Abstract
Aims
So far, a total of five patients with eclipsed mitral regurgitation (MR) have been reported in the literature by three different teams. The aim of this article was to detail clinical and echocardiographic characteristics, and outcome of patients presenting eclipsed MR.
Methods and results
We defined eclipsed MR as spontaneous appearance, at rest, from 1 min to the next of an acute restriction in the motion of mitral leaflets preventing coaptation and leading to massive MR in patients with normal left ventricular end-diastolic diameter, left ventricular ejection fraction >45%, and baseline MR ≤2. Spontaneous regression occurred within 30 min, and no obvious trigger such as acute hypertension, new-onset arrhythmia, or myocardial ischaemia is present. Clinical data, ECG, echocardiographic data, surgery report, and follow-up status of six patients with eclipsed MR are reported: all were post-menopausal women with median age of 74 [57–80] years presenting hypertension (4/6), chronic kidney disease (5/6), or chronic anaemia (4/6). Five out of six patients experienced acute pulmonary oedema requiring hospitalization and underwent mitral valve replacement because of heart failure recurrence. Two patients died in the first days after surgery while the three others are free of symptoms at, respectively, 56, 18, and 10 months follow-up.
Conclusion
Eclipsed MR is a clinical and echocardiographic syndrome responsible for heart failure with preserved EF. It is presently underdiagnosed and should be evoked in cases of recurrent acute pulmonary oedema without obvious trigger, in particular in patients presenting discordant evaluation of MR severity over time.
Keywords: acute mitral regurgitation, transient acute mitral regurgitation, heart failure with preserved LVEF, eclipsed mitral regurgitation, functional mitral regurgitation, echocardiography
Introduction
Secondary mitral regurgitation (MR) is a chronic disease resulting from geometrical distorsion of the subvalvular apparatus secondary to left ventricular (LV) enlargement and remodelling. The tethering of the valves results from apical displacement of papillary muscles in dilated left ventricle with systolic dysfunction and dyssynchronism. The severity of secondary MR may vary over time, and transient severe ischaemic MR has been identified as a cause of acute pulmonary oedema in patients with impaired left ventricular ejection fraction (LVEF) and moderate MR at baseline.1
However, half of the patients with acute heart failure do not present impaired LVEF.2 Pathophysiological mechanisms underlying acute heart failure with preserved LVEF (HFPEF) are not fully understood yet, and treatments modifying prognosis are lacking in HFPEF.
The brutal occurrence of transient severe MR at rest in patients with non-dilated LV and normal baseline EF is possible and has previously been described in rare instances. This phenomenon was first reported by Avierinos et al.3 in three patients. They called this new entity of acute transient severe MR occurring without obvious trigger from 1 min to the next ‘eclipsed mitral regurgitation’. Because it was triggered by methylergonovine, reversed by nitroglycerin, and prevented by calcium antagonist, they concluded that this transient MR was secondary to epicardial coronary spasm. However, in another case report, methylergonovine was not a trigger for the eclipsed MR and the patient required surgery for recurrence of severe symptomatic MR.4
Finally, very few data are available on this particular type of MR, and neither its pathophysiology nor the appropriate management and treatment are known. The clinical presentation usually includes recurrent unexplained acute pulmonary oedema in patients with varying intensity of MR murmur overtime, preserved LVEF, left atrium dilatation, and no more than mild MR at baseline. This eclipsed MR needs to be recognized since it may lead to repeated hospitalizations and be life threatening.
We report six women with preserved LVEF and normal LV volumes presenting an eclipsed MR with apparition and resolution within few minutes. The aim of this article was to detail patients' clinical and echocardiographic characteristics, and their outcome.
Methods
Between 2006 and 2014, six patients were successively referred to Bichat or Montfermeil cardiology departments for left heart failure symptoms and were diagnosed with eclipsed MR (chronologic presentation from n = 1 to 6).
The data collected in all patients were personal history, clinical examination, 12-lead electrocardiogram, rest transthoracic echocardiography (TTE), trans-oesophageal echocardiography (TOE), and coronary angiography.
