Why was the cohort set up?
A demographic change towards an increasing proportion of old and oldest - old in high-income countries has taken place since World War II (WW2). The past decades’ improved survival among older people is the main driving force, but it is further strengthened by declining birth rates and the large post-WW2 birth cohorts (‘the Baby Boomers’) entering the old age segment.1 The increasing proportion of individuals reaching their 10th and 11th decade2,3 is a success in terms of survival, but concerns have been expressed that this comes with a cost. The ‘Failure of Success’ hypothesis states that an increasing proportion of individuals surviving to very old ages (Success) will also show higher mean levels of disability and disease at these ages (Failure), thus challenging the welfare of societies.4 However, an alternative hypothesis could be that of a ‘Success of Success’, i.e. more people living to the highest ages because of better functional health.5 Studies investigating which of the two hypotheses seems to prevail have mainly been conducted in people younger than 85 years.6–8 To assess secular trends in the health and functioning of the very old we investigated four complete Danish birth cohorts in the period from 1995 to 2015: the 1895, 1905, 1910 and 1915 birth cohorts.
Who is in the cohort? Study designs of the 1895, 1905, 1910 and 1915 Birth Cohort Studies
The four cohort studies were organized from the Unit of Epidemiology, University of Southern Denmark. They were identical in key respects: all were population-based nationwide studies that included all individuals born in the respective birth year and living in Denmark. There were no exclusion criteria, and proxy interviews were sought if a potential participant was considered unable to participate. The surveys received approval from the Scientific Ethical Review Board (trial numbers, 1895: 95/93 and 95/93 MC; 1905: VF-20040240; 1910/1915-East and baseline: S-20100011; 1915-West: S-20140099) and the Danish Data Protection Agency (1905: 2015-41-3834; 1910/1915: 2016-41-4552).
The exact numbers of eligible nonagenarians and centenarians in the four different cohorts were identified through the Danish Civil Registration System (CRS).9 Eligible participants first received a letter explaining the purpose of the study. Two weeks later, contact was made by phone or personal visit. If the invited participant accepted, an appointment was made. All participants were visited in their homes, including nursing homes, and informed consent was collected at the start of the visit.
However, the four studies differed in one methodological aspect: the assessments of the 1895 cohort and the second wave of the 1915 cohort in the western region of Denmark were conducted by a geriatrician and a nurse, and participants were visited shortly after their birthday (all participants were nearly the same age). The assessments of the 1905, 1910, 1915-first wave and 1915-second wave in the east were carried out by trained lay interviewers from the Danish Institute of Social Research and participants were visited in a predefined period (participant age could vary by up to 1 year in each survey). The start of the predefined period was set to the interview date of the first person to be interviewed. Moreover, the studies differed in the number of follow-up visits, i.e. the 1895, 1905 and 1915 birth cohort studies included one to seven follow-up visits, whereas the 1910 birth cohort was interviewed only in a baseline survey.
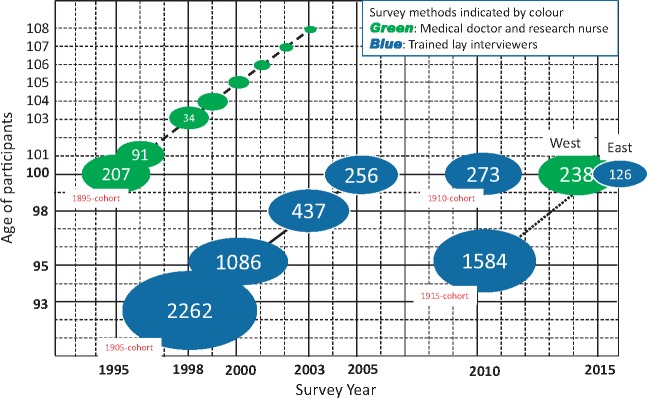
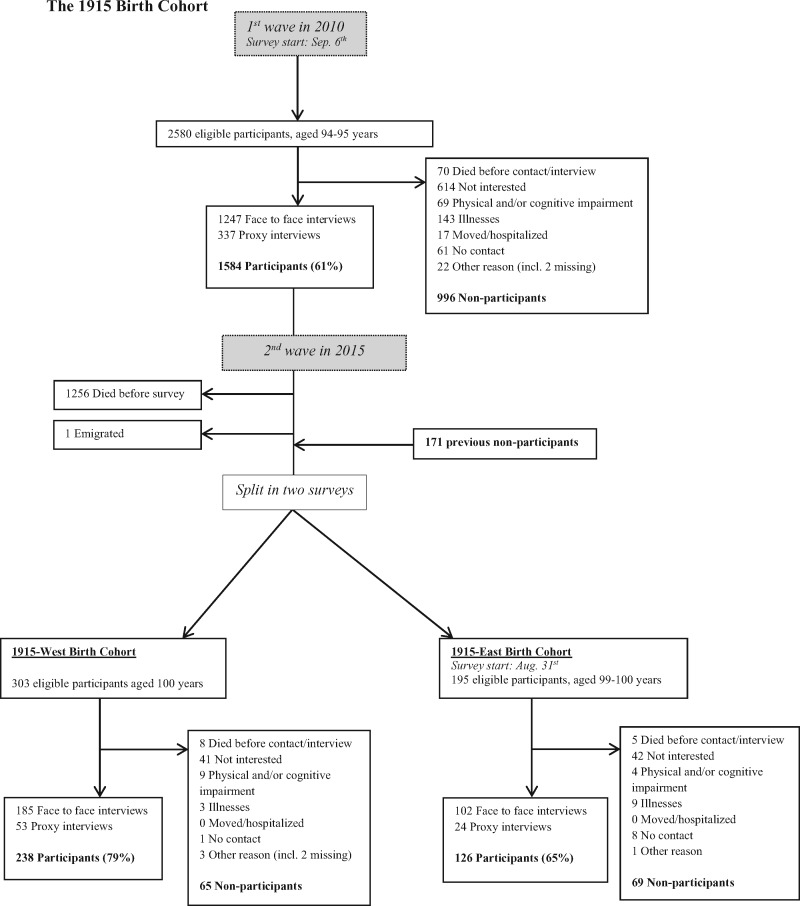
Figure 1 presents an overview of the four cohorts, and the flow chart (Figures 2–5) for each of the cohort studies provides details. Additionally, Table 1 provides details about participation status and 6-month mortality for participants and non-participants.
Figure 1.
Lexis diagram of the 1895, 1905, 1910 and 1915 Danish Birth Cohorts a section Ellipse: indicates each survey and the number indicates the participants in the survey.
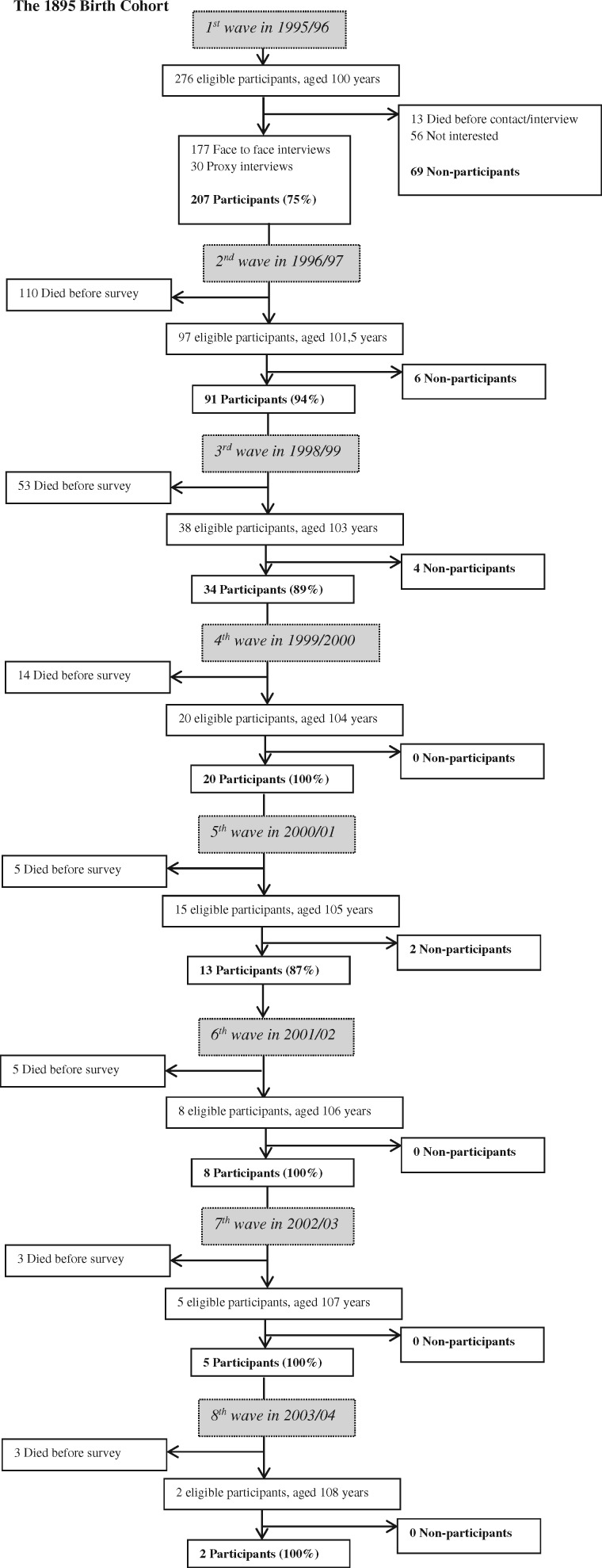
Figure 2.
Flowchart of the 1895 Birth Cohort (% participated).
Table 1.
Participation status and six-month mortality in the 1895, 1905, 1910, and 1915 Birth Cohort Studies
| Cohort | 1895 baseline | 1905 baselinea | 1905 4th wavea | 1910 | 1915 baseline | 1915–West | 1915–East | |
|---|---|---|---|---|---|---|---|---|
| Survey data | Age of participants, years | 100 | 92–93 | 99–100 | 99–100 | 94–95 | 100 | 99–100 |
| Survey period: time of year | All year | Autumn | Spring | Autumn | Autumn | All year | Autumn | |
| Invited: total (male/female), n | 276 (54/222) | 3725 (877/2848) | 439 (70/369) | 428 (77/351) | 2580 (582/1998) | 303 (46/257) | 195 (24/171) | |
| Participation | Total participation rate, n (%)b | 207 (75) | 2262 (61) | 256 (58) | 273 (64) | 1584 (61) | 238 (79) | 126 (65) |
| Male participation rate, n (%) | 45 (83) | 584 (67) | 42 (60) | 59 (77) | 394 (68) | 40 (87) | 20 (83) | |
| Female participation rate, n (%) | 162 (73) | 1678 (59) | 214 (58) | 214 (61) | 1190 (60) | 198 (77) | 106 (62) | |
| Male/female participation rate ratio (95% CI)c | 1.14 (0.99;1.32) | 1.13 (1.07;1.20) | 1.03 (0.84;1.28) | 1.26 (1.08;1.46) | 1.14 (1.06;1.22) | 1.13 (0.99;1.29) | 1.34 (1.09;1.67) | |
| Six-month mortality | Total deaths, n (%) | 65 (24) | 512 (14) | 102 (23) | 123 (29) | 384 (15) | 53 (17) | 39 (20) |
| dNon-participants deaths, n (%) | 21 (30) | 273 (19) | 57 (31) | 50 (32) | 195 (20) | 20 (31) | 14 (20) | |
| eParticipants deaths, n (%) | 44 (21) | 239 (11) | 45 (18) | 73 (27) | 189 (12) | 33 (14) | 25 (20) | |
| fNon-participant vs participant relative risk of death (95% CI) | 1.43 (0.92;2.23) | 1.77 (1.50;2.07) | 1.77 (1.26;2.49) | 1.21 (0.89;1.63) | 1.64 (1.37;1.97) | 2.22 (1.37;3.60) | 1.02 (0.57;1.84) |
1905 birth cohort: data only shown for baseline and 4th wave.
Both sexes combined.
Male/female ratio shown with 95% CI = 95% confidence interval for the ratio.
Non-participants: 6-month mortality was evaluated as the risk of death after 6 months of follow-up from 100 years of age for the 1895 baseline and the 1915-West Birth Cohort study or from the interview date of the first person interviewed in the other cohort studies. There was no loss to follow-up in this period.
Participants: 6-month mortality was evaluated as the risk of death after 6 months of follow-up from the interview date of each participant in all four different cohort studies. There was no loss to follow-up in this period.
Risk of death in non-participants compared with participants. If adjusted by sex and age at the date of the first interview, the results were similar.
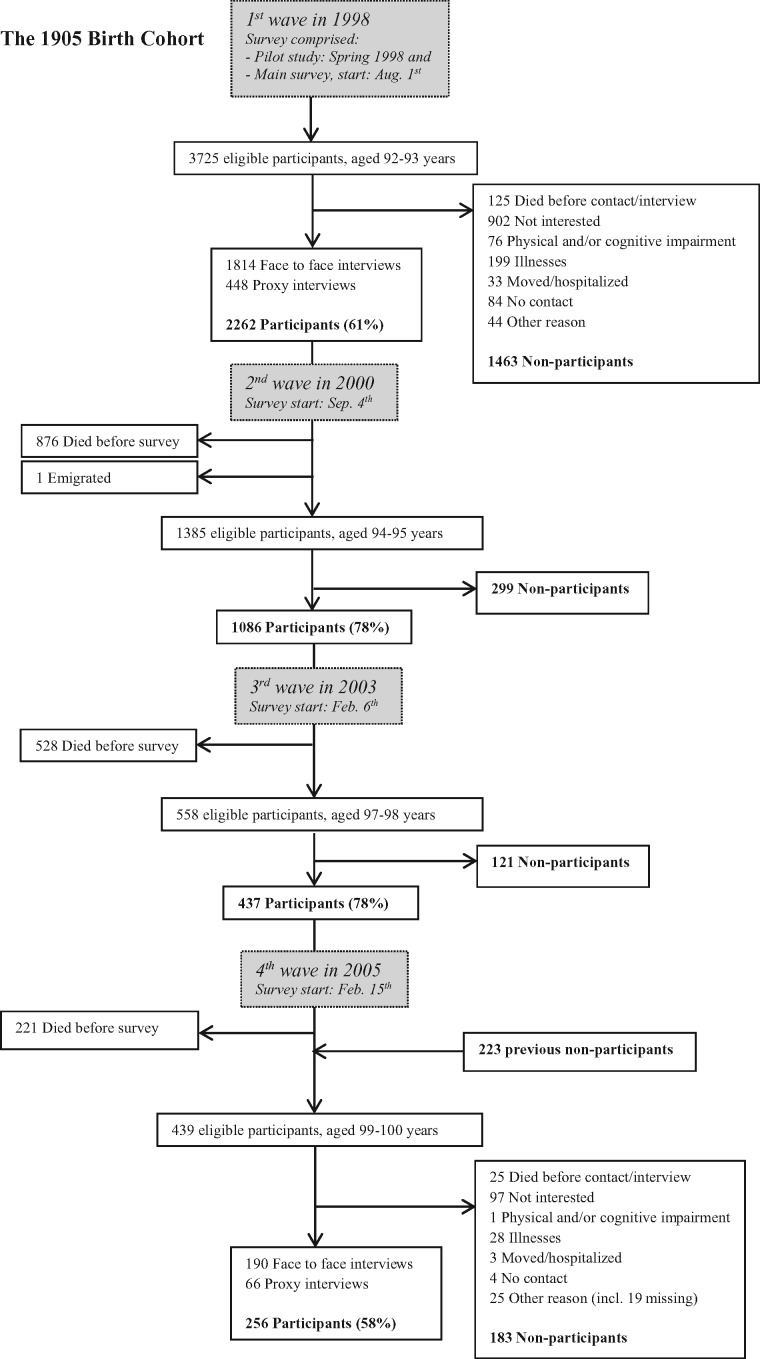
Figure 3.
Flowchart of the 1905 Birth Cohort (% participated).
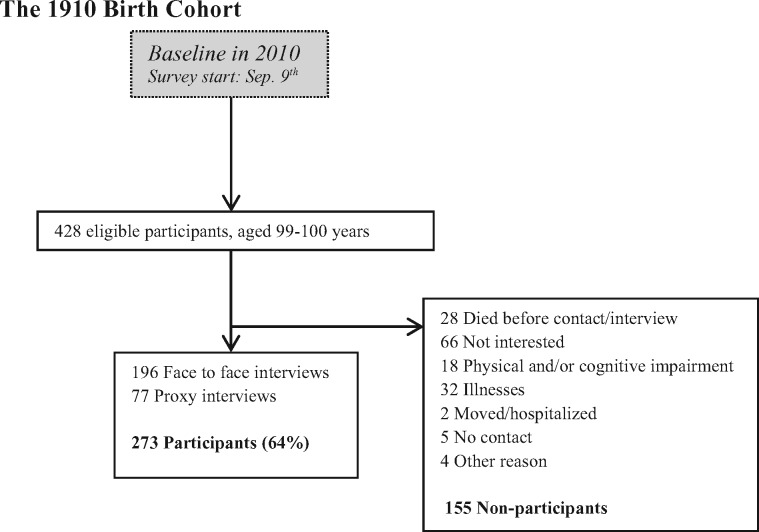
Figure 4.
Flowchart of the 1910 Birth Cohort (% participated).
Figure 5.
Flowchart of the 1915 Birth Cohort (% participated).
The 1895 Birth Cohort Study
The study was initiated by K.A.R., B.J. and J.W.V. It included all persons born in the period from 1 April 1895 to 31 May 1896.10 The baseline survey took place within 3 months of the participant's 100th birthday. Out of 276 eligible individuals, 207 (75%) participated, of whom 22% were males and 14% were proxy interviewees. Males had a higher participation rate compared with females,11 and non-participants had a higher 6-month mortality than participants. The same survey team conducted seven follow-ups until the cohort was deceased.
The 1905 Birth Cohort Study
This study was initiated by K.C., M.M., B.J. and J.W.V. It comprised four waves of 3-5 months each during a 7-year period from 1998 to 2005 and included all individuals born in 1905.12,13 Out of 3725 persons at baseline, a total of 2262 (61%) participated in a pilot study in the spring of 1998 and in the main study from August to October 1998, of whom 26% were males and 20% were proxy interviewees. The pilot study included 200 participants out of 281 invited and used the same methodology as the main study. Males had a higher participation rate compared with females, and non-participants had a higher six-month mortality than participants.13 Surviving participants were followed up in person in 2000 and 2003. From February to July 2005, all the surviving birth cohort members were invited to participate irrespective of previous participation. Out of 439 invited individuals, 256 (58%) participated, of whom 16% were males and 26% were proxy interviewees.
In the fourth survey (in 2005) there were no differences between non-participants and participants with respect to sex. However, there was a higher 6-month mortality among non-participants than participants.
The 1910 Birth Cohort Study
This study was initiated by K.C., M.M., J.W.V. and B.J. It included those born in 1910 and took place from September to November 2010.14 Out of 428 eligible individuals, 273 (64%) participated. Of these, 22% were males and 28% were proxy interviewees.14 Males had a higher participation rate compared with females, and non-participants had a higher 6-month mortality than participants.
The 1915 Birth Cohort Study
This cohort was initiated by K.C., B.J., J.W.V. and M.M. It was first surveyed from September to November 2010.5 Of the 2580 eligible individuals, 1584 (61%) participated, of whom 25% were males and 21% were proxy interviewees. Males had a higher participation rate compared with females, and non-participants had a higher 6-month mortality than participants.
A follow-up was conducted in 2015, when all the surviving birth cohort members were invited again to participate irrespective of previous participation. The increasing proportion surviving to 100 years made it possible to divide the sample into two. The methodology of the 1895 cohort study was applied to roughly half of the population living in the country west of the Great Belt (‘1915-West’), and the methodology used in the 1905, 1910 and the first survey of the 1915 Cohort Study was used east of the Great Belt (‘1915-East’). This division of the second wave enabled a comparison of the 1915 cohort with all the other birth cohorts, hereby avoiding potential bias due to differences in methodology.14
1915-West Birth Cohort
This study included cohort members born in 1915, turning 100 and living in the west of Denmark. The survey took place within 3 months from the participant's 100th birthday. Out of 303 eligible individuals, 238 (79%) participated, of whom 17% were males and 22% were proxy interviewees. Males had a higher participation rate compared with females, and non-participants had a higher 6-month mortality than participants.
1915-East Birth Cohort
This study included those born in 1915, living in the east of Denmark, and the survey took place from August to November 2015. Out of 195 eligible individuals, 126 participated (65%) of whom 16% were males 19% were proxy interviewees. Males had a higher participation rate compared with females; however, non-participants had similar 6-month mortality compared with participants. The supplementary material (available as Supplementary data at IJE online) includes a detailed description of the second wave of the 1915 survey (1915-East and 1915-West), as this has not been described previously.
How often have they been followed up?
Figures 1–5 provide details about the in-person assessments. Each of the cohort studies is linked to national health and population registers, thereby obtaining complete follow-up on, for example, hospitalization and mortality (except for five persons of whom four emigrated and one was lost to follow-up). The Danish National Discharge Register15 (since 1977) holds individual information on all in- and outpatient hospital contacts, including discharge diagnoses and operations. Also, a linkage to the Danish Cancer Registry16 (established in 1943) was made. The most recent linkage to these two registers was made in 2011 for all the cohorts. Causes of death have been obtained by linkage to the Danish Register of Causes of Death,17 and the latest linkage was in 2013 for all the cohorts. Information on vital status and migration is obtained through yearly linkage to the CRS9 in order to follow up on the cohorts until death of all cohort members. By 1 June 2016, 100% were deceased in the 1895 and 1905 cohorts, whereas 96% were deceased in 1910 birth cohort and 86% in the 1915 birth cohort.
What has been measured?
The birth cohorts are described according to the two survey methods used, i.e. the 1895 and 1915-West study method and the 1905, 1910 and 1915-East study method, respectively. Table 2 gives an overview of the measurements in the four cohort studies.
Table 2.
Survey data and measures of the 1895, 1905, 1910 and 1915 Birth Cohort Studies
| Cohort | 1895 | 1905 | 1910 | 1915 baseline | 1915-West | 1915-East | |
|---|---|---|---|---|---|---|---|
| Survey data | Survey year | 1995-96 (baseline) | 1998 (baseline) | 2010 | 2010 (baseline) | 2015 (follow-up) | 2015 (follow-up) |
| 1996-2004 (follow-up) | 2000/2003 (2nd/3rd wave) | ||||||
| 2005 (4th wave) | |||||||
| Age participants, years (survey) | 100 (baseline) | 92-93 (baseline) | 99-100 | 94-95 | 100 | 99-100 | |
| 101-108 (2nd to 8th wave) | 94-98 (2nd to 3rd wave) | ||||||
| 99-100 (4th wave) | |||||||
| Participation rate, % (survey) | 75 (baseline) | 61 (baseline) | 64 | 61 | 79 | 65 | |
| 87-100 (follow-up) | 78 (2nd and 3rd wave) | ||||||
| 58 (4th wave) | |||||||
| Survey method | Nationwide cohort study | Nationwide cohort study | Nationwide cohort study | Nationwide cohort study | Nationwide cohort study | Nationwide cohort study | |
| Interviewer | MD/nurse | Lay interviewer | Lay interviewer | Lay interviewer | MD/nurse | Lay interviewer | |
| Follow-up, n | 7 | 3 | 0 | 1 | - | - | |
| Measures | |||||||
| Sociodemography | Education, previous work | Yes | Yes | Yes | Yes | Yes | Yes |
| Lifestyle | Alcohol and tobacco habit | Yes | Yes | Yes | Yes | Yes | Yes |
| Physical function | Activities of daily livinga | Yes | Yes | Yes | Yes | Yes | Yes |
| Health | Information on healtha | Yes | Yes | Yes | Yes | Yes | Yes |
| Medicationa | Yes | Yes | Yes | Yes | Yes | Yes | |
| Cognition | MMSEb | Yes | Yes | Yes | Yes | Yes | Yes |
| Composite Scorec | No | Yes | Yes | Yes | Yes | Yes | |
| Dementia | CDRd | Yes | No | No | No | No | No |
| Depression | Camdexe | No | Yes | Yes | Yes | Yes | Yes |
| Physical tests | Gait speed | No | Yes | Yes | Yes | No | Yes |
| Grip strenght | No | Yes | Yes | Yes | Yes | Yes | |
| Chair stand | No | Yes | Yes | Yes | Yes | Yes | |
| Other physical testf | Yes | Yes | No | No | No | No | |
| Lung function | Peak flow/spirometry | Yes | Yes | Yes | Yes | Yes | Yes |
| Cardiovascular | Blood pressure | Yes | No | No | No | Yes | Yes |
| Ankle brachial index | Yes | No | No | No | Yes | No | |
| Electrocardiogram | Yes | No | No | No | Yes | No | |
| Echocardiography | No | No | No | No | Yes | No | |
| Orthostatic blood pressure | No | No | No | No | Yes | No | |
| Pulse measure (manual) | No | Yes | Yes | Yes | No | No | |
| Thyroid | Gland volumeg | Yes | No | No | No | No | No |
| Blood sample | Venous blood sample | Yes | Yesh | No | No | Yes | No |
| DNA from blood spot/ cheek swap | No | Yes | Yes | Yes | No | No | |
Information based on self-report.
The Mini Mental State Examination to evaluate cognitive function, scores from 0 to maximum 30 points.
Comprises five cognitive tests to evaluate cognitive function.
Clinical Dementia Rating to diagnose and rate dementia.
Scale to measure symptoms of depression.
Other physical tests. In 1895 cohort: picking up a coin from the floor; turning 360 degrees. In 1905 cohort: moving the arms above the head, behind the neck/back and down to the foot.
The 1895 cohort: from a subsample (n = 50) in the first follow-up (aged 101.5 years).
Venous blood sample from the 1905 cohort: in 1998 (n = 181 participants aged 92-93 years), and in 2005 (n = 127 participants aged 99-100 years).
The 1895 and 1915-West Birth Cohorts
Both surveys comprised an interview including questions regarding socio-demographic factors, lifestyle, activities of daily living (ADL scales by Avlund18 and Katz19), self-reported health, and medication. Cognition was evaluated by Mini-Mental State Examination (MMSE).20 The surveys also included a broad medical examination that involved measurements of arm and ankle blood pressure, electrocardiogram (ECG), spirometry (lung function) and collection of a venous blood sample. But there were also differences: the 1915-West comprised an additional composite of five cognitive tests21 and measurements of symptoms of depression [scale: Cambridge Mental Disorders of the Elderly Examination (CAMDEX)22,23]. Additionally, the examination included an echocardiography and measurements of orthostatic blood pressure, peak flow, chair stand5 and grip strength.5 In the 1895 cohort an instrumental ADL scale (Lawton24), a short physical performance test and a neurological assessment were also carried out. Furthermore, dementia diagnosis and rating were assessed by cognitive performance tests and Clinical Dementia Rating.25
At each follow-up of the 1895 cohort, information on changes in health since the last visit, hospitalization, change of housing, ADL, medication and cognition (MMSE) was collected together with a venous blood sample. Thyroid gland volume was carried out in 50 randomly selected individuals aged 101.5 years.26
The 1905, 1910 and 1915 (baseline and East) Birth Cohorts
The interview, cognitive tests and depression assessment were similar to those described for the 1915-West cohort. Moreover, physical tests including grip strength, chair stand, gait speed5 and clinical measurements such as arm blood pressure, manual pulse measure and lung peak flow assessment were also carried out. Biological material for genetic analyses was obtained from the 1905, 1910 and 1915 cohorts (only at baseline) by collection of dry blood spots, cheek swabs or a venous blood sample as specified in Table 2.
Key findings and publications
The aim of the cohort studies was to assess health and physical and cognitive abilities among the oldest-old and how these may have changed over the past two decades - as a ‘failure of success’ or a ‘success of success’. Up through 2016, studies of the cohorts have resulted in 114 publications. Among the key findings of these studies are the following.
1895 Birth Cohort - healthy centenarians do not exist, but autonomous centenarians do
In the 1895 cohort, the prevalence of chronic diseases was high. Major cardiovascular diseases (chronic heart failure, myocardial infarction, atrial fibrillation, hypertension and pacemaker implant) and dementia affected 72%11 and 51%27, respectively. According to ADL (Katz index19), 41% were described as being relatively independent of help in basic activities of daily living.11 Despite the high prevalence of chronic diseases and the high level of functional dependency, a minor proportion (n = 25, 12%) could be described as autonomous, i.e. they were non-institutionalized, functionally independent in basic ADL and cognitively intact. However, this independent but small group of 100-year-olds had the same mean level of morbidities as the remaining 88% of the study population.11
The 1905 Birth Cohort - exceptional longevity does not lead to exceptional levels of disability
The 1905 Cohort Survey in 1998 (at age 92–93) found that 43% were relatively independent in basic ADL.28 Self-rated health showed that 56% considered their health to be excellent or good.
The four assessments from age 92–93 to 99–100 made large-scale studies of change possible. The analysis showed that compared with intake at age 92–93, the mean of cognitive and physical function measurements of the surviving cohort members at follow-up did not change over the following years to age 99–100.12 Also, the proportion of independent cohort members was almost constant in the study periods from 1998 to 2005. For the individuals who survived to 99–100 years, however, the proportion that could live independently fell from 70% when they were 92–93 years old to 33% when they were 99–100 years old. The explanation for this finding is selective mortality: the most frail and disabled cohort members were the most likely to die - leaving a fairly unchanged cohort composition over time. So, on average, a 100-year-old was not more disabled than a 93-year-old, despite a decline on the individual level.
The 1905 Birth Cohort vs the 1915 Birth Cohort - a success of success
The chance of surviving to 93 and 95 years was around 30% higher in the 1915 cohort than in the 1905 cohort. A comparison of the baseline studies of the 1915 birth cohort (aged 94–95 years) and the 1905 birth cohort (aged 92–93 years) revealed that despite the participants in the 1915 cohort being on average 2.2 years older than those in the 1905 cohort, the most recent cohort performed better in cognitive functioning and had a higher ADL-score. These findings indicate that more people are living to older ages and with better overall functioning.5
No survival association with the ‘usual suspects’ in the oldest-old
Despite a large sample size and virtually complete follow-up, the well-known mortality predictors in middle-aged and young old, e.g. smoking, obesity, education and a number of chronic diseases, were not found to be associated with mortality in the oldest - old.29–31 However, measures of ADL and cognitive and physical abilities were strong predictors of mortality among the oldest - old-and to some degree also an optimistic personality.29,30,32
The MMSE test combined with a chair stand test provided a simple, powerful differentiation of the survival probabilities of nonagenarians. Nonagenarian men and women not being able to stand from a chair had only a 2% chance of surviving to 100, whereas for those with a high MMSE-score (28-30) and being able to stand up without using hands, the likelihood increased to 22% and 34% for men and women, respectively.30 Similar results were shown if the chair stand was replaced with an ADL score (Katz index19).
Twin and family studies have indicated that the influence of genetic factors on survival probability increases with age.33 In the 1905 Cohort Study, Apo-E was associated with mortality, but the effect size was modest.34 Comparison of Apo-E across the four birth cohorts showed a lower prevalence in the most recent cohorts with the better survival.35
Centenarians - a useful model of healthy ageing
A register-based study of hospitalizations in the 1905 birth cohort from 1977 to 2004 showed that those who survived to age 100 had lower hospitalization rates and shorter in-hospital stays in their 70s and 80s than their shorter-lived peers,36 indicating healthier ageing throughout old age.
Strengths of the studies
A major strength is that the studies comprised complete national birth cohorts with no exclusion criteria. Furthermore, participation rates were comparable in the cohorts where the same study design was used. Because of the Danish CRS,9 complete follow-up and testing for differences between non-participants and participants were possible. The studies are further strengthened by the methodology of conducting in-person domiciliary interviews, hereby including a greater proportion of the frail population, as well as clinical examinations and linkage to registers with respect to diseases. To determine health profiles, a physical examination and linkage to registers provide higher reliability of the health information than does a comparison with self-reported information alone.37 In the very old, some diseases may stay unrecognized due to possible ageism or because of subtle symptoms of, for example, heart disease.38 Some diseases can be revealed by a clinical examination together with the interview.
Weaknesses of the studies
A potential weakness is the non-participation rates, particularly in the cohorts interviewed by lay interviewers, as they obtained the relatively lowest participation rates (range 58-65%, see Table 1), leaving room for healthy participation bias.14,39 In all surveys, males had higher participation rates than females and the male/female participation rate ratio was fairly similar between the surveys (see Table 1). By allowing for proxy interviews and by also including nursing home residents, it was possible for even the frailest person to participate, thereby reducing selection bias. However, we did find that in all studies non-participants had a higher risk of dying within 6 months of follow-up, indicating that terminal illness might be a reason for not participating either in person or by proxy (see Table 1).
It might be expected that the percentage of proxy visits would differ between the surveys conducted by a geriatrician and a nurse and those conducted by lay interviewers, because of the differences in participation rates (about 75% vs about 62%). If there was a selection bias towards more healthy participants in the studies with the lowest participation rates, then more proxy visits might be expected in the surveys with the highest participation rates. But the proportion of proxy visits did not differ, being approximately 20% in both survey types, indicating a good sample representativeness of the different cohort populations.
