Abstract
Background
Mexicans and US Mexican Hispanics share modifiable determinants of premature mortality. We compared trends in mortality at ages 30–69 in Mexico and among US Mexican Hispanics from 1995 to 2015.
Methods
We examined nationally representative statistics on 4.2 million Mexican and 0.7 million US deaths to examine cause-specific mortality. We used lung cancer indexed methods to estimate smoking-attributable deaths stratified by high and lower burden Mexican states.
Results
In 1995–99, Mexican men had about 30% higher relative risk of death from all causes than US Mexican Hispanic men, and this difference nearly doubled to 58% by 2010–15. The divergence between Mexican and US Mexican Hispanic women over this time period was less marked. Among US Mexican Hispanics, declines in the risk of smoking-attributable death constituted about 25–30% of the declines in the overall risk of death. However, among Mexican men the declines in the risk of smoking-attributable deaths were offset by increases in causes of death not due to smoking. Homicide rates (mostly from guns) rose among men in Mexico from 2005 to 2010, but not among Mexican women or US Mexican Hispanic men or women. The probability at 30–69 years of death from cardiac disease diverged significantly between Mexicans and US Mexican Hispanics, reaching 10% and 5% for men, and 7% and 2% for women, respectively.
Conclusions
Large differences in premature mortality between otherwise genetically and culturally similar groups arise from a few modifiable factors, most notably smoking, untreated diabetes and homicide.
Keywords: Mortality, smoking-attributable deaths, vascular, homicide, trends, Mexican, US Mexican Hispanic
Introduction
Global life expectancy is currently about 71 years, up from about 56 years in 1970. There has been widespread and rapid progress in reducing mortality before age 30 years, mostly due to substantial declines in childhood mortality since 1970. However, mortality declines in middle age (which we define in this paper as 30–69 years) have been slower over the same time period.1
In many populations, middle-age mortality is becoming relatively more important as child mortality decreases and the effects of smoking and other risk factors increase.2 Mexico is a country that has rapidly reduced premature childhood and early adult mortality. Progress in reducing mortality in middle age requires understanding the impact of changing risk factors, and changing coverage of health services.3,4 The 50 million Mexicans aged 30–69 years share common genetic, cultural, dietary and other lifestyle exposures with the 24 million US Mexican Hispanics (comprising US-born and foreign-born Hispanics of Mexican origins) of the same ages. In both populations, the main causes of premature mortality at 30–69 years are vascular, respiratory and neoplastic disease, each of which can be made more common by smoking.5,6 Over the past decade, smoking prevalence has declined modestly in Mexico7,8 and among US Mexican Hispanic populations.9 Still, about 30% of adult Mexican men smoke, which exceeds the prevalence among US Mexican Hispanics (or indeed among US non-Hispanic White men).10 About 10% percent of Mexico’s adult women smoke, which is similar to US Mexican Hispanic women.7–9 Mexicans smoke fewer cigarettes than US Mexican Hispanic, but have similar ages of initiation. Adiposity, particularly leading to diabetes that remains untreated, is an important cause of vascular deaths.11,12 Adiposity levels are notably high in Mexican and US Mexican Hispanic adults (compared with US Whites) and have risen in recent decades.13
Mortality patterns are influenced by untreated or poorly treated diabetes,14 in some Mexican states by homicide (mostly arising from gun violence),15 by expansion of health insurance in Mexico and by the introduction of the Affordable Care Act in the USA.16 Here we examine and contrast trends in overall mortality, vascular mortality, smoking-attributable mortality and homicide mortality in Mexico and among US Mexican Hispanics from 1995 to 2015. Our goal was to elucidate the convergence and divergence in overall and cause-specific mortality, as well as in the important factors for premature adult mortality. Specifically, we apply indirect methods indexed on absolute lung cancer mortality to quantify smoking risks, and examine trends in specific causes of death made particularly more common by untreated diabetes.
Methods
Death rates nationally, by state and ethnicity
We obtained age, sex, race/ethnicity (non-Hispanic Whites and Mexican Hispanics) and disease-specific mortality data for the USA from the National Center for Health Statistics Multiple Cause of Death Files17 and similar data for Mexico from the National Institute of Geography and Statistics.18 Causes of death were based on the routine medically certified death certificates, coded to the ninth or tenth revision of the International Classification of Diseases (ICD).19 Nearly 100% of deaths in the USA and Mexico are medically certified. We used population denominators for US Mexican Hispanics from the Current Population Surveys before 2000 and subsequently from the American Community Surveys,20,21 and for Mexico from the Mexican Population Council.22 We focus on deaths at ages 30–69 years, as the causes of death are better classified in middle age than in old age,23 and as these deaths are more avoidable than are deaths in older age.1 To avoid annual fluctuations, we present smoothed averages for 1995–99, 2000–04, 2005–09 and 2010–15.
Indirect estimation of smoking-attributable mortality
In countries without direct epidemiological studies about the effects of smoking on adult mortality, the approximate contribution of smoking to adult mortality can be estimated indirectly from the disease-specific death rates in that population, using the absolute lung cancer rates to indicate the proportions due to smoking of the mortality from other diseases strongly attributable to smoking (lung and other cancers, vascular disease, respiratory disease, other medical conditions affected by smoking, as defined earlier).24–26 The main requirements are near universal registration and medical certification of the causes of all deaths, along with sufficient levels of lung cancer mortality so as to use their absolute rates (after subtracting the expected rates of lung cancer among non-smokers) as an index of exposure. These indirect methods have the advantage of not requiring any knowledge of current or past smoking patterns in the target population.