We defined eclipsed MR as a spontaneous appearance, at rest, from 1 min to the next of an acute restriction in the motion of mitral leaflets preventing coaptation and leading to massive MR in patients with normal LV end-diastolic diameter, LVEF >45%, and baseline MR ≤2. Spontaneous regression without therapeutic intervention of the MR occurred within 30 min, and no obvious trigger such as acute hypertension, new-onset arrhythmia, or myocardial ischaemia is present.
In all patients, LVEDD, end-diastole mitral annulus, and tenting area were measured using TTE in the parasternal long-axis view and mitral angles in the apical four-chamber view at baseline and during eclipsed MR (except in Patient 3 because eclipsed MR was only observed during TOE).
MR severity at baseline was quantitated with effective regurgitant orifice (ERO) measured by the proximal isovelocity surface area method.5
Quantitative variables were expressed as median and [25–75th percentiles]. Qualitative variables were expressed as n (percentages).
Results
Clinical presentation and circumstances of diagnostics
These six patients were all post-menopausal women, and their main characteristics are detailed in Table 1. The youngest one was diagnosed at the age of 49 years and had underwent thoracic radiotherapy and chemotherapy for Hodgkin disease 15 years earlier. Median age at diagnosis was 74 years [57–80]. None had a smoking history and four out of six had hypertension while five presented with chronic kidney disease (median creatinine clearance: 38 [27–42] mL/min/1.73 m²) and four with chronic anaemia (median Hb = 9.6 [9.0–10.5] g/dL).
Table 1.
Patients’ clinical characteristics at eclipsed MR diagnosis
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | |
|---|---|---|---|---|---|---|
| Sex | F | F | F | F | F | F |
| Age | 73 | 75 | 49 | 80 | 80 | 65 |
| Cardiovascular risk factors | Hypertension treated with captopril Dyslipidaemia Diabetes mellitus |
No | No | Hypertension treated with candesartan and sotalol Dyslipidaemia |
Hypertension treated with irbesartan Dyslipidaemia Diabetes mellitus |
Hypertension treated with bisoprolol |
| Atrial fibrillation | Paroxysmal | Permanent | No | Permanent | Paroxysmal | Paroxysmal |
| QRS width (ms) | 134 LBBB | 97 | 140 LBBB | 160 Pacing | 160 LBBB | 85/240 Intermittent LBBB |
| Creatinine clearance (mL/min/1.73 m²) | 46 | 38 | 70 | 22 | 38 | 32 |
| Haemoglobin (g/dL) | 9.2 | 10 | 13.9 | 12.5 | 8.7 | 11 |
Either rhythm or conductive disorders were recorded in all the patients. In five patients indeed, a history of atrial fibrillation (AF) was found: permanent AF in two and paroxysmal AF in three. Moreover, left bundle branch block (LBBB) was recorded in five patients: three had a permanent LBBB, one an intermittent rate-dependent LBBB, and one a permanent ventricular pacing. Finally, only one patient presented with permanent QRS duration <0.12 s but suffered from permanent AF.
The main clinical presentation was acute pulmonary oedema in five out of the six patients, who needed repeated hospitalizations (median: 2.5 hospitalizations/patient) before eclipsed MR was diagnosed. The median time from first hospitalization for acute heart failure to eclipsed MR diagnosis was 9 months. Moreover, most acute pulmonary oedemas were severe with three patients requiring intensive care unit (ICU) at admission and one surviving a hypoxic cardiac arrest. Symptoms varied within minutes with quiescent phase and brutal acute exacerbations. We found in all patients' medical records a great variability of the intensity of the mitral murmur heard overtime.
The details are provided below for each patient.
In Patient 1, eclipsed MR was observed during TTE performed the day after admission for acute pulmonary oedema (see Supplementary data online, Video S1). During the next 2 months, she experienced several acute pulmonary oedemas without clear precipitating factor, and a great variability in the severity of MR was recorded on repeated echocardiographic examinations.
Eclipsed MR was diagnosed in Patient 2 during TTE performed after admission for acute pulmonary oedema. MR was massive at the beginning of TTE examination then became mild after a few minutes of rest.
Patient 3 complained of dyspnoea and orthopnoea and presented with 3/6 MR murmur. She is the only patient who has not been hospitalized for acute heart failure. She underwent ambulatory TTE and TOE for evaluation of this MR. TTE revealed mild MR, whereas at the beginning of TOE, a massive restrictive MR appeared and decreased a few minutes later.
