Abstract
Aims
To determine if progression of mitral annular calcium (MAC) detected by cardiac computed tomography (CT) predicts incident atrial fibrillation (AF).
Methods and results
This analysis included 5683 participants (mean age 64 ± 10 years; 52% women; 40% whites; 27% blacks; 21% Hispanics; 12% Chinese–Americans) from the Multi-Ethnic Study of Atherosclerosis. MAC was measured by cardiac CT at baseline and at a follow-up CT scan over a mean time of 2.4 ± 0.84 years. AF was ascertained by review of hospital discharge records and from Medicare claims data through 31 December 2012. Cox regression was used to compute hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between MAC progression and AF. Over a median follow-up of 8.6 years, a total of 533 (9.4%) incident AF cases were detected. In a model adjusted for age, sex, race/ethnicity, education, income, baseline MAC, systolic blood pressure, body mass index, diabetes, smoking, total cholesterol, high-density lipoprotein cholesterol, antihypertensive medications, lipid-lowering therapies, and aspirin, any MAC progression (>0/year) was associated with an increased risk for AF (HR = 1.50, 95% CI = 1.20–1.87). Multiplicative interactions were not significant between MAC progression and AF by age (<65 year vs. older), sex, or race/ethnicity (whites vs. non-whites).
Conclusion
Important prognostic information regarding AF risk is obtained with follow-up MAC measurement, as the risk for participants with any MAC progression was substantively greater than participants without progression. MAC progression may detect underlying left atrial abnormalities that predispose to AF.
Keywords: mitral calcium , atrial fibrillation , cardiac CT
Introduction
Mitral annular calcification (MAC) is a chronic degenerative process that commonly affects the base of the mitral valve. Risk factors for its development include advanced age and female sex.1,2 The presence of MAC has been shown to predict future cardiovascular events.3–7 Additionally, reports from the Multi-Ethnic Study of Atherosclerosis (MESA) and the Framingham Heart Study have shown that MAC independently predicts the development of atrial fibrillation (AF).8,9 However, it is yet to be established whether the risk of AF associated with MAC also depends on the rate at which it develops (e.g. progression). It is possible that MAC progression is a better tool to identify individuals who are high risk for AF development than MAC measurements from a single point in time. Therefore, we hypothesized that MAC progression is an independent predictor of AF, and the predictive ability associated with this phenomenon exceeds the simple presence of MAC. Accordingly, we explored this hypothesis in MESA.
Methods
Study population
MESA is a prospective study with aims to determine characteristics related to the progression of subclinical to clinical cardiovascular disease, and details have been previously reported.10 Briefly, between July 2000 and September 2002, a total of 6814 persons were recruited at 6 field centres (Baltimore, MD; Chicago, IL; Forsyth County, NC; Los Angeles, CA; New York, NY; and St. Paul, MN). Participants were required to be between 45 and 84 years of age and to have no clinical cardiovascular disease at baseline. All participants provided informed consent and the study protocol was approved by the institutional review boards at each participating institution.
This study was a retrospective analysis of prospectively collected data to examine the relationship between MAC progression and AF development. For the purpose of this analysis, we included participants with MAC measurements at baseline (2000–02) and follow-up (either Exam 2: 2002–04 or Exam 3: 2004–05). Participants were excluded if clinically recognized AF was present before the follow-up MAC measurement, or if they were missing baseline characteristics or follow-up data.
Mitral annular calcium
Mitral annular calcium (MAC) was assessed by cardiac computed tomography (CT) using either cardiac-gated electron-beam CT or multi-detector CT systems, depending on the study site.11 All participants in MESA underwent two consecutive CT scans. The two scans were independently analysed by two analysts and MAC was defined by the presence of calcium (Agatston score > 0) on the mitral valve. The MAC score was computed using the phantom-adjusted Agatston method,12 and the mean MAC value was recorded. Inter-observer (κ-statistic, 0.90) and intra-observer (κ-statistic, 0.93) agreement between different CT image analysts who measured MAC on the same cardiac CT image was excellent.11,13 Phantom-adjusted Agatston scores for baseline and follow-up measurements were used to compute the change in MAC per year. Participants who had >0 units of change/year were compared with those who had no change or reductions (≤0 units/year) in MAC values between CT scans.14
Participant characteristics
Participant characteristics were collected during the second MAC measurement (either Exam 2: 2002–04 or Exam 3: 2004–05). Age, sex, race/ethnicity, income, and education were self-reported. Annual income was categorized as <$20 000 or ≥$20 000 and education was categorized as ‘high school or less’, or ‘some college or more’. Smoking was defined as the current use of cigarettes. Blood samples were obtained after a 12-h fast and measurements of total cholesterol, high-density lipoprotein cholesterol, and plasma glucose were used. Diabetes was defined as fasting glucose values ≥126 mg/dL or diabetes medication use. Blood pressure was measured for each participant after 5 min in the seated position. Systolic measurements were recorded three separate times and the mean of the last two values was used. Aspirin, antihypertensive, and lipid-lowering medication use were ascertained by self-report or pill bottle review. Body mass index was computed as the weight in kilograms divided by the square of the height in metres.
