Abstract
Objective
Current treatments for long‐term depression – medication and psychotherapy – are effective for some but not all clients. New approaches need to be developed to complement the ones already available. This study was designed to test the feasibility of using an effective post‐traumatic stress disorder treatment for people with long‐term depression.
Design
A single‐case experimental design with replications was undertaken as a feasibility study of eye movement desensitization and reprocessing (EMDR) in treating long‐term depression.
Methods
Thirteen people with recurrent and/or long‐term depression were recruited from primary care mental health services and given standard protocol EMDR for a maximum of 20 sessions. Levels of depression were measured before and after treatment and at follow‐up, clients also rated their mood each day.
Results
Eight people engaged with the treatment; seven of these had clinically significant and statistically reliable improvement on the Hamilton Rating Scale for Depression. Daily mood ratings were highly variable both during baseline and intervention.
Conclusions
EMDR is a feasible treatment for recurrent and/or long‐term depression. Research on treatment efficacy and effectiveness is now required.
Practitioner points
EMDR may be an effective treatment for depression.
EMDR could be considered if first‐line approaches (CBT and counselling) have been tried and failed.
EMDR may be particularly helpful for service users with a history of trauma.
Keywords: eye movement desensitization and reprocessing, long‐term depression, feasibility, single‐case experimental design
Background
Long‐term depression comprises of recurrent major depressive disorder (MDD; two or more episodes) and persistent depressive disorder (a chronic episode of depression that lasts for more than 2 years; APA, 2013). Although some consider recurrent and chronic depression to be different illnesses (Klein & Santiago, 2003), identifying the correct diagnosis in a particular client is hampered by incomplete remission and memory bias. Current recommended treatments for depression include antidepressant medication, cognitive behavioural therapy (CBT), counselling, and interpersonal therapy (NCCMH, 2010). However, despite the efficacy of these interventions (Butler, Chapman, Forman, & Beck, 2006; Olfson, Marcus, Tedeschi, & Wan, 2006), they do have limitations. In long‐term depression, typical response rates to both medication and psychotherapy may be <50% (Torpey & Klein, 2008). Psychotherapy for long‐term depression may be less effective than for acute‐phase depression (Cuijpers et al., 2010).
Eye movement desensitization and reprocessing (EMDR; Shapiro, 1995) is a psychotherapy that was initially developed for the treatment of post‐traumatic stress disorder (PTSD). A Cochrane Collaboration review of treatments for chronic PTSD recommended EMDR, trauma‐focussed CBT (group and individual) and non‐trauma‐focussed CBT (Bisson, Roberts, Andrew, Cooper, & Lewis, 2013). There is interest amongst EMDR clinicians in using EMDR with other diagnoses. The theoretical model behind EMDR, the adaptive information processing model (AIP), suggests that problematic memories of trauma events are the cause of pathology and these are not limited to PTSD (Solomon & Shapiro, 2008). Four randomized controlled trials into EMDR for PTSD have also reported significant improvements in comorbid depression (Arabia, Manca, & Solomon, 2011; Ironson et al., 2002; Lee, Gavriel, Drummond, Richards, & Greenwald, 2002; van der Kolk et al., 2007). However, there is little research into EMDR for clients who have a primary diagnosis of depression without PTSD; this is limited to case studies and clinical reports (Wood & Ricketts, 2013).
Life events describe any stressful occurrence in a person's life, these can be positive such as moving house or getting married, or negative such as getting ill or being assaulted. In the EMDR literature, life events are sometimes referred to as ‘small t traumas’ (as opposed to ‘big T traumas’ which are the life‐threatening events associated with PTSD onset). Depression is often associated with negative life events (Lenze, Cyranowski, Thompson, Anderson, & Frank, 2008), and people with chronic depression tend to report greater levels of early life adversity (Riso & Newman, 2003). Childhood trauma is a direct and strong risk factor for developing depression later in life (Heim, Newport, Mletzko, Miller, & Nemeroff, 2008). There is a strong dose–response relationship between adverse childhood experiences and lifetime depressive illness (Chapman et al., 2004), and it can be considered a determinate for chronicity (Wiersma et al., 2009), earlier onset (Bernet & Stein, 1999), more lifetime episodes (Bernet & Stein, 1999), and treatment resistance (Kaplan & Klinetob, 2000). In theory, if EMDR is designed to treat the effect of being traumatized and depression is associated with a high incidence of trauma, then EMDR should be able to treat depression. Therefore, the aim of this research was to investigate whether EMDR has the potential to be a treatment for long‐term depression without PTSD by testing whether it is (1) feasible to deliver, (2) acceptable to patients, and (3) associated with reductions in symptoms of depression.
Method
As there is little research on EMDR and depression (Wood & Ricketts, 2013), this study followed the Medical Research Council guidelines (Craig et al., 2008) and began with a feasibility study.
Design
A single‐case experimental design (SCED) with replications (Barlow & Hersen, 1984) was used. Before and after, measures were used to see whether change occurred, with the primary outcome being change on the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960). A daily measure of low mood was also completed to investigate whether change in mood was associated with delivery of EMDR. An AB design was used, with baseline periods during which the participant rated their mood on the daily measure before receiving treatment. The baselines were between 9 and 48 days long and were used to predict natural fluctuations in mood. Once treatment started, the daily measure ratings continued and were used to show how and when change occurred, if it occurred at all.
Participants
Thirteen patients were recruited with a primary diagnosis of long‐term depression (defined as at least 2 years in duration or two or more episodes over the lifetime; APA, 2003). Although they did not need to be native English speakers, they did need sufficient English to be able to understand the testing and fully describe their memories. They had all received treatment from the United Kingdom improving access to psychological therapy (IAPT) primary care mental health service. Their therapist then introduced them to the research, and if interested, their details were passed to the researcher. They were screened using the Mini‐international neuropsychiatric interview (MINI; Sheehan et al., 1998).
Inclusion criteria – People aged 18 and over, with long‐term depression, confirmed through structured interview (MINI) to ensure they met the DSM‐IV‐R criteria. Participants must meet the criteria for a current major depressive episode AND have had at least two episodes (i.e., it is recurrent depression) OR the current episode lasted 2 years or more (long‐term MDD or dysthymia were accepted). Participants had to be able to give informed consent. Participants must have tried at least one‐first‐line treatment and not responded.
