Abstract
Objective
Gout patient self-management knowledge and adherence to treatment regimens are poor. Our objective was to assess the feasibility and acceptability of a multidisciplinary team-based pilot program for the education and monitoring of gout patients.
Methods
Subjects completed a Gout Self-Management Knowledge Exam, along with gout flare history and compliance questionnaires, at enrollment and at 6 and 12 months. Each exam was followed by a nursing educational intervention via a structured gout curriculum. Structured monthly follow-up calls from pharmacists emphasized adherence to management programs. Primary outcomes were subject and provider program evaluation questionnaires at 6 and 12 months, program retention rate and success in reaching patients via monthly calls.
Results
40/45 subjects remained in the study at 12 months. At 12 months, on a scale of 1 (most) to 5 (least), ratings of 3 or better were given by 84.6% of subjects evaluating the usefulness of the overall program in understanding and managing their gout, 81.0% of subjects evaluating the helpfulness of the nursing education program and 50.0% of subjects evaluating the helpfulness of the calls from the pharmacists. Knowledge Exam questions that were most frequently answered incorrectly on repeat testing concerned bridge therapy, the possibility of being flare-free, and the genetic component of gout.
Conclusion
Our multidisciplinary program of gout patient education and monitoring demonstrates feasibility and acceptability. We identified variability in patient preference for components of the program and persistent patient knowledge gaps.
KEY INDEXING TERMS: gout, patient education, self-management, self-care, gouty arthritis
INTRODUCTION
Gout is poorly managed internationally (1–7). Gout is common (8), is increasing in frequency (3), impacts patients’ quality of life, and causes significant lost time from work (9–10). Adherence to medications is worse in gout than in many other diseases (12). A recent study found that only 14% of gout patients knew their serum urate (SUA) goal (13). Forty-nine percent of U.S. patients taking urate-lowering therapy (ULT) have serum urate ≥ 6.0 (14). Adequate teaching resources are currently unavailable for patients with gout (16). Studies document provider knowledge gaps about gout management (2–5, 16), and inadequate gout patient self-management knowledge (2,3,5,7,17,18). Online resources and mobile applications are not presently sufficient to provide all the education and monitoring needed by gout patients (19–20).
Maintaining patients at their SUA goal is effective in preventing attacks, shrinking tophi and preventing joint damage (14,21). Careful up-titration of ULT successfully achieves this goal (3,12,22,23). Although guidelines and editorials recommend ULT for the great majority of patients with gout, along with anti-inflammatory prophylaxis during the early stage of ULT, these recommendations are often not followed (5,14,21,24,25). Gout is largely managed in the U.S. by primary care providers (26).
Successful pharmacist management in many conditions is well-documented (27). The Nurse Educator role is also strongly supported. A study of perceptions of rheumatic disease patients, given drug information by a rheumatology nurse, found that the patients achieved a sense of “autonomy, power and security (28).” Nursing-led (29) and pharmacy-led (30) gout management programs have been successful in getting patients to their SUA goal. We hypothesized that combining the skills of a multi-disciplinary team that included rheumatology providers (physicians and nurse practitioner), trained RN gout educators, pharmacists and a social worker would create an effective program that allowed division of labor and permitted each team member to practice at the “top of their license.”
It is important for gout patients to understand management principles, since the needed plan is complex, long-term and difficult to sustain. The plan includes diet, exercise, lifetime medication adherence and early treatment of flares. Patients need to know the difference between medications for flares, urate-lowering, and bridge therapy. Gout has multiple co-morbidities (4); patients, asked to add new medications to an already-complex regimen, need to understand the rationale.
Educational principles stress the value of reinforcement of educational interventions over time (31,32). Accordingly, we designed our program to include nurse educator intervention at 6 month intervals and monthly pharmacist calls. In this study, we aimed to demonstrate the feasibility and acceptability of such a program.
PATIENTS AND METHODS
Study design and procedures
The study has been approved by Hospital for Special Surgery’s IRB (#14073). We conducted a single-arm one year pilot study of a multi-disciplinary team gout education and management program consisting of (a) a Gout Patient Self-Management Knowledge Exam (see “Gout Self-Management Examination “ - Supplementary Appendix A) at enrollment, 6 and 12 months, (b) a nurse-taught curriculum (See “Gout Curriculum” - Supplementary Appendix B) after the initial knowledge exam and at 6 and 12 months, and (c) monthly phone calls from pharmacists (Figure 1). Subjects completed questionnaires regarding their gout flares in the prior 6 months and a compliance questionnaire at enrollment and at 6 and 12 months. Program evaluation questionnaires were completed at 6 and 12 months by subjects and providers. Laboratory testing was at provider discretion and urate results were obtained via chart review. Gout care was determined by the provider on an individual basis. Pharmacist calls were scripted to obtain data on adherence to gout management plan, including medications, planned provider visits and laboratory testing.
Figure 1. Education and Monitoring Schedule.
Timing of data gathering, educational interventions and pharmacist monitoring calls
Patients
Eligible patients were seen at their first visit to our institution for gout, met the 1977 ARA Criteria for Diagnosing Gout (33), were ≥ age 18, and were English-speaking. Exclusions included pregnancy and non-use of birth control methods in females of child-bearing potential. Recruitment was via exam room posters, rheumatology staff emails and staff meeting announcements.
Data collection
Study data were collected and managed using REDCap electronic data capture tools hosted at Hospital for Special Surgery (34).
