Abstract
The Centers for Disease Control and Prevention’s Screen for Life: National Colorectal Cancer Action Campaign (SFL) is one of the longest running national multimedia campaigns to promote colorectal cancer screening. Since its inception in 1999, no study has quantified the benefits and costs of SFL. We modeled the impact of SFL campaign on screening rates, assuming that the effect size would range from 0.5% to 10% of the unscreened population exposed to the campaign in the last 14 years. Given the estimated benefits of the campaign and costs, we calculated the cost per person screened (2012 dollars). We hypothesize that if 0.5% of the population exposed to campaign messages were screened for colorectal cancer, an additional 251,000 previously unscreened individuals would be screened. The average cost of SFL per person screened would be $2.44. On the other hand, if 10% of the population exposed to campaign messages were screened, an additional 5.01 million individuals would be screened. The average cost per person screened would be $0.12. Results indicate that SFL improves screening rates at a relatively low cost per person screened. The findings in this study provide an important starting point and benchmark for future research efforts to determine the benefits and costs of health communication campaigns to promote cancer prevention.
Keywords: colorectal cancer, cancer prevention and control, costs, benefits, mass media, health communication, health promotion
INTRODUCTION
Colorectal cancer (CRC) is the second leading cause of cancer deaths in the United States among cancers that affect both men and women and the third most commonly diagnosed cancer in adults aged 50 years and older (U.S. Cancer Statistics Working Group, 2009). Each year, more than 135,000 people are diagnosed with CRC and more than 51,000 die from this cancer (U.S. Cancer Statistics Working Group 2009). Despite strong scientific evidence that CRC screening reduces the burden of illness and recommendations from the U.S. Preventive Services Task Force (USPSTF; 2011) that adults ages 50 to 75 years receive regular screening tests, screening rates remain low. In recent studies, CRC screening rates are estimated to range from 54.5% to 65.4% (Centers for Disease Control and Prevention [CDC], 2011; Shapiro et al., 2012) and lag behind screening rates for breast and cervical cancers, which are 72.4% and 83.0%, respectively (CDC, 2010). The federal government has undertaken a number of initiatives to promote CRC screening (Colorectal Cancer Control Program). Recently, the CDC launched a population-based Colorectal Cancer Control Program (http://www.cdc.gov/cancer/crccp/index.htm) designed to provide screening and promote activities to increase CRC screening rates in the population. In 2000, the U.S. Congress designated March as “National Colorectal Cancer Awareness Month” to increase public awareness about the disease and encourage CRC screening among persons 50 years and older. This followed the March 1999 launch of CDC’s Screen for Life: National Colorectal Cancer Action Campaign (SFL), a multimedia initiative to increase knowledge and promote CRC screening (CDC, 2012).
Since the launch of the SFL campaign, studies have reported on the development, implementation, and dissemination of campaign materials to target populations (Cooper et al., 2005; Jorgensen, Gelb, Merritt, & Seeff, 2001; Lengerich, Rubio, Brown, Knight, & Wyatt, 2012; Vanderpool & Coyne, 2006; Ward, Coffey, Lengerich, & Piccinin, 2006). During this period, no study has quantified the potential benefits and costs of the campaign in reaching and encouraging target populations to be screened. The cost of cancer screening promotion activities have rarely been factored into estimates of the effectiveness or cost-effectiveness of screening programs. Omission of promotional costs in the estimation of cost-effectiveness of CRC screening may provide an incomplete account of resources expended on CRC screening and potentially may result in the underestimation of intervention costs. The purpose of this study was to quantify the potential benefits and costs associated with screening uptake among eligible U.S. adults resulting from exposure to SFL campaign messages.
MATERIALS
Overview of the SFL Campaign
SFL is a national multimedia campaign that was developed by the CDC and launched in March 1999 by the U.S. Department of Health and Human Services (CDC, 2012). The goals were to (a) promote CRC screening, (b) inform and educate men and women 50 years and older about the importance of having regular CRC screening tests as recommended by the USPSTF (2011), and (c) communicate how CRC screening saves lives through early detection of cancer and by finding precancerous polyps that can be removed before they become cancerous (Rex, Johnson, Lieberman, Burt, & Sonnenberg, 2000).