Exclusion criteria – those under 18, those unable to give informed consent, those with current suicidal intent or behaviour, psychosis, bipolar disorder, PTSD, dementia, brain injury, current drug/alcohol dependence, epilepsy, pregnancy, current opiate analgesic use, ECT in the last 6 months, primary mental health diagnosis was not long‐term depression.
Measures
The primary outcome measure for the study was the HRSD (Hamilton, 1960). This was collected at entry to the study and after the intervention and at 3‐month follow‐up by the first author who was trained to use all measures. Also collected at the start, end, and follow‐up were the Impact of Event Scale – revised (IES‐r; Creamer, Bell, & Failla, 2003), the Patient Health Questionnaire – 9 items (PHQ‐9; Kroenke, Spitzer, & Williams, 2001) and the Beck Depression Inventory (v.2) (BDI‐II; Beck, Steer, & Brown, 1996). At the start of every session, the clients completed the PHQ‐9.
Hamilton Rating Scale for Depression
The HRSD is a 24‐item clinician‐rated scale for depression symptoms. It has been shown to have good reliability between raters (Hamilton, 1960) and is sensitive to change over time and treatment (Miller, Bishop, Norman, & Maddever, 1985). This is the primary outcome for the indicators of symptoms change. Scores range from 0 to 75 and 8 or less = no symptoms, 9 to 18 = mild, 19 to 26 = moderate, 27 to 34 = severe, 35+ (max score 75) = very severe.
Hamilton Rating Scale for Depression was the primary outcome measure as this is a validated and recognized scale worldwide. It has been the gold standard in depression rating scales for 40 years (Bagby, Ryder, Schuller, & Marshall, 2004). It enables the research to be compared to other research. The HRSD is heavily biological in its design whereas the BDI is more responsive to the cognitive aspects of depression. It is advisable to have more than one scale covering differing perspectives and symptom domains (Roth & Fonagy, 2005). The HRSD and the BDI‐II are considered two of the best tested and reliable rating scales available for depression (Cusin, Yang, Yeung, & Fava, 2009) but are not commonly used in clinical practice in the United Kingdom. The BDI‐II is regularly used in American studies but less so in the United Kingdom. The PHQ‐9 is a standard measure used in IAPT in the United Kingdom so allows the results to be comparable to the IAPT data set should that be appropriate.
The Patient Health Questionnaire – 9 items
The PHQ‐9 (Kroenke & Spitzer, 2002) is a self‐rated depression measure routinely used in IAPT services that takes about two minutes to complete, and it is validated in a UK population (Gilbody, Richards, & Barkham, 2007). The IAPT handbook recommends the following interpretation of PHQ‐9 scores, 1–4 minimal depression, 5–9 mild depression, 10–14 moderate depression, 15–19 moderately severe depression, and 20–27 severe depression (Department of Health, 2011).
Beck Depression Inventory (v.2)
The BDI‐II is a 21‐item self‐report rating scale for depression (Beck et al., 1996), it covers all nine of the DSM diagnostic criteria rather than the six of the BDI, and it includes increases as well as decreases in somatic symptoms (Dozois, Dobson, & Ahnberg, 1998). It is used in many research studies into depression and is the primary depression tool in the United States (Sharp & Lipsky, 2002). It has good validity when compared with other self‐rate scales and clinician‐rated measures for depression (Steer, Ball, Raneeri, & Beck, 1997). The interpretation of the score should 1–10 no depression, 11–16 mild mood disturbance, 17–20 borderline clinical depression, 21–30 moderate depression, 31–40 severe depression, and over 40 extreme depression (Beck et al., 1996).
Impact of Event Scale – revised
The IES‐r is a self‐report scale measuring traumatic stress; it was developed to improve the IES scale, which did not include persistent hyper‐arousal (Creamer et al., 2003). It is a useful instrument for measuring traumatic stress, and a score of 33 or more gives optimal diagnostic accuracy for PTSD (Creamer et al., 2003).
To assess whether participants had made clinically significant and statistically significant changes, the reliable change index (RCI) was used. Reliable change is a way of determining whether the change you see is likely to be real or simply an artefact due to the unreliability of the instrument (Jacobson & Truax, 1991). A RCI can be determined for each measure. If the client's score on the measure changes between the initial and end of therapy reading by more than the RCI, then we can be confident that in 95% of cases this change will be real and not due to error in the measure (i.e., it is statistically reliable). The RCI was calculated for all of the scales. Due to the small sample size in this study, previously published means, standard deviations, and internal consistency scores derived from larger samples were used to calculate the RCIs as they may be considered more reliable.
Although it is important to know that change is reliable, it must be meaningful to the clinicians as well and therefore needs to be related to caseness and severity of illness. The RCI tells us whether the change is statistically reliable, and it does not necessarily tell us whether it is clinically meaningful (Barkham & Mellor‐Clark, 2003). Many articles reporting a clinical measure will assign a cut‐off level (Table 1) to determine what levels of symptoms are clinically significant enough to be considered a ‘case’. Sometimes they also suggest levels of change that can be considered clinically significant or an adequate response to treatment. This acknowledges that although a client's symptoms may not disappear entirely this does not mean that a treatment has not made a major improvement to their life.
Table 1.
