Abstract
Background: Children placed in out-of-home care (OHC) have exceedingly high rates of health problems. Their poor health tends to persist across adolescence and into young adulthood, resulting in increased risks of mortality. Yet, very little is known about this group’s mortality risks later in life. The aim of this study was to investigate whether OHC was associated with the risk of all-cause mortality across adulthood, and whether these risks varied across different placement characteristics. Moreover, the study addressed potential confounding by including two comparison groups with children who grew up under similarly adverse living conditions but did not experience placement.
Methods: Data were derived from a 60-year follow-up of a Stockholm cohort born in 1953 (n = 15 048), of whom around 9% have had experiences of OHC. The associations between OHC and subsequent all-cause mortality were analysed by means of Cox’s proportional hazards regression models.
Results: Individuals who were placed in OHC at any point during their formative years had increased mortality risks across ages 20 to 56 years. Elevated risk of mortality was particularly pronounced among those who were placed in adolescence and/or because of their own behaviours. Children who were exposed to OHC had increased risks of mortality also when compared with those who grew up under similar living conditions but did not experience placement.
Conclusions: Children in OHC constitute a high-risk group for subsequent mortality. In order to narrow the mortality gap, interventions may need to monitor not only health aspects but also to target the cognitive and social development of these children.
Keywords: Cohort studies, foster home care, longitudinal studies, mortality
Introduction
Out-of-home care (OHC) is a social intervention where a child is temporarily or permanently removed from the parents due to an adverse family situation or own antisocial behaviour, and placed in family-based foster care or residential care. From society’s point of view, the intention is to provide the child with significantly improved opportunities for growing and learning in those cases where the family of origin has failed.1 OHC thus has the potential to ameliorate the child’s opportunities and outcomes. Yet, empirical studies of children in OHC paint a dismal picture of their health situation.2,3 Children in OHC have been found to have higher levels of emotional, psychological and behavioural problems, such as poor well-being, conduct disorder, attention disorder, aggressiveness, depression and psychopathology.4,5 These health problems seem to persist into young adulthood: for example, this group consumes more psychotropic drugs6 and has higher rates of substance abuse7 as well as all-cause and cause-specific (e.g. suicide, accidents and violence) mortality.8–12 Only a few studies have examined health-related outcomes beyond young adulthood and into early midlife. The results from these studies indicate higher risks of depression and low self-efficacy,13 chronic health problems such as asthma, diabetes, hypertension, stroke, heart disease, cancer and epilepsy,14 and receipt of disability pension.15 Due to the lack of large-scale prospective data, however, we know very little about whether the exposure to OHC in childhood translates into poor health outcomes, as indicated through increased mortality, throughout the entire span of adulthood.
Based on a cohort of more than 15 000 individuals born in Stockholm, Sweden in 1953, the aim of the current study was, first, to examine whether exposure to OHC in childhood (ages 0–19 years) is associated with the risk of subsequent all-cause mortality (ages 20–56). The second aim was to investigate whether mortality risks vary across different placement characteristics, including age at first placement (early childhood, middle childhood or adolescence), reason for placement (family-related circumstances and/or own behaviours) and type of placement (family foster care and/or residential care). Third, the study sought to improve causal inference in two ways: by considering various characteristics of the family of origin (parental occupational class, maternal age and parental marital status), and by including two comparison groups consisting of other types of welfare recipients, where one group had experience of social assistance but not placement and the other was investigated by the child welfare committee but did not experience placement.
Methods
Data material
The data material used was the Stockholm Birth Cohort Study (SBC), comprising all children born in 1953 who were living in the greater Stockholm metropolitan area in 1963 (n = 15 117).16 The SBC currently covers various kinds of register- and survey-based data of the cohort members and their families between 1953 and 2009. Ethical permission for the SBC has been obtained from the Stockholm Regional Ethics Committee (no. 739-03-629).