The campaign is based on extensive research, including over 200 focus groups in more than 30 cities across the United States. The SFL uses social cognitive theory and the theory of planned behavior as the primary foundation to guide both the development and evaluation of activities (Glanz, Lewis, & Rimer, 1997). Furthermore, other aspects of the study such as cancer screening and economic costs are supported by strong theoretical foundations (Eddy, 1980; Gold, Siegel, Russel, & Weinstein, 1996). Since the campaign’s launch, its messages have been included in a wide variety of materials, including brochures, fact sheets, posters, broadcast and print public service announcements (PSAs), digital media, and out-of-home advertising. The TV PSAs are distributed to more than 1,000 TV stations in all 210 U.S. designated media markets, including national networks and regional cable systems. The radio PSAs are distributed nationwide to nearly 1,200 radio stations. The print PSAs are distributed to nearly 2,000 magazines and 6,000 daily and weekly newspapers nationwide. The campaign’s out-of-home displays are available in many public places, such as airport and shopping mall dioramas; as advertisements in transit stations; on trains and buses; in transit shelters; in elevator video monitors; and other venues. The campaign also maintains a robust website and a presence on social media channels such as Facebook and YouTube.1 To further maximize exposure and increase awareness of CRC screening to the target population, the campaign includes professional actors, actresses, and well-known public figures (e.g., a news-woman and a former U.S. Surgeon General) as spokes-persons in PSAs. Most campaign materials are available in both English and Spanish.
Measuring Impact and Estimating Population Screened Through Exposure to the SFL Campaign
According to previous studies of the impact of mass media campaigns (Cram et al., 2003; Hornik, 2002; Myhre & Flora, 2000; Randolph & Viswanath, 2004; Sequist, Franz, & Ayanian, 2010; Snyder, 2007; Snyder & Hamilton, 2002), the necessary conditions for successful public health preventive campaigns to have substantial effects in the target population are (a) widespread dissemination of campaign materials, (b) high saturation through constant PSAs, (c) novel placement spots and diversity of PSAs to different subgroups of the target population, (d) endurance of the campaign to ensure that the exposure time is long enough to change people’s behavior, and (e) having a celebrity and/or public figure spokesperson for the campaign. The SFL campaign meets all these criteria. Because we were unable to estimate the impact of SFL directly, we modeled the impact of the campaign using a range of effect sizes obtained from prior studies of the impact of public health media campaigns (Cram et al., 2003; Sequist et al., 2010; Snyder, 2007). We assumed that the effect size (i.e., the proportion of the target population exposed to the campaign who are screened as a direct result of the campaign) would range from a minimum of 0.5% to a maximum of 10% (Cram et al., 2003; Sequist et al., 2010; Snyder, 2007) of unscreened persons exposed to the campaign in the past 14 years (i.e., 1999–2012). Using the assumed effect size and other data obtained from the literature, we estimated the benefits of SFL defined as the incremental population screened resulting from exposure to campaign messages.
Estimating Intermediate Outcome of the Campaign Measured by Incremental Population Screened
We estimated the number of persons who did not receive a CRC screening test over the period 1999 to 2012 based on (a) the total average U.S. population age 50 to 80 years from 1999 to 2012, which was about 86 million (U.S. Census Bureau, Population Division, 2012), (b) the proportion of the population that is already adhering to CRC screening recommendations, which was reported to be 58.3% (range: 50.0% to 70%; Shapiro et al., 2012); and (c) the proportion of the population that has already received a CRC screening test. We assume that 60% (range: 54.5% to 65.4%) of persons in the target age range were screened and the remainder were unscreened (CDC, 2011; Shapiro et al., 2012). We estimated the impact of the SFL campaign on the number of persons screened by applying the effect size, 0.5% to 10%, to the baseline estimate of the unscreened population.
