Abstract
Introduction
Complications of pregnancy and childbirth can pose serious risks to the health of women, especially in resource‐poor settings. Zambia has been implementing a program to improve access to emergency obstetric and neonatal care, including expansion of maternity waiting homes‐residential facilities located near a qualified medical facility where a pregnant woman can wait to give birth. Yet it is unclear how much support communities and women would be willing to provide to help fund the homes and increase sustainability.
Methods
We conducted a mixed‐methods study to estimate willingness to pay for maternity waiting home services based on a survey of 167 women, men, and community elders. We also collected qualitative data from 16 focus group discussions to help interpret our findings in context.
Results
The maximum willingness to pay was 5.0 Zambian kwacha or $0.92 US dollars per night of stay. Focus group discussions showed that willingness to pay is dependent on higher quality of services such as food service and suggested that the pricing policy (by stay or by night) could influence affordability and use.
Discussion
While Zambians seem to value and be willing to contribute a modest amount for maternity waiting home services, planners must still address potential barriers that may prevent women from staying at the shelters. These include cash availability and affordability for the poorest households.
Keywords: maternal health, maternity waiting home, obstetric complications, use of health care services, willingness to pay, Zambia
INTRODUCTION
Complications of pregnancy and childbirth can pose serious risks to the health of women, especially in resource‐poor settings. Obstructed or prolonged labor and failure to progress are associated with higher rates of maternal, fetal, and neonatal death; postpartum hemorrhage; and maternal and neonatal infection.1 Worldwide, about 73% of maternal deaths between 2003 and 2009 were due to obstetric causes, including hemorrhage (27.1%), hypertension (14.0%), and sepsis (10.7%).2 Lack of access to assisted services during labor and birth exacerbates poor outcomes. Women who give birth without a skilled birth attendant are also 2.8 times more likely to experience a stillbirth; overall, stillbirth rates in low‐ and middle‐income countries are 10 times greater than high‐income countries.3
Maternal mortality, defined as the death of women during pregnancy, childbirth, or in the 42 days after birth, has negative impacts on household economic activity.4 Households may experience catastrophic health expenditures prior to the maternal death, increasing the risk the household will fall into poverty. A study in Kenya found that households that experienced a maternal death spent 30% of annual per‐capita consumption expenditure to cover costs including facility fees, transport, medicines, bedding, food, and hotel stay for the woman and people accompanying the woman to seek care.4
In Zambia, a southern African country with a population of 14.5 million, maternal mortality is estimated at 398 deaths per 100,000 live births,5 and women experience 21.3 stillbirths per 1000 live births.3 The majority of women give birth at home: 62% of births in rural Zambia occur without skilled care, in part due to improperly equipped and staffed facilities.6 Poor roads and inadequate transport compound the problem. 7, 8
Emergency obstetric and neonatal care has been shown to improve maternal and neonatal outcomes if implemented appropriately.9, 10 Zambia started a program to improve access to high‐quality obstetric care in 4 districts. An evaluation after one year noted many accomplishments, including 1010 community members trained (including Safe Motherhood Action Group members), 12 midwives hired, 179 health workers trained in emergency care for women and newborns, and the purchase of ambulances and motorcycle‐ambulance vehicles.11 To complement increased availability of emergency services in Zambia and to overcome physical and logistic barriers, many communities have built maternity waiting homes, referred to locally as “mothers’ shelters.”6, 12
Defined as a residential facility located near a qualified medical facility where a pregnant woman can wait to give
Quick Points
-
✦
Maternity waiting homes (shelters) are residential facilities located near qualified medical facilities where pregnant woman can wait to give birth.
-
✦
Shelters could play a key role in helping ensure access to comprehensive maternity care, provided communities are willing to help sustain them.
-
✦
In rural Zambia, most women, men, and elders surveyed were willing to contribute at least a small sum to stay in a shelter, suggesting that they would gain utility and satisfaction from this service.
-
✦
Contributions, either in the form of individual donations or an annual community contribution, have potential to support the long‐term financial sustainability of the shelters.
birth, the shelters can play a role in systems of comprehensive maternity care.13 Studies from African countries suggest that shelters may help to reduce life‐threatening delays that occur in management of obstetric complications.14, 15, 16, 17 While external funding can catalyze initial investment, ongoing quality and sustainability are concerns. Shelters in Zambia are not always well utilized and some have fallen into disrepair.18
As part of a strategy to inform the development of financially and operationally sustainable shelters, we studied how much women or their families might be willing to contribute to use community‐managed shelters. Our goal was to understand preferences, information that could help inform interventions to make shelters more available in Zambia. Introducing a suggested donation, coupled with appropriate mechanisms for exemption, was considered a possible approach to improve sustainability of these community‐owned and managed shelters.