Variables
Independent variables (1953–72)
Information about placement in OHC was based on the decisions made by the Child Welfare Committee, as recorded in the Social Register. It covers the period between 1953 and 1972 (from birth until the respondent turns 19). As a first step, a variable indicating placement in OHC was created with the options: ‘No OHC’ and ‘OHC’. Three types of placement characteristics were further explored: age at first placement, reason for placement and type of placement. Regarding age at first placement, the data had originally been categorized into three periods: ‘Early childhood’ (ages 0–6), ‘Middle childhood’ (ages 7–12), and ‘Adolescence’ (ages 13–19). Reasons for placement were categorized into: ‘Family-related circumstances’, ‘Own behaviours’ and ‘Both’, whereas type of placement was coded as: ‘Family foster care’, ‘Residential care’ and ‘Both’. The category called ‘Both’ was used in those cases where the individual had multiple placements and where the reason/type of placement varied between the occasions.
Dependent variable (1973–2009)
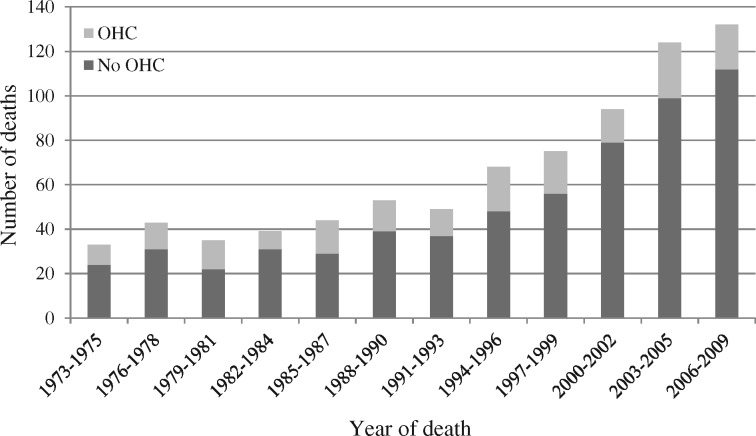
Data on mortality were retrieved from the Causes of Death Register and included the main diagnosis as well as the year of death. In the present study, the mortality follow-up period started on the 1 January 1973 and, due to data availability, ended on the 28 February 2009 (ages 20–56). The most common causes of death were cancer (e.g. cancer of lung or breast), disorders related to alcohol and drug use (e.g. drug dependence, alcoholic liver disease, alcohol poisoning), circulatory diseases (e.g. ischaemic heart disease), injuries (e.g. skull fractures and open wounds) and suicide. Since the cause-specific rates were too low to enable an examination of specific groups of diagnosis, the current study used all-cause mortality as the outcome. See Figure 1 for the distribution of deaths across the follow-up period.
Figure 1.
The frequency distribution of deaths between 1973 and 2009 (n = 15, 048).
Confounders at birth (1953)
Three types of confounding variables at birth were included: parental occupational class, maternal age and parental marital status. Parental occupational class was based on information about the occupation of the head of the household (usually the husband), commonly provided by the mother at the time of delivery. It is therefore reasonable to believe that this information concerns the biological father also for children who were placed in OHC at very early age. Six categories were created: ‘Upper and upper-middle class’, ‘Lower middle class, officials’, ‘Lower middle class, self-employed’, ‘Working class, skilled’, ‘Working class, non-skilled’ and ‘Unclassified’ (e.g. housewives, students, pensioners, unemployed). In order to distinguish between relatively young mothers and relatively old mothers at the time of the cohort member’s birth, information about maternal age was collapsed into: ‘Age 19 or younger’, ‘Ages 20–39’, ‘Age 40 or older’ and ‘No information’. It should be noted that alternative categorizations or keeping the measure continuous did not alter the main results. Concerning parental marital status, the category of ‘Married’ included those cases where the biological parents were married at the time of birth of the child, whereas the category of ‘Unmarried’ concerned all other cases (e.g. non-married biological parents, single mothers).
Other types of welfare recipiency (1953–72)
Two comparison groups were included. For the first one, information on receipt of social assistance was used, derived from the Social Register. A variable with three categories was created: ‘No social assistance or OHC’, ‘Social assistance but no OHC’, and ‘OHC’. Receipt of social assistance could have taken place at any point between 1953 and 1972. The second comparison group was based on information about decisions from the Child Welfare Committee (CWC) that had not resulted in placement in OHC. Instead, the committee could recommend, for example, assistance, admonition or supervision – or ad acta (no measures taken). A variable with the following categories was subsequently constructed: ‘No investigation by the CWC’, ‘Investigation but no OHC’ and ‘OHC’.
