259–67. doi: 10.1016/j.jad.2016.02.060. [DOI] [PubMed] [Google Scholar]
- 25.Cross RL, Kumar R, Macey PM, Doering LV, Alger JR, et al. Neural alterations and depressive symptoms in obstructive sleep apnea patients. Sleep. 2008;31(8):1103–1109. [PMC free article] [PubMed] [Google Scholar]
- 26.Akashiba T, Kawahara S, Akahoshi T, Omori C, Saito O, et al. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest. 2002;122(3):861–865. doi: 10.1378/chest.122.3.861. [DOI] [PubMed] [Google Scholar]
- 27.Epstein LJ, Kristo D, Strollo PJ, Jr, Friedman N, Malhotra A, et al. Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263–276. [PMC free article] [PubMed] [Google Scholar]
- 28.Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6(8):e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marshall NS, 1, Wong KK, Liu PY, Cullen SR, Knuiman MW, et al. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31(8):1079–1085. [PMC free article] [PubMed] [Google Scholar]
- 30.Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28(11):1405–1411. doi: 10.1093/sleep/28.11.1405. [DOI] [PubMed] [Google Scholar]
- 31.Canessa N, Castronovo V, Cappa SF, Aloia MS, Marelli S, et al. Obstructive sleep apnea: brain structural changes and neurocognitive function before and after treatment. Am J Respir Crit Care Med. 2011;183(10):1419–1426. doi: 10.1164/rccm.201005-0693OC. [DOI] [PubMed] [Google Scholar]
- 32.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217–1239. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 33.He J, Kryger MH, Zorick FJ, Conway W, Roth T. Mortality and apnea index in obstructive sleep apnea: experience in 385 male patients. Chest. 1988;94(1):9–14. [PubMed] [Google Scholar]
- 34.Young T, Palta M, Dempsey J, Skatrud J, Weber S, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 35.Phillips B. Sleep-disordered breathing and cardiovascular disease. Sleep Med Rev. 2005;9(2):131–140. doi: 10.1016/j.smrv.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 36.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 37.Yamamoto H, Akashiba T, Kosaka N, Ito D, Horie T. Long-term effects nasal continuous positive airway pressure on daytime sleepiness, mood and traffic accidents in patients with obstructive sleep apnoea. Respir Med. 2000;94(1):87–90. doi: 10.1053/rmed.1999.0698. [DOI] [PubMed] [Google Scholar]
- 38.Parish JM, Shepard JW., Jr Cardiovascular effects of sleep disorders. Chest. 1990;97(5):1220–1226. doi: 10.1378/chest.97.5.1220. [DOI] [PubMed] [Google Scholar]
- 39.Waterman L, Stahl ST, Buysse DJ, Lenze EJ, Blumberger D, et al. Self-reported obstructive sleep apnea is associated with nonresponse to antidepressant pharmacotherapy in late-life depression. Depress Anxiety. 2016;33(12):1107–1113. doi: 10.1002/da.22555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Björnsdóttir E, Benediktsdóttir B, Pack AI, Arnardottir ES, Kuna ST, et al. The prevalence of depression among untreated obstructive sleep apnea patients using a standardized psychiatric interview. J Clin Sleep Med. 2016;12(1):105–112. doi: 10.5664/jcsm.5406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Loomba RS, Aggarwal S, Arora R. Depressive symptom frequency and prevalence of cardiovascular diseases—Analysis of patients in the national health and nutrition examination survey. Am J Ther. 2015;22(5):382–387. doi: 10.1097/MJT.0000000000000043. [DOI] [PubMed] [Google Scholar]
- 42.Pelletier R, Bacon SL, Arsenault A, Dupuis J, Laurin C, et al. Relative associations between depression and anxiety on adverse cardiovascular events: does a history of coronary artery disease matter? A prospective observational study. BMJ Open. 2015;5(12):e006582. doi: 10.1136/bmjopen-2014-006582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bezgin CH, Bezgin T, Kesebir S. Temperament and Character Profiles and Psychiatric Comorbidities in Patients With Coronary Artery or Valvular Heart Disease: Relationship With Cardiac Disease Severity. J Clin Med Res. 2016;8(3):202–209. doi: 10.14740/jocmr2440w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jespersen L, Abildstrøm SZ, Hvelplund A, Prescott E. Persistent angina: highly prevalent and associated with long-term anxiety, depression, low physical functioning, and quality of life instable angina pectoris. Clin Res Cardiol. 2013;102(8):571–581. doi: 10.1007/s00392-013-0568-z. [DOI] [PubMed] [Google Scholar]