We first calculated the absolute age-specific lung cancer rates at ages 30–69 years for each gender for US Whites and US Mexican Hispanics, and for Mexico nationally and separately for 13 states where smoking risks are higher and more prolonged.27,28 The average age-standardized lung cancer mortality rates from 1995 to 2015 in these states exceeded the national average in Mexico (18.9 and 8.3 deaths per 100 000 men or women, respectively). These ‘high-burden states’ are in descending order of population: Jalisco, Nuevo León, Chihuahua, Tamaulipas, Baja California, Sinaloa, Coahuila, Sonora, Durango, Aguascalientes, Nayarit, Colima, Baja California Sur). The remaining states are ‘low-burden states’ (eFigure 1 in the Supplementary data, available at IJE online).
Second, for each of these populations we matched their lung cancer rates to the lung cancer rates in a mixture of smokers and non-smokers in a large prospective study conducted in the 1980s of 1 million Americans.29 We subtracted the stable rates of lung cancer not due to smoking in the American prospective study (averaging about 8 deaths per 100 000 non-smokers).
Third, we applied the mortality rates in such a mixture of smokers and non-smokers from various other causes of death (upper aero-digestive cancer, other cancer, chronic obstructive lung disease, other respiratory disease, vascular disease and diabetes, and certain other diseases; no deaths from cirrhosis or from non-medical causes are attributed to smoking) to estimate the smoking-attributed proportion of the mortality from those other diseases. This relied on application of the smoker: non-smoker relative risks for the major causes of death using the 2014 US Surgeon General’s Report (Table 12.3, page 658).30 Mexican coding conventions often assign cardiac deaths as diabetic deaths for the underlying cause,14 so we applied the same relative risks for both conditions, and retained this classification and relative risk procedure for US deaths. The death rate (R per 1000) is the simple mean of the rates in the eight 5-year age ranges. The 40-year risk of death is then 1–exp(–40 R/1000), assuming that observed death rates would apply to the population of 30-year-olds.
Lung cancer death rates in the low-burden Mexican states for women were close to the rates among never smokers in the US prospective study. Thus, the indirect method was unreliable in estimating smoking-attributable mortality among women in low-burden states of Mexico (and to a lesser extent among men in these states). Moreover, these low-burden states in South Mexico are mostly those with the highest proportion of exposure to small airborne particulate matter, in particular from wood smoke, that can also contribute to lung cancer, especially among women exposed during cooking.31 Thus, most of the analyses for both men and women focus on contrasting the burden in Mexico as a whole with high-burden states in Mexico and US Mexican Hispanics and Whites. We further compared smoking and ex-smoking prevalence and amount smoked, and age at initiation for specific birth cohorts of smokers (born in the 1940 s, 1950 s or 1960 s) from a nationally representative survey of smoking conducted in 2000 in Mexico7 and the ongoing US National Health Interview Survey.32
Cause-specific mortality trends
We analysed myocardial infarction, stroke, respiratory disease, all cancers, renal failure and homicides for cause-specific mortality trends. We pre-specified myocardial infarction and renal diseases as those conditions strongly linked to untreated adult-onset (i.e. ‘type 2’) diabetes, based on a recent prospective study in Mexico City.14 We excluded deaths due to acute diabetic crises, as these are more likely to reflect childhood-onset diabetes.
Results
We examined about 4.9 million individual death records at ages 30–69 years from 1995 to 2015; 4.2 million in Mexico and 0.7 million in the USA. The proportion of ill-defined cause at ages 30–69 provides a robust measure of the quality of medical certification.33 From 1995 to 2015, this proportion fell from 1.1% to 0.01% in the USA and from 1.2% to 0.6% in Mexico (with similar results across states with higher or lower lung cancer mortality; data not shown). Table 1 provides the summary statistics for the population and deaths from all causes, vascular disease, homicide and smoking in Mexico, in the subgroup of 13 high-burden states with higher lung cancer mortality and among US Mexican Hispanics. The high-burden Mexican states had about one-third of Mexico’s population, but constituted about three-fifths (3300/5500) of the male smoking deaths nationally at ages 30–69 years. By 2012, the smoking prevalence was similar in high and low lung cancer-burden states in Mexico among males and females, and male smoking prevalence was much higher in Mexico than among US Mexican Hispanics. In 2015, vascular deaths were a larger proportion of all deaths in Mexico than among US Mexican Hispanics in both sexes, and homicide was a larger proportion of male deaths in Mexico.
Table 1.