Statistical analysis
The associations between OHC and subsequent all-cause mortality were analysed by means of Cox’s proportional hazards regression models, producing hazard ratios (HR). Subjects entered the study on 1 January 1973 and were censored in the event of death or at the end of follow-up (28 February 2009). Rates of migration and imprisonment were low and were therefore not included as censored events. Since only information about year of death was available, the month and day were set at the 15 June in the appropriate year. The issue of tied failure times was handled by controlling the results through the exactm-command in Stata; an exact marginal-likelihood method that is appropriate when tied failures are numerous. Of the 15 117 cohort members, 69 had died before 1973 and were thus excluded from the analysis, rendering a study sample of 15 048 individuals. Two sets of analyses were performed: the first concerned the associations between the different OHC placement characteristics and all-cause mortality, whereas the second focused on comparing children in OHC and the two other types of welfare recipients with regard to subsequent all-cause mortality. In both instances, each independent variable was examined separately in two models: Model 1 adjusted only for gender, and Model 2 also included the confounders at birth (parental occupational class, maternal age and parental marital status). Gender-separate analyses were performed at an initial stage but, since no interaction effects between gender and the independent variables were found, the decision was made to analyse males and females in joint models.
Results
The descriptive statistics for the study variables are shown in Table 1. Approximately 5.2% of the cohort had died between 1973 and 2009. Regarding placement in OHC, 9.3% were placed at some point between birth and age 19. A majority of them experienced their first placement in early childhood. The most common reason for placement was family-related circumstances and the most common type of placement was residential care. Concerning the confounding variables measured at birth, a vast majority of the parents belonged to the working class (skilled or non-skilled), followed by officials from the lower middle class. Although most mothers were between age 20 and 39 when giving birth to the cohort member, 3.2% experienced teenage motherhood. Moreover, approximately 12.7% of the biological parents were not married at the time of the birth of the cohort member. With regard to the other types of welfare recipiency, 14.9% were found to have received social assistance but had not been exposed to OHC, whereas 12.4% had been investigated by the CWC but had not been placed in OHC.
Table 1.
Descriptive statistics for the study variables (n = 15048)
| n | % | % deaths | % OHC | |
|---|---|---|---|---|
| Outcome (1973-2009) | ||||
| All-cause mortality | ||||
| No | 14259 | 94.8 | – | 8.5 |
| Yes | 789 | 5.2 | – | 23.1 |
| Placement characteristics (1953-72) | ||||
| Placement in OHC | ||||
| No | 13648 | 90.7 | 4.5 | – |
| Yes | 1400 | 9.3 | 13.0 | – |
| Age at first placement | ||||
| No OHC | 13648 | 90.7 | 4.5 | – |
| Early childhood | 873 | 5.8 | 8.7 | – |
| Middle childhood | 176 | 1.2 | 15.3 | – |
| Adolescence | 351 | 2.3 | 22.5 | – |
| Reason for placement | ||||
| No OHC | 13648 | 90.7 | 4.5 | – |
| Family-related circumstances | 913 | 6.1 | 7.6 | – |
| Own behaviours | 341 | 2.3 | 25.2 | – |
| Both | 146 | 1.0 | 18.5 | – |
| Type of placement | ||||
| No OHC | 13648 | 90.7 | 4.5 | – |
| Family foster home | 304 | 2.0 | 13.5 | – |
| Residental care | 733 | 4.9 | 10.1 | – |
| Both | 363 | 2.4 | 18.5 | – |
| Confounders at birth (1953) | ||||
| Parental occupational class | ||||
| Upper and upper middle class | 2004 | 13.3 | 4.2 | 2.3 |
| Lower middle class, officials | 4638 | 30.8 | 5.1 | 6.9 |
| Lower middle class, self-employed | 922 | 6.1 | 4.2 | 9.6 |
| Working class, skilled | 4108 | 27.3 | 5.8 | 11.6 |
| Working class, non-skilled | 2800 | 18.6 | 5.8 | 14.3 |
| Unclassified | 576 | 3.8 | 4.9 | 11.9 |
| Maternal age | ||||
| Age 19 or younger | 487 | 3.2 | 8.6 | 25.7 |
| Ages 20-39 | 11397 | 75.7 | 5.4 | 9.4 |
| Age 40 or older | 529 | 3.5 | 4.0 | 10.0 |
| No information | 2635 | 17.5 | 4.4 | 6.0 |
| Parental marital status | ||||
| Married | 13134 | 87.3 | 5.1 | 7.4 |
| Unmarried | 1914 | 12.7 | 6.4 | 22.4 |
| Other types of welfare recipiency (1953-72) | ||||
| Social assistance | ||||
| No social assistance or OHC | 11404 | 75.8 | 4.1 | 0.0 |
| Social assistance but no OHC | 2244 | 14.9 | 6.2 | 0.0 |
| OHC | 1400 | 9.3 | 13.0 | 100.0 |
| Child welfare | ||||
| No investigation by the CWC | 11789 | 78.3 | 3.7 | 0.0 |
| Investigation but no OHC | 1859 | 12.4 | 9.2 | 0.0 |
| OHC | 1400 | 9.3 | 13.0 | 100.0 |
Table 2 reports on the associations between different OHC placement characteristics—each analysed separately—and subsequent all-cause mortality. According to Model 1, which is adjusted only for gender, individuals who have experience of OHC at any point between 1953 and 1972 (ages 0–19) have nearly a 3-fold increased mortality risk [hazard ratio (HR) = 2.99; 95% confidence interval (CI) = 2.53-3.53]. Regarding age at first placement, excessive risks of all-cause mortality are found across all periods, with the highest risks for those placed in adolescence (HR = 5.48; 95% CI = 4.33-6.94). Being placed because of own behaviours is associated with considerably higher mortality risks (HR = 6.12; 95% CI = 4.88-7.68) compared with those placed due to family-related circumstances (HR = 1.71; 95% CI = 1.33-2.19). This is also the case for those who have been placed for both reasons (HR = 4.29; 95% CI = 2.91-6.30)—most likely due to the occurrence of repeated placements in this group. Concerning type of placement, those who were placed in family foster homes and in residential care show increased risks of mortality, particularly for the former type (HR = 3.19; 95% CI = 2.32-4.38 and HR = 2.25; 95% CI = 1.77-2.87, respectively). A comparable higher HR is however found among individuals who experienced both type of placement (HR = 4.41; 95% CI = 3.42-5.67). Again, this is probably reflecting their higher frequency of placement (or placement instability). Model 2 shows the associations adjusted for gender and the confounders at birth (parental occupational class, maternal age, and parental marital status). Although the HRs overall are slightly attenuated, the patterns remain the same.
Table 2.
The associations between different OHC placement characteristics (1953-72) and subsequent all-cause mortality (1973-2009). Results from Cox regression analysis, presented as HRs with 95% confidence intervals (n = 15048)
| All-cause mortality (1973-2009) |
||
|---|---|---|
| Placement characteristics (1953-72) | Model 1a | Model 2b |
| HR (95% CI) | HR (95% CI) | |
| Placement in OHC | ||
| No OHC (ref.) | 1.00 | 1.00 |
| OHC | 2.99 (2.53-3.53) | 2.85 (2.39-3.39) |
| Age at first placement | ||
| No OHC (ref.) | 1.00 | 1.00 |
| Early childhood | 1.96 (1.54-2.49) | 1.81 (1.42-2.32) |
| Middle childhood | 3.55 (2.41-5.22) | 3.48 (2.36-5.14) |
| Adolescence | 5.48 (4.33-6.94) | 5.25 (4.13-6.67) |
| Reason for placement | ||
| No OHC (ref.) | 1.00 | 1.00 |
| Family circumstances | 1.71 (1.33-2.19) | 1.60 (1.24-2.07) |
| Own behaviours | 6.12 (4.88-7.68) | 5.88 (2.67-7.40) |
| Both | 4.29 (2.91-6.30) | 3.93 (2.66-5.82) |
| Type of placement | ||
| No OHC (ref.) | 1.00 | 1.00 |
| Family foster home | 3.19 (2.32-4.38) | 3.09 (2.24-4.27) |
| Residental care | 2.25 (1.77-2.87) | 2.18 (1.70-2.78) |
| Both | 4.41 (3.42-5.67) | 4.14 (3.18-5.38) |
Each independent variable analysed separately. Adjusted for gender.
