Abstract
Background and Aims
Considerable variation of outcome variables used to measure recovery in the gambling treatment literature has precluded effective cross‐study evaluations and hindered the development of best‐practice treatment methodologies. The aim of this systematic review was to describe current diffuse concepts of recovery in the gambling field by mapping the range of outcomes and measurement strategies used to evaluate treatments, and to identify more commonly accepted indices of recovery.
Methods
A systematic search of six academic databases for studies evaluating treatments (psychological and pharmacological) for gambling disorders with a minimum 6‐month follow‐up. Data from eligible studies were tabulated and analysis conducted using a narrative approach. Guidelines of the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) were adhered to.
Results
Thirty‐four studies were reviewed systematically (RCTs = 17, comparative designs = 17). Sixty‐three different outcome measures were identified: 25 (39.7%) assessed gambling‐specific constructs, 36 (57.1%) assessed non‐gambling specific constructs, and two instruments were used across both categories (3.2%). Self‐report instruments ranged from psychometrically validated to ad‐hoc author‐designed questionnaires. Units of measurement were inconsistent, particularly in the assessment of gambling behaviour. All studies assessed indices of gambling behaviour and/or symptoms of gambling disorder. Almost all studies (n = 30; 88.2%) included secondary measures relating to psychiatric comorbidities, psychological processes linked to treatment approach, or global functioning and wellbeing.
Conclusions
In research on gambling disorders, the incorporation of broader outcome domains that extend beyond disorder‐specific symptoms and behaviours suggests a multi‐dimensional conceptualization of recovery. Development of a single comprehensive scale to measure all aspects of gambling recovery could help to facilitate uniform reporting practices across the field.
Keywords: Gambling disorder, intervention, outcome measures, problem gambling, recovery, systematic review, treatment outcome
Introduction
Treatment outcomes for gambling disorders are defined poorly and measured inconsistently across studies 1, 2. In particular, the concept of recovery itself is rarely operationalized, with outcomes referring variably to abstinence, controlled gambling or broader psychosocial or other impacts 3. Lack of conceptual clarity and consensus on operational criteria in defining and measuring recovery compromises the capacity to determine which treatment interventions achieve optimal outcomes 4. Establishing uniform operational criteria would facilitate meaningful cross‐study evaluations that enable researchers to determine the relative efficacy of treatments. The development of meta‐analytical techniques has provided a powerful statistical tool to combine data between studies and calculate overall effect sizes. Although moderate heterogeneity among studies is to be expected in meta‐analysis, high degrees of inconsistency can seriously limit its application and validity 5, 6, 7.
Analogous to gambling disorders, the substance use disorders (SUDs) field also demonstrates inconsistency in the outcomes and metrics utilized to quantify treatment success 8. There is no consensus regarding best‐practice outcomes for SUD clinical trials, and the field is yet to adopt a core set of ‘ancillary’ domains or optimal methods of assessment 9. The relative importance of specific outcomes is fuelled by differences in intervention type (behavioural, pharmacological), therapeutic targets (abstinence, controlled use) and expectations of stakeholders (clinician, researcher, client or policymaker) 10.
Despite this, the SUD field accepts that recovery is the fundamental goal of treatment programmes, and hence the benchmark for evaluating treatment efficacy 11, 12, 13, 14, 15, 16. Recovery, in a contemporary sense, refers broadly to improvements extending beyond target problem symptoms to pertinent functional areas and quality of life domains 16. A scoping review conducted by Laudet 17 identified psychometrically validated measures of recovery across several addiction fields. She found that, in contrast to the mental health field, no dedicated measure of recovery existed for addictions, despite the evident need. In response, Neale et al. 18 developed and validated the first instrument designed specifically to assess recovery in SUD populations (Substance Use Recovery Evaluator; SURE). Reflecting the more ‘inclusive’ approach to recovery, the scale comprises five factors, one specific to substance use and the remaining four assessing a range of life areas (material resources, outlook on life, self‐care and relationships) 18, 19, 20.
Similarly, the gambling field has moved to establish a core set of reporting standards for treatment studies. A frequently cited paper by Walker et al. 21 describes a reporting framework constructed by an expert panel (the ‘Banff Consensus’), including three relevant outcome domains. The first includes measures of gambling frequency and expenditure, although such outcomes are known to be inherently difficult to measure. The alcohol field has established a standardized unit of consumption that is related directly to personal risk of alcohol‐related harm 22. In contrast, a standardized unit of gambling is not possible, as the negative consequences associated with gambling expenditure are contingent upon the gambler's unique financial resources. Additionally, there are no biological markers of gambling behaviour as there are with substance use (e.g. blood alcohol). Consequently, measuring levels of involvement relies entirely upon self‐report methods, which have been shown to be unreliable 23, 24, 25, 26, 27. Although Walker et al.’s 21 paper aims to facilitate cross‐comparability of outcomes, it does not endorse specific instruments designed to assess each domain. Consequently, researchers are afforded significant flexibility relating to their selection of appropriate instruments, which may contribute to the variability of reported outcomes in treatment studies.
Other than investigations of ‘natural recovery’ 28, 29, there is a distinct lack of literature addressing how recovery as an outcome should be operationalized and measured in gambling disorders. Nower & Blaszczynski 4 proposed a spectrum of recovery that includes improvements across several areas. At the fundamental level, recovery is described as decreased time and money spent gambling not leading to added consequences. The highest level represents an absence of negative consequences and sustained improvements in quality of life over time. There appears to be more acceptance of controlled use in alcohol and gambling disorders compared to illicit drug use. This may be because of their relative legality and, hence, social acceptability; or because lower levels of consumption are perceived to be comparatively safe 30, 31. Furthermore, there is a growing body of literature demonstrating the viability of moderation‐based treatment goals and their link to positive treatment outcomes 32, 33, 34, 35.
The degree to which gambling treatment studies have adhered to reporting standards advanced by the Banff Consensus 21 is unclear. Additionally, there is no indication of the impact of early conceptualizations of recovery 4 on determining relevant metrics of treatment success. The purpose of this paper was to detail how recovery is portrayed currently in the gambling field by extracting and mapping the range of outcome variables used to evaluate treatment efficacy. Identifying outcome variables that are commonly utilized provides one indication of their relative importance to recovery, as perceived by researchers. The derived information will help the field move closer towards a unified operationalization of recovery and attendant measurement criteria, thus maximizing the potential for advancements in therapy. Although studies have commented previously on the inconsistent reporting standards in the gambling treatment literature 2, 4, 21, 36, this systematic review is the first to document rigorously the degree of variability and present clinically relevant domains of recovery based on empirical data.
Methods
A systematic literature review was undertaken in accordance with guidelines outlined by the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) 37. The protocol details of this systematic review were registered with the International Prospective Register of Systematic Reviews (PROSPERO) under the registration code: CRD42016039905.
Search strategy
The following databases were searched for peer‐reviewed journal papers published between 2005 and 2016: (1) PsycINFO, (2) Scopus, (3) PubMed, (4) Medline, (5) Web of Science and (6) Google Scholar. The search strategy included the following terms: gambl* AND (problem* OR patholog* OR disorder*) AND (treatment OR therap* OR intervention) AND (outcome OR variable OR metric OR measure OR criteri*) AND (recover* OR success* OR respon* OR effective* OR efficacy). Additional hand‐searches were conducted on the bibliography and ‘cited by others’ section of key papers, and recent literature reviews of gambling disorder treatments 38, 39, 40, 41, 42, 43, 44.
Screen for eligibility
Titles and abstracts of the initial search results were screened. Articles deemed relevant were downloaded into Zotero—a reference collection and organization tool. Two reviewers screened the full texts independently to determine eligibility. The eligibility criteria consisted of: (1) an adult treatment‐seeking sample of n > 10 with a primary gambling disorder diagnosis (based on validated metrics; > 3 DSM‐IV‐TR, > 4 SOGS, > 5 PGSI; see 45, 46, 47); (2) treatment interventions for gambling disorders excluding harm‐minimization strategies (i.e. pre‐commitment, self‐exclusion, personalized feedback, warning messages); (3) fully or quasi‐randomized controlled trials, prospective cohort and descriptive/case–series designs; and (4) quantitative outcomes reported over at least 6 months of follow‐up post‐baseline assessment.
Quality assessment
Design quality and risk of bias was assessed independently by two reviewers using the Meta‐Analysis of Statistics Assessment and Review Instrument (MAStARI) 48. The MAStARI was applied because it provides separate criteria relevant to specific study designs, including randomized controlled trials (RCTs), cohort/case–controlled studies and observational/descriptive studies. Inter‐rater reliability was calculated (criteria agreed upon/total number of criteria) and any discrepancies that could not be resolved between the two reviewers were mediated by a third reviewer. Studies were classified as ‘high’ (> 75% criteria met), ‘moderate’ (50–75% criteria met) and ‘low’ (< 50%). Papers that met fewer than 25% of criteria were deemed unacceptable for review and were removed from remaining analyses.
Data extraction and summary
Data from the selected studies were tabulated in the following format: author and publication year, country, sample characteristics, intervention type, study design and ranking, follow‐up duration, gambling and non‐gambling specific outcome measure, and whether treatment success or recovery were defined. Study designs were ranked according to the National Health and Medical Research Council's (NHMRC) 49 levels of evidence and grading system. The extracted data were summarized using a narrative approach with a focus on treatment outcome type. Meta‐analytical techniques were not utilized, as the aims of the review were not to evaluate relative treatment effectiveness.