Atrial fibrillation
Follow-up phone calls to study participants every 9–12 months were used to identify hospitalizations. Medical records, including discharge diagnoses, were obtained for each hospitalization. Additionally, for participants 65 years or older enrolled in fee-for-service Medicare, Medicare claims data were used to identify AF diagnoses in the inpatient and outpatient settings. Incident AF was defined by International Classification of Disease Ninth Revision codes 427.31 or 427.32.
Statistical analysis
Baseline characteristics were compared by those with and without MAC progression. Categorical variables were reported as frequency and percentage while continuous variables were recorded as mean ± standard deviation (SD). Statistical significance for categorical variables was tested using the chi-square method and for continuous variables using the Student’s t-test. Follow-up time was defined as the time between the second CT scan until a diagnosis of AF, death, loss to follow-up, or end of follow-up (31 December 2012). Cox regression was used to compute hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between MAC progression and AF. Kaplan–Meier estimates were used to compute cumulative incidence of AF by MAC progression and the differences in estimates were compared using the log-rank procedure.15 Multivariable models were constructed with incremental adjustment as follows: Model 1 adjusted for age, sex, race/ethnicity, education, income, and baseline MAC; Model 2 adjusted for Model 1 covariates with the addition of systolic blood pressure, body mass index, diabetes, smoking, total cholesterol, high-density lipoprotein cholesterol, antihypertensive medications, lipid-lowering therapies, and aspirin. The proportional hazards assumption was not violated in our analysis. Additionally, we tested for multiplicative interactions using the likelihood ratio method by age (dichotomized at 65 years), sex, and race/ethnicity (white vs. non-white). We also examined if the association between MAC progression and AF was dependent on baseline values by limiting the analysis to participants with baseline MAC (n = 495). To demonstrate that the association between MAC progression and AF possibly is stronger than MAC measured at one time period, we compared the magnitude of the association for MAC progression in persons who had baseline MAC (n = 495) and those who did not have baseline MAC (n = 5188) per 1-SD increase in MAC progression. Statistical significance for all comparisons and tests for interaction was defined as P < 0.05. SAS version 9.4 (Cary, NC) was used for all analyses.
Results
A total of 5683 participants (mean age 64 ± 10 years; 52% women; 40% whites; 27% blacks; 21% Hispanics; 12% Chinese–Americans) were included in the final analysis. A total of 547 (9.6%) participants had MAC progression between CT scans and 5136 (90.4%) did not have MAC progression. Baseline characteristics for participants by MAC progression are shown in Table 1.
Table 1.
Participant characteristics from MESA visit 3 by MAC progression (N = 5683)
| Characteristic | No MAC progression (n = 5136) | MAC progression (n = 547) | P-valuea |
|---|---|---|---|
| Age, mean ± SD, years | 63 ± 10 | 72 ± 8.1 | <0.001 |
| Male (%) | 2481 (48) | 225 (41) | 0.0014 |
| Race | |||
| White (%) | 1970 (38) | 280 (51) | <0.001 |
| Chinese–Americans (%) | 625 (12) | 41 (7.0) | |
| Black (%) | 1434 (28) | 107 (20) | |
| Hispanic (%) | 1107 (22) | 119 (22) | |
| Education, high school or less (%) | 1741 (34) | 216 (39) | 0.0089 |
| Income, <$20 000 (%) | 1392 (27) | 209 (38) | <0.001 |
| Current smoker (%) | 593 (12) | 48 (9.0) | 0.052 |
| Diabetes (%) | 754 (15) | 119 (22) | <0.001 |
| Body mass index, mean ± SD, kg/m2 | 28 ± 5.5 | 29 ± 5.7 | <0.001 |
| Systolic blood pressure, mean ± SD, mmHg | 123 ± 20 | 131 ± 23 | <0.001 |
| Total cholesterol, mean ± SD, mg/dL | 191 ± 36 | 189 ± 35 | 0.34 |
| HDL cholesterol, mean ± SD, mg/dL | 52 ± 15 | 52 ± 15 | 0.58 |
| Antihypertensive medications (%) | 2063 (40) | 312 (57) | <0.001 |
| Aspirin (%) | 1646 (32) | 244 (45) | <0.001 |
| Lipid-lowering therapies (%) | 1164 (23) | 171 (31) | <0.001 |
HDL, high-density lipoprotein; MAC, mitral annular calcium; SD, standard deviation.