Each independent variable analysed separately. Adjusted for gender and confounders at birth (parental occupational class, maternal age, parental marital status).
In Table 3, the comparisons between children placed in OHC and the other two types of welfare recipients are shown. According to Model 1, individuals who were placed in OHC, in comparison with those who grew up in a family that received social assistance but did not experience OHC, have more than a 2-fold risk of all-cause mortality (HR = 2.14; 95% CI = 1.71-2.66). Smaller, but still robust, relative differences are seen for those placed in OHC as compared with the group of individuals who were investigated by the CWC but were not placed (HR = 1.62; 95% CI = 1.31-2.00). The inclusion of the confounders at birth in Model 2 does not alter these overall conclusions.
Table 3.
Comparing children in OHC and other welfare recipients (1953-72) with regard to subsequent all-cause mortality (1973-2009). Results from Cox regression analysis, presented as HRs with 95% confidence intervals (n = 15048)
| All-cause mortality (1973-2009) |
||
|---|---|---|
| Other types of welfare recipiency (1953-72) | Model 1a | Model 2b |
| HR (95% CI) | HR (95% CI) | |
| Social assistance | ||
| No social assistance or OHC | 0.66 (0.54-0.80) | 0.67 (0.55-0.82) |
| Social assistance but no OHC | 1.00 | 1.00 |
| OHC | 2.14 (1.71-2.66) | 2.11 (1.69-2.64) |
| Child welfare | ||
| No investigation by the CWC | 0.46 (0.38-0.55) | 0.46 (0.38-0.55) |
| Investigation but no OHC | 1.00 | 1.00 |
| OHC | 1.62 (1.31-2.00) | 1.59 (1.29-1.97) |
Each independent variable analysed separately. Adjusted for gender.
Each independent variable analysed separately. Adjusted for gender and confounders at birth (parental occupational class, maternal age, parental marital status).
Discussion
The aim of this study was to examine whether exposure to OHC in childhood (ages 0–19) was associated with the risk of all-cause mortality across adulthood (ages 20–56). The results suggest that individuals who were placed in OHC at any point during their formative years have increased mortality risks across ages 20 to 56. This result points in the same direction as studies regarding the mortality risk in young adulthood of former OHC clients.9,10 The fact that the current study did not find any gender differences in the associations between OHC and all-cause mortality stands in contrast to previous studies, which frequently have demonstrated stronger associations among males compared with females.1,9 This discrepancy might be due to mortality in younger ages to a higher extent being represented by external causes such as suicide or substance abuse—causes which are more common among males.1,6,9,11
Whereas the higher mortality risks compared with the majority population were found regardless of age at first placement, reason for placement or type of placement, it can be noted that the elevated risks of mortality were particularly pronounced among those who were placed in adolescence. Other studies have also found that children who enter OHC during adolescence constitute a high-risk group of adverse outcomes later in life.17–19 It should be noted that adolescent placement was over-represented by those who had behaviour problems (data not presented), which may indicate that the elevated mortality risks may to some extent reflect a selection effect. However, there are also reasons to believe that adolescence is a sensitive period. First, adolescence is a transitional phase of life when individuals undergo great psychological and biological changes.20 The adverse effect of being placed outside the home may thus be magnified. For example, adolescents have to leave their familiar environment and to establish new relationship with foster parents or caregivers.8 Separation from the family of origin combined with insecure attachment in the new placement can largely increase adolescents’ vulnerability and further lead to suicidal ideation or self-harming behaviours.21 Second, a number of studies have demonstrated that individuals who entered OHC during adolescence had greater risks of facing a disadvantaged life situation in young adulthood, such as low educational attainment or young parenthood.22–24 These factors are in themselves associated with poor mental or physical health,14,15 which in turn increases the risk of mortality.