Results
Study selection
The initial search yielded more than 1400 citations (see Fig. 1). Given the vast number of results returned by Google Scholar (29 000 results), screening in Google Scholar ceased 10 pages (10 results per page) after the last eligible reference was returned. One hundred and seventy papers were screened and retained initially. The hand‐search method identified a further 27 relevant papers. After applying the eligibility criteria to 197 papers, a total of 34 papers were retained in the final review (Fig. 1). Inter‐rater reliability between the two reviewers was good, with initial agreement on 87.82% of papers, ĸ = 0.673, 95% confidence interval (CI) = 0.55, 0.79. The most common reasons for exclusion fell under design issues (see Fig. 1). One paper was excluded because it did not meet minimum quality assessment standards (< 25% MAStARI rating; described in Methods).
Figure 1.
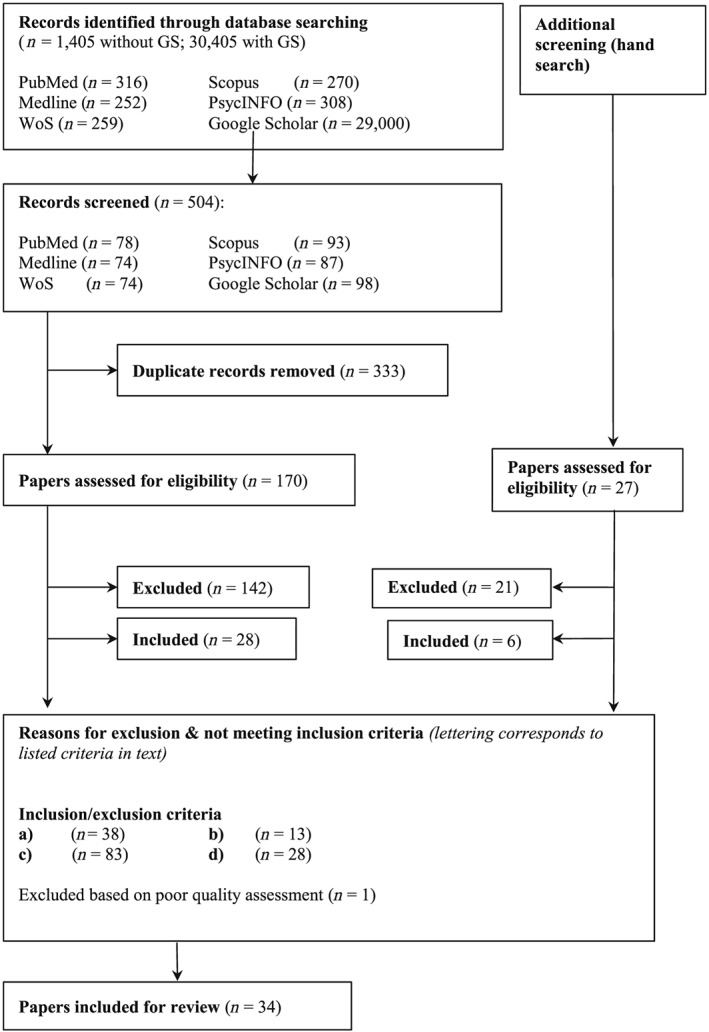
Consort diagram adapted from Zorzela et al. (2016) 89
Quality assessment
Seventeen RCT studies and 17 comparative designs: two cohort/case–control studies and 15 observational/descriptive studies were assessed using the corresponding MAStARI criteria. Overall inter‐rater reliability for quality assessment between the two reviewers was 73.5%. A third reviewer was enlisted to resolve three items of discrepancy. Studies were on average classified as of ‘moderate’ quality [mean = 68.61%; standard deviation (SD) = 13.72]. Quality assessment for each of the three research designs can be seen in their respective tables (Tables 1, 2 and 3).
Table 1.
Results of quality assessment for randomized controlled trial (RCT) studies [based on Joanna Briggs Institute Meta Analysis of Statistics Assessment and Review Instrument (JBI MAStARI) checklist criteria].
| Study | Assessment quality criteria | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| Carlbring et al. (2010) 90 | + | NA | + | + | ? | ? | − | + | − | + | 55.6% |
| Carlbring & Smit (2008) 91 | + | NA | + | + | + | + | + | − | + | + | 88.9% |
| Dowling et al. (2006) 53 | ? | NA | ? | − | ? | + | + | + | + | + | 55.6% |
| Grant et al. (2011) 78 | + | NA | ? | − | + | + | − | + | + | + | 66.7% |
| Grant et al. (2014) 92 | ? | + | ? | ? | ? | + | + | + | + | + | 60.0% |
| Hodgins et al. (2007) 82 | ? | + | ? | + | + | + | + | + | ? | + | 70.0% |
| Korman et al. (2008) 93 | ? | NA | ? | + | − | + | − | + | + | + | 55.6% |
| Lloret et al. (2014) 75 | − | NA | ? | + | ? | + | − | + | + | + | 55.6% |
| Marceaux & Melville (2011) 94 | ? | NA | ? | + | ? | + | + | + | + | + | 66.7% |
| McIntosh et al. (2016) 66 | ? | NA | ? | + | ? | − | + | + | + | + | 55.6% |
| Myrseth et al. (2011) 76 | + | − | − | + | − | + | + | + | + | + | 70.0% |
| Petry et al. (2006) 72 | + | NA | ? | + | ? | + | + | + | + | + | 77.8% |
| Rosenberg et al. (2013) 68 | ? | ? | ? | ? | ? | + | + | + | + | ? | 40.0% |
| Rossini‐Dib et al. (2015) 73 | − | NA | ? | + | ? | NA | + | + | + | + | 62.5% |
| Saiz‐Ruiz et al. (2005) 81 | ? | + | ? | + | + | + | + | + | + | + | 80.0% |
| Smith, Battersby, et al. (2015) 95 | + | + | + | + | + | + | + | + | + | + | 100.0% |
| Toneatto et al. (2009) 96 | ? | + | + | + | + | + | + | + | + | + | 90.0% |
Criteria: (1) Assignment to treatment group truly random. (2) Participants blinded to treatment allocation. (3) Allocation to treatment groups concealed from allocator. (4) Outcomes of people who withdrew described and included in analysis. (5) Researchers assessing outcomes blind to treatment allocation. (6) Control and treatment group comparable at entry. (7) Groups treated identically other than for named interventions. (8) Outcomes measured in the same way for all groups. (9) Outcomes measured in a reliable way. (10) Appropriate statistical analysis used.
+ = yes; − = no; ? = not enough information; NA = not applicable.
Table 2.
Results of quality assessment for comparable cohort/case–control studies [based on Joanna Briggs Institute Meta Analysis of Statistics Assessment and Review Instrument (JBI MAStARI) checklist criteria].
| Study | Assessment quality criteria | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| Odlaug et al. (2013) 71 | + | + | + | + | + | ‐ | + | + | + | 88.9% |
| Ramos‐Grille et al. (2015) 97 | + | + | + | ‐ | + | ‐ | + | ? | + | 66.7% |
Criteria: (1) Sample is representative of patients in population as a whole. (2) Patients are at a similar point in the course of their condition/illness. (3) Bias minimized in relation to selection of cases and controls. (4) Confounding factors identified and strategies to deal with them stated. (5) Outcomes assessed using objective criteria. (6) Follow‐up carried out of a sufficient time‐period. (7) Outcomes of people who withdrew described and included in analysis. (8) Outcomes measured in a reliable way. (9) Appropriate statistical analysis used.
+ = yes; − = no; ? = not enough information; NA = not applicable.
Table 3.
Results of quality assessment for observational/ descriptive studies [based on Joanna Briggs Institute Meta Analysis of Statistics Assessment and Review Instrument (JBI MAStARI) checklist criteria].
| Study | Assessment quality criteria | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| Aragay et al. (2015) 57 | + | + | NA | + | + | − | + | + | + | 75.0% |
| Carlbring et al. (2012) 98 | − | + | + | + | + | + | + | + | + | 88.9% |
| Guo et al. (2014) 99 | + | + | − | + | NA | − | + | + | + | 75.0% |
| Jackson et al. (2013) 70 | + | − | − | + | NA | − | + | + | − | 50.0% |
| Jiménez‐Murcia et al. (2015) 74 | + | + | − | + | + | − | + | + | + | 66.7% |
| Jimenez‐Murcia et al. (2007) 55 | + | + | − | + | + | − | + | + | + | 66.7% |
| Ladouceur et al. (2009) 34 | − | + | − | + | + | + | + | ? | + | 66.7% |
| Morefield et al. (2013) 100 | + | − | + | + | NA | + | − | + | + | 75.0% |
| Muller et al. (2016) 58 | + | + | − | + | + | + | + | + | + | 88.9% |
| Myrseth et al. (2013) 79 | − | − | − | + | + | − | + | + | + | 55.6% |
| Sander & Peters (2009) 56 | + | + | − | − | + | + | + | + | + | 77.8% |
| Smith et al. (2010) 101 | + | ? | − | + | + | − | + | + | + | 66.7% |
| Smith, Harvey, et al. (2015) 102 | + | ? | + | + | + | − | − | − | + | 55.6% |
| Tolchard & Battersby (2013) 80 | + | − | − | + | NA | + | + | + | ? | 62.5% |
| Toneatto & Wang (2009) 103 | + | − | − | + | + | − | + | + | − | 55.6% |
Criteria: (1) Was the study based on a random or pseudo‐random sample? (2) Were the criteria for inclusion in the sample clearly defined? (3) Were confounding factors identified and strategies to deal with them stated? (4) Were outcomes assessed using objective criteria? (5) If comparisons were being made, was there sufficient description of groups? (6) Was follow‐up carried out over a sufficient time‐period? (7) Were the outcomes of people who withdrew described and included in the analysis? (8) Were outcomes measured in a reliable way? (9) Was appropriate statistical analysis used?