Patient 4 had been admitted for the fourth time in 4 months for acute pulmonary oedema when TTE after admission revealed eclipsed MR. During the previous hospitalizations, MR was found to be mild on echocardiography.
Patient 5 was admitted for acute pulmonary oedema initially attributed to new-onset AF. MR was severe at admission but decreased to mild grade after medical treatment and spontaneous return in normal sinus rhythm. One month later, acute pulmonary oedema recurred requiring hospitalization while she was in sinus rhythm. Eclipsed MR was evidenced on TTE during this second hospitalization (see Supplementary data online, Video S2).
Patient 6 experienced acute respiratory distress without identified trigger leading to ICU hospitalization for ventilatory support. After diuresis, the patient recovered and remained initially with few or no symptoms for 5 months. She was then admitted for planned cardiac evaluation because of exertional dyspnoea and paroxystic orthopnoea. During this hospitalization, TTE and TOE found only mild MR, a severe left atrial dilatation, and moderate elevation of systolic pulmonary artery pressure (sPAP). During right heart catheterization, pulmonary pressure increased abruptly, with the concomitant recording of an important V wave; spontaneous return to previous values occurred within minutes. As the diagnostic was unclear, she was discharged with the same treatment, and exercise echocardiography was planned in the next month. However, 3 weeks later, she was admitted in emergency for severe acute pulmonary oedema, and the TTE examination performed after admission revealed eclipsed MR.
Echocardiographic results
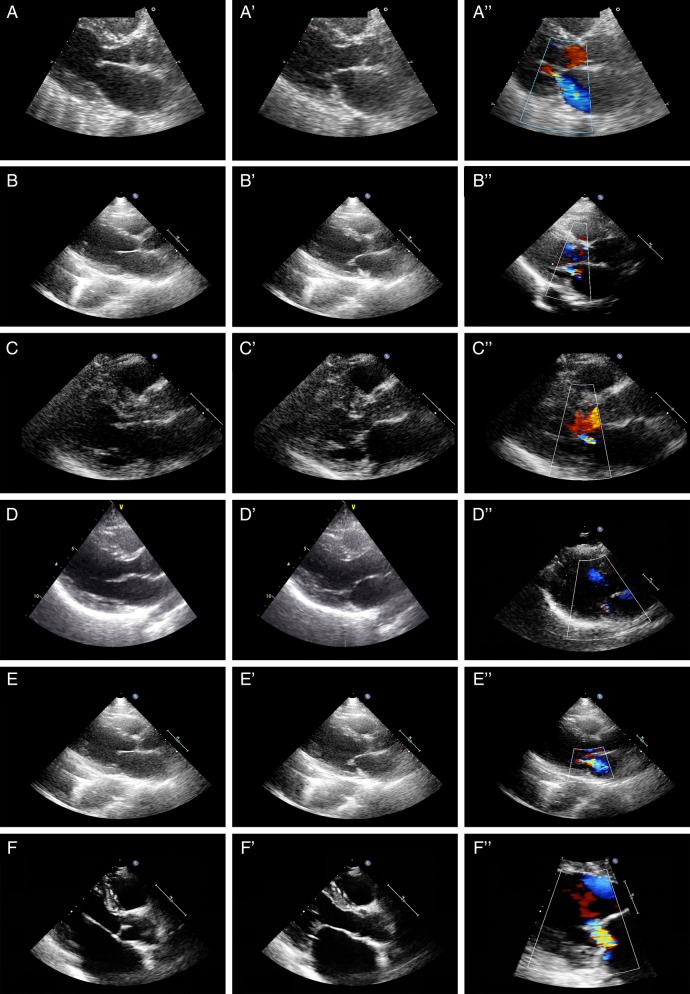
At baseline, mitral leaflets were normal in four patients and presented only minor and localized thickening in two patients (Table 2; Figure 1). MR ≤2 in all patients. sPAP was normal or near normal in all patients (median: 44 [33–45]mmHg).
Table 2.