Consistent with earlier studies,17 mortality risks were also higher among individuals who were placed in OHC because of their own behaviour compared with those placed due to family-related circumstances. This is expected, since some of the specific causes behind these placements due to own behavior were mental health problems as well as alcohol and illicit drug use. The current study found, moreover, that individuals placed in family foster care had slightly elevated risks of mortality compared with those who were placed in residential care. This finding differs from a previous study,17 something which could be explained by that study’s focus on adolescent placements only and, additionally, that a recent study sample was used. In the 1953 Stockholm birth cohort investigated in the current study, it was much more common to place young children in residential care. Also, the composition of residential care clients is different in recent cohorts, with adolescents and refugee children being over-represented. It should be noted that individuals who were exposed to both types of reason for placement and both types of placement had particularly elevated mortality risks. This result may reflect that exposure to multiple placements or placement instability is related to even worse outcomes, a conclusion that is supported by past research.25–27
The observational design of the current study cannot fully answer whether the increased mortality risks among children who experienced placement in OHC are caused by the exposure itself or whether OHC is simply a risk marker for adverse living conditions and other types of health-damaging exposures during childhood. It should however be highlighted that the associations between exposure to OHC and subsequent all-cause mortality were not explained by parental occupational class, maternal age or parental marital status at the birth of the child. Still, there is potential for residual confounding: had data been available, it would have been preferable to also incorporate other indicators of early socioeconomic conditions.
In order to improve the potential for causal inference, the current study moreover brought two other types of welfare recipients into the analyses as comparison groups: individuals who experienced social assistance recipiency during upbringing but were not placed, and individuals who were investigated by the child welfare committee but remained in their families. It is reasonable to assume that these children in many ways were similar to those placed in OHC. The results suggested, however, that individuals who were exposed to OHC still had considerably higher risks of subsequent all-cause mortality than these two comparison groups.
Strengths and limitations
This is the first prospective study that has been able to examine mortality risks in the OHC population across adulthood (ages 20–56). Thanks to the high-quality, full-coverage administrative registers kept in Sweden, there was very little attrition and loss to follow-up. Another strength is the detailed information about placement in OHC, which rendered it possible to investigate how the associations between placement in OHC and mortality varied according to age at first placement, reason for placement and type of placement. The rich data material also enabled the inclusion of several important confounders at birth as well as two credible comparison groups which grew up under the similar conditions but did not experience OHC.
Some limitations should however be highlighted. First of all, whereas the attrition rates were overall low, a substantial proportion of individuals (17.5%) lacked information about maternal age. The inclusion of these individuals as a separate category in the analysis is not optimal. but it should be noted that their removal (i.e. limiting the analysis to complete cases only) did not alter the main results in any substantial way (see online supplement A, available as Supplementary data at IJE online).
Moreover, the data did not state the exact age at placement or specific reasons for placement, and nothing has been recorded regarding the living conditions of the child while in OHC, for example related to characteristics of the foster family or residential care unit. Regarding mortality, the follow-up period was lengthy and, when assessing the proportional hazard assumption using Shoenfeld residuals, the results indicated some problems. This could be due to the relatively large sample size, and we investigated this issue further by stratifying the mortality follow-up into four periods of approximately equal length. The results (see online supplement B, available as Supplementary data at IJE online) indicate that the size of the hazard ratios decrease across the four periods, but that the differences between children placed and not placed in OHC remain robust.
Finally, although the mortality follow-up was lengthy, it was still truncated at a relatively early age. Causes of death before the age of 60 are to a higher extent represented by mental and behavioural disorders as well as external causes, compared with deaths occurring at later stages of life. Although the number of deaths was not sufficient to examine cause-specific mortality, additional analyses (see online supplement C, available as Supplementary data at IJE online) separated between ‘unnatural’ (i.e. external causes such as suicide and accidents) and ‘natural’ causes of death. These show that there are robust associations between OHC and mortality regardless of whether unnatural or natural causes are targeted, although the relative size of the estimates to some extent varies across placement characteristics and outcomes. The same conclusion is drawn when children in OHC are compared with other welfare recipients (see online supplement D, available as Supplementary data at IJE online).