+ = yes; − = no; ? = not enough information; NA = not applicable.
Characteristics of included studies
Data extracted from the 34 studies are summarized in Table 4. Sample sizes varied considerably and ranged from n = 19 to n = 566 (mean = 144); a greater percentage of participants were male (mean = 71.2%) and the mean age of participants was 41.6 years (SD = 5.95; range = 30.7–55.5). Nationalities were diverse, with several studies originating from Spain, Australia, the United States and Canada. More than half the reviewed studies (n = 18; 52.9%) were designed as RCTs, three of which employed pseudo‐randomization (i.e. non‐random allocation to intervention), and met levels II and III‐1 of the National Health and Medical Research Council (NHMRC) study design hierarchy, respectively. The remainder of the studies reported data from comparative studies (levels III‐2/3), involving pre–post intervention scores.
Table 4.
Study characteristics and treatment outcomes.
| Study | Country | Sample (n, % female, age) | Type of intervention | Design | Follow‐up (post‐treatment, months) | Gambling‐specific outcome(s) | Non‐gambling outcomes(s) | Recovery defined? |
|---|---|---|---|---|---|---|---|---|
| Aragay et al. (2015) 57 | Spain | 566, 8%, 43.5 | CBT | Pre–post level III‐3 | 6 | Lapse, relapse | Dropout | No |
| Carlbring & Smit (2008) 91 | Sweden | 66, 6%, 31.9 | Internet CBT self‐help w/ telephone support | RCT – level II | 6, 18, 36 | NODS | HADS‐A; HADS‐D; QOLI | No |
| Carlbring et al. (2010) 90 | Sweden | 127, 16.5%, 40.5 | MI and CBGT | RCT – level II | 6, 12 | NODS; TLFB (gambl. days/ time/$ wagered–won–lost) | BDI‐II; BAI | No |
| Carlbring et al. (2012) 98 | Sweden | 284, 9%, 32.2 | Internet CBT w/ minimal therapist support | Pre–post level III‐3 | 6, 18, 36 | NODS | HADS‐A; HADS‐D; QOLI | No |
| Dowling et al. (2006) 53 | Australia | 19, 100%, 44.8 | CBT | RCT – level II | 6 | Diary: weekly (freq./time/$ spent); abstinence/ control; DSM‐IV‐TR; GAS | BDI‐II; STAI; CSEI | No |
| Grant et al. (2011) 78 | United States | 68, 38%, 49.0 | IDMI, GA | RCT – level II | 6 | PG‐YBOCS; G‐SAS; PG‐CGI | SDS; HAM‐A; HAM‐D; QOLI | Yes |
| Grant et al. (2014) 92 | United States | 28, 18%, 47.6 | IDMI + N‐acetylcysteine, IDMI + placebo | RCT –level II | 3 | PG‐YBOCS | FTND; HAM‐A; HAM‐D | No |
| Guo et al. (2014) 99 | Singapore | 80, 7.5%, 36.7 | CBT | Pre–post level III‐3 | 3, 6, 12 (baseline) | Abstinence; freq. (monthly); G‐SAS | PWI | No |
| Hodgins et al. (2007) 82 | Canada | 169, 42%, 32 | Relapse prevention booklet | RCT – level II | 6 weeks, 6, 12 (baseline) | TLFB w/ collaterals (gambl. days $ per sess.); GASS; SOGS; NODS; goal achievement | CES‐D | No |
| Jackson et al. (2013) 70 | Australia | 30, 70%, 51–60 | (Re)Making meaning program | Pre–post level III‐3 | 3 | GAMT: fortnight (freq./ time/$ spent); TGQ | K6; WSAS; RSE; DGLS; Social capital | No |
| Jimenez‐Murcia et al. (2015) 74 | Spain | 440, 5.5%, 41.2 | CBGT | Pre–post level III‐3 | 1, 3 | SOGS; relapse | SCL‐90‐R; Dropout | Yes |
| Jimenez‐Murcia et al. (2007) 55 | Spain | 290, 2%, 39.9 | Group CBT | Pre–post level III‐3 | 1, 3, 6 | SOGS; relapse | SCL‐90‐R; Dropout | No |
| Korman et al. (2008) 93 | Canada | 42, 14%, 47.6 | Anger and Addiction Therapy, TAU (CBT) | RCT –level II | 3 | CPGI | DHQ; STAXI | No |
| Ladouceur et al. (2009) 34 | Canada | 89, 52%, 52 | CBT | Pre–post level III‐3 | 6, 12 | DSM‐IV; freq./ time/$ spent (past week); control self‐efficacy; SLUGS; severity/ consequences; erroneous beliefs | QOLI; BDI‐II; BAI | No |
| Lloret et al. (2014) 75 | Spain | 49, 14.3%, 37.8 | CBT, CBT + self‐hypnosis | Level III‐1 | 6 | Abstinence | Dropout | Yes |
| Marceaux & Melville (2011) 94 | United States | 49, 65.3%, 46.57 | Wait list, 12‐step group therapy, CBGT | RCT – level II | 6 | DSM‐IV; control; TLFB (freq./$ spent) | BDI‐II; BAI | No |
| Mcintosh et al. (2016) 66 | Australia | 77, 28.6%, 38.48 | CBT, Mindfulness, TAU (CBT) | RCT – level II | 3, 6 | SOGS; DSM‐5; urges (freq./intensity), days abstinent, freq./$ spent | DASS‐21; FFMQ‐SF; WBSI; RRQ; SF‐12 | Yes |
| Morefield et al. (2013) 100 | Australia | 53, 42%, 43.5 | CBT w/ exposure emphasis | Pre–post level III‐3 | 1, 3, 6, 12 | VGS | K10; GSSI; WSAS | No |
| Muller et al. (2016) 58 | Germany | 76, 5%, 40.3 | CBT + added holistic approaches | Pre–post level III‐3 | 12 | L/BQ; SOGS | RPWB; SCL‐9 | Yes |
| Myrseth et al. (2011) 76 | Norway | 35, 13%, 32.8 | CBT + escitalopram, escitalopram, CBT | RCT – level II | 3, 6 | G‐SAS; PGVAC; PGBS: past week ($ spent/ freq./total time) | BDI‐II | Yes |
| Myrseth et al. (2013) 79 | Norway | 112, 15%, 35.7 | Internet & telephone CBT | Pre–post level III‐3 | 3 | SOGS; GBQ | SCL‐90‐R | Yes |
| Odlaug et al. (2013) 71 | United States | 385, 54%, 43.7 | Individual/group therapy in‐/out‐patient centre (mode unspecified) | Pre–post level III‐3 | 6 | ASI‐PG; TLFB: past month (gamb. days), GAMTOMS; SOGS | Financial concerns; treatment completion | No |
| Petry et al. (2006) 72 | United States | 231, 45%, 44.9 | GA, GA + CBT workbook, GA + CBT | RCT – level II | 6, 12 | ASI‐PG; SOGS; TLFB past month w/ collaterals (gambl. days/$ spent) | BSI | Yes |
| Ramos‐Grille et al. (2015) 97 | Spain | 132, 9%, 39.8 | CBT | Pseudo RCT – level III‐1 | 6 | Relapse | Dropout | No |
| Rosenberg et al. (2013) 68 | Israel | 78, 0%, 30.7 | Naltrexone, bupropion, escitalopram, topiramate | RCT – level II | 1, 6, 24, 48 (baseline) | Abstinence | HAM‐D; HAM‐A; GAF; VAS (well‐being); dropout | No |
| Rossini‐Dib et al. (2015) 73 | Brazil | 72, 44%, 48.6 | Psycho‐ed., psycho‐ed. + group CBT | Pseudo RCT – level III‐1 | 6 (baseline) | GFS; DSM‐5; GBQ | BDI‐II; BAI; BIS‐11; WCST; ROCF; GST; IGT | Yes |
| Saiz‐Ruiz et al. (2005) 81 | Spain | 60, 10%, 38.9 | Sertraline, placebo | RCT – level II | 6 (baseline) | CCPGQ; PG‐CG‐I; VAS (freq./severity/$ spent/improvement); SOGS | EIQ | Yes |
| Sanders & Peters (2009) 56 | Germany | 281, 12%, 38.2 | In‐patient CBT | Pre–post level III‐3 | 12 | Abstinence (12 months); Abstaining (3 months); relapse | No | |
| Smith et al. (2010) 101 | Australia | 127, 46%, 43.1 | ET | Pre–post level III‐3 | 1, 3, 6, 12 (baseline) | VGS ‘harm to self’ subscale; GRCS; GUS | DASS‐21; WSAS | No |
| Smith, Battersby et al. (2015) 95 | Australia | 87, 50%, 46.5 | CT, ET | RCT – level II | 1, 3, 6 | VGS; freq./ time/$ spent (past month); GRCS; GUS | K10; WSAS | No |
| Smith, Harvey et al. (2015) 102 | Australia | 380, 45%, 44.0 | CBT + ET | Pre–post level III‐3 | 1, 3, 6, 12 | VGS ‘harm to self’ subscale | WSAS | No |
| Tolchard & Battersby (2013) 80 | Australia | 205, 58%, 36–45 | CBT | Pre–post level III‐3 | 1, 3, 6, 12 | VAS (statement of main problem) | BDI; BAI; WSAS | Yes |
| Toneatto et al. (2009) 96 | Canada | 52, 7%, 40.0 | Naltrexone + CBT, placebo + CBT | RCT – Level II | 3, 6, 12 | Abstinence; TLFB (freq. Past month $ spent per day) | TLFB: alcohol (freq. past month/ quantity per day) | No |
| Toneatto & Wang (2009) 103 | Canada | 60, 27%, 45.4 | CBT | Pre–post level III‐3 | 6 | Abstinence; CPGI ($ spent); DSM‐IV; severity (11‐Likert); IGS | BSI‐18 | No |
ASI‐PG = Addiction Severity Index‐Problem Gambling; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; BDI‐II = Beck Depression Inventory‐2; BIS‐11 = Barratt Impulsivity Scale; BSI = Brief Symptom Inventory; BSI‐18 = Brief Symptom Inventory 18; CES‐D = Centre of Epidemiologic Studies‐Depressed Mood Scale; CCPGQ = Control of Pathological Gambling Questionnaire; CSEI = Coopersmith Self‐Esteem Inventory; CSQ‐8 = Client Satisfaction Questionnaire‐8; DASS‐21 = Psychological Distress; DGLS = Dejong Giervald Loneliness Scale; DHQ = Drug History Questionnaire; DSM‐5 = Diagnostic and Statistical Manual of Mental Disorders Fifth Edition; DSM‐IV = Diagnostic and Statistical Manual of Mental Disorders Fourth Edition; EIQ = Eysenck Impulsiveness Questionnaire; FFMQ‐SF = Five Factor Mindfulness Questionnaire‐Short Form; FTND = Fagerstrom Test for Nicotine Dependence; G‐SAS = Gambling Symptom Assessment Scale; GAF = Global Assessment of Functioning; GAMT = Gambling Activity Measurement Tool; GAMTOMS = Gambling Treatment Outcome Monitoring System; GAS = Goal achievement Scale; GASS = Gambling Abstinence Self‐efficacy Scale; GBQ = Gambling Beliefs Questionnaire; GFS = Gambling Followup Scale; GSSI = The Goldney Scale of Suicidal Ideation; GRCS = Gambling Related Cognitions Scale; GSI = Global Severity Index; GST = Go‐Stop Test; GUS = Gambling Urges Scale; HADS = Hospital Anxiety & Depression Scale; HAM‐A = Hamilton Anxiety Rating Scale; HAM‐D = Hamilton Depression Rating Scale; IGS = Inventory of Gambling Situations; IGT = Iowa Gambling Task; L/BQ = Lie/Bet Questionnaire; K6 = Kessler 6‐item; K10 = Kessler 10‐item; NODS = NORC DSM‐IV Screen for gambling problems; PGBS = Pathological Gambling Behavioral Scale; PGSI = Problem Gambling Severity Index; PG‐YBOCS = Yale–Brown Obsessive Compulsive Scale Modified for Pathological Gambling; PHQ‐PRIME‐MD = Patient Health Questionnaire; PG‐CGI = Clinical Global Impression Scales for Pathological Gambling; PGVAC = Pathological Gambling Visual Analogue Craving Scale; PWI = Personal Well‐being Index; QOLI = Quality of Life Inventory; ROCF = Rey–Osterrieth Complex Figure Test; RRQ = Rumination Reflection Questionnaire; RSE = Rosenberg Self‐Esteem Scale; RPWB = Ryff's Scales of Psychological Well‐Being; SAS = Social Adaptation Scale; SCL‐9 = Symptom Checklist‐9; SCL‐90‐R = Symptom Checklist‐Revised; SDS = Sheehan Disability Scale; SF‐12 = Short Form Health Survey; SOGS = South Oaks Gambling Screen; SSI = Semi‐structured Interview; STAI = State–Trait Anxiety Inventory; STAXI = State–Trait Anger Expression Inventory; SLUGS = Sydney‐Laval Gambling Scale; TGQ = Temptations for Gambling Questionnaire; TLFB = Timeline follow‐back; TPQ = Treatment Perceptions Questionnaire; VAS = Visual Analogue Scale; VGS = Victorian Gambling Scale; WBSI = White bear Suppression Index; WCST = Wisconsin Card Sorting Test; WSAS = Work and Social Adjustment Scale
CBGT = cognitive behaviour group therapy; CBT = cognitive behaviour therapy; ET = exposure therapy; GA = Gamblers Anonymous; IDPMI = imaginal desensitization plus motivational interviewing; MI = motivational interviewing; TAU = treatment as usual.
Most studies (n = 23; 67.6%) used psychological interventions [e.g. cognitive–behavioural therapy (CBT)], five of the studies evaluated pharmacological interventions, while other interventions included self‐help material, group programmes and miscellaneous psychological techniques (e.g. self‐hypnosis, imaginal desensitization). Large portions of pharmacological and brief intervention studies were excluded because they did not meet the minimum follow‐up period criteria. The median follow‐up duration was 6 months (range = 3–36). Some post‐treatment follow‐up periods could not be determined because the length of treatment was not described, or because treatment was ongoing at the time of follow‐up.
Outcome measures
Among the studies reviewed, 25 (39.7%) primarily gambling‐specific outcome measures (e.g. gambling pathology, severity etc.; see Fig. 2), 36 (57.1%) primarily non‐gambling outcome measures (e.g. depression, anxiety, wellbeing, etc.; see Fig. 3) and two (3.2%) outcome measures utilized for both categories (time‐line follow‐back/diary method and visual analogue scale), were used to assess and evaluate treatment success, response or recovery from gambling problems. Gambling outcome measures were under‐represented in RCTs compared to pre–post‐designed studies (16 : 19), whereas a larger proportion of non‐gambling measures were used in RCTs compared to pre–post‐designed studies (26 : 17). Taking into account the number of times each measure was used, non‐gambling measures overall were used more than gambling outcome measures (65 : 59).
Figure 2.
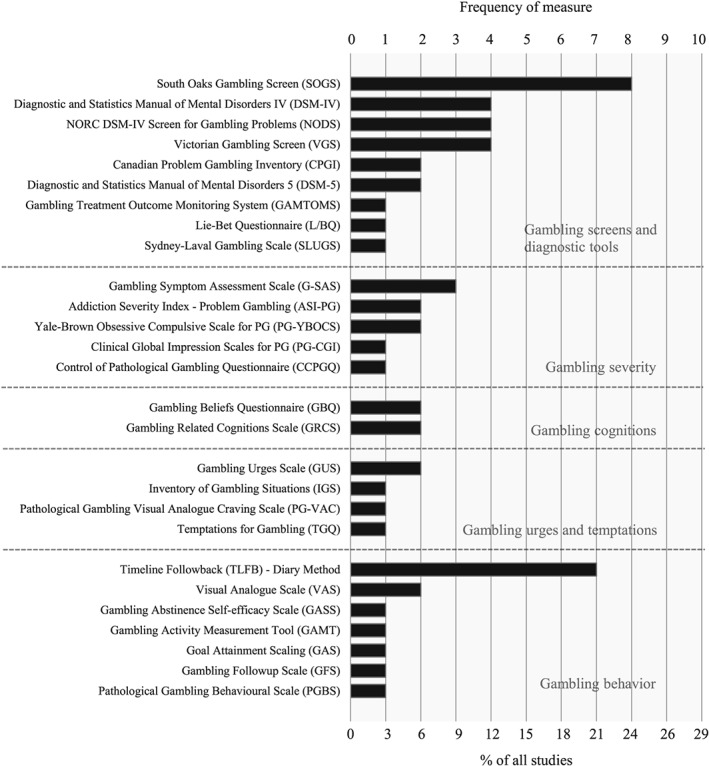
Frequency of gambling specific measures as a percentage of all studies reviewed and separated into outcome domains
Figure 3.