Gout Patient Educational Curriculum
A rheumatologist (TF), RN (KK) and social worker (AB) developed the curriculum, based on American College of Rheumatology gout management guidelines (25,26), and designed for easy comprehension and for use as future reference by subjects. The curriculum included discussion of medications, diet, lifestyle, lab testing and setting goals. (See Appendix B).
Primary Outcome Measures
Retention rate
Retention rates for the program at 6 and 12 months were defined by patients who completed, at a minimum, the Gout Self-Management Exam or the Program Evaluation Questionnaire.
Program Evaluation
Six- and 12- month questionnaires to subjects and providers entering at least 1 patient included Likert scale and open-ended questions.
Evaluation of Nurse Education Program by subjects and providers
Subjects were asked the following question: “Was the education session with the nurse helpful in your understanding and management of your gout?” rated 1 (very helpful) to 5 (not at all). Providers were asked “If manpower were available, how likely would you be to employ the Educational Sessions by Nurse in your own practice in the future for your gout patients?” rated 1 (very likely) to 5 (very unlikely).
Evaluation of Pharmacist Monitoring Program by subjects and providers
Subjects were asked: “Were the calls from the Pharmacist helpful in your management of your gout?” rated 1 (very much) to 5 (not at all). “Did you find the number of phone calls about the right number, too many or too few?” rated 1 (too few) to 5 (too many), with comments. Providers were asked “If manpower were available, how likely would you be to employ monthly phone calls from pharmacist in your own practice in the future for your gout patients?” rated 1 (very likely) to 5 (very unlikely).
Evaluation of overall Program by subjects and providers
Subjects were asked a series of questions: “Rate the usefulness of this program in helping you to understand gout and to be able to deal with the condition” rated 1 (extremely) to 5 (not at all), with comments; “Did this program improve your ability to ask questions about your gout when you saw your doctor or nurse practitioner?” (yes/no); and “Would you recommend this program of gout education and monitoring be further studied and considered for other people with gout?” (yes/no with comments). Providers were asked: “Please rate the usefulness of this program in improving patient education about gout” rated 1 (extremely) to 5 (not at all); “Please rate the usefulness of this program in improving patient compliance with gout treatment, labs and appointments” rated 1 (extremely) to 5 (not at all); and “Will participating in this program change the way you approach patients with gout in the future?” (yes/no with comments).
Phone call review
The percentage of successful attempts at patient phone contact and duration of calls were logged.
Secondary outcome measures
Patient Gout Self-Management Knowledge exam
This 12-question examination was developed with review of the literature on prior knowledge and/or self-management questionnaires (35,36,37) and with review of principles in a self-management knowledge questionnaire for asthma, which has many comparable educational issues with gout (38). We also incorporated pre-study patient feedback, and reviewed previously published data on myths about gout often believed by patients (39). We recorded the responses to each question at enrollment, 6 and 12 months.
Morisky Compliance Index
Patients completed the validated Morisky compliance questionnaire (40) at enrollment, 6 and 12 months, which includes 4 yes/no questions related to circumstances when medications are not taken as directed, where yes=0 and No= 1 and “0” answers reflect high compliance and “1” answers reflect low compliance, with lowest level of compliance scoring 4.
Gout flare frequency and severity questionnaire
At baseline, 6 and 12 months subjects replied to 5 frequency and severity questions: Question #1: “Number of gouty attacks in previous 6 months.” #2: “How painful have gout attacks in previous 6 months been?” – rated 1 (mild), 2 (between mild and moderate), 3 (moderate), 4 (between moderate and extremely severe), or 5 (not applicable). #3: “How tender have joints been during flares in the previous 6 months?” – rated with the same scale. #4: “How well did flares respond to medications”- rated 1 (very well), 2 (between very well and moderate), 3 (moderate), 4 (between moderate and very poorly) or 5 (not applicable). #5: “How long did gout attacks last in the past 6 months” – rated 1 (1 day), 2 (2 days), 3 (3 days), 4 (4 days), 5 (5 days or more) or 6 (not applicable).
Urate levels
Urate levels done in the course of standard-of-care practice were recorded at baseline, 6 and 12 months.
Statistical Analysis
No formal power analysis was performed because the primary goal of this study was to explore the feasibility and acceptability of our gout education and monitoring program. However, we determined a priori to enroll 3 times the minimum recommended sample size of 12 patients (41), with an additional 25% to account for attrition. Therefore, a total of 45 patients were enrolled in our study. Continuous variables are presented as means with standard deviations or medians with first and third quartiles, depending upon the distribution of the data. Categorical variables are presented as counts and percentages.
