Abstract
Aims
Epidemiological studies indicate that traffic noise increases the incidence of coronary artery disease, hypertension and stroke. The underlying mechanisms remain largely unknown. Field studies with nighttime noise exposure demonstrate that aircraft noise leads to vascular dysfunction, which is markedly improved by vitamin C, suggesting a key role of oxidative stress in causing this phenomenon.
Methods and results
We developed a novel animal model to study the vascular consequences of aircraft noise exposure. Peak sound levels of 85 and mean sound level of 72 dBA applied by loudspeakers for 4 days caused an increase in systolic blood pressure, plasma noradrenaline and angiotensin II levels and induced endothelial dysfunction. Noise increased eNOS expression but reduced vascular NO levels because of eNOS uncoupling. Noise increased circulating levels of nitrotyrosine, interleukine-6 and vascular expression of the NADPH oxidase subunit Nox2, nitrotyrosine-positive proteins and of endothelin-1. FACS analysis demonstrated an increase in infiltrated natural killer-cells and neutrophils into the vasculature. Equal mean sound pressure levels of white noise for 4 days did not induce these changes. Comparative Illumina sequencing of transcriptomes of aortic tissues from aircraft noise-treated animals displayed significant changes of genes in part responsible for the regulation of vascular function, vascular remodelling, and cell death.
Conclusion
We established a novel and unique aircraft noise stress model with increased blood pressure and vascular dysfunction associated with oxidative stress. This animal model enables future studies of molecular mechanisms, mitigation strategies, and pharmacological interventions to protect from noise-induced vascular damage.
Keywords: Environmental stressor , Noise exposure , Endothelial dysfunction , Oxidative stress , eNOS uncoupling , NADPH oxidase , Vascular inflammation
Introduction
The health burden of environmental noise exposure has been increasingly acknowledged. The World Health Organization (WHO) estimates that each year almost 1 million disability adjusted life years are lost due to noise exposure in the Western European population.
Epidemiological studies have demonstrated that traffic noise exposure is associated with cardiovascular diseases such as hypertension, myocardial infarction, and stroke.1–3 Noise is a non-specific stressor that arouses the autonomic nervous system and endocrine system. Chronic low levels of noise can cause disturbances of activity, sleep, and communication leading to emotional responses such as annoyance and subsequent stress.4,5 Chronic stress in turn has been demonstrated to generate its own cardiovascular risk factors such as increased blood pressure and dyslipidemia, increased blood viscosity and blood glucose and activation of blood clotting factors in animal models6,7 and humans.8–12 Persistent chronic noise exposure increases the risk of cardiovascular and metabolic diseases such as hypertension, coronary artery disease, diabetes, and stroke.13–17 A recent meta-analysis reported on a linear relationship between exposure to transportation noise and the incidence of ischaemic heart diseases, warranting further studies to understand the mechanistic basis of this association.18
We recently studied the effects of nighttime aircraft noise on vascular (endothelial) function in healthy subjects19 and demonstrated that nighttime noise dose-dependently impairs endothelial function, disrupts sleep quality and tends to increase blood pressure. Importantly, in a subgroup of subjects, vitamin C significantly improved flow-mediated dilation (FMD) suggesting that increased production of reactive oxygen species (ROS) in response to noise exposure contributes to vascular dysfunction.19 In our subsequent clinical study, we reported on synergistic adverse cardiovascular effects of noise exposure in patients with pre-established cardiovascular diseases, further supporting the role of oxidative stress.20
Since previous animal models employed high dBA levels (up to 100 dBA),21–23 which can lead to direct auditory damage, we developed a novel noise exposure model in mice (C57Bl/6j) with lower peak sound levels (<85 dBA), lower mean sound pressure levels (72 dBA) and shorter exposure times (1–4 days), which has been shown to be safe and to cause mainly non-auditory effects to animals such as stress reactions.24 To our knowledge, no study has so far investigated directly the vascular consequences of noise exposure. In the present studies we sought to characterize the mechanisms of aircraft noise-induced vascular (endothelial) dysfunction, e.g. to identify the sources of ROS production, to assess the degree of imbalance of vascular NO/− production and the extent of inflammation in the vasculature of noise-exposed animals. We also tested the consequences of noise on the gene expression profile in the vasculature by performing Illumina transcriptomic next generation sequencing.
Methods
Noise exposure
All animals were treated in accordance with the Guide for the Care and Use of Laboratory Animals as adopted by the U.S. National Institutes of Health and approval was granted by the Ethics Committee of the University Medical Center Mainz and the Landesuntersuchungsamt Rheinland-Pfalz (Koblenz, Germany; permit number: 23 177-07/G 12-1-021 E3 and 23 177-07/G 15-1-094). Noise exposure consisted of repetitive playbacks of a 2 hour long noise pattern of 69 aircraft noise events with a duration of 43 s and a maximum sound pressure level of 85 dB(A) and a mean sound pressure level of 72 dB(A), which does not lead to hearing loss.24 Noise events were separated by silent periods with irregular distribution to prevent early adaptation. The noise pattern was played back from downward facing loudspeakers mounted approximately 30 cm above the mouse cages with a Grundig MS 540 compact sound system with a total output of 65 W. Loudness and corresponding sound pressure levels were calibrated with a Class II Sound level meter (Casella CEL-246) within one the cages at initial setup. Actual SPLs during exposure was continuously recorded during the study period with the same device placed between cages with upward facing microphone. The average SPL (Leq3) is 72 dB(A) at a usual background noise level of 48 dB(A) in the animal facility. In control experiments, mice were exposed to ‘white noise’ (this is a random noise with constant spectral density within the range of human hearing from 20 Hz to 20 kHz) using exactly the same average SPL as for aircraft noise. All SPL and maximum sound pressure levels were measured within the mouse cages.
For further information of the methodology employed for determination of blood pressure, stress hormones, vascular function, nitric oxide quantification, oxidative stress parameters, inflammatory pathways, gene and protein expression, next generation sequencing see the Supplementary material online.
Results
Effects of noise exposure on laboratory values, blood pressure and stress hormone levels
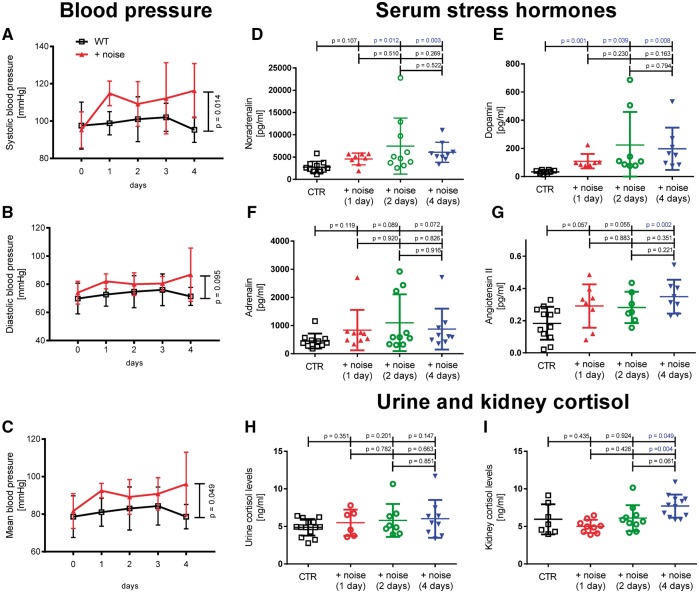
Noise exposure for 1–4 days caused no significant changes in heart/body weight ratio (Supplementary material online, Figure 1S). Blood glucose levels were increased compared with controls during the entire noise exposure period, while triglyceride levels were not changed (Supplementary material online, Figure 1S). Four days of noise exposure also increased systolic and mean blood pressure (Figure 1A, C) while diastolic blood pressure did not change significantly (Figure 1B). Plasma catecholamine levels (noradrenaline, dopamine significantly and adrenaline by trend) and angiotensin II levels increased (Figure 1D–G). Cortisol levels in urine showed no significant change (although a trend for increased values in response to noise exposure) and were increased in kidney after 4 days of noise exposure (Figure 1H, I).
