Structured Abstract
Objectives
Outline methods used to describe centre‐level variation in treatment and outcome in children in the Cleft Care UK (CCUK) study. Report centre‐level variation in dento‐facial outcomes.
Setting and Sample Population
Two hundred and sixty‐eight five‐year‐old British children with non‐syndromic unilateral cleft lip and palate (UCLP).
Materials and Methods
Between January 2011 and December 2012, data were collected on a comprehensive range of outcomes. Child facial appearance and symmetry were assessed using photographic pictures. Dental arch relationships were assessed from standardized dental study models. Hierarchical statistical models were used to predict overall means and the variance partition coefficient (VPC)—a measure of amount of variation in treatment or outcome explained by the centre.
Results
Data on dento‐alveolar arch relationships and facial appearance were available on 197 and 252 children, respectively. The median age of the children was 5.5 years, and 68% were boys. Variation was described across 13 centres. There was no evidence of centre‐level variation in good or poor dento‐alveolar arch relationships with a VPC of 4% and 3%, respectively. Similarly, there was no evidence of centre‐level variation in good or poor facial appearance with a VPC of 2% and 5%, respectively.
Conclusions
There was no evidence of centre‐level variation for dento‐facial outcomes although this study only had the power to detect large variation between sites.
Keywords: centralization, cleft lip and palate, treatment outcomes, variation
1. INTRODUCTION
Care for children born with a cleft of the lip and/or palate in the United Kingdom is now centralized and multidisciplinary1, and outcomes have improved.2, 3, 4, 5, 6, 7 These changes have been implemented since the Clinical Standards Advisory Group (CSAG) reported in 1998.8 A key recommendation was that the number of centres offering cleft services should be reduced from 57 to approximately 8 to 15. Since the report, the number of centres was reduced to eleven managed clinical networks. Care in these centres is now provided by multidisciplinary teams, and the surgeons in these teams operate on at least 35 cases each year.1
We conducted the Cleft Care UK (CCUK) study fifteen years later to evaluate the impact of these changes to care.4 CCUK is a national cross‐sectional survey of the treatment and outcomes of 5‐year‐old children born with UCLP that used a comparable design with similar measurements to a previous survey.4 We reported the results in detail in a previous supplement of this journal.2, 3, 4, 5, 6, 7 Briefly, treatment had changed—the range of surgical procedures used was less varied, hearing aids were used more often and grommets placed less frequently; and some outcomes had improved—dentoalveolar relations and speech were considerably better, but the prevalence of dental caries and hearing loss was unchanged. Although the changes were generally positive, comparative data suggest that outcomes for children in the UK are still not as good as the best centres in Europe.9, 10, 11 Furthermore, a significant proportion of children still experienced poor outcomes within this centralized service.3
In this supplement, we explore centre‐level variation in treatment and outcomes and predictors of outcomes for children UCLP treated within this centralized multidisciplinary service. We hope that describing and exploring this variation may identify further areas where care and outcomes can be improved. In this study, we outline the approach we have adopted to describe centre‐level variation and illustrate this by reporting the results for facial growth (dento‐alveolar relationship) and facial appearance. Subsequent papers in this supplement employ the same approach to describe centre‐level variation in audiology,12 oral health,13 speech14 and behavioural outcomes.15 The final paper summarizes the results of these analyses and discusses implications.16
2. METHODS
2.1. Study sample
We used data from CCUK. This is a UK‐wide cross‐sectional study of 5‐year‐old children born between April 2005 and March 2007 with UCLP. A full description of recruitment procedures and eligibility criteria can be found elsewhere.4 Briefly of 359 eligible children, consent for participation was obtained from 268 (75%) children and parents.
2.2. Cleft centres and managed clinical networks
We collected data from every cleft centre in the UK (n=18) at designated audit clinics. Several of the centres are managed by a single Clinical Director as part of a clinical network or hub. For example, the centres Liverpool and Manchester are part of the North West and North Wales network, and Bristol and Swansea are part of the South West and South Wales network. These 18 centres function within 11 managed clinical networks. The full list of centres and their associated clinical network is shown in Table 1.
Table 1.