aStatistical significance for continuous data was tested using the Student’s t-test and categorical data was tested using the chi-square test.
The mean time between CT scans for study participants was 2.4 ± 0.84 years. The mean change in MAC per year was 7.8 ± 95 units. Participants with baseline MAC (n = 495, 8.7%) were more likely to have MAC progression (n = 323, 65%) compared with participants without baseline MAC (n = 224, 4.3%) (P < 0.001).
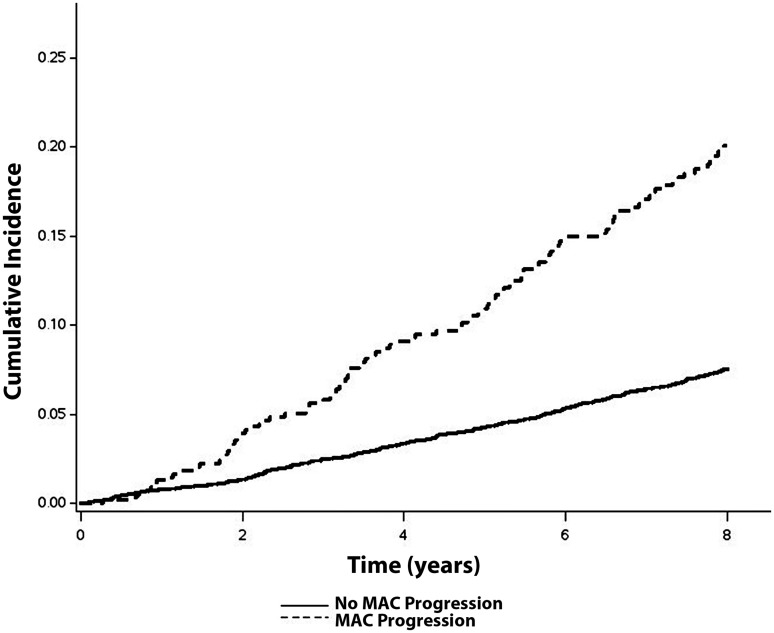
Over a median follow-up of 8.6 years (25th, 75th percentile = 7.8, 9.6), a total of 533 (9.4%) incident AF cases were detected. A higher incidence (per 1000 person-years) of AF was observed in those with MAC (>0/year) progression (incidence rate = 28.9, 95% CI = 24.1–34.7) than those without MAC progression (incidence rate = 9.9, 95% CI = 8.9–10.8). The unadjusted cumulative incidence of AF among those with and without MAC progression is shown in Figure 1 (log-rank P < 0.001).
Figure 1.
Unadjusted cumulative incidence of atrial fibrillation by MAC progression*. *Cumulative incidence curves are different (log-rank P < 0.001). MAC, mitral annular calcium.
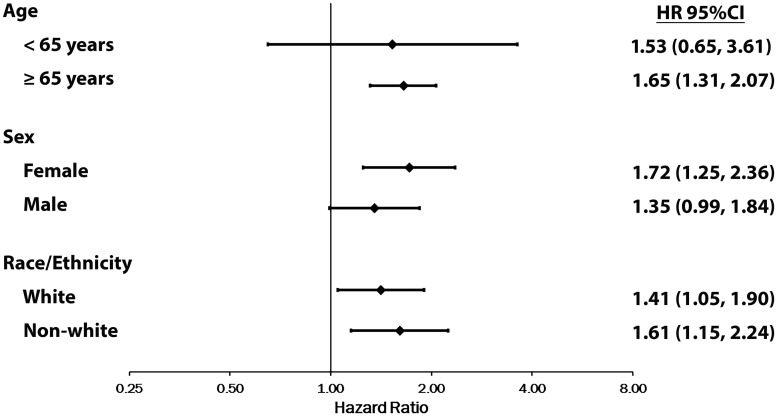
When we adjusted for age, sex, race/ethnicity, education, income, and baseline MAC, any MAC progression (>0/year) was associated with an increased risk for AF (Table 2). Similar results were obtained with further adjustment in Model 2 (Table 2). There was no evidence of multiplicative or additive interactions by age, sex, or race/ethnicity (Figure 2).