Figure 1.
Effects of noise for 1, 2, and 4 days on blood pressure and stress hormone release. Noise increased significantly systolic and mean arterial (A, C) but not diastolic (B) blood pressure. Noise increased noradrenalin, dopamine and angiotensin II levels significantly and adrenalin by trend (D–G). Cortisol levels in urine and kidney showed a weak trend for an increase under noise exposure, which was significant for kidney cortisol on day 4 (H, I). Data are mean ± SD from n = 8–16 mice/day (A–C), 8–11 (D), 7–8 (E), 9–11 (F), 7–12 (G), 6–14 (H) and 7–12 (I) mice/group.
Effects of noise exposure on vascular function
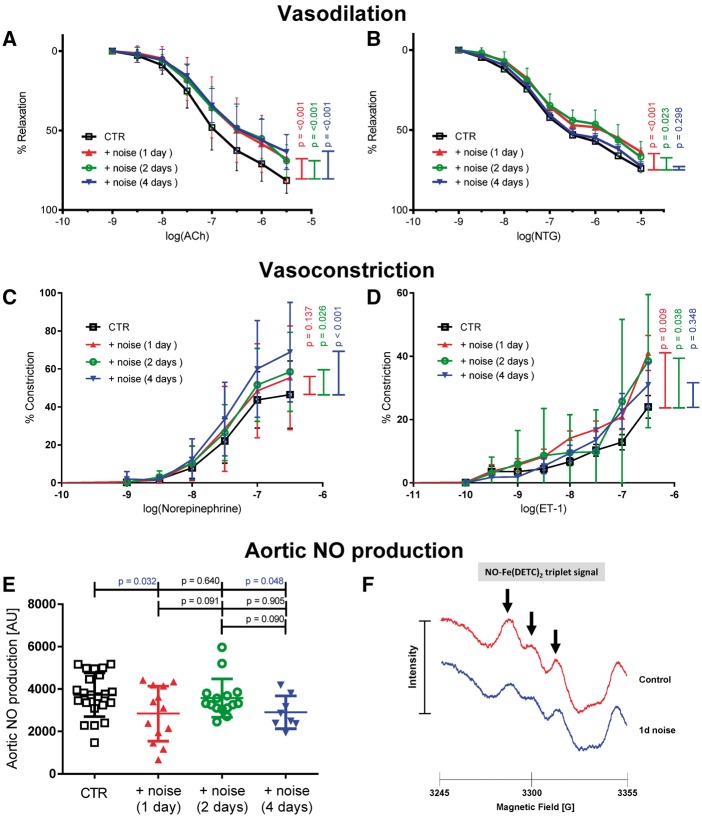
Noise exposure for 1, 2, and 4 days caused a significant attenuation of ACh-induced relaxation of mouse aorta (Figure 2A, Supplementary material online, Table 2S). Responses to the endothelium independent vasodilator GTN were also significantly modified (Figure 2B, Supplementary material online, Table 2S). Noise exposure induced an increase in sensitivity of the aorta to norepinephrine- and ET-1 mediated vasoconstriction (Figure 2C, D,Supplementary material online, Table 3S).
Figure 2.
Effects of noise on vascular function, sensitivity to vasoconstrictors and vascular NO production. Relaxation by the endothelium-dependent and -independent vasodilators acetylcholine (ACh, A) and nitroglycerin (NTG, B) were impaired by noise exposure. The sensitivity of the aorta to vasoconstrictors like norepinephrine (C) and endothelin-1 (D) was increased upon noise exposure. Noise exposure for 1 and 4 days significantly reduced the aortic NO production and bioavailability measured by EPR. (E) Quantification of the NO signal detected by Fe(DECT)2 spin trapping. (F) Representative NO traces of mice not exposed (Ctr.) and exposed to noise. For detailed statistical analysis see Supplementary material online, Tables 2S and 3S. Data are mean ± SD from n = 13–26 (A, B), 8–22 (C, D), 8–22 (E) mice/group.
Effects of noise exposure on eNOS expression, eNOS-mediated NO production and the functionality of the NO/cGMP signaling pathway
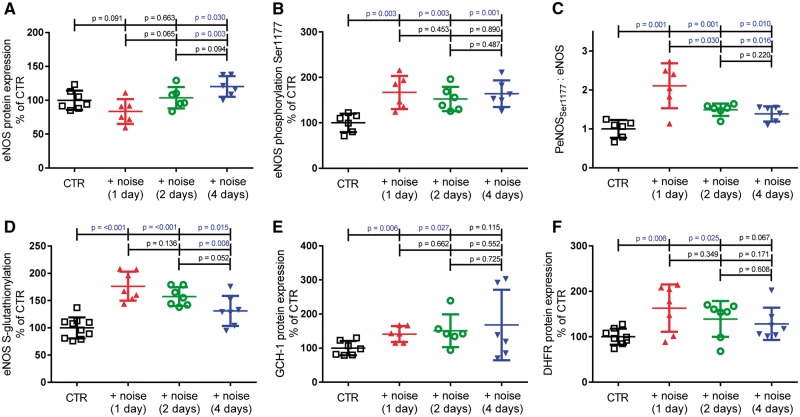
Endothelial dysfunction was paralleled by a decrease in vascular NO production assessed by electron paramagnetic resonance (EPR) (Figure 2E, F). Paradoxically, eNOS was up-regulated in vascular tissue on day 4 of noise exposure (Figure 3A) and phosphorylation of eNOS at Ser1177 was enhanced over the entire time period of noise exposure (Figure 3B, C). Since eNOS-mediated NO production was decreased despite up-regulation of eNOS expression and Ser1177 phosphorylation, we tested whether eNOS was uncoupled. Using DHE staining vascular superoxide production was increased in vessels from noise exposed animals and treatment with the eNOS inhibitor L-NAME consistently decreased endothelial superoxide production, identifying eNOS as a significant superoxide source (Supplementary material online, Figure 2S). Noise causes S-glutathionylation of eNOS, an established mechanism of eNOS uncoupling in the aorta (Figure 3D) and the heart (Figure 4H). The expression of GCH-1 and DHFR, both responsible for providing the eNOS cofactor tetrahydrobiopterin (BH4), were up-regulated, compatible with a counter regulatory response (Figure 3E, F).
Figure 3.
Effects of noise for 1, 2, and 4 days on endothelial NO-synthase protein expression and activity. (A–C) Endothelial NO synthase protein expression is increased after 4 days noise exposure and activating phosphorylation at Ser1177 is increased significantly at all time points measured. (D) eNOS S-glutathionylation as a surrogate marker for uncoupling of the protein was increased significantly at all time points of noise exposure. (E, F) Noise increased GTP-cyclohydrolase I (GCH-I) and dihydrofolate reductase (DHFR) expression leading to increased synthesis of the eNOS cofactor tetrahydrobiopterin (BH4) responsible for the coupling of the enzyme. Data are mean ± SD from n = 6–8 samples (pooled from 2 to 3 mice per sample) (A–C, E, F) and 7–10 samples (pooled from 2 mice per sample) (D).