Estimating Cost per Person Screened Due to the SFL Campaign
We estimated the cost per person screened based on the total cost of the campaign from 1999 to 2012. Total costs include the direct cost and the value of in-kind services donated to the campaign. The direct costs include costs incurred in developing and testing campaign messages and creative approaches for all TV, radio, video, and print PSAs. It includes costs for developing out-of-home displays and patient materials such as posters, fact sheets, brochures, and airport dioramas. The direct cost of the campaign also includes costs for professional consultation, formative research activities, travel to and from study sites, supplies, and other consumables.
The indirect cost category includes the value of time for public figures who donated their services as spokes-persons and are featured in the campaign PSAs and the value of time and placements donated to the campaign by local, regional, and national media outlets for PSAs and out-of-home displays. To measure the value of these in-kind donated services, we used the equivalent market value reported for each element of the campaign. The equivalent market value was obtained from the campaign administrator at CDC and was defined as the amount of money CDC would have paid to hire celebrity spokespersons and purchase airtime and space if these campaign-related advertising placements were not donated. This approach provides an accurate estimate of the total campaign cost and is recommended by the U.S. Panel on Cost-Effectiveness (Gold et al., 1996).
We adjusted costs to 2012 U.S. dollars using the all-item consumer price index (U.S. Bureau of Labor Statistics, 2012). We estimated the cost per person exposed to campaign messages at any time during the past 14 years, for various levels of the campaign’s effect size.
RESULTS
If 0.5% of the target population exposed to campaign messages were screened as a result of the exposure, an additional 251,000 persons would have been screened over the period 1999–2012. If the effect size was 10%, an additional 5.01 million persons would have received screening during this time period as a result of the campaign.
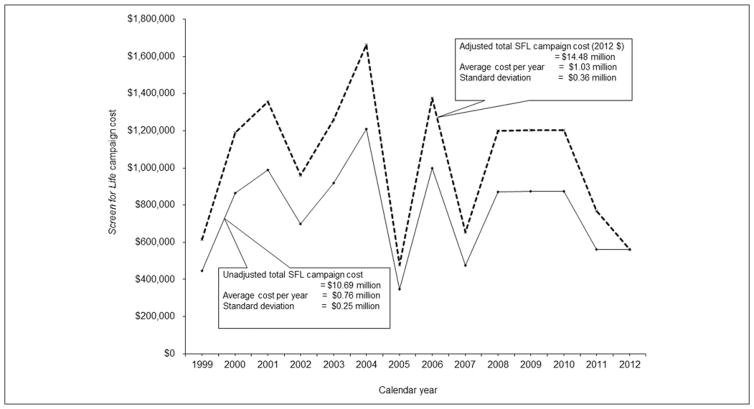
Figure 1 presents the adjusted and unadjusted direct cost of the campaign over 14 years. The total direct cost of SFL was $14.48 million (2012 dollars), or $1.03 million per year, with a standard deviation (SD) of $0.36 million. These costs varied considerably from year to year.
FIGURE 1.
Trends in the Costs of the Screen for Life Campaign 1999–2012
The total value of in-kind donated services to the campaign was $147.78 million, with an average of $10.56 million and an SD of $6.73 million (Table 1). The value of in-kind donated services represented 86% of the total cost of the campaign. As mentioned earlier, in-kind donated services to the campaign include a broad variety of media channels. Among these channels, the total value of donated TV airtime was the highest, estimated to be $86.56 million, with an annual average cost of $6.18 million and an SD of $2.72 million. The total value of donated patient educational materials was the lowest, estimated to be $12.18 million, with an annual average cost was $0.87 million and an SD of $1.23 million (Table 1).
TABLE 1.