Echocardiographic characteristics
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | |
|---|---|---|---|---|---|---|
| LV hypertrophy | No | Apicolateral | No | Septoapical | No | No |
| Mitral leaflets | Normal | Mildly thickened | Normal | Normal | Normal | Mildly thickened |
| Left atrium area (cm²) | 24 | 38 | 20 | 36 | 40 | 37 |
| MR ERO at baseline (cm²) | 0.10 | 0.12 | 0.15 | 0.23 | 0.12 | 0.19 |
| Tenting area (cm²) | ||||||
| At baseline | 2.6 | 2.5 | 1.7 | 2.7 | 2.1 | 2.3 |
| During eclipsed MR | 3.2 | 3.1 | ND | 2.9 | 4 | 4.2 |
| Leaflet angles | ||||||
| At baseline: AV/PV | 38/41 | 21/40 | 18/40 | 39/41 | 38/47 | 31/35 |
| During eclipsed MR: AV/PV | 39/51 | 25/49 | ND/ND | 41/45 | 41/60 | 39/52 |
| LVEDD (mm) | ||||||
| At baseline | 42 | 51 | 49 | 50 | 49 | 42 |
| During eclipsed MR | 49 | 59 | ND | 55 | 54 | 52 |
| Mitral annulus (mm) | ||||||
| At baseline | 35 | 37 | 33 | 37 | 39 | 40 |
| During eclipsed MR | 39 | 42 | ND | 41 | 43 | 44 |
| sPAP (mmHg) | ||||||
| At baseline | 39 | 45 | ND | 27 | 45 | 44 |
| During eclipsed MR | 55 | 90 | ND | 51 | 69 | 97 |
Figure 1.
Mitral valve of the six patients at baseline in the parasternal long-axis view in diastole (X), systole (X′) without Doppler colour and with Doppler colour (X′′).
During eclipsed MR, all six patients fulfilled the echocardiographic criteria, i.e. a restrictive motion of mitral leaflets, without leaflet coaptation leading to massive MR, lasting <30 min in patients without baseline LV dysfunction and dilatation.
Severe restrictive MR without leaflet coaptation was associated with triangular MR flow signal shape in continuous Doppler measurements and dramatic acute increase of sPAP (from 44 [33–45]mmHg at baseline to 69 [53–94]mmHg during eclipsed MR), Figure 2.
Figure 2.
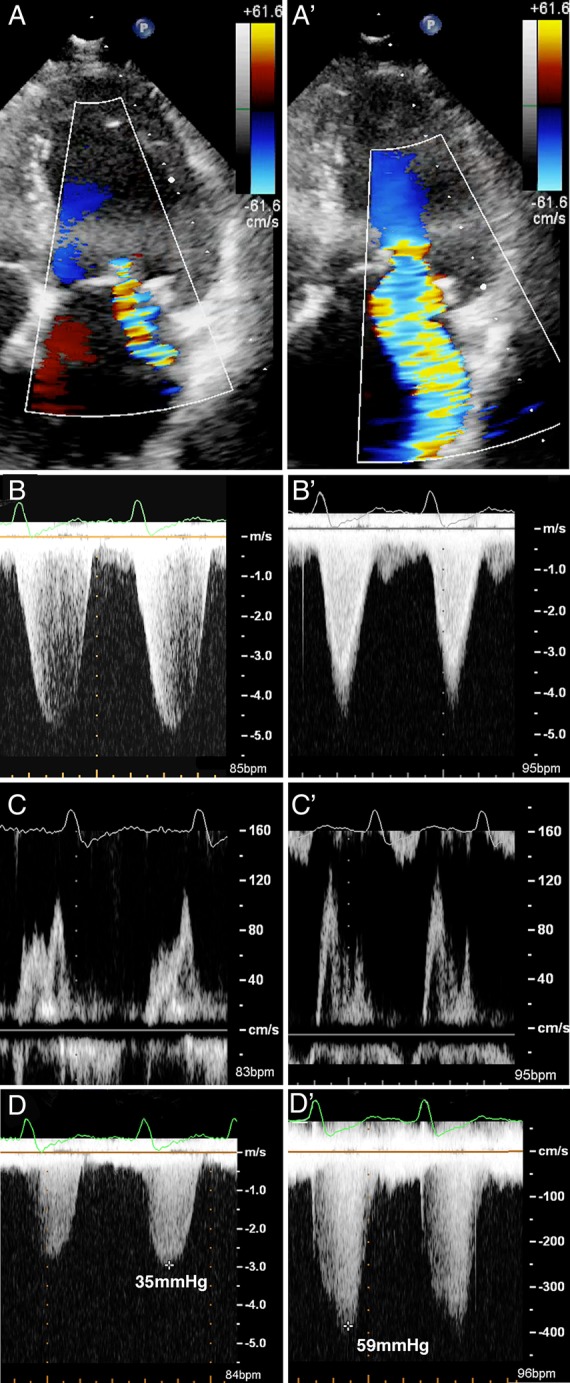
Example of the dramatic change associated with eclipsed MR (Patient 5): (A) MR colour flow at baseline; (B) MR colour flow during eclipsed MR. Eclipsed MR appearance is concomitant to the occurrence of a triangular shape of the MR signal with continuous Doppler (B and B′), an inversion of the E/A waves ratio (C and C′) and a dramatic increase of the sPAP (D and D′) within minutes.
All patients were found to have acute LV changes, both anatomical modification with relative dilatation (LVEDD increased from 49 [42–51]mm at baseline to 54 [51–57]mm during eclipsed MR) and was associated with functional changes with transient hyperkinesia and an increase in mitral annulus diameter and tenting area, respectively, from 37 [36–40]mm and 2.5 (2.2–2.7)cm² at baseline to 42 [40–44]mm and 3.2 (3.0–4.1)cm² during eclipsed MR. The echocardiographic features are detailed in Table 2 and Figure 3.
Figure 3.
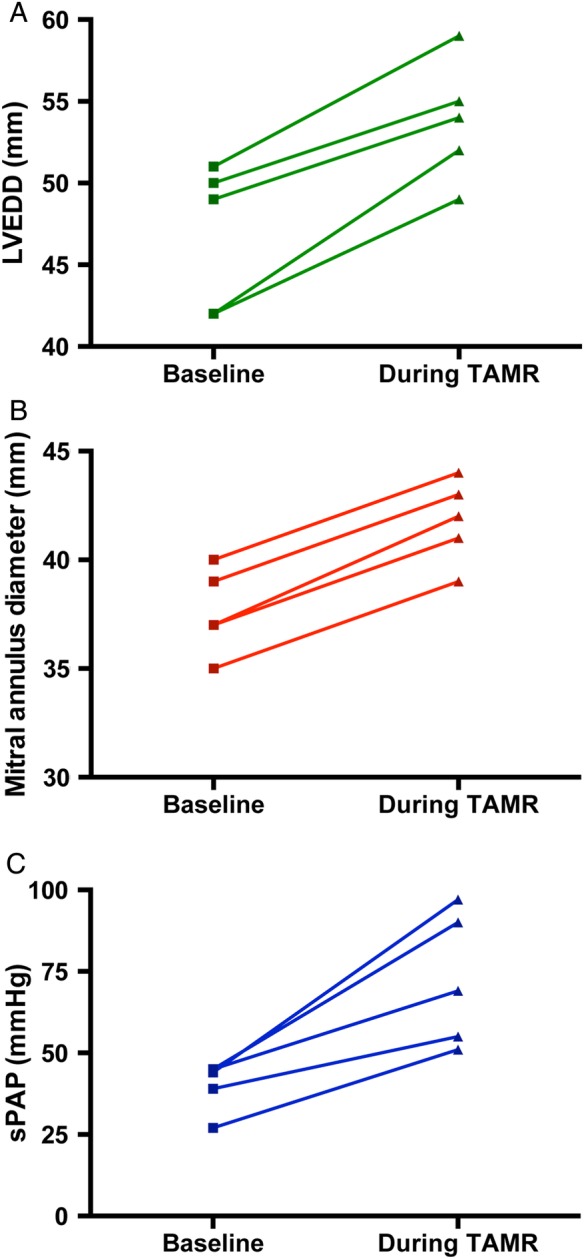
Variations of LV diameter, mitral annulus diameter, and sPAP at baseline and during eclipsed MR.
Visual LV dyssynchrony was present in five patients during eclipsed MR: permanent in four patients (permanent LBBB in three patients and permanent ventricular pacing in one) and heart rate dependant in one (rate-dependant LBBB).
