The original cohort
In a previous cohort profile we described the Doetinchem Cohort Study from round one starting in 1987–91 as a monitoring study, and its development into a cohort study with a second measurement in 1993–97 and a third in 1998–2002.1 The original sample was an age-sex-stratified sample of the population register of inhabitants of Doetinchem, with equal numbers of men and women and equal numbers in 10-year age categories: 20–29, 30–39, 40–49 and 50–59. In the first round the focus was on cardiovascular health, and this was broadened to other major chronic conditions in the second round. The Doetinchem Cohort Study is carried out by the Dutch National Institute for Public Health and the Environment.
What is the reason for the new data collection?
The study continued into a fourth round (2003–07) and a fifth round (2008–12), and now a sixth round (2013–17) is ongoing. From round four onwards we expanded the measurement protocol even further with research themes to serve current public health research questions on lifestyle, chronic diseases and ageing. The Doetinchem Cohort covers a large part of the life course from young adulthood to old age because the initial general population sample aged between 20 and 59 years has been followed for more than 25 years, and is currently between 46 and 85 years.
What will be the new areas of research?
First, with extension of the period of data collection, the cohort is increasingly used for research questions on changes over the life course and in particular while ageing. This refers to changes in lifestyle, biomarkers, health and disease and the relations between them. Second, the traditional risk factors for chronic conditions can now be studied in relation to new measures such as sleep, muscle strength, loneliness and depressive symptoms. Third, the availability of biomaterial in every round (including DNA) gives numerous research possibilities (including epigenetic analyses). Fourth, having such an infrastructure gives also the possibility to add side studies. Some of our participants participated in a study on 24-h urine collection for salt consumption,2 a pilot study for a new Food Frequency Questionnaire or a study on immunosenescence, which required extra blood collection.
Who is in the cohort?
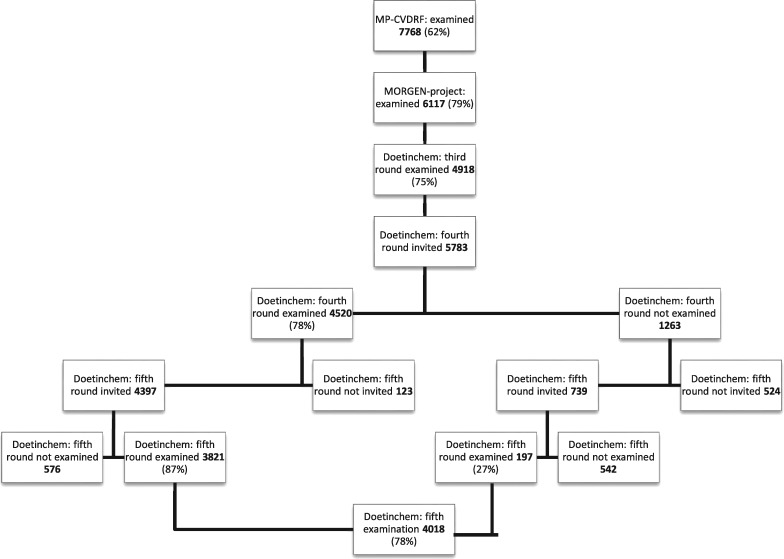
Table 1 presents the numbers invited and measured in the different rounds and Figure 1 presents a flow chart. In round 1 we examined 7768 participants, and in round 5 there were 4018 participants. The number of persistent participants, those participating in all five rounds, is 3456; those who dropped out after one or two rounds are considered to be the early dropouts (n = 2309). Those who skipped one or more rounds are the returners (n = 562), and the group of late dropouts consists of 1044 participants. Those groups differ somewhat in their socioeconomic, lifestyle and health characteristics (Table 2).
Table 1.