Estimated Mean and Median Costs of Screen for Life Campaign by Different Media Channels, 1999–2012a
| Cost in Million, $ | |||||
|---|---|---|---|---|---|
|
| |||||
| Television | Patient Educational Materials | Radio | Out-of-Home Display | Total Value of In-Kind Donated Services | |
| No. of years | 14 | 14 | 6b | 6c | |
| Total cost | 86.56 | 12.18 | 19.11 | 29.94 | 147.78d |
| Mean | 6.18 | 0.87 | 3.18 | 4.99 | 10.56 |
| SD | 2.72 | 1.23 | 1.88 | 4.92 | 6.73 |
| 95% Confidence interval | [4.76, 7.61] | [0.22, 1.52] | [1.68, 4.69] | [1.05, 8.93] | [7.032, 14.08] |
| Median | 6.12 | 0.35 | 2.86 | 3.78 | 9.59 |
| 25th percentiles | 4.18 | 0.02 | 2.44 | 1.09 | 4.49 |
| 75th percentiles | 7.55 | 0.78 | 4.47 | 8.36 | 16.36 |
The costs reported in this table represent the value of in-kind services donated to the campaign by individuals and private organizations. These costs were converted to 2012 dollars using the Consumer Price Index.
This media channel was not funded in the following years: 1999–2001, 2003–2005, and 2011–2012.
This media channel was not funded in the following years: 1999–2001, 2003–2004, 2006, 2008, and 2012.
This value represents 86.33% of the total cost of the campaign.
Based on the adjusted direct cost of the campaign, the average annual cost per person screened was estimated to be $2.44 (SD of $0.90) when the campaign effect size was 0.5% (Table 2). The estimated average annual cost per person screened was only $0.24 (SD of $0.09) and $0.12 (SD of $0.04) when the campaign effect size was 5% and 10%, respectively. In Table 2 we also present the median cost per person screened, the associated interquartile range, and the average annual cost per person screened using both the direct cost and the cost of in-kind donated services. As expected, the average annual cost per person screened using the combined costs was substantially higher compared with the direct cost alone.
TABLE 2.
Estimated Mean and Median Cost per Person Screened due to Screen for Life (SFL) Campaign by Percentage of Campaign Effect Size, 1999–2012a
| Campaign Effect Size | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| 0.5% | 5% | 10% | ||||
|
|
|
|
||||
| SFL Campaign Cost Only | SFL Campaign Cost and the Value of In-Kind Donated Services | SFL Campaign Cost Only | SFL Campaign Cost and the Value of In-Kind Donated Services | SFL Campaign Cost Only | SFL Campaign Cost and the Value of In-Kind Donated Services | |
| No. of years | 14 | 14 | 14 | 14 | 14 | 14 |
| Mean | 2.44 | 26.57 | 0.24 | 2.66 | 0.12 | 1.33 |
| SD | 0.90 | 15.21 | 0.09 | 1.52 | 0.04 | 0.76 |
| 95% Confidence interval | [1.96, 2.91] | [18.60, 34.54] | [0.20, 0.29] | [1.86, 3.45] | [0.10, 0.15] | [0.93, 1.73] |
| Median | 2.55 | 22.63 | 0.26 | 2.26 | 0.13 | 1.13 |
| 25th percentiles | 1.64 | 14.74 | 0.16 | 1.47 | 0.08 | 0.74 |
| 75th percentiles | 3.10 | 38.41 | 0.31 | 3.84 | 0.16 | 1.92 |
All costs were adjusted to 2012 dollars.