Additional investigations
In three patients indeed, eclipsed MR was present immediately after the installation of the patient for echocardiography examination, resolved after few minutes of rest and exercise (grasping or cycling) few minutes later was associated with eclipsed MR recurrence (see Supplementary data online, Video S3). In two patients, we chose not to propose exercise echocardiography because of recurrent severe acute pulmonary oedemas and clinical instability. Patient 2 underwent a dobutamine echocardiography that was negative for ischaemia and with no change of the MR grade, whereas exercise echocardiography a few weeks later was associated with eclipsed MR occurrence.
A coronary angiogram was performed in all patients to eliminate an ischaemic aetiology and did not find any significant coronary stenosis. Methylergonovine injection was performed in Patient 1 and did not result in significant changes in MR grade and ECG and no coronary spasm occurred.
Exercise myocardial scintigraphy was performed in Patient 6 with additional injection of dipyridamole: no myocardial defect suggesting ischaemia was found, whereas LBBB occurred with simultaneous TTE showing eclipsed MR.
Treatment and prognosis
The Patient 3 has a less severe clinical course (no hospitalization for acute heart failure). During the last 7 years with close cardiological follow-up, she described only mild exertional dyspnoea under medical treatment associating furosemide, bisoprolol, and ramipril.
For the other five patients, eclipsed MR recurred despite optimal medical treatment. One patient underwent cardiac resynchronization therapy without efficacy on recurrence of eclipsed MR, and surgery was finally advised in all of them. In the five patients undergoing surgical treatment, intra-operative description reported mitral annulus dilation and normal or mildly thickened restrictive mitral leaflets.
The first two patients underwent mitral valve replacement after a long stay in hospital because of recurrence of several acute pulmonary oedemas despite medical treatment. They died in 2006 and 2008, 2 and 4 days after mitral surgery because of refractory cardiogenic shock (Patients no. 1 and 2). Three patients underwent successful mitral valve replacement with a bioprosthesis. Post-operative period was difficult necessitating inotrope support and non-invasive ventilation in ICU during 2, 6, and 8 days, respectively (patients no. 4, 5, and 6).
They had uneventful cardiac evolution after, respectively, 56, 18, and 17 months follow-up and remain in NYHA Class I. The last echographic follow-up found normal LV dimension, LVEF >45%, and sPAPs of, respectively, 35, 53, and 42 mmHg.
Discussion
Eclipsed MR is a newly recognized entity: Avierinos et al. described three patients in 20073 and two further patients were later reported, including one also included in our series.4,6 Therefore 10 patients have been reported until now including our series of six patients. This highlights the extreme rarity of this phenomenon but also probably its misdiagnosis and the under recognition.
Population
Patients with eclipsed MR both in our series and in the literature share common features: 9 of 10 patients were post-menopausal women, with cardiovascular risk factors (hypertension in 7, diabetes in 3) and renal dysfunction (5 out of 6 patients with renal evaluation). Moreover, all but one had either conductive disorders (LBBB or pacing-induced widening of QRS in six patients) or rhythm disorders (AF in seven patients, either paroxysmal or permanent). Finally, all patients but one presented at least one acute heart failure episode with pulmonary oedema, and usually several recurrences before the diagnosis was made.
Diagnosis
At baseline echocardiography, mitral leaflets were normal or mildly thickened with normal motion and MR ≤2. Within minutes, we observed that mitral annulus and LV diameters increased and a restriction of mitral leaflet motion and 10 leading to massive MR and dramatic sPAP increase (Figure 3; Table 2).
Both mitral annulus dilatation and tenting have been described as factors fostering MR in HF with preserved LVEF.7 Moreover, MR decreases when left atrial size and mitral annular diameter decrease after AF reduction in patients with normal LV volume.8 In one of our patients, Labbe et al.6 already described with 3D TOE the change in mitral annulus shape during eclipsed MR from a normal oval shape to a circular mitral annulus and clearly showed the restrictive nature of the regurgitation with a transient and sudden tenting of the mitral leaflets. All these data suggest that eclipsed MR is secondary to extreme tenting of both leaflets caused by transient LV and mitral annulus dilatation resulting in a total lack of leaflet coaptation while LVEF remained normal or increased.