Selected descriptive characteristics of the study population age 30–69 years, Mexico and the United States, 1995–2015
| Mexico national | Mexico, high burden lung cancer statesa | Mexico, low burden lung cancer states | US Mexican Hispanic | |
|---|---|---|---|---|
| Men, aged 30–69 years | ||||
| Population 2015, millions | 23.9 | 7.9 | 16.0 | 7.5 |
| Deaths all causes 2015, thousands | 155.4 | 50.4 | 105.0 | 27.7 |
| Renal deaths 2015, thousands (% all deaths) | 3.3 (2.1%) | 1.0 (1.9%) | 2.3 (2.2%) | 0.5 (1.8%) |
| All vascular deaths 2015, thousands (% all deaths) | 52.9 (34.0%) | 17.3 (34.2%) | 35.6 (33.9%) | 7.6 (27.5%) |
| Homicide 2015, thousands (% all deaths) | 9.9 (6.4%) | 3.5 (6.9%) | 6.4 (6.1%) | 0.7 (2.5%) |
| Smoking deaths 2015, thousands (% all deaths) | 5.5 (3.6%) | 3.3 (6.6%) | 2.2 (2.1%) | 1.7(6.0%) |
| Lung cancer mortality ratesb per 100000, 1995–2015 | 18.9 | 31.8 | 13.2 | 27.4 |
| Number of smokers 2012, millions (prevalence %) | 6.4 (30.0%) | 2.1 (30.3%) | 4.3 (29.9%) | 1.8 (17.3%) |
| Women, aged 30–69 years | ||||
| Population 2015, millions | 26.7 | 8.4 | 18.2 | 7.2 |
| Deaths all causes 2015, thousands | 100.3 | 30.3 | 69.9 | 15.5 |
| Renal deaths 2015, thousands (% all deaths) | 2.9 (2.8%) | 0.8 (2.7%) | 2.0 (2.9%) | 0.4 (2.4%) |
| All vascular deaths 2015, thousands (% all deaths) | 38.3 (38.2%) | 11.1 (36.5%) | 27.2 (38.9%) | 3.7 (24.1%) |
| Homicide 2015, thousands (% all deaths) | 1.1 (1.1%) | 0.4 (1.2%) | 0.7 (1.0%) | 0.2 (1.0%) |
| Smoking deaths 2015, thousands (% all deaths) | n/ac | 0.8 (2.5%) | n/ac | 0.5 (3.4%) |
| Lung cancer mortality ratesb per 100000, 1995–2015 | 8.3 | 11.7 | 7.0 | 12.6 |
| Number of smokers 2012, millions (prevalence %) | 2.4 (9.7%) | 0.8 (11.5%) | 1.4 (8.8%) | 0.9 (8.0%) |
aHigh-burden states include: Jalisco, Nuevo León, Chihuahua, Tamaulipas, Baja California, Sinaloa, Coahuila, Sonora, Durango, Aguascalientes, Nayarit, Colima, Baja California Sur.
bRates are means of the age-specific rates for the eight 5-year age categories from 30 to 69 for the time period of 1995–2015.
cn/a, not available; real risk too low to estimate reliably.
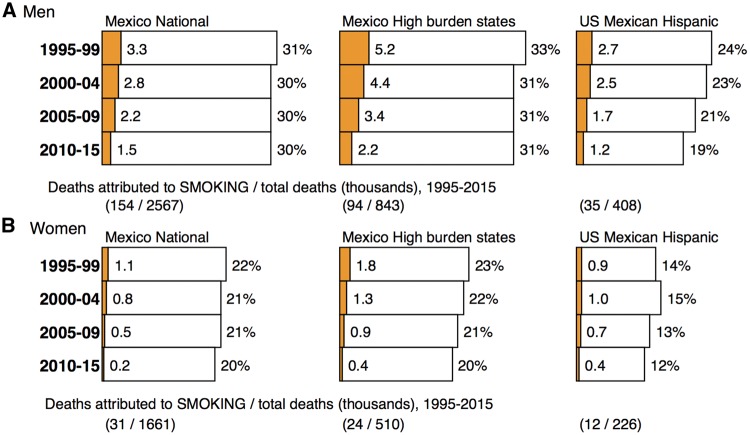
The overall risk of death at ages 30–69 years fell across the three populations and for each gender, but variably (Figure 1). Among US Mexican Hispanics, the overall risk of death fell in men by about 21% (5/24) and in women by about 14% (2/14). The US results for ages 30–69 years were similar if we excluded those aged 65–69 years who receive Medicare health insurance coverage (data not shown). By contrast, among Mexicans, the overall risk of death did not fall appreciably in men (3%, 1/31) or in women (9%, 2/22), with similar stagnation in the high-burden lung cancer states. In 1995–99, Mexican men had about 30% higher relative overall risk of death (31/24) than US Mexican Hispanic men, and this divergence nearly doubled to 58% by 2010–15 (30/19). The divergence between Mexican and US Mexican Hispanic women over this time period was less marked.
Figure 1.
Risk of a 30-year-old dying at ages 3069 from smoking (shaded) or from any cause (shaded and white) Mexico and the United States, 1995–2015. Mortality data for ages 30–69 were standardized to a uniform age distribution by averaging the age-specific death rates for the eight 5–year age groups within the 40-year age range. The death rate (R per 1000) in each 40-year age range is the mean of the rates in the eight 5–year age ranges. The 40–year risk of death is then 1-exp(-40R/1000).