METHODS
Study Design and Sampling
The study used a cross‐sectional, mixed‐methods approach to capture information from the perspective of multiple stakeholders. We applied a multistage, random sampling design, stratified by distance from a health facility with a shelter.18 Data were collected in October and November 2013 in the catchment areas of 4 randomly selected health facilities with an existing shelter in Choma and Kalomo Districts in Southern Province, Zambia. We randomly selected villages in each catchment area at varying distances from the health facility (< 5 kilometers [km], 5‐10 km, > 10 km). Within each village, data collectors started at the village center and proceeded in a randomly chosen direction to every nth household (dependent on catchment size) to identify eligible respondents. Participants were ineligible if someone else in the household had participated in the survey; therefore, no participants represented the same household. Using purposive sampling, health facility staff and volunteer extension workers invited participants from within their networks to participate in focus group discussions at the health facilities. Focus groups were designed to elicit qualitative information specific to perceptions of affordability, payment preferences, how quality influences willingness to pay, and alternatives for those who could not afford to pay. We asked questions about bartering goods or work in exchange for the stay, and the types of items or chores women might be willing to contribute.
Instrumentation
To elicit willingness‐to‐pay estimates, we used interviewer‐administered questions adapted from a US Agency for International Development–funded user's manual on conducting willingness‐to‐pay surveys.19 The survey methodology, applied previously in 6 countries including Ghana and Mali, uses a contingent valuation approach, asking individuals to place a value on a hypothetical commodity or service to determine the maximum amount a person is willing to pay to have the good or service in question.20 In addition, we applied generally accepted methods to reduce potential bias, including face‐to‐face interviewing, closed‐ended questions, specified increments for the service that would be familiar to participants, and a hypothetical summary of the service, which reminded respondents that spending on the service would have to come from their household income and that substitutes exist.19, 21
Participants were first asked whether they had previously used a shelter and the amount paid during the most recent stay. Then we described the hypothetical, improved service as follows:
Imagine that this mothers’ shelter is safe, provides a space for you and your caretaker to sleep, has basic cooking facilities, and is adjacent to a health facility with quality services for you to deliver. In answering these questions, please bear in mind the following: 1) assume that your household income stays the same; 2) most women stay on average about 10 days, but you will not know in advance exactly how many days you will be staying. You will have to pay a fee for each day you stay; and 3) you have alternatives to staying in the mothers’ shelter (for example, stay with a relative or with a friend).
Next we asked participants questions related to the hypothetical situation: Would they be willing to use the shelter if it required paying a medium price per night (7 kwacha or $1.29 US dollars [USD]), a price higher than the medium price (10 kwacha or $1.84 USD), or a price lower than the medium price (5 kwacha or $0.92 USD). Finally, we asked an open‐ended question about the maximum willingness to pay. Price probes were determined by the researchers based on local context and prior conversations with government key informants. The survey also captured basic demographics (ie, assets, employment, household income).
Participants
Survey participants included women who had given birth in the past 24 months, men who had a child under 24 months, and community elders. We included men and elders because research has shown that their opinions may influence attitudes and behavior of pregnant women,22, 23, 24 and in Zambia in particular, elders and husbands play an important role in the final decision of where a woman gives birth.7, 25 Questions were adjusted for the audience: pregnant women or those who had recently given birth were asked about their own experience, men with small children were asked to consider their spouse's experience, and elders were asked to consider their daughter's or granddaughter's experience. In addition, focus group discussions were organized with women of reproductive age, men, traditional birth attendants, Safe Motherhood Action Group members, and mothers‐in‐law.
Procedures
The study instruments were translated into the local language of Tonga and back‐translated into English by an independent translator to check for equivalence.26 Nine data collectors fluent in English and Tonga attended a 5‐day training in research ethics and methods for administering surveys and conducting focus groups. The training included pilot testing of the study instruments, which resulted in minor adjustments. All data collection was conducted over a period of 6 weeks. To reduce reticence related to collecting financial information, verbal informed consent was obtained. Participants were given a copy of the verbal consent form. Ethical permission to conduct this study was obtained from ERES Converge in Zambia and the Boston University institutional review board.