Overview of measurement rounds of the Doetinchem Cohort Studya
| Name | Monitoring Project on Cardiovascular Disease Risk Factors (MP-CVDRF) | Monitoring Project on Chronic Disease Risk Factors (MORGEN-Project) | Doetinchem cohort study, round 3 | Doetinchem cohort study, round 4 | Doetinchem cohort study, round 5 | Doetinchem cohort study, round 6 |
|---|---|---|---|---|---|---|
| Years | 1987–91 | 1993–97 | 1998–2002 | 2003–07 | 2008–12 | 2013–17 |
| Age range | 20–59 yrs | 26–65 years | 31–70 years | 36–75 years | 41–80 years | 46–86 years |
| Numbers participated | 12404b | 6117 | 4918 | 4520 | 4018 | About 3450 |
| Response | 62% | 79% | 75% | 78% | 78% | About 77% |
| Numbers invited | 20154 | 7768b | 6581 | 5783 | 5136 | About 4474 |
| Who were invited | Age- and sex-stratified random sample of population | A random two-thirds of those measured in round one | Those who were invited in round 2 excluding those who emigrated, actively withdrew from the study or died | Those who were invited in round 3 excluding those who emigrated, actively withdrew from the study or died | Those who were invited in round 4 excluding those who emigrated, actively withdrew from the study or died | Those who were invited in round 5 excluding those who emigrated, actively withdrew from the study or died |
aIn the year 1992, no measurements were carried out: in this year preparation for the next measurement (protocol development) was carried out.
bOf those participating in round 1, a sample was drawn for round 2.
Figure 1.
Flow chart of the Doetinchem Cohort Study.
Table 2.
Baseline characteristics of different participation groups
| Persistent participants | Early dropoutsa | Late dropoutsb or returnersc | |
|---|---|---|---|
| N = 3456 | N = 2309 | N = 1044/562 | |
| Sociodemographic characteristics | |||
| Age | |||
| 20–29 years | 18% | 20% | 19% |
| 30–39 years | 35% | 29% | 32% |
| 40–49 years | 30% | 27% | 28% |
| 50–59 years | 17% | 24% | 21% |
| Male | 47% | 45% | 46% |
| Not married or living together | 14% | 28% | 18% |
| Low educational level | 56% | 72% | 68% |
| No paid job | 32% | 44% | 40% |
| Lifestyle characteristics | |||
| Overweight (BMI ≥ 25.0 kg/m2) | 37% | 46% | 43% |
| Obese (BMI ≥ 30.0 kg/m2) | 5% | 12% | 9% |
| Smoking cigarettes | 28% | 44% | 41% |
| Inactived | 30% | 35% | 33% |
| Health characteristics | |||
| Self-perceived health (% less than good) | 21% | 28% | 28% |
| Hypercholesterolaemia (% ≥ 6.5 mmol/l) | 14% | 19% | 17% |
| Hypertensione | 15% | 24% | 21% |
| Chronic diseasesf | 2% | 4% | 3% |
aDropout after one or two measurement rounds.
bDropout after round 3 or 4.
cThose who skipped one or more measurement rounds.
dLess active than Dutch recommended levels for adults, i.e. ≤ 3.5 h per week (Picavet 2011).
eHypertension is mean systolic blood pressure ≥ 140 and/or mean diastolic blood pressure ≥ 90 or using blood pressure-lowering medication.
fSelf-reported diabetes mellitus, cancer, myocardial infarction or cerebral vascular accident (CVA).
For 3456 participants we have information from all five measurement rounds, for 1019 from four rounds, 776 from three rounds, 1140 from two measurement rounds and 1377 from only one, i.e. the baseline measurement.
During follow-up, 243 incident cases of cancer have arisen, 355 incident cases of type 2 diabetes [based on self-reports or elevated (non- fasting) glucose] and 614 cases of cardiovascular disease (CVD) (425 coronary heart disease and 146 cerebrovascular).
What has been measured?
From the start, standard themes and measurements related to chronic diseases were included with special attention to cardiovascular diseases, diabetes, musculoskeletal disorders, respiratory diseases and cancer. These have all been continued during later rounds, including the collection of blood. From round 4 onwards we expanded the measurement protocol and we have added measurements related to ageing, such as functioning and frailty, and to emerging public health topics, such as shift work. Box 1 gives an overview of the measurements in rounds 5 and 6. These new measurements are described below as well as information on the biobank.
Box 1.