Table 2.
Risk of atrial fibrillation with MAC progressiona
| Events/number at risk | Model 1b | P-value | Model 2c | P-value | |
|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | ||||
| MAC progression | |||||
| No | 417/5136 | Reference | — | Reference | — |
| Yes | 116/547 | 1.54 (1.24–1.92) | <0.001 | 1.50 (1.20–1.87) | <0.001 |
CI, confidence interval; HR, hazard ratio; MAC, mitral annular calcium.
aHRs presented are for any progression (>0/year).
bAdjusted for age, sex, race/ethnicity, education, income, and baseline MAC.
cAdjusted for Model 1 covariates plus systolic blood pressure, body mass index, diabetes, smoking, total cholesterol, high-density lipoprotein cholesterol, antihypertensive medications, lipid-lowering therapies, and aspirin.
Figure 2.
Risk of atrial fibrillation with MAC progression by age, sex, and race*. *HRs presented are for any progression (>0/year). Estimates adjusted for age, sex, race/ethnicity, education, income, baseline MAC, systolic blood pressure, body mass index, diabetes, smoking, total cholesterol, high-density lipoprotein cholesterol, antihypertensive medications, lipid-lowering therapies, and aspirin. Estimates were not different by age (P-interaction = 0.81), sex (P-interaction = 0.41), or race/ethnicity (P-interaction = 0.77). CI, confidence interval; HR, hazard ratio; MAC, mitral annular calcium.
After excluding participants who did not have baseline MAC, a trend was observed for the association between MAC progression and AF (HR = 1.49, 95% CI = 0.94–2.16; P = 0.092). When we examined the risk of AF associated with MAC progression per 1-SD increase among participants with baseline MAC, a trend for significance was observed for increases in MAC progression (HR = 1.13, 95% CI = 0.99–1.27; P = 0.055). In contrast, MAC progression was not associated with AF risk among participants without baseline MAC (per 1-SD increase in MAC: HR = 0.99, 95% CI = 0.92–1.06; P = 0.76).
Discussion
In this analysis from MESA, we have demonstrated that the accumulation of higher levels of MAC over time is associated with an increased risk for AF development. Compared with participants who had no MAC progression, a 50% increase in AF risk was observed for those who had any progression, and this risk did not depend on the baseline level of MAC. Overall, our data suggest that important prognostic information regarding AF risk is obtained with follow-up MAC measurements.
Several reports have examined the predictive ability of MAC measurements in the prediction of AF events. Data from the racially and ethnically diverse population of MESA using cardiac CT have demonstrated that baseline MAC predicts incident AF.8 Similar results were reported from the Framingham Heart Study in which MAC, detected by echocardiography, was associated with an increased AF risk.9 The aforementioned studies examined the predictive ability of MAC from measurements at single time points, and although different modalities were used to measure MAC, both studies implicate MAC in the prediction of AF.
To our knowledge, our findings are the first to report that increases in MAC measurements over time are associated with an increased risk for AF. Our data also suggest that MAC progression plays an important role in the development of AF among persons who have detectable levels of MAC at a single point in time. This is supported by the fact that participants who had baseline MAC had a greater risk for AF development if MAC progression was observed. In contrast, participants with baseline MAC who did not have MAC progression had a lower risk of AF development. Although participants with baseline MAC were more likely to have MAC progression, these findings suggest that the risk of AF increases with further accumulation of MAC. Overall, the data presented in this report demonstrate that follow-up MAC measurements provide important prognostic information in the prediction of AF events, especially among persons who already have detectable MAC.
The pathophysiologic link between MAC and AF remains unclear. Several cardiovascular risk factors have been implicated in the development and progression of MAC (e.g. advanced age, hypertension, and diabetes).1,2 Notably, many of these risk factors are well-known AF risk factors.16,17 Although MAC progression was associated with AF independent of these shared risk factors, it is possible that the accumulation of MAC reflects an unfavourable cardiovascular profile in which AF is likely to develop. This is supported by data that have demonstrated an association between MAC and left atrial enlargement,9,18 a well-known risk factor for AF propagation.19 Therefore, the severity of MAC, and rate of progression, possibly represent a surrogate marker for left atrial abnormalities in which the occurrence of AF is likely.
The findings of this analysis have important clinical implications. MAC has been shown to predict incident stroke,20 and it is possible that AF is an intermediate event. Additionally, patients with AF who have evidence of MAC have an increased risk of cardiovascular mortality.3 Therefore, MAC not only predicts AF development but its presence confers an increased risk for adverse cardiovascular outcomes among those who already have the arrhythmia. Although the clinical utility of MAC measurements by cardiac CT to assess AF risk remains uncertain, the current study provides clinicians with important information, as they aim to implement strategies to prevent AF and to reduce the burden of adverse outcomes if AF is apparent. Furthermore, as the utilization of cardiac CT and other imaging modalities are incorporated into clinical practice,21 the assessment of AF risk associated with MAC will be more widely available. Despite the potential clinical utility of MAC detection to identify persons in whom AF is likely to develop, further studies are needed before recommendations in clinical practice are made.
Our results should be interpreted in the context of certain limitations. The progression of MAC was presumed to be linear based on 2 CT scans over an average of 2 years. However it is possible that MAC progression was not linear and the relationship between MAC progression and AF varies with different intervals. Participants with complete MAC measurements were included in our analysis and possibly this resulted in selection bias. Incident AF cases were ascertained from hospitalization discharge records and Medicare claims data using International Classification of Disease codes, which possibly resulted in misclassification. However, these codes have adequate positive predictive value for the identification of inpatient AF events.22 Additionally, a trend was observed for the association between MAC progression and AF after excluding participants who did not have baseline MAC, as our analysis likely did not have the power to detect a statistically significant result. Furthermore, we included several potential confounders in our multivariable models that likely influenced the development of AF, but we acknowledge that residual confounding remains a possibility. For example, data on left atrial size were not collected and we were unable to incorporate this into our models.
In conclusion, the findings of this analysis suggest that MAC progression is an important marker of AF risk. MAC progression likely detects persons who have the necessary substrate for AF development. Further studies are needed to explore the utility of detecting MAC by cardiac CT, and its ability to reduce the occurrence of AF.
Acknowledgements
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Conflict of interest: S.N. is the principal investigator for research funds awarded to Johns Hopkins University from Biosense Webster Inc. and is also a consultant to Biosense Webster, St Jude Medical, CardioSolv, and Spectranetics. The other authors have no conflicts of interest to declare.
Funding
This research was supported by contracts N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168, and N01-HC-95169 from the National Heart, Lung, and Blood Institute and by grants UL1-TR-000040 and UL1-TR-001079 from NCRR, R01-HL-127659 from the National Heart, Lung, and Blood Institute, and American Heart Association grant 16EIA26410001. W.T.O. is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number F32-HL-134290. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1. Kanjanauthai S, Nasir K, Katz R, Rivera JJ, Takasu J, Blumenthal RS. et al. Relationships of mitral annular calcification to cardiovascular risk factors: the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis 2010;213:558–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Elmariah S, Budoff MJ, Delaney JA, Hamirani Y, Eng J, Fuster V. et al. Risk factors associated with the incidence and progression of mitral annulus calcification: the multi-ethnic study of atherosclerosis. Am Heart J 2013;166:904–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Potpara TS, Vasiljevic ZM, Vujisic-Tesic BD, Marinkovic JM, Polovina MM, Stepanovic JM. et al. Mitral annular calcification predicts cardiovascular morbidity and mortality in middle-aged patients with atrial fibrillation: the Belgrade Atrial Fibrillation Study. Chest 2011;140:902–10. [DOI] [PubMed] [Google Scholar]