There was convergence among the three male populations in the risks of smoking-attributable death from 1995 to 2015, which fell by about 55–58% in [for example 58% (3/5.2)] in Mexican high-burden states (Figure 1). In Mexican women, the risk of smoking-attributable death was smaller and reliably documented only in the high-burden states. In these states, the risk of smoking-attributable death fell by about three-quarters, from 1.8% to 0.4%. In US Mexican Hispanic women, the comparable risk was also small and fell by over half. Among US Mexican Hispanics, declines in the risk of smoking-attributable death constituted 30% (1.5/5) and 25% (0.5/2), respectively, of the declines in the overall risk of death in men and women. However, among Mexican men, the declines in the risk of smoking-attributable deaths were offset by increases in causes of death not due to smoking.
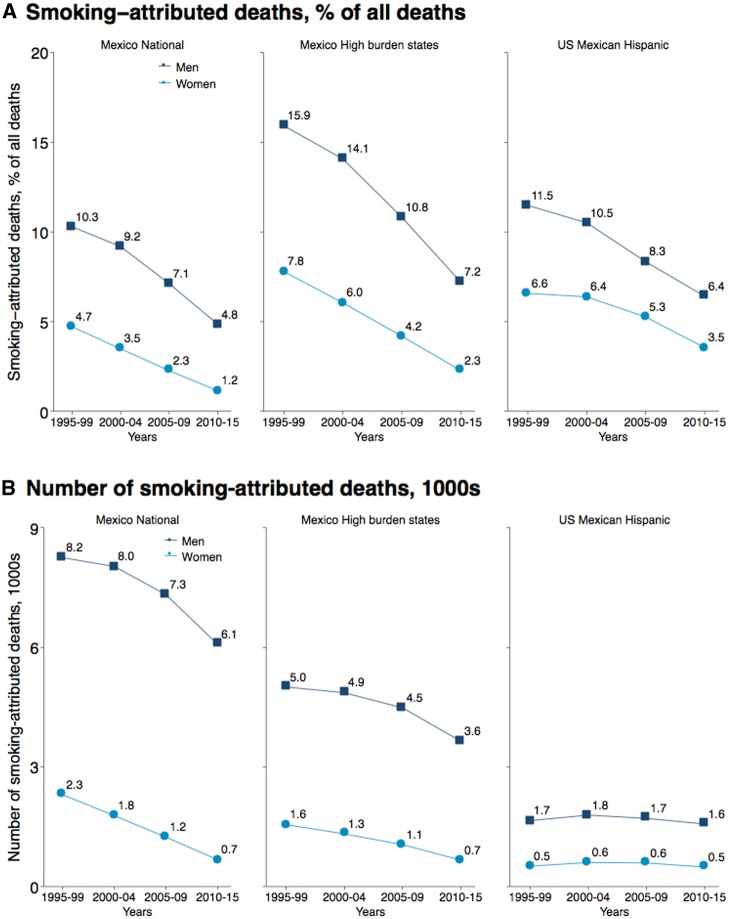
The proportion of all deaths at ages 30–69 years attributable to smoking fell substantially in all study populations, most dramatically among US Mexican Hispanic men from about 12% to 6%, among Mexican men in high-burden states from 16% to 7% and in Mexican men from10% to 5% (Figure 2). In 2015, smoking constituted 6%, 7% and 6% of all deaths in men aged 30–69 years in all Mexican states, in high-burden Mexican states and in US Mexican Hispanics, respectively. Among women at these same ages, smoking constituted 2% and 4% in high-burden Mexican states and in US Mexican Hispanics, respectively. The absolute numbers of smoking deaths at ages 30–69 years in Mexico fell modestly from about 8000 to 6000 in men and from 2000 to a few hundred in women over the two decades. By contrast, the absolute numbers of deaths due to smoking changed relatively little among US Mexican Hispanics, as there was a substantial increase in the population size.34
Figure 2.
Number of smoking-attributed deaths (1000s) and percentage of all deaths attributed to smoking-related causes in men and women at ages 30–69 in Mexico and the United States, 1995–2015.
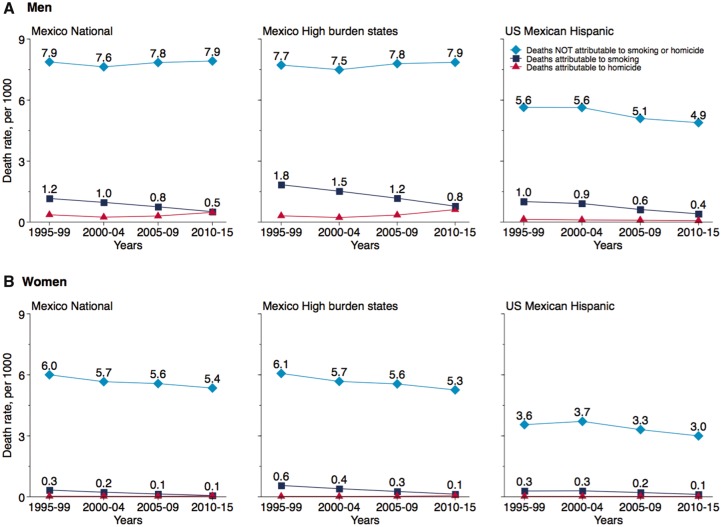
The methods of indexing relative cause-specific mortality with absolute lung cancer rates permit comparisons of the contribution of diseases not attributable to smoking with those attributable to smoking (Figure 3). Homicide rates rose among men in Mexico from 2005 to 2010 and in its high lung cancer-burden states, but not among Mexican women or US Mexican Hispanic men or women. About 60% of the male and 50% of the female homicides were gun-related (data not shown). The mortality rates not due to either smoking or homicide did not change appreciably in Mexico or its high lung cancer-burden states, but fell slowly among Mexican women and substantially among US Mexican men and women.
Figure 3.
Trends in age standardized all-cause mortality rates attributed to smoking and not attributed to smoking or homicide in men (A) and women (B) at ages 30-69 in Mexico and the United States, 1995-2015 Mortality data for ages 30-69 were standardized to a uniform age distribution by averaging the age-specific death rates for the eight 5-year age groups within the 40-year age range. ICD codes for homicide (ICD-9: 960 -969; ICD-10: X85 - Y09).
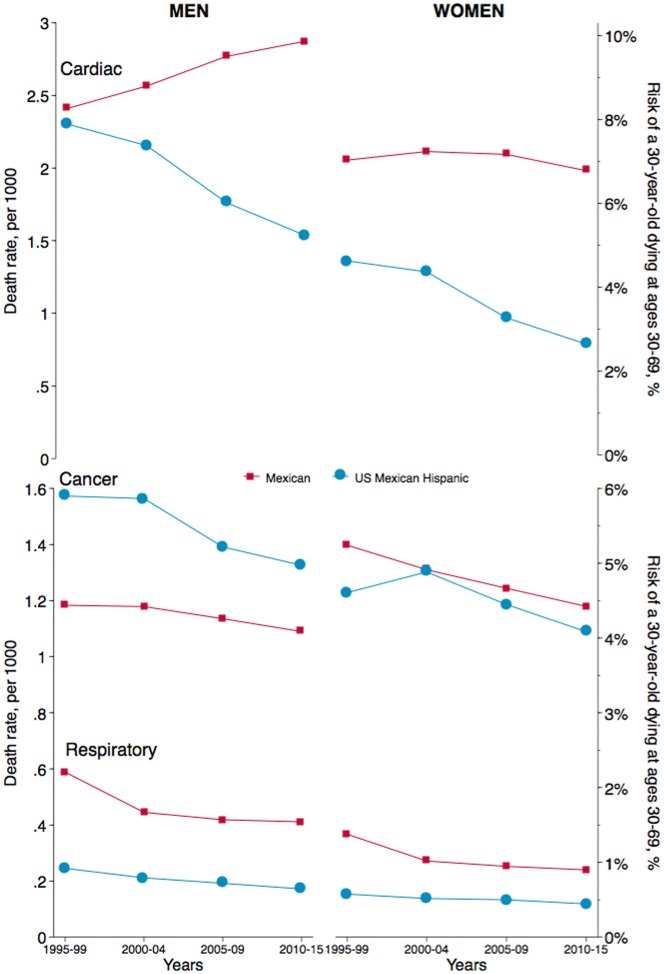
By 2010–15, the probability of a 30-year-old man dying by age 70 from cardiac disease diverged significantly between Mexicans and US Mexican Hispanics, reaching 10% and 5%, respectively (Figure 4). The comparable figures for Mexican and US Mexican Hispanic women were 7% and 2%, respectively. By contrast, in 1995–99, the mortality rates from cardiac disease among Mexican and US Mexican Hispanic men were similar. Stroke was a much less common cause of death in both countries, and fell modestly in all four comparison groups. Renal failure death was also less common, and fell modestly among each group except US Mexican Hispanic men, where it rose slightly (eFigure 2, available at IJE online). Cancer and respiratory mortality rates fell modestly among Mexican and US Mexican Hispanic men and women, with no divergence as seen as for cardiac disease.
Figure 4.
Cardiac, cancer and respiratory mortality rates and 40-year risks of death among men and women in Mexico and the United States, 1995–2015. The death rate (R per 1000) in each 40-year age range is the mean of the rates in the eight 5-year age ranges. The 40-year risk of death is then 1exp(40R/1000). ICD codes used: Cardiac (ICD-9: 390–409, 410–414, 415–429, 440–459; ICD-10: I70–I99 including diabetes ICD-9: 250; ICD-10: E10-E14); Respiratory (ICD-9: 460-519: ICD-10: J00J99) and Cancer (ICD-9140-208; ICD-10: C00C97). The vertical scales are different for the top and bottom panels.
Discussion
We have demonstrated that overall mortality risks in middle age have diverged over the past two decades between Mexicans and US Mexican Hispanics, most notably among men. In Mexican men, this divergence is mostly due to a sharp increase in risks of death from myocardial infarction and from homicide, the latter due mostly to gun violence. Cardiac mortality has declined much less in Mexican women than in US Mexican Hispanic women, contributing to a divergence in the overall risk of death over the past two decades.