This type of acute MR is different from the dynamic ischaemic MR reported by Pierard and Lancellotti1 during exercise in patient with history of acute pulmonary oedema: patient with recent acute pulmonary oedema had increase ERO during exercise, but none of the patient had ERO above 40 mm² at exercise. On the contrary, eclipsed MR is spontaneous, occurs at rest, and results in a massive MR resulting from the total absence of mitral leaflets coaptation. The dynamic nature of MR in HFPEF has also been reported, but concerned mild MR and the decreases occur within hours or days after diuretics and vasodilatory treatments.7
This idiopathic acute transient MR has been called ‘eclipsed MR’: one can say that this term is incorrect, because eclipse is a predictable phenomenon in contrary to eclipsed MR; however, this term is used in all references describing such MR after the first description by Avierinos, and it is easier to use it.
Treatment and outcome
In our series, acute pulmonary oedema due to eclipsed MR recurred despite medical treatment. One patient also underwent cardiac resynchronization without improvement and had to be operated on.
Mitral valve replacement was therefore required in five out of six patients. However, post-operative course was complicated in all patients including two deaths. Post-hospital discharge course was uneventful with few or no symptoms. Given the high morbi-mortality of surgery, percutaneous techniques such as MitraClip may be attractive in these high-risk patients.
Pathophysiological hypothesis of eclipsed MR
Avierinos et al.3 proposed that epicardial coronary vasospasm could be responsible for sudden apical tenting. They reported that eclipsed MR was triggered by methylergonovine injection in their three patients and was reversible after nitroglycerine administration. The vasospasm hypothesis was further supported by a reversible perfusion defect on scintigraphy during eclipsed MR in one of their patients. However, spasm was focal in only one patient, diffuse in one, and absent in the last. In addition, one patient had to be operated on due to eclipsed MR recurrence despite calcium channel blockers therapy.
Of note, methylergonovine injection did not induce eclipsed MR or epicardial vasospasm in the case report from Messas et al.4 Similarly, we found no argument for an epicardial vasospasm after methylergonovine injection in one patient. Moreover, no perfusion defect was observed in one of our patients who had a cardiac scintigraphy while eclipsed MR occurred.
In our experience, eclipsed MR was mostly triggered by physical exercise (grasping or cycling) and resolved within minutes after resting following exercise.
A vascular hypothesis remains though possible given the high-risk profile of the patients for endothelial microvascular dysfunction. This hypothesis was also suggested by Avierinos et al. in one of their patients, whose coronary arteries remained strictly normal after methylergonovine injection despite induction of MR.3 Interestingly, methylergonovine has been described to trigger microvascular dysfunction.9 In the present series as well as in the literature, all patients but one were post-menopausal women, with risk factors for microvascular dysfunction such as diabetes, hypertension, and mild renal failure. These characteristics are usually found in patients with Takotsubo cardiomyopathy, another transient phenomenon without clear pathophysiology implicating microvascular function.10,11 Therefore, eclipsed MR might be a consequence of underlying coronary microvascular dysfunction with a superimposed trigger such as exercise. However, coronary spasm or microvascular dysfunction is associated with acute localized hypokinesia or akinesia in segments of the LV wall, but none of the patients described in the literature or in our series was found to have such abnormalities.
Eclipsed MR seems to be mainly the consequence of acute LV modifications: LV and mitral annulus dilatation, circular mitral annulus shape, and intraventricular asynchronism related to wide QRS. This hypothesis of a primary LV function abnormality is reinforced by the fact that mitral valve replacement is associated with poor outcomes and need for post-operative inotropic support while no MR remains. New technics evaluating LV asynchronism and longitudinal function (myocardial strain) will probably help to understand the mechanism of eclipsed MR. Unfortunately, in our series, TTE exam was performed since 2006 on different echocardiography machines, preventing reproducible and reliable LV strain measurement.
Study limitations
Our study has several limitations since it is a small series concerning patients from two cardiology departments. Since it is a new entity, no systematic evaluation has been proposed. However, to date it is to our knowledge the largest series reported. In the future, we need a systematic and standardized evaluation.
Clinical implications
Eclipsed MR is a rare cause of acute heart failure with normal LV volumes and preserved LVEF. Since it is a transient phenomenon rarely reported, the diagnosis is probably underestimated. Eclipsed MR should be considered in the case of pulmonary oedema with no clear precipitating factor, in particular in patients with risk factors for microvascular dysfunction. The clinical presentation usually includes recurrent unexplained acute pulmonary oedema in patients with varying intensity of MR murmur overtime, preserved LVEF, left atrium dilatation, and no more than mild MR at baseline. Discordant clinical examinations (mitral systolic murmur intensity) or echocardiographic results (MR grade) may be other arguments for advocating an eclipsed MR. Less severe presentations may be overlooked as suggested by Patient 3.
Since eclipsed MR is a transient phenomenon, echocardiography has to be repeated to establish diagnosis with mitral annulus and LV diameter increase and restrictive mitral leaflet motion. Exercise echocardiography or grasping might help for the diagnosis.
The best therapeutic option is still to be determined. Surgery has been favoured in highly symptomatic patients with advanced eclipsed MR but is associated with high mortality. Earlier recognition of this entity may allow less severe patients to be diagnosed and less invasive therapeutic options to be effective.
Supplementary data
Supplementary data are available at European Journal of Echocardiography online.
Conflict of interest: None declared.
Supplementary Material
References
- 1. Pierard LA, Lancellotti P. The role of ischemic mitral regurgitation in the pathogenesis of acute pulmonary edema. N Engl J Med 2004;351:1627–34. [DOI] [PubMed] [Google Scholar]
- 2. Senni M, Tribouilloy CM, Rodeheffer RJ, Jacobsen SJ, Evans JM, Bailey KR et al. . Congestive heart failure in the community: a study of all incident cases in Olmsted County, Minnesota, in 1991. Circulation 1998;98:2282–9. [DOI] [PubMed] [Google Scholar]
- 3. Avierinos JF, Thuny F, Tafanelli L, Renard S, Chalvignac V, Guedj E et al. . Eclipsed mitral regurgitation: a new form of functional mitral regurgitation for an unusual cause of heart failure with normal ejection fraction. Cardiology 2008;110:29–34. [DOI] [PubMed] [Google Scholar]
- 4. Messas N, Samet H, Brocchi J, Billaud P, Kremer H, Jesel L et al. . Mitral valve surgery for transient severe mitral regurgitation: an alternative to medical treatment? Int J Cardiol 2014;175:e40–2. [DOI] [PubMed] [Google Scholar]
- 5. Lancellotti P, Tribouilloy C, Hagendorff A, Popescu BA, Edvardsen T, Pierard LA et al. . Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2013;14:611–44. [DOI] [PubMed] [Google Scholar]
- 6. Labbe V, Charlier P, Brochet E, Iung B, Vahanian A, Messika-Zeitoun D. Transient severe reversible functional mitral regurgitation: a three-dimensional transoesophageal perspective. Eur J Echocardiogr 2010;11:E3. [DOI] [PubMed] [Google Scholar]
- 7. Ennezat PV, Marechaux S, Bouabdallaoui N, Le Jemtel TH. Dynamic nature of pulmonary artery systolic pressure in decompensated heart failure with preserved ejection fraction: role of functional mitral regurgitation. J Card Fail 2013;19:746–52. [DOI] [PubMed] [Google Scholar]
- 8. Gertz ZM, Raina A, Saghy L, Zado ES, Callans DJ, Marchlinski FE et al. . Evidence of atrial functional mitral regurgitation due to atrial fibrillation: reversal with arrhythmia control. J Am Coll Cardiol 2011;58:1474–81. [DOI] [PubMed] [Google Scholar]
- 9. Horimoto M, Igarashi K, Takenaka T, Inoue H, Yamazaki K, Sakuragi H. Acetylcholine- and ergonovine-induced coronary microvascular spasm reflected by increased coronary vascular resistance and myocardial lactate production. Clin Cardiol 2000;23:221–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dawson DK, Neil CJ, Henning A, Cameron D, Jagpal B, Bruce M et al. . Tako-tsubo cardiomyopathy: a heart stressed out of energy? J Am Coll Cardiol Imag 2015;8:985–7. [DOI] [PubMed] [Google Scholar]
- 11. Bouleti C, Attias D, Serfaty JM, Vahanian A. Correlations between echocardiography and cardiovascular magnetic resonance in a patient with midventricular stress cardiomyopathy. Arch Cardiovasc Dis 2011;104:204–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.