RESULTS
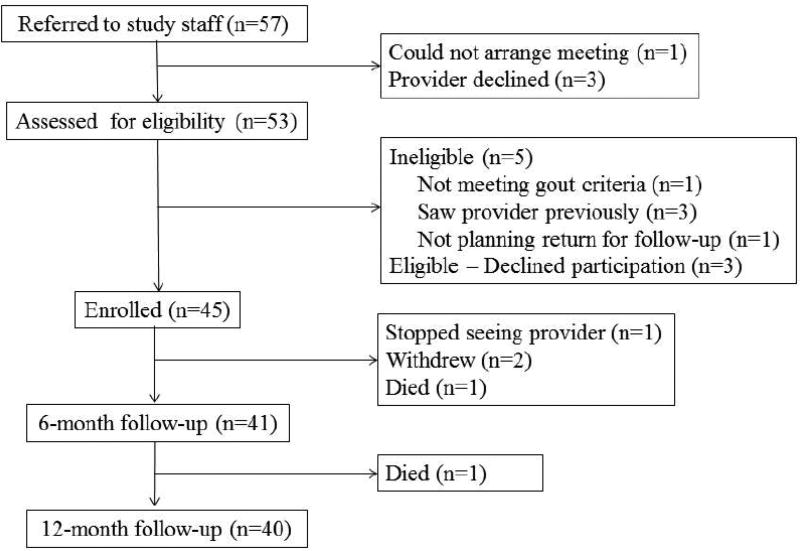
Of 57 patients consecutively referred to study staff, 45 were enrolled, as detailed in Figure 2. In addition to meeting the 1977 ARA Criteria for Diagnosing Gout, as a condition for enrollment, retrospective evaluation found that all met the 2015 ACR/EULAR Gout Classification Criteria (42). Mean ± SD age was 57.0 ± 14.3 years, sex was 84.4% male. Gout duration was median 5 years (Q1=2, Q3=12). Although 73.3% had seen a rheumatologist outside our institution previously for gout, only 28.9% were on ULT at the time of study entry (Table 1).
Figure 2. Patient Flow Diagram.
Table 1. Demographics.
| Variable | N = 45 | |
|---|---|---|
| Age, mean ± SD | 57.0 ± 14.3 | |
| Male, n | 38 (84.4) | |
| Highest education, n (%) | ||
| Graduated high-school | 11 (24.4) | |
| Some college | 2 (4.4) | |
| Graduated college | 18 (40.0) | |
| Post graduate school | 14 (31.1) | |
| Ethnicity, n (%) | ||
| Hispanic or Latino | 2 (4.4) | |
| Not Hispanic or Latino | 43 (95.6) | |
| Race, n (%) | ||
| Asian | 7 (15.6) | |
| Black or African American | 3 (6.7) | |
| White | 35 (77.8) | |
| Serum uric acid, median (Q1,Q3)1 | 7.6 (6.3, 9.1) | |
| Dyslipidemia, n (%) | 20 (44.4) | |
| Hypertension, n (%) | 19 (42.2) | |
| Diabetes mellitus, n (%) | 3 (6.7) | |
| Coronary heart disease, n (%) | 5 (11.1) | |
| Renal dysfunction2, n (%) | 8 (17.8) | |
| Nephrolithiasis, n (%) | 7 (15.6) | |
| Tophi present, n (%) | 10 (22.2) | |
| Has seen rheumatologist at outside institution for gout, n | 33 (73.3) | |
| Has seen primary care in outpatient setting for gout, n | 33 (73.3) | |
| Previously took ULT3, n (%) | 17 (37.8) | |
| Taking ULT at the time of enrollment, n (%) | 13 (28.9) | |
| Years with gout, median (Q1,Q3) | 5 (2,12) | |
Q1,Q3 = First and third quartiles.
Renal dysfunction = eGFR <60 ml/min.
ULT = urate-lowering therapy.
Primary Outcomes
Retention rate
At 6 months, 42 patients (93%) remained in the study and 40 at 12 months (89%) (Figure 2).
Evaluation of Nurse Education Program by subjects and providers
Most patients found the nurse education program to be helpful, with 79.5% at 6 months and 82.1% at 12 months giving scores of 3 or better (Table 2). All providers (8/8) replied “very likely” at 6 and 12 months to the question: “If manpower were available, how likely would you be to employ the Educational Sessions by Nurse in your own practice in the future for your gout patients?”
Table 2. Feasibility Measures.
Subject evaluation of overall program, Nursing and Pharmacist Interventions and phone call frequency.
| Question | 6 month visit (n=39) |
12 month visit (n=39) |
|---|---|---|
| Was the education session with the nurse helpful in your understanding and management of your gout? (1=Very helpful, 5=Not at all) | ||
| 1 10 (25.6) | 12 (30.8) | |
| 2 6 (15.4) | 9 (23.1) | |
| 3 15 (38.5) | 11 (28.2) | |
| 4 5 (12.8) | 6 (15.4) | |
| 5 3 (7.7) | 1 (2.6) | |
| Were the calls from the pharmacist helpful in your management of gout? (1=Very much, 5=Too many) | ||
| 1 7 (17.9) | 7 (17.9) | |
| 2 3 (7.7) | 8 (20.5) | |
| 3 13 (33.3) | 3 (7.7) | |
| 4 4 (10.3) | 7 (17.9) | |
| 5 12 (30.8) | 14 (35.9) | |
| Did you find the number of phone calls about the right number, too many or too few? (1=Too few, 5= Too many) | ||
| 1 1 (2.6) | 1 (2.6) | |
| 2 0 | 0 | |
| 3 33 (84.6) | 27 (69.2) | |
| 4 4 (10.3) | 4 (10.3) | |
| 5 1 (2.6) | 7 (17.9) | |
| Please rate the usefulness of this program in helping you to understand gout and to be able to deal with the condition. (1=Extremely, 5=Not at all) | ||
| 1 9 (23.1) | 10 (25.6) | |
| 2 4 (10.3) | 12 (30.3) | |
| 3 12 (30.8) | 11 (28 2) | |
| 4 8 (20.5) | 5 (12.8) | |
| 5 6 (15.4) | 1 (2.6) | |
| Did this program improve your ability to ask questions about your gout when you saw your doctor or nurse practitioner? | ||
| Yes 17 (43.6) | 23 (59.0) | |
| Would you recommend this program be further studied and considered for other people with gout? | ||
| Yes 38 (97.4) | 35 (89.7) |
Numbers are shown as count (percentage)
Evaluation of Pharmacist Monitoring Program by subjects and providers
More than half of subjects (58.9%) scored the helpfulness of the pharmacist monitoring program at 3 or better at 6 months, and slightly less than half (46.1%) did so at 12 months (Table 2). Subjects found the number of phone calls to be at the correct number in 84.6% at 6 months and 69.2% at 12 months. Providers were asked “If manpower were available, how likely would you be to employ monthly phone calls from pharmacist in your own practice in the future for your gout patients?” At both 6 and 12 months 7/8 (87.5%) replied “very likely.”
Evaluation of overall Multidisciplinary Program by subjects and providers
A majority of subjects rated the usefulness of the overall program to them in managing their gout at a score of 3 or better (64.2% at 6 months and 84.6% at 12 months). Comments included 23.1% stating that they “already knew this information” or “did not need help being compliant.” Subjects asked if the program improved their ability to ask questions of their provider, 43.5% replied “yes” at 6 months and 59.0% at 12 months. Asked if they would recommend this program be further studied and considered for other people with gout they 97.4% replied “yes” at 6 months and 89.7% at 12 months. Comments included that there was perceived value for others, although not so much for them (25.6%), that expanding the scope of the calls (e.g. diet) would be helpful (10.3%) and that the program would be improved by use of other modalities such as email or texting (5.1% ). 9 of 10 providers (90%) rated the overall program as “extremely useful” in improving patient education about gout at both 6 and 12 months. 9 of 10 also rated the program “extremely useful” in improving patient compliance with gout treatment, labs and appointments at both 6 and 12 months. All providers (9/9), at both 6 and 12 month surveys, felt that participating in this program will change the way they approach patients with gout in the future.
Phone call review
The median (Q1, Q3) percentage of enrolled patients reached by phone per month was 67.5% (58.5, 68.9), with a range from 52.5% to 79.5%. Enrolled patients were reached 72.7% (32/44) of the time at month 1 and 67.5% (27/40) of the time at month 12. The median (Q1, Q3) percentage of completed calls < 2 minutes was 66.1% (60.0, 74.2), calls during month 1 were < 2 minutes in 21.9%, and at month 12 were < 2 minutes in 81.5%.
Secondary outcomes
Patient scores on gout knowledge questionnaire
Of the 12 questions (Table 3) (full questionnaire in Supplementary Appendix A), median baseline score for our subjects was 8 (Q1=5, Q3=10) and at 6 months was 10 (Q1=8, Q3=11) and at 12 months 10 (Q1=10, Q3=11). Three questions were especially difficult for subjects: in question #2, regarding possibility of gout flares stopping completely, at 12 months 72.5% of subjects did not correctly identify the goal of gout treatment as “complete resolution of attacks” with the most common incorrect response (in 65.0%) being “get less flares” In question #6, regarding length of bridge medication, at 12 months 27.5% of subjects did not choose the correct 6 month duration. In responding to question #9, 30.0% did not select “genetic makeup” as the most important difference between people who get gout and people who don’t.
Table 3. Gout Self-Management Knowledge Exam.
Scares on individual questions
| Baseline (n=42) |
6 month visit (n=39) |
12 month visit (n=40) |
|
|---|---|---|---|
| Total number of correct responses, median (Q1, Q3) 1 | 8 (5, 10) | 10 (8, 11) | 10 (10, 11) |
| Correct response to individual questions Q1-Q12, 2 n (%) | |||
| Q1 - Importance of avoiding gout triggers | 22 (52.4) | 35 (89.7) | 37 (92.5) |
| Q2 - Success of ULT in completely stopping gout flares | 7 (16.7) | 9 (23.1) | 11 (27.5) |
| Q3 - Defining gout triggers | 31 (73.8) | 33 (84.6) | 36 (90.0) |
| Q4 - Need for both medications and diet | 28 (66.7) | 29 (74.4) | 33 (82.5) |
| Q5 - Need for continuing ULT long-term | 24 (57.1) | 32 (82.1) | 35 (87.5) |
| Q6 - Length of bridge medication when start ULT | 16 (38.1) | 23 (59.0) | 29 (72.5) |
| Q7 - Definition of “rescue” gout medication | 36 (85.7) | 36 (92.3) | 39 (97.5) |
| Q8 - Duration of treatment for gout flare | 34 (81.0) | 35 (89.7) | 38 (95.0) |
| Q9 - Genetic basis of gout | 25 (59.5) | 25 (64.1) | 28 (70.0) |
| Q10 - Identifying bridge medication | 19 (45.2) | 27 (69.2) | 34 (85.0) |
| Q11 - Need for lab monitoring of urate | 38 (90.5) | 38 (97.4) | 40 (100.0) |
| Q12 - Importance of urate goal < 6 | 33 (78.6) | 32 (82.1) | 38 (95.0) |
Q1, Q3 = First and third quartiles.
Q1 to Q12= Question 1 to Question 12.
Morisky Compliance Index
At enrollment, the median Morisky score was 3 (Q1=1, Q3= 3) with 4= best compliance. 6-month median Morisky score was 4 (Q1= 3, Q3=4), and at 12 months it was 4 (Q1=3, Q3=4).
Urate levels
At baseline, serum urate levels for all patients with urate levels determined (n=44) (Table 4) the median was 7.6 (Q1=6.3, Q3=9.1),and at 6 months was 5.5 (Q1=4.4, Q3=6.5) and at 12 months 5.1 (Q1=4.3, Q3=6.2) (Table 4). In patients without tophi, 5/34 (14.7%) were at urate <6 at baseline, and at 6 months 19/30 (63.3%) were < 6.0 and at 12 months 20/28 (71.4%) were < 6.0. In patients with tophi, 0/10 (0%) were at urate <5 at baseline, at 6 months 4/9 (44.4%) were < 5.0 and at 12 months 4/8 (50%) were < 5.0.
Table 4. Gout Outcomes.
Urate Levels and gout flare characteristics
| n | Baseline | n | 6 month visit | n | 12 month visit | ||
|---|---|---|---|---|---|---|---|
| Uric acid level, median (Q1, Q3)1 | 44 | 7.6 (6.3, 9.1) | 39 | 5.5 (4.4, 6.5) | 36 | 5.1 (4.3, 6.2) | |
| No tophi and uric acid level < 6 | 34 | 5 (14.7) | 30 | 19 (63.3) | 28 | 20 (71.4) | |
| Tophi and uric acid level < 5 | 10 | 0 | 9 | 4 (44.4) | 8 | 4 (50.0) | |
| Number of Gouty Attacks in previous 6 months | 42 | 2 (1, 3) | 39 | 1 (0, 2) | 40 | 1 (0, 1) | |
| How painful have gout attacks in previous 6 months been? | 42 | 39 | 40 | ||||
| Mild | 4 (9.5) | 7 (17.9) | 6 (15.0) | ||||
| Between mild and moderate | 4 (9.5) | 3 (7.7) | 1 (2.5) | ||||
| Moderate | 8 (19.0) | 9 (23.1) | 11 (27.5) | ||||
| Between moderate and extremely severe | 14 (33.3) | 5 (12.8) | 1 (2.5) | ||||
| Extremely severe | 11 (26.2) | 0 | 2 (5.0) | ||||
| No flares | 1 (2.4) | 15 (38.5) | 19 (47.5) | ||||
| How tender have joints been during flarespriro 6 months? | 42 | 39 | 40 | ||||
| Mild | 3 (7.1) | 10 (25.6) | 8 (20.0) | ||||
| Between mild and moderate | 4 (9.5) | 0 | 2 (5.0) | ||||
| Moderate | 11 (26.2) | 8 (20.5) | 9 (22.5) | ||||
| Between moderate and extremely severe | 11 (26.2) | 5 (12.8) | 1 (2.5) | ||||
| Extremely severe | 12 (28.6) | 1 (2.6) | 1 (2.5) | ||||
| No flares | 1 (2.4) | 15 (38.5) | 19 (47.5) | ||||
| How well did flares respond to medications? | 42 | 39 | 40 | ||||
| Very well | 13 (31.0) | 12 (30.8) | 15 (37.5) | ||||
| Between very well and moderate | 5 (11.9) | 9 (23.1) | 2 (5.0) | ||||
| Moderate | 14 (33.3) | 2 (5.1) | 3 (7.5) | ||||
| Between moderate and very poor | 3 (7.1) | 0 | 0 | ||||
| Very poor | 1 (2.4) | 0 | 0 | ||||
| Not applicable (not on medication) | 5 (11.9) | 1 (2.6) | 1 (2.5) | ||||
| No flares | 1 (2.4) | 15 (38.5) | 19 (47.5) | ||||
| How long did gout attacks last in the past 6 months? | 42 | 39 | 40 | ||||
| 1 day | 5 (11.9) | 3 (7.7) | 4 (10.0) | ||||
| 2 days | 4 (9.5) | 8 (20.5) | 10 (25.0) | ||||
| 3 days | 5 (11.9) | 3 (7.7) | 2 (5.0) | ||||
| 4 days | 5 (11.9) | 4 (10.3) | 2 (5.0) | ||||
| 5 days or more | 22 (52.4) | 6 (15.4) | 3 (7.5) | ||||
| No flares | 1 (2.4) | 15 (38.5) | 19 (47.5) | ||||
Q1, Q3 = First and third quartiles.
Gout flare frequency and severity questionnaire
(See Table 4). Q#1. The number of gout attacks on completed baseline questionnaires (n=42) showed median gout attacks in the prior 6 months was 2 (Q1=1, Q3=3), at 6 months (n=39) median was 1 (Q1=0, Q3=2) and at 12 months (n=40) median 1 (Q1=1, Q3=0). Level of pain of attacks at baseline was severe to extremely severe in 59.5%, at 6 months in 12.8% and in 7.5% at 12 months. Tenderness of joints at baseline was severe to extremely severe in 54.8%, 15.4% at 6 months and 7.5% at 12 months. The level of response of attacks to medication at baseline was poor to very poor in 9.5%, but at this level in none of the subjects at 6 and 12 months. The length of gout attacks at baseline was 3 days or greater in 76.2%, at 6 months in 33.4% and at 12 months in 17.5%.
DISCUSSION
We are reporting on the feasibility of a multidisciplinary team approach to comprehensive gout management. The model was designed for spaced and sustained learning, beginning with a Gout Self-Management Knowledge Exam followed an RN educational session, both repeated at 6 month intervals. This was coupled with monthly pharmacist phone calls focused on encouragement of overall regimen adherence and addressing patient questions and social work intervention as needed to address potential barriers to care.
Our results support feasibility and acceptability of our program based on program evaluations completed by subjects and providers, success in reaching patients via phone calls and overall program retention. Subjects were very likely to feel the program was helpful to them, to recommend that the program be extended to others with gout and that the monthly phone calls from pharmacists were at the right frequency. Approximately 80% of patients felt their nurse-educator experience made a positive impact on their management and 55% stated this about the pharmacist intervention. Perceived positive impact of the nursing intervention increased from 6 to 12 months and perceived positive impact of the pharmacy intervention decreased at the 12 month mark. Formal questionnaires completed by providers reported that they were very likely to use our program if available outside the study, felt strongly that the program helped gout patient with their regimen adherence, and strongly felt that this program changed the way they would approach patients with gout in the future. Pharmacist phone calls tended to be shorter as the program progressed, at <2 minutes in 81.5% of calls by month 12.
Subjects and providers offered a number of comments via formalized questionnaires that may help future program design. Comments suggested that tailoring the communication route according to patient preference may improve satisfaction. Some subjects found the pharmacist phone calls especially helpful, some less so. We felt that phone calls provided the best opportunity for scripted uniformity and interactivity, although a subject commented that using an email and/or text-based compliance program would be preferable.
As secondary outcomes, we did exploratory analyses of scores on Self-Management Questionnaires, patient assessment of their r overall medication compliance, urate levels and number of gout flares. Scores on Self-Management Questionnaires improved at 6 months and mildly further improved at 12 months. Morisky compliance scores improved from median baseline score at 6 months and minimally further increased at 12 months. At 12 months, 71% of all patients reached urate < 6.0, 69.2% of non-tophaceous patients reached <6.0 and 50% of with tophi reached < 5.0. Gout flares per 6 months were reduced from a median of 2 at baseline to 1 at both 6 and 12 months.
A multidisciplinary program such as ours can likely improve the value of care for gout patients. Current medical practice is moving towards a “team approach” which has the potential for optimizing efficiency, cost-saving and maximizing the advantages of technology (43). Our program lends itself well to electronic medical record coordination and can allow providers to spend less visit time in patient education.
Studies of inter-professional teams have stressed the importance of clear definition of each team-member’s role (44) and sharing tasks and responsibilities between professionals (45), along with each professional having tasks that allow them to practice at the “top of their license.” We found that our team approach fostered a high level of inter-professional communication, e.g. the pharmacists were frequently contacting providers regarding patients being unsure of recent medication changes, upcoming lab testing or timing of next appointment.
Others have pointed out that education is critical in chronic disease self-management but it needs to be combined developing an action plan and carrying it out long-term (46). Patients need healthcare team input between scheduled visits (47). A multi-disciplinary team can divide the labor needed to assist the patient in developing an initial action plan as well as provide the monitoring and interactive continuing education needed to optimize long-term outcomes. Our findings may also be relevant in gout care settings where assembling a multi-disciplinary team is not practical, where either a pharmacist (27) or a nurse (28) may take on the roles that both played in our study.
Limitations of our study include a limited number of patients, a single arm and single center involvement. Our study population had a high educational attainment, and it is possible that patients with lower education levels might benefit more (or less) from a program such as ours. Future studies with a larger and more educationally diverse population will be valuable. Strengths include our documentation of the details of each pharmacist intervention, and formal evaluative input from subjects and providers regarding multiple aspects of the program. Close monitoring of the rate of reaching patients by phone and the length of calls can assist in future analysis of phone vs alternative communication strategies.
Our program of sustained and spaced team education appears feasible, and future modifications could include patient selection of specific aspects of the education and monitoring program, as well as focusing the program on patients felt to be at high risk of non-adherence based on gout knowledge exam or prior non-adherence. Our study suggests several gaps in gout patient knowledge, including bridge therapy, genetic aspects and the achievability of a flare-free state. The irony of poor outcomes despite excellent available gout treatment calls for new strategies. Significant improvement in the quality of life of gout patients seems a likely result of further study of optimal teams to maximize and sustain patients’ self-management knowledge in combination with an effective long-term monitoring program.
Supplementary Material
Acknowledgments
We appreciate the review of our manuscript by Michael Lockshin, MD. We thank the participating patients who stayed with our program and provided critical insights for future improvements in this program, and the non-investigator clinicians who entered their patients and who responded to our program evaluation questionnaires.
FINANCIAL SUPPORT:
Hospital for Special Surgery Academy of Medical Educators, the Joseph and Arlene Taub Foundation and the Frederick W. Richmond Foundation. The REDCap electronic data capture tools are funded by the CTSC grant (grant number UL1 TR000457-06) from the National Center for Advancing Translational Sciences, National Institutes of Health, Bethesda, MD. None of our supporters were involved in the study design, collection, analysis or interpretation of data, the writing of the report or the decision to submit the article for publication.
References
- 1.Becker MA, Fitz-Patrick D, Choi HK, Dalbeth N, Storgard C, Cravets M, et al. An open-label, 6-month study of allopurinol safety in gout: The LASSO study. Sem Arth Rheum. 2015;45:174–83. doi: 10.1016/j.semarthrit.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 2.Doherty M, Jansen TL, Nuki G, Pascual E, Perez-Ruiz F, Punzi L, et al. Gout: why is this curable disease so seldom cured? Ann Rheum Dis. 2012;71:1765–70. doi: 10.1136/annrheumdis-2012-201687. [DOI] [PubMed] [Google Scholar]
- 3.Kuo C-F, Grainge MJ, Mallen C, Zhang W, Doherty M. Rising burden of gout in the UK but continuing suboptimal management: a nationwide population study. Ann Rheum Dis. 2015;74:661–7. doi: 10.1136/annrheumdis-2013-204463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Annemans L, Spaepen E, Gaskin M, Bonnemaire M, Malier V, Gilbert T, et al. Gout in the UK and Germany: prevalence, comorbidities and management in general practice 2000–2005. Ann Rheum Dis. 2008;67:960–6. doi: 10.1136/ard.2007.076232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edwards NL. Quality of care in patients with gout: Why is management suboptimal and what can be done about it? Curr Rheumatol Rep. 2011;13:154–9. doi: 10.1007/s11926-010-0154-6. [DOI] [PubMed] [Google Scholar]
- 6.Roddy E, Zhang W, Doherty M. Concordance of the management of chronic gout in a UK primary-care population with the EULAR gout recommendations. Ann Rheum Dis. 2007;66:1311–5. doi: 10.1136/ard.2007.070755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Solomon DH, Avorn J, Levin R, Brookhart MA. Uric acid lowering therapy: prescribing patterns in a large cohort of older adults. Ann Rheum Dis. 2007;67:609–13. doi: 10.1136/ard.2007.076182. [DOI] [PubMed] [Google Scholar]
- 8.Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the US general population: The National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 2011;63:3136–41. doi: 10.1002/art.30520. [DOI] [PubMed] [Google Scholar]
- 9.DiBonaventura MD, Andrews LM, Yadao AM, Kahler KH. The effect of gout on health-related quality of life, work productivity, resource use and clinical outcomes among patients with hypertension. Expert Rev Pharmacoecon Outcomes Res. 2012;12:821–9. doi: 10.1586/erp.12.60. [DOI] [PubMed] [Google Scholar]
- 10.Chandratre P, Roddy E, Clarson L, Richardson J, Hider SL, Mallen CD. Health-related quality of life in gout: a systematic review. Rheumatology (Oxford) 2013;52:2031–40. doi: 10.1093/rheumatology/ket265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khanna PP, Perez-Ruiz F, Maranian P, Khanna D. Long-term therapy for chronic gout results in clinically important improvements in the health-related quality of life: short form-36 is responsive to change in chronic gout. Rheumatology (Oxford) 2011;50:740–5. doi: 10.1093/rheumatology/keq346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Briesacher BA, Andrade SE, Fouayzi H, Chan KA. Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy. 2008;28:437–43. doi: 10.1592/phco.28.4.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coburn BW, Bendlin KA, Sayles H, Hentzen KS, Hrdy MM, Mikuls TR. Target serum urate: do gout patients know their goal?: Knowledge of target serum urate. Arthritis Care Res. 2016;68:1028–35. doi: 10.1002/acr.22785. [DOI] [PubMed] [Google Scholar]
- 14.Juraschek SP, Kovell LC, Miller ER, Gelber AC. Gout, urate-lowering therapy, and uric acid levels among adults in the United States: Target serum uric acid levels and ULT in gout. Arthritis Care Res. 2015;67:588–92. doi: 10.1002/acr.22469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnston ME, Treharne GJ, Chapman PT, Stamp LK. Patient information about gout: an international review of existing educational resources. J Rheumatol. 2015;42:975–8. doi: 10.3899/jrheum.141442. [DOI] [PubMed] [Google Scholar]
- 16.Kuo C-F, Grainge MJ, Mallen C, Zhang W, Doherty M. Rising burden of gout in the UK but continuing suboptimal management: a nationwide population study. Ann Rheum Dis. 2015;74:661–7. doi: 10.1136/annrheumdis-2013-204463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spencer K, Carr A, Doherty M. Patient and provider barriers to effective management of gout in general practice: a qualitative study. Ann Rheum Dis. 2012;71:1490–5. doi: 10.1136/annrheumdis-2011-200801. [DOI] [PubMed] [Google Scholar]
- 18.Harrold LR, Mazor KM, Peterson D, Naz N, Firneno C, Yood RA. Patients’ knowledge and beliefs concerning gout and its treatment: a population based study. BMC Musculoskelet Disord. 2012;13:1–8. doi: 10.1186/1471-2474-13-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jimenez-Liñan LM, Edwards L, Abhishek A, Doherty M. Online patient information resources on gout provide inadequate information and minimal emphasis on potentially curable urate lowering treatment. Arthritis Care Res. 2016 doi: 10.1002/acr.22981. (Epub) [DOI] [PubMed] [Google Scholar]
- 20.Nguyen AD, et al. Mobile Applications to enhance self-management of gout. Int J Med Inform. 2016 doi: 10.1016/j.ijmedinf.2016.06.021. (Epub) [DOI] [PubMed] [Google Scholar]
- 21.Stamp LK, Merriman TR, Barclay ML, Singh JA, Roberts RL, Wright DFB, et al. Impaired response or insufficient dosage?—Examining the potential causes of “inadequate response” to allopurinol in the treatment of gout. Sem Arth Rheum. 2014;44:170–4. doi: 10.1016/j.semarthrit.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perez-Ruiz F. Treating to target: a strategy to cure gout. Rheumatology (Oxford) 2009;48:ii9–14. doi: 10.1093/rheumatology/kep087. [DOI] [PubMed] [Google Scholar]
- 23.Jennings CG, Mackenzie IS, Flynn R, Ford I, Nuki G, De Caterina R, et al. Up-titration of allopurinol in patients with gout. Sem Arth Rheum. 2014;44:25–30. doi: 10.1016/j.semarthrit.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 24.Khanna D, Khanna PP, Fitzgerald JD, Singh MK, Bae S, Neogi T, et al. 2012 American College of Rheumatology guidelines for management of gout. Part 2: Therapy and antiinflammatory prophylaxis of acute gouty arthritis. Arthritis Care Res. 2012;64:1447–61. doi: 10.1002/acr.21773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khanna D, Fitzgerald JD, Khanna PP, Bae S, Singh MK, Neogi T, et al. 2012 American College of Rheumatology guidelines for management of gout. Part 1: Systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res. 2012;64:1431–46. doi: 10.1002/acr.21772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krishnan E, Lienesch D, Kwoh CK. Gout in ambulatory care settings in the United States. J Rheumatol. 2008;35:498–501. [PubMed] [Google Scholar]
- 27.Greer N, et al. Pharmacist-led chronic disease management: A systematic review of effectiveness and harms Compared with Usual Care. Ann Intern Med. 2016 doi: 10.7326/M15-3058. (Epub) [DOI] [PubMed] [Google Scholar]
- 28.Larsson I, Arvidsson S, Bergman S, Arvidsson B. Patients’ perceptions of drug information given by a rheumatology nurse: A phenomenographic study. Musculoskeletal Care. 2010;8:36–45. doi: 10.1002/msc.164. [DOI] [PubMed] [Google Scholar]
- 29.Rees F, Jenkins W, Doherty M. Patients with gout adhere to curative treatment if informed appropriately: proof-of-concept observational study. Ann Rheum Dis. 2013;72:826–30. doi: 10.1136/annrheumdis-2012-201676. [DOI] [PubMed] [Google Scholar]
- 30.Goldfien RD, Ng MS, Yip G, Hwe A, Jacobson A, Pressman A, et al. Effectiveness of a pharmacist-based gout care management programme in a large integrated health plan: results from a pilot study. BMJ Open. 2014 doi: 10.1136/bmjopen-2013-003627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kelley P, Whatson T. Making long-term memories in minutes: a time pattern from memory research in education. Front Hum Neurosci. 2013;7:589. doi: 10.3389/fnhum.2013.00589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lambert C. Learning by degrees. Harvard Magazine. 2009 Nov-Dec;:10–2. [Google Scholar]
- 33.Wallace SL, Robinson H, Masi AT, Decker JL, McCarty DJ, Yü TF. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 1977;20:895–900. doi: 10.1002/art.1780200320. [DOI] [PubMed] [Google Scholar]
- 34.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Colwell HH, Hunt BJ, Pasta DJ, Palo WA, Mathias SD, Joseph-Ridge N. Gout Assessment Questionnaire: initial results of reliability, validity and responsiveness. Internat J Clin Pract. 2006;60:1210–7. doi: 10.1111/j.1742-1241.2006.01104.x. [DOI] [PubMed] [Google Scholar]
- 36.Spaetgens B, Linden S van der, Boonen A. The Gout Assessment Questionnaire 2.0: cross-cultural translation into Dutch, aspects of validity and linking to the International Classification of Functioning, Disability and Health. Rheumatology. 2014;53:678–85. doi: 10.1093/rheumatology/ket423. [DOI] [PubMed] [Google Scholar]
- 37.Harrold LR, Mazor KM, Peterson D, Naz N, Firneno C, Yood RA. Patients’ knowledge and beliefs concerning gout and its treatment: a population based study. BMC Musculoskelet Dis. 2012;13:180. doi: 10.1186/1471-2474-13-180. (Epub) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mancuso CA, Sayles W, Allegrante JP. Development and testing of the Asthma Self-Management Questionnaire. Ann Allergy Asthma Immunol. 2009;102:294–302. doi: 10.1016/S1081-1206(10)60334-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ogdie AR, Hoch S, Dunham J, Von Feldt JM. A roadmap for education to improve the quality of care in gout. Curr Opin Rheumatol. 2010;22:173–80. doi: 10.1097/BOR.0b013e328335eee3. [DOI] [PubMed] [Google Scholar]
- 40.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat. 2005;4:287–91. [Google Scholar]
- 42.2015 Gout Classification Criteria: An American College of Rheumatology/European League Against Rheumatism Collaborative Initiative. Arthritis Rheum. 2015;67:2557–68. doi: 10.1002/art.39254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Landro, Laura The doctor’s team will see you now: Why visit one doctor when some offices offer a medical entourage? Wall Street Journal. 2014 Feb 17; sect.D1. [Google Scholar]
- 44.Farrell B, Pottie K, Woodend K, Yoa VH, Kennie N, Sellors C, et al. Developing a tool to measure contributions to medication-related processes in family practice. J Interprof Care. 2008;22:17–29. doi: 10.1080/13561820701828845. [DOI] [PubMed] [Google Scholar]
- 45.Peron, Noelle J, Cerutti B, Picchilottino P, Empeyta S, Cinter F, van Gessel E. Needs assessment for training in interprofessional skills in Swiss primary care: a Delphi study. J Interprof Care. 2014;28:273–5. doi: 10.3109/13561820.2013.878321. [DOI] [PubMed] [Google Scholar]
- 46.Ory MG, Ahn S, Jiang L, Smith ML, Ritter PL, Whitelaw N, Lorig K. Successes of a national study of the Chronic Disease Self-Management Program: meeting the triple aim of health care reform. Med Care. 2013;1:992–8. doi: 10.1097/MLR.0b013e3182a95dd1. [DOI] [PubMed] [Google Scholar]
- 47.Asch DA, Muller RW, Volpp KG. Automated Hovering in Health Care — Watching Over the 5000 Hours. N Engl J Med. 2012;367:1–3. doi: 10.1056/NEJMp1203869. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.