Large differences in premature mortality between otherwise similar cultural groups can arise from just a few modifiable factors, most notably smoking, untreated vascular disease and diabetes, and homicide. First, there has been convergence in smoking-attributable mortality between Mexican and US Mexican Hispanic males. Indeed, without declines in smoking-attributable deaths, the overall mortality differences between Mexicans and US Mexican Hispanics would have likely diverged further. In the Mexican states with high burden of lung cancer and adjacent to the US border, the declines in overall risks of smoking-attributable mortality among men have been similar to those of US Mexican Hispanic men, reaching about 2% absolute risk in 2010–15. In 2015, the overall proportion of men killed in middle age from smoking was about 40% lower among Mexican men compared to US Mexican Hispanic men (3.6% versus 6.0%). The proportion of smoking-related deaths was similar for Mexican men in high burden states (6.6%) and their US Mexican counterparts (6.0%). Among women in both countries, smoking accounts for an even smaller proportion of premature deaths. In large part, these likely reflect the lower number of daily cigarettes consumed per smoker (eTable 1, available at IJE online), and are consistent with the declines in smoking prevalence observed in both countries (eTable 2, available at IJE online) in the past two decades.7–9 However, we noted a linear relationship between the cohort-specific smoking amount and smoking mortality a few decades hence (eFigure 3, available at IJE online). About two-thirds of Mexicans live in the low-burden states where men who smoke consume an average of 6.6 cigarettes daily. If the mean daily amount were to increase only modestly to 10, as seen in Sinaloa state in north Mexico, or more substantially to 12 as seen among US Mexican Hispanic men, the increases would result in about 6% and 9% higher absolute risk of smoking-attributable death, respectively. The absolute total of smoking-attributable deaths over the two decades was substantial, killing 185 000 Mexicans and 47 000 US Mexican Hispanics in middle age alone. Hence ongoing efforts to deter smoking and raise quit rates remain essential.5,6
Our retrospective methods could not directly estimate the impact of diabetes, most of which is related to adiposity. However, a recent prospective study in Mexico City found that under-treated or poorly treated diabetes accounts for a substantial amount of life-years lost, mostly from cardiac and renal disease.14 Global estimates of adiposity also find much greater hazards in men and women,35 matching our observation of greater cardiac mortality among men. In the USA, where data are better available, the prevalence of self-diagnosed or clinically diagnosed diabetes among US Mexican Hispanics which is uncontrolled (defined as a glycosylated haemoglobin proportion >9%) is roughly 16%, about twice the level among US Whites, even after taking into account the lower health insurance access among US Mexican Hispanics.36 However, in Mexico, the comparable prevalence was 50% in 2012 (a decline from even greater levels in 2006).37 The prospective study in Mexico City found the highest relative risks for untreated diabetes were from renal disease and cardiac mortality, with greatest relative (but not absolute risks) at younger cohorts aged 35–44. Consistent with this, we conducted age, period and cohort analyses which found birth cohort effects for myocardial infarction, but not for stroke or renal disease among Mexicans, and no effects for any of these three conditions among US Mexican Hispanics (data not shown). If untreated hypertension were a strong explanatory factor, we would expect greater divergence between Mexican and US Mexican Hispanic in stroke mortality, as the effects of blood pressure are greater on stroke than on cardiac risk.38–40 Expansion of health insurance coverage in the US Affordable Care Act and the Mexican Seguro Popular might further lower the future proportions of untreated people with diabetes in both countries.16,41,42 Third, homicide, and in particular gun-related homicide in Mexico, is heavily concentrated in males in the 2005–10 time period, corresponding to a national strategy to fight drug cartels’ operations in Mexico.15 Indeed, the risk of homicide became comparable to the risk of smoking-attributable death in many states. Notably in the state of Chihuahua, homicide death rates per 100 000 people rose from 15 in 2007 to 186 in 2010, representing about 6000 additional murders.43 Gun violence has fallen since about 2012, and this might help improve life expectancy, particularly for men.
We do not directly address the noted ‘Hispanic paradox’, in which longevity in US Hispanics is higher than that of US Whites of comparable socioeconomic levels.44 Unlike the smaller contribution of tobacco to mortality differences between Mexicans and US Hispanics (men, in particular), lower smoking levels and amounts may account for a large proportion of the higher longevity among US Hispanics.45 We relied on routine mortality statistics which have some limitations in coverage and coding norms over time, but have the benefit of capturing nearly 100% of all deaths, independent of lawful residence status in the USA. The proportion of ill-defined codes at ages 30–69 years, as a measure of quality of medical classification, was similar in US Whites and Mexican Hispanics and fell over time. Despite problems in misclassifying Mexican cardiac deaths as diabetic on Mexican death certificates, we did not observe a change in such coding practices over time. Moreover, we analysed cardiac and diabetic deaths together. The indirect methods indexed on lung cancer do not work where lung cancer is too uncommon, as in women in low-burden states of Mexico, (or men and women in India46 or in populations such as China where much of the lung cancer is due not only to smoking but also to indoor air pollution).47 However, results were stable among men, particularly in the high-burden states where smoking is more established. We estimated about 15 000 smoking deaths annually at ages 30 or older in 2014. The Mexican Global Burden of Disease project12 estimated about 15 000 deaths from smoking at ages 30–69 years in 2013, suggesting that these model-based estimates might be overestimating smoking deaths in Mexico.
These results suggest the need for ongoing attention to avoidable mortality in Mexico and among US Mexican Hispanics, most notably ensuring effective tobacco taxation and other control steps to raise cessation rates,5,6 treatment of vascular disease and diabetes14,39 and efforts to reduce gun and drug-related violence.15 Robust use of cause-specific mortality provides a powerful, low-cost way to monitor changes in these key risk factors.23
Supplementary Data
Supplementary data are available at IJE online.