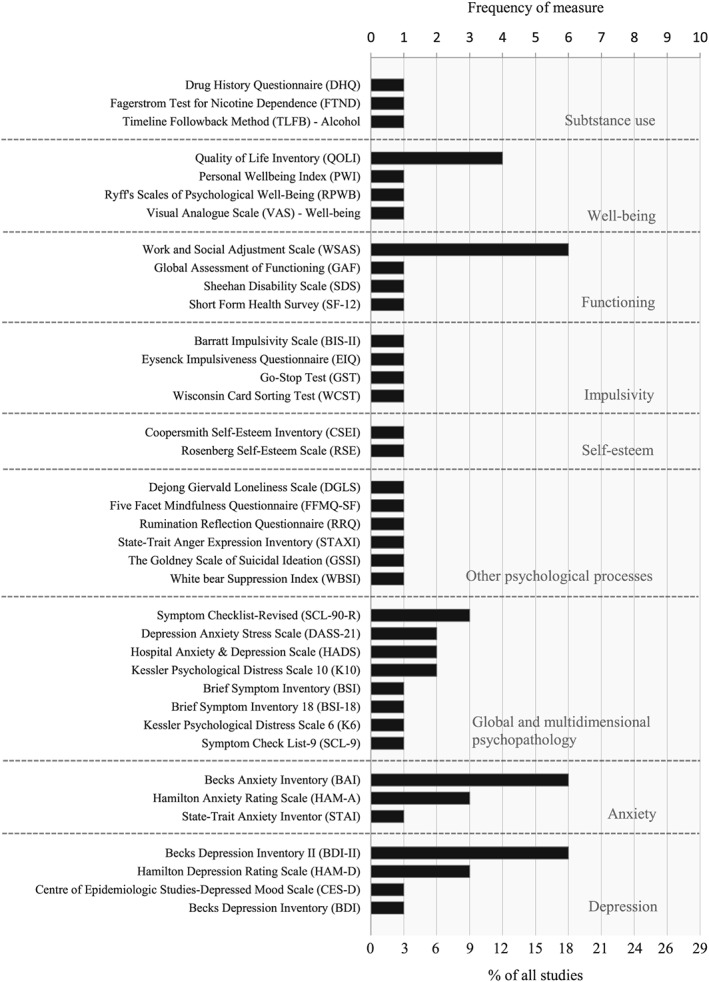
Frequency of non‐gambling measures as a percentage of all studies reviewed and separated into outcome domains
Gambling symptoms and severity
Signs and symptoms of gambling disorders were included as outcome variables in 82.4% (n = 28) of the reviewed studies. Validated self‐report psychometric instruments designed to screen for problem or pathological gambling were most popular. The South Oaks Gambling Screen (SOGS) 50, based on the DSM‐III 51 criteria for Pathological Gambling, was the most frequently employed gambling screen (n = 8; 23.5%) (see Fig. 2). In terms of the reporting metrics used, nine studies analysed significant improvement or reduction of total scores, one study calculated decreases in the percentage of participants fulfilling threshold criteria and four studies reported both. DSM criteria were administered directly to participants in six studies (20.6%); one analysed the number of symptoms endorsed, two reported on changes in gambling disorder prevalence and three studies reported both.
Several studies also employed self‐report measures that evaluated the severity of symptoms during shorter periods (between 1 and 4 weeks); the most frequent was the Gambling Symptom Assessment Scale (G‐SAS) 52 (n = 3). Most of the studies assessing gambling severity reported changes in overall scores (n = 4), three used validated cut‐offs to indicate shifts to minimal or mild symptom severity and one study defined a specific percentage of symptom reduction (35%). One study had participants define their own problem in a short statement and indicate improvement with an eight‐point Visual Analogue Scale (VAS).
A number of studies also analysed specific psychological indicators; these were typically the processes targeted by the intervention, and were linked theoretically to changes in other outcome variables, including gambling behaviour. Gambling urges and cravings, for example, were assessed by five measures throughout seven separate studies (20.6%), and erroneous cognitions about gambling were included as outcomes in five studies (8.8%).
Gambling behaviour
Time and money
Twenty‐four of the included studies (70.6%) measured some aspect of gambling behaviour as an outcome of treatment. The time indices of gambling behaviour were measured in terms of frequency (n = 14; 41.2%) and/or less commonly, duration (n = 6; 17.6%). Studies often used more than one metric to measure frequency and included varied assessments of: days gambled over different time‐frames, gambling episodes, days since last gambled, days binge gambling and ranges from ‘never (0)’ to ‘very often (100)’. Similarly, a variety of assessment metrics were used to measure duration, including hours/minutes spent gambling over the past week, month or gambling day/session.
The other major behavioural aspect of gambling involvement reported was monetary expenditure (n = 13; 38.2%). Gambling expenditure was again assessed during different time‐periods via changes in money wagered, total expenditure, net losses, amount gambled on primary form, money inserted and a scale from ‘nothing (0)’ to ‘very much (100)’. One study included money planned to wager.
The most common measure of gambling activity was the time‐line follow‐back (TLFB) method (n = 6). Two studies included collateral validations (corroborating data from significant others) and structured retrospective questions (n = 4).
Abstinence and relapse
The rates of abstinence and/or relapse were reported in slightly more than half the studies (n = 19; 55.9%). The majority of these studies did not define abstinence explicitly; however, it can be implied by its definition as absolutely no gambling on any form. One study 53 specified abstinence from gaming machines only (i.e. main problem form), another study defined abstinence as fulfilling none of the DSM‐IV‐TR 54 criteria for pathological gambling 55 and the term ‘abstainer’ was proposed in reference to participants who were abstinent for at least 3 months post‐relapse 56. The definition of relapse was also mainly implied as any episodes of gambling during the assessment period where abstinence was the treatment goal 56. Aragay et al. 57, 59 differentiated ‘lapse’—an ‘isolated gambling episode with only mild consequence’—from ‘relapse’—‘two or more consecutive episodes or one episode with loss of control’ (expenditure higher than the week prior to treatment.
Lastly, concepts of controlled gambling were evaluated in two studies (5.9%). This was defined as reduced time and money spent gambling that did not cause adverse consequences 34, and continued gambling in the absence of any DSM‐5 criteria 58.
Psychological functioning
Outcomes not specific to gambling were included as secondary outcomes in all but four studies (88.2%). The most prevalent were self‐report measures of affective disorders. Depression was evaluated in 12 different studies (35.3%), while anxiety was incorporated into 11 (32.4%). The two most popular measures were the Beck Depression Inventory (BDI) 59, 60 (n = 6) and the Beck Anxiety Inventory (BAI) 61 (n = 5), respectively.
Several studies (n = 10; 29.4%) included global and multi‐dimensional measures of psychopathology. Six such measures were used a total of 11 times throughout the 10 studies. The most comprehensive of these was the Symptom Checklist‐90–Revised (SCL‐90‐R) 62 (n = 3), which comprises nine independent mental health symptom dimensions. Other briefer measures that provided psychopathological dimensions and an overall distress composite included the Brief Symptom Inventory (BSI) 63 (n = 2) and the Depression, Anxiety and Stress Scale (DASS‐21) 64 (n = 2).
Treatment outcomes relating to substance use were also included in five studies (14.7%). Inclusion of such outcomes was consistent with the treatment modality and presence of concurrent disorders in the study populations. Additionally, two studies administered the comprehensive Addiction Severity Index (ASI) 65 modified for gambling disorders that provides not only data on patterns of gambling behaviour and substance use, but also the various psychosocial domains which may be affected by addictive disorders.
In several instances, main outcomes were selected based on their appropriateness to the individual research aims or to the intent of treatment within the sample population. For example, McIntosh et al. 66 employed a mindfulness‐based treatment approach to problem gambling, and subsequently evaluated treatment success via outcome variables related to mindfulness practice (cognitive flexibility, thought suppression, etc.).
Global functioning and wellbeing
Global functioning across multiple domains was evaluated as a secondary outcome measure in eight (23.5%) of the studies. Most commonly, the Work and Social Adjustment Scale (WSAS) 67 was employed in six different studies to measure the experiential impact of a gambling disorder on participants’ day‐to‐day functioning. Eight studies (23.5%) included a quality of life outcome measure, with only one of these studies also measuring global functioning 68. The self‐report instrument with the highest frequency of use was the Quality of Life Inventory (QOLI) 69 (n = 4). Two other constructs relevant to this category include social capital (i.e. the subjective value of social networks and bonds) 70 and financial consequences 71, which were measured in both studies with author‐designed questions.
Operationalization of recovery
Approximately one‐third of the reviewed studies (n = 11; 32.4%) provided an operational definition of recovery, or treatment response or success. Four studies defined being recovered as no longer meeting DSM criteria for a gambling disorder, one of which also required a > 50% reduction in gambling frequency and expenditure 66, another > 80% decreased gambling expenditure 72 and one set an additional cut‐off score > 33 on the gambling follow‐up scale 73. Two studies specified that recovery required the maintenance of abstinence during the assessment period 74, 75. Recovered or successful participants were also defined as those scoring between 0–7 on the G‐SAS 76, a > 35% decrease in symptoms based on the (PG‐YBOCS) 77 maintained for at least 1 month at final assessment 78, a SOGS score between 0–2 reflecting no problem 79, a > 50% reduction of a self‐defined ‘main problem’ statement 80, and those responding ‘yes’ to the second (ability to control/resist impulses to gamble) and fourth (substantial decrease in gambling problem) questions of the Control of Pathological Gambling Questionnaire (CCPGQ) 81.
In the studies that did not state explicitly the criteria for treatment success (n = 25; 73.5%), success was implied as the maintenance of abstinence and/or clinically significant improvements in main outcome variables during the treatment and follow‐up periods. Only two studies assessed client treatment goals (i.e. control versus abstinence) and evaluated these at follow‐ups as outcome measures for treatment 34, 82.
Discussion
Thirty‐four treatment studies for gambling disorders, including psychological and pharmacological interventions, met the eligibility criteria for this systematic review. Results revealed a selection of outcome domains that were frequently assessed. Primary domains included gambling symptoms and behaviour. Secondary domains consisted of psychiatric comorbidities, psychological processes relevant to treatment approaches and global functioning and wellbeing. Evolved from early gambling treatment studies that adopt the traditional medical model of pathological gambling (with a singular goal of abstinence 83), this selection of studies incorporated a broad array of outcome domains that represent a multi‐dimensional conceptualization of recovery. This is consistent with the contemporary ‘recovery‐orientated’ model that characterizes the modern framework of addiction treatment services and policy 15, 16, 84, 85, 86.