Overview of themes measured in the Doetinchem Cohort Study
| Lifestyle factors: smoking (current and history), physical activity by questionnaire and Actigraph,b sedentary time,b alcohol consumption, sleep (hours and qualitya), chronotype.b |
| Biological factors: standing height, weight, blood pressure (arm and ankle), total and HDL-cholesterol, blood glucose, (and several blood samples stored for future analyses), lung function, body mass index, waist and hip circumference, for women: reproductive history and additional characteristics on menstruation, contraception use; heel bone mass,a accumulation of advanced glycation endproducts (AGEs) in the skin,b urine sample (storage for future research questions).a |
| Functioning: quality of life [Short Form (SF)36], cognitive functioning, hearing and eyesight issues, hand grip test,a balance test,a chair test.a |
| Psycho-social aspects: depressive symptoms,a loneliness,a social support,a health literacy,b perception of living environmentb (in particular of possibilities for recreational physical activity). |
| Chronic diseases: diabetes, cardiovascular disease (claudication, stroke, heart disease), migraine, musculoskeletal pain, cancer, asthma and chronic obstructive pulmonary disease (COPD), (history of) fractures,a list of chronic conditions (including incontinence, falling, osteoarthritis).a |
| Diverse: family history of diseases (heart diseases, fractures,a dementia,b menopauseb), oral healthb (teeth and gums), (historical) sound pollution,b contact with (small) children,b consumption of tap waterb |
| Health careb: use of health care services, self-management, giving and receiving informal care, acceptance of vaccination. |
| Background characteristics: age, sex, marital status, educational level, work status and household characteristics, (historical) shift work,b participationb (engagement in social activities), birthweightb |
| Registry links: mortality, hospital discharge by diagnosis, cancer register and pharmacy register. |
aIncluded from round 5 (2008–12) onwards.
bIncluded in round 6 (2013–17) additionally.
New measurements during the physical examination
In rounds 5 and 6 we added a number of items that are relevant for the study of healthy ageing and frailty. Muscle strength was measured through hand grip strength (HGS) of the preferred hand by means of a hydraulic hand-held dynamometer (Jamar) in the sitting position. We also included the timed chair stand test3,4 and the balance test as additional indicators of physical functioning.
For osteoporosis we measured fracture history and also heel bone mass using quantitative ultrasound (QUS) measurements with a Hologic Sahara bone densitometer (Hologic Inc., USA).
Physical activity is a key topic for prevention and ageing research, and as well as the extensive questionnaire we used for many years, we added in round 6 the Actigraph GT3X+,5 for the more objective measurement of physical activity. The Actigraph measures accelerations on three axes (tri-axial) to assess the frequency, duration and intensity of PA over time. Participants wear the Actigraph non-stop for 7 days. A small diary was added with questions on wake-up time, non-wearing time and reasons for it and time spent on biking (and whether an ebike was used).
In human nutrition and biology, advanced glycation end products, known as AGEs, are substances that can be a factor in ageing and in the development or worsening of many degenerative diseases, such as diabetes, atherosclerosis, chronic renal failure and Alzheimer’s disease.6 In order to contribute to this research we added a non-invasive measurement which measures AGEs in the skin of the arm by means of fluorescence techniques [skin autofluorescence (skin AF)] using the AGEs reader made by Diagnoptics Technology, The Netherlands.
New themes in questionnaires
The main themes for which the questionnaires have been extended are as follows.
Sedentary behavior
The measurement of physical activity has traditionally been focused on time spent on specific activities as walking, sports, gardening and biking. Evidence is accumulating that sedentary behavior–the other end of the physical activity continuum–has an effect on health that is independent from physical activity.7 We added questions on time spent sitting separately for transportation, work, computer activities and watching television.
Shift work
Long-term exposure to shift work may influence health, so we included a series of questions on lifetime exposure to shift work, measuring major domains of shift work that have been identified by the international consensus report by Stevens et al.,8i.e. shift system, cumulative exposure and shift intensity.
Health care, self-care, informal care
We measured use of health care: contact with a variety of health care professionals (including GP, medical specialists, dentist, physiotherapist, home care worker, psychologist etc.), similar to usual monitoring of health care use in The Netherlands. In addition we included questions on receiving and providing informal care, and types of and problems with self-care, using the Patient Assessment of Self-management questionnaire (PAST).9
Depressive symptoms
These were measured with a Dutch version of the Center for Epidemiologic Studies Depression scale (CES-D).10,11 In addition we measured loneliness12 and social support [the Social Support List (SSL)-Interaction 12].13
Social participation
One key theme in health policy among elderly is to promote participation within all areas of society. We used a series of questions assessing participation in work, informal care, volunteer work, sports etc.
Sleep characteristics and chronotype
For every round, we asked for the average number of hours of sleep. In round 5 we included a number of questions on sleep quality: ‘Do you lie awake for a long time before you fall asleep?’, ‘Do you wake up during the night?’, ‘Do you experience difficulty falling asleep after you woke up during the night?’, ‘Do you wake up very early in the morning after which you cannot fall asleep again?’, ‘Do you feel not rested after a ‘normal’ night?’ and ‘Do you have a need for a nap?’. Answering options were: ‘often’, ‘always’, ‘seldom or never,’ or ‘now and then’. In round 6 we included the 12 items on sleep as developed by the Medical Outcome Study (MOS)14 and an indication of a person’s chronotype, which refers to the propensity for the individual to sleep at a particular time during a 24 h period. We used a self-reported classification in: morning type (clear or probable), evening type (clear or probable), no type or unknown.
Oral health
Oral health is affected by ageing and is also associated with several chronic diseases. We used a number of questions to assess the condition of teeth and gums, and tooth brushing habits.
Health literacy
Health literacy is defined as the degree to which people are able to access, understand, appraise and communicate information to engage with the demands of different health contexts to promote and maintain health across the life course. We included the often-used screening questionnaire as developed by Chew et al.15
Perception of living environment
This was measured for physical activity (e.g. availability of specific sports facilities), the perception of safety and nature areas, and the exposure to noise pollution. Also we measured historical exposure to noise at work.
Biobank samples and measures
A total of 25 ml of non-fasting venous blood is collected in every round using three types of vacutainers: NaF, serum and EDTA. Samples are centrifuged and aliquoted in 25 cryovial tubes, including plasma, serum, erythrocytes and buffy coat. Standard storage is at -80̊ C. Blood samples are available for all participants for all rounds, though there are some differences per measurement round referring to storage conditions (in round 1 only -20̊ C, and additional -196° C storage in round 2 only) or number of tubes.
Total cholesterol and HDL cholesterol were measured until 1998 in non-fasting EDTA-plasma, and from 1998 onwards in serum at the Lipid Reference Laboratory of Erasmus Medical Center (former University Hospital Dijkzigt) in Rotterdam, using standardized enzymatic methods. Random plasma glucose was measured with the hexokinase method.16
From round 5 onwards we took spot urine samples and stored those at −80° C, after testing the sample for urinary tract infection.
In 2012 we measured several biochemical markers using all available samples of rounds 1 through 5 for each participant. Such single-run measurement maximally reduces inter-assay variation.17 Measures included gamma-glutamyltransferase (GGT), uric acid, triglycerides (GPO-PAP assay), alanine aminotransferase (ALT) (kinetic UV assay), high sensitivity C-reactive protein (CRP), cystatin C and creatinine.
In 2017 all participants with a least three rounds of examination will be included in a genome-wide association study (GWAS).
What has it found? Key findings and publications
As the original focus was CVD, many studies were published on cardiovascular diseases.18–22 With a view over a substantial part of the life course of adults, the research questions have been extended yo life course and ageing topics. These research questions relate to changes in lifestyle over the life course23 and whether these changes are related to health outcomes.19,24 We focus also on the analyses of the course of health characteristics over time 25–27 and the determinants of changes in health, e.g. cognitive decline.28–32 We are also interested in the differences between generations.33,34 Examples of research using our extensive biobank focus on changes in metabolic risk factors over the life course35 and renal on function.36 We also participate in genetic studies.37,38
Round 2 of the Doetinchem Cohort Study was part of the international EPIC study,39,40 and of the spin-off projects on diabetes (EPIC- Interact)41 and cardiovascular disease (EPIC-CVD).42
Cooperation with other studies includes meta-analyses.43 We also used data from the Doetinchem Cohort Study with many other Dutch studies to give the best estimates for disability in Dutch population.44,45 Together with the Longitudinal Ageing Study Amsterdam,46 we analysed the prevalence of smoking for a broad range of generations.47 The Doetinchem Cohort Study is also used as a ‘normal comparison’ for clinical samples, for instance a cohort of patients with rheumatic diseases.48
Some key measurements (blood pressure, blood lipids, body weight, smoking) of the participants in round 5 are presented by sex in Table 3.
Table 3.
Characteristics [mean (SD)] of participants of the Doetinchem Cohort Study, fifth round of examination (2008–12)
| Men | Women | Total | |
|---|---|---|---|
| N = 1901 | N = 2116 | N = 4017 | |
| Age, years [mean (SD)] | 60.5 (9.5) | 59.4 (9.7) | 59.9 (9.6) |
| Blood pressure | |||
| Diastolic, mmHg [mean, (SD)] | 82 (10) | 79 (10) | 80 (10) |
| Systolic in mmHg [mean, (SD)] | 135 (17) | 129 (18) | 131 (18) |
| Hypertension (%)a | 52 | 44 | 48 |
| Blood lipids | |||
| Total cholesterol, mmol/l [mean, (SD)] | 5.4 (1.02) | 5.7 (1.06) | 5.6 (1. 05) |
| Hypercholesterolaemia (≥ 6.5 mmol/l) (%) | 15 | 25 | 21 |
| HDL cholesterol, mmol/l [mean, (SD)] | 1.3 (0.35) | 1.6 (0.42) | 1.4 (0.42) |
| Low HDL cholesterol (≤ 0.9 mmol/l) (%) | 12 | 3 | 7 |
| Body weight | |||
| BMI, kg/m2 [mean, (SD)] | 27.0 (3.5) | 26.7 (4.8) | 26.8 (4.2) |
| Overweight (25 kg/m2 < BMI < 30 kg/m2) (%) | 54 | 38 | 45 |
| Obesity (BMI ≥ 30 kg/m2) (%) | 17 | 21 | 19 |
| Cigarette smoking | |||
| Smokers (%) | 17 | 17 | 17 |
| Ex-smokers (%) | 52 | 42 | 47 |
| Never smokers (%) | 31 | 41 | 37 |
| Mean (SD) number of cigarettes smoked per day (in smokers) | 14.2 (8.1) | 12.0 (6.6) | 13.0 (7.4) |
SD, standard deviation.
aSystolic ≥ 140 mmHg and/or diastolic ≥ 90 mmHg and/or anti-hypertensive medication.
What are the main strengths and weaknesses?
The main strengths of the Doetinchem Cohort Study are: (i) long-term follow-up of randomly selected individuals of a broad age range; (ii) extensive characterization of lifestyle (including nutrition) and health and disease, including lung function, biological material (extensive biobank, including DNA in every round) and cognition in every round; and (iii) the linkage to data from many registries, e.g. cause of death, hospital registries, pharmacy records and cancer registries.
The main weaknesses are: (i) the limited size of the cohort for infrequent health problems; (ii) the lack of ethnic subgroups; and, due to financial limitations, (iii) we were not able to sample new cohorts from the younger age categories during follow-up.
The main challenges we face in carrying out the study refer to attrition and financing of the study. Participating in the physical examination and filling out questionnaires become a bigger challenge, with the longer follow-up of the study. Participants may not like to notice that they are doing worse compared with 5 years earlier. This is in particular a challenge for re-running the cognition measurements. We particularly want to prevent participants from dropping out of the study when they become frail.
We are in the privileged position of having been able to carry out this study already for 30 years. However, continuation of the study with a 7th measurement round, the maintenance of the biobank with samples from all previous rounds, and the more complex organization of carrying out the study with increasingly expanding topics, as well as finding funding for harvesting these rich data, remain a challenge.
Can I get hold of the data? Where can I find out more?
We welcome collaboration with other researchers. Several types of collaboration to exploit the data are possible. Please contact: Professor WMM Verschuren, [monique.verschuren@rivm.nl].
Cohort Profile Update in a nutshell
Originated from a monitoring study on cardiovascular disease risk factors, the Doetinchem Cohort study has been expanded to a study on lifestyle and other determinants of chronic conditions and ageing, with individual data covering 25 years.
In 1987 it started with an age-sex-stratified sample (20–59 years) of the inhabitants of Doetinchem, a mid-size Dutch town, of whom 12 404 (62%) participated in the baseline examination between 1987 and 1991.
Two-thirds of those measured at baseline (n = 7768) were invited for first follow-up measurement in 1993–97 (round 2: n = 6117), a second follow-up in 1998–2002 (round 3: n = 4918). We continued with a round 4 in 2003–07 (n = 4520), round 5 in 2008–12 (n = 4018) and round 6 in 2013–17 (ongoing), with an average response of 78% of those invited.
A broad range of lifestyle, biological, health (physical and psycho-social), well-being, disease and care factors are measured. Unique characteristics include a broad age-range, biological material collected every measurement round (biobank), an extensive lung function measurement and cognition measured from a young age onwards.