Organization of cleft services in the UK at the time of the study
| Clinical network | Centre |
|---|---|
| Cleft Net East | Cambridge |
| West Midlands | Birmingham |
| Northern & Yorkshire | Leeds |
| Newcastle | |
| Northern Ireland | Belfast |
| North Thames | Great Ormond Street |
| Chelmsford | |
| North West & North Wales | Liverpool |
| Manchester | |
| Scotland | Glasgow |
| Edinburgh | |
| Aberdeen | |
| South Thames | Guys & St Thomas’ |
| South West & South Wales | Bristol |
| Swansea | |
| Spires | Salisbury |
| Oxford | |
| Trent | Nottingham |
2.3. Outcomes
We report on dento‐alveolar relationship and facial appearance in this paper. Full details of the methodology for these two variables have been reported elsewhere.4 Dental arch relationships were assessed from standardized casts of impressions taken of each child's teeth and mouth. The models were assessed using the established 5‐Year‐Olds' Index, creating an ordinal response on a five‐point Likert‐type scale (1=Excellent, 2=Good, 3=Fair, 4=Poor or 5=Very Poor). Facial appearance was assessed from photographs using a standardized and validated aesthetic outcome assessment tool for the evaluation of cleft lip and palate surgical repairs. An orthodontist, blinded to the centre, rated each cropped image using a 5‐point Likert‐type scale (1=Excellent, 2=Good, 3=Fair, 4=Poor or 5=Very Poor). This five‐point ordinal scale was adapted and developed by the Birmingham Institute of Paediatric Plastic Surgery from an existing method.17
2.4. Co‐variables
Differences in age and gender may have effects on developmental outcomes such as facial structure and speech, so age and gender were considered as potential confounders of centre‐level differences. Although the target age was between 5 years 3 months and 5 years 9 months, the mean age in the study was 5 years and 7 months and the range was 4 years 6 months to 7 years and 6 months. The cleft centres scheduled special audit clinics when the children were the required age. However, where appointments were missed, clinics had to be rescheduled and children would then have been seen at different ages.
2.5. Coding of outcomes
Both of the outcome variables in this study are ordinal. To focus the results on the between‐centre variation in good outcomes and the between‐centre variation in poor outcomes, each variable was recoded into two binary variables. To capture the good outcomes, for both variables, children scored as a one (excellent) or two (good) were coded as one with all others zero; and to capture the poor outcomes, children scored as a four (poor) or five (very poor) were coded as one with all others zero.
2.6. Statistical model
Hierarchical models (also known as multilevel, mixed‐effects or random‐effects models) were fitted to each of the binary outcome variables. Centre was treated as a random effect, and sex and age were modelled as fixed binary and continuous covariates. A logit‐link function was used (ie, logistic) giving the following model.
| (1) |
In the model above (Equation 1), y ij is the binary response (0 or 1) for child i in centre j, is the between‐centre variance in the outcome adjusting for age and sex differences, β 0 is the log odds of y in girls at age 5.5 years (age was centred at the median of 5.5 years and boys were coded as 1) when μ j = 0 (i.e, in the so‐called average centre). Lastly, μ j is an estimate of the difference in log odds of having the outcome (y = 1) between centre j and the so called average centre β 0. The models were estimated by maximizing the likelihood function using numerical integration (adaptive Gauss‐Hermite approximation). In cases where estimation of failed, we used (a) a quasi‐likelihood method using penalized iteratively reweighted least squares18 and if (a) failed then (b) Bayesian estimation via Markov Chain Monte Carlo methods.19 We used R (vers 3.3.2), and the lme4, blme and R2MLwiN packages package to estimate the hierarchical models. Stata (vers 14.2) was used for all other analyses.
2.7. Describing variation between centres
The variance partition coefficient (VPC) was estimated from these models as a measure of the variability in outcomes between centres. The VPC captures the proportion of the total variation in each outcome that is explained by differences between hubs. A VPC has the same interpretation as an intraclass correlation coefficient (ICC), and in certain models, they are the same. In our models, which contain the fixed covariates age and sex, the VPC can also be interpreted as the residual correlation between individuals from the same centre. As fixed covariates were included in the model, we used a simulation approach to estimate the VPC (http://www.bristol.ac.uk/cmm/software/support/support-faqs/pval.html#b). A likelihood ratio test of the null hypothesis that there is no variation between hubs (ie, ) was also performed.