Operational criteria for measuring recovery in treatment, however, were rarely specified. In the few studies that defined this construct operationally, specific criteria differed significantly, although almost always related to abstaining or the absence of diagnostic criteria for a gambling disorder. Failure to incorporate broader psychosocial outcomes into definitions indicates that researchers, while recognizing their value as supplementary measures, do not perceive such indices as integral to recovery. The finding contrasts with Nower & Blaszczynski's 4 recommendation that treatment studies provide clear conceptualizations of recovery. They argue that in addition to basic reductions of gambling behaviour and symptomatology, definitions should include a combination of indices specifying improvements in gambling urges, psychosocial consequences and quality of life. Furthermore, when operationalized, criteria for recovery were almost always pre‐defined by the investigators and imposed upon participants, despite potential conflicting client goals. For example, participants may want to reduce their gambling, or their problem form of gambling. In this case, there is conflict between the individual and researcher/clinician regarding what is considered recovery. Only two studies assessed client treatment goals as outcome measures 34, 82
Although the selected studies demonstrated multi‐dimensional treatment measures, there was large variability in the range of outcomes used and inconsistency in specific measurement methods. This issue has been reported previously in the SUD literature 8, 10, as well as intervention trials for gambling disorders 1, 2, and supports the need to introduce a clear and uniform definition of recovery across fields. Sixty‐three different instruments were documented, almost twice the number of reviewed studies. Instruments varied from validated psychometric measures and selective subdomains of measures to ad‐hoc author‐designed items. Units of measurement and time‐frames were also highly inconsistent in assessing gambling frequency and expenditure. Although some studies followed guidelines outlined by Walker et al. 21 (e.g. reporting net loss, frequency in days/month and utilizing diary/time‐line follow‐back methods), most did not. This suggests that many researchers fail to consider expert guidelines when nominating primary outcomes. The median post‐treatment follow‐up period was 6 months, which falls far below recommendations by López Viets & Miller 87 for a minimum 1‐year follow‐up post‐treatment. Monitoring longer‐term outcomes is a core aspect of the recovery framework 12; it allows researchers to determine whether or not the benefits of treatment are sustained over time, particularly with high rates of relapse in gambling disorders 88.
Much of the measurement criteria for recovery in treatment has been adapted and developed from the substance use field. It may be for this reason that only two of the reviewed studies included outcomes relating to financial status and gambling debt 34, 71. A critical feature differentiating recovery in gambling disorder from all other forms of addiction is financial recovery. Financial instability and debt serves as a chronic and severe harm from gambling problems, and is not alleviated upon abstinence or cessation. Future models of recovery must consider the unique impairment financial consequences present in gambling disorders, its distinct risk for relapse (chasing) and the extended length of time it takes to recover from.
This review followed a strict systematic search protocol; however, it is not without limitations. Strict eligibility criteria were applied in selecting relevant treatment studies and therefore represent only a sample of published gambling treatment studies. Consequently, the studies reviewed may not encompass the full array of measurement instruments and treatment success outcomes. A large proportion of screened pharmacological and brief intervention studies were excluded from the final review due to the brevity in follow‐up. The identified recovery domains were derived from the perspective of the researcher. Consequently, other stakeholder views were not accounted for, particularly those of problem gamblers. In‐depth qualitative interviews with treatment‐seeking gamblers may help to shed more light on the different components of recovery.
Conclusions and recommendations
This systematic review provides a rigorous investigation of the methods and practices used to assess treatment outcomes in gambling disorders. The use of outcomes extended beyond gambling symptoms and behaviour to include measures of positive health as manifested by physical, mental and social wellbeing. This suggests a multi‐dimensional conceptualization of recovery that is consistent with the contemporary ‘recovery‐orientated’ health model. The findings, however, revealed substantial diversity of measurement approaches, rendering it difficult to conduct cross‐study comparisons and impeding the refinement of effective treatments for gambling disorders. Researchers of future treatment studies must consider carefully the selection of appropriate outcome variables and measurement strategies in the early developmental stages of their research design. Walker et al.’s 21 paper serves as a useful resource providing minimum reporting standards for treatment efficacy.
Recovery is a complex phenomenon, and defining it in the context of gambling disorders requires further investigation on a conceptual level with input from similar fields, including substance use disorders. The literature would benefit immensely from the development of a single comprehensive multi‐dimensional scale to measure recovery. The availability of such a scale would enable clinicians and researchers to triangulate improvements in various domains of functioning when reporting outcomes for the successful treatment of gambling disorders.
Declaration of interests
None.
Acknowledgements
Funding for this study and support for open access publication was provided by The Gambling Research Exchange Ontario (GREO) (www.greo.ca).
Pickering, D. , Keen, B. , Entwistle, G. , and Blaszczynski, A. (2018) Measuring treatment outcomes in gambling disorders: a systematic review. Addiction, 113: 411–426. doi: 10.1111/add.13968.
References
- 1. Petry N. M. Pathological Gambling: Etiology, Comorbidity, and Treatment. Washington, DC: American Psychological Association; 2005. [Google Scholar]
- 2. Smith G. J., Hodgins D., Williams R. Research and Measurement Issues in Gambling Studies, 1st edn. Amsterdam/Boston: Emerald Group Publishing Limited; 2007. [Google Scholar]
- 3. Stinchfield R., Winters K. C. Outcome of Minnesota's gambling treatment programs. J Gambl Stud 2001; 17: 217–245. [DOI] [PubMed] [Google Scholar]
- 4. Nower L., Blaszczynski A. Recovery in pathological gambling: an imprecise concept. Subst Use Misuse 2008; 43: 1844–1864. [DOI] [PubMed] [Google Scholar]
- 5. Higgins J. P. T., Thompson S. G., Deeks J. J., Altman D. G. Measuring inconsistency in meta‐analyses. BMJ 2003; 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Greco T., Zangrillo A., Biondi‐Zoccai G., Landoni G. Meta‐analysis: pitfalls and hints. Heart Lung Vessel 2013; 5: 219–225. [PMC free article] [PubMed] [Google Scholar]
- 7. Bangdiwala S. I., Bhargava A., O'Connor D. P., Robinson T. N., Michie S., Murray D. M. et al Statistical methodologies to pool across multiple intervention studies. Transl Behav Med 2016; 6: 228–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. White W., Godley M. Addiction treatment outcomes: who and what can you believe? Counselor 2005; 6: 52–55. [Google Scholar]
- 9. Tiffany S. T., Friedman L., Greenfield S. F., Hasin D. S., Jackson R. Beyond drug use: a systematic consideration of other outcomes in evaluations of treatments for substance use disorders. Addiction 2012; 107: 709–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Donovan D. M., Bigelow G. E., Brigham G. S., Carroll K. M., Cohen A. J., Gardin J. G. et al Primary outcome indices in illicit drug dependence treatment research: systematic approach to selection and measurement of drug use end‐points in clinical trials. Addiction 2012; 107: 694–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Clarke S., Oades L. G., Crowe T. P. Recovery in mental health: a movement towards well‐being and meaning in contrast to an avoidance of symptoms. Psychiatr Rehabil J 2012; 35: 297. [DOI] [PubMed] [Google Scholar]
- 12. DuPont R. L. Creating a New Standard For Addiction Treatment Outcomes: a Report from the Institute for Behavior and Health, Inc. Rockville, MD: Institute for Behavior and Health, Inc.; 2014. [Google Scholar]
- 13. El‐Guebaly N. The meanings of recovery from addiction: evolution and promises. J Addict Med 2012; 6: 1–9. [DOI] [PubMed] [Google Scholar]
- 14. Laudet A. B. What does recovery mean to you? Lessons from the recovery experience for research and practice. J Subst Abuse Treat 2007; 33: 243–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Laudet A. B., Humphreys K. Promoting recovery in an evolving policy context: what do we know and what do we need to know about recovery support services? J Subst Abuse Treat 2013; 45: 126–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McLellan A. T., Chalk M., Bartlett J. Outcomes, performance, and quality—what's the difference? J Subst Abuse Treat 2007; 32: 331–340. [DOI] [PubMed] [Google Scholar]