Analysis
Quantitative data were captured in CSPro public domain software and analyzed in SAS v9.3 (SAS, Cary, NC). We calculated mean and standard deviation for demographic variables, using chi‐square and analysis of variance (ANOVA) to test for differences between groups. We measured the mean and median assuming that an individual's maximum willingness to pay was the highest amount explicitly agreed to in response to the 3 individual price probes or the open‐ended question (method 1). We also measured willingness to pay by analyzing the open‐ended question alone (method 2). We report the median for data that were not normally distributed. Bivariate correlation coefficients were calculated to assess relationships among willingness to pay and other variables such as income and distance. Qualitative data were translated and transcribed, then analyzed in NVivo 10 (QSR international, Doncaster, Australia). Two investigators (T.V. and E.W.) coded 2 transcripts together, using focus group questions as a priori themes. The lead author then applied the coding scheme to each additional transcript to analyze content relating to willingness to pay. Coded segments of the text were sorted, and similar themes were then grouped into broad domains.27
RESULTS
Respondent Numbers and Demographics
A total of 167 surveys were administered to 59 women, 53 men, and 55 elders. Respondents were 51% female, with median age of 41 including the elders (Table 1). Excluding elders, male respondents were older than female respondents (median age of 32.5 vs 27.6 years). Women reported having experienced 3.9 pregnancies on average, while men with children reported 5.6 pregnancies experienced by their spouses or partners. Mean monthly household income was 557.2 kwacha ($102 USD). Based on a chi‐square test of trend, there were statistically significant differences between the groups by age, marital status, number of pregnancies reported, and individual income.
Table 1.
Survey Respondents’ Demographic Characteristics and Attitudes
| Characteristic | Womena (n = 59) | Menb (n = 35) | Elders (n = 55) | Total (N = 167) |
|---|---|---|---|---|
| Female, n (%) | 59 (100) | 0 (0) | 26 (47) | 85 (51) |
| Age, mean (SD), y | 27.6 (8.3) | 32.5 (6.7) | 64.1 (8.2) | 41.0 (17.9) |
| Married, n (%) | 54 (92) | 53 (100) | 41 (75) | 148 (89) |
| Pregnancies experienced by self or partner, mean (SD) c | 3.9 (2.1) | 5.6 (4.2) | — | 3.3 (3.6) |
| Individual monthly income, mean (SD), kwacha d | 112.2 (161.2) | 573.1 (942.1) | 151.7 (201.0) | 271.5 (585.7) |
| Household monthly income, mean (SD), kwacha d | 518.1 (449.1) | 773.4 (1432.8) | 390.8 (612.9) | 557.2 (927.6) |
| Own mobile phone, n (%) | 42 (71) | 40 (75) | 44 (80) | 126 (76) |
| Distance from health facility, n (%), km | ||||
| < 5 | 22 (37) | 16 (30) | 16 (29) | 54 (32) |
| 5‐10 | 21 (36) | 18 (34) | 21 (38) | 60 (36) |
| > 10 | 16 (27) | 19 (36) | 18 (33) | 53 (32) |
| Shelters are important for the health of mothers and infants, n (%) | ||||
| Agree | 8 (14) | 6 (11) | 7 (13) | 21 (13) |
| Strongly agree | 48 (81) | 46 (87) | 46 (84) | 140 (84) |
| It is worthwhile for someone like me/my wife/my daughter to stay in a shelter, n (%) | ||||
| Agree | 8 (14) | 7 (13) | 9 (16) | 24 (14) |
| Strongly agree | 48 (81) | 46 (87) | 46 (84) | 140 (84) |
Pregnant women or women who had given birth within past 2 years.
Men with children under 2 years of age.
Elders were not asked this question.
Currency is Zambian Kwacha. At the time of the study, 1 kwacha was worth $0.184 USD.
We had 135 participants in 16 focus group discussions. Eleven discussions included only women, 3 included only men, and 2 were mixed groups of men and women.
Knowledge and Experience With Shelters
Respondents had good knowledge and positive attitudes about shelters. Virtually all respondents had heard of shelters, strongly agreed that shelters are important for the health of mothers and newborns, and agreed that it was very worthwhile for a woman to stay at a shelter during the last weeks of her pregnancy. Almost half (46%) of respondents had stayed in a shelter before (or had a spouse, child, or grandchild who had stayed in a shelter); no respondents reported paying a nightly fee to sleep in the shelter. People who used the shelter in the past stayed 9.6 days on average. There were no statistically significant differences in knowledge or experience with shelters between the groups studied.