Conflict of interest: None declared.
Key Messages
Large differences in premature mortality between otherwise genetically and culturally similar groups can arise from just a few modifiable factors, most notably smoking, untreated diabetes and homicide.
The overall mortality risks in middle age have diverged over the past two decades between Mexican and US Mexican Hispanics, most notably among men. This is due to marked divergence in the risk of cardiac death, most likely from poorly or untreated diabetes, as well as to homicide (mostly from gun violence).
Smoking-attributable mortality has fallen by over half both in Mexico and among US Mexican Hispanics, suggesting that ongoing efforts to deter smoking and to raise quit rates are essential.
Supplementary Material
References
- 1. Norheim OF, Jha P, Admasu K, et al. Avoiding 40% of the premature deaths in each country, 2010–30: review of national mortality trends to help quantify the UN sustainable development goal for health. Lancet 2015;385:239–52. [DOI] [PubMed] [Google Scholar]
- 2. Jamison DT, Jha P, Malhotra V, Verguet S. The 20th Century Transformation of Human Health: Its Magnitude and Value. Copenhagen: Copenhagen Consensus on Human Challenges, 2011. [Google Scholar]
- 3. Gonzalez-Pier E, Barraza-Llorens M, Beyeler N, et al. Mexico's path towards the Sustainable Development Goal for health: an assessment of the feasibility of reducing premature mortality by 40% by 2030. Lancet Glob Health 2016;4:e714–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gomez-Dantes H, Fullman N, Lamadrid-Figueroa H, et al. Dissonant health transition in the states of Mexico, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2016;388:2386–402. [DOI] [PubMed] [Google Scholar]
- 5. Jha P, Peto R. Global effects of smoking, of quitting, and of taxing tobacco. N Engl J Med 2014;370:60–68. [DOI] [PubMed] [Google Scholar]
- 6. Jha P. Avoidable global cancer deaths and total deaths from smoking. Nat Rev Cancer. 2009;9:655–64. [DOI] [PubMed] [Google Scholar]
- 7. Guerrero-López CM, Muños-Hernández JA, Sáenz de Miera-Juárez B, Reynales-Shigematsu LM. Consumo de tabaco, mortalidad y política fiscal en México (Tobacco consumption, mortality and fiscal policy in Mexico.). Salud Pública Mex 2013;55(Suppl 2):276–81. [PubMed] [Google Scholar]
- 8. National Institute of Statistics and Geography. Encuesta Nacional de Adicciones (ENA) (National Addictions Survey). Aguascalientes, Mexico: National Institute of Statistics and Geography, 2002. [Google Scholar]
- 9. Blanco L, Garcia R, Perez-Stable EJ, et al. National trends in smoking behaviors among Mexican, Puerto Rican, and Cuban men and women in the United States. Am J Public Health 2014;104:896–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Martell BN, Garrett BE, Caraballo RS. Disparities in adult cigarette smoking – United States, 2002–2005 and 2010–2013. MMWR Morb Mortal Wkly Rep 2016;65:753–58. [DOI] [PubMed] [Google Scholar]
- 11. Hernández-Ávila M, Gutiérrez JP, Reynoso-Noverón N. Diabetes mellitus en México. El estado de la epidemia (Diabetes Mellitus in Mexico. The state of the epidemic.). Public Health Mex 2013;55(Supp 2):7. [PubMed] [Google Scholar]
- 12. Institute for Health Metrics and Evaluation, Institute of Public Health. Global Burden of Disease Study 1990–2013, Mexico. 2015. http://www.healthdata.org/sites/default/files/files/country_profiles/Subnational/Mexico/CountryProfile_Subnational_Mexico_Mexico_2015.pdf(6 April 2016, date last accessed). [Google Scholar]
- 13. Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016;315:2284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alegre-Diaz J, Herrington W, Lopez-Cervantes M, et al. Diabetes and cause-specific mortality in Mexico City. N Engl J Med 2016;375:1961–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aburto JM, Beltran-Sanchez H, Garcia-Guerrero VM, Canudas-Romo V. Homicides in Mexico reversed life expectancy gains for men and slowed them for women, 2000–10. Health Aff (Millwood) 2016;35:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Obama B. United States health care reform: progress to date and next steps. JAMA 2016;316:525–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. National Bureau of Economic Research. Mortality Data: Vital Statistics NCHS' Multiple Cause of Death Data, 1959–2014. 2014. http://www.nber.org/data/vital-statistics-mortality-data-multiple-cause-of-death.html(2 July 2015, date last accessed). [Google Scholar]
- 18. National Institute of Statistics and Geography. Mortalidad. [Mortality.] 2015. http://www3.inegi.org.mx/sistemas/microdatos/encuestas.aspx?c=33398&s=est(8 January 2015, date last accessed). [Google Scholar]
- 19. WHO. International Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Geneva: World Health Organization,1992. [Google Scholar]
- 20. Flood S, King M, Ruggles S, Warren JR. Integrated public use microdata series. Current Population Survey: Version 4.0. University of Minnesota, 2015. [Google Scholar]
- 21. Ruggles S, Genadek K, Goeken R, Josiah G, Sobek M. Integrated public use microdata series. Version 6.0 (dataset). University of Minnesota, 2015. [Google Scholar]