Implications for policy and practice
There was no national placement policy in Sweden in the 1950s and 1960s, which resulted in an extremely heterogeneous child welfare system. Generally however, Swedish authorities believed strongly in the preventive abilities of the child welfare work. The cohort members thus grew up in an environment where child welfare services were an important and invasive tool for the advanced social engineering ambitions of the Swedish welfare state.29,30 This is also reflected in the high prevalence of placement in the SBC. Although the issue of causality could not be fully addressed in the current study, the findings suggest that OHC did not exert the expected function, that is to improve the life chances of a vulnerable group of children. It can be speculated that the lack of preventive health care may partly account for the excessive mortality risks. Previous studies have consistently shown that children in OHC are a high-risk group for unmet health needs and medical treatment, as well as inadequate health screening and monitoring.1,28A way to narrow the mortality gap would hence be for health services to direct their efforts toward these children, particularly for those who enter OHC in adolescence and/or because of own problem behaviours. Apart from preventions and interventions directly related to health, the social and cognitive development of children placed in OHC should be highlighted. Some recent studies have suggested that appropriate educational interventions during the care period could improve children’s cognitive abilities and school performance, which could in turn help them with the transition out of care and into young adulthood.31,32 To empirically investigate these pathways as potential mediators—or moderating factors—for the association between OHC and adult all-cause mortality is an important task for future studies.
Supplementary Data
Supplementary data are available at IJE online.
Supplementary Material
Acknowledgement
The creation and maintenance of the Stockholm Birth Cohort study is a collaboration between Centre for Health Equity Studies (CHESS) and Swedish Institute for Social Research (SOFI).
Funding
This work was supported by the Swedish Research Council for Health, Working Life and Welfare [2012-0201].
Conflict of interest: None declared.
Key Messages
Exposure to out-of-home care (OHC) in childhood is associated with a 3-fold risk of adult all-cause mortality.
Particularly pronounced mortality risks are found among children placed in adolescence and/or because of own problem behaviours.
Children in OHC have increased mortality risks also when compared with children who grew up under similarly adverse living conditions without experiencing placement.
References
- 1. Fernandez E, Barth RP. How Does Foster Care Work? International Evidence on Outcomes. London: Jessica Kingsley Publishers, 2011. [Google Scholar]
- 2. McCann JB, James A, Wilson S, Dunn G.. Prevalence of psychiatric disorders in young people in the care system. BMJ 1996;313:1529–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McMillen JC, Zima TB, Scott DL. et al. Prevalence of psychiatric disorders among older youths in the foster care system. J Am Acad Sci Child Adolesc Psychiatry 2005;44:88–95. [DOI] [PubMed] [Google Scholar]
- 4. Berlin M, Vinnerljung B, Hjern A.. School performance in primary school and psychosocial problems in young adulthood among care leavers from long term foster care. Child Youth Serv Rev 2011;33:2489–97. [Google Scholar]
- 5. Leslie LK, Landsverk J, Ezzet-Lofstrom R, Tschann JM, Slymen DJ, Garland AF.. Children in foster care: Factors influencing outpatient mental health service use. Child Abuse Negl 2000; 24:465–76. [DOI] [PubMed] [Google Scholar]
- 6. Vinnerljung B,, Hjern A.. Consumption of psychotropic drugs among adults who were in societal care during their childhood. Nord J Psychiatry 2014;68:611–19. [DOI] [PubMed] [Google Scholar]
- 7. von Borczyskowski A, Vinnerljung B, Hjern A.. Alcohol and drug abuse among young adults who grew up in substitute care: Findings from a Swedish national cohort study. Child Youth Serv Rev 2013;35:1954–61. [Google Scholar]
- 8. Hjern A,, Vinnerljung B,, Lindblad F.. Avoidable mortality among child welfare recipients and intercountry adoptees: A national cohort study. Jf Epidemiol Community Health 2004;58:412–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vinnerljung B,, Ribe M.. Mortality after care among young adult foster children in Sweden. Int J Soc Welfare 2001;10:164–73. [Google Scholar]