Reliable change and clinically significant response
| Measure | Caseness cut‐off | Clinically significant response | Reliable change |
|---|---|---|---|
| Hamilton Rating Scale for Depression (Hamilton, 1960; Schramm et al., 2011) | <8 is non‐clinical | At least 50% reduction in score and score is now <15 | 5.95 |
| Patient Health Questionnaire – 9 items (Kroenke et al., 2001; Smarr and Keefer, 2011) | <10 is non‐clinical | At least a 5‐point reduction | 6.33 |
| BDI‐II = Beck Depression Inventory (v.2) (Smarr and Keefer, 2011) | No official level of caseness but some have suggested at least 16 points is required for diagnosis |
5‐point decrease = minimal improvement 10–19 = moderate 20+ = large |
8.94 |
| Impact of Event Scale – revised (Creamer et al., 2003) | 33 or more indicates PTSD | 17.84 |
The repeated measure
Using this repeated measure, it was possible to track fluctuations in mood in between the sessions; this aims to add insight into the before and after measures and enabled the research to be placed in context of the natural changes in depressive symptoms over time (Turpin, 2001). As has been used in other time series evaluations, the repeated measure was based on the DSM‐IV‐R criteria for the disorder of interest (Kellett, 2007), in this case MDD. The questions were derived from the wording of the PHQ‐9 (Kroenke et al., 2001), and reflected the essential criteria from both the DSM‐IV‐R criteria for MDD (APA, 2003) and the essential criteria for MDD from the ICD‐10 (WHO, 1993; question 3). It was piloted and the wording was borrowed from the PHQ‐9 which has been validated for British adults with depression (Gilbody et al., 2007). The participants were given a paper copy of the scale to complete every day. Three questions addressed low mood/depression, loss of interest or pleasure in activities, and energy levels. The questions were set out in the standard visual analogue form, and the participant had to make a mark on the line representing their mood at that time. The scales had anchored endpoints, for instance ‘I am extremely low or depressed’ to ‘I don't have low mood’ (see Appendix). Completed forms were returned to the therapy session where participants collected the next week's diary. Afterwards, the mark was measured from the right‐hand side to give a decreasing number as the symptoms improved.
At the end of the treatment, all participants were asked the NHS ‘Friends and Family’ question, would you recommend this treatment to friends or family in the same situation?
The intervention
The EMDR adhered to the manualized eight‐phase standard protocol design by Francine Shapiro and approved by the EMDRIA institute (Shapiro, 2001). There are numerous different protocols for EMDR for a range of illnesses, conditions, and situations, but only the original standard protocol has been used in clinical trials. For this reason, the standard protocol was chosen for this study. To ensure the therapists adhered to the standard protocol, they were asked to complete a therapy process record each session. Therapy was twice a week in 60‐min sessions in a National Health Service building that provided psychological therapies. Participants could receive up to 20 sessions, but the final number was a clinical decision. Three therapists provided EMDR; they were all fully qualified to do so and had been trained by EMDRIA institute approved trainers to at least level three.
The eight phases of EMDR are (1) Client history and treatment planning, (2) Preparation, (3) Assessment (of the trauma), (4) Desensitization, (5) Installation, (6) Body Scan, (7) Closure, and (8) Re‐evaluation (Shapiro, 2001). It is phase four where the bilateral stimulation, that is the key (and controversial) component of EMDR, begins. Some early EMDR researchers only counted the number of sessions from the moment bilateral stimulation began. This study counts the number of sessions from the moment of first contact with the therapist. However, there is no set time period for the length of time each of these phases should take. Depending on the client, it may be necessary to spend several sessions planning and preparing, others may get through to phase four or five in one session. This is entirely a clinical decision and is based on the needs of the client.
Analysis
For the before and after standardized measures, reliable change indices (Jacobson & Truax, 1991) and clinically significant change (Barkham & Mellor‐Clark, 2003) were calculated. For the primary measure, the HRSD, clinically significant change can be defined as the participant scoring below eight (for remission) or having a 50% drop in score and now scored under 15 (for response; Hamilton, 1960). MS Excel and SPSS were used for the analysis.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The research was approved by the Research Ethics Committee on behalf of the UK National Research Ethics Services.
Results
Participants
Fifteen people were screened; two were excluded as they had PTSD. Of the 13 who signed consent forms, three did not begin treatment. One was no longer depressed so was instead referred to relapse prevention work, one repeatedly turned down appointments and finally stopped responding to contacts and one could not start EMDR as a therapist could not be found for him. Ten people began treatment, and two dropped out. One dropped out after two sessions reporting family issues and not being able to commit to the treatment. One was referred to the community mental health team. This left eight people who fully engaged with the treatment programme (Figure 1).
Figure 1.
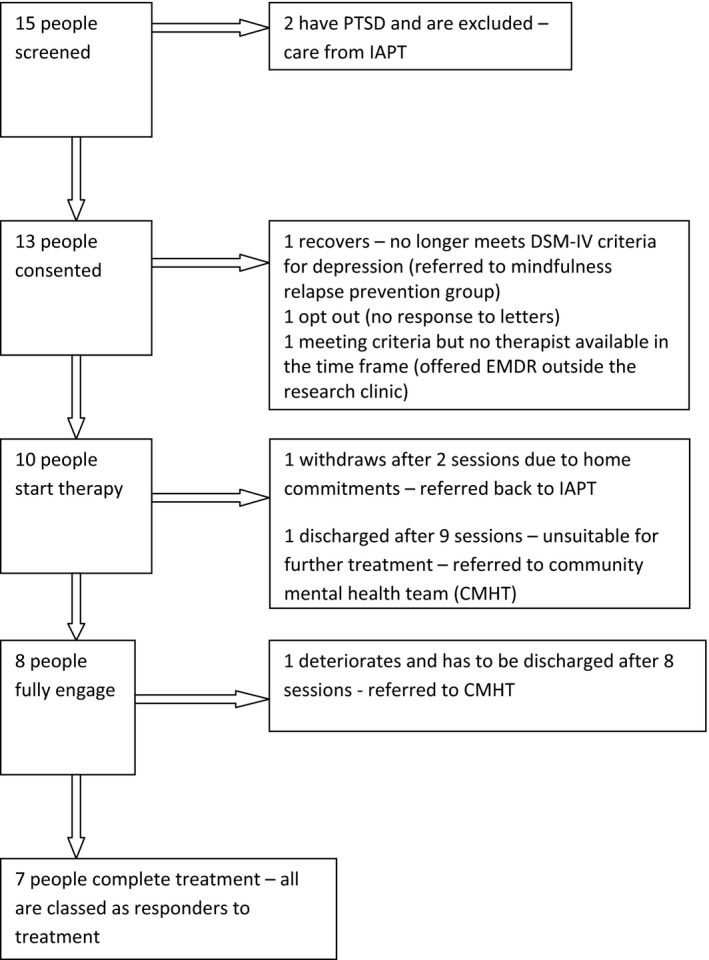
Flow chart of participant recruitment and retention.
The participants ranged in age from 29 to 65 years old with a mean age of 46 (standard deviation 13.1); eight of the 13 were women. The reported first onset of depression ranged from 9 to 43 years, and the self‐reported length of the current episode ranged from 1 month to 10 years. All had received at least one talking therapy and at least one antidepressant medication in the past. The range of talking therapies were CBT, computerized CBT, cognitive analytic therapy, counselling, bereavement counselling, workplace well‐being, psychodynamic therapy, hypnotherapy, and pain‐team psychology. All had MDD confirmed by structured clinical interview, most reported recurrent depression (11/13), just over half had chronic depression (7/13), and some had both (5/13).
Of the 13 participants recruited, three received no treatment sessions. As this is a feasibility study, an intention‐to‐treat analysis was not conducted and their pre‐therapy data were excluded. Only one other participant did not provide after therapy outcome data, participant 008. He did begin therapy but he was discharged after eight sessions, as the therapist deemed him unsuitable for treatment at the present time. After his discharge, he did not respond to our requests to meet for end measures. This was then treated as a dropout. As this is a failure of treatment, his scores are included in the analyses.
Participants who received treatment had between eight and twenty sessions (average 17.6 SD 3.8). Phases 2, 3, and 4 of the standard protocol were the most frequently recorded. Phase two is resourcing where the psychological resources and coping strategies of the participant are assessed and strengthened (present in 9–19 sessions). Phase three is the assessment phase where the target memory is assessed (present in 5–17 sessions). Phase four is desensitization and is when the bilateral stimulation is used to desensitize the client to the traumatic memory (present in 1–16 sessions). All participants preferred tapping to eye movements, so the majority of bilateral stimulation sessions used this method.
Clinical measures
The mean change score on the HRSD was a decrease of 14.1 (SD 4.8). Table 2 shows the detail of the changes for each participant.
Table 2.
The change in Hamilton Rating Scale for Depression (HRSD), if that change was reliable and clinically significant and if any change in symptoms was maintained at follow‐up
| Participant | HRSD Pre | HRSD Post | Change | Reliable?a | Clinically sig?a | HRSD F/U | Are benefits maintained? |
|---|---|---|---|---|---|---|---|
| 1 | 17 | 3 | −14 | Yes | Yes – remission | 4 | Yes |
| 3 | 13 | 5 | −8 | Yes | Yes – remission | 6 | Yes |
| 4 | 25 | 9 | −16 | Yes | Yes – response | 7 | Yes |
| 5 | 26 | 3 | −23 | Yes | Yes – remission | 7 | Yes |
| 6 | 13 | 25 | 12 | Yes | Yes but deteriorated | 5 | Improved |
| 7 | 21 | 5 | −16 | Yes | Yes – remission | 4 | Yes |
| 8 | 22 | – | Dropout | – | |||
| 10 | 23 | 11 | −12 | Yes | Yes – response | – | |
| 11 | 10 | 2 | −8 | Yes | Yes – remission | 5 | Yes |
| 12 | 26 | 8 | −18 | Yes | Yes – response | – | |
| Mean (SD) | 19.6 (5.9) | 7.9 (7.1) | −14.1 (4.8) | 5.4 (1.3) |
A 6‐point change is required for change to be considered reliable on the HRSD, for change to be clinically significant the participants post‐score must be below 8 or have dropped by at least 50% and now be below 15.
Figure 2 is a Jacobson plot (Jacobson & Truax, 1991) of the before and after scores for the HRSD, which shows if any change is reliable, as measured on the RCI, and if it is clinically significant. Any point below the diagonal ‘no change’ line is a participant who improved during the course of therapy. If that point is outside the tramlines (dashed), then the change is statistically reliable, and if it is below the horizontal line, then the participant is now in remission. On the HRSD, change can be clinically significant but not reach the point of remission; that is, the participant has shown a major improvement in his or her symptoms, but they are not yet well enough to be considered in remission; Table 2 shows this in more detail.
Figure 2.
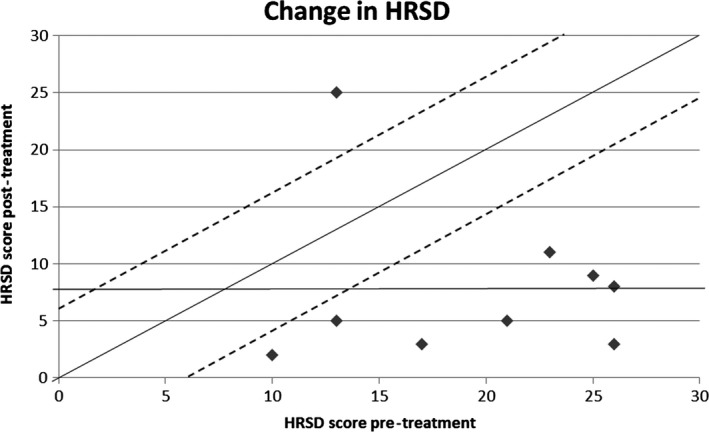
Jacobson plot for the Hamilton Rating Scale for Depression (HRSD).
The table and Jacobson plot show that of the nine people with before and after measures, only one deteriorated and all the others meet the criteria for response. Of these, five are in remission (001, 003, 005, 007, and 011) and three responded to treatment with at least a 50% reduction in HRSD score and are now rated as having mild depression (004, 010, and 012). The person who deteriorated (006) went from mild‐to‐moderate depression with an almost 50% increase in his HRSD score. Two people dropped out and did not receive a full treatment of EMDR but did provide pre‐/post‐data; their scores correspond to the points at coordinates 13, 25 and 23, 11.
The secondary measures also showed clinically significant improvement as Table 3 summarizes. Table 3 also shows how the results seen on the clinician‐rated HRSD are remarkably consistent with the client rated BDI‐II and PHQ‐9. On the three depression measures, HRSD, BDI‐II, and PHQ‐9, there is agreement on almost all cases. Participant 10 did not improve as much on the self‐report scales as she did on the clinician‐rated score and participant 11 did not improve as much on the PHQ‐9 as she did on the other two measures.
Table 3.