Figure 4.
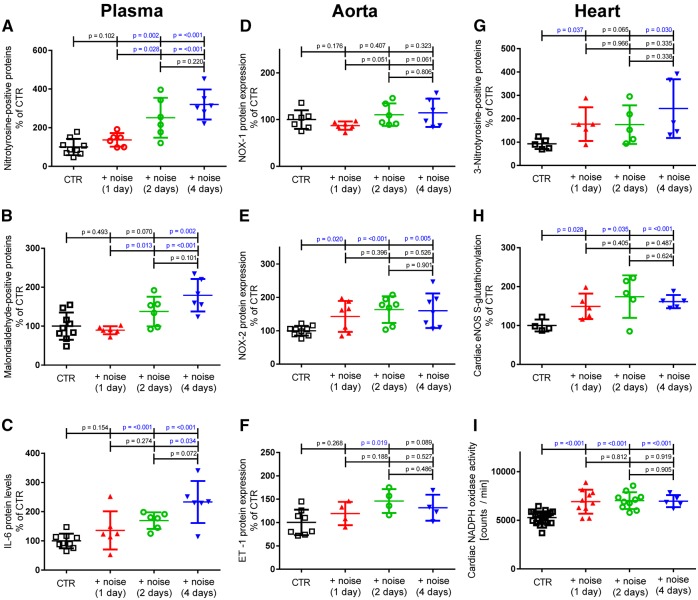
Effects of noise (1, 2, and 4 days) on oxidative stress markers in mouse plasma and vascular tissue. (A, B) Levels of 3-nitrotyrosine- and malondialdehyde-positive proteins, surrogate markers for oxidative stress, were significantly increased in mouse plasma. (C) IL-6 levels were significantly elevated in mouse plasma compatible with increased inflammation. (D, E) The vascular NADPH oxidase subunit NOX-2 was significantly up-regulated after noise exposure, while NOX-1 was not changed. (F) Endothelin-1 expression was increased in mouse aorta upon noise exposure. Cardiac 3-nitrotyrosine-positive proteins were significantly increased (G). Cardiac S-glutathionylation of eNOS, the marker for eNOS uncoupling, was increased on all days of noise exposure (H), which also correlated with cardiac NADPH oxidase activity as measured by NADPH (200 µM)-stimulated lucigenin (5 µM) ECL in heart membrane fractions (I). Data are mean ± SD from n = 6–9 (A–C), 4–9 samples (pooled from 2 to 3 mice per sample) (D–F), 4–5 samples/group (pooled from 2 to 3 mice per sample) (G, H) and n = 22 (Ctr), 10 (1 + 2 days), 5 (4 days) mice/group (I).
With respect to the NO/cGMP/cGK-I signaling pathway, we did not observe any changes in the expression of the sGC subunits (Supplementary material online, Figure 3S). However in parallel to the decrease in NO production on d1 we observed a decrease in the activity of cGK-I as assessed by the diminished phosphorylation of the VAsodilator-Stimulated Phosphoprotein at serine 239 (P-VASP) (Supplementary material online, Figure 3S).
Effects of noise exposure on ROS production in plasma, heart and the vasculature
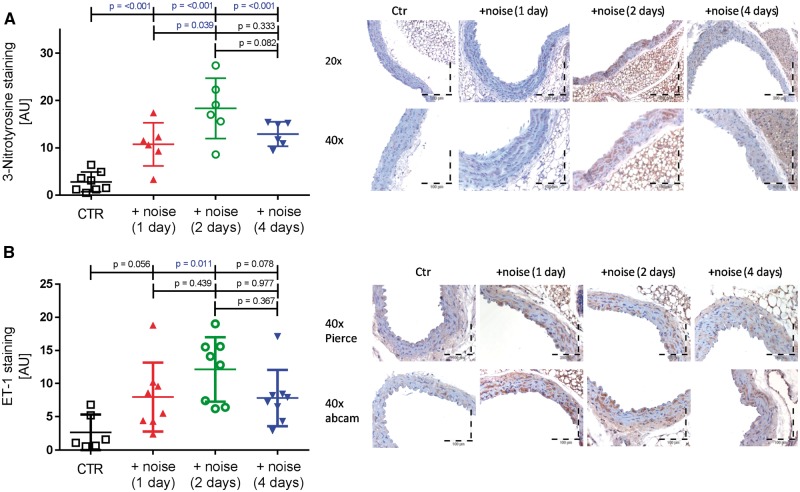
In plasma, noise exposure led to an increase in 3-nitrotyrosine-positive proteins (day 2–4), MDA-positive proteins (day 4) and interleukin 6 (day 2–4) as established by Dot Blot measurements (Figure 4A–C). In vascular tissue, noise exposure increased expression of the NADPH oxidase subunit NOX-2 (day 1–4) and ET-1 (day 2), while the NOX-1 subunit was not modified (Figure 4D–F). Likewise, we observed an increase in NADPH oxidase activity and 3-nitrotyrosine-positive proteins in heart homogenates (Figure 4G, I). Immunohistochemical analysis revealed that noise exposure enhanced 3-nitrotyrosine staining throughout the vasculature (day 1–4, Figure 5A), augmented 4-hydroxynonenal staining (day 1–4, Supplementary material online, Figure 2S) and increased vascular ET-1 levels on day 2, mainly within the endothelium (Figure 5B).
Figure 5.
Effects of 4 days noise on vascular 3-nitrotyrosine and ET-1 levels as assessed by immunohistochemistry. (A) Noise markedly increased immunostaining of 3-nitrotyrosine of intact aortic rings (brown color). The densitometric analysis revealed a significant increase in all noise-exposed groups. (B) Endothelin-1 immunostaining (brown color) is markedly increased in response to noise. The densitometric analysis showed significant progression of ET-1 protein expression on day 2 of noise exposure. Data are mean ± SD from n = 6–8 mice/group.
Effects of noise on gene expression in MLEC
Noise exposure caused a significant increase in eNOS, HO-1, PGC-1α and NOX-1 expression in freshly isolated mouse lung endothelial cells (Supplementary material online, Figure 4S) from noise-exposed animals. The changes in eNOS gene expression obtained in MLEC`s in response to noise parallel changes in the aorta.
Effects of noise on invasion of the vasculature with inflammatory cells
FACS analysis of mouse aorta revealed that noise exposure led to a significant increase of myelomonocytic cells and natural killer cells within the vasculature on day 1 or 4 (Supplementary material online, Figure 5S, panelsA, B). No significant increase in infiltration was observed for neutrophils (Supplementary material online, Figure 5S, panel C) and at least one significantly increased day for leucocytes in general as well as macrophages and monocytes (Supplementary material online, Figure 5S, panel D). No significant changes were observed for T cells (Supplementary material online, Figure 5S, panel D). The gating strategy for FACS analysis is shown in Supplementary material online, Figure 6S.