Can I get hold of the data? Where can I find out more?
The research group of the Danish Aging Research Center at the University of Southern Denmark welcomes collaboration. Anonymous data are available to researchers after they have applied for access and their project has been approved by the research group. The cohorts have been used in multiple international collaborations on, for example, genetics of longevity40 and international comparisons of oldest-old populations.41 More information can be found on the webpage [www.sdu.dk/en/om_sdu/institutter_centre/darc]. For further details or requests, please contact Professor Kaare Christensen at [kchristensen@health.sdu.dk].
Danish Birth Cohorts profile in a nutshell
The aim of the cohort studies was to assess health and physical and cognitive abilities among the oldest-old and how this may have changed over the past two decades.
Participants were recruited from four complete Danish birth cohorts: the 1895, 1905, 1910 and 1915 birth cohorts. All were population-based nationwide studies.
More than 6500 in-home visits have been carried out since 1995. Participants were aged 93-100 at intake. Follow-ups have been conducted from 0 to 7 times in each cohort. Participation rates were between 58% and 100%, with an overall rate of 81%. The latest follow-up was completed in 2016.
The assessments included a comprehensive interview, cognitive and physical testing, clinical examination (only in the 1895 cohort and 1915-West) and collection of biological material. Moreover, virtually complete follow-up was achieved through national health and mortality registers.
The research group welcomes collaboration. More information can be found on the webpage [www.sdu.dk/en/om_sdu/institutter_centre/darc]
Supplementary Data
Supplementary data are available at IJE online.
Funding
The various studies of the Danish Birth Cohorts have received funding from different contributors. They are presented here as an assembled list: Danish National Research Foundation; U.S. National Institute on Aging - National Institutes of Health [grant PO1-AG08761]; Danish Health Insurance Foundation [grant 2006B139]; Danish Agency for Science, Technology and Innovation; Danish Interdisciplinary Research Council; Danish Council for Independent Research – Medical Science [grant 09-070081]; Novo Nordisk Foundation; Faculty of Health Sciences, University of Southern Denmark; Clinical Institute of Research, University of Southern Denmark; Agnes and Knut Mørk Foundation; Health Foundation (Helsefonden) [grant 16-B-0271]. The Danish Aging Research Center is supported by a grant from the Velux Foundation.
Conflict of interest: None declared.
Supplementary Material
References
- 1. Christensen K, Doblhammer G, Rau R, Vaupel JW.. Ageing populations: the challenges ahead. Lancet 2009;374:1196–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vaupel JW, Carey JR, Christensen K. et al. Biodemographic trajectories of longevity. Science 1998;280:855–60. [DOI] [PubMed] [Google Scholar]
- 3. Kannisto V. Development of Oldest-old Mortality, 1950-1990: Evidence From 28 Developed Countries. Monograph. Odense, Denmark: Odense University Press, 1994. [Google Scholar]
- 4. Gruenberg EM. The failures of success, 1977. Milbank Q, 2005;83:779–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Christensen K, Thinggaard M, Oksuzyan A. et al. Physical and cognitive functioning of people older than 90 years: a comparison of two Danish cohorts born 10 years apart. Lancet 2013;382:1507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Parker M, Schon P, Lagergren M, Thorslund M.. Functional ability in the elderly Swedish population from 1980 to 2005. Eur J Ageing 2008;5:299–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Martin LG, Schoeni RF, Andreski PM, Jagger C.. Trends and inequalities in late-life health and functioning in England. J Epidemiol Community Health 2012;66:874–80. [DOI] [PubMed] [Google Scholar]
- 8. Murabito JM, Pencina MJ, Zhu L, Kelly-Hayes M, Shrader P, D’Agostino RB.. Temporal trends in self-reported functional limitations and physical disability among the community-dwelling elderly population: The Framingham Heart Study. Am J Public Health 2008;98:1256–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pedersen CB, Gøtzsche H, Møller JØ, Mortensen PB.. The Danish civil registration system. Dan Med Bull 2006;53:441–49. [PubMed] [Google Scholar]
- 10. Andersen-Ranberg K, Christensen K, Jeune B, Skytthe A, Vasegaard L, Vaupel JW.. Declining physical abilities with age: a cross-sectional study of older twins and centenarians in Denmark. Age Ageing 1999;28:373–77. [DOI] [PubMed] [Google Scholar]
- 11. Andersen-Ranberg K, Schroll M, Jeune B.. Healthy centenarians do not exist, but autonomous centenarians do: A population-based study of morbidity among Danish centenarians. J Am Geriatr Soc 2001;49(7):900–08. [DOI] [PubMed] [Google Scholar]
- 12. Christensen K, McGue M, Petersen I, Jeune B, Vaupel JW.. Exceptional longevity does not result in excessive levels of disability. Proc Natl Acad Sci U S A 2008;105:13274–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nybo H, Gaist D, Jeune B. et al. The Danish 1905 cohort: a genetic-epidemiological nationwide survey. J Aging Health 2001;13:32–46. [DOI] [PubMed] [Google Scholar]
- 14. Vestergaard S, Andersen-Ranberg K, Skytthe A, Christensen K, Robine JM, Jeune B.. Health and function assessments in two adjacent Danish birth cohorts of centenarians: Impact of design and methodology. Eur J Ageing 2016;13:15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lynge E, Sandegaard JL, Rebolj M.. The Danish National Patient Register. Scand J Public Health 2011;39(Suppl 7):30–33. [DOI] [PubMed] [Google Scholar]