- 45.Hayek S, Ko Y, Awad M, Del Mar SA, Ahmed H, et al. Depression and chest pain in patients with coronary artery disease. International journal of cardiology. 2017;230:420–426. doi: 10.1016/j.ijcard.2016.12.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Maes M. Evidence for an immune response in major depression: a review and hypothesis. Prog Neuropsychopharmacol Biol Psychiatry. 1995;19(1):11–38. doi: 10.1016/0278-5846(94)00101-m. [DOI] [PubMed] [Google Scholar]
- 47.Tajfard M, Latiff LA, Rahimi HR, Mouhebati M, Esmaeily H, et al. Serum inflammatory cytokines and depression in coronary artery disease. Iran Red Crescent Med J. 2014;16(7):e17111. doi: 10.5812/ircmj.17111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tiemeier H, Hofman A, Van Tuijl HR, Kiliaan AJ, Meijer J, et al. Inflammatory proteins and depression in the elderly. Epidemiology. 2003;14(1):103–107. doi: 10.1097/00001648-200301000-00025. [DOI] [PubMed] [Google Scholar]
- 49.Malan L, Mashele N, Malan NT, Harvey BH, Potgieter JC, et al. Depression symptoms facilitated fibrinolytic dysregulation and future coronary artery disease risk in a black male cohort: the sympathetic activity and ambulatory blood pressure in Africans study. J Cardiovasc Nurs. 2017;32(4):401–408. doi: 10.1097/JCN.0000000000000358. [DOI] [PubMed] [Google Scholar]
- 50.Najafipour H, Banivaheb G, Sabahi A, Naderi N, Nasirian M. Prevalence of anxiety and depression symptoms and their relationship with other coronary artery disease risk factors: A population-based study on 5900 residents in Southeast Iran. Asian J Psychiatr. 2016;20:55–60. doi: 10.1016/j.ajp.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 51.DiSante JL, Bires AM, Cline TW, Waterstram-Rich K. An Analysis of the Prevalence of Depression Post-Myocardial Infarction. Crit Care Nurs Q. 2017;40(2):124–136. doi: 10.1097/CNQ.0000000000000149. [DOI] [PubMed] [Google Scholar]
- 52.Strehmel R, Valo M, Teupe C. Natriuretic Peptide and High-Sensitive Troponin T Concentrations Correlate with Effectiveness of Short-Term CPAP in Patients with Obstructive Sleep Apnea and Coronary Artery Disease. Clin Med Insights Circ Respir Pulm Med. 2016;10:33–39. doi: 10.4137/CCRPM.S40939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Valo M, Wons A, Moeller A, Teupe C. Markers of Myocardial Ischemia in Patients With Coronary Artery Disease and Obstructive Sleep Apnea: Effect of Continuous Positive Airway Pressure Therapy. Clin Cardiol. 2015;38(8):462–468. doi: 10.1002/clc.22419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rethorst CD, Sunderajan P, Greer TL, Grannemann BD, Nakonezny PA, et al. Does exercise improve self-reported sleep quality in non-remitted major depressive disorder? Psychol Med. 2013;43(4):699–709. doi: 10.1017/S0033291712001675. [DOI] [PubMed] [Google Scholar]
- 55.Peterson JC, Charlson ME, Wells MT, Altemus M. Depression, coronary artery disease, and physical activity: how much exercise is enough? Clin Ther. 2014;36(11):1518–1530. doi: 10.1016/j.clinthera.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Farvolden P, Kennedy SH, Lam RW. Recent developments in the psychobiology and pharmacotherapy of depression: optimising existing treatments and novel approaches for the future. Expert Opin Investig Drugs. 2003;12(1):65–86. doi: 10.1517/13543784.12.1.65. [DOI] [PubMed] [Google Scholar]
- 57.Rosenblat JD, Kakar R, McIntyre RS. The Cognitive Effects of Antidepressants in Major Depressive Disorder: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Int J Neuropsychopharmacol. 2016;19(2) doi: 10.1093/ijnp/pyv082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Frampton JE. Vortioxetine: A Review in Cognitive Dysfunction in Depression. Drugs. 2016;76(17):1675–1682. doi: 10.1007/s40265-016-0655-3. [DOI] [PubMed] [Google Scholar]
- 59.McIntyre RS, Florea I, Tonnoir B, Loft H, Lam RW, et al. Efficacy of Vortioxetine on Cognitive Functioning in Working Patients With Major Depressive Disorder. J Clin Psychiatry. 2017;78(1):115–121. doi: 10.4088/JCP.16m10744. [DOI] [PubMed] [Google Scholar]
- 60.Hamon M, Blier P. Monoamine neurocircuitry in depression and strategies for new treatments. Prog Neuropsychopharmacol Biol Psychiatry. 2013;45:54–63. doi: 10.1016/j.pnpbp.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 61.Wernicke J, Lledó A, Raskin J, Kajdasz DK, Wang F. An Evaluation of the Cardiovascular Safety Profile of Duloxetine. Drug Saf. 2007;30(5):437–455. doi: 10.2165/00002018-200730050-00007. [DOI] [PubMed] [Google Scholar]
- 62.Deshwal S, Di Sante M, Di Lisa F, Kaludercic N. Emerging role of monoamine oxidase as a therapeutic target for cardiovascular disease. Curr Opin Pharmacol. 2017;33:64–69. doi: 10.1016/j.coph.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 63.Dold M, Kautzky A, Bartova L, Rabl U, Souery D, et al. Pharmacological treatment strategies in unipolar depression in European tertiary psychiatric treatment centers-A pharmacoepidemiological cross-sectional multicenter study. Eur Neuropsychopharmacol. 2016;26(12):1960–1971. doi: 10.1016/j.euroneuro.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 64.Amiri H, Zamani N, Hassanian-Moghaddam H, Shadnia S. Cardiotoxicity of tricyclic antidepressant treated by 2650 mEq sodium bicarbonate: A case report. JRSM Cardiovasc Dis. 2016;5 doi: 10.1177/2048004016682178. 2048004016682178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dianat S, Zarei MR, Hassanian-Moghaddam H, Rashidi-Ranjbar N, Rahimian R, et al. Tricyclic antidepressants intoxication in Tehran, Iran: Epidemiology and associated factors. Hum Exp Toxicol. 2010;30(4):283–288. doi: 10.1177/0960327110371701. [DOI] [PubMed] [Google Scholar]
- 66.Liebelt EL, Ulrich A, Francis PD, Woolf A. Serial electrocardiogram changes in acute tricyclic antidepressant overdoses. Crit Care Med. 1997;25(10):1721–1726. doi: 10.1097/00003246-199710000-00024. [DOI] [PubMed] [Google Scholar]
- 67.Cooke MJ, Waring WS. Citalopram and cardiac toxicity. Eur J Clin Pharmacol. 2013;69(4):755–760. doi: 10.1007/s00228-012-1408-1. [DOI] [PubMed] [Google Scholar]
- 68.Jasiak NM, Bostwick JR. Risk of QT/QTc prolongation among newer non-SSRI antidepressants. Ann Pharmacother. 2014;48(12):1620–1628. doi: 10.1177/1060028014550645. [DOI] [PubMed] [Google Scholar]
- 69.Jimmink A, Caminada K, Hunfeld NG, Touw DJ. Clinical toxicology of citalopram after acute intoxication with the sole drug or in combination with other drugs: overview of 26 cases. Ther Drug Monit. 2008;30(3):365–371. doi: 10.1097/FTD.0b013e3181379ef6. [DOI] [PubMed] [Google Scholar]
- 70.Lung DD, Wu AH, Gerona RR. Cardiotoxicity in a citalopram and olanzapine overdose. J Emerg Med. 2013;45(4):554–558. doi: 10.1016/j.jemermed.2013.04.033. [DOI] [PubMed] [Google Scholar]
- 71.Tarabar AF, Hoffman RS, Nelson Citalopram overdose: late presentation of torsades de pointes (TdP) with cardiac arrest. J Med Toxicol. 2008;4(2):101–105. doi: 10.1007/BF03160963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Macey PM, Woo MA, Kumar R, Cross RL, Harper RM. Relationship between obstructive sleep apnea severity and sleep, depression and anxiety symptoms in newly-diagnosed patients. PLoS One. 2010;5(4):e10211. doi: 10.1371/journal.pone.0010211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Song Y, Washington DL, Yano EM, McCurry SM, Fung CH, et al. Caregiving-Related Sleep Problems and Their Relationship to Mental Health and Daytime Function in Female Veterans. Behav Sleep Med. 2016;3:1–12. doi: 10.1080/15402002.2016.1228640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Stepnowsky CJ, Palau JJ, Zamora T, Ancoli-Israel S, Loredo JS. Fatigue in sleep apnea: The role of depressive symptoms and self-reported sleep quality. Sleep Med. 2011;12(9):832–837. doi: 10.1016/j.sleep.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 75.Fawale MB, Ibigbami O, Ismail I, Mustapha AF, Komolafe MA, et al. Risk of obstructive sleep apnea, excessive daytime sleepiness and depressive symptoms in a Nigerian elderly population. Sleep Sci. 2016;9(2):106–111. doi: 10.1016/j.slsci.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sockalingam S, Tehrani H, Taube-Schiff M, Van Exan J, Santiago V, et al. The relationship between eating psychopathology and obstructive sleep apnea in bariatric surgery candidates: A retrospective study. Int J Eat Disord. 2017;50(7):801–807. doi: 10.1002/eat.22701. [DOI] [PubMed] [Google Scholar]
- 77.Liu D, Myles H, Foley DL, Watts GF, Morgan VA, et al. Risk factors for Obstructive Sleep Apnea are prevalent in people with psychosis and correlate with impaired social functioning and poor physical health. Front Psychiatry. 2016;7:139. doi: 10.3389/fpsyt.2016.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.James BO, Inogbo CF, 1, Archibong AO. Risk of obstructive sleep apnoea syndrome among in-patients at a neuropsychiatric hospital in Nigeria: a short report. Afr Health Sci. 2015;15(3):967–971. doi: 10.4314/ahs.v15i3.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dai Y, Li X, Zhang X, Wang S, Sang J, et al. Prevalence and predisposing factors for depressive status in chinese patients with obstructive sleep apnoea: a large-sample survey. PLoS One. 2016;11(3):e0149939. doi: 10.1371/journal.pone.0149939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Isidoro SI, Salvaggio A, Lo Bue A, Romano S, Marrone O, et al. Effect of obstructive sleep apnea diagnosis on health related quality of life. Health Qual Life Outcomes. 2015;13(1):68. doi: 10.1186/s12955-015-0253-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hayley AC, Williams LJ, Venugopal K, Kennedy GA, Berk M, et al. The relationships between insomnia, sleep apnoea and depression: findings from the American National Health and Nutrition Examination Survey, 2005-2008. Aust N Z J Psychiatry. 2015;49(2):156–170. doi: 10.1177/0004867414546700. [DOI] [PubMed] [Google Scholar]
- 82.Vaessen TJ, Overeem S, Sitskoorn MM. Cognitive complaints in obstructive sleep apnea. Sleep Med Rev. 2015;19:51–58. doi: 10.1016/j.smrv.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 83.Lee IS, Bardwell W, Ancoli-Israel S, Natarajan L, Loredo JS, et al. The Relationship between psychomotor vigilance performance and quality of life in obstructive sleep apnea. J Clin Sleep Med. 2011;7(3):254–260. doi: 10.5664/JCSM.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shapiro AL. Anxiety in middle-aged men with obstructive sleep apnea: State of the science. J Am Assoc Nurse Pract. 2014;26(12):689–695. doi: 10.1002/2327-6924.12118. [DOI] [PubMed] [Google Scholar]
- 85.Usmani ZA, Chai-Coetzer CL, Antic NA, McEvoy RD. Obstructive sleep apnoea in adults. Postgrad Med J. 2012;89(1049):148–56. doi: 10.1136/postgradmedj-2012-131340. [DOI] [PubMed] [Google Scholar]
- 86.Cheshire K, Engleman H, Deary I, Shapiro C, Douglas NJ. Factors impairing daytime performance in patients with sleep apnea/hypopnea syndrome. Arch Intern Med. 1992;152(3):538–541. [PubMed] [Google Scholar]
- 87.Sanders MH, Redline S. Obstructive sleep apnea/hypopnea syndrome. Current Treatment Options in Neurology. 1999;1(4):279–290. doi: 10.1007/s11940-999-0018-4. [DOI] [PubMed] [Google Scholar]
- 88.Werli KS, Otuyama LJ, Bertolucci PH, Rizzi CF, Guilleminault C, et al. Neurocognitive function in patients with residual excessive sleepiness from obstructive sleep apnea: a prospective, controlled study. Sleep Med. 2016;26:6–11. doi: 10.1016/j.sleep.2016.06.028. [DOI] [PubMed] [Google Scholar]
- 89.Diamanti C, Manali E, Ginieri-Coccossis M, Vougas K, Cholidou K, et al. Depression, physical activity, energy consumption, and quality of life in OSA patients before and after CPAP treatment. Sleep Breath. 2013;17(4):1159–1168. doi: 10.1007/s11325-013-0815-6. [DOI] [PubMed] [Google Scholar]
- 90.Dixon JB, O'Brien PE. Changes in comorbidities and improvements in quality of life after LAP-BAND placement. Am J Surg. 2002;184(6):S51–S54. doi: 10.1016/s0002-9610(02)01181-9. [DOI] [PubMed] [Google Scholar]