Willingness to Pay
Table 2 shows the results of the analysis of willingness to pay. Overall, 7 respondents (4%) were not willing to pay any amount to stay in a shelter. Of those willing to pay something, the median maximum willingness to pay per night was 5.0 kwacha ($0.92 USD). Using method 1 (open‐ended probes) women were willing to pay 40% more (7.0 kwacha or $1.29 USD) than men (4.0 kwacha or $0.74 USD), while elders were at the median of 5.0 kwacha. However, looking only at the open‐ended question (method 2), women's willingness to pay was 5.0 kwacha, or 25% more than men or elders, whose willingness to pay was 4.0 kwacha.
Table 2.
Willingness to Pay per Night in a Maternity Waiting Home
| Women (n = 59) | Men (n = 53) | Elders (n = 55) | Total (N = 167) | |
|---|---|---|---|---|
| Not willing to pay any amount, n (%) | 2 (3) | 3 (6) | 2 (4) | 7 (4) |
| Median maximum willingness to pay per night (Method 1), a range, kwacha | 7 (1‐10) | 7 (1‐50) | 5 (1‐10) | 7 (1‐50) |
| Median maximum willingness to pay per night (Method 2), b range, kwacha | 5 (1‐10) | 4.5 (1‐50) | 4.5 (1‐10) | 5 (1‐50) |
| Willing to pay, n (%), kwacha c | ||||
| 5 | 41 (71) | 38 (72) | 30 (55) | 109 (66) |
| 7 | 32 (55) | 26 (49) | 22 (40) | 80 (48) |
| 10 | 18 (31) | 10 (19) | 13 (24) | 41 (25) |
| Maximum no. nights at each price in kwacha, n (SD) | ||||
| 5 | 7.8 (10.0) | 6.8 (6.5) | 5.8 (9.7) | 6.8 (8.9) |
| 7 | 7.3 (5.2) | 5.8 (5.6) | 5.4 (5.7) | 6.2 (5.5) |
| 10 | 4.0 (2.8) | 3.1 (5.1) | 3.2 (3.5) | 3.5 (3.8) |
| Preference for type of fee, n (%) | ||||
| Flat amount per stay | 40 (68) | 32 (60) | 37 (67) | 109 (65) |
| Fee per day | 14 (24) | 16 (30) | 11 (20) | 41 (25) |
| It depends on amount | 5 (8) | 5 (9) | 7 (13) | 17 (10) |
Method 1 calculates the median using the probe‐method of analysis (highest price explicitly agreed to based on pricing probe questions or open‐ended question on maximum willingness to pay). Excludes those who were not willing to pay any amount (2 women, 3 men, 2 elders). Total N = 160.
Method 2 calculates the median using only the answer to the open‐ended question on maximum willingness to pay. Excludes those who were not willing to pay any amount (2 women, 3 men, 2 elders) and one elder who did not answer the open‐ended question. Total N = 159.
Currency is Zambian kwacha. At the time of data collection (Oct‐Nov 2013) 1 kwacha was worth 0.184 USD; 5 kwacha was worth $0.92 USD, 7 Kwacha was worth $1.29 USD, and 10 kwacha was worth $1.84 USD.
Using the highest amount in response to the price probes or the open‐ended willingness to pay question (method 1), we found that 84% to 90% of respondents were willing to pay between 1 and 5 kwacha ($0.18‐$0.92 USD) per night of stay (see Supporting Information: Appendix S1). Figure 1 calculates the percentage of users who would be excluded at different price points; a suggested donation of 2 kwacha ($0.37 USD) per night would exclude 14.4% of users, while a suggested donation set at 5 kwacha ($0.92 USD) would exclude 31.7% of users. “Users excluded” reflects the flip side of willingness to pay, a salient consideration in most lower‐income countries.
Figure 1.
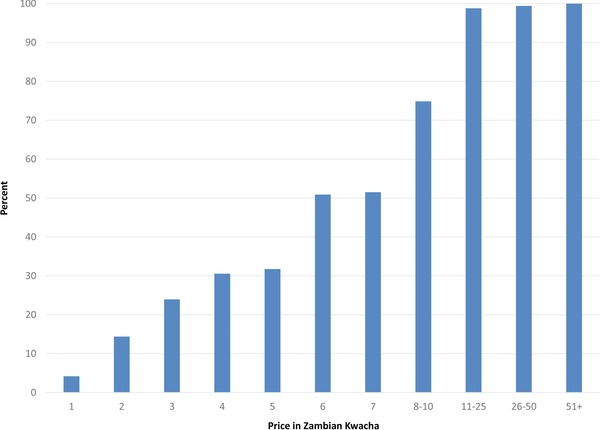
Percent of Users Excluded at Different Price Points, Based on Willingness to Pay for All Respondents Combined (Women, Men and Elders).