- 16. Gjerstorff ML. The Danish Cancer Registry. Scand J Public Health 2011;39(Suppl 7):42–45. [DOI] [PubMed] [Google Scholar]
- 17. Helweg-Larsen K. The Danish Register of Causes of Death. Scand J Public Health 2011;39(Suppl 7):26–29. [DOI] [PubMed] [Google Scholar]
- 18. Avlund K, Schultz-Larsen K, Kreiner S.. The measurement of instrumental ADL: content validity and construct validity. Aging (Milano) 1993;5:371–83. [DOI] [PubMed] [Google Scholar]
- 19. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW.. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963;185:914–19. [DOI] [PubMed] [Google Scholar]
- 20. Folstein MF, Folstein SE, McHugh PR.. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- 21. McGue M, Christensen K.. The heritability of level and rate-of-change in cognitive functioning in Danish twins aged 70 years and older. Exp Aging Res 2002;28:435–51. [DOI] [PubMed] [Google Scholar]
- 22. McGue M, Christensen K.. Genetic and environmental contributions to depression symptomatology: evidence from Danish twins 75 years of age and older. J Abnorm Psychol 1997;106:439–48. [DOI] [PubMed] [Google Scholar]
- 23. Roth M, Tym E, Mountjoy CQ. et al. CAMDEX. A standardised instrument for the diagnosis of mental disorder in the elderly with special reference to the early detection of dementia. Br J Psychiatry 1986;149:698–709. [DOI] [PubMed] [Google Scholar]
- 24. Lawton MP, Brody EM.. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–86. [PubMed] [Google Scholar]
- 25. Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL.. A new clinical scale for the staging of dementia. Br J Psychiatry 1982;140:566–72. [DOI] [PubMed] [Google Scholar]
- 26. Andersen-Ranberg K, Jeune B, Hoier-Madsen M, Hegedus L.. Thyroid function, morphology and prevalence of thyroid disease in a population-based study of Danish centenarians. J Am Geriatr Soc 1999;47:1238–43. [DOI] [PubMed] [Google Scholar]
- 27. Andersen-Ranberg K, Vasegaard L, Jeune B.. Dementia is not inevitable: A population-based study of Danish centenarians. J Gerontol B Psychol Sci Soc Sci 2001;56:P152–59. [DOI] [PubMed] [Google Scholar]
- 28. Nybo H, Gaist D, Jeune B, McGue M, Vaupel JW, Christensen K.. Functional status and self-rated health in 2,262 nonagenarians: the Danish 1905 Cohort Survey. J Am Geriatr Soc 2001;49:601–09. [DOI] [PubMed] [Google Scholar]
- 29. Nybo H, Petersen HC, Gaist D. et al. Predictors of mortality in 2,249 nonagenarians - the Danish 1905-Cohort Survey. J Am Geriatr Soc 2003;51:1365–73. [DOI] [PubMed] [Google Scholar]
- 30. Thinggaard M, Mcgue M, Jeune B, Osler M, Vaupel JW, Christensen K.. Survival prognosis in very old adults. J Am Geriatr Soc 2016;64:81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Thinggaard M, Jacobsen R, Jeune B, Martinussen T, Christensen K.. Is the relationship between BMI and mortality increasingly U-shaped with advancing age? A 10-year follow-up of persons aged 70-95 years. J Gerontol A Biol Sci Med Sci 2010;65:526–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Engberg H, Jeune B, Andersen-Ranberg K, Martinussen T, Vaupel JW, Christensen K.. Optimism and survival: does an optimistic outlook predict better survival at advanced ages? A twelve-year follow-up of Danish nonagenarians. Aging Clin Exp Res 2013;25:517–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hjelmborg JV, Iachine I, Skytthe A. et al. Genetic influence on human lifespan and longevity. Hum Genet 2006;119:312–21. [DOI] [PubMed] [Google Scholar]
- 34. Gerdes LU, Jeune B, Ranberg KA, Nybo H, Vaupel JW.. Estimation of apolipoprotein E genotype-specific relative mortality risks from the distribution of genotypes in centenarians and middle-aged men: apolipoprotein E gene is a ‘frailty gene’, not a ‘longevity gene’. Genet Epidemiol 2000;19:202–10. [DOI] [PubMed] [Google Scholar]
- 35. Nygaard M, Lindahl-Jacobsen R, Soerensen M. et al. Birth cohort differences in the prevalence of longevity-associated variants in APOE and FOXO3A in Danish long-lived individuals. Exp Gerontol 2014;57:41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Engberg H, Oksuzyan A, Jeune B, Vaupel JW, Christensen K.. Centenarians - a useful model for healthy aging? A 29-year follow-up of hospitalizations among 40,000 Danes born in 1905. Aging Cell 2009;8:270–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Andersen-Ranberg K, Fjederholt KT, Madzak A, Nybo M, Jeune B.. Cardiovascular diseases are largely underreported in Danish centenarians. Age Ageing 2013;42:249–53. [DOI] [PubMed] [Google Scholar]
- 38. Collerton J, Davies K, Jagger C. et al. Health and disease in 85 year olds: baseline findings from the Newcastle 85+ cohort study. BMJ 2009;339:b4904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Riedel-Heller SG, Schork A, Matschinger H, Angermeyer MC.. Recruitment procedures and their impact on the prevalence of dementia. Results from the Leipzig Longitudinal Study of the Aged (LEILA75+). Neuroepidemiology 2000;19:130–40. [DOI] [PubMed] [Google Scholar]
- 40. Deelen J, Beekman M, Uh HW. et al. Genome-wide association meta-analysis of human longevity identifies a novel locus conferring survival beyond 90 years of age. Hum Mol Genet 2014;23:4420–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Robine JM, Cheung SL, Saito Y, Jeune B, Parker MG, Herrmann FR. Centenarians today: new insights on selection from the 5-COOP Study. Curr Gerontol Geriatr Res 2010;2010:120354. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.