- 10. Kalland M, Pensola TH, Meriläinen J, Sinkkonen J.. Mortality in children registered in the Finnish child welfare registry: population based study. BMJ 2001;323:207–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Barth RP, Blackwell DL.. Death rates among California's foster care and former foster care populations. Child Youth Serv Rev 1998;20:577–604. [Google Scholar]
- 12. Christoffersen MN. Risikofaktorer i barndommen. [In English: Risk factors in childhood]. København: Socialforskningsinstitutet,1999. [Google Scholar]
- 13. Dregan A, Gulliford M.. Foster care, residential care and public care placement patterns are associated with adult life trajectories: population-based cohort study. Soc Psychiatry Psychiatr Epidemiol 2012;47:1517–26. [DOI] [PubMed] [Google Scholar]
- 14. Zlotnick C, Tam TW, Soman LA.. Life course outcomes on mental and physical health: the impact of foster care on adulthood. Am J Public Health 2012;102:534–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vinnerljung B,, Brännström L,, Hjern A.. Disability pension among adult former child welfare clients: A Swedish national cohort study. Child Youth Serv Rev 2015;56:169–76. [Google Scholar]
- 16. Stenberg S-Å, Vågerö D.. Cohort profile: The Stockholm birth cohort of 1953. Int J Epidemiol 2006;35:546–48. [DOI] [PubMed] [Google Scholar]
- 17. Vinnerljung B,, Sallnäs M.. Into adulthood: a follow‐up study of 718 young people who were placed in out‐of‐home care during their teens. Child Fam Soc Work 2008;13:144–55. [Google Scholar]
- 18. Collins ME, Schwartz IM, Epstien I.. Risk factors for adult imprisonment in a sample of youth released from residential child care. Child Youth Serv Revren and Youth Services Review 2001; 23:203–26. [Google Scholar]
- 19. Helgeland IM. Ungdom med atferdsvansker:hvordan går det med dem som 30-åringer? En longitudinell studie. [In English: Adolescents with behavioural problems at age 30: A longitudinal study]. Oslo: Universitetet i Oslo, 2001. [Google Scholar]
- 20. Kazdin AE. Adolescent mental health: Prevention and treatment programs. Am Psychol 1993;48:127. [DOI] [PubMed] [Google Scholar]
- 21. Fergusson DM, Beautrais AL, Horwood LJ.. Vulnerability and resiliency to suicidal behaviours in young people. Psychol Med 2003;33:61–73. [DOI] [PubMed] [Google Scholar]
- 22. Viner RM,, Taylor B.. Adult health and social outcomes of children who have been in public care: population-based study. Pediatrics 2005;115:894–99. [DOI] [PubMed] [Google Scholar]
- 23. Vinnerljung B,, Öman M,, Gunnarson T.. Educational attainments of former child welfare clients: A Swedish national cohort study. Int J Soc Welfare 2005;14:265–76. [Google Scholar]
- 24. Warburton WP,, Warburton RN,, Sweetman A,, Hertzman C.. The impact of placing adolescent males into foster care on education, income assistance, and convictions. Can J Econ 2014;47:35–69. [Google Scholar]
- 25. Ford T,, Vostanis P,, Meltzer H,, Goodman R.. Psychiatric disorder among British children looked after by local authorities: comparison with children living in private households. Br J Psychiatry 2007;190:319–25. [DOI] [PubMed] [Google Scholar]
- 26. Rubin DM, Alessandrini EA, Feudtner C, Mandell DS, Localio AR, Hadley T.. Placement stability and mental health costs for children in foster care. Pediatrics 2004;113:1336–41. [DOI] [PubMed] [Google Scholar]
- 27. Rubin DM, O'Reilly AL, Luan X, Localio AR.. The impact of placement stability on behavioral well-being for children in foster care. Pediatrics 2007;119:336–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kling S, Vinnerljung B, Hjern A.. Somatic assessments of 120 Swedish children taken into care reveal large unmet health and dental care needs. Acta Paediatr 2016;105:416–20. [DOI] [PubMed] [Google Scholar]
- 29. Vinnerljung B. Fosterbarn som vuxna [Foster children as adults]. Lund, Sweden: Arkiv Förlag, 1996. [Google Scholar]
- 30. Hessle S, Vinnerljung B.. Child Welfare in Sweden:an Overview Stockholm: Department of Social Work, Stockholm University, 1999.
- 31. Forsman H,, Vinnerljung B.. Interventions aiming to improve school achievements of children in out-of-home care:A scoping review. Child Youth Serv Rev 2012;34:1084–91. [Google Scholar]
- 32. Harper J, Schmidt F.. Effectiveness of a group-based academic tutoring program for children in foster care: A randomized controlled trial. Child Youth Serv Rev 2016;67:238–46. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.