Abstract
Background
Pesticide self-poisoning is a major problem in Bangladesh. Over the past 20-years, the Bangladesh government has introduced pesticide legislation and banned highly hazardous pesticides (HHPs) from agricultural use. We aimed to assess the impacts of pesticide bans on suicide and on agricultural production.
Methods
We obtained data on unnatural deaths from the Statistics Division of Bangladesh Police, and used negative binomial regression to quantify changes in pesticide suicides and unnatural deaths following removal of WHO Class I toxicity HHPs from agriculture in 2000. We assessed contemporaneous trends in other risk factors, pesticide usage and agricultural production in Bangladesh from 1996 to 2014.
Results
Mortality in hospital from pesticide poisoning fell after the 2000 ban: 15.1% vs 9.5%, relative reduction 37.1% [95% confidence interval (CI) 35.4 to 38.8%]. The pesticide poisoning suicide rate fell from 6.3/100 000 in 1996 to 2.2/100 000 in 2014, a 65.1% (52.0 to 76.7%) decline. There was a modest simultaneous increase in hanging suicides [20.0% (8.4 to 36.9%) increase] but the overall incidence of unnatural deaths fell from 14.0/100 000 to 10.5/100 000 [25.0% (18.1 to 33.0%) decline]. There were 35 071 (95% CI 25 959 to 45 666) fewer pesticide suicides in 2001 to 2014 compared with the number predicted based on trends between 1996 to 2000. This reduction in rate of pesticide suicides occurred despite increased pesticide use and no change in admissions for pesticide poisoning, with no apparent influence on agricultural output.
Conclusions
Strengthening pesticide regulation and banning WHO Class I toxicity HHPs in Bangladesh were associated with major reductions in deaths and hospital mortality, without any apparent effect on agricultural output. Our data indicate that removing HHPs from agriculture can rapidly reduce suicides without imposing substantial agricultural costs.
Keywords: Bangladesh, pesticides, suicide, prevention, agriculture
Key Messages
Between 1996 and 2007, 21 pesticides were partially or completely banned by the Bangladeshi regulator, resulting in a shift towards the use of less hazardous WHO toxicity class II, III and U pesticides. All WHO Class I toxicity HHPs were banned in 2000.
During the post-ban years (2001–14), there were 35 071 (95% CI 25 959 to 45 666) fewer pesticide suicide deaths in Bangladesh compared with pre-ban period (1996–2000).
There was also evidence of a decline in total unnatural deaths in the post-ban years, with an estimated 76 642 (95% CI 53 493 to 103 161) fewer unnatural deaths.
The pesticide regulation had an influence on pesticide suicide and overall unnatural death rates without any apparent harmful effect on agricultural production.
Introduction
Pesticide self-poisoning is a major global means of suicide, responsible for around 150 000 deaths each year.1–5 Widespread use of pesticides in rural Asian communities allows easy access in households and through vendors at times of stress.6,7 A key means of reducing the global suicide rate is to reduce access to highly hazardous pesticides (HHPs) through reducing their use in agriculture, safer use and storage, and particularly through regulating and banning HHPs.4,8–11 Additional approaches to suicide prevention include surveillance, means restriction, media guidelines, stigma reduction and raising of public awareness, as well as training for health workers, educators, police and other gatekeepers.4
Bangladesh is an agrarian country (current population 161 million in 2015)12 with agriculture responsible for 30% of the country's gross domestic product (GDP), 51% of the labour force and >90% of rural employment.13 There is extensive use of pesticides in agriculture.14 Self-poisoning by pesticide is a serious health problem responsible for about 40% of poisoning cases admitted to hospital and 8–10% of overall mortality in medical wards.15,16 According to government statistics, it is the second most common cause of hospitalization and ninth most common cause of death.17 The exact burden of pesticide-related suicide is unknown in Bangladesh. In addition to acute poisoning, pesticides have also been associated with chronic diseases such as cancer, endocrine disruption and neurological disease as well as pollution of the ecosystem.3
Synthetic insecticides were introduced in agricultural practice in the 1950s (Supplementary Table 1, available as Supplementary data at IJE online).14 Over the past two decades, the Bangladesh Government has introduced pesticide legislation, established government bodies to implement the legislation and removed HHPs from agricultural use. The effect of this government action on national suicide rates from pesticide poisoning and from all causes, as well as its effect on agricultural output, has not thus far been investigated. In this study, we found that pesticide regulation was associated with a major reduction in the incidence of suicide by pesticide poisoning and in overall unnatural death rates, without any apparent harmful influence on agricultural production.
Methods
We collected national Bangladeshi data on pesticide regulatory activities, suicide rates, pesticide poisoning case fatality in hospital, pesticide imports and usage, agricultural outputs and risk factors for suicide, for the years 1996 to 2014.15
National pesticide regulation
Information on national pesticide regulatory activities was obtained from the Plant Protection Wing, Department of Agricultural Extension, Ministry of Agriculture, Government of Bangladesh, and from discussions with people working in the Bangladeshi pesticide industry.
Suicide data
Suicide data were obtained from the Statistics Division of the Bangladesh Police, which has collected national data on annual unnatural deaths since 1996. These police data identify suicides due to the two main forms, pesticide poisoning (ICD-10: X68) and hanging suicides (X70), while grouping all other forms of suicide in unnatural deaths.18 Other categories within the unnatural deaths classification included road traffic crashes, railway and waterway accidents, falls from height, construction injuries, snake bite, drowning, electrocution, lightning injuries and burn-related deaths. No sex- or age-specific data were recorded. Annual population data estimates for 1996 to 2014 were taken from the World Bank.19
Data on risk factors for suicide
Unemployment and agriculture employment data were obtained from the World Bank19,20 and data on divorce rates for 2002 to 2010 from the Bangladesh Bureau of Statistics.21 Data on alcohol misuse were obtained from a paper summarizing yearly reports for 2006 to 2011 of the Department of Narcotics Control (DNC), Bangladesh, and from the World Health Organization’s (WHO’s) Global Status Report on Alcohol and Health (for 2004, 2011 and 2014).22,23
Data on crop production and pesticide use
Longitudinal trend data on rice production (the principal national crop) for Bangladesh and other South Asian countries were obtained from the Statistical Division of the Food and Agricultural Organization of the United Nations (FAO) and from the International Rice Research Institute.24,25 Pesticide use data were obtained from the Bangladesh Pesticide Association and from the Journal of International Development and Cooperation.26 Pesticides were classified according to the WHO Classification of Pesticides (Class Ia (extremely hazardous), Class Ib (highly hazardous), Class II (moderately hazardous), Class III (slightly hazardous), and Class U (unlikely to present acute hazards).27
Data analysis
Data analysis was performed on GraphPad Prism 7 and Stata version 14. We examined trends in overall unnatural deaths, suicides by pesticide poisoning or hanging, and other causes of unnatural deaths, graphically using descriptive statistics. There was statistical evidence of over-dispersion in the Poisson regression models and therefore we used negative binomial regression to quantify changes in the rate and number of: (i) pesticide suicides; and (ii) unnatural deaths, following removal of all Class I pesticides from agricultural use in 2000. We calculated rate ratios (and the change in the number of suicides) for each year in 2001–14 compared with predicted rates based on extrapolated trends before the ban (1996–2000). Negative binomial regression models included a single trend term for calendar year and a dummy variable for each of the post-ban years (14 dummy variables: 2001–14). We carried out sensitivity analyses using 1999 and 2001 as cut-points for pre-/post-ban effects, consistent with the approach used in our recent analysis of the impact of the most recent pesticide legislation in Sri Lanka.28
Using the rate ratios and confidence intervals from the primary negative binomial model, we calculated the number of expected pesticide and unnatural deaths for each of the post-ban years (i.e. after 2000). We did this by dividing the observed number of pesticide suicide and unnatural deaths by the rate ratio estimates and confidence intervals. We subtracted the number of expected deaths (pesticide suicide and unnatural) based on pre-ban trends (1996–2000) from the observed number of deaths. In the absence of age-specific mortality data, all analyses were based on crude mortality rates.
Results
Pesticide regulation
Between 1996 and 2007, 21 pesticides were partially or completely banned by the Bangladeshi regulator (Table 1), resulting in a shift towards the use of less hazardous WHO toxicity classes II, III and U pesticides. Organochlorine compounds were the main pesticides used in Bangladesh from 1950 until their withdrawal in the mid 1990s.14 The widely used organophosphorus (OP) insecticide HHPs were banned at the end of 2000 when all Class I pesticides were banned from agricultural practice.14
Table 1.
Pesticides banned or withdrawn from agricultural practice in Bangladesh
| Year | Compound(s) | Reasons for ban/withdrawal |
|---|---|---|
| 1960 | Endrinw | Toxic to fish and aquatic organisms |
| 1997 | Chlordane,w DDT,a dieldrin,b heptachlorw | Phasing out of persistent organic pollutants (POPs) |
| 1998 | Pyrethroidsb | Toxic to fish and aquatic organisms |
| Endosulfanb | Environmental concerns | |
| 2000 | Dichlorvos,b dicrotophos,b disulfoton,b ethyl parathion,b methyl parathion,b mercury compounds,b monocrotophos b phosphamidonb | Removal of all class Ia and Ib pesticides from agricultural use |
| 2004 | Methyl bromideb | Montreal protocol on Ozone Layer Depleting Substances (1987) |
| 2007 | Hexachlorobenzene,b mirex,b toxapheneb | Stockholm Treaty on Persistent Organic Pollutants (2001) |
aRestricted use only permitted in vector control.
bBanned for use on rice and other lowland crops.
WWithdrawn for all uses.
Correlation between regulations on pesticides and case fatalities in hospitals
To reflect the active implementation of pesticide legislation in late 1990s, we compared data for indicators of pesticide poisoning up to and after 2000 (date of the key ban of the most toxic WHO Class I toxicity HHPs, Table 2) using data from the literature.15 There was a 37.1% [95% confidence interval (CI) 35.4 to 38.8%] relative reduction in case fatality from pesticide poisoning, falling from 413/2719 (15.1%, 95% CI 13.9 to 16.6%) in the years up to 2000 to 315/3296 (9.5%, 95% CI 8.6 to 10.6%) after 2001 (P < 0.0001). No difference in rate of hospital admission for pesticide poisoning or the proportion of self-poisoning cases using pesticides was noted (Table 2).
Table 2.