Change in BDI‐II, PHQ‐9, and IES, if that change was statistically reliable and clinically significant and if any change was maintained at follow‐up
| Participant | IES‐r pre | IES‐r post | Change | IES‐r F/U | PHQ‐9 pre | PHQ‐9 post | Change | PHQ‐9 F/U | BDI‐II pre | BDI‐II post | Change | BDI‐II F/U |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 13 | 4 | −9 | 8 | 17 | 7 | −10a , b | 4c | 33 | 10 | −23a , b | 6c |
| 3 | 11 | 5 | −6 | 12 | 10 | 3 | −7a , b | 6c | 21 | 2 | −19a , b | 8c |
| 4 | 50 | 13 | −37a , b | 15c | 24 | 11 | −13a , b | 7c | 48 | 29 | −19a , b | 27c |
| 5 | 54 | 12 | −42a , b | 0c | 19 | 4 | −15a , b | 5c | 43 | 9 | −34a , b | 2c |
| 6 | 19 | 68 | 49a , b | 28 | 10 | 25 | 15a , b | 13 | 26 | 5 | −24a , b | 25 |
| 7 | 45 | 20 | −35a , b | 22c | 18 | 6 | −12a , b | 7c | 34 | 17 | −17a , b | 8c |
| 8 | 33 | – | Drop out | – | 17 | – | – | 28 | – | – | ||
| 10 | 25 | 24 | −1 | – | 13 | 14 | 1 | – | 23 | 28 | 5 | – |
| 11 | 15 | 1 | −14 | 20 | 10 | 6 | −4 | 4c | 24 | 0 | −24a , b | 12c |
| 12 | 35 | 13 | −22a , b | – | 17 | 5 | −12a , b | – | 37 | 17 | −20a , b | – |
| Mean (SD) | 30.0 (15.9) | 17.8 (20.2) | −13.0 (27.5) | 11.7 (10.5) | 15.5 (4.6) | 9.0 (6.9) | −6.3 (9.4) | 6.6 (3.1) | 31.7 (9.0) | 13.0 (10.6) | −19.4 (10.4) | 12.6 (9.7) |
IES‐r = Impact of Event Scale – revised; PHQ‐9 = Patient Health Questionnaire – 9 items; BDI‐II = Beck Depression Inventory (v.2).
aChange is statistically reliable, bchange is clinically significant, and cpre‐/post‐improvement in symptoms maintained for improved at 3‐month follow‐up (F/U).
The IES‐r clinically significant changes need to be read with care. The change is only clinically significant if the participant moves across a specified cut‐off point, but not all the participants started on the pathological side of the cut‐off (i.e., they did not have evidence of being traumatized or had normal social functioning). These participants cannot achieve clinically significant change no matter how much they improve. Change in participant 6 was clinically significant and statistically reliable but he deteriorated.
The daily measure
The daily measure showed so much variability across all participants for all three questions that the results are difficult to interpret. However, there was no evidence of spontaneous improvement during the baseline across participants. An example is shown in Figure 3.
Figure 3.
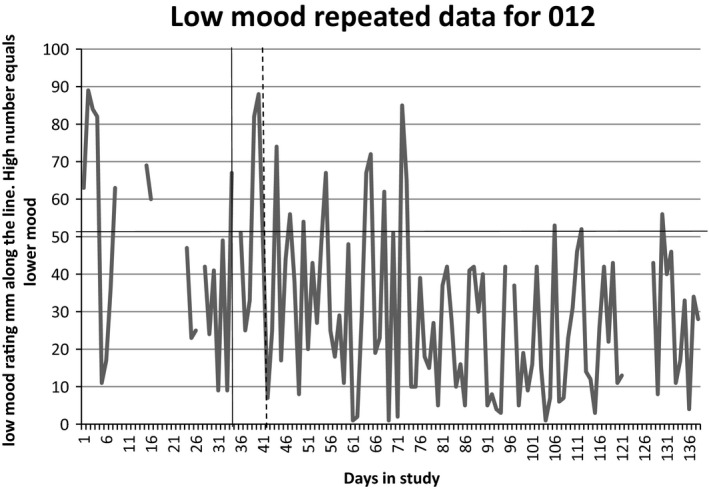
An example of one of the daily measure graph.
Friends and family question
Every participant who responded to the friends and family question reported that, yes, they would recommend EMDR as a treatment for depression to friends and family in the same situation. In fact, two of them did approach the researcher to see if they could get friends into the research clinic. The respondents included the participant whose depression got worse, but he still said he would recommend it and would accept it again himself if offered in the future.
Discussion
Of the nine people who fully engaged with the treatment programme, eight had a clinically significant and statistically reliable positive response. Five people scored as subclinical for depression at the end of treatment. All participants would recommend it to friends and family. This indicates that (1) EMDR can be delivered to this patient group with no observed difficulties in this small sample, (2) the treatment was acceptable, and (3) the treatment was associated with reduction in the symptoms of depression. Although due to the lack of an active control group and the very small sample size here, the magnitude of the effect or its reliability in a larger sample cannot be known.
One person's depression worsened during treatment. When asked about this, the participant did not feel the EMDR had been a cause of the deterioration, and he reported that he would like to try it again in the future. Treatment safety should be taken as seriously in psychotherapy as it is in pharmacology (Parry, Crawford, & Duggan, 2016). Based on Parry et al. (2016) suggested terminology, this participant saw a clinically significant deterioration in his mental state, but with no evidence of harm. The EMDR therapists involved suggested that there needs to be a careful assessment of the psychological resources and coping methods available to the client before starting bilateral stimulation. They found this part of the protocol took longer in the clients within the study than would be expected when working with clients with PTSD.
Many EMDR proponents claim it can be used for far more than just PTSD (Shapiro, 1995, 2005). This clinical case series complements clinical reports of the success of EMDR to treat depression (Bae, Kim, & Park, 2008; Grey, 2011), but the literature still lacks a large randomized controlled trial to provide confirmation of efficacy and effect size (Wood & Ricketts, 2013).
