Abstract
Aim
We compared the 2013 American College of Cardiology/American Heart Association (ACC/AHA) and the 2016 European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) guidelines on prevention of atherosclerotic cardiovascular disease (ASCVD) using different risk prediction models [US Pooled Cohort Equations (US-PCE for any ASCVD) and European Systematic COronary Risk Evaluation system (European-SCORE for fatal ASCVD)] and different statin eligibility criteria.
Methods and results
We examined 44 889 individuals aged 40–75 recruited in 2003–09 in the Copenhagen General Population Study, all free of ASCVD, diabetes, and statin use at baseline. We detected 2217 any ASCVD events and 199 fatal ASCVD events through 2014. The predicted-to-observed event ratio was 1.2 using US-PCE for any ASCVD and 5.0 using European-SCORE for fatal ASCVD. The US-PCE, but not the European-SCORE, was well-calibrated around decision thresholds for statin therapy. For a Class I recommendation, 42% of individuals qualified for statins using the ACC/AHA guidelines vs. 6% with the ESC/EAS guidelines. Using ACC/AHA- vs. ESC/EAS-defined statin eligibility led to a substantial gain in sensitivity (+62% for any ASCVD and +76% for fatal ASCVD) with a smaller loss in specificity (−35% for any ASCVD and −36% for fatal ASCVD). Similar differences between the ACC/AHA and ESC/EAS guidelines were found for men and women separately, and for Class IIa recommendations. The sensitivity and specificity of a US-PCE risk of 5% were similar to those of a European-SCORE risk of 1.4%, whereas a US-PCE risk of 7.5% was similar to a European-SCORE risk of 2.4%.
Conclusions
The ACC/AHA guidelines were superior to the ESC/EAS guidelines for primary prevention of ASCVD, that is, for accurately assigning statin therapy to those who would benefit.
Keywords: Atherosclerosis, Guideline, Lipids, Lipoproteins, Myocardial infarction, Stroke
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is mainly caused by modifiable risk factors and is preventable.1 Nevertheless, ASCVD remains a leading cause of death, disability, and high healthcare costs worldwide.1,2 The first ASCVD presentation is often sudden and unexpected death, in which major advances in secondary prevention are of no help.3 Thus, the only efficient approach to restrict this undue loss of life, quality of life, and healthcare resources is primary prevention. For this purpose, public health initiatives are important,4,5 but so is personalized prevention for those at the highest risk.6
The high risk strategy for primary prevention of ASCVD, including treatment of high blood cholesterol with statins, was revised recently in both the USA and Europe.7–10 These guidelines, issued by the American College of Cardiology (ACC) jointly with the American Heart Association (AHA) and by the European Society of Cardiology (ESC) jointly with the European Atherosclerosis Society (EAS), are all endorsing the principle of matching the intensity of preventive efforts with the absolute ASCVD risk of the individual. However, different risk prediction models are provided to estimate such risk, and different decision thresholds for, respectively, any ASCVD (ACC/AHA) