Abstract
Background: With an increasing number of individuals surviving natural disasters, it is crucial to understand who is most at risk for developing post-traumatic stress disorder (PTSD). The objective of this study was to prospectively examine the role that pre-existing psychopathology plays in developing PTSD after a disaster.
Methods: This study uses data from a prospective 5-wave longitudinal cohort (years 2003-11) of Chilean adults from 10 health centres (N = 1708). At baseline, participants completed the Composite International Diagnostic Interview (CIDI), a comprehensive psychiatric diagnostic instrument. In 2010, the sixth most powerful earthquake on record struck Chile. One year later, a modified version of the PTSD module of the CIDI was administered. Marginal structural logistic regressions with inverse probability censoring weights were constructed to identify pre-disaster psychiatric predictors of post-disaster PTSD.
Results: The majority of participants were female (75.9%) and had a high-school/college education (66.9%). After controlling for pre-disaster PTSD, pre-existing dysthymia [odds ratio (OR) = 2.21; 95% confidence interval (CI) = 1.39-3.52], brief psychotic disorder (OR = 2.67; 95% CI = 1.21-5.90), anxiety disorders (not including PTSD; OR = 1.49; 95% CI = 1.27-1.76), panic disorder (OR = 2.46; 95% CI = 1.37-4.42), agoraphobia (OR = 2.23; 95% CI = 1.22-4.10), social phobia (OR = 1.86; 95% CI = 1.06-3.29), specific phobia (OR = 2.07; 95% CI = 1.50-2.86) and hypochondriasis (OR = 2.10; 95% CI = 1.05-4.18) were predictors of post-disaster PTSD. After controlling for pre-disaster anxiety disorders, dysthymia, and non-affective psychotic disorders, individuals with pre-disaster PTSD (vs those without pre-disaster PTSD) had higher odds of developing post-disaster PTSD (OR = 2.53; 95% CI = 1.37-4.65).
Conclusions: This is the first Chilean study to demonstrate prospectively that pre-disaster psychiatric disorders, independent of a prior history of other psychiatric disorders, increase the vulnerability to develop PTSD following a major natural disaster.
Keywords: PTSD, natural disaster, Latin America, longitudinal cohort, Chile, adult
Introduction
Between 2001 and 2010, there was an average of 384 natural disasters each year, affecting 232 million victims worldwide.1 However, because catastrophes are unpredictable, the vast majority of studies examining their psychological impacts, such as PTSD, do not have pre-disaster psychiatric data.2 Therefore, post-disaster-only designs ignore the effect of pre-existing psychopathologies on the incidence and prevalence of subsequent PTSD.3–5 Additionally, the majority of information on disaster-related PTSD is based on cross-sectional studies only and typically on convenience samples.6 These limitations have resulted in few advances in understanding the effects of previous psychiatric events on post-disaster PTSD, leading to a lack of clarity on appropriate secondary prevention interventions for disaster victims most at risk of developing adverse psychological outcomes.7 With an increasing number of individuals surviving natural disasters in the general population, it is critical to determine who is at elevated risk for developing PTSD when faced with a trauma, with the overall goal of reducing the incidence of PTSD.8–11
On 27 February 2010, the sixth most powerful earthquake on record since 1900, measuring 8.8 on the Richter Scale, struck the coast of central Chile.12 This disaster resulted in at least 523 deaths and left 24 people missing, 12 000 injured, 800 000 displaced and hundreds of thousands of buildings damaged or destroyed.12 The province of Concepciόn was the major urban centre that experienced the most damage. In addition to the earthquake, a 2.35 meter tsunami wave hit Talcahuano, causing further damage.12 As the Chilean disaster occurred in the midst of an existing longitudinal prospective cohort study, the current analysis provides a rare opportunity to study adults located at the epicentre of the disaster who had undergone a structured diagnostic psychiatric interview before exposure to a major traumatic event.
The main objective of this study was to identify the strongest pre-disaster psychiatric predictors of post-disaster PTSD.13–22 We had three hypotheses: (i) individuals with pre-disaster PTSD will have a higher probability of developing post-disaster PTSD, compared with those with no pre-disaster PTSD; (ii) pre-existing psychiatric disorders will increase the risk for post-disaster PTSD, independent of a previous history of PTSD; and (iii) individuals with pre-disaster PTSD will have a higher probability of developing post-disaster PTSD (compared with those with no pre-disaster PTSD), independent of a previous history of other psychiatric disorders.
Methods
The PREDICT s tudy
The PREDICT study took place in six European and one Latin American country (Chile), with the aim of developing a multi-factor risk index to predict onset of depression among primary care attendees.23–25 In Chile, a sample of 3000 adults were recruited by the University of Concepciόn from 10 primary care centres from the national health care service (used by ∼75% of the population) in Concepciόn and Talcahuano.23 Participants were consecutively selected from daily patient logs based on the age and gender distribution of the primary care centres.23 Of the 3000 participants that initially agreed to participate, 2839 completed the baseline assessment (94.6%). Wave 1 (baseline) occurred in 2003, and included a comprehensive psychiatric assessment [Composite International Diagnostic Interview (CIDI), Spanish version 2.126]. Waves 2-4 occurred 6-24 months later but either did not include PTSD assessments or involved subsamples only. Wave 5 occurred in 2011 (1 year after the disaster), and included a post-disaster PTSD assessment. Data from Waves 1 (hereinafter referred as ‘pre-disaster data’) and 5 (hereinafter referred as ‘post-disaster data’) will be used for the current analyses.
Study d esign
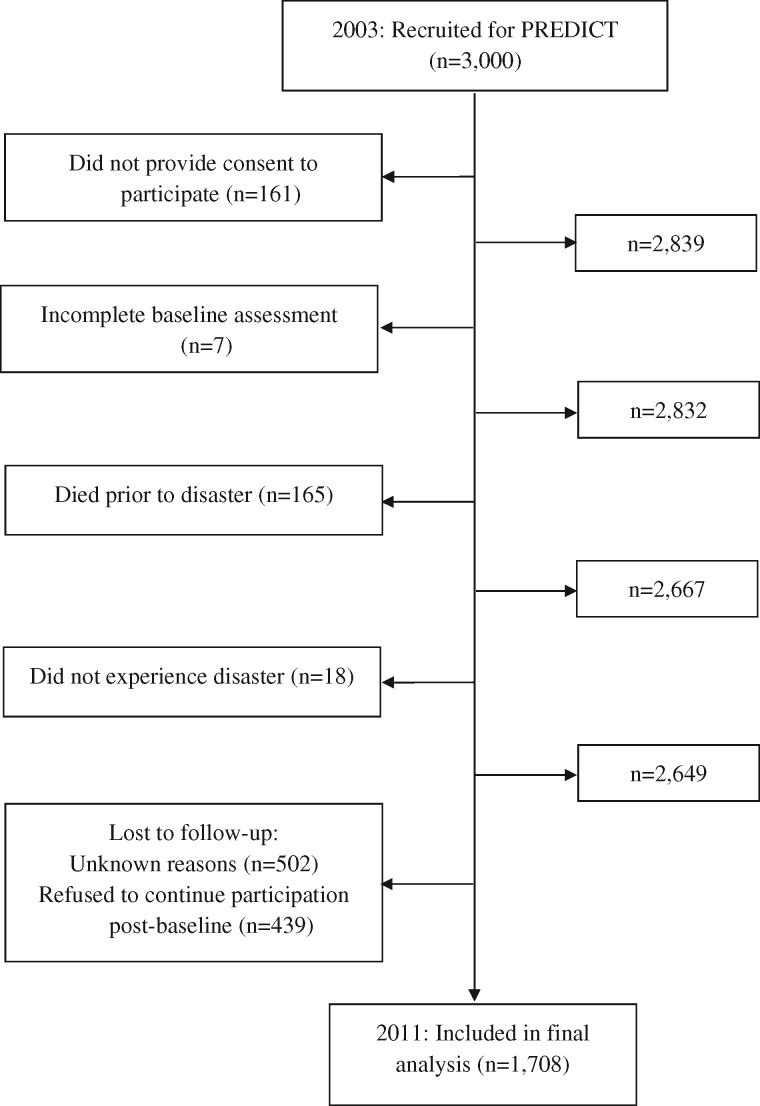
The current study used pre- and post-disaster data from the PREDICT study (N = 1708). A flow chart of how the analytical sample was obtained is illustrated in Figure 1. The institutional review board (IRB) at the University of Concepciόn approved this study.
Figure 1.
Flow diagram of excluded/ineligible individuals: The PREDICT study (2003-2011) .
Measurements
Dependent variable: post-disaster PTSD
One year after the disaster, a modified version of the PTSD module of the CIDI (described below) Spanish version 2.126 was used as the primary outcome (hereinafter referred to as ‘post-disaster PTSD’). This interview assessed all 21 PTSD symptoms from the DSM-IV-TR,27 and was tailored such that the only potentially traumatic event that could be endorsed was if the participant was involved in the 2010 disaster. All questions were anchored to the 2010 disaster as the point of reference. For example, the questions that assessed for avoidance was: ‘Were you trying to force yourself to not think or talk about the earthquake/tsunami?’. No other modules from the CIDI were used in the post-disaster assessment.
Independent variables: pre-disaster psychiatric disorders
The majority of pre-disaster psychiatric disorder information was measured via the CIDI Spanish version 2.1.26 The CIDI is a comprehensive, fully structured psychiatric diagnostic instrument that generates lifetime and current Axis I mental disorders by means of computerized algorithms according to ICD-10 and DSM-IV criteria.28 The CIDI has good psychometric properties, with excellent inter-rater reliability, good test-retest reliability and good validity.29 It is the most widely used interview in large psychiatric epidemiological studies worldwide. The CIDI is administered by lay interviewers, does not use outside informants or medical records and does not assume the presence of a current disorder.30 The Chilean CIDI is an official World Health Organization (WHO) Spanish version.31,32 A validation study of this instrument indicated an overall kappa statistic of 0.94 (with anxiety disorders having a kappa of 0.85).33
In the current study, a lifetime pre-disaster PTSD diagnosis was the primary exposure of interest (hereinafter referred to as ‘pre-disaster PTSD’). This PTSD module assessed all 21 PTSD symptoms from the DSM-IV-TR,27 and a PTSD diagnosis could be a result of a variety of potentially traumatic events (e.g. combat, rape). The only pre-disaster disorder not based on the CIDI was substance misuse. Participants who had an elevated score (≥ 8) from the Alcohol Use Disorders Identification Test34 or reported ever using illicit drugs were categorized as having substance misuse.
Pre-disaster confounder variables
The potential pre-disaster confounder variables were based on background literature regarding known risk factors for PTSD:35-37 age, gender, educational attainment and family history of psychiatric disorders (i.e. if any self-reported family members had mental illness or committed suicide). The demographic confounder variables were obtained from the baseline CIDI assessment. Family history of psychiatric disorders was obtained from a questionnaire designed specifically for the PREDICT study. Controlling for confounding did not change the effect estimates (results not shown); therefore, the more parsimonious models are presented.
Loss to f ollow-up
Sensitivity analysis
Due to the longitudinal design of the secondary data analysis, there is potential for selection bias due to differential loss to follow-up. A sensitivity analysis using χ2 and multivariable logistic regression analyses was conducted to examine the participant characteristics of those who were lost to follow-up (n = 941 [33.1%]; Figure 1). Of note, those who died before Wave 5 did not have higher levels of baseline PTSD (results not shown). Among the 941 individuals who were lost to follow-up, there were more females than males (69% vs 30%; χ2 = 14.84, p < 0.001), more individuals with a high-school/college education compared with lower levels of educational attainment (73.4% vs 26.6%; χ2 = 11.89, p = 0.001), and more individuals who were not middle-aged relative to those who were middle-aged (45-55 years; 83.5% vs 16.5%; χ2 = 4.71, p = 0.03). Additionally, among those lost to follow-up, there were no differences among those with pre-disaster PTSD vs those with no pre-disaster PTSD diagnosis (16.5% vs 83.5%; χ2 = 0.03, p = 0.87). Multivariable logistic regression models predicting loss to follow-up replicated these findings (results not shown).
Inverse probability weights
To mitigate the potential selection bias due to differential loss to follow-up, stabilized inverse probability censoring weighting methods (IPCW) were used. Unlike standard regression models, IPCW re-weights the study population such that the contributions of individuals who share characteristics of those who dropped out, but who remain in the study, are increased.38 If IPCW model specification is correct, potential biases arising due to selection bias are mitigated. A detailed description of this methodology is documented elsewhere.38–40 To estimate the weights, we modelled each participant’s probability of not dropping out based on each participant’s exposure (pre-disaster PTSD) and confounder values, using a logistic regression model. The confounders included in the weights were gender and age because they predicted loss to follow-up and were associated with both pre- and post-disaster PTSD. Although education also was a predictor of loss to follow-up, it was not included in the weights because subsequent analyses indicated that education was not associated with both pre- and post-disaster PTSD (i.e. not a confounding variable). The formula for calculating the stabilized IPCW was as follows:
where:
C: Participant lost to follow-up (1 = yes, 0 = no}
A: Pre-disaster PTSD (1 = yes, 0 = no)
L1: Gender (1 = female, 0 = male)
L2: Age [1 = middle age, 0 = not middle age])
The final set of weights can be described as the number of participants who are like individual i in terms of their exposure and confounder values, who would have been in the risk set at time t in the absence of dropout. Individuals are up-weighted if they do not drop out but have the highest probability (based on his/her exposure and confounder values) of dropout. In sum, the IPCW weights create a pseudo-population that would have been observed had dropout been random (with respect to exposure and confounder values). The stabilization of the weights was used to preserve the amount of information in the observed data and to minimize variability of the weights.41
Statistical a nalyses
We first calculated frequencies of baseline demographic variables and pre-disaster Axis I disorders. The prevalence of post-disaster PTSD was subsequently calculated in relation to each variable. Of note, age was collapsed into ‘middle age’ or ‘not middle age’ (i.e. 45-55 years vs other) because subsequent post hoc analyses only showed significant differences for these two age groups. Additionally, education was collapsed into ‘illiterate/elementary school’ or ‘high-school/college’, and alcohol misuse and illicit drugs were collapsed into ‘substance misuse’ for the same reason.
To identify the most robust pre-disaster predictors of post-disaster PTSD, marginal structural logistic models (with robust error variance estimators) were used, with post-disaster PTSD as the outcome. Independent variables that were associated with post-disaster PTSD (after controlling for pre-disaster PTSD) and had sufficient sample sizes were used in the final marginal structural logistic models to determine if pre-disaster PTSD remained an independent predictor after controlling for other pre-disaster Axis I disorders. Although several individual anxiety disorders were associated with post-disaster PTSD, these were collapsed into a single category ‘anxiety disorders’, to maintain statistical power and because controlling for the disorders individually did not substantially change the odds ratio coefficients. STATA MP version 12 and SAS version 9.22 were used for data management and statistical analyses.42,43
Results
Description of s ample
The majority of the sample was female (75.9%), not middle-aged (80.1%) and had a high-school/college education (66.9%; Table 1). The majority of the sample had at least one lifetime pre-disaster psychiatric disorder (62.3%). Approximately 11.5% (n = 196) of the total sample had pre-disaster PTSD, 10.2% (n = 175) of individuals had post-disaster PTSD and 2% (n = 34) of the sample had both pre-disaster and post-disaster PTSD. The most common pre-disaster disorder categories were mood disorders (30.4%) and anxiety disorders (not including PTSD; 41.4%), whereas the least common pre-disaster disorder categories were eating disorders (1%) and non-affective psychotic disorders (2.6%). Among those with post-disaster PTSD, most had a pre-disaster anxiety disorder (58.9%), followed by pre-disaster mood disorders (38.9%).
Table 1.
Demographic and psychiatric information of 2010 Chilean disaster victims: the PREDICT study (2003-11)
| Pre-disaster characteristic | Total sample (n = 1708) |
Individuals with post-disaster PTSD (n = 175) |
||
|---|---|---|---|---|
| n | % | n | % | |
| Gender | ||||
| Male | 412 | 24.1 | 25 | 14.3 |
| Female | 1296 | 75.9 | 150 | 85.7 |
| Age | ||||
| 45-54 | 340 | 19.9 | 51 | 29.1 |
| < 45 and 55+ | 1368 | 80.1 | 124 | 70.9 |
| Education | ||||
| High school/college | 1142 | 66.9 | 112 | 64.0 |
| Illiterate/elementary school | 564 | 33.0 | 63 | 36.0 |
| Unknown | 2 | 0.1 | – | – |
| Family history of psychiatric disorders/suicide | ||||
| Yes | 305 | 17.9 | 37 | 21.1 |
| No | 1403 | 82.1 | 138 | 78.9 |
| Pre-disaster potentially traumatic events | ||||
| Combat | ||||
| Yes | 12 | 0.7 | 2 | 1.1 |
| No | 1692 | 99.1 | 173 | 98.9 |
| Rape | ||||
| Yes | 118 | 6.9 | 12 | 6.9 |
| No | 1586 | 92.9 | 163 | 93.1 |
| Missing | 4 | 0.2 | – | – |
| Molested | ||||
| Yes | 239 | 14.0 | 29 | 16.6 |
| No | 1465 | 85.8 | 146 | 83.4 |
| Missing | 4 | 0.2 | – | – |
| Life-threatening accident | ||||
| Yes | 363 | 21.3 | 32 | 18.3 |
| No | 1341 | 78.5 | 143 | 81.7 |
| Missing | 4 | 0.2 | – | – |
| Disaster | ||||
| Yes | 377 | 22.1 | 40 | 22.9 |
| No | 1327 | 77.7 | 135 | 77.1 |
| Missing | 4 | 0.2 | – | – |
| Witness others’ injury/death | ||||
| Yes | 517 | 30.3 | 54 | 30.9 |
| No | 1187 | 69.5 | 121 | 69.1 |
| Missing | 4 | 0.2 | – | – |
| Physically assaulted/attacked | ||||
| Yes | 378 | 22.1 | 49 | 28.0 |
| No | 1326 | 77.6 | 126 | 72.0 |
| Missing | 4 | 0.2 | – | – |
| Threatened with weapon/kidnapped | ||||
| Yes | 175 | 10.3 | 21 | 12.0 |
| No | 1529 | 89.5 | 154 | 88.0 |
| Missing | 4 | 0.2 | – | – |
| Tortured | ||||
| Yes | 16 | 0.9 | 1 | 0.6 |
| No | 1688 | 98.8 | 174 | 99.4 |
| Missing | 4 | 0.2 | – | – |
| Other | ||||
| Yes | 115 | 6.7 | 11 | 6.3 |
| No | 1589 | 93.0 | 164 | 93.7 |
| Missing | 4 | 0.2 | – | – |
| Childhood psychological abuse | ||||
| Yes | 541 | 31.7 | 71 | 40.6 |
| No | 1165 | 68.2 | 104 | 59.4 |
| Missing | 2 | 0.1 | – | – |
| Childhood physical abuse | ||||
| Yes | 658 | 38.5 | 77 | 44.0 |
| No | 1048 | 61.4 | 98 | 56.0 |
| Missing | 2 | 0.1 | – | – |
| Childhood sexual abuse | ||||
| Yes | 161 | 9.4 | 18 | 10.3 |
| No | 1545 | 90.5 | 157 | 89.7 |
| Missing | 2 | 0.1 | – | – |
| Any Pre-disaster disorder | ||||
| Yes | 1064 | 62.3 | 142 | 81.1 |
| No | 644 | 37.7 | 33 | 18.9 |
| Pre-disaster lifetime psychiatric diagnosis | ||||
| Eating disorders | ||||
| Yes | 17 | 1.0 | 2 | 1.1 |
| No | 1691 | 99.0 | 173 | 98.9 |
| Anorexia | ||||
| Yes | 0 | 0 | 0 | 0 |
| No | 1706 | 99.9 | 175 | 100.0 |
| Unknown | 2 | 0.1 | – | – |
| Bulimia | ||||
| Yes | 17 | 1.0 | 2 | 1.1 |
| No | 1691 | 99.0 | 173 | 98.9 |
| Mood disorders | ||||
| Yes | 520 | 30.4 | 68 | 38.9 |
| No | 1888 | 69.6 | 107 | 61.1 |
| Major depressive disorder | ||||
| Yes | 417 | 24.4 | 46 | 26.3 |
| No | 1284 | 75.2 | 129 | 73.7 |
| Unknown | 7 | 0.4 | – | – |
| Bipolar I | ||||
| Yes | 36 | 2.1 | 7 | 4.0 |
| No | 1672 | 97.9 | 168 | 96.0 |
| Bipolar II | ||||
| Yes | 0 | 0 | 0 | 0 |
| No | 1697 | 99.4 | 175 | 100.0 |
| Unknown | 11 | 0.6 | – | – |
| Dysthymia | ||||
| Yes | 133 | 7.8 | 28 | 16.0 |
| No | 1557 | 91.2 | 146 | 83.4 |
| Unknown | 18 | 1.1 | 1 | 0.6 |
| Non-affective psychotic disorders | ||||
| Yes | 45 | 2.6 | 10 | 5.7 |
| No | 1658 | 97.1 | 165 | 94.3 |
| Unknown | 5 | 0.3 | – | – |
| Schizophrenia | ||||
| Yes | 6 | 0.4 | 1 | 0.6 |
| No | 1632 | 95.6 | 164 | 93.7 |
| Unknown | 70 | 4.1 | 10 | 5.7 |
| Schizophreniform | ||||
| Yes | 1 | 0.1 | 0 | 0 |
| No | 1692 | 99.1 | 175 | 100.0 |
| Unknown | 15 | 0.9 | – | – |
| Schizoaffective | ||||
| Yes | 2 | 0.1 | 0 | 0 |
| No | 1686 | 98.7 | 174 | 99.4 |
| Unknown | 20 | 1.2 | 1 | 0.6 |
| Delusional | ||||