Participants with PTSD, as assessed by the structured clinical interview, were excluded from the study. Despite this, the IES‐r results show that those who were classified as traumatized before the treatment were no longer traumatized at the end and this remained true at follow‐up. Despite screening negative for PTSD, many of the participants (7/13) scored highly for trauma on the IES‐r. This may highlight the difference between PTSD criterion A events (sometimes referred to as ‘big T trauma’ in the EMDR literature) and negative life events (‘small t trauma’). Negative life events may not be life‐threatening, but they can still have a profoundly damaging effect on a person's mental state (Shapero et al., 2014; Shapiro, 2001). The AIP model states that the memory of these events can fail to be fully processed regardless of whether or not the event is life‐ threatening (Solomon & Shapiro, 2008). It also predicts that it is these memories that cause negative thinking styles and that by processing the memory, the negative thinking style can be altered.
This study adds to a small, but growing body of literature that indicates EMDR has potential to treat depression (Bae et al., 2008; Grey, 2011; Hofmann et al., 2014) and symptoms of depression and hypomania in bipolar patients (Novo et al., 2014). It also shows that EMDR does not necessarily need to be an adjunct to another therapy but can be used as the standard protocol describes (Shapiro, 2001). The Hofmann study used EMDR sessions (between 3 and 16) as an adjunct to CBT (around 38 sessions), with the CBT+EMDR group achieving significantly greater improvements in depression symptoms than those receiving CBT alone. By using only standard protocol EMDR, this study appears to have seen results equivalent to the German study but in half the number of sessions (20 instead of 40–50 sessions; Hofmann et al., 2014).
Limitations
This is a feasibility study involving a case series without a control group and therefore does not aim to establish efficacy. As all the participants received EMDR, the evaluators were not blind to treatment. The use of a predictive baseline and continuous measurement sought to partially control for the passage of time. The length of the baseline period was determined by how quickly a therapist became available and was not randomized. This means it is not a true experimental design, but it was considered clinically more appropriate.
Recommendations for research
This small feasibility study has shown that it is feasible to use EMDR to treat long‐term depression. There is therefore a case for further research to investigate its efficacy, compare it to CBT and mechanism of action. Work will also be needed to see whether EMDR needs to be targeted at service users with depression that clearly links to a traumatic past or if it can be used with anyone with depression. As long‐term depression is a relapsing/remitting condition, a significant follow‐up period (preferably at least 12 months) is required to ensure improvements are maintained.
Conclusions
This study reports clinically significant and statistically reliable improvement in eight of nine participants who received a complete treatment of EMDR, with one client withdrawing from therapy. One participant dropped out. As no single talking therapy or treatment has ever proved to be all things to all people, numerous psychotherapies should be researched to provide a wider range of treatment options for these prevalent and disabling disorders. EMDR has the potential to be a treatment for long‐term depression.
Funding
This research was funded by the NIHR Collaboration for Leadership in Applied Health Research and Care for South Yorkshire (NIHR CLAHRC SY), a pilot which ended in 2013. Further details about the new NIHR CLAHRC Yorkshire and Humber can be found at www.clahrc-yh.nihr.ac.uk. The views and opinions expressed are those of the authors, and not necessarily those of the NHS, the NIHR, or the Department of Health.
The funding body (NIHR CLAHRC SY) had no role in the conduct of the research or preparation of the article.
Table A1. An example of 1 day of the repeated questions
| Date | |||
| Low mood/depression | ‘I am extremely low or depressed’ | __________________ | ‘I don't have low mood’ |
| Interest or pleasure in activities | ‘I have no interest in doing things’ | __________________ | ‘I get involved’ |
| Energy levels | ‘I have no energy’ | __________________ | ‘I have enough energy’ |
References
- APA . (2003). Diagnostic and statistical manual of mental disorders. 4th Edition. Text revision. DSM‐IV‐TR. Washington, DC: Author. [Google Scholar]
- APA . (2013). Diagnostic and statistical manual of mental disorders. 5th Edition. DSM 5. Washington, DC: Author. [Google Scholar]
- Arabia, E. , Manca, M. L. , & Solomon, R. M. (2011). EMDR for survivors of life‐threatening cardiac events: Results of a pilot study. Journal of EMDR Practice and Research, 5(1), 2–13. https://doi.org/10.1891/1933-3196.5.1.2 [Google Scholar]
- Bae, H. , Kim, D. , & Park, Y. (2008). Eye movement desensitization and reprocessing for adolescent depression. Psychiatry Investigation, 5(1), 60–65. https://doi.org/10.4306/pi.2008.5.1.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagby, R. M. , Ryder, A. G. , Schuller, D. R. , & Marshall, M. B. (2004). The Hamilton Depression Rating Scale: Has the gold standard become a lead weight? American Journal of Psychiatry, 161, 2163–2177. https://doi.org/10.1176/appi.ajp.161.12.2163 [DOI] [PubMed] [Google Scholar]
- Barkham, M. , & Mellor‐Clark, J. (2003). Bridging evidence‐based practice and practice‐based evidence: Developing a rigorous and relevant knowledge for the psychological therapies. Clinical Psychology & Psychotherapy, 10, 319–327. https://doi.org/10.1002/cpp.379 [Google Scholar]
- Barlow, D. , & Hersen, M. (1984). Single case experimental design. New York, NY: Pergamon Press. [Google Scholar]