- 22. Mexican Population Council (MPC). Estimaciones y Proyecciones de la Población por Entidad Federativa – Datos de Proyecciones (Estimates and projections of population by state – Projections data.). 2014. http://www.conapo.gob.mx/es/CONAPO/Proyecciones_Datos(6 October 2014, date last accessed). [Google Scholar]
- 23. Jha P. Reliable direct measurement of causes of death in low- and middle-income countries. BMC Med 2014;12:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Peto R, Lopez AD, Boreham J, Thun M, Heath C Jr. Mortality from tobacco in developed countries: indirect estimation from national vital statistics. Lancet 1992;339:1268–78. [DOI] [PubMed] [Google Scholar]
- 25. Peto R, Lopez AD, Boreham J, Thun M, Heath C Jr. Mortality from Smoking in Developed Countries 1950–2000: Indirect Estimates From National Vital Statistics. Oxford, UK: Oxford University Press, 1994. [Google Scholar]
- 26. Jha P, Peto R, Zatonski W, Boreham J, Jarvis MJ, Lopez AD. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet 2006;368:367–70. [DOI] [PubMed] [Google Scholar]
- 27. Tovar-Guzmán VJ, López-Antuñano FJ, Rodríguez-Salgado N. Tendencias de la mortalidad por cáncer pulmonar en México, 1980–2000 (Trends in mortality by lung cancer in Mexico, 1980–2000.). Rev Panam Salud Publica 2005;17:4. [DOI] [PubMed] [Google Scholar]
- 28. Ruiz-Godoy L, Rizo Rios P, Sanchez Cervantes F, Osornio-Vargas A, Garcia-Cuellar C, Meneses Garcia A. Mortality due to lung cancer in Mexico. Lung Cancer 2007;58:184–90. [DOI] [PubMed] [Google Scholar]
- 29. Garfinkel L. Selection, follow-up, and analysis in the American Cancer Society prospective studies. Natl Cancer Inst Monogr 1985;67:49–52. [PubMed] [Google Scholar]
- 30. National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Reports of the Surgeon General. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention (US), 2014. [PubMed] [Google Scholar]
- 31. Serrano-Medrano M, Arias-Chalico T, Ghilardi A, Masera A. Spatial and temporal projection of fuelwood and charcoal consumption in Mexico. Energy for Sustainable Development 2014;19:7. [Google Scholar]
- 32. Minnesota Population Center and State Health Access Data Assistance Center. Integrated Health Interview Series: Version 6.11. Minneapolis, MO: University of Minnesota, 2015. [Google Scholar]
- 33. Aleksandrowicz L, Malhotra V, Dikshit R, et al. Performance criteria for verbal autopsy-based systems to estimate national causes of death: development and application to the Indian Million Death Study. BMC Med 2014;12:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. National Population Council. Yearbook of Migration and Remittances: Mexico 2016. Mexico City: Ministry of the Interior, 2015. [Google Scholar]
- 35. Global BMI Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016;388:776–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ali MK, McKeever Bullard K, Imperatore G, Barker L, Gregg EW. Characteristics associated with poor glycemic control among adults with self-reported diagnosed diabetes - National Health and Nutrition Examination Survey, United States, 2007–2010. MMWR Suppl 2012;61:32–37. [PubMed] [Google Scholar]
- 37. Flores-Hernandez S, Saturno-Hernandez PJ, Reyes-Morales H, Barrientos-Gutierrez T, Villalpando S, Hernandez-Avila M. Quality of diabetes care: the challenges of an increasing epidemic in Mexico. Results from two national health surveys (2006 and 2012). PloS One 2015;10:e0133958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bailey SR, O'Malley JP, Gold R, Heintzman J, Marino M, DeVoe JE. Receipt of diabetes preventive services differs by insurance status at visit. Am J Prev Med 2015;48:229–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Stark Casagrande S, Cowie CC. Health insurance coverage among people with and without diabetes in the U.S. adult population. Diabetes Care 2012;35:2243–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease. Part 1, Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990;335:765–74. [DOI] [PubMed] [Google Scholar]
- 41. Blumenthal D, Abrams M, Nuzum R. The Affordable Care Act at 5 years. N Engl J Med 2015;373:1580. [DOI] [PubMed] [Google Scholar]
- 42. Frenk J, Gonzalez-Pier E, Gomez-Dantes O, Lezana MA, Knaul FM. Comprehensive reform to improve health system performance in Mexico. Lancet 2006;368:1524–34. [DOI] [PubMed] [Google Scholar]
- 43. INEGI. Datos Preliminares Revelan que en 2014 se Registraron 19 Mil 669 Homicidios. Aguascalientes, Mexico: Instituto Nacional de Estadística y Geografía, 2016. [Google Scholar]
- 44. Ruiz JM, Steffen P, Smith TB. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. Am J Public Health 2013;103:e52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fenelon A. Revisiting the Hispanic mortality advantage in the United States: the role of smoking. Social Sci Med 2013;82:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jha P, Jacob B, Gajalakshmi V, et al. A nationally representative case-control study of smoking and death in India. N Engl J Med 2008;358:1137–47. [DOI] [PubMed] [Google Scholar]
- 47. Chen Z, Peto R, Zhou M, et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet 2015;386:1447–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.