- 17. Laudet A. B. Environmental scan of measures of recovery. Washington, DC: US Department of Health and Human Services; 2009. [Google Scholar]
- 18. Neale J., Vitoratou S., Finch E., Lennon P., Mitcheson L., Panebianco D. et al Development and validation of ‘sure’: a patient reported outcome measure (PROM) for recovery from drug and alcohol dependence. Drug Alcohol Depend 2016; 165: 159–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Neale J., Tompkins C., Wheeler C., Finch E., Marsden J., Mitcheson L. et al ‘You're all going to hate the word “recovery” by the end of this’: service users’ views of measuring addiction recovery. Drugs Educ Prev Policy 2015; 22: 26–34. [Google Scholar]
- 20. Neale J., Panebianco D., Finch E., Marsden J., Mitcheson L., Rose D. et al Emerging consensus on measuring addiction recovery: findings from a multi‐stakeholder consultation exercise. Drugs Educ Prev Policy 2016; 23: 31–40. [Google Scholar]
- 21. Walker M. B., Toneatto T., Potenza M. N., Petry N., Ladouceur R., Hodgins D. C. et al A framework for reporting outcomes in problem gambling treatment research: the Banff, Alberta consensus. Addiction 2006; 101: 504–511. [DOI] [PubMed] [Google Scholar]
- 22. Kerr W. C., Stockwell T. Understanding standard drinks and drinking guidelines. Drug Alcohol Rev 2012; 31: 200–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Blaszczynski A., Dumlao V., Lange M. ‘How much do you spend gambling?’: ambiguities in survey questionnaire items. J Gambl Stud 1997; 13: 237–252. [DOI] [PubMed] [Google Scholar]
- 24. Blaszczynski A., Ladouceur R., Goulet A., Savard C. ‘How much do you spend gambling?’: ambiguities in questionnaire items assessing expenditure. Int Gambl Stud 2006; 6: 123–128. [Google Scholar]
- 25. Blaszczynski A., Ladouceur R., Goulet A., Savard C. Differences in monthly versus daily evaluations of money spent on gambling and calculation strategies. J Gambl Issues 2008; 21: 98–105. [Google Scholar]
- 26. Volberg R. A., Gerstein D. R., Christiansen E. M., Baldridge J. Assessing self‐reported expenditures on gambling. Manag Decis Econ 2001; 22: 77–96. [Google Scholar]
- 27. Wood R. T., Williams R. J. How much money do you spend on gambling?’ The comparative validity of question wordings used to assess gambling expenditure. Int J Soc Res Methodol 2007; 10: 63–77. [Google Scholar]
- 28. Hodgins D. C., el‐Guebaly N. Natural and treatment‐assisted recovery from gambling problems: a comparison of resolved and active gamblers. Addiction 2000; 95: 777–789. [DOI] [PubMed] [Google Scholar]
- 29. Slutske W. S. Natural recovery and treatment‐seeking in pathological gambling: results of two U.S. national surveys. Am J Psychiatry 2006; 163: 297–302. [DOI] [PubMed] [Google Scholar]
- 30. Blaszczynski A., Ladouceur R., Shaffer H. J. A science‐based framework for responsible gambling: the Reno model. J Gambl Stud 2004; 20: 301–317. [DOI] [PubMed] [Google Scholar]
- 31. National Health and Medical Research Council (NHMRC) Australian Guidelines to Reduce Health Risks From Drinking Alcohol. Canberra, Australia: Commonwealth of Australia; 2009. [Google Scholar]
- 32. Dowling N. A., Smith D., Thomas T. A comparison of individual and group cognitive‐behavioural treatment for female pathological gambling. Behav Res Ther 2007; 45: 2192–2202. [DOI] [PubMed] [Google Scholar]
- 33. Hodgins D. C., Leigh G., Milne R., Gerrish R. Drinking goal selection in behavioral self‐management treatment of chronic alcoholics. Addict Behav 1997; 22: 247–255. [DOI] [PubMed] [Google Scholar]
- 34. Ladouceur R., Lachance S., Fournier P.‐M. Is control a viable goal in the treatment of pathological gambling? Behav Res Ther 2009; 47: 189–197. [DOI] [PubMed] [Google Scholar]
- 35. Stea J. N., Hodgins D. C., Fung T. Abstinence versus moderation goals in brief motivational treatment for pathological gambling. J Gambl Stud 2014; 31: 1029–1045. [DOI] [PubMed] [Google Scholar]
- 36. Blaszczynski A. Conceptual and methodological issues in treatment outcome research. J Gambl Stud 2005; 21: 5–11. [DOI] [PubMed] [Google Scholar]
- 37. Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gøtzsche P. C., Ioannidis J. P. A. et al The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Med 2009; 6: e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cowlishaw S., Merkouris S., Dowling N., Anderson C., Jackson A., Thomas S. Psychological therapies for pathological and problem gambling. Cochrane Database Syst Rev 2012; Art. No.: CD008937. https://doi.org/10.1002/14651858.CD008937.pub2. [DOI] [PubMed] [Google Scholar]
- 39. Grant J. E., Odlaug B. L., Schreiber L. R. N. Pharmacological treatments in pathological gambling. Br J Clin Pharmacol 2014; 77: 375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Marchica L., Derevensky J. L. Examining personalized feedback interventions for gambling disorders: a systematic review. J Behav Addict 2016; 5: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Merkouris S. S., Thomas S. A., Browning C. J., Dowling N. A. Predictors of outcomes of psychological treatments for disordered gambling: a systematic review. Clin Psychol Rev 2016; 48: 7–31. [DOI] [PubMed] [Google Scholar]
- 42. Raylu N., Loo J., Oei T. P. S. Treatment of gambling problems in Asia: comprehensive review and implications for Asian problem gamblers. J Cogn Psychother 2013; 27: 297. [DOI] [PubMed] [Google Scholar]
- 43. Yakovenko I., Hodgins D. C. Latest developments in treatment for disordered gambling: review and critical evaluation of outcome studies. Curr Addict Rep 2016; 3: 299–306. [Google Scholar]
- 44. Yakovenko I., Quigley L., Hemmelgarn B. R., Hodgins D. C., Ronksley P. The efficacy of motivational interviewing for disordered gambling: systematic review and meta‐analysis. Addict Behav 2015; 43: 72–82. [DOI] [PubMed] [Google Scholar]
- 45. Williams R. J., Volberg R. A. Impact of survey description, administration format, and exclusionary criteria on population prevalence rates of problem gambling. Int Gambl Stud 2009; 9: 101–117. [Google Scholar]
- 46. Williams R. J., Volberg R. A. Best Practices in the Population Assessment of Problem Gambling. Alberta, Canada: University of Lethbridge; 2010. [Google Scholar]
- 47. Williams R. J., Volberg R. A. The classification accuracy of four problem gambling assessment instruments in population research. Int Gambl Stud 2014; 14: 15–28. [Google Scholar]
- 48. The Joanna Briggs Institute Joanna Briggs Institute Reviewers’ Manual: 2011 edition. South Australia, Australia: The Joanna Briggs Institute; 2011. [Google Scholar]
- 49. National Health and Medical Research Council (NHMRC) Additional levels of evidence and grades for recommendations for developers of guidelines. Canberra ACT, National Health and Medical Research Council; 2009. [Google Scholar]
- 50. Lesieur H. R., Blume S. B. The south oaks gambling screen (SOGS): a new instrument for the identification of pathological gamblers. Am J Psychiatry 1987; 144: 1184–1188. [DOI] [PubMed] [Google Scholar]
- 51. Spitzer R. L., Kroenke K., Williams J. B. W. Diagnostic and statistical Manual of Mental Disorders, 3rd edn. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- 52. Kim S. W., Grant J. E., Potenza M. N., Blanco C., Hollander E. The gambling symptom assessment scale (G‐SAS): a reliability and validity study. Psychiatry Res 2009; 166: 76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Dowling N. A., Smith D., Thomas T. Treatment of female pathological gambling: the efficacy of a cognitive‐behavioural approach. J Gambl Stud 2006; 22: 355–372. [DOI] [PubMed] [Google Scholar]
- 54. American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, 4th edn. Text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 55. Jimenez‐Murcia S., Alvarez‐Moya E. M., Granero R., Aymami M. N., Gomez‐Pena M., Jaurrieta N. et al Cognitive‐behavioral group treatment for pathological gambling: analysis of effectiveness and predictors of therapy outcome. Psychother Res 2007; 17: 544–552. [Google Scholar]
- 56. Sander W., Peters A. Pathological gambling: influence of quality of life and psychological distress on abstinence after cognitive‐behavioral inpatient treatment. J Gambl Stud 2009; 25: 253–262. [DOI] [PubMed] [Google Scholar]
- 57. Aragay N., Jiménez‐Murcia S., Granero R., Fernández‐Aranda F., Ramos‐Grille I., Cardona S. et al Pathological gambling: understanding relapses and dropouts. Compr Psychiatry 2015; 57: 58–64. [DOI] [PubMed] [Google Scholar]
- 58. Muller K. W., Naab L., Wolfling K., Beutel M. E., Dickenhorst U., Koch A. Psychological well‐being as an additional outcome parameter in the treatment of patients with gambling disorder: results from a clinical multicenter follow‐up study. J Happiness Stud 2016. 1–15. [Google Scholar]
- 59. Beck A. T., Steer R. A., Carbin M. G. Psychometric properties of the Beck depression inventory: twenty‐five years of evaluation. Clin Psychol Rev 1988; 8: 77–100. [Google Scholar]
- 60. Beck A. T., Steer R. A., Brown G. K. BDI‐II, Beck Depression Inventory: Manual. San Antonio, TX/Boston: Psychological Corporation/Harcourt Brace; 1996. [Google Scholar]