- Beck, A. , Steer, R. , & Brown, G. (1996). Manual for the Beck Depression Inventory‐II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bernet, C. Z. , & Stein, M. B. (1999). Relationship of childhood maltreatment to the onset and course of major depression in adulthood. Depression and Anxiety, 9, 169–174. https://doi.org/10.1002/(SICI)1520-6394(1999)9:4<169::AID‐DA4>3.0.CO;2‐2 [PubMed] [Google Scholar]
- Bisson, J. , Roberts, N. , Andrew, M. , Cooper, R. , & Lewis, C. (2013). Psychological therapies for chronic post‐traumatic stress disorder (PTSD) in adults (Review). The Cochrane Library, CD003388. https://doi.org/10.1002/14651858.CD003388.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler, A. C. , Chapman, J. E. , Forman, E. M. , & Beck, A. T. (2006). The empirical status of cognitive‐behavioral therapy: A review of meta‐analyses. Clinical Psychology Review, 26(1), 17–31. https://doi.org/10.1016/j.cpr.2005.07.003 [DOI] [PubMed] [Google Scholar]
- Chapman, D. P. , Whitfield, C. L. , Felitti, V. J. , Dube, S. R. , Edwards, V. J. , & Anda, R. F. (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82, 217–225. https://doi.org/10.1016/j.jad.2003.12.013 [DOI] [PubMed] [Google Scholar]
- Craig, P. , Dieppe, P. , Macintyre, S. , Michie, S. , Nazareth, I. , Petticrew, M. , & Medical Research Council Guidance . (2008). Developing and evaluating complex interventions: the new Medical Research Council guidance. British Medical Journal, 337, a1655. https://doi.org/10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer, M. , Bell, R. , & Failla, S. (2003). Psychometric properties of the Impact of Event Scale—Revised. Behaviour Research and Therapy, 41(12), 1489–1496. https://doi.org/10.1016/j.brat.2003.07.010 [DOI] [PubMed] [Google Scholar]
- Cuijpers, P. , van Straten, A. , Schuurmans, J. , van Oppen, P. , Hollon, S. D. , & Andersson, G. (2010). Psychotherapy for chronic major depression and dysthymia: A meta‐analysis. Clinical Psychology Review, 30(1), 51–62. https://doi.org/10.1016/j.cpr.2009.09.003 [DOI] [PubMed] [Google Scholar]
- Cusin, C. , Yang, H. , Yeung, A. , & Fava, M. (2009). Rating scales for depression In Handbook of clinical rating scales and assessment in psychiatry and mental health (pp. 7–35). Totowa, NJ: Humana Press. [Google Scholar]
- Department of Health (2011). The IAPT data handbook. London, UK: The Stationary Office. [Google Scholar]
- Dozois, D. J. A. , Dobson, K. S. , & Ahnberg, J. L. (1998). A psychometric evaluation of the Beck Depression Inventory‐II. Psychological Assessment, 10(2), 83–89. https://doi.org/10.1037/1040-3590.10.2.83 [Google Scholar]
- Gilbody, S. , Richards, D. , & Barkham, M. (2007). Diagnosing depression in primary care using self‐completed instruments: UK validation of PHQ–9 and CORE–OM. British Journal of General Practice, 57(541), 650–652. [PMC free article] [PubMed] [Google Scholar]
- Grey, E. (2011). A pilot study of concentrated EMDR: A brief report. Journal of EMDR Practice and Research, 5(1), 14–24. https://doi.org/10.1891/1933-3196.5.1.14 [Google Scholar]
- Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heim, C. , Newport, D. J. , Mletzko, T. , Miller, A. H. , & Nemeroff, C. B. (2008). The link between childhood trauma and depression: Insights from HPA axis studies in humans. Psychoneuroendocrinology, 33, 693–710. https://doi.org/10.1016/j.psyneuen.2008.03.008 [DOI] [PubMed] [Google Scholar]
- Hofmann, A. , Hilgers, A. , Lehnung, M. , Liebermann, P. , Ostacoli, L. , Schneider, W. , & Hase, M. (2014). Eye movement desensitization and reprocessing as an adjunctive treatment of unipolar depression: A controlled study. Journal of EMDR Practice and Research, 8, 103–112. https://doi.org/10.1891/1933-3196.8.3.103 [Google Scholar]
- Ironson, G. , Freud, B. , Strauss, J. L. L. , Williams, J. , Freund, B. , Strauss, J. L. L. , … Byrnes, D. (2002). Comparison of two treatments for traumatic stress: A community‐based study of EMDR and prolonged exposure. Journal of Clinical Psychology, 58(1), 113–128. https://doi.org/10.1002/jclp.1132 [DOI] [PubMed] [Google Scholar]
- Jacobson, N. S. , & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. https://doi.org/10.1037/0022-006X.59.1.12 [DOI] [PubMed] [Google Scholar]
- Kaplan, M. J. , & Klinetob, N. A. (2000). Childhood emotional trauma and chronic posttraumatic stress disorder in adult outpatients with treatment‐resistant depression. Journal of Nervous & Mental Disease, 188, 596–601. [DOI] [PubMed] [Google Scholar]
- Kellett, S. (2007). A time series evaluation of the treatment of histrionic personality disorder with cognitive analytic therapy. Psychology and Psychotherapy: Theory, Research and Practice, 80, 389–405. https://doi.org/10.1348/147608306X161421 [DOI] [PubMed] [Google Scholar]
- Klein, D. N. , & Santiago, N. J. (2003). Dysthymia and chronic depression: Introduction, classification, risk factors, and course. Journal of Clinical Psychology, 59, 807–816. https://doi.org/10.1002/jclp.10174 [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , & Spitzer, R. L. (2002). The PHQ‐9: A new depression diagnostic and severity measure. Psychiatric Annals, 32, 509–515. https://doi.org/10.3928/0048-5713-20020901-06 [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. W. (2001). The PHQ‐9. Journal of General Internal Medicine, 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, C. , Gavriel, H. , Drummond, P. , Richards, J. , & Greenwald, R. (2002). Treatment of PTSD: Stress inoculation training with prolonged exposure compared to EMDR. Journal of Clinical Psychology, 58, 1071–1089. https://doi.org/10.1002/jclp.10039 [DOI] [PubMed] [Google Scholar]
- Lenze, S. N. , Cyranowski, J. M. , Thompson, W. K. , Anderson, B. , & Frank, E. (2008). The cumulative impact of nonsevere life events predicts depression recurrence during maintenance treatment with interpersonal psychotherapy. Journal of Consulting and Clinical Psychology, 76, 979–987. https://doi.org/10.1037/a0012862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, I. W. , Bishop, S. , Norman, W. H. , & Maddever, H. (1985). The modified Hamilton rating scale for depression: Reliability and validity. Psychiatry Research, 14, 131–142. https://doi.org/10.1016/0165-1781(85)90057-5 [DOI] [PubMed] [Google Scholar]