| Yes | 0 | 0 | 0 | 0 |
| No | 1657 | 97.0 | 170 | 97.1 |
| Unknown | 51 | 3.0 | 5 | 2.9 |
| Brief psychotic | ||||
| Yes | 37 | 2.2 | 9 | 5.1 |
| No | 1581 | 92.6 | 157 | 89.7 |
| Unknown | 90 | 5.3 | 9 | 5.1 |
| Anxiety disorders (not including PTSD) | ||||
| Yes | 707 | 41.4 | 103 | 58.9 |
| No | 1001 | 58.6 | 72 | 41.1 |
| Obsessive compulsive disorder | ||||
| Yes | 24 | 1.4 | 2 | 1.1 |
| No | 1603 | 93.9 | 162 | 92.6 |
| Unknown | 81 | 4.7 | 11 | 6.3 |
| PTSD | ||||
| PTSD | 196 | 11.5 | 34 | 19.4 |
| Any diagnosis except PTSD | 868 | 50.8 | 108 | 61.7 |
| No diagnosis | 644 | 37.7 | 33 | 18.9 |
| Panic | ||||
| Yes | 75 | 4.4 | 17 | 9.7 |
| No | 1622 | 95.0 | 154 | 88.0 |
| Unknown | 11 | 0.6 | 4 | 2.3 |
| Agoraphobia | ||||
| Yes | 70 | 4.1 | 15 | 8.6 |
| No | 1613 | 94.4 | 155 | 88.6 |
| Unknown | 25 | 1.5 | 5 | 2.9 |
| Social phobia | ||||
| Yes | 90 | 5.3 | 17 | 9.7 |
| No | 1595 | 93.4 | 155 | 88.6 |
| Unknown | 23 | 1.4 | 3 | 1.7 |
| Generalized anxiety | ||||
| Yes | 20 | 1.2 | 4 | 2.3 |
| No | 1684 | 98.6 | 171 | 97.7 |
| Unknown | 4 | 0.2 | – | – |
| Specific phobia | ||||
| Yes | 659 | 38.6 | 98 | 56.0 |
| No | 1044 | 61.1 | 77 | 44.0 |
| Unknown | 5 | 0.3 | – | – |
| Somatoform disorders | ||||
| Yes | 177 | 10.4 | 25 | 14.3 |
| No | 1531 | 89.6 | 150 | 85.7 |
| Somatization | ||||
| Yes | 1 | 0.1 | 0 | 0 |
| No | 1705 | 99.8 | 175 | 100.0 |
| Unknown | 2 | 0.1 | – | – |
| Conversion | ||||
| Yes | 89 | 5.2 | 13 | 7.4 |
| No | 1491 | 87.3 | 145 | 82.9 |
| Unknown | 128 | 7.5 | 17 | 9.7 |
| Pain | ||||
| Yes | 104 | 6.1 | 14 | 8.0 |
| No | 1467 | 85.9 | 144 | 82.3 |
| Unknown | 137 | 8.0 | 17 | 9.7 |
| Hypochondriasis | ||||
| Yes | 57 | 3.3 | 11 | 6.3 |
| No | 1645 | 96.3 | 164 | 93.7 |
| Unknown | 6 | 0.4 | – | – |
| Substance misuse | ||||
| Yes | 231 | 13.5 | 30 | 17.1 |
| No | 1477 | 86.5 | 145 | 82.9 |
Missing pre-disaster disorders were not counted in the grouped disorder categories; estimates presented are un-weighted.
Marginal structural logistic regression models
Table 2 displays the predictors associated with developing post-disaster PTSD, after weighing the sample by gender and age. Dysthymia, non-affective psychotic disorders, any anxiety disorder (not including PTSD), panic disorder, agoraphobia, social phobia and specific phobia were associated with post-disaster PTSD. Compared with those with no diagnosis, individuals with pre-disaster PTSD had higher odds of developing post-disaster PTSD.
Table 2.
Marginal structural logistic regression models predicting post-disaster PTSD in Chilean disaster victims (N = 1708): the PREDICT study (2003-11)
| Pre-disaster independent variable | Age and gender weighted* |
Age and gender weighted,* adjusted for pre-disaster PTSD |
|||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | ||
| Model 1: | Education | ||||||
| High school/college | 0.86 | 0.62-1.19 | 0.354 | 0.87 | 0.63-1.21 | 0.419 | |
| Illiterate/elementary school | 1.0 | – | – | 1.0 | – | – | |
| Model 2: | Family history of psychiatric disorders/suicide | ||||||
| Yes | 1.27 | 0.86-1.87 | 0.229 | 1.16 | 0.78-1.72 | 0.460 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 3: | Any diagnosis | ||||||
| Yes | 2.90 | 1.96-4.30 | 0.000 | 2.67 | 1.78-4.00 | 0.000 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 4: | Eating disorders | ||||||
| Yes | 1.20 | 0.27-5.28 | 0.813 | 1.02 | 0.23-4.52 | 0.981 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 5: | Bulimia | ||||||
| Yes | 1.20 | 0.27-5.28 | 0.813 | 1.02 | 0.23-4.52 | 0.981 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 6: | Mood disorders | ||||||
| Yes | 1.54 | 1.12-2.13 | 0.009 | 1.40 | 1.01-1.96 | 0.046 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 7: | Major depressive disorder | ||||||
| Yes | 1.13 | 0.79-1.62 | 0.488 | 1.06 | 0.74-1.53 | 0.752 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 8: | Bipolar I | ||||||
| Yes | 2.16 | 0.93-5.01 | 0.073 | 1.83 | 0.79-4.23 | 0.158 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 9: | Dysthymia | ||||||
| Yes | 2.56 | 1.63-4.02 | 0.000 | 2.21 | 1.39-3.52 | 0.001 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 10: | Non-affective psychotic disorders | ||||||
| Yes | 2.72 | 1.32-5.59 | 0.007 | 2.42 | 1.17-5.02 | 0.017 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 11: | Schizophrenia | ||||||
| Yes | 2.03 | 0.24-17.51 | 0.519 | 1.73 | 0.23-12.94 | 0.593 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 12: | Brief psychotic disorder | ||||||
| Yes | 3.02 | 1.40-6.53 | 0.005 | 2.67 | 1.21-5.90 | 0.015 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 13: | Anxiety disorders (not including PTSD) | ||||||
| Yes | 2.23 | 1.62-3.07 | 0.000 | 2.07 | 1.49-2.87 | 0.000 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 14: | Obsessive compulsive | ||||||
| Yes | 0.82 | 0.19-3.50 | 0.784 | 0.65 | 0.15-2.85 | 0.570 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 15: | PTSD | ||||||
| PTSD | 3.99 | 2.40-6.65 | 0.000 | – | – | – | |
| Any diagnosis except PTSD | 2.67 | 1.78-4.00 | 0.000 | – | – | – | |
| No diagnosis | 1.0 | – | – | – | – | – | |
| Model 16: | Panic | ||||||
| Yes | 2.86 | 1.62-5.04 | 0.000 | 2.46 | 1.37-4.42 | 0.003 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 17: | Agoraphobia | ||||||
| Yes | 2.61 | 1.44-4.74 | 0.002 | 2.23 | 1.22-4.10 | 0.009 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 18: | Social phobia | ||||||
| Yes | 2.18 | 1.25-3.79 | 0.006 | 1.86 | 1.06-3.29 | 0.032 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 19: | Generalized anxiety | ||||||