Effects of white noise on parameters of vascular function and oxidative stress
Exposure of mice to white noise did not change ACh-dependent relaxation (Supplementary material online, Figure 7S). Also other parameters of NO/cGMP signaling such as eNOS phosphorylation of eNOS at Ser1177 and of VASP at Ser239, BH4 generating enzymes GCH-1 and DHFR, sGC, cGK-1 showed no major changes in the white noise group (Supplementary material online, Figure 7S and 8S). Plasma 3-nitrotyrosine positive proteins and IL-6 were not changed (Supplementary material online, Figure 7S). Aortic NADPH oxidase subunits NOX-1 and NOX-2 were not up-regulated (Supplementary material online, Figure 7S) and endothelial superoxide formation was not changed with no indication of eNOS uncoupling as determined by L-NAME incubation (Supplementary material online, Figure 9S) and as supported by unaltered S-glutathionylation of eNOS (Supplementary material online, Figure 8S). Aortic ET-1 protein expression showed no major changes (Supplementary material online, Figure 7S).
Next generation sequencing
Comparative analysis of the transcriptomes of aortic tissue from noise treated animals vs. controls showed numerous differentially expressed genes. If a threshold of P < 0.05 and Log2 fold change ≥0.5 is applied, 224 genes were categorized as transcriptionally either up- or down-regulated over the entire experimental period. The majority of these genes are down-regulated. Depending on the length of noise treatment, the level of gene expression of individual genes can fluctuate (see Supplementary material online, Figure 10S). In Supplementary material online, Figure 11S, highly differentially expressed gene products from the NGS data are presented in box plots over day 1, 2, and 4 of noise treatment. The four strongest up-regulated genes compared with controls were Zbtb44, Setad4, Ypel2, and Ihh. Similarly, the amount of transcripts of Sacs, Nbeal1, PTPN4, and NR4A3 were significantly reduced by noise. In Supplementary material online, Tables 4S and 5S, the 30 most highly up- and down-regulated genes are listed. Pathway analysis by gene ontology annotation from NGS data revealed major changes in vascular smooth muscle cell (VSMC) contraction pathway and TGFβ- and Smad signalling (Supplementary material online, Figure 12S). Significant changes were detected in the NF-κB related pathway, adrenergic signal transduction, focal adhesion, cell cycle control, apoptosis, and kinase mediated growth and proliferation signaling centred around the Foxo transcription factors herein (Supplementary material online, Figures 13S and 14S). Changes were also observed in expression of genes being involved in the regulation of the circadian rhythm, insulin, and calcineurin signaling pathways.
Discussion
In this study, we introduce a novel animal model enabling study of the vascular consequences of chronic low level noise exposure.24 Aircraft noise (but not equal levels of white noise), applied for up to 4 days, increased circulating stress hormones and blood pressure, caused vascular (endothelial) dysfunction, eNOS uncoupling and increased oxidative stress within plasma and the vasculature, increased the expression of the NADPH oxidase and stimulated invasion of inflammatory cells in the vasculature. In addition, noise-exposed animals had significant changes of many important genes in part responsible for the regulation of vascular function, vascular remodelling and cell death.
Animal models of noise exposure
We employed substantially lower peak and mean sound pressure levels of noise (<85 dB(A); 72 dB(A)) than previously used in experimental conditions (100 dB(A)).22,23 This noise level was chosen since previous studies have shown that sound levels below 85 dB(A) are considered to be safe24 while higher levels (100 dB(A) and higher) have been demonstrated to be harmful to the cochlea and to cause hearing loss. Thus, vascular effects such as endothelial dysfunction observed in previous studies in response to extremely high noise levels (>100 dB(A)) and long exposure periods (2–4 weeks)22,23 might be, at least in part, secondary to direct effects of noise on the auditory system. In contrast, non-auditory effects were reported upon exposure to long-term noise with substantially lower intensities (70 and 85 dB(A)) leading to increased corticosterone levels, altered parameters of the endocrine glands, cardiac function and oxidative stress markers.24,25 Importantly, none of these studies investigated effects of noise on vascular function and vascular oxidative stress directly, nor on inflammatory markers and NGS.
Effects of noise on vascular function and oxidative stress
We have demonstrated that low levels of aircraft noise for 1–4 days cause an increase in stress hormone release and in circulating angiotensin II levels with significant stress-induced increase in blood pressure (Figure 1). Noise exposure also induced endothelial dysfunction with decreased vascular responses to the endothelium dependent vasodilator acetylcholine (Figure 2). This was paralleled by an increase in vascular sensitivity to vasoconstrictors norepinephrine and endothelin-1. Thus, using five-fold lower levels of noise, we reproduced previous observations of endothelial dysfunction of the aorta and the mesenteric artery as well as increases in sensitivity of the vasculature to vasoconstrictors in rats at sound levels of 100 dB(A).22,23
Endothelial dysfunction was associated with an increase in the expression of eNOS and a decrease in vascular NO production, as assessed by EPR, pointing to uncoupling of eNOS as a potential mechanism. Indirect evidence of eNOS uncoupling was provided by DHE fluorescence and L-NAME-dependent inhibition of eNOS-derived ROS formation. While L-NAME increased vascular superoxide levels in control vessels by reducing NO synthesis by functional eNOS (NO is a potent scavenger of superoxide), the inhibitor of eNOS decreased consistently detectable superoxide levels in vessels from animals exposed to noise for 1, 2, and 4 days identifying uncoupled eNOS as a significant superoxide source, which was further supported by eNOS S-glutathionylation, a marker of eNOS uncoupling.26
What are the mechanisms causing eNOS uncoupling? One concept suggests that increased endothelial superoxide formation from NADPH oxidase (NOX) isoforms, xanthine oxidase or mitochondria leads to increased oxidative break-down of NO yielding the highly reactive peroxynitrite,27,28 which may cause oxidation of the eNOS essential cofactor BH4 to the •BH3 radical29 leading to eNOS uncoupling. Indeed, we demonstrated substantially increased vascular tyrosine nitration within the endothelial cell layer (but also within the rest of the vasculature and in the plasma) in aircraft noise exposed animals, compatible with increased vascular (endothelial) peroxynitrite formation.30
A second mechanisms for eNOS uncoupling is S-glutathionylation of a critical cysteine residue in the reductase domain of eNOS.26 Immunoprecipitation experiments of eNOS revealed that there is substantial S-glutathionylation of eNOS fitting to the uncoupling concept. We also showed an increase in serine 1177 phosphorylation of eNOS and an increase in the expression of BH4 synthesis and recycling enzymes GCH-1 and DHFR, which may represent futile counter regulatory mechanisms to prevent eNOS uncoupling.
In addition to eNOS uncoupling we observed an increase in the expression of the NADPH oxidase subunit NOX-2 in aorta and an increase in the expression of NOX-1 in MLEC. The increase in NOX-2 in vascular tissue may be secondary to infiltration with inflammatory cells and showed that noise exposure increases the invasion of the vasculature with NK cells, myelomonocytic cells, leucocytes and macrophages/monocytes. The activation, adhesion and transmigration of immune cells to the vascular wall represent key steps for the development of arterial hypertension31,32 and these infiltrated immune cells provide the trigger for further stimulation of other vascular sources of oxidative stress leading to tissue damage.27,33 We also established an increase in vascular ET-1 production and an increase in circulating MDA-positive proteins and IL-6 levels, phenomena, which may be secondary to oxidative stress within the vasculature.34–36
The demonstration of vascular dysfunction and high oxidative stress fits to the results of our previous field studies in healthy subjects and patients with coronary artery disease.19,20 These studies showed that one night of aircraft noise is sufficient to cause an increase in stress hormone release19 and endothelial dysfunction,19,20 a phenomenon, which was reversed by the acute administration of the antioxidant vitamin C compatible with a noise-induced increase in vascular oxidative stress.19 Charakida and Deanfield proposed that noise-induced endothelial dysfunction may be primarily the consequence of increased vascular production of reactive oxygen species e.g. produced by the NADPH oxidase and/or secondary to infiltration of inflammatory cells in the vascular tissue,37 a concept which is now confirmed by the results of our translational studies.
Interestingly, the same mean noise levels caused by white noise failed to induce vascular dysfunction, oxidative stress and stress hormone release within a 4 days exposure period (Supplementary material online, Figures 7S, 8S, and 9S). This underlines the importance of the characteristics of the noise stimulus (pattern, frequency content, exposure time and intensity) besides the peak dB level. Thus, white noise is clearly less damaging to the vasculature within this short time frame compatible with recent observations that white noise can even provide benefit for patients undergoing coronary bypass surgery, probably by masking other annoying and potentially stress-inducing background noise in the coronary care unit.38
Effects of noise on aortic gene expression profile
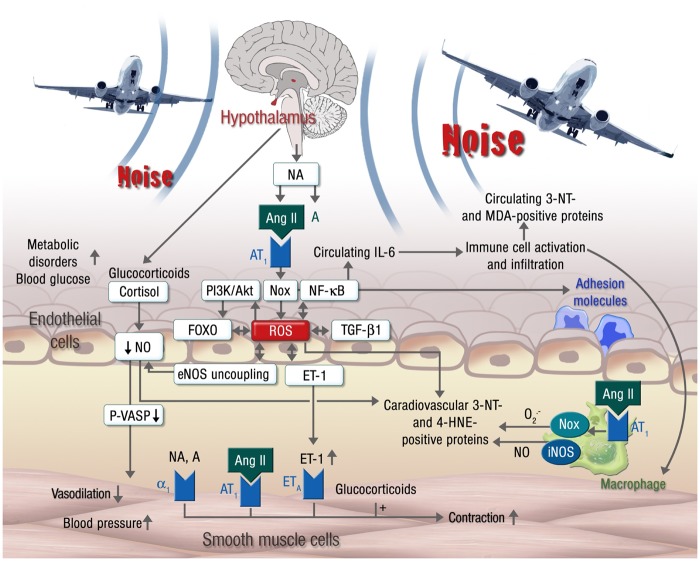
We also studied the effects of noise on the transcriptomes of aortic tissue. In an approach to interconnect the nitro-oxidative stress-induced modification of the eNOS/sGC/cGK-I pathway and the observed changes in the gene expression profile and signaling cascades (Figure 6, Supplementary material online, Figure 17S), we propose that gene expression has been altered by directed and undirected redox modifications/regulations of transcription factors (e.g. oxidation of zinc-finger motifs).
Figure 6.
Proposed mechanisms of aircraft noise-induced vascular dysfunction. Noise exposure leads to an over-activation of the sympathetic system, resulting in elevated levels of noradrenalin (NA), adrenalin (A) and angiotensin II (Ang II) and subsequently cortisol. Ang II, in turn, activates endothelial NADPH oxidase causing oxidative stress, which may induce direct scavenging of nitric oxide (NO) and eNOS uncoupling through oxidation of BH4 and eNOS S-glutathionylation. Reactive oxygen species (ROS) play a key role in linking different pathways, including PI3K/Akt signaling, the FOXO transcription factors, TGF-β1 and NF-κB signaling as well as the endothelin-1 (ET-1) system (see text for details), increasing the circulating levels of IL-6 and the expression of vascular adhesion molecules. Superoxide and nitric oxide produced by infiltrating immune cells (neutrophils, NK cells and monocytes/macrophages) promotes the formation of 3-nitrotyrosine-, malondialdehyde- and 4-hydroxynonenal-positive proteins and inflicts additional cellular oxidative damage. The uncoupling of eNOS not only reduces NO production, but also potentiates the pre-existing oxidative stress. Endothelial NO production is further reduced by glucocorticoids like cortisol, leading to impaired vasodilation and increased blood pressure. The overproduction of NA, A and ET-1 enhances contraction, which is further potentiated by glucocorticoids. All of these vascular alterations support the development of metabolic disorders as envisaged by increased blood glucose levels.
Aircraft noise exposure leads to a marked activation of the sympathetic nerve system, which in turn stimulates the renin angiotensin system (RAS). This leads to a stimulation of the phagocytic and non-phagocytic (vascular) NADPH oxidase causing increased ROS production and nitro-oxidative stress.39 Nitro-oxidative stress in turn activates the endothelin system, which will further increase vascular oxidative stress in a positive feedback fashion.33 Increased vascular peroxynitrite formation will cause a desensitization of soluble guanylyl cyclase and eNOS uncoupling, thereby further enhancing ROS production and impairing NO signaling (Figure 6, Supplementary material online, Figure 17S).40
ROS play a key role in linking the different pathways in the present NGS analysis. The IGF-1/Insulin/PI3K/Akt pathway, for instance, can be activated via redox-sensitive mechanisms.41 Subsequently, Akt regulates the activity of FOXO transcription factors by phosphorylation, which has a transcriptional factor binding site on the NR4A3 (not shown), Cu/Zn superoxide dismutase and glutathione peroxidase 1 gene promoter explaining at least in part the observed changes in transcription level of the NGS experiment.42 Oxidative stress also directly regulates transcription factors FOXO and NF-κB through reversible oxidation and reduction of cysteine residues,43 all of which may affect other transcription factors such as cysteine rich zinc-finger proteins like zbtb44 (see extended Discussion and Supplementary material online, Figures 11S, 13S, 14S, and 17S). The changes in FOXO factor activity and other transcription factors may modulate cellular resistance capacity to oxidative stress by regulating key detoxification enzymes (e.g. manganese superoxide dismutase and catalase).43 By a similar mechanism, TGF-β1 contributes to oxidative stress via decreasing the expression of antioxidant enzymes (e.g. superoxide dismutase, catalase, glutathione peroxidase, Figure 6 and Supplementary material online, Figure 17S).44 These events may result in increased vascular ROS production and reduced vascular NO-bioavailability in favor of the formation of the NO/superoxide reaction product peroxynitrite, leading to decreased cGMP concentrations and sGC sensitivity along with an inhibition of the activity of the cGMP dependent kinase (cGK-I), which is able to induce major structural and transcriptional changes in smooth muscle cells. cGK-I may interact with the TGFbeta/Smad pathway, MAPK-signaling as well as PI3K and FOXO pathways,45–47 which shows relevant changes in the NGS transcription data (Supplementary material online, Figures 12S, 14S, and 17S). Some of the pathways modulated by nitro-oxidative stress represent pathological mechanisms potentially mediating the detrimental effects of noise, while others are likely to reflect compensatory mechanisms in response to noise-induced injury.
The most strongly regulated genes in the NGS experiments depicted in Supplementary material online, Figure 11S are quite novel in the context of cardiovascular physiology, in part poorly understood (see extended Discussion). Their exact role in noise-induced pathophysiology, however, warrants further investigation.
Limitations of the study
Since the present study was based on short-term exposure to aircraft noise we cannot predict whether the observed increases in blood pressure in response to short-term noise exposure may ultimately lead to persistent arterial hypertension. Nevertheless, field studies in subjects with coronary artery disease and epidemiological studies demonstrated that exposure to traffic noise increases the risk of hypertension.16,20,48 Other traffic noise (road, railway) may share the adverse effects of aircraft noise as also shown in several clinical studies.
The presented NGS data do not reflect post-translational modifications of proteins (including kinases, phosphatases and transcription factors), which undergo substantial changes in an oxidative stress milieu largely affecting enzymatic function via sulfoxidation, S-nitros(yl)ation, S-glutathionylation but also phosphorylation.
The data on oxidative stress and NO/cGMP signaling were mainly collected in aorta or lung endothelial cells. Since blood pressure is largely determined by the tone of resistance vessels, the heterogeneity in the endothelium of these territories with respect to eNOS expression and activity, sensitivity to oxygen, stress hormones, vasoconstrictors, and generation of ROS is remarkable.
Another important aspect is the timeline of systemic and vascular changes induced by aircraft noise. Some increased continuously with duration of exposure to aircraft noise (e.g. plasma 3-nitrotyrosine, MDA and IL-6, aortic and lung eNOS protein) whereas others seemed to be more transiently regulated (e.g. aortic DHFR protein and ET-1 expression/dependent constriction, plasma catecholamine levels: up-regulation on day 1 or 2 with subsequent down-regulation on day 2 or 4). This may imply that some stress-triggered changes decline over time (potentially due to adaptation to the noise exposure or counter-regulatory mechanisms), while some changes represent more persistent alterations such as oxidative protein modifications and activation of transcription factors. Further investigations are required to elucidate whether the transient (acutely activated) processes account for the immediate adverse functional consequences of noise exposure (e.g. increased blood pressure, endothelial dysfunction, drop in P-VASP, activation/infiltration of immune cells), and whether ROS formation plays an essential role in rendering noise-induced damage from transient to persistent state.
The use of DHE staining assay for aortic ROS formation is a methodological limitation as the use of electron spin resonance-based techniques are strongly recommended.49 In addition, the lack of real markers of immune cell activation such as MCP-1/CCR-2, besides infiltration to the vascular wall, represents a limitation of the study (despite having characterized the different subsets of immune cells in the vascular wall, Supplementary material online, Figure 5S). Also markers of oxidative stress in immune cells would have been important indicators of their activation since we and others have previously shown that the presence of Nox2 in immune cells is required for their infiltration to vascular tissues.31,32
Conclusions and clinical implications
Short-term exposure to aircraft noise for 1–4 days (in contrast to white noise) causes vascular dysfunction primarily due to the stimulatory effects on vascular ROS production. The characteristics of noise-induced vascular dysfunction strikingly resemble the mechanisms of vascular dysfunction observed in hypercholesterolemia,50 arterial hypertension,51 chronic smoking52 and diabetes mellitus53 In addition, as hypothesized recently, the mechanisms of vascular dysfunction also resemble that of particulate matter-induced vascular dysfunction, suggesting that in the presence of both environmental stressors and especially pre-existing cardiovascular disease, additive adverse effects on vascular function may develop.2 Thus, based on epidemiological findings1–3 and now novel mechanistic insight provided by the current investigations, noise should be considered as a novel and significant environmental cardiovascular risk factor and should be mentioned in the ESC-guidelines for cardiovascular prevention.54 The strongest up- or down-regulation in genes with noise exposure modulated either transcription factors or genes involved at the top of signaling cascades, per se implying major changes in cellular signaling. Up to now it is not clear how the most strongly affected 8 genes contribute to the adverse cardiovascular changes observed after noise (Supplementary material online, Figure 11S). However, the on/off-like manner in which they are up- or down-regulated prompts speculation that they might represent so far uncharacterized (noise) stress-response genes. The most significant changes revealed by NGS were identified in vascular signaling, control of cell death and FOXO-based pathways for stress adaptation, all of which supports the functional data on endothelial dysfunction and oxidative stress. Our novel aircraft noise exposure animal model will enable study of the effects of noise mitigation maneuvers e.g. such as exercise and the efficacy of cardiovascular pharmacologic agents to prevent noise-induced vascular dysfunction.
Translational perspective
Environmental stressors such as air pollution and noise are getting more and more acknowledged as cardiovascular risk factors. While the adverse mechanisms of air pollution (especially particulate matter) on vascular function are well characterized, there is still a great need to develop experimental noise exposure models. Recently we demonstrated that nighttime aircraft noise causes in healthy volunteers endothelial dysfunction, which was partially corrected by the acute administration of vitamin C pointing to increased oxidative stress within the vasculature as a key mechanism. With the presented data we can demonstrate, in a novel experimental model, the adverse effects of noise exposure on stress hormone levels, haemodynamics, vascular function, oxidative stress and inflammation. We also characterized gene regulation in the vasculature in response to noise by performing next generation sequencing demonstrating major changes in gene expression being in part responsible for the regulation of vascular function, vascular remodelling, growth factor signaling and cell death. Thus, this animal model will allow to study the effects of noise mitigation strategies and pharmacological interventions on noise-induced vascular damage.
Supplementary material
Supplementary material is available at European Heart Journal online.
Supplementary Material
Acknowledgements
We are indebted to Angelica Karpi (University Medical Center Mainz, 55131 Mainz, Germany), Jörg Schreiner (University Medical Center Mainz, 55131 Mainz, Germany), Jessica Rudolph (University Medical Center Mainz, 55131 Mainz, Germany), Nicole Glas (University Medical Center Mainz, 55131 Mainz, Germany), and Bettina Mros (University Medical Center Mainz, 55131 Mainz, Germany) for expert technical assistance.
Funding
The present work was supported by a vascular biology research grant from the Boehringer Ingelheim Foundation for the collaborative research group; ‘Novel and neglected cardiovascular risk factors: molecular mechanisms and therapeutic implications’. The pilot studies were supported by a vascular biology research grant from the Foundation Heart of Mainz (S.S. and T.M.). T.M. is PI of the DZHK (German Center for Cardiovascular Research), Partner Site Rhine-Main, Mainz, Germany.
Conflict of interest: none declared.
References
- 1. Munzel T, Gori T, Babisch W, Basner M.. Cardiovascular effects of environmental noise exposure. Eur Heart J 2014;35:829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Munzel T, Sorensen M, Gori T, Schmidt FP, Rao X, Brook FR, Chen LC, Brook RD, Rajagopalan S.. Environmental stressors and cardio-metabolic disease: part II-mechanistic insights. Eur Heart J 2017;38:557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Munzel T, Sorensen M, Gori T, Schmidt FP, Rao X, Brook J, Chen LC, Brook RD, Rajagopalan S.. Environmental stressors and cardio-metabolic disease: part I-epidemiologic evidence supporting a role for noise and air pollution and effects of mitigation strategies. Eur Heart J 2017;38:550–556. [DOI] [PubMed] [Google Scholar]
- 4. Babisch W. Stress hormones in the research on cardiovascular effects of noise. Noise Health 2003;5:1–11. [PubMed] [Google Scholar]
- 5. Babisch W, Ising H, Gallacher JE.. Health status as a potential effect modifier of the relation between noise annoyance and incidence of ischaemic heart disease. Occup Environ Med 2003;60:739–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marvar PJ, Harrison DG.. Stress-dependent hypertension and the role of T lymphocytes. Exp Physiol 2012;97:1161–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marvar PJ, Vinh A, Thabet S, Lob HE, Geem D, Ressler KJ, Harrison DG.. T lymphocytes and vascular inflammation contribute to stress-dependent hypertension. Biol Psychiatry 2012;71:774–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nyberg ST, Fransson EI, Heikkila K, Ahola K, Alfredsson L, Bjorner JB, Borritz M, Burr H, Dragano N, Goldberg M, Hamer M, Jokela M, Knutsson A, Koskenvuo M, Koskinen A, Kouvonen A, Leineweber C, Madsen IE, Magnusson Hanson LL, Marmot MG, Nielsen ML, Nordin M, Oksanen T, Pejtersen JH, Pentti J, Rugulies R, Salo P, Siegrist J, Steptoe A, Suominen S, Theorell T, Vaananen A, Vahtera J, Virtanen M, Westerholm PJ, Westerlund H, Zins M, Batty GD, Brunner EJ, Ferrie JE, Singh-Manoux A, Kivimaki M, Consortium IP-W.. Job strain as a risk factor for type 2 diabetes: a pooled analysis of 124,808 men and women. Diabetes Care 2014;37:2268–2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Babu GR, Jotheeswaran AT, Mahapatra T, Mahapatra S, Kumar A Sr., Detels R, Pearce N.. Is hypertension associated with job strain? A meta-analysis of observational studies. Occup Environ Med 2014;71:220–227. [DOI] [PubMed] [Google Scholar]
- 10. Chida Y, Steptoe A.. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: a meta-analysis of prospective evidence. Hypertension 2010;55:1026–1032. [DOI] [PubMed] [Google Scholar]
- 11. Fransson EI, Nyberg ST, Heikkila K, Alfredsson L, Bjorner JB, Borritz M, Burr H, Dragano N, Geuskens GA, Goldberg M, Hamer M, Hooftman WE, Houtman IL, Joensuu M, Jokela M, Knutsson A, Koskenvuo M, Koskinen A, Kumari M, Leineweber C, Lunau T, Madsen IE, Hanson LL, Nielsen ML, Nordin M, Oksanen T, Pentti J, Pejtersen JH, Rugulies R, Salo P, Shipley MJ, Steptoe A, Suominen SB, Theorell T, Toppinen-Tanner S, Vahtera J, Virtanen M, Vaananen A, Westerholm PJ, Westerlund H, Zins M, Britton A, Brunner EJ, Singh-Manoux A, Batty GD, Kivimaki M.. Job strain and the risk of stroke: an individual-participant data meta-analysis. Stroke 2015;46:557–559. [DOI] [PubMed] [Google Scholar]
- 12. Booth J, Connelly L, Lawrence M, Chalmers C, Joice S, Becker C, Dougall N.. Evidence of perceived psychosocial stress as a risk factor for stroke in adults: a meta-analysis. BMC Neurol 2015;15:233.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sorensen M, Andersen ZJ, Nordsborg RB, Becker T, Tjonneland A, Overvad K, Raaschou-Nielsen O.. Long-term exposure to road traffic noise and incident diabetes: a cohort study. Environ Health Perspect 2013;121:217–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sorensen M, Andersen ZJ, Nordsborg RB, Jensen SS, Lillelund KG, Beelen R, Schmidt EB, Tjonneland A, Overvad K, Raaschou-Nielsen O.. Road traffic noise and incident myocardial infarction: a prospective cohort study. PLoS One 2012;7:e39283.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sorensen M, Hvidberg M, Andersen ZJ, Nordsborg RB, Lillelund KG, Jakobsen J, Tjonneland A, Overvad K, Raaschou-Nielsen O.. Road traffic noise and stroke: a prospective cohort study. Eur Heart J 2011;32:737–744. [DOI] [PubMed] [Google Scholar]
- 16. Sorensen M, Hvidberg M, Hoffmann B, Andersen ZJ, Nordsborg RB, Lillelund KG, Jakobsen J, Tjonneland A, Overvad K, Raaschou-Nielsen O.. Exposure to road traffic and railway noise and associations with blood pressure and self-reported hypertension: a cohort study. Environ Health 2011;10:92.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chang TY, Su TC, Lin SY, Jain RM, Chan CC.. Effects of occupational noise exposure on 24-hour ambulatory vascular properties in male workers. Environ Health Perspect 2007;115:1660–1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vienneau D, Schindler C, Perez L, Probst-Hensch N, Roosli M.. The relationship between transportation noise exposure and ischemic heart disease: a meta-analysis. Environ Res 2015;138:372–380. [DOI] [PubMed] [Google Scholar]
- 19. Schmidt FP, Basner M, Kroger G, Weck S, Schnorbus B, Muttray A, Sariyar M, Binder H, Gori T, Warnholtz A, Munzel T.. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur Heart J 2013;34:3508–314a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schmidt F, Kolle K, Kreuder K, Schnorbus B, Wild P, Hechtner M, Binder H, Gori T, Munzel T.. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin Res Cardiol 2015;104:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Said MA, El-Gohary OA.. Effect of noise stress on cardiovascular system in adult male albino rat: implication of stress hormones, endothelial dysfunction and oxidative stress. Gen Physiol Biophys 2016;35(3):371–7. [DOI] [PubMed] [Google Scholar]
- 22. Wu CC, Chen SJ, Yen MH.. Effects of noise on blood pressure and vascular reactivities. Clin Exp Pharmacol Physiol 1992;19:833–838. [DOI] [PubMed] [Google Scholar]
- 23. Wu CC, Chen SJ, Yen MH.. Attenuation of endothelium-dependent relaxation in mesenteric artery during noise-induced hypertension. J Biomed Sci 1994;1:49–53. [DOI] [PubMed] [Google Scholar]
- 24. Turner JG, Parrish JL, Hughes LF, Toth LA, Caspary DM.. Hearing in laboratory animals: strain differences and nonauditory effects of noise. Comp Med 2005;55:12–23. [PMC free article] [PubMed] [Google Scholar]
- 25. Gannouni N, Mhamdi A, Tebourbi O, El May M, Sakly M, Rhouma KB.. Qualitative and quantitative assessment of noise at moderate intensities on extra-auditory system in adult rats. Noise Health 2013;15:406–411. [DOI] [PubMed] [Google Scholar]
- 26. Chen CA, Wang TY, Varadharaj S, Reyes LA, Hemann C, Talukder MA, Chen YR, Druhan LJ, Zweier JL.. S-glutathionylation uncouples eNOS and regulates its cellular and vascular function. Nature 2010;468:1115–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Karbach S, Wenzel P, Waisman A, Munzel T, Daiber A.. eNOS uncoupling in cardiovascular diseases–the role of oxidative stress and inflammation. Curr Pharm Des 2014;20:3579–3594. [DOI] [PubMed] [Google Scholar]