2.8. Estimating mean levels for treatment and outcome for each centre
We used to estimate the proportion of children with the outcome in the so‐called average centre. As age and sex were included in the models, represents the predicted log odds of the outcome for girls of median age 5.5 years. The equation in (1) was rearranged to convert from logs odds to a proportion . In a similar way, was used to predict the proportion of children in each centre with each outcome. These predicted proportions are model‐based estimates of the mean in each centre and are more likely to be closer to the true value than a simple description of the raw data because they borrow information from the overall mean in a way that is proportional to the sample size in each centre and to the amount of clustering or similarity in outcomes from individuals within each centre.
3. RESULTS
3.1. Sample description and grouping of centres
The median age of children in CCUK was 5.5 years (IQR: 5.4‐5.7 years), and 181 of 268 (68%) were boys. Data on dento‐alveolar arch relationships and facial appearance were available on 197 and 252 children, respectively. Table 2 shows the number of children treated in each centre. As the sample size was small for particular centres, we grouped centres by their managed clinical networks except for those centres that had treated more than 15 children. This resulted in 13 centres all of which had more than 15 children (Table 2).
Table 2.
Number of children (n) treated in each centre and n in final grouping of centres used in the analyses (ordered by centre size)
| n (%) in each centre | n (%) in each centre/hub unit | |
|---|---|---|
| 1 | 3 (1.1) | 16 (6.0) |
| 2 | 6 (2.2) | 16 (6.0) |
| 3 | 8 (3.0) | 16 (6.0) |
| 4 | 10 (3.7) | 17 (6.3) |
| 5 | 10 (3.7) | 17 (6.3) |
| 6 | 11 (4.1) | 19 (7.1) |
| 7 | 13 (4.9) | 19 (7.1) |
| 8 | 13 (4.9) | 20 (7.5) |
| 9 | 13 (4.9) | 21 (7.8) |
| 10 | 16 (6.0) | 23 (8.6) |
| 11 | 16 (6.0) | 24 (9.0) |
| 12 | 16 (6.0) | 30 (11.2) |
| 13 | 17 (6.3) | 30 (11.2) |
| 14 | 17 (6.3) | |
| 15 | 19 (7.1) | |
| 16 | 20 (7.5) | |
| 17 | 30 (11.2) | |
| 18 | 30 (11.2) | |
| Total | 268 (100) | 268 (100) |
3.2. Age and sex distribution by centres
There was evidence of an association between cleft centre and age at assessment (P<.001). However, the mean age of the children in each centre was within 2 months of the overall mean for all centres except one. The single centre outside of this limit assessed children that were on average more than 6 months older than the mean. There was also evidence of an association between the sex of the child and centre (P=.017), although the variation was small—in all but one centre, more boys were assessed than girls.
3.3. Centre‐level variation in dento‐alveolar relations
Table 3 shows the results for the good and poor dento‐alveolar relationship outcomes. The overall percentage of children with a good outcome and with a poor outcome in so‐called average centres was 60% (95% CI: 48%‐71%) and 14%, respectively (95% CI: 7%‐28%). There was no evidence for any centre‐level variation in these outcomes—after adjusting for age and sex, only 2% and 4% of the variability in good and poor outcomes, respectively, was attributable to differences between centres. Figure 1 shows the predicted proportions with good and poor dento‐alveolar relationships for each centre. It is clear that outcomes were broadly similar across all centres.
Table 3.
Predicted proportions with each outcome for the so‐called “average” centre and the between‐centre variability variance partition coefficient (VPC)
| Outcome | n | Proportion (95% CI) | VPC | P‐valuea | |
|---|---|---|---|---|---|
| Dento‐alveolar | Good (1 or 2) | 197 | 0.6 (0.48, 0.71) | 0.04 | .6 |
| Poor (4 or 5) | 0.14 (0.07, 0.28)b | 0.03 | .9 | ||
| Facial appearance | Good (1 or 2) | 252 | 0.37 (0.24, 0.52)b | 0.02 | .9 |
| Poor (4 or 5) | 0.18 (0.09, 0.34)b | 0.05 | .9 | ||
All results are adjusted for age and sex.
a test of the null hypothesis that there is no between‐centre variation.
Due to small estimated level 2‐variance , the CI was estimated using Bayesian approach by maximizing model's posteriori.