| Yes | 2.21 | 0.73-6.70 | 0.161 | 1.99 | 0.63-6.27 | 0.237 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 20: | Specific phobia | ||||||
| Yes | 2.23 | 1.62-3.06 | 0.000 | 2.07 | 1.50-2.86 | 0.000 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 21: | Somatoform disorders | ||||||
| Yes | 1.56 | 0.99-2.46 | 0.055 | 1.39 | 0.86-2.25 | 0.179 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 22: | Conversion | ||||||
| Yes | 1.59 | 0.86-2.94 | 0.137 | 1.41 | 0.73-2.73 | 0.300 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 23: | Pain | ||||||
| Yes | 1.48 | 0.82-2.68 | 0.191 | 1.35 | 0.74-2.48 | 0.333 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 24: | Hypochondriasis | ||||||
| Yes | 2.23 | 1.13-4.39 | 0.021 | 2.10 | 1.05-4.18 | 0.035 | |
| No | 1.0 | – | – | 1.0 | – | – | |
| Model 25: | Substance misuse | ||||||
| Yes | 1.38 | 0.91-2.10 | 0.134 | 1.32 | 0.86-2.03 | 0.208 | |
| No | 1.0 | – | – | 1.0 | – | – | |
*All models are weighted by age and gender via stabilized inverse probability censoring weights with robust variance estimators.
After controlling for pre-disaster PTSD in the marginal structural logistic models, the following pre-disaster disorders/diagnostic categories remained predictors of post-disaster PTSD: dysthymia, brief psychotic disorder, anxiety disorders (not including PTSD), panic disorder, agoraphobia, social phobia, specific phobi, and hypochondriasis.
Pre-disaster disorders that were predictors in all models from Table 2 and had sufficient sample sizes were included in the final marginal structural logistic regression models. Posthoc false detection rate adjustment tests44–46 indicated that the findings from Table 2 were not due to Type I errors (results not shown).
Final marginal structural logistic regression models
Table 3 displays the marginal structural logistic regression analyses predicting post-disaster PTSD, with pre-disaster PTSD as the main independent variable of interest. All models indicate that individuals with pre-disaster PTSD, relative to those with no disorder, had the highest odds of developing post-disaster PTSD. When pre-disaster anxiety disorders (not including PTSD), dysthymia and non-affective psychotic disorders were added to the models, the PTSD odds ratio coefficients became slightly attenuated.
Table 3.
Marginal structural logistic regression models predicting post-disaster PTSD (N = 1708): the PREDICT study (2003-11)
| Pre-disaster predictors | Model 1 |
Model 2 |
Model 3 |
Model 4 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| PTSD | ||||||||||||
| PTSD | 3.99 | 2.40-6.65 | 0.000 | 3.16 | 1.77-5.64 | 0.000 | 2.73 | 1.50-4.98 | 0.001 | 2.53 | 1.37-4.65 | 0.003 |
| Any diagnosis except PTSD | 2.67 | 1.78-4.00 | 0.000 | 2.14 | 1.30-3.51 | 0.003 | 2.01 | 1.21-3.45 | 0.007 | 1.90 | 1.13-3.19 | 0.015 |
| No diagnosis | 1.0 | – | – | 1.0 | – | – | 1.0 | – | – | 1.0 | – | – |
| Other anxiety disorders | – | – | – | 1.39 | 0.93-2.06 | 0.104 | 1.41 | 0.95-2.09 | 0.092 | 1.46 | 0.98-2.18 | 0.065 |
| Dysthymia | – | – | – | – | – | – | 1.80 | 1.13-2.86 | 0.013 | 1.83 | 1.15-2.92 | 0.011 |
| Non-affective psychotic disorder | – | – | – | – | – | – | – | – | – | 2.05 | 0.99-4.26 | 0.055 |
All models weigh age and gender utilizing stabilized inverse probability censoring weights with robust variance estimators; Model 1 is repeated from Table 2 for ease of reading.
Discussion
The current study takes advantage of a rare opportunity to examine the effects of a natural experiment by studying adults who had undergone a structured psychiatric diagnostic interview in a large sample before being exposed to one of the most powerful earthquakes in history, thus providing a clearer understanding of the pre-existing psychiatric risk factors for developing disaster-related PTSD. The major findings include: (i) several pre-disaster Axis I psychiatric disorders predicted the development of disaster-related PTSD; and (ii) individuals with pre-disaster PTSD had the highest odds of developing post-disaster PTSD relative to individuals with no pre-disaster diagnosis, even after taking into account other pre-disaster Axis I disorders. These results produce valuable insights into which pre-existing psychopathologies are associated with developing disaster-related PTSD, as well as cross-national variations in the risk of developing disaster-related PTSD.
There have been few studies examining whether pre-existing PTSD predicts subsequent PTSD longitudinally in civilian samples.47,48 In our study, pre-disaster PTSD predicted post-disaster PTSD even after controlling for other pre-disaster Axis I disorders. Results support the stress sensitization hypothesis, which suggests that individuals who have experienced previous PTSD have greater vulnerability to subsequent traumas.47,49 Besides earlier psychiatric history, there are several other vulnerabilities that may also have influenced the increased risk and maintenance of post-disaster PTSD:50 genetics,51 predisposition to a pathological reaction to stressors,47 pre- and post-trauma psychosocial stressors (e.g. childhood poverty),36 acute biological/emotional reactions after the traumatic event (e.g. peritraumatic dissociation),36,47,48 other personal vulnerabilities (e.g. poor coping mechanisms),47,49 environmental factors (e.g. relationship with family of origin20), occupational/financial stressors52 and contextual risk factors (e.g., property destruction.53 Although these variables were not included in the present study, they merit additional investigation in future longitudinal studies.