- 28. Schulz E, Wenzel P, Munzel T, Daiber A.. Mitochondrial redox signaling: Interaction of mitochondrial reactive oxygen species with other sources of oxidative stress. Antioxid Redox Signal 2014;20:308–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kuzkaya N, Weissmann N, Harrison DG, Dikalov S.. Interactions of peroxynitrite, tetrahydrobiopterin, ascorbic acid, and thiols: implications for uncoupling endothelial nitric-oxide synthase. J Biol Chem 2003;278:22546–22554. [DOI] [PubMed] [Google Scholar]
- 30. Crow JP, Beckman JS.. Reaction between nitric oxide, superoxide, and peroxynitrite: footprints of peroxynitrite in vivo. Adv Pharmacol 1995;35:17–43. [DOI] [PubMed] [Google Scholar]
- 31. Wenzel P, Knorr M, Kossmann S, Stratmann J, Hausding M, Schuhmacher S, Karbach SH, Schwenk M, Yogev N, Schulz E, Oelze M, Grabbe S, Jonuleit H, Becker C, Daiber A, Waisman A, Munzel T.. Lysozyme M-positive monocytes mediate angiotensin II-induced arterial hypertension and vascular dysfunction. Circulation 2011;124:1370–1381. [DOI] [PubMed] [Google Scholar]
- 32. Guzik TJ, Hoch NE, Brown KA, McCann LA, Rahman A, Dikalov S, Goronzy J, Weyand C, Harrison DG.. Role of the T cell in the genesis of angiotensin II induced hypertension and vascular dysfunction. J Exp Med 2007;204:2449–2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Daiber A,D, Lisa F, Oelze M, Kroller-Schon S, Steven S, Schulz E, Munzel T.. Crosstalk of mitochondria with NADPH oxidase via reactive oxygen and nitrogen species signalling and its role for vascular function. Br J Pharmacol 2015; doi: 10.1111/bph.13403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kahler J, Ewert A, Weckmuller J, Stobbe S, Mittmann C, Koster R, Paul M, Meinertz T, Munzel T.. Oxidative stress increases endothelin-1 synthesis in human coronary artery smooth muscle cells. J Cardiovasc Pharmacol 2001;38:49–57. [DOI] [PubMed] [Google Scholar]
- 35. Kahler J, Mendel S, Weckmuller J, Orzechowski HD, Mittmann C, Koster R, Paul M, Meinertz T, Munzel T.. Oxidative stress increases synthesis of big endothelin-1 by activation of the endothelin-1 promoter. J Mol Cell Cardiol 2000;32:1429–1437. [DOI] [PubMed] [Google Scholar]
- 36. Knappe D, Sill B, Tharun B, Koester R, Baldus S, Muenzel T, Meinertz T, Kahler J.. Endothelin-1 in humans is increased by oxygen-derived radicals ex vivo and in vivo. J Investig Med 2007;55:306–314. [DOI] [PubMed] [Google Scholar]
- 37. Charakida M, Deanfield JE.. Nighttime aircraft noise exposure: flying towards arterial disease. Eur Heart J 2013;34:3472–3474. [DOI] [PubMed] [Google Scholar]
- 38. Farokhnezhad Afshar P, Bahramnezhad F, Asgari P, Shiri M.. Effect of white noise on sleep in patients admitted to a coronary care. J Caring Sci 2016;5:103–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Li H, Horke S, Forstermann U.. Oxidative stress in vascular disease and its pharmacological prevention. Trends Pharmacol Sci 2013;34:313–319. [DOI] [PubMed] [Google Scholar]
- 40. Daiber A, Steven S, Weber A, Shuvaev VV, Muzykantov VR, Laher I, Li H, Lamas S, Munzel T.. Targeting vascular (endothelial) dysfunction. Br J Pharmacol 2016; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Anselm E, Socorro VF, Dal-Ros S, Schott C, Bronner C, Schini-Kerth VB.. Crataegus special extract WS 1442 causes endothelium-dependent relaxation via a redox-sensitive Src- and Akt-dependent activation of endothelial NO synthase but not via activation of estrogen receptors. J Cardiovasc Pharmacol 2009;53:253–260. [DOI] [PubMed] [Google Scholar]
- 42. Tzivion G, Dobson M, Ramakrishnan G.. FoxO transcription factors; regulation by AKT and 14-3-3 proteins. Biochim Biophys Acta 2011;1813:1938–1945. [DOI] [PubMed] [Google Scholar]
- 43. Martins R, Lithgow GJ, Link W.. Long live FOXO: unraveling the role of FOXO proteins in aging and longevity. Aging Cell 2016;15:196–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Richter K, Konzack A, Pihlajaniemi T, Heljasvaara R, Kietzmann T.. Redox-fibrosis: Impact of TGFbeta1 on ROS generators, mediators and functional consequences. Redox Biol 2015;6:344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lincoln TM, Dey N, Sellak H.. Invited review: cGMP-dependent protein kinase signaling mechanisms in smooth muscle: from the regulation of tone to gene expression. J Appl Physiol (1985) 2001;91:1421–1430. [DOI] [PubMed] [Google Scholar]
- 46. Feil R, Lohmann SM, de Jonge H, Walter U, Hofmann F.. Cyclic GMP-dependent protein kinases and the cardiovascular system. Insights Genetic Modif Mice 2003;93:907–916. [DOI] [PubMed] [Google Scholar]
- 47. Gong K, Xing D, Li P, Hilgers RH, Hage FG, Oparil S, Chen YF.. cGMP inhibits TGF-beta signaling by sequestering Smad3 with cytosolic beta2-tubulin in pulmonary artery smooth muscle cells. Mol Endocrinol 2011;25:1794–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jarup L, Babisch W, Houthuijs D, Pershagen G, Katsouyanni K, Cadum E, Dudley ML, Savigny P, Seiffert I, Swart W, Breugelmans O, Bluhm G, Selander J, Haralabidis A, Dimakopoulou K, Sourtzi P, Velonakis M, Vigna-Taglianti F.. Team Hs Hypertension and exposure to noise near airports: the HYENA study. Environ Health Perspect 2008;116:329–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Griendling KK, Touyz RM, Zweier JL, Dikalov S, Chilian W, Chen YR, Harrison DG, Bhatnagar A, American Heart Association Council On Basic Cardiovascular S. Measurement of reactive oxygen species, reactive nitrogen species, and redox-dependent signaling in the cardiovascular system: a scientific statement from the American Heart Association. Circ Res 2016;119:e39–e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Oelze M, Mollnau H, Hoffmann N, Warnholtz A, Bodenschatz M, Smolenski A, Walter U, Skatchkov M, Meinertz T, Munzel T.. Vasodilator-stimulated phosphoprotein serine 239 phosphorylation as a sensitive monitor of defective nitric Oxide/cGMP signaling and endothelial dysfunction. Circ Res 2000;87:999–1005. [DOI] [PubMed] [Google Scholar]
- 51. Mollnau H, Wendt M, Szocs K, Lassegue B, Schulz E, Oelze M, Li H, Bodenschatz M, August M, Kleschyov AL, Tsilimingas N, Walter U, Forstermann U, Meinertz T, Griendling K, Munzel T.. Effects of angiotensin II infusion on the expression and function of NAD(P)H oxidase and components of nitric oxide/cGMP signaling. Circ Res 2002;90:E58–E65. [DOI] [PubMed] [Google Scholar]
- 52. Heitzer T, Brockhoff C, Mayer B, Warnholtz A, Mollnau H, Henne S, Meinertz T, Munzel T.. Tetrahydrobiopterin improves endothelium-dependent vasodilation in chronic smokers: evidence for a dysfunctional nitric oxide synthase. Circ Res 2000;86:E36–E41. [DOI] [PubMed] [Google Scholar]
- 53. Hink U, Li H, Mollnau H, Oelze M, Matheis E, Hartmann M, Skatchkov M, Thaiss F, Stahl RA, Warnholtz A, Meinertz T, Griendling K, Harrison DG, Forstermann U, Munzel T.. Mechanisms underlying endothelial dysfunction in diabetes mellitus. Circ Res 2001;88:E14–E22. [DOI] [PubMed] [Google Scholar]
- 54. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Richard Hobbs FD, Lochen ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, Bart van der Worp H, van Dis I, Monique Verschuren WM.. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Rev Esp Cardiol (Engl Ed) 2016;69:939. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.