We did not find significant correlations between willingness to pay and distance from a health facility; however, we observed a significant correlation (0.61, P < .001) between income and maximum willingness to pay. Those with higher reported individual or household income were willing to pay more for a night of stay.
A majority of respondents (65%) preferred to pay a flat total amount per stay, rather than paying per night.
Focus Group Discussions
Four broad domains emerged from the qualitative analysis: 1) perceptions of affordability, 2) fee type preferences, 3) the relationship between quality and willingness to pay, and 4) reasons or actions related to unwillingness to pay.
Affordability
Focus group participants discussed the affordability of different rates per night and per stay. While willingness to pay depended on the expected length of stay, flat rates per stay of 40, 50, and even 100 kwacha ($7.36‐$18.40 USD) were thought by some to be affordable, especially if food and bedding were provided. A common theme was that if the total amount is known in advance, women should be able to plan ahead and save the funds needed. One participant noted, “When you get pregnant, you don't deliver the following day. You have 9 months to plan for the delivery.”
Fee Type Preferences
Focus group participants had mixed opinions about contributing on a daily basis versus a flat rate per stay (see Supporting Information: Appendix S2). Those who preferred a flat rate per stay mentioned that it protects against the risk of a large expenditure if a woman does not give birth right away and has an extended shelter stay. In such a case, having paid a flat rate gives the waiting woman peace of mind, and participants noted that the woman is able to plan for the fee and save the money ahead of time. A participant observed, “A woman can start saving money soon after knowing she is pregnant. … She will pay that money and not worry about paying daily.” Paying a flat rate in advance also alleviates the risk that the money will be spent on other things or stolen during the stay.
Those who preferred a daily rate said it was fairer because one would pay only for the days actually used. Proponents said it was then possible to only pay for a day or 2, which might be less expensive than the flat rate, considering the average length of stay for all women. One participant voiced concern that a flat fee might incentivize people to stay a long time at the shelter, “Paying every day is better because if there is a flat fee, mothers will opt to stay longer. They may even come at 8 months so that they are sure to use their money.”
Shelter Quality and Willingness to Pay
Participants often stated that their willingness to pay was contingent on good quality. They were willing to pay if the shelter had amenities such as beds and mattresses, water and lighting, and food. The participants shared: “The price people are willing to pay will depend on what the community says after seeing the way the house has been repaired and what furniture is present”; “I feel they can stay because soap, food, and good sleeping is there—aaaa! They will stay”; and “If we will be paying, what we want is electricity, beds, and provision of food.”
Unwillingness to Pay and Alternatives
Focus group participants discussed several reasons for unwillingness to pay, including poverty and cash flow problems: “People cannot manage to pay for their wives to be staying at the shelter because they only find some money annually, after selling their farm produce.” The fact that staying at a shelter incurs additional costs for food was also noted: “When a pregnant woman stays at the shelter, she has to buy her own food as if she was staying in town. Everything she has to buy.” Some respondents said they needed to spend their limited resources on food for the family, rather than the shelter.
When asked what a woman would do if she could not afford the price, participants suggested she might give birth at home: “The women would not come to stay at the shelter if the price was beyond what we can afford to pay.” Other options were to offer to work at the shelter or try to pay in‐kind: “It is good as long as the vegetables you give are of the same amount to what your friends pay in cash.” Participants also suggested that the husband might try to negotiate a lower rate or offer to pay later. A few respondents emphasized that the money would be found somehow because they value the service: “There is nothing we can do—we will be paying because we want to be helped. That's why we come here”; and “We are going to follow what they will say because what we need here is development.”
Many participants mentioned they could barter food items which could be sold by the managers of the shelter for cash or which might be used in the food service. Items included chickens, goats, ground nuts, maize, charcoal, fire wood, or bricks. Women also said they would be willing to engage in chores such as cleaning, cooking, making beds, washing linens, working in the garden, or weeding the shelter surroundings. “It is OK to do barter services because some people can manage to give a chicken, even if they have no money,” said one participant, while another noted that “Both barter and working can work for those who don't have money.”
DISCUSSION
This study examined willingness to pay for a night of stay in a maternity waiting home. We found that most women, men, and elders were willing to pay at least a small sum, suggesting that they would gain utility and satisfaction from this service. The median maximum willingness to pay for a night of stay was 5 kwacha ($0.92 USD). Willingness to pay of pregnant or recently pregnant women was higher than men or elders, and correlated with income, as expected. Willingness to pay did not seem to be related to distance from facility in our study, which is different from some studies that report that distance is negatively related to willingness to pay for some health services.28, 29 Yet another recent study reported mixed findings on the relationship between distance and willingness to pay, with rural residents sometimes willing to pay more than urban residents for health care quality improvements.30
Most respondents preferred to pay a flat amount per stay, and study participants saw value in knowing in advance how much the stay would cost so they could plan. The findings align with qualitative research done in a different region of Zambia, which found that women were willing to pay a small fee for a shelter stay if they could be assured that the facility would offer high‐quality, respectful services.12
Our study found that many respondents were willing to pay less when asked the open‐ended question compared to when they were asked specific price probes. This could be because the price probe questions were asked in a different format (eg, “Suppose that the price of a night of stay in the mothers’ shelter is 5 kwacha. Would you stay at the mothers’ shelter if the price were 5 kwacha per night?” compared to the open‐ended question, “What would be the highest price you would be willing to pay per night of stay in the mothers’ shelter?”) The formulation of the price probe question assumes the price has been set, and the respondents are being asked if they would accept this set price. According to the Hofstede model of dimensions of national culture, Zambia is a hierarchical society where less powerful members “expect and accept that power is distributed unequally … centralization is popular, subordinates expect to be told what to do, and the ideal boss is a benevolent autocrat.”31 In such a setting, respondents may have felt it was natural to accept a price determined by a “benevolent” authority. Yet when asked the open‐ended question, which was more clearly soliciting the respondent's own opinion, they felt free to express a lower willingness to pay.
Our theory of change suggests that if women utilize maternity homes, they will then give birth at a facility where complications are more likely to be managed appropriately, resulting in better clinical outcomes. However, it is important to identify strategies to sustain the shelters. Overall, our results suggest potential for community contributions to increase the long‐term financial sustainability of the maternity waiting homes. The average monthly census per maternity home is expected to be approximately 15 to 20. Assuming a relatively affordable fixed fee of 20 kwacha per stay (based on 2 kwacha for 10 days of stay), a shelter might expect revenue of 300 to 400 kwacha ($55‐$74 USD) per month. What we do not know is whether the respondents’ stated willingness to pay would translate into actually paying for the services.
Additionally, findings show that Zambians have high expectations for service quality. This is an important consideration when building or renovating shelters, particularly if the intervention will be taken to scale. Furnishings and food seem especially important. Currently when women stay in shelters, they often do not have to pay, but they must cook for themselves, bring their own bedding, and sleep on the floor. If the provision of food improves utilization, it may be beneficial but will be an added cost. It will be important to determine the recurrent cost for a renovated shelter that provides food and to assess this cost in relation to willingness to pay. Given that a price of 3 kwacha ($0.55 USD) per night already excludes 24% of users, other sources of financing will likely be needed to supplement community contributions.
Importantly, our qualitative findings suggest that pregnant women who cannot afford the suggested donation at the maternity waiting home are likely to give birth at home. An annual collection from community members at harvest time might be an alternative method to cover operating costs. Such a strategy could tap into community members’ willingness to contribute while avoiding the need to operate an exemption system for those too poor to pay or unable to pay at the time of need. Additionally, a system allowing women to perform light housekeeping or gardening, or to barter food items, could be established to defray operating costs, keeping access affordable.
Our study has several limitations. Women's preferences for birth‐related care, including maternity home stay, may change over the course of the pregnancy, and the optimum time to measure willingness to pay in this population is not known.32 Our study interviewed women who were pregnant or had recently given birth, as well as men who had a child under 24 months of age. It is possible that if informants were interviewed at another point (eg, men were interviewed when their wives were again pregnant), estimates would vary.
CONCLUSION
This study explored community interest in maternity waiting homes, factors that influence the decision to use shelters prior to labor and birth, and willingness to contribute to a stay at the shelter. Findings suggest that women and their families may be willing to contribute to a maternity waiting home that meets standards and expectations. Participants identified options for mobilizing support for shelters while recognizing that not all women may be able to pay for services.
While shelters could increase access to skilled care for labor and birth, they would be an added cost to the Zambian health system. The findings may help health professionals and communities as they consider scaling‐up maternity waiting homes in Zambia. However, given the preference for the provision of food, costs to ensure high quality, and the uncertainty of whether stated willingness to pay would translate into actual contributions, it is important to explore other channels for financial sustainability of shelters. Important next steps would be to determine the operating costs for improved homes; assess costs against willingness to contribute; and develop and test approaches in order to refine an overarching sustainability strategy for maternity waiting homes.