- NCCMH . (2010). Depression: The NICE guidance on the treatment and management of depression in adults. Updated Edition. National Clinical Practice Guideline 90. London, UK: British Psychological Society and The Royal College of Psychiatrists. [Google Scholar]
- Novo, P. , Landin‐Romero, R. , Radua, J. , Vicens, V. , Fernandez, I. , Garcia, F. , … Amann, B. L. (2014). Eye movement desensitization and reprocessing therapy in subsyndromal bipolar patients with a history of traumatic events: A randomized, controlled pilot‐study. Psychiatry Research, 219(1), 122–128. https://doi.org/10.1016/j.psychres.2014.05.012 [DOI] [PubMed] [Google Scholar]
- Olfson, M. , Marcus, S. C. , Tedeschi, M. , & Wan, G. J. (2006). Continuity of antidepressant treatment for adults with depression in the United States. American Journal of Psychiatry, 163(1), 101–108. https://doi.org/10.1176/appi.ajp.163.1.101 [DOI] [PubMed] [Google Scholar]
- Parry, G. D. , Crawford, M. J. , & Duggan, C. (2016). Iatrogenic harm from psychological therapies – time to move on. The British Journal of Psychiatry, 208(3), 210–212. https://doi.org/10.1192/bjp.bp.115.163618 [DOI] [PubMed] [Google Scholar]
- Riso, L. P. , & Newman, C. F. (2003). Cognitive therapy for chronic depression. Journal of Clinical Psychology, 59, 817–831. https://doi.org/10.1002/jclp.10175 [DOI] [PubMed] [Google Scholar]
- Roth, A. , & Fonagy, P. (2005). What works for whom? A critical review of psychotherapy research (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Schramm, E. , Hautzinger, M. , Zobel, I. , Kriston, L. , Berger, M. , & Härter, M. (2011). Comparative efficacy of the Cognitive Behavioral Analysis System of Psychotherapy versus Supportive Psychotherapy for early onset chronic depression: Design and rationale of a multisite randomized controlled trial. BMC Psychiatry, 11, 134 https://doi.org/10.1186/1471-244X-11-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapero, B. G. , Black, S. K. , Liu, R. T. , Klugman, J. , Bender, R. E. , Abramson, L. Y. , & Alloy, L. B. (2014). Stressful life events and depression symptoms: The effect of childhood emotional abuse on stress reactivity. Journal of Clinical Psychology, 70, 209–223. https://doi.org/10.1002/jclp.22011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro, F. (1995). Eye movement desensitization and reprocessing (EMDR): Basic principles, protocols and procedures. New York, NY: Guilford. [Google Scholar]
- Shapiro, F. (2001). Eye movement desensitization and reprocessing: Basic principles, protocols, and procedures (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Shapiro, R. (2005). EMDR solutions: Pathways to healing. New York, NY: W W Norton & Co. [Google Scholar]
- Sharp, L. K. , & Lipsky, M. S. (2002). Screening for depression across the lifespan: A review of measures for use in primary care settings. American Family Physician, 66, 1001–1008. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12358212 [PubMed] [Google Scholar]
- Sheehan, D. V. , Lecrubier, Y. , Sheehan, K. H. , Amorim, P. , Janavs, J. , Weiller, E. , … Dunbar, G. C. (1998). The Mini‐International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM‐IV and ICD‐10. The Journal of Clinical Psychiatry, 59(Suppl 20), 22–33. [PubMed] [Google Scholar]
- Smarr, K. L. , & Keefer, A. L. (2011). Measures of depression and depressive symptoms: Beck Depression Inventory‐II (BDI‐II), Center for Epidemiologic Studies Depression Scale (CES‐D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire ‐9 (PHQ‐9). Arthritis Care and Research, 63(511), 5454–5466. https://doi.org/10.1002/acr.20556 [DOI] [PubMed] [Google Scholar]
- Solomon, R. M. , & Shapiro, F. (2008). EMDR and the adaptive information processing model. Potential mechanisms of change. Journal of EMDR Practice and Research, 2(4), 315–325. https://doi.org/10.1891/1933-3196.2.4.315 [Google Scholar]
- Steer, R. A. , Ball, R. , Raneeri, W. F. , & Beck, A. T. (1997). Further evidence for the construct validity of the Beck Depression Inventory – II with psychiatric outpatients. Psychological Reports, 80, 443–446. https://doi.org/10.2466/pr0.1997.80.2.443 [DOI] [PubMed] [Google Scholar]
- Torpey, D. C. , & Klein, D. N. (2008). Chronic depression: Update on classification and treatment. Current Psychiatry Reports, 10, 458–464. https://doi.org/10.1007/s11920-008-0074-6 [DOI] [PubMed] [Google Scholar]
- Turpin, G. (2001). Single case methodology and psychotherapy evaluation In Mace C., Moorey S. & Roberts B. (Eds.), Evidence in the psychological therapies: A critical guide for practitioners (pp. 91–113). Hove, UK: Brunner‐Routledge. [Google Scholar]
- van der Kolk, B. A. , Spinazzola, J. , Blaustein, M. E. , Hopper, J. W. , Hopper, E. K. , Korn, D. L. , … Simpson, W. B. (2007). A randomized clinical trial of eye movement desensitization and reprocessing (EMDR), fluoxetine, and pill placebo in the treatment of posttraumatic stress disorder: Treatment effects and long‐term maintenance. The Journal of Clinical Psychiatry, 68(1), 37–46. [DOI] [PubMed] [Google Scholar]
- WHO . (1993). The ICD‐10 classification of mental and behavioural disorders. Clinical descriptions and diagnostic guidelines. Geneva, Switzerland: Author. [Google Scholar]
- Wiersma, J. , Hovens, J. , van Oppen, P. , Giltay, E. , van Schaik, D. , Beekman, A. , & Penninx, B. (2009). The importance of childhood trauma and childhood life events for chronicity of depression in adults. Journal of Clinical Psychiatry, 70, 983–989. Retrieved from http://www.nesda.nl/nesda/wp-content/uploads/2015/06/Wiersma_JClinPsych_2009.pdf [DOI] [PubMed] [Google Scholar]
- Wood, E. , & Ricketts, T. (2013). Is EMDR an evidenced‐based treatment for depression? A review of the literature. Journal of EMDR Practice and Research, 7, 225–235. https://doi.org/10.1891/1933-3196.7.4.225 [Google Scholar]