- 61. Beck A. T., Epstein N., Brown G., Steer R. A. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988; 56: 893–897. [DOI] [PubMed] [Google Scholar]
- 62. Derogatis L. R. SCL‐90‐R: Administration, Scoring of Procedures Manual‐II for the Revised Version and other Instruments of the Psychopathology Rating Scale Series. Towson, MD: Clinical Psychometric Research Inc.; 1992. [Google Scholar]
- 63. Derogatis L. R., Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med 1983; 13: 595–605. [PubMed] [Google Scholar]
- 64. Lovibond S. H., Lovibond P. H. Manual for the Depression Anxiety Stress Scales [kit], 2nd edn. Sydney NSW: Psychology Foundation of Australia; 1995. [Google Scholar]
- 65. Lesieur H. R., Blume S. B. Modifying the addiction severity index for use with pathological gamblers. Am J Addict 1992; 1: 240–247. [Google Scholar]
- 66. McIntosh C. C., Crino R. D., O'Neill K. Treating problem gambling samples with cognitive behavioural therapy and mindfulness‐based interventions: a clinical trial. J Gambl Stud 2016; 32: 1305–25. [DOI] [PubMed] [Google Scholar]
- 67. Mundt J. C., Marks I. M., Shear M. K., Greist J. M. The work and social adjustment scale: a simple measure of impairment in functioning. Br J Psychiatry 2002; 180: 461–464. [DOI] [PubMed] [Google Scholar]
- 68. Rosenberg O., Dinur L. K., Dannon P. N. Four‐year follow‐up study of pharmacological treatment in pathological gamblers. Clin Neuropharmacol 2013; 36: 42–45. [DOI] [PubMed] [Google Scholar]
- 69. Frisch M. B., Cornell J., Villanueva M., Retzlaff P. J. Clinical validation of the quality of life inventory. A measure of life satisfaction for use in treatment planning and outcome assessment. Psychol Assess 1992; 4: 92–101. [Google Scholar]
- 70. Jackson A. C., Francis K. L., Byrne G., Christensen D. R. Leisure substitution and problem gambling: report of a proof of concept group intervention. Int J Ment Health Addict 2013; 11: 64–74. [Google Scholar]
- 71. Odlaug B. L., Stinchfield R., Golberstein E., Grant J. E. The relationship of tobacco use with gambling problem severity and gambling treatment outcome. Psychol Addict Behav 2013; 27: 696–704. [DOI] [PubMed] [Google Scholar]
- 72. Petry N. M., Ammerman Y., Bohl J., Doersch A., Gay H., Kadden R. et al Cognitive‐behavioral therapy for pathological gamblers. J Consult Clin Psychol 2006; 74: 555–567. [DOI] [PubMed] [Google Scholar]
- 73. Rossini‐Dib D., Fuentes D., Tavares H. A naturalistic study of recovering gamblers: what gets better and when they get better. Psychiatry Res 2015; 227: 17–26. [DOI] [PubMed] [Google Scholar]
- 74. Jiménez‐Murcia S., Granero R., Fernández‐Aranda F., Arcelus J., Aymamí M. N., Gómez‐Peña M. et al Predictors of outcome among pathological gamblers receiving cognitive behavioral group therapy. Eur Addict Res 2015; 21: 169–178. [DOI] [PubMed] [Google Scholar]
- 75. Lloret D., Montesinos R., Capafons A. Waking self‐hypnosis efficacy in cognitive‐behavioral treatment for pathological gambling: an effectiveness clinical assay. Int J Clin Exp Hypn 2014; 62: 50–69. [DOI] [PubMed] [Google Scholar]
- 76. Myrseth H., Molde H., Stoylen I. J., Johnsen B. H., Holsten F., Pallesen S. A pilot study of CBT versus escitalopram combined with CBT in the treatment of pathological gamblers. Int Gambl Stud 2011; 11: 121–141. [Google Scholar]
- 77. Pallanti S., DeCaria C. M., Grant J. E., Urpe M., Hollander E. Reliability and validity of the pathological gambling adaptation of the Yale–Brown obsessive‐compulsive scale (PG‐YBOCS). J Gambl Stud 2005; 21: 431–443. [DOI] [PubMed] [Google Scholar]
- 78. Grant J. E., Donahue C. B., Odlaug B. L., Kim S. W. A 6‐month follow‐up of imaginal desensitization plus motivational interviewing in the treatment of pathological gambling. Ann Clin Psychiatry 2011; 23: 3–10. [PMC free article] [PubMed] [Google Scholar]
- 79. Myrseth H., Brunborg G. S., Eidem M., Pallesen S. Description and pre‐post evaluation of a telephone and internet based treatment programme for pathological gambling in Norway: a pilot study. Int Gambl Stud 2013; 13: 205–220. [Google Scholar]
- 80. Tolchard B., Battersby M. W. Cognitive behaviour therapy for problem gamblers: a clinical outcomes evaluation. Behav Change 2013; 30: 12–23. [Google Scholar]
- 81. Saiz‐Ruiz J., Blanco C., Ibanez A., Masramon X., Gomez M. M., Madrigal M. et al Sertraline treatment of pathological gambling: a pilot study. J Clin Psychiatry 2005; 66: 28–33. [DOI] [PubMed] [Google Scholar]
- 82. Hodgins D. C., Currie S. R., el‐Guebaly N., Diskin K. M. Does providing extended relapse prevention bibliotherapy to problem gamblers improve outcome? J Gambl Stud 2007; 23: 41–54. [DOI] [PubMed] [Google Scholar]
- 83. Blaszczynski A., McConaghy N., Frankova A. A comparison of relapsed and non‐relapsed abstinent pathological gamblers following behavioural treatment. Br J Addict 1991; 86: 1485–1489. [DOI] [PubMed] [Google Scholar]
- 84. Australian Health Ministers’ Advisory Council National framework for recovery‐oriented mental health services. Canberra, Australia: Australian Government Department of Health; 2013. [Google Scholar]
- 85. Best D. W., Lubman D. I. The recovery paradigm: a model of hope and change for alcohol and drug addiction. Aust Fam Physician 2012; 41: 593. [PubMed] [Google Scholar]
- 86. Lancaster K. Rethinking recovery. Addiction 2016; 112: 758–759. [DOI] [PubMed] [Google Scholar]
- 87. López Viets V. C., Miller W. R. Treatment approaches for pathological gamblers. Clin Psychol Rev 1997; 17: 689–702. [DOI] [PubMed] [Google Scholar]
- 88. Hodgins D. C., el‐Guebaly N. Retrospective and prospective reports of precipitants to relapse in pathological gambling. J Consult Clin Psychol 2004; 72: 72–80. [DOI] [PubMed] [Google Scholar]
- 89. Zorzela L., Loke Y. K., Ioannidis J. P., Golder S., Santaguida P., Altman D. G. et al PRISMA harms checklist: Improving harms reporting in systematic reviews. BMJ 2016; 352: i157. [DOI] [PubMed] [Google Scholar]
- 90. Carlbring P., Jonsson J., Josephson H., Forsberg L. Motivational interviewing versus cognitive behavioral group therapy in the treatment of problem and pathological gambling: a randomized controlled trial. Cogn Behav Ther 2010; 39: 92–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Carlbring P., Smit F. Randomized trial of internet‐delivered self‐help with telephone support for pathological gamblers. J Consult Clin Psychol 2008; 76: 1090–1094. [DOI] [PubMed] [Google Scholar]
- 92. Grant J. E., Odlaug B. L., Black D. W., Fong T., Davtian M., Chipkin R. et al A single‐blind study of ‘as needed’ ecopipam for gambling disorder. Ann Clin Psychiatry 2014; 26: 179–186. [PubMed] [Google Scholar]
- 93. Korman L., Collins J., Littman‐Sharp N., Skinner W., McMain S., Mercado V. Randomized control trial of an integrated therapy for comorbid anger and gambling. Psychother Res 2008; 18: 454–465. [DOI] [PubMed] [Google Scholar]
- 94. Marceaux J. C., Melville C. L. Twelve‐step facilitated versus mapping‐enhanced cognitive‐behavioral therapy for pathological gambling: a controlled study. J Gambl Stud 2011; 27: 171–190. [DOI] [PubMed] [Google Scholar]
- 95. Smith D., Battersby M. W., Harvey P. W., Pols R. G., Ladouceur R. Cognitive versus exposure therapy for problem gambling: randomised controlled trial. Behav Res Ther 2015; 69: 100–110. [DOI] [PubMed] [Google Scholar]
- 96. Toneatto T., Brands B., Selby P. A randomized, double‐blind, placebo‐controlled trial of naltrexone in the treatment of concurrent alcohol use disorder and pathological gambling. Am J Addict 2009; 18: 219–225. [DOI] [PubMed] [Google Scholar]
- 97. Ramos‐Grille I., Goma‐i‐Freixanet M., Aragay N., Valero S., Valles V. Predicting treatment failure in pathological gambling: the role of personality traits. Addict Behav 2015; 43: 54–59. [DOI] [PubMed] [Google Scholar]
- 98. Carlbring P., Degerman N., Jonsson J., Andersson G. Internet‐based treatment of pathological gambling with a three‐year follow‐up. Cogn Behav Ther 2012; 41: 321–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Guo S., Manning V., Thane K. K. W., Ng A., Abdin E., Wong K. E. Predictors of treatment outcome among Asian pathological gamblers (PGs): clinical, behavioural, demographic, and treatment process factors. J Gambl Stud 2014; 30: 89–103. [DOI] [PubMed] [Google Scholar]
- 100. Morefield K., Walker C., Smith D., Harvey P., Dunn K., Battersby M. An inpatient treatment program for people with gambling problems: synopsis and early outcomes. Int J Ment Health Addict 2013; 12: 367–379. [Google Scholar]
- 101. Smith D., Harvey P., Battersby M., Pols R., Oakes J., Baigent M. Treatment outcomes and predictors of drop out for problem gamblers in South Australia: a cohort study. Aust NZ J Psychiatry 2010; 44: 911–920. [DOI] [PubMed] [Google Scholar]
- 102. Smith D., Harvey P., Humeniuk R., Battersby M., Pols R. Effects of affective and anxiety disorders on outcome in problem gamblers attending routine cognitive–behavioural treatment in South Australia. J Gambl Stud 2015; 31: 1069–1083. [DOI] [PubMed] [Google Scholar]
- 103. Toneatto T., Wang J. J. Community treatment for problem gambling: sex differences in outcome and process. Community Ment Health J 2009; 45: 468–475. [DOI] [PubMed] [Google Scholar]