CONFLICT OF INTEREST
The authors have no conflicts of interest to report.
Supporting information
Appendix S1. Percent of Respondents Who are Willing to Pay 1–5, 6–9, and 10+ Zambian Kwacha for a Night's Stay in Maternity Waiting Home
Appendix S2. Focus Group Participants’ Opinions Regarding Payment Modes
ACKNOWLEDGMENTS
The activities discussed in this publication were supported by funding from Merck through its Merck for Mothers program (Grant GHH‐I‐00‐07‐0023‐00). The content of this publication is solely the responsibility of the authors and does not represent the official views of Merck. Thank you to Jacob Bor for his ideas on data presentation.
Biographies
Taryn Vian, SM, PhD, is Associate Professor and the Associate Chair for Education in the Department of Global Health at the Boston University School of Public Health. She is also faculty director of the dual‐degree MBA‐MPH degree at Boston University.
Emily E. White, MPH, is a data analyst at Last Mile Health. Her work focuses on research and evaluation of global health programs and interventions to improve the health status of women and children in low‐resource settings in Liberia and Zambia.
Godfrey Biemba, MBChB, MSc, is Assistant Professor of Global Health at Boston University School of Public Health. He is also country director of the Zambia Centre for Applied Health Research and Development (ZCAHRD) Limited.
Kaluba Mataka, MSc, is project director of the Increasing Equitable Access to Safe Delivery in Southern and Eastern Province, Zambia. She oversees the project's field operations in the targeted provinces.
Nancy Scott, MPH, DrPH, is currently the principal investigator of the Increasing Equitable Access to Safe Delivery in Southern and Eastern Province, Zambia, and Assistant Professor in the Department of Global Health at the Boston University School of Public Health.
[The copyright line for this article was changed on February 9, 2018, after original publication.]
REFERENCES
- 1. Harrison MS, Ali S, Pasha O, et al. A prospective population‐based study of maternal, fetal, and neonatal outcomes in the setting of prolonged labor, obstructed labor and failure to progress in low‐ and middle‐income countries. Reprod Health. 2015;12(Suppl 2):S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323‐e333. [DOI] [PubMed] [Google Scholar]
- 3. McClure EM, Saleem S, Goudar SS, et al. Stillbirth rates in low‐middle income countries 2010‐2013: a population‐based, multi‐country study from the Global Network. Reprod Health. 2015;12(Suppl 2):S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kes A, Ogwang S, Pande R, et al. The economic burden of maternal mortality on households: evidence from three sub‐counties in rural western Kenya. Reprod Health. 2015;12(Suppl 1):S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Central Statistical Office Zambia, Ministry of Health, ICF International . Zambia Demographic and Health Survey 2013‐14. Rockville, MD: Central Statistical Office, Ministry of Health and ICF International; 2014. [Google Scholar]
- 6. Sialubanje C, Massar K, van der Pijl MS, Kirch EM, Hamer DH, Ruiter RA. Improving access to skilled facility‐based delivery services: women's beliefs on facilitators and barriers to the utilisation of maternity waiting homes in rural Zambia. Reprod Health. 2015;12:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sialubanje C, Massar K, Hamer DH, Ruiter RA. Reasons for home delivery and use of traditional birth attendants in rural Zambia: a qualitative study. BMC Pregnancy Childbirth. 2015;15(1):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sacks E, Vail D, Austin‐Evelyn K, et al. Factors influencing modes of transport and travel time for obstetric care: a mixed methods study in Zambia and Uganda. Health Policy Plan. 2015;31(3):293‐301. [DOI] [PubMed] [Google Scholar]
- 9. Campbell OM, Graham WJ, Lancet Maternal Survival Series steering group. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368(9543):1284‐1299. [DOI] [PubMed] [Google Scholar]
- 10. Otolorin E, Gomez P, Currie S, Thapa K, Dao B. Essential basic and emergency obstetric and newborn care: from education and training to service delivery and quality of care. Int J Gynaecol Obstet. 2015;130(Suppl 2):S46‐S53. [DOI] [PubMed] [Google Scholar]
- 11. Kruk ME, Rabkin M, Grepin KA, et al. “Big push” to reduce maternal mortality in Uganda and Zambia enhanced health systems but lacked a sustainability plan. Health Aff (Millwood). 2014;33(6):1058‐1066. [DOI] [PubMed] [Google Scholar]
- 12. Lori J, R. , Mdluli EA, Chimedza PP, Musonda GK, Boyd CJ. Zambian mothers shelters: examining acceptability, feasibility, and sustainability. J Midwifery Womens Health. 2015;60(5):639‐640. [Google Scholar]
- 13. Lee AC, Lawn JE, Cousens S, et al. Linking families and facilities for care at birth: what works to avert intrapartum‐related deaths? Int J Gynaecol Obstet. 2009;107(Suppl 1):S65‐85, S86‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Andemichael G, Haile B, Kosia A, Mufunda J. Maternity waiting homes: a panacea for maternal/neonatal conundrums in Eritrea. J Eritrean Med Assoc. 2009;4(1):18‐21. [Google Scholar]
- 15. Kelly J, Kohls E, Poovan P, et al. The role of a maternity waiting area (MWA) in reducing maternal mortality and stillbirths in high‐risk women in rural Ethiopia. BJOG. 2010;117(11):1377‐1383. [DOI] [PubMed] [Google Scholar]
- 16. Lori JR, Munro ML, Rominski S, et al. Maternity waiting homes and traditional midwives in rural Liberia. Int J Gynaecol Obstet. 2013;123(2):114‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van Lonkhuijzen L, Stegeman M, Nyirongo R, van Roosmalen J. Use of maternity waiting home in rural Zambia. Afr J Reprod Health. 2003;7(1):32‐36. [PubMed] [Google Scholar]
- 18. Scott N, Biemba G, Hamer D, et al. Improving Equitable Access to Safe Deliveries in Zambia: Findings From a Formative Evaluation. Boston, MA: Boston University Center for Global Health and Development;2014. [Google Scholar]
- 19. Fleischman Foreit KG, Foreit JR. Willingness to Pay Surveys for Setting Prices for Reproductive Health Products and Services: A User's Manual. New York, NY: The Population Council; 2004. [Google Scholar]
- 20. Gyrd‐Hansen D, Jensen ML, Kjaer T. Framing the willingness‐to‐pay question: impact on response patterns and mean willingness to pay. Health Econ. 2014;23(5):550‐563. [DOI] [PubMed] [Google Scholar]
- 21. Olsen JA, Smith RD. Theory versus practice: a review of “willingness‐to‐pay” in health and health care. Health Econ. 2001;10:39‐52. [DOI] [PubMed] [Google Scholar]
- 22. Dudgeon MR, Inhorn MC. Men's influences on women's reproductive health: medical anthropological perspectives. Soc Sci Med. 2004;59(7):1379‐1395. [DOI] [PubMed] [Google Scholar]
- 23. Cofie LE, Barrington C, Singh K, Sodzi‐Tettey S, Akaligaung A. Birth location preferences of mothers and fathers in rural Ghana: implications for pregnancy, labor and birth outcomes. BMC Pregnancy Childbirth. 2015;15:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Some DT, Sombie I, Meda N. How decision for seeking maternal care is made—a qualitative study in two rural medical districts of Burkina Faso. Reprod Health. 2013;10:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Iganus R, Hill Z, Manzi F, et al. Roles and responsibilities in newborn care in four African sites. Trop Med Int Health. 2015;20(10):1258‐1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Varkevisser CM, Pathmanathan I, Brownlee A. Designing and Conducting Health Systems Research Projects. Amsterdam, Netherlands: KIT Publishers; 2003. [Google Scholar]
- 27. Corbin J, Strauss A. Basics of Qualitative Research. Third Edition. Thousand Oaks, CA: Sage Publications, Inc; 2008. [Google Scholar]
- 28. Aleme A, Girma E, Fentahun N. Willingness to pay for insecticide‐treated nets in Berehet District, Amhara Region, Northern Ethiopia. Implication of social marketing. Ethiop J Health Sci. 2014;24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dong H, Kouyate B, Snow R, Mugisha F, Sauerborn R. Gender's effect on willingness‐to‐pay for community‐based insurance in Burkina Faso. Health Policy. 2003;64. [DOI] [PubMed] [Google Scholar]
- 30. Pavel MS, Chakrabarty S, Gow J. Assessing willingness to pay for health care quality improvements. BMC Health Services Research. 2015;15(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hofstede Center . Zambia country comparison http://geert-hofstede.com/zambia.html. Published 2015. Accessed December 22, 2015.
- 32. Donaldson C, Hundley V, Mapp T. Willingness to pay: a method for measuring preferences for maternity care? Birth. 1998;25(1):32‐39. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Percent of Respondents Who are Willing to Pay 1–5, 6–9, and 10+ Zambian Kwacha for a Night's Stay in Maternity Waiting Home
Appendix S2. Focus Group Participants’ Opinions Regarding Payment Modes