We welcome collaboration for using the data, please contact: Professor WMM Verschuren [monique.verschuren@rivm.nl].
Funding
The Doetinchem Cohort Study is supported by the Dutch Ministry of Health, Welfare and Sport and the National Institute for Public Health and the Environment.
Acknowledgements
We thank the respondents, epidemiologists and fieldworkers of the Municipal Health Service in Doetinchem for their contribution to the data collection for this study.
The authors want to acknowledge the logistic management which was provided by P Vissink, and the data managers J van der Laan, R J de Kleine, I Toxopeus. Further, we thank all (senior) researchers who contributed to the data for collection, in particular in (alphabetical order): J M A de Boer, H B Bueno de Mesquita, P Engelfriet, G C Herber-Gast, G Hulsegge, D Kromhout, L Launer, A C J Nooyens, M C Ocké, S H van Oostrom, K Proper, J C Seidell, H A Smit, W G C Wendel-Vos.
Author Contributions
The team of the Doetinchem Cohort Study consists of the authors: W.M.M.V. as principal investigator, H.S.J.P. as project leader, A.B. as head of data management and A.M.W.S. as senior researcher.
Conflict of interest: None declared.
References
- 1. Verschuren WMM, Blokstra A, Picavet HSJ, Smit HA. Cohort Profile: The Doetinchem Cohort Study . Int J Epidemiol 2008;37:1236–41. [DOI] [PubMed] [Google Scholar]
- 2. Hendriksen MAH, van Raaij JMA, Geleijnse JM, Wilson-van den Hooven C, Ocké MC, van der A DL. Monitoring salt and iodine intakes in Dutch adults between 2006 and 2010 using 24 h urinary sodium and iodine excretions. Public Health Nutr 2014;17:1431–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Csuka M, McCarty DJ. A simple method for measurement of lower extremity muscle strength. Am J Med 1985;78:77–81. [DOI] [PubMed] [Google Scholar]
- 4. Guralnik JM, Ferrucci L, Simonsick EM, Salive M, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability . N Engl J Med 1995;332:556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Evenson KR, Buchner DM, Morland KB. Objective measurement of physical activity and sedentary behavior among US Adults aged 60 years or older . Prev Chronic Dis 2012;9:110109. [PMC free article] [PubMed] [Google Scholar]
- 6. Mulder DJ, Van De Water T, Lutgers HL. et al. Skin autofluorescence, a novel marker for glycemic and oxidative stress-derived advanced glycation endproducts: An overview of current clinical studies, evidence, and limitations. Diabetes Technol Ther 2006;8:523–35. [DOI] [PubMed] [Google Scholar]
- 7. Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: The population health science of sedentary behavior. Exerc Sport Sci Rev 2010;38:105–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stevens RG, Hansen J, Costa G. et al. Considerations of circadian impact for defining ‘shift work’ in cancer studies: IARC Working Group Report. Occup Environ Med 2011;68:154–62. [DOI] [PubMed] [Google Scholar]
- 9. Van Houtum L, Rijken M, Heijmans M, Groenewegen P. Patient-perceived self-management tasks and support needs of people with chronic illness: generic or disease specific?. Ann Behav Med 2015;49:221–29 [DOI] [PubMed] [Google Scholar]
- 10. Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401. [Google Scholar]
- 11. Bouma J, Ranchor AV, Sanderman R, Van Sonderen E. Het meten van symptomen van depressie met de CES-D, een handleiding. Noordelijk Centrum voor Gezondheidsvraagstukken, University of Groningen, 1995. [Google Scholar]
- 12. De Jong-Gierveld J. Developing and testing a model of loneliness. J Pers Soc Psychol 1987;53:119–28. [DOI] [PubMed] [Google Scholar]
- 13. Kempen GIJM, Van Eijk LM. The psychometric properties of the SSL12-I, a short scale for measuring social support in the elderly. Soc Indic Res 1995;35:303–12. [Google Scholar]
- 14. Hays RD, Stewart AL. Sleep measures. In: Stewart AL, Ware JE (eds.). Measuring Functioning and Well-being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press, 1992. [Google Scholar]
- 15. Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med 2004;36:588–94. [PubMed] [Google Scholar]
- 16. Tietz NW. Clinical Guide to Laboratory Tests. 3rd edn Philadelphia, PA: Saunders, 1995. [Google Scholar]
- 17. Vart P, Bakker SJ, Schottker B. et al. Relevance of correction for drift and day-to-day variation in cystatin C measurement: A post-hoc analysis of the PREVEND cohort, with independent replication in the ESTHER cohort. Clin Chem Lab Med 2014;53:1381–90 [DOI] [PubMed] [Google Scholar]
- 18. Hulsegge G, Smit HA, van der Schouw YT, Daviglus ML, Verschuren WMM. Quantifying the benefits of achieving or maintaining long-term low risk profile for cardiovascular disease: The Doetinchem Cohort Study. Eur J Prev Cardiol 2015;22:1307–16. [DOI] [PubMed] [Google Scholar]
- 19. Hulsegge G, Looman M, Smit HA, Daviglus ML, van der Schouw YT, Verschuren WMM. Lifestyle changes in young adulthood and middle age and risk of cardiovascular disease and all‐cause mortality: The Doetinchem Cohort Study. J Am Heart Assoc 2016;5:e002432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hulsegge G, Spijkerman AMW, van der Schouw YT. et al. Trajectories of metabolic risk factors and biochemical markers prior to the onset of cardiovascular disease – The Doetinchem Cohort Study. PLoS One 2016;11:e0155978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hoevenaar-Blom MP, Spijkerman AMW, Boshuizen HC, Boer JMA, Kromhout D, Verschuren WMM. Effect of using repeated measurements of a Mediterranean style diet on the strength of the association with cardiovascular disease during 12 years: the Doetinchem Cohort Study. Eur J Nutr 2014;53:1209–15 [DOI] [PubMed] [Google Scholar]
- 22. De Jong HJI, Damoiseaux JGMC, Vandebriel RJ. et al. Use and markers of immunity in the Doetinchem Cohort Study. PLoS One 2013;8:e77587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Picavet HSJ, Wendel-Vos GCW, Vreeken HL, Schuit AJ, Verschuren WMM. How stable are physical activity habits among adults? the Doetinchem Cohort Study. Med Sci Sport Exerc 2011;43:74–79. [DOI] [PubMed] [Google Scholar]
- 24. Van Oostrom SH, Smit HA, Wendel-Vos GCW, Visser M, Verschuren WMM, Picavet HSJ. Adopting an active lifestyle during adulthood and health-related quality of life: The Doetinchem Cohort study. Am J Public Health 2012;102:e62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Van Oostrom SH, Verschuren WMM, De Vet HCW, Picavet HSJ. Ten year course of low back pain in an adult population-based cohort – The Doetinchem Cohort Study. Eur J Pain 2011;15:993–98. [DOI] [PubMed] [Google Scholar]
- 26. Van Hulst R, Van Oostrom SH, Verschuren WMM, Ostelo R, Picavet HSJ. Long-term patterns of chronic complaints of the arms, neck and shoulders and their determinants -The Doetinchem Cohort Study. Pain 2016;157:1114–21. [DOI] [PubMed] [Google Scholar]
- 27. Rooth V, van Oostrom SH, Deeg DJH, Verschuren WMM, Picavet HSJ. Common trajectories of physical functioning in the Doetinchem Cohort Study. Age Ageing 2016;45:382–88. [DOI] [PubMed] [Google Scholar]
- 28. Nooyens ACJ, Van Gelder BM, Verschuren WMM. Smoking and cognitive decline among middle-aged men and women: The Doetinchem Cohort Study. Am J Public Health 2008;98:2244–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nooyens ACJ, Baan CA, Spijkerman AMW, Verschuren WMM. Type 2 diabetes and cognitive decline in middle-aged men and women: The Doetinchem Cohort study. Diabetes Care 2010;33:1964–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nooyens ACJ, Bueno-De-Mesquita HB, Van Boxtel MPJ, Van Gelder BM, Verhagen H, Verschuren WMM. Fruit and vegetable intake and cognitive decline in middle-aged men and women: The Doetinchem Cohort Study. Br J Nutr 2011;106:752–61. [DOI] [PubMed] [Google Scholar]
- 31. Nooyens ACJ, Bueno-De-Mesquita HB, Van Gelder BM, Van Boxtel MPJ, Verschuren WMM. Consumption of alcoholic beverages and cognitive decline at middle age: The Doetinchem Cohort Study. Br J Nutr 2014;111:715–23. [DOI] [PubMed] [Google Scholar]
- 32. Nooyens, Milder IEJ, van Gelder BM, Bueno-de-Mesquita HB, van Boxtel MPJ, Verschuren WMM. Diet and cognitive decline at middle age: the role of antioxidants. Br J Nutr 2015;113:1410–17. [DOI] [PubMed] [Google Scholar]
- 33. Nooyens ACJ, Visscher TLS, Verschuren WMM. et al. Age period and cohort effects on body weight and body mass index in adults: The Doetinchem Cohort Study. Public Health Nutr 2009;12:862–70. [DOI] [PubMed] [Google Scholar]
- 34. Hulsegge G, Picavet HSJ, Blokstra A. et al. Today’s adult generations are less healthy than their predecessors: Generation shifts in metabolic risk factors: The Doetinchem Cohort Study. Eur J Prev Cardiol 2014;21:1134–44. [DOI] [PubMed] [Google Scholar]
- 35. Hulsegge G, Herber-Gast GM, Spijkerman AMW. et al. Obesity and age-related changes in markers of oxidative stress and inflammation across four generations. Obesity (Silver Spring) 2016;24:1389–96 [DOI] [PubMed] [Google Scholar]
- 36. Herber-Gast G-CM, Hulsegge G, Hartman L. et al. Physical activity is not associated with estimated glomerular filtration rate among young and middle-aged adults: Results from the population-based longitudinal Doetinchem study. PLoS One 2015;10:e0133864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lu Y, Feskens EJM, Dollé MET. et al. Dietary n-3 and n-6 polyunsaturated fatty acid intake interacts with FADS1 genetic variation to affect total and HDL-cholesterol concentrations in the Doetinchem Cohort Study. Am J Clin Nutr 2010;92:258–65. [DOI] [PubMed] [Google Scholar]
- 38. Dijkstra AE, Smolonska J, Van Den Berge M. et al. Susceptibility to chronic mucus hypersecretion, a genome wide association study. PLoS One 2014;9:e91621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Riboli E, Kaaks R. The EPIC Project: Rationale and study design. Int J Epidemiol 1997;26:S6–14. [DOI] [PubMed] [Google Scholar]
- 40. Beulens JWJ, Monninkhof EM, Verschuren WMM. et al. Cohort Profile: The EPIC-NL. Int J Epidemiol 2010;39:1170–78. [DOI] [PubMed] [Google Scholar]
- 41. Langenberg C, Sharp S, Forouhi NG. et al. ; InterAct Consortium. Design and cohort description of the InterAct Project: an examination of the interaction of genetic and lifestyle factors on the incidence of type 2 diabetes in the EPIC Study. Diabetologia 2011;54:2272–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Crowe FL, Roddam AW, Key TJ. et al. Fruit and vegetable intake and mortality from ischaemic heart disease: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Heart study. Eur Heart J 2011;32:1235–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cloostermans L, Wendel-Vos WGC, Howard BJ. et al. The independent and combined effect of physical activity and body mass index on the development of type 2 diabetes – A meta-analysis of 10 prospective cohort studies. Int J Behav Nutr Phys Act 2015;12:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hoeymans N, Wong A, Van Gool CH. et al. Late-life activity limitations and the contribution of chronic conditions. The Dutch population between 1990 and 2007 . Am J Public Health 2012;102:163–70.22095363 [Google Scholar]
- 45. Van Gool CH, Picavet HSJ, Deeg DJH. et al. Trends in late-life activity limitations. The Dutch population between 1990 and 2007 . Int J Epidemiol 2011;40:1056–67. [DOI] [PubMed] [Google Scholar]
- 46. Huisman M, Poppelaars J, van der Horst M. et al. Cohort Profile: The Longitudinal Aging Study Amsterdam. Int J Epidemiol 2011;40:868–76. [DOI] [PubMed] [Google Scholar]
- 47. Raho E, Van Oostrom SH, Visser M. Generation shifts in smoking prevalence – the Doetinchem Cohort Study and the Longitudinal Aging Study Amsterdam. BMC Public Health 2015;15:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Meek IL, Picavet HSJ, Vonkeman HE, Verschuren WMM, van de Laar MAFJ. Overrepresentation of cardiovascular risk factors in all (common) rheumatic diseases. Rheumatology 2013;52:210–16. [DOI] [PubMed] [Google Scholar]