Figure 1.
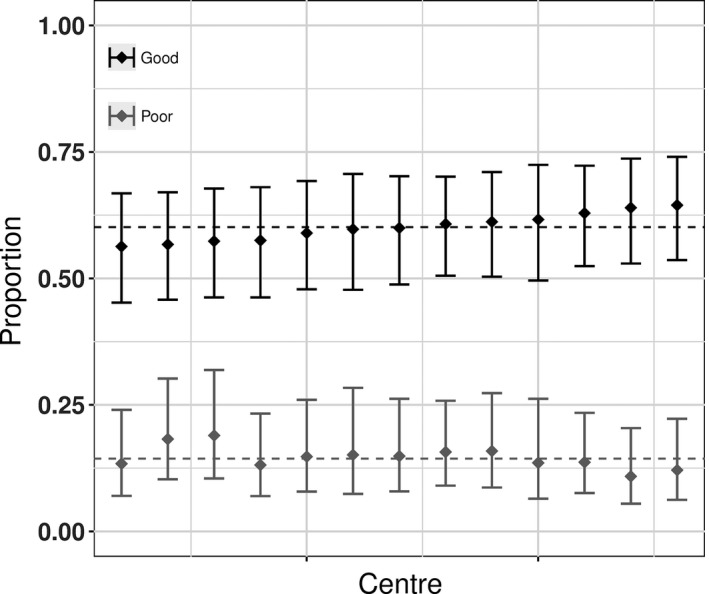
Predicted proportion in each centre with a good outcome (black) and a poor outcome (grey) for dento‐alveolar relationship. The bars are 95% confidence intervals, and the dashed line is the predicted mean for the average centre adjusted for age and sex
3.4. Centre‐level variation in facial appearance
Table 3 shows the results for the good and poor facial appearance outcomes. The overall percentage of children with a good outcome and with a poor outcome in so‐called “average” centres was 37% (95% CI: 24%‐52%) and 18%, respectively (95% CI: 9%‐34%). As with dento‐alveolar relations, there was no evidence of centre‐level variation for these outcomes. After adjusting for age and sex, only 3% and 5% of the variability in good and poor outcomes, respectively, was attributable to differences between treatment centres. Figure 2 shows the predicted proportions for each centre. It is clear that outcomes did not vary between centres beyond what would be expected from random sampling variation.
Figure 2.
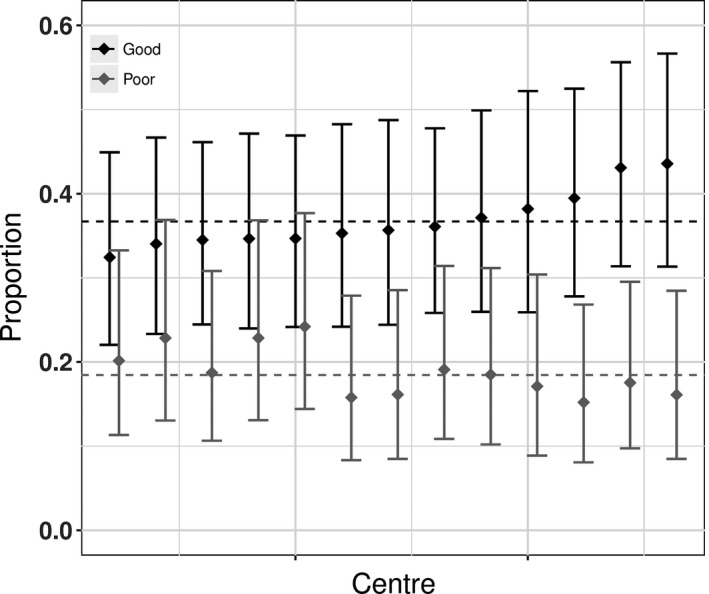
Predicted proportion in each centre with a good outcome (black) and a poor outcome (grey) for facial appearance. The bars are 95% confidence intervals, and the dashed line is the predicted mean for the average centre. Adjusted for age and sex
4. DISCUSSION
We have described a standard hierarchical statistical model to predict centre‐level means and centre‐level variation and highlighted how to interpret the output from these models using the expository examples of facial growth and appearance. We found modest differences between centres in the age at assessment and gender of the children over and above that which may be expected from sampling variation and so we controlled for these differences in the analysis presented in this paper and in the subsequent papers in this supplement.12, 13, 14, 15 We found no evidence of centre‐level variation in dento‐alveolar relationships and facial appearance.
4.1. Strengths and limitations
Cleft Care UK is a large study (for children with cleft lip and palate), nationwide and contains a substantial set of validated measures of key outcomes measured with enough precision to demonstrate improvements over time.2, 3, 4, 5, 6, 7 The response rate was also good. Nonetheless, our study has limited power to detect modest centre‐level variation in treatment and outcome, so our results with respect to centre‐level variation need to be interpreted with caution. We tried to minimize this risk by pooling smaller centres with their respective regional network.
4.2. The importance of exploring centre‐level variation
In this supplement, we have explored centre‐level variability across a range of treatment and outcome measures. Our results, which are reported in full in each respective paper in this supplement,12, 13, 14, 15, 16 suggest that there was centre‐level variation in several of these treatment indicators and outcomes across the domains of oral health,13 audiology12 and speech.14 Describing and exploring these centre‐level variations is important for several reasons. First, it may describe differences in treatment and outcome between centres that can be explored and that may ultimately result in improvements in care and outcome. Second, centre may act as a confounder of certain association. Third, if there is a correlation between individuals from the same centre or clustering of observations then the assumption of independent observations that is made for conventional statistical analysis does not hold. This leads to invalid inference through standard errors that are estimated to be too small. The multilevel models used here deal with these issues.
It is important to remember the work that led to the changes in cleft services in the UK which raised expectations with regard to potential influences to improve outcomes. Seminal work in the late 1970s in Europe (known as the Eurocleft study) showed between‐centre variation in outcomes irrespective of protocols or surgical techniques.20 Six centres submitted consecutive UCLP cases treated within a given time period. When dento‐alveolar outcomes were examined, the centre with the worst results had multiple surgeons and no standardized policy for surgery. The efficacy of individual elements of different treatment programmes could not be detected by examining dento‐alveolar outcomes. As cleft services have centralized in the UK, there is evidence that variations in surgical techniques are narrowing which would explain, in part, limited centre differences in this outcome.21 The Eurocleft study also examined soft tissues using both cephalometrics and naso‐labial appearance.22, 23 Similar outcome rankings were seen across the six centres whether using dento‐alveolar, cephalometric or nasolabial measures. However, sample size variations between centres and the “coarseness” of these measures limited identification of factors which contributed to the good or poor outcomes.
In the UK, data on outcomes from the CSAG study originated from 57 centres which included dento‐alveolar relations and naso‐labial appearance.24, 25 None of these cleft centres had sufficient cases to enable meaningful comparison with other centres or indeed the overall national outcomes. Post‐centralization of cleft care, the number of cases that each surgeon treats per year has increased. In 2009‐2010, seventeen of the nineteen primary cleft surgeons in the UK operated on 40‐50 cases annually,1 whereas only a single surgeon achieved this in the original CSAG.25 Arguments were made as to what would be a volume of surgery sufficient to detect differences between centres, surgeons and techniques. Even if one restricts follow‐up to 5 years, only operators treating 60 new cases per year would be able to audit their outcomes within a decade.26 This was highlighted in a recent well‐designed adequately powered study.27 Three parallel randomized clinical trials were undertaken as an international multicentre study by 10 cleft teams in five countries: Denmark, Finland, Sweden, Norway and the UK. All children included were born with UCLP and randomized to three different surgical procedures for primary palatal repair. There was no evidence that one technique is better than the others used. The possible influence of individual surgical skill was recognized.27 This factor was not analysed in the current study where individual surgical volumes preclude meaningful analysis.
4.3. Centre‐level variation in dento‐alveolar relationships and facial appearance
Although outcomes for dento‐alveolar relationships and facial appearance have improved with the introduction of a centralized multidisciplinary service2 there was no evidence of variation between centres within this centralized service. There are several reasons for this. First, this study only had the power to detect large differences so it is possible that modest but important differences do exist between centres but our study did not have the power to detect these. Second, it is possible that these outcomes are not measured accurately enough to detect modest centre‐level differences—although we used standard photographic protocols and approaches to coding, facial appearance is difficult to measure accurately and reliably. Furthermore, intraoral photographs were used in some children rather than study models in some centres to assess dento‐alveolar relationships. We have previously shown that reliability of scoring is reduced for intraoral photographs compared with dental study casts and that on the currently available evidence, dental study casts still provide the gold standard when assessing primary surgical outcome in cleft care.28 Thus, the use of intraoral photographs instead of dental study casts may have reduced variation in assessing dento‐alveolar relationships between centres. Third, it is possible that variation between surgeons rather than centres is important in determining these outcomes.27 Finally, it is possible that care is now so uniform in this centralized service that variations in these outcomes between centres do not exist.21
5. CONCLUSION
Children with cleft lip and palate in the UK are now treated by a centralized multidisciplinary service that has resulted in improved outcomes. Variation in treatment and outcomes between centres may still exist within this centralized service. Describing and exploring centre‐level differences in treatment and outcome may help improve care and outcomes for children with cleft lip and palate. We found no evidence of centre‐level variation in dento‐alveolar arch relationship and facial appearance.
ACKNOWLEDGEMENTS
We would like to thank the families that took part in this study. We would also like to thank the clinicians and staff in the cleft centres that supported this project. We have listed people who made key contributions to this research in the Appendix 1.
This publication presents independent research commissioned by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research scheme (RP‐PG‐0707‐10034). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
APPENDIX 1.
List of local study PIs, Co‐ordinators and staff who contributed to the collection of data for the CCUK project
| Cleft Centre | |
|---|---|
| Cleft NetEast, Cambridge | Per Hall (PI); Sue Burgess (Co‐ordinator) |
| West Midlands, Birmingham | Rona Slator (PI); Alexander Levine (Co‐ordinator) Victoria Clark; Lars Enocson; Alison Jeremy |
| South Wales South West, Bristol | Liz Albery (PI); Richard Willerton |
| North Thames, Great Ormond Street Hospital for Children | Loshan Kangesu (PI); Laura Sennett (Co‐ordinator) Norman Hay; Karen Wilson; Raouf Chorbachi; Marie Pinkstone; Natalie Pancewicz; Anne Mayne; Brijesh Patel; James Green; Debbie Sell; Laura Sennett; Lauren Baillie; John Volcano |
| South Thames, Guys and St Thomas’ | Alex Cash (PI); Peggy Mo (Co‐ordinator) |
| Spires, Oxford | Stephen Robinson (PI); Steven Berry (Co‐ordinator) |
| Northern and Yorkshire, Leeds | Alistair Smyth (PI); Heather Jamieson (Co‐ordinator) |
| South Wales South West, Swansea | Adrian Sugar (PI); Andrea Thomas (Co‐ordinator) |
| Trent, Nottingham | John Rowson (PI); Vicky Nightingale (Co‐ordinator) |
| Royal Aberdeen Children's Hospital | Felicity Mehendele (PI) |
| West of Scotland, Glasgow | Toby Gilgrass (PI); Elaine Simpson (Co‐ordinator) |
| East of Scotland, Edinburgh | Felicity Mehendele (PI) |
| Northwest England, Isle of Man, North Wales Liverpool | Joyce Russell (PI); Helen McCormick (Co‐ordinator) |
| Royal Manchester Children's Hospital | Haydn Bellardie (PI); Claire Richardson (Co‐ordinator) Jeanette Mooney, Jill Painter, Melanie Bowden, Julie Davies, Jayne O'Connor, David Whitby, Jenny Williams, Vicky Beale. |
| Northern and Yorkshire, Newcastle | Peter Hodgkinson (PI); Paula Spence (Co‐ordinator) |
| Spires, Salisbury | Stephen Robinson (PI); Mary Ann Brewer (Co‐ordinator) |
| North Thames, St. Andrew's Centre, Chelmsford | Loshan Kangesu (PI); Karen Wilson (Co‐ordinator) |
| Northern Ireland | Chris Hill (PI); Pamela Foster (Co‐ordinator) |
Wills AK, Mahmoud O, Hall A, et al. Centre‐level variation of treatment and outcome in 5‐year‐old children with non‐syndromic unilateral cleft lip and palate: The Cleft Care UK study. Part 1: Methodology and results for dento‐facial outcomes. Orthod Craniofac Res. 2017;20(Suppl. 2):1–7. https://doi.org/10.1111/ocr.12183
REFERENCES
- 1. Scott JK, Leary SD, Ness AR, et al. Centralization of services for children born with orofacial clefts in the United kingdom: a cross‐sectional survey. Cleft Palate Craniofac J. 2014;51:e102‐e109. [DOI] [PubMed] [Google Scholar]
- 2. Al‐Ghatam R, Jones TE, Ireland AJ, et al. Structural outcomes in the Cleft Care UK study. Part 2: dento‐facial outcomes. Orthod Craniofac Res. 2015;18(Suppl 2):14‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ness AR, Wills AK, Waylen A, et al. Centralization of cleft care in the UK. Part 6: a tale of two studies. Orthod Craniofac Res. 2015;18(Suppl 2):56‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Persson M, Sandy JR, Waylen A, et al. A cross‐sectional survey of 5‐year‐old children with non‐syndromic unilateral cleft lip and palate: the Cleft Care UK study. Part 1: background and methodology. Orthod Craniofac Res. 2015;18(Suppl 2):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sell D, Mildinhall S, Albery L, Wills AK, Sandy JR, Ness AR. The Cleft Care UK study. Part 4: perceptual speech outcomes. Orthod Craniofac Res. 2015;18(Suppl 2):36‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Smallridge J, Hall AJ, Chorbachi R, et al. Functional outcomes in the Cleft Care UK study–Part 3: oral health and audiology. Orthod Craniofac Res. 2015;18(Suppl 2):25‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Waylen A, Ness AR, Wills AK, Persson M, Rumsey N, Sandy JR. Cleft Care UK study. Part 5: child psychosocial outcomes and satisfaction with cleft services. Orthod Craniofac Res. 2015;18(Suppl 2):47‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Group CSA . Cleft Lip and/or Palate. London: HSMO; 1998. ISBN 0‐11‐322103‐7. [Google Scholar]
- 9. Fudalej P, Hortis‐Dzierzbicka M, Dudkiewicz Z, Semb G. Dental arch relationship in children with complete unilateral cleft lip and palate following Warsaw (one‐stage repair) and Oslo protocols. Cleft Palate Craniofac J. 2009;46:648‐653. [DOI] [PubMed] [Google Scholar]
- 10. Lilja J, Mars M, Elander A, et al. Analysis of dental arch relationships in Swedish unilateral cleft lip and palate subjects: 20‐year longitudinal consecutive series treated with delayed hard palate closure. Cleft Palate Craniofac J. 2006;43:606‐611. [DOI] [PubMed] [Google Scholar]
- 11. Sinko K, Caacbay E, Jagsch R, Turhani D, Baumann A, Mars M. The GOSLON yardstick in patients with unilateral cleft lip and palate: review of a Vienna sample. Cleft Palate Craniofac J. 2008;45:87‐92. [DOI] [PubMed] [Google Scholar]
- 12. Hall A, Wills AK, Mahmoud O, et al. Centre‐level variation in outcomes and treatment for otitis media with effusion and hearing loss and the association of hearing loss with developmental outcomes at ages 5 and 7 years in children with non‐syndromic unilateral cleft lip and palate: The Cleft Care UK study. Part 2. Orthod Craniofac Res. 2017;1‐11. https://doi.org/10.1111/ocr.12184. [DOI] [PubMed] [Google Scholar]
- 13. Smallridge J, Wills AK, Mahmoud O, et al. Centre‐level variation in dental treatment and oral health and individual‐and area‐level predictors of oral health in 5‐year‐old children with non‐syndromicunilateral cleft lip and palate: the Cleft Care UK study. Part 3. Orthod Craniofac Res. 2017;1‐8. https://doi.org/10.1111/ocr.12185. [DOI] [PubMed] [Google Scholar]