It is worth noting the lack of association between pre-disaster major depressive disorder (MDD) and post-disaster PTSD, which contradicts previous findings.35,54Posthoc analyses indicated that MDD and PTSD were comorbid at the pre- and post-disaster assessment (results not shown). However, most of the individuals with comorbid (lifetime) MDD-PTSD at baseline were not the same individuals who had comorbid (12-month) MDD-PTSD at the post-disaster assessment. There are several speculations as to why this pattern emerged. First, the baseline interview assessed for a lifetime history of psychiatric disorders, compared with the post-disaster assessment which assessed for 12-month disorders. As a result, some participants during the pre-disaster assessment had to recall symptoms/diagnoses from years (or decades) previously, which may have led to memory biases. Second, the average age of onset of pre-disaster PTSD preceded pre-disaster MDD by a substantial amount of time, i.e., 46.7 years [standard deviation (SD) = 16.3] vs 20.7 (SD = 10), and the two disorders may have not occurred simultaneously. Third, the pre-disaster PTSD interview assessed PTSD symptoms due to a variety of potentially traumatic events, whereas the post-disaster PTSD interview only assessed symptoms relating to the disaster. We may have found the same individuals with comorbid PTSD-MDD at both waves if other post-disaster potentially traumatic events (e.g. combat, assault etc.) were assessed.
Surprisingly, an association between pre-disaster dysthymia (but not MDD) and post-disaster PTSD was found. There are several reasons why this finding may have occurred. First, posthoc analyses indicated that individuals with pre-disaster dysthymia had more pre-disaster psychiatric disorders (mean = 2.38; SD = 1.82; median = 2.0) than individuals with pre-disaster MDD (mean = 1.56; SD = 1.47; median = 1.0; results not shown). Additionally, individuals with pre-disaster dysthymia were significantly more likely to be illiterate/have an elementary school education (vs a high-school/college education) compared with those with pre-disaster MDD (χ2 = 20.12, p = 0.000). Together, these results suggest that the participants with pre-disaster dysthymia had a higher overall vulnerability to developing post-disaster PTSD compared with individuals with pre-disaster MDD.35 Second, most disaster studies use checklists (instead of diagnostic interviews) to measure depressive symptoms, which do not differentiate between MDD and dysthymia. It is possible that dysthymia (a long-lasting chronic disorder), rather than MDD (a cyclical disorder) predicted PTSD in these studies.55 Third, there was a significant relationship between pre-disaster lifetime MDD and pre-disaster lifetime dysthymia (χ2 = 29.95, p = 0.000), which is consistent with other studies demonstrating a significant symptom overlap between MDD and dysthymia.27,56 Further research examining the association between dysthymia and PTSD is warranted given the novelty of these results.
This study’s findings have the potential to inform targeted public health interventions to reduce disaster-related PTSD. Natural disasters are a continuous threat to countries throughout the world, especially Chile, due to its geographical location.12 In this study, we found that the majority of individuals who developed post-disaster PTSD had symptoms for over a year (results not shown), illustrating the need for clinical interventions in future disasters. Although the majority of individuals exposed to a disaster will not develop PTSD nor need formal intervention, a minority will require acute post-disaster psychological support.35 Fortunately, Chile uses primary prevention in the form of strict building codes, which is beneficial as several studies have found that building destruction, injury and death increase the risk of post-disaster PTSD. Public health disaster efforts can focus on triaging individuals with pre-existing PTSD and other comorbid disorders, in order to allocate resources to individuals most at risk for developing post-disaster PTSD. Because Chile has a national mental health care system, this process can be streamlined by completing a brief PTSD assessment during routine mental health visits, enabling the identification and treatment of those at risk for developing post-disaster PTSD. This will likely lead to the increased resiliency of the victims, reducing the burden of secondary functional impairment and costs to both the individual and the public.57
The present study has some limitations that should be kept in mind when interpreting results. First, there is potential for non-differential misclassification of pre-disaster PTSD. As the baseline examination was administered 7 years before the disaster, new cases of PTSD may have been missed which occurred between the baseline assessment and the earthquake.
Second, we do not capture individuals who may have had PTSD after the disaster due to non-disaster traumatic events. Therefore, results should only be generalized to individuals with PTSD due to experiencing a natural disaster. Future studies should use multiple time points before and after a disaster to more accurately examine the longitudinal course of disaster-related PTSD.
Third, because this study recruited a non-psychiatric sample, some of the disorders had sparse sample sizes, leading to imprecision in those estimates.
Fourth, although data were collected in a longitudinal and prospective fashion, the results may not reflect a causal relationship between pre-disaster PTSD and post-disaster PTSD, due to residual confounding, unmeasured confounding and random error.
Fifth, several post-disaster moderators of post-disaster PTSD (e.g. destruction) were not included in the present analysis, as the preliminary focus was to examine the association between pre-disaster psychopathology and post-disaster PTSD.
Sixth, the pre-disaster disorders are lifetime accounts, which may be susceptible to memory biases.
Seventh, a substantial proportion of the sample was lost to follow-up, inducing potential selection bias. However, we circumvented this bias with probability censoring weights.
Eighth, given the CIDI uses lay interviewers to collect diagnostic information, there is concern regarding the ability of this instrument to accurately assess non-affective psychotic disorders in US populations.58–62 However, there are insufficient data on Latin American populations to draw this conclusion.
Ninth, because the sampling was based on attendance at primary care clinics, we have an over-representation of females compared with the general Chile population, and it is possible that here the prevalence of psychiatric disorders is higher than those from a population-based sample.63
Finally, the findings may not necessarily generalize to non-health-care seeking populations in Chile or populations outside Chile.
Despite its limitations, the current study has many strengths. It provides the unprecedented opportunity to examine PTSD before and after a natural disaster in a large sample, using a validated, cross-cultural diagnostic psychiatric interview, while simultaneously controlling for comorbid Axis I psychiatric disorders using a methodologically robust study design. This type of rich longitudinal data does not exist in the disaster literature.64
Previous studies that have attempted to address these study questions have been severely limited by small convenience samples, lack of diagnostic instruments and lack of any pre-disaster information.20,64 The current study overcomes these limitations and this database allows for testing of hypotheses not previously possible. This information is critical to understanding variations in risk, course and diagnostic subtypes of disaster-related PTSD, with the overall goal of reducing the incidence of post-disaster PTSD. By determining who has PTSD after a disaster, one can more accurately determine the mechanisms of disaster-related PTSD in an understudied international population.65,66
In conclusion, this study uses a methodologically robust design aimed at identifying the mechanisms of disaster-related PTSD, thereby furthering understanding of the longitudinal course of PTSD and facilitating the development of more appropriate interventions targeted to high-risk individuals. The analyses take advantage of a unique and rare opportunity to examine the effects of a natural experiment by studying adults who had undergone a structured psychiatric diagnostic interview in a large sample before being exposed to one of the most powerful earthquakes in history, thus providing a clearer understanding of the trajectory of disaster-related PTSD and its determinants among groups in whom PTSD resolves spontaneously and those in whom it persists in the long term. An increased knowledge regarding the variations of disaster-related PTSD is essential in order to inform more sensitive treatment strategies, especially among international populations.
Funding
This work was supported in part by: the National Institute of Mental Health [F31MH104000]; FONDEF Chile [DO2I-1140]; FONDECYT Chile [1110687]; and the National Institute of General Medical Sciences [R25GM083270].
Conflict of interest: Authors declare no conflict of interest.
Key Messages
With an increasing number of individuals surviving natural disasters, it is crucial to understand who is most at risk for developing post-disaster PTSD.
The objective of this study was to prospectively examine the role that pre-existing psychopathology plays in developing PTSD after a disaster.
After controlling for pre-disaster anxiety disorders, dysthymia and non-affective psychotic disorders, results indicated that individuals with pre-disaster PTSD (vs those without pre-disaster PTSD) had higher odds of developing post-disaster PTSD (OR = 2.53; 95% CI = 1.37-4.65).
This is the first study to demonstrate prospectively that pre-disaster psychiatric disorders, independent of a prior history of other psychiatric disorders, increase the vulnerability to developing PTSD following a major natural disaster in Chile.
References
- 1. Guha-Sapir D, Vos F, Below R, Ponserre S.. Annual Disaster Statistical Review 2010: The Numbers and Trends. Brussels: CRED; 2011. http://www.cred.be/sites/default/files/ADSR_2010.pdf (10 May 2016, date last accessed). [Google Scholar]
- 2. Canino G, Bravo M, Maritza R, Woodbury M.. The impact of disaster on mental health: Prospective and retrospective analyses. Int J Ment Health 1990;19:51–69. [Google Scholar]
- 3. Neria Y, Nandi A, Galea S.. Post-traumatic stress disorder following disasters: A systematic review. Psychol Med 2008;38: 467–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Galea S, Nandi A, Vlahov D.. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev 2005;27: 78–91. [DOI] [PubMed] [Google Scholar]
- 5. Norris FH. Disaster research methods: past progress and future directions. J Trauma Stress 2006;19:173–84. [DOI] [PubMed] [Google Scholar]
- 6. Norris FH, Murphy AD, Baker CK, Perilla JL.. Postdisaster PTSD over four waves of a panel study of Mexico’s 1999 flood. J Trauma Stress 2004;17:283–92. [DOI] [PubMed] [Google Scholar]
- 7. Norris FH. The Impact of Disasters and Political Violence on Mental Health in Latin America: National Centre for PTSD Fall 2009. http://www.ptsd.va.gov/professional/newsletters/research-quarterly/v20n4.pdf. (10 May 2016, date last accessed).
- 8. Norris FH. Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J Consult Clin Psychol 1992;60:409–18. [DOI] [PubMed] [Google Scholar]
- 9. Cloitre M, Stolbach BC, Hern JL. et al . A developmental approach to complex PTSD: childhood and adult cumulative trauma as predictors of symptom complexity. J Trauma Stress 2009;22:399–408. [DOI] [PubMed] [Google Scholar]
- 10. Elliott DM. Traumatic events: prevalence and delayed recall in the general population. J Consult Clin Psychol 1997;65:811–20. [DOI] [PubMed] [Google Scholar]
- 11. Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry 2000;61(Suppl 5):4–12. [PubMed] [Google Scholar]
- 12. Earthquakes Hazard Program. Magnitude 8.8: Offshore Bio-Bio Chile World Data Centre for Seismology. Denver, CO: U.S. Geological Survey, National Earthquake Information Centre. http://earthquake.usgs.gov/earthquakes/eqinthenews/2010/us2010tfan/#details (10 May 2016, date last accessed).
- 13. Asarnow J, Glynn S, Pynoos RS. et al. When the earth stops shaking: earthquake sequelae among children diagnosed for pre-earthquake psychopathology. J Am Acad Child Adolesc Psychiatry 1999; 38:1016–23. [DOI] [PubMed] [Google Scholar]
- 14. Weems CF, Pina AA, Costa NM, Watts SE, Taylor LK, Cannon MF. Predisaster trait anxiety and negative affect predict posttraumatic stress in youths after hurricane Katrina. J Consult Clin Psychol 2007;75:154–59. [DOI] [PubMed] [Google Scholar]
- 15. Parslow RA, Jorm AF, Christensen H.. Associations of pre-trauma attributes and trauma exposure with screening positive for PTSD: analysis of a community-based study of 2,085 young adults. Psychol Med 2006;36:387–95. [DOI] [PubMed] [Google Scholar]
- 16. Parslow RA, Jorm AF.. Pretrauma and posttrauma neurocognitive functioning and PTSD symptoms in a community sample of young adults. Am J Psychiatry 2007;164:509–15. [DOI] [PubMed] [Google Scholar]
- 17. Nolen-Hoeksema S, Morrow J.. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. J Pers Soc Psychol 1991;61: 115–21. [DOI] [PubMed] [Google Scholar]
- 18. La Greca AM, Silverman WK, Wasserstein SB.. Children's predisaster functioning as a predictor of posttraumatic stress following Hurricane Andrew. J Consult Clin Psychol 1998;66:883–92. [DOI] [PubMed] [Google Scholar]
- 19. Sullivan G, Vasterling JJ, Han X. et al. Preexisting mental illness and risk for developing a new disorder after hurricane Katrina. J Nerv Ment Dis 2013;201:161–66. [DOI] [PubMed] [Google Scholar]
- 20. Digangi JA, Gomez D, Mendoza L, Jason LA, Keys CB, Koenen KC.. Pretrauma risk factors for posttraumatic stress disorder: A systematic review of the literature. Clin Psychol Rev 2013;33: 728–44. [DOI] [PubMed] [Google Scholar]
- 21. Osofsky JD, Osofsky HJ, Weems CF, Hansel TC, King LS.. Effects of Stress Related to the Gulf Oil Spill on Child and Adolescent Mental Health. J Pediatr Psychol 2016;41:65–72. [DOI] [PubMed] [Google Scholar]
- 22. Martin NC, Felton JW, Cole DA. Predictors of Youths' Posttraumatic Stress Symptoms Following a Natural Disaster: The 2010 Nashville, Tennessee Flood. J Clin Child Adolesc Psychol 2015, Jan 20:1–13. [DOI] [PubMed] [Google Scholar]
- 23. King M, Weich S, Torres-Gonzalez F. et al. Prediction of depression in European general practice attendees: the PREDICT study. BMC Public Health 2006;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. King M, Walker C, Levy G. et al. Development and validation of an international risk prediction algorithm for episodes of major depression in general practice attendees: the PREDICT study. Arch Gen Psychiatry 2008;65:1368–76. [DOI] [PubMed] [Google Scholar]
- 25. Bottomley C, Nazareth I, Torres-Gonzalez F. et al. Comparison of risk factors for the onset and maintenance of depression. Br J Psychiatry 2010;196:13–17. [DOI] [PubMed] [Google Scholar]
- 26. World Health Organization. Composite International Diagnostic Interview (CIDI, Version 2.1) Geneva: WHO, 1997. [Google Scholar]
- 27. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th edn Washington DC: American Psychiatric Association, 2000. [Google Scholar]
- 28. Robins LN, Wing J, Wittchen HU. et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry 1988;45:1069–77. [DOI] [PubMed] [Google Scholar]
- 29. Andrews G, Peters L.. The psychometric properties of the Composite International Diagnostic Interview. Soc Psychiatry Psychiatr Epidemiol 1998;33:80–88. [DOI] [PubMed] [Google Scholar]
- 30. Kessler RC, McGonagle KA, Zhao S. et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry 1994;51:8–19. [DOI] [PubMed] [Google Scholar]
- 31. Vicente B, Kohn R, Rioseco P, Saldivia S, Levav I, Torres S.. Lifetime and 12-month prevalence of DSM-III-R disorders in the Chile psychiatric prevalence study. Am J Psychiatry 2006;163:1362–70. [DOI] [PubMed] [Google Scholar]
- 32. Vicente B, Kohn R, Rioseco P. et al. Regional differences in psychiatric disorders in Chile. Soc Psychiatry Psychiatr Epidemiol 2006;41:935–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vielma M, Vicente B, Rioseco P, Castro P, Castro N, Torres S.. Validacion en Chile de la entrevista diagnostica estandarizada para estudios epidemiologicos CIDI. (In English :Chilean validation of a standardized diagnostic instrument for epidemiological studies). Rev Psiquiatr 1992;9: 1039–49. [Google Scholar]
- 34. Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. Geneva: World Health Organization, Department of Mental Health and Substance Dependence, 2001. [Google Scholar]
- 35. Friedman MJ, Keane TM, Resick PA.. Handbook of PTSD: Science and Practice. 2nd edn New York, NY: Guilford Press, 2014. [Google Scholar]
- 36. Brewin CR, Andrews B, Valentine JD.. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol 2000;68:748–66. [DOI] [PubMed] [Google Scholar]
- 37. Ozer EJ, Best SR, Lipsey TL, Weiss DS.. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull 2003;129):52–73. [DOI] [PubMed] [Google Scholar]
- 38. Cole SR, Hernan MA.. Constructing inverse probability weights for marginal structural models. Am J Epidemiol 2008;168: 656–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hernan MA, Robins JM.. Causal Inference. Boca Raton, FL: Chapman & Hall/CRC, 2016. [Google Scholar]
- 40. Hernan MA, Hernandez-Diaz S, Robins JM.. A structural approach to selection bias. Epidemiology 2004;15:615–25. [DOI] [PubMed] [Google Scholar]
- 41. Robins JM, Hernan MA, Brumback B.. Marginal structural models and causal inference in epidemiology. Epidemiology 2000; 11: 550–60. [DOI] [PubMed] [Google Scholar]
- 42. StataCorp. Stata Statistical Software: Release 12. College Station TX: 2011. [Google Scholar]
- 43. SAS Institute. Survey Data Analysis 9.3. Cary, NC: SAS, 2012. [Google Scholar]
- 44. Sainani KL. The problem of muliple testing. PM R. 2009;1:1098–103. [DOI] [PubMed] [Google Scholar]
- 45. Benjamini Y, Yekutieli D.. The control of the false discovery rate in multiple testing under dependency. Ann Stat 2001;29: 1152–75. [Google Scholar]
- 46. Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J R Stat Soc B 1995;57:289–300. [Google Scholar]
- 47. Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: a prospective epidemiological study. Arch Gen Psychiatry 2008;65:431–37. [DOI] [PubMed] [Google Scholar]
- 48. Breslau N, Chilcoat H, Kessler RC, Davis GC.. Previous exposure to trauma and PTSD effects of subsequent trauma: Results from the Detroit Area Survey of Trauma. Am J Psychiatry 1999;156: 902–07. [DOI] [PubMed] [Google Scholar]
- 49. Zaidi LY, Foy DW.. Childhood abuse experiences and combat-related PTSD. J Trauma Stress 1994;7:33–42. [DOI] [PubMed] [Google Scholar]
- 50. North CS, Smith EM, Spitznagel EL.. Posttraumatic stress disorder in survivors of a mass shooting. Am J Psychiatry 1994; 151: 82–88. [DOI] [PubMed] [Google Scholar]
- 51. King DW, King LA, Foy DW, Keane TM, Fairbank JA.. Posttraumatic stress disorder in a national sample of female and male Vietnam veterans: risk factors, war-zone stressors, and resilience-recovery variables. J Abnorm Psychol 1999;108: 164–70. [DOI] [PubMed] [Google Scholar]
- 52. Wright KM, Cabrera OA, Eckford RD, Adler AB, Bliese PD. The impact of predeployment functional impairment on mental health after combat. Psychol Trauma 2012;4:260–69. [Google Scholar]
- 53. Kohn R, Levav I, Donaire I, Machuca M, Tamashiro R.. Psychological and psychopathological reactions in Honduras following Hurricane Mitch: implications for service planning. Rev Panam Salud Publica 2005;18:287–95. [DOI] [PubMed] [Google Scholar]
- 54. Adams RE, Boscarino JA.. Predictors of PTSD and delayed PTSD after disaster: The impact of exposure and psychosocial resources. J Nerv Ment Dis 2006;194:485–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Tang B, Liu X, Liu Y, Xue C, Zhang L.. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health 2014;14:623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Moore MT,, Brown TA.. Are there meaningful differences between major depressive disorder, dysthymic disorder, and their subthreshold variants? J Nerv Ment Dis 2012;200:766–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Norris FH, Friedman MJ, Watson PJ.. 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry. 2002;65:240–60. [DOI] [PubMed] [Google Scholar]
- 58. Eaton WW, Romanoski A, Anthony JC, Nestadt G.. Screening for psychosis in the general population with a self-report interview. J Nerv Ment Dis 1991;179:689–93. [DOI] [PubMed] [Google Scholar]
- 59. Spengler PA, Wittchen HU.. Procedural validity of standardized symptom questions for the assessment of psychotic symptoms - a comparison of the DIS with two clinical methods. Compr Psychiatry 1988;29:309–22. [DOI] [PubMed] [Google Scholar]
- 60. Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE.. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:617–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry 1996;53:1022–31. [DOI] [PubMed] [Google Scholar]
- 62. Lewis-Fernandez R, Horvitz-Lennon M, Blanco C, Guarnaccia PJ, Cao Z, Alegria M.. Significance of endorsement of psychotic symptoms by US Latinos. J Nerv Ment Dis 2009;197:337–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Slone LB. Prevalence of PTSD in Primary Care Settings. PTSD Res Q 2006;17:1–8. [Google Scholar]
- 64. Norris FH, Elrod CL.. Psychosocial consequences of disaster: a review of past research In: Norris FH, Galea S, Friedman MJ, Watson PJ (eds). Methods for Disaster Mental Health Research. New York, NY: Guilford Press, 2006. [Google Scholar]
- 65. Zubizarreta JR, Cerda M, Rosenbaum PR.. Effect of the 2010 Chilean earthquake on posttraumatic stress: reducing sensitivity to unmeasured bias through study design. Epidemiology 2013;24:79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Vera-Villarroel P, Zych I, Celis-Atenas K, Cordova-Rubio N, Buela-Casal G.. Chilean validation of the Posttraumatic Stress Disorder Checklist-Civilian version (PCL-C) after the earthquake on February 27, 2010. Psychol Rep 2011;109:47–58. [DOI] [PubMed] [Google Scholar]