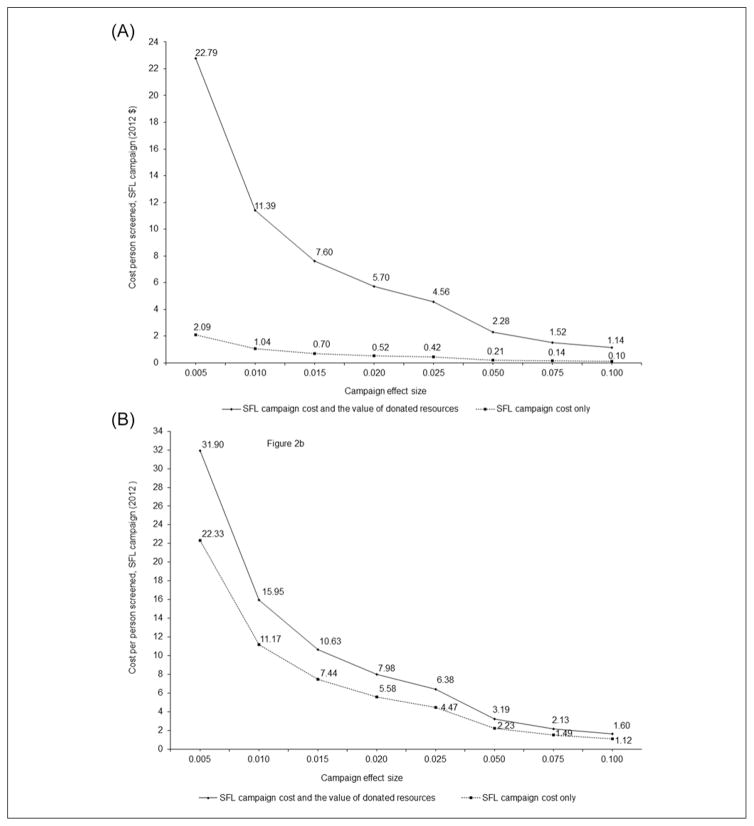
The estimated average annual cost per person screened for different values of the CRC screening compliance rate (50% and 70%) are presented in Figures 2A and B, respectively. When the compliance rate was 50% (the lowest rate) and the campaign effect size was 0.5% (also the lower rate), the estimated direct cost per person screened was $2.09. The direct and indirect cost per person screened was $22.79 (Figure 2A). Conversely, when the compliance rate was low and the effect size was high (10%), the estimated direct cost per person screened was $0.10. When the compliance rate was 70% (the higher rate) and the campaign effect size was 0.5% (the lower rate), the estimated direct cost per person screened was $22.33. When the compliance rate was high and the effect size was also high, the estimated direct cost per person screened was $1.12 (Figure 2B).
FIGURE 2.
(A) Estimated Average Annual Cost per Person Screened Due to Screen for Life Campaign by Different Values of Effect Size When the Compliance of Colorectal Cancer Screening Rates Was 50.0% (Lower Value); (B) Estimated Average Annual Cost per Person Screened Due to Screen for Life Campaign by Different Values of Effect Size When the Compliance of Colorectal Cancer Screening Rates Was 70.0% (Higher Value)
DISCUSSION
Under reasonable assumptions about the effectiveness of the SFL campaign, we estimate that the direct cost per additional person screened was $0.12 to $2.44. These figures represent 0.02% to 0.5% of the cost of a colonoscopy to the Medicare program (approximately $500; Zauber 2010). On average, persons screened via colonoscopy gain an extra 0.1 life years at a cost of $690 in direct medical costs (Zauber, 2010). Assuming that the cost per additional person screened is $2.44, then the cost per life year gained of the SFL program is $6,924 ([$690 + $2.44] ÷ 0.1). This calculation assumes that there are people who would not have been screened in the absence of the SFL campaign. For a “price” of $2.44, these persons received a service that costs $690 and provides 0.1 life year. The cost per life year gained is well below thresholds typically used to assess whether services are cost-effective. We have chosen to illustrate cost-effectiveness using cost and effectiveness figures for colonoscopy because it is one of the most commonly used CRC screening modalities in the United States. However, many other commonly used screening tests are at least as cost-effective as colonoscopy (Zauber, 2010).