- 4. Fox CS, Vasan RS, Parise H, Levy D, O'Donnell CJ, D'Agostino RB. et al. Mitral annular calcification predicts cardiovascular morbidity and mortality: the Framingham Heart Study. Circulation 2003;107:1492–6. [DOI] [PubMed] [Google Scholar]
- 5. Kohsaka S, Jin Z, Rundek T, Boden-Albala B, Homma S, Sacco RL. et al. Impact of mitral annular calcification on cardiovascular events in a multiethnic community: the Northern Manhattan Study. JACC Cardiovasc Imaging 2008;1:617–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fox E, Harkins D, Taylor H, McMullan M, Han H, Samdarshi T. et al. Epidemiology of mitral annular calcification and its predictive value for coronary events in African Americans: the Jackson Cohort of the Atherosclerotic Risk in Communities Study. Am Heart J 2004;148:979–84. [DOI] [PubMed] [Google Scholar]
- 7. Pradelli D, Faden G, Mureddu G, Rossi A, Cioffi G, Gaibazzi N. et al. Impact of aortic or mitral valve sclerosis and calcification on cardiovascular events and mortality: A meta-analysis. Int J Cardiol 2013;170:e51–5. [DOI] [PubMed] [Google Scholar]
- 8. O'Neal WT, Efird JT, Nazarian S, Alonso A, Heckbert SR, Soliman EZ.. Mitral annular calcification and incident atrial fibrillation in the Multi-Ethnic Study of Atherosclerosis. Europace 2015;17:358–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fox CS, Parise H, Vasan RS, Levy D, O'Donnell CJ, D'Agostino RB. et al. Mitral annular calcification is a predictor for incident atrial fibrillation. Atherosclerosis 2004;173:291–4. [DOI] [PubMed] [Google Scholar]
- 10. Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR. et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol 2002;156:871–81. [DOI] [PubMed] [Google Scholar]
- 11. Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR Jr. et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology 2005;234:35–43. [DOI] [PubMed] [Google Scholar]
- 12. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R.. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827–32. [DOI] [PubMed] [Google Scholar]
- 13. Budoff MJ, Takasu J, Katz R, Mao S, Shavelle DM, O'Brien KD. et al. Reproducibility of CT measurements of aortic valve calcification, mitral annulus calcification, and aortic wall calcification in the multi-ethnic study of atherosclerosis. Acad Radiol 2006;13:166–72. [DOI] [PubMed] [Google Scholar]
- 14. O'Neal WT, Efird JT, Qureshi WT, Yeboah J, Alonso A, Heckbert SR. et al. Coronary artery calcium progression and atrial fibrillation: the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Imaging 2015;8:e003786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gray RJ, Tsiatis AA.. A linear rank test for use when the main interest is in differences in cure rates. Biometrics 1989;45:899–904. [PubMed] [Google Scholar]
- 16. Schnabel RB, Sullivan LM, Levy D, Pencina MJ, Massaro JM, D'Agostino RB Sr. et al. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort study. Lancet 2009;373:739–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kannel WB, Wolf PA, Benjamin EJ, Levy D.. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol 1998;82:2N–9. [DOI] [PubMed] [Google Scholar]
- 18. Kizer JR, Bella JN, Palmieri V, Liu JE, Best LG, Lee ET. et al. Left atrial diameter as an independent predictor of first clinical cardiovascular events in middle-aged and elderly adults: the Strong Heart Study (SHS). Am Heart J 2006;151:412–8. [DOI] [PubMed] [Google Scholar]
- 19. Parkash R, Green MS, Kerr CR, Connolly SJ, Klein GJ, Sheldon R. et al. The association of left atrial size and occurrence of atrial fibrillation: a prospective cohort study from the Canadian Registry of Atrial Fibrillation. Am Heart J 2004;148:649–54. [DOI] [PubMed] [Google Scholar]
- 20. Benjamin EJ, Plehn JF, D'Agostino RB, Belanger AJ, Comai K, Fuller DL. et al. Mitral annular calcification and the risk of stroke in an elderly cohort. N Engl J Med 1992;327:374–9. [DOI] [PubMed] [Google Scholar]
- 21. Ladapo JA, Jaffer FA, Hoffmann U, Thomson CC, Bamberg F, Dec W. et al. Clinical outcomes and cost-effectiveness of coronary computed tomography angiography in the evaluation of patients with chest pain. J Am Coll Cardiol 2009;54:2409–22. [DOI] [PubMed] [Google Scholar]
- 22. Alonso A, Agarwal SK, Soliman EZ, Ambrose M, Chamberlain AM, Prineas RJ. et al. Incidence of atrial fibrillation in whites and African-Americans: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J 2009;158:111–7. [DOI] [PMC free article] [PubMed] [Google Scholar]