- 14. Sell D, Southby L, Wren Y, et al. Centre‐level variation in speech outcome and interventions, and factors associated with poor speech outcomes in 5‐year‐old children with non‐syndromic unilateral cleft lip and palate: The Cleft Care UK study. Part 4. Orthod Craniofac Res. 2017;1‐13. https://doi.org/10.1111/ocr.12186. [DOI] [PubMed] [Google Scholar]
- 15. Waylen A, Mahmoud O, Wills AK, Sell D, Sandy JR, Ness AR. Centre‐level variation in behaviour and the predictors of behaviour in 5‐year‐old children with non‐syndromic unilateral cleft lip: The Cleft Care UK study. Part 5. Orthod Craniofac Res. 2017;1‐8. https://doi.org/10.1111/ocr.12187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ness AR, Wills AK, Mahmoud O, et al. Centre‐level variation in treatment and outcomes and predictors of outcomes in 5‐year‐Old children with non‐syndromic unilateral cleft lip treated within a centralized service: the Cleft Care UK study. Part 6: summary and implications. Orthod Craniofac Res. 2017;1‐4. https://doi.org/10.1111/ocr.12188. [DOI] [PubMed] [Google Scholar]
- 17. Kim JB, Strike P, Cadier MC. A simple assessment method for auditing multi‐centre unilateral cleft lip repairs. J Plast Reconstr Aesthet Surg. 2011;64:195‐200. [DOI] [PubMed] [Google Scholar]
- 18. Chung Y, Rabe‐Hesketh S, Dorie V, Gelman A, Liu J. A nondegenerate penalized likelihood estimator for variance parameters in multilevel models. Psychometrika. 2013;78:685‐709. [DOI] [PubMed] [Google Scholar]
- 19. Chung Y, Rabe‐Hesketh S, Gelman A, Liu J, Dorie V. Avoiding boundary estimates in linear mixed models through weakly informative priors (February 2012). U.C. Berkeley Division of Biostatistics Working Paper Series. Working Paper 284. 2012.
- 20. Mars M, Asher‐McDade C, Brattstrom V, et al. A six‐center international study of treatment outcome in patients with clefts of the lip and palate: part 3. Dental arch relationships. Cleft Palate Craniofac J. 1992;29:405‐408. [DOI] [PubMed] [Google Scholar]
- 21. Fitzsimons KJ, Mukarram S, Copley LP, Deacon SA, van der Meulen JH. Centralisation of services for children with cleft lip or palate in England: a study of hospital episode statistics. BMC Health Serv Res. 2012;12:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Asher‐McDade C, Brattstrom V, Dahl E, et al. A six‐center international study of treatment outcome in patients with clefts of the lip and palate: part 4. Assessment of nasolabial appearance. Cleft Palate Craniofac J. 1992;29:409‐412. [DOI] [PubMed] [Google Scholar]
- 23. Molsted K, Asher‐McDade C, Brattstrom V, et al. A six‐center international study of treatment outcome in patients with clefts of the lip and palate: part 2. Craniofacial form and soft tissue profile. Cleft Palate Craniofac J. 1992;29:398‐404. [DOI] [PubMed] [Google Scholar]
- 24. Sandy JR, Williams AC, Bearn D, et al. Cleft lip and palate care in the United Kingdom–the Clinical Standards Advisory Group (CSAG) Study. Part 1: background and methodology. Cleft Palate Craniofac J. 2001;38:20‐23. [DOI] [PubMed] [Google Scholar]
- 25. Williams AC, Bearn D, Mildinhall S, et al. Cleft lip and palate care in the United Kingdom–the Clinical Standards Advisory Group (CSAG) Study. Part 2: dentofacial outcomes and patient satisfaction. Cleft Palate Craniofac J. 2001;38:24‐29. [DOI] [PubMed] [Google Scholar]
- 26. Bearn D, Mildinhall S, Murphy T, et al. Cleft lip and palate care in the United Kingdom–the Clinical Standards Advisory Group (CSAG) Study. Part 4: outcome comparisons, training, and conclusions. Cleft Palate Craniofac J. 2001;38:38‐43. [DOI] [PubMed] [Google Scholar]
- 27. Heliovaara A, Kuseler A, Skaare P, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 6. Dental arch relationships in 5 year‐olds. J Plast Surg Hand Surg. 2017;51:52‐57. [DOI] [PubMed] [Google Scholar]
- 28. Jones T, Leary S, Atack N, et al. Are photographs a suitable alternative to dental study casts when assessing primary surgical outcome in children born with unilateral cleft lip and palate? Eur J Orthod. 2016;38:341‐344. [DOI] [PMC free article] [PubMed] [Google Scholar]