Comparison of common pesticide poisoning indicators pre- and post-bans of HHPs15
| Indicators | Time frame |
P-value | |
|---|---|---|---|
| 1970 to 2000 | 2001 to 2014 | ||
| Poisoning cases as a proportion of total admissions (%) | 3.4 (n = 1737) | 7.1 (n = 6456) | <0.001 |
| Pesticide poisoning admission rate (per 100 000/year) | 2.9a | 3.1 | 0.57 |
| Proportion of self-poisoning using pesticides (%) | 70.1 (n = 240) | 72.2 (n = 5316) | 0.40 |
| In-hospital case fatality from pesticide poisoning (%) | 15.1 (n = 413) | 9.5 (n = 315) | <0.001 |
aData for the period 1988 to 2000.
Influence of pesticide regulation on pesticide suicides
From 1996 to 2014, the Bangladesh Police Statistics Department recorded 311 208 unnatural deaths. Intentional pesticide self-poisoning was the most common cause of suicidal death, being responsible for 115 423 [37.1%, 95% confidence interval (CI) 36.9% to 37.3%] of these deaths. Hanging and other causes of unnatural death were responsible for 95 063 (30.5%, 95% CI 30.4 to 30.7%) and for 100 722 (32.4%, 95% CI 32.2 to 32.5%) deaths, respectively. These proportions changed over time: in 1996, 44.7% of unnatural deaths were due to pesticide suicides compared with 20.9% in 2014. Hanging and other causes of unnatural deaths increased from 25.2% and 30.1% in 1996 to 40.1% and 38.9% in 2014, respectively.
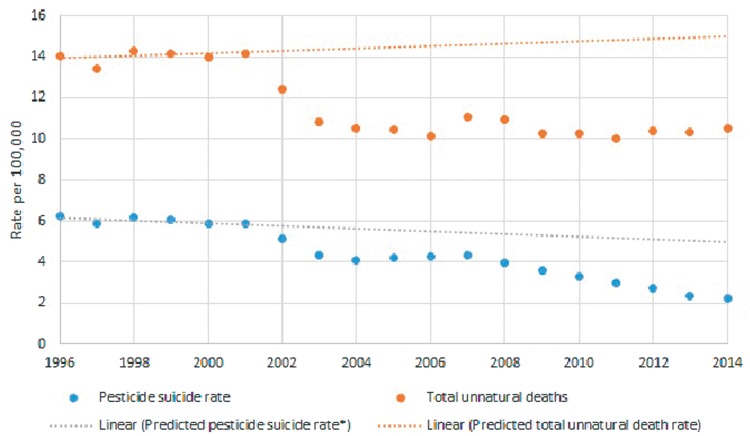
Before 2000, the rates of all causes of unnatural death were fairly constant, except for hanging suicides which appear to have increased over this time (Figure 1). From 2002 onwards, there was a sharp decline in the pesticide suicide death rate, as well as a decline in hanging suicides and other causes of unnatural death. The decline in pesticide suicides continued until 2005, at which point there was a slight rise followed by a decline from 2008 onwards. The fall in hanging suicides continued from 2000 until 2003 when the rate plateaued before steadily rising from 2011 onwards (Figure 1). The mortality rate due to other causes of unnatural deaths fell between 2000 and 2006 before increasing from 2007 onwards.
Figure 1.
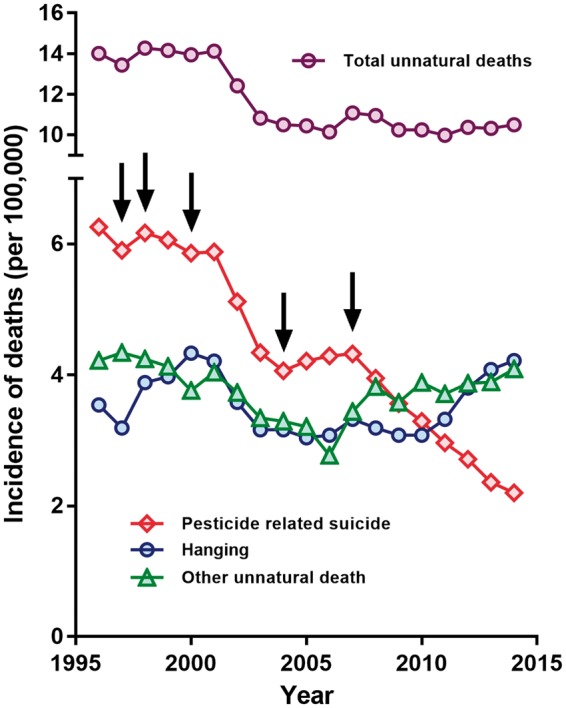
Trends of unnatural deaths in Bangladesh 1996 to 2014. The arrows mark the timing of national pesticide regulation, see Table 1 for timing of the bans. Suicides not using either pesticides or hanging are included in the ‘Other unnatural death’ category.
The incidence of pesticide suicides declined by 65.1% (95% CI 52.0 to 76.7%) over this period, from 6.3/100 000 in 1996 to 2.2/100 000 in 2014 (Figure 1). At the same time, there was a 20.0% (95% CI 8.4 to 36.9%) increase in the incidence of hanging from 3.5/100 000 in 1996 to 4.2/100 000 in 2014, and a 2.4% (95% CI 0.1 to 12.6%) decrease in other causes of unnatural death from 4.2/100 000 in 1996 to 4.1/100 000 in 2014. The incidence of all unnatural deaths fell by 25.0% (95% CI 18.1 to 33.0%), from 14.0/100 000 in 1996 to 10.5/100 000 in 2014.
The pesticide suicide rate was lower in each post-ban year (2001–14) than would be expected based on previous trends (1996 2000) (Table 3 and Figure 2). We estimate that in the post-ban years there were 35 071 (95% CI 25 959 to 45 666) fewer pesticide suicide deaths than predicted based on trends between 1996 and 2000. There was also evidence of a decline in total unnatural deaths in the post-ban years, with an estimated 76 642 (95% CI 53 493 to 103 161) fewer unnatural deaths. Our sensitivity analyses, which altered the start of the post-ban period from 2000 to 1999 and 2001, showed results consistent with our primary analysis (Table 4).
Table 3.
Rate ratios and change in the number of pesticide suicides and total unnatural deaths in years 2001–14, after ban of WHO class I pesticides, relative to those expected based on pre-band trend 1996–2000
| Pesticide suicides |
Unnatural deaths |
|||||
|---|---|---|---|---|---|---|
| Rate ratio (95% CI) | P-values | Change in number of suicides (95% CI) | Rate ratio (95% CI) | P-values | Change in number of deaths (95% CI) | |
| Post ban yearsa | ||||||
| 2001 | 1.00 (0.98, 1.03) | 0.79 | 28 (−179, 229) | 1.00 (0.98, 1.02) | 0.93 | −21 (−471, 419) |
| 2002 | 0.88 (0.85, 0.91) | <0.001 | −919 (−1198, −649) | 0.87 (0.85, 0.90) | <0.001 | −2421 (−3039, −1823) |
| 2003 | 0.76 (0.72, 0.79) | <0.001 | −1938 (−2297, −1595) | 0.76 (0.73, 0.79) | <0.001 | −4764 (−5571, −3988) |
| 2004 | 0.71 (0.68, 0.75) | <0.001 | −2277 (−2719, −1858) | 0.73 (0.70, 0.77) | <0.001 | −5379 (−6391, −4416) |
| 2005 | 0.75 (0.70, 0.80) | <0.001 | −2008 (−2536, −1513) | 0.73 (0.69, 0.77) | <0.001 | −5624 (−6852, −4465) |
| 2006 | 0.77 (0.72, 0.83) | <0.001 | −1830 (−2444, −1258) | 0.70 (0.66, 0.75) | <0.001 | −6236 (−7690, −4876) |
| 2007 | 0.79 (0.72, 0.86) | <0.001 | −1714 (−2417, −1067) | 0.76 (0.71, 0.82) | <0.001 | −5025 (−6715, −3460) |
| 2008 | 0.73 (0.66, 0.80) | <0.001 | −2196 (−2988, −1475) | 0.75 (0.69, 0.82) | <0.001 | −5358 (−7291, −3583) |
| 2009 | 0.66 (0.60, 0.73) | <0.001 | −2721 (−3603, −1926) | 0.70 (0.64, 0.77) | <0.001 | −6624 (−8811, −4634) |
| 2010 | 0.62 (0.55, 0.69) | <0.001 | −3078 (−4052, −2209) | 0.70 (0.63, 0.77) | <0.001 | −6738 (−9191, −4529) |
| 2011 | 0.56 (0.50, 0.64) | <0.001 | −3526 (−4593, −2583) | 0.68 (0.60, 0.76) | <0.001 | −7320 (−10048, −4885) |
| 2012 | 0.52 (0.45, 0.60) | <0.001 | −3877 (−5039, −2861) | 0.70 (0.62, 0.79) | <0.001 | −6899 (−9915, −4233) |
| 2013 | 0.46 (0.40, 0.53) | <0.001 | −4382 (−5640, −3293) | 0.69 (0.61, 0.79) | <0.001 | −7162 (−10478, −4258) |
| 2014 | 0.43 (0.37, 0.50) | <0.001 | −4605 (−5961, −3443) | 0.70 (0.61, 0.81) | <0.001 | −7071 (−10698, −3924) |
aCompared with pre-ban trend 1996–2000.
Figure 2.
Rates of pesticide suicides and unnatural deaths in 1996–2014, with predicted line based on trend in 1996 2000.
Table 4.
Sensitivity analysis changing the post-ban period from 2001–14 to 2000–14 and 2002–14
| Pesticide suicides rate ratio (95% CI) |
Unnatural deaths rate ratio (95% CI) |
|||
|---|---|---|---|---|
| Start of ban |
Start of ban |
|||
| 1999 | 2001 | 1999 | 2001 | |
| Post ban years | ||||
| 2000 | 0.97 (0.95, 1.00) | 0.98 (0.95, 1.00) | ||
| 2001 | 0.98 (0.95, 1.02) | 0.98 (0.95, 1.01) | ||
| 2002 | 0.86 (0.82, 0.90) | 0.88 (0.87, 0.90) | 0.85 (0.81, 0.89) | 0.88 (0.86, 0.89) |
| 2003 | 0.73 (0.69, 0.78) | 0.75 (0.73, 0.77) | 0.74 (0.70, 0.78) | 0.76 (0.74, 0.78) |
| 2004 | 0.69 (0.64, 0.74) | 0.71 (0.69, 0.74) | 0.71 (0.66, 0.76) | 0.73 (0.71, 0.76) |
| 2005 | 0.72 (0.66, 0.79) | 0.75 (0.72, 0.78) | 0.70 (0.64, 0.76) | 0.73 (0.70, 0.75) |
| 2006 | 0.74 (0.66, 0.82) | 0.77 (0.73, 0.81) | 0.67 (0.61, 0.74) | 0.70 (0.67, 0.73) |
| 2007 | 0.75 (0.66, 0.84) | 0.78 (0.74, 0.83) | 0.73 (0.65, 0.81) | 0.77 (0.73, 0.80) |
| 2008 | 0.69 (0.60, 0.78) | 0.72 (0.68, 0.77) | 0.71 (0.63, 0.80) | 0.75 (0.71, 0.80) |
| 2009 | 0.62 (0.54, 0.72) | 0.66 (0.61, 0.71) | 0.66 (0.58, 0.75) | 0.70 (0.66, 0.75) |
| 2010 | 0.58 (0.49, 0.68) | 0.61 (0.57, 0.66) | 0.65 (0.57, 0.76) | 0.70 (0.65, 0.75) |
| 2011 | 0.52 (0.44, 0.62) | 0.56 (0.51, 0.61) | 0.63 (0.54, 0.74) | 0.68 (0.63, 0.73) |
| 2012 | 0.48 (0.40, 0.58) | 0.52 (0.47, 0.57) | 0.65 (0.55, 0.77) | 0.70 (0.65, 0.76) |
| 2013 | 0.42 (0.35, 0.51) | 0.45 (0.41, 0.50) | 0.64 (0.53, 0.77) | 0.70 (0.63, 0.76) |
| 2014 | 0.39 (0.32, 0.49) | 0.43 (0.38, 0.48) | 0.65 (0.53, 0.79) | 0.70 (0.64, 0.78) |
Influence of pesticide regulation on rice production
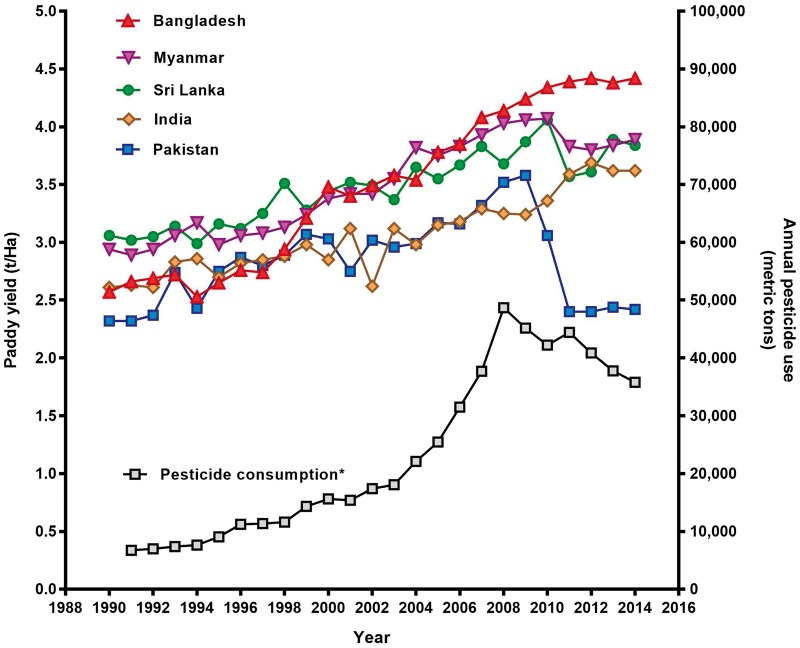
The main crop of Bangladesh is rice paddy, accounting for 75% of total agricultural land use and 80% of pesticide use.14 Comparing annual rice production in Bangladesh with production in India, Pakistan, Sri Lanka and Myanmar from 1996 to 2014 (Figure 3) revealed no apparent influence of the pesticide bans on crop production. Of note, overall pesticide, and insecticide, consumption increased for much of the period during which there was the rapid reduction in incidence of pesticide suicides.
Figure 3.
Risk factors for suicide
Although data were not complete for the whole period, we could not find evidence that the reduction in pesticide suicides was brought about by changes in employment, divorce or alcohol use rates. Unemployment levels varied between a minimum of 2.5% and a maximum of 5.0% of the total labour force between 1991 and 2014; levels were 2.5% in 1996 and 4.3% in 2014.19 The size of the work force in the agricultural sector also did not vary markedly during the study period. According to the World Bank, from 1984 to 2010, the percentage of total direct employment in the agricultural sector ranged from 48% to 66%.20 Since 2000, about 87% of rural households rely on agriculture for at least part of their income.29 The absolute number of the work force (aged 15+) was 36.0 million in 1995–96, increasing to 56.7 million in 2010.20
Available data suggest that the divorce rate increased only modestly in Bangladesh during this period: increasing among women and men from 0.95 to 1.22/1000 and 0.29 to 0.40/1000, between 2002 and 2010, respectively.21 Alcohol consumption is also increasing in Bangladesh but is still low compared with global use, with an estimated 1.9% (95% CI 1.7 to 2.1) of the population using alcohol [men: 3.6% (95% CI 3.3 to 4.1), women 0.3% (95% CI 0.2–0.5)] in 2010.22,23 There are no data to suggest a significant change in alcohol misuse patterns at the same time as the marked fall in pesticide suicides in the 2000s; unfortunately, national data from before 2004 were not available.
Discussion
In this study, we assessed the association of pesticide regulations carried out in Bangladesh, in particular the ban of all WHO Class I toxicity HHPs in 2000, with changes in pesticide suicides and agriculture. We found that, although use of pesticides for self-poisoning remained steady over the past two decades, there were major 37.1%, 65.1% and 25.0% reductions in the case fatality for pesticide poisoning and incidence of pesticide suicides and total unnatural deaths, respectively. At the same time, we found no apparent influence on the production of rice paddy, the country’s key agricultural crop and food staple, as well as increased pesticide use. We found no indication that changes in known contributors to suicide rates—unemployment, alcohol misuse or divorce30—had changed significantly during this period.
Legislative removal of the most hazardous pesticides from agricultural practice by the Bangladeshi Government is the most likely reason for these effects, as has been noted previously in Sri Lanka31,32 and South Korea.33 In the 14 years following the pesticide regulations in 2000, there were 35 000 fewer suicides by pesticide poisoning than expected based on trends between 1996 and 2000; this is a similar number to the tens of thousands of suicides that pesticide regulation prevented in Sri Lanka after 1995.34 The chronological association between pesticide legislation and reductions in pesticide suicide are not so clear in Bangladesh as they were in Sri Lanka, but the trend is clear. The difference is likely due to the comparative ease of controlling pesticide imports and use in an island like Sri Lanka compared with Bangladesh with its multiple land borders across which imports may cross.
The lack of an association with changes in paddy yield is important, since a detrimental effect on agricultural costs and yields is the major concern with pesticide legislation for HHPs. The data from Bangladesh add to the supportive data from both Sri Lanka35 and South Korea,33 indicating that careful pesticide legislation can reduce suicides without clearly affecting agricultural output.
China and Taiwan have also seen marked reductions in suicide rates from pesticide poisoning;36–38 however, these reductions may have been more associated with urbanization and reduction in the agricultural work force than pesticide regulation.36,39,40
Hospital-based studies have shown that, from 2005 onwards, the majority of poisoning admissions in Bangladesh have been due to a mixture of Class II and Class III products rather than the previously common WHO class I pesticides.15 At present, the WHO class III insecticide malathion is the commonest agent used for self-poisoning.15 The in-hospital mortality from pesticide poisoning in Bangladesh after the legislation was found to be 37% lower than before the bans. We hypothesize that this is due to the resulting reduced toxicity of pesticides taken in self-harm; however, bans of highly hazardous pesticides with switches to moderately but still toxic pesticides can actually result in more patients dying in hospital, since the former often resulted in people dying quickly, before presentation to health services.41 It is also possible that the reduced case fatality was due to increased awareness among physicians of how to treat these patients, increased local research on pesticide poisoning management,42,43 the publication and use of national guidelines for poisoning management in 200544 and/or better management of admitted patients. However, there is no evidence of a consistent marked improvement in the management of pesticide-poisoned patients during this period. The lack of adequate training for physicians, a shortage of antidotes and a lack of intensive care unit (ICU) facilities means that moderate-to-severe pesticide poisoning remains a challenging issue in Bangladesh.15
National representative data on the annual incidence of suicides in Bangladesh are not yet available. We therefore used police data collected from whole country only for this report. In 2001, the WHO estimated the national suicide rate to have been 8/100 000 in 1972–88 and 10/100 000 in 1992–93.45 More recently, the WHO estimated the national suicide rate to be 6.6/100 000 in 2012.4 A cross-sectional study in 2003 of a population of 819 429 found a suicide rate of 7.3 (95% CI 5.6 to 9.5) per 100 000 per year.46 These estimates are similar to the estimated incidence in police data presented here of 10.4/100 000 for all unnatural deaths, including at least 6.51/100 000 suicides (hanging + pesticide poisoning). It is surprising that non-suicide injury deaths in Bangladesh are estimated to be as low as 4/100 000 per year. It is possible that these injuries are not all reported to the police.
Suicide rates are likely to be higher in rural areas.47,48 Studies in rural Jessore district49 and Matlab upazila (sub-district) of Chandpur district50 found rates of 39/100 000 during 1983–2002, and 13/100 000 in women and 8/100 000 per year in men in 1982–98, respectively. The large cross-sectional study reported above found suicide rates to be 17-fold higher (95% CI 5.4 to 54.6) in the rural population, compared with urban rates.46 This is likely to be due to the easy availability of pesticides in these rural communities, as well other characteristics of rural life.
Limitations
Our study is based on data from the police statistics division, which have not been validated against other sources of information on suicides. Since suicide is a crime in Bangladesh, it is likely to be under-reported, lowering the absolute rates but probably not affecting the rates over time. Absence of age- and sex-specific stratified suicide records was a limitation of the analysed data. Data for many of the risk factors were only available for some of the period under study, and so it was not possible to completely rule out the role of other risk factors.
Conclusions
Removal of HHPs from agricultural practice by government legislation was associated with a marked reduction in suicide by pesticide poisoning, without affecting agricultural outputs. Widespread global adoption of this practice will rapidly reduce global suicide numbers, by preventing nearly all pesticide suicides. The data presented here add to data already collected from Sri Lanka and South Korea.
Supplementary Data
Supplementary data are available at IJE online.
Funding
DK is an Economic and Social Research Council (U.K) postdoctoral fellow (ES/P009735/1).
Supplementary Material
Acknowledgements
We acknowledge Mr M Nazem Ahmed, Additional Superintendent of Police, Bangladesh Police Headquarters, for his relentless effort to gather the suicide data. We also thank Mr Mohammad Habibullah, Stewardship Manager, and Mr Mohammad Ahsan Kabir, Manager, Registration and Regulatory Affairs, Syngenta Bangladesh Ltd, for data on pesticide consumption and timing of pesticide bans.
Conflict of interest: D.G. was during 2003–11 a member of scientific advisory groups for Syngenta-funded studies to assess the toxicity of a new paraquat formulation, a pesticide storage project, and medical management of paraquat poisoning; he received travel costs to attend research meetings but no other fees. He was an expert adviser to WHO’s First Consultation on Best Practices on Community Action for safer access to pesticides [Geneva (2006)]. The other authors have no conflicts of interest.
References
- 1. Eddleston M. Patterns and problems of deliberate self-poisoning in the developing world. Q J Med 2000;93:715–31. [DOI] [PubMed] [Google Scholar]
- 2. Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: systematic review. BMC Public Health 2007;7:357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. Public Health Impact of Pesticides Used in Agriculture. Geneva: WHO, 1990. [Google Scholar]
- 4. World Health Organization. Preventing Suicide. A Global Imperative. Geneva: WHO, 2014. [Google Scholar]
- 5. Mew EJ, Padmanathan P, Konradsen F, et al. The global burden of fatal self-poisoning with pesticides 2006–15: Systematic review. Affect Disord 2017;219:93–104. [DOI] [PubMed] [Google Scholar]
- 6. Eddleston M, Karunaratne A, Weerakoon M, et al. Choice of poison for intentional self-poisoning in rural Sri Lanka. Clin Toxicol 2006;44:283–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weerasinghe M, Pearson M, Peiris R, et al. The role of private pesticide vendors in preventing access to pesticides for self-poisoning in rural Sri Lanka. Inj Prev 2013;20:134–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eddleston M, Karalliedde L, Buckley N, et al. Pesticide poisoning in the developing world – a minimum pesticides list. Lancet 2002;360:1163–67. [DOI] [PubMed] [Google Scholar]
- 9. Food and Agriculture Organization of the United Nations. International Code of Conduct on Pesticide Management. Guidelines on Highly Hazardous Pesticides. Rome: FAO, 2016. [Google Scholar]
- 10. Konradsen F, van der Hoek W, Cole DC, et al. Reducing acute poisoning in developing countries – options for restricting the availability of pesticides. Toxicology 2003;192:249–61. [DOI] [PubMed] [Google Scholar]
- 11. World Health Organization. Guns, Knives, and Pesticides: Reducing Access to Lethal Means. (Series of briefings on violence prevention: the evidence). Geneva: WHO, 2009. [Google Scholar]
- 12. World Bank. Bangladesh Country Data – Population. Washington, DC: World Bank, 2016. [Google Scholar]
- 13. Mohajan HK. Food, agriculture and economic situation of Bangladesh. Proceedings of the 2nd International Conference on Global Sustainable Development (2nd ICGSD-2013), 5–6 October 2013. Karachi: KASBIT, 2013. [Google Scholar]
- 14. Matin MA. Pesticides in Bangladesh. In: Taylor MD, Klaine SJ, Carvalho FP, Barcelo D, Evaraarts J (eds). Pesticide Residues in Coastal Tropical Ecosystems: Distribution, Fate and Effects. London and New York: Taylor & Francis, 2003. [Google Scholar]
- 15. Dewan G. Analysis of recent situation of pesticide poisoning in Bangladesh: Is there a proper estimate? Asia Pac J Med Toxicol 2014;3:76–83. [Google Scholar]
- 16. Chowdhury FR, Rahman AU, Mohammed FR, Chowdhury A, Ahasan HA, Bakar MA. Acute poisoning in southern part of Bangladesh – the case load is decreasing. Bangladesh Med Res Counc Bull. 2011;37(2):61–5. [DOI] [PubMed] [Google Scholar]
- 17. Director General of Health Services, Ministry of Health and Family Welfare, Government of Bangladesh. Health Bulletin; Dhaka; 2014. [Google Scholar]
- 18. International Classification of Diseases Geneva: World Health Organization; 1990 (Available from: http://www.who.int/classifications/icd/en/.
- 19. World Bank. Unemployment, total (% of total labor force) (modeled ILO estimate) World bank; 2016 (updated 04/11/2016. Available from: http://data.worldbank.org/indicator/SL.UEM.TOTL.ZS?end=2014&locations=BD&start=1991&view=chart.
- 20. Employment in agriculture (% of total employment): The World Bank; 2016 (Available from: http://data.worldbank.org/indicator/SL.AGR.EMPL.ZS?end=2010&locations=BD&start=1984&view=chart&year_low_desc=false.
- 21. Bangladesh Bureau of Statistics, Statistics and Informatics, Division Ministry of Planning. Gender statistics of Bangladesh 2012. Dhaka: 2013. [Google Scholar]
- 22. World Health Organization. Global status report on alcohol and health, 2014. Geneva: World Health Organization; 2014. [Google Scholar]
- 23. Dewan G, Chowdhury FR. Alcohol use and alcohol use disorders in Bangladesh. Asia Pac J Med Toxicol. 2015;4:83–90. [Google Scholar]
- 24. International Rice Research Institute. World Rice Statistics Online Query Facility: IRRI; 2016 (Available from: http://ricestat.irri.org:8080/wrsv3/entrypoint.htm.
- 25. Statistical Division, Food and Agricultural Organization of the United Nations (FAO). Food and agriculture data Rome: FAO; 2016 (Available from: http://www.fao.org/faostat/en/#home.
- 26. Parveen S, Nakagoshi N. An analysis of pesticide use for rice pest management in Bangladesh. J Int Dev Coop 2001;8:107–26. [Google Scholar]
- 27. World Health Organization. The WHO Recommended Classification of Pesticides by Hazard and Guidelines to Classification: 2009. Geneva: WHO;,2010. [Google Scholar]
- 28. Knipe DW, Chang SS, Dawson A, et al. Suicide prevention through means restriction: Impact of the 2008–2011 pesticide restrictions on suicide in Sri Lanka. PloS One 2017;12:e0172893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. World Bank. Bangladesh: Growing the Economy Through Advances in Agriculture. Washington, DC: World Bank, 2016. [Google Scholar]
- 30. Gunnell DJ. Time trends and geographical differences in suicide: implications for prevention. In: Hawton K. (ed). Prevention and Treatment of Suicidal Behaviour: From Science to Practice. Oxford, UK: OUP, 2005. [Google Scholar]
- 31. Gunnell D, Fernando R, Hewagama M, Priyangika WDD, Konradsen F, Eddleston M. The impact of pesticide regulations on suicide in Sri Lanka. Int J Epidemiol 2007;36:1235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Knipe DW, Metcalfe C, Fernando R, et al. Suicide in Sri Lanka 1975–2012: age, period and cohort analysis of police and hospital data. BMC Public Health 2014;14:839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cha ES, Chang SS, Gunnell D, Eddleston M, Khang YH, Lee WJ. Impact of paraquat regulation on suicide in South Korea. Int J Epidemiol 2016;45:470–79. [DOI] [PubMed] [Google Scholar]
- 34. Knipe DM, Gunnell D, Eddleston M. Preventing deaths from pesticide self-poisoning - learning from Sri Lanka's remarkable success. Lancet Glob Health 2017;5:e651–52. [DOI] [PubMed] [Google Scholar]
- 35. Manuweera G, Eddleston M, Egodage S, Buckley NA. Do targeted bans of insecticides to prevent deaths from self-poisoning result in reduced agricultural output? Environ Health Perspect 2008;116:492–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chang SS, Lu TH, Eddleston M, et al. Factors associated with the decline in suicide by pesticide poisoning in Taiwan: a time trend analysis, 1987–2010. Clin Toxicol 2012;50:471–80. [DOI] [PubMed] [Google Scholar]
- 37. Liu S, Page A, Yin P, et al. Spatiotemporal variation and social determinants of suicide in China, 2006–2012: findings from a nationally representative mortality surveillance system. Psychol Med 2015;45:3259–68. [DOI] [PubMed] [Google Scholar]
- 38. Page A, Liu S, Gunnell D, et al. Suicide by pesticide poisoning remains a priority for suicide prevention in China: Analysis of national mortality trends 2006–2013. J Affect Disord 2016;208:418–23. [DOI] [PubMed] [Google Scholar]
- 39. Chang SS, Lu TH, Sterne JA, Eddleston M, Lin JJ, Gunnell D. The impact of pesticide suicide on the geographic distribution of suicide in Taiwan: a spatial analysis. BMC Public Health 2012;12:260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wang Z, Wang J, Bao J, Gao X, Yu C, Xiang H. Temporal trends of suicide mortality in mainland China: results from the age-period-cohort framework. Int J Environ Res Public Health 2016;13:784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Roberts DM, Karunarathna A, Buckley NA, Manuweera G, Sheriff MHR, Eddleston M. Influence of pesticide regulation on acute poisoning deaths in Sri Lanka. Bull World Health Organ 2003;81:789–98. [PMC free article] [PubMed] [Google Scholar]
- 42. Abedin MJ, Sayeed AA, Basher A, Maude RJ, Hoque G, Faiz MA. Open-label randomized clinical trial of atropine bolus injection versus incremental boluses plus infusion for organophosphate poisoning in Bangladesh. J Med Toxicol 2012;8:108–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Basher A, Rahman SH, Ghose A, Arif SM, Faiz MA, Dawson AH. Phase II study of magnesium sulfate in acute organophosphate pesticide poisoning. Clin Toxicol 2013;51:35–40. [DOI] [PubMed] [Google Scholar]
- 44. Hospital Services Management, Directorate General of Health Services. Management of Acute Poisoning. A Practical Manual. Dhaka: Directorate General of Health Services, 2005. [Google Scholar]
- 45. World Health Organization, Regional Office for South East Asia. Suicide Prevention: Emerging from Darkness. New Delhi: SEARO, 2001. [Google Scholar]
- 46. Mashreky SR, Rahman F, Rahman A. Suicide kills more than 10,000 people every year in Bangladesh. Arch Suicide Res 2013;17:387–96. [DOI] [PubMed] [Google Scholar]
- 47. Hadi A. Risk factors of violent death in rural Bangladesh, 1990–1999. Death Stud 2005;29:559–72. [DOI] [PubMed] [Google Scholar]
- 48. Eddleston M, Phillips MR. Self poisoning with pesticides. BMJ 2004;328:42–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. International Centre for Diarrhoeal Disease Research, Bangladesh. Mortality due to suicide in rural Bangladesh. ICDDR,B Health and Science Bulletin 2003;1:7–10. [Google Scholar]
- 50. Ahmed MK, van Ginneken J, Razzaque A, Alam N. Violent deaths among women of reproductive age in rural Bangladesh. Soc Sci Med 2004;59:311–19. [DOI] [PubMed] [Google Scholar]
- 51. Bangladesh Bureau of Statistics. Statistical Yearbook of Bangladesh – 2010. Dhaka: Ministry of Planning, 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.