The SFL campaign is one of the longest running national health communication campaigns to promote CRC. Because of its longevity, it is difficult to estimate its impact on screening rates because there are so many other factors that could have accounted for increases in screening rates since its inception. Unfortunately, most mass media campaigns to promote cancer screening are not subject to rigorous evaluation (Sabatino et al., 2012). Going forward, it is important that newly initiated health promotion campaigns are designed with more comprehensive evaluation components. Given the lack of estimates of the direct impact of the SFL, we were very cautious in estimating the potential benefits. The results presented in this article will be useful for planning health communication campaigns to promote colorectal and other cancers.
The SFL campaign is part of a coordinated effort by the CDC to use evidence-based interventions to help reduce the burden of CRC in the population. These efforts include the CDC’s Colorectal Cancer Control Program and applied research to identify effective methods to increase the use of CRC screening services (http://www.cdc.gov/cancer/crccp/index.htm). Each of these and other efforts have used SFL campaign materials tailored to specific local partners to support public education and outreach. This collaborative work between SFL and other CDC CRC-related initiatives creates synergy and perhaps reduces the initial cost of providing public education and outreach campaigns to these initiatives.
Donated services were 86% of the total cost of the campaign. This is not surprising. Many public health communication campaigns depend on donations from media outlets for PSAs (Rideout & Hoff, 2002). Unfortunately, reliance on donated airtime for PSAs often results in campaign messages being played during less optimal time slots, leading to limited message exposure to the intended audience (Gantz, Schwartz, & Angelini, 2008; Rideout & Hoff, 2002). Sponsors of health communication campaigns such as CDC’s SFL are aware of this limitation and have supplemented the donated PSA messages with Internet and “small media” strategies that included distribution of printed materials such as posters, brochures, fact sheets, and videos featuring personal testimony from actors and actresses. SFL also works closely with its partners in health departments in all 50 states, two tribal organizations, and the District of Columbia to provide localized options for PSAs and printed educational materials.
This study has some limitations. The reported incremental benefits and costs of the campaign were not separated by different CRC screening tests. We do not have outcome measures of the campaign and do not want to speculate on the potential effectiveness of the campaign on the use of different CRC screening tests. Our inability to separately estimate the impact of SFL on the use of different types of screening tests does not substantially affect the usefulness of our results because it is well documented that all screening modalities are effective in reducing CRC mortality (Hardcastle et al., 1996; Kronborg, Fenger, Olsen, Jorgensen, & Sondergaard, 1996; Mandel et al., 1993). The effectiveness data used were obtained from population-based CRC screening activities (Cram et al., 2003; Sequist et al., 2010) and from meta-analysis and research syntheses conducted in the past two decades which examined the effectiveness of communication campaigns (Snyder, 2007). In light of the results from this literature, our assumptions represent a reasonable range of effect sizes.
Future Directions in the Economics of Health Communication Campaigns to Promote Cancer Screening
According to the Community Preventive Services Task Force (2012), there are no economic studies conducted to date to ascertain the cost-effectiveness of health communication campaigns in promoting cancer screening. Economic analysis can provide a valuable contribution to the field of health communication by estimating the cost and cost-effectiveness of different components of social media campaigns used in promoting cancer prevention. Given the rapidly changing media landscape in health communication technology, this is an important area of future research. Today, many health communication campaigns use different social media strategies to reach their intended audience. However, little information is available on the cost-effectiveness of these social media campaigns in changing behavior for primary and secondary prevention of cancer.
CONCLUSIONS
Most health communication campaigns, particularly those in cancer prevention and control, have very low budgets to cover their campaign activities. However, these health communication campaigns need to demonstrate effectiveness and accountability to patients, taxpayers, and other stakeholders. In this study, we demonstrated how economic analysis can be used to assess health communication campaigns if effectiveness and cost data from these campaigns are available. Our results suggest that the SFL campaign may have contributed to improving CRC screening rates at a minimal cost. The findings in this study provide an important starting point and benchmark for future evaluation research efforts to determine the benefits and costs of health communication campaigns to promote cancer prevention.
Acknowledgments
The study was funded by the Centers for Disease Control and Prevention. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Use of trade names is for identification purposes only and does not imply endorsement by the authors, the CDC, or the U.S. Department of Health and Human Services.
References
- Centers for Disease Control and Prevention. Cancer screening— United States, 2010. Morbidity and Mortality Weekly Report. 2010;61:41–45. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: Colorectal cancer screening, incidence, and mortality–United States, 2002–2010. Morbidity and Mortality Weekly Report. 2011;60:884–889. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Screen for Life: National Colorectal Cancer Action Campaign. 2012 Retrieved from cdc.gov/cancer/screenforlife.
- Community Preventive Services Task Force. Guide to community preventive services. Health communication & social marketing: Health communication campaigns that include mass media and health-related product distribution. 2012 Retrieved from www.thecommunityguide.org/healthcommunication/campaigns.html.
- Cooper CP, Gelb CA, Jameson H, Macario E, Jorgensen CM, Seeff L. Developing English and Spanish television public service announcements to promote colorectal cancer screening. Health Promotion Practice. 2005;6:385–393. doi: 10.1177/1524839905278759. [DOI] [PubMed] [Google Scholar]
- Cram P, Fendrick AM, Inadomi J, Cowen ME, Carpenter D, Vijan S. The impact of a celebrity promotional campaign on the use of colon cancer screening: The Katie Couric effect. Archives of Internal Medicine. 2003;163:1601–1605. doi: 10.1001/archinte.163.13.1601. [DOI] [PubMed] [Google Scholar]
- Eddy DM. Screening for cancer: Theory, analysis, and design. Englewood Cliffs, NJ: Prentice Hall; 1980. [Google Scholar]
- Gantz W, Schwartz JR, Angelini V. Rideout shouting to be heard: Public advertising in a changing television world. Menlo Park, CA: Kaiser Family Foundation; 2008. (Kaiser Family Foundation Publication No.7715) [Google Scholar]
- Glanz K, Lewis FM, Rimer BK. Health behavior and health education: Theory, research and practice. 2. San Francisco, CA: Jossey-Bass; 1997. [Google Scholar]
- Gold MR, Siegel JE, Russel LB, Weinstein MC, editors. Cost-effectiveness in health and medicine. New York, NY: Oxford University Press; 1996. [Google Scholar]
- Hardcastle JD, Chamberlain JO, Robinson MH, Moss SM, Amar SS, Balfour TW, … Mangham CM. Randomised controlled trial of faecal occult-blood screening for colorectal cancer. Lancet. 1996;348:1472–1477. doi: 10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- Hornik RC. Public health communication: Making sense of contradictory evidence. In: Hornik RC, editor. Public health communication: Evidence for behavior change. Mahwah, NJ: Erlbaum; 2002. pp. 1–22. [Google Scholar]
- Jorgensen CM, Gelb CA, Merritt TL, Seeff LC. Observations from the CDC—CDC’s screen for life: A national colorectal cancer action campaign. Journal of Women’s Health & Gender-Based Medicine. 2001;10:417–422. doi: 10.1089/152460901300233876. [DOI] [PubMed] [Google Scholar]
- Kronborg O, Fenger C, Olsen J, Jorgensen OD, Sondergaard O. Randomised study of screening for colorectal cancer with faecal occult-blood test. Lancet. 1996;348:1467–1471. doi: 10.1016/S0140-6736(96)03430-7. [DOI] [PubMed] [Google Scholar]
- Lengerich EJ, Rubio A, Brown PK, Knight EA, Wyatt SW. Results of coordinated investigations of a national colorectal cancer education campaign in Appalachia. Preventing Chronic Disease. 2006:3. Retrieved from www.cdc.gov/pcd/issues/2006/apr/05_0160.htm. [PMC free article] [PubMed]
- Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, Ederer F. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. New England Journal of Medicine. 1993;328:1365–1371. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- Myhre SL, Flora JA. HIV/AIDS communication campaigns: Progress and prospects. Journal of Health Communication. 2000;5(Suppl):29–45. [PubMed] [Google Scholar]
- Randolph W, Viswanath K. Lessons learned from public health mass media campaigns: Marketing health in a crowded media world. Annual Review of Public Health. 2004;25:419–437. doi: 10.1146/annurev.publhealth.25.101802.123046. [DOI] [PubMed] [Google Scholar]
- Rex DK, Johnson DA, Lieberman DA, Burt RW, Sonnenberg A. Colorectal cancer prevention 2000: Screening recommendations of the American College of Gastroenterology. American Journal of Gastroenterology. 2000;95:868–877. doi: 10.1111/j.1572-0241.2000.02059.x. [DOI] [PubMed] [Google Scholar]
- Rideout V, Hoff T. Shouting to be heard: Public service advertising in a new media age (Executive summary) Menlo Park, CA: Henry J. Kaiser Family Foundation; 2002. [Google Scholar]
- Sabatino SA, Lawrence B, Elder R, Mercer SL, Wilson KM, DeVinney B, … Glanz K. Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: Nine updated systematic reviews for the guide to community preventive services. American Journal of Preventive Medicine. 2012;43:97–118. doi: 10.1016/j.amepre.2012.04.009. [DOI] [PubMed] [Google Scholar]
- Sequist TD, Franz C, Ayanian JZ. Cost-effectiveness of patient mailings to promote colorectal cancer screening. Medical Care. 2010;48:553–557. doi: 10.1097/MLR.0b013e3181dbd8eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro JA, Klabunde CN, Thompson TD, Nadel MR, Seeff LC, White A. Patterns of colorectal cancer test use, including CT colonography, in the 2010 National Health Interview Survey. Cancer Epidemiology, Biomarkers & Prevention. 2012;21:895–904. doi: 10.1158/1055-9965.EPI-12-0192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder LB. Health communication campaigns and their impact on behavior. Journal of Nutrition Education and Behavior. 2007;39(2 Suppl):S32–S40. doi: 10.1016/j.jneb.2006.09.004. [DOI] [PubMed] [Google Scholar]
- Snyder LB, Hamilton MA. A meta-analysis of U.S. health campaign effects on behavior: emphasize enforcement, exposure, and new information, and beware the secular trend. In: Hornik RC, editor. Public health communication: evidence for behavior change. Mahwan, NJ: Lawrence Erlbaum; 2002. pp. 357–383. [Google Scholar]
- U.S. Bureau of Labor Statistics. Consumer price index. 2012 Retrieved from www.bls.gov/cpi/data.htm.
- U.S. Cancer Statistics Working Group. United States cancer statistics: 1999–2009 Incidence and mortality web-based report. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, and National Cancer Institute; 2009. [Google Scholar]
- U.S. Census Bureau, Population Division. 2012 National population projections. 2012 Retrieved from www.census.gov/population/www/projections/summarytables.html.
- U.S. Preventive Services Task Force. Recommendations for adults: Cancer. Rockville, MD: Author; 2011. Retrieved from http://www.uspreventiveservicestaskforce.org/adultrec.htm. [Google Scholar]
- Vanderpool RC, Coyne CA. Qualitative assessment of local distribution of Screen for Life mass media materials in Appalachia. Preventing Chronic Disease. 2006 Retrieved from www.cdc.gov/pcd/issues/2006/apr/05_0031.htm. [PMC free article] [PubMed]
- Ward AJ, Coffey KB, Lengerich EJ, Piccinin AM. The impact of cancer coalitions on the dissemination of colorectal cancer materials to community organizations in rural Appalachia. Preventing Chronic Disease. 2006 Retrieved from www.cdc.gov/pcd/issues/2006/apr/05_0087.htm. [PMC free article] [PubMed]
- Zauber AG. Cost-effectiveness of colonoscopy. Gastrointestinal Endoscopy Clinics of North America. 2010;20:751–770. doi: 10.1016/j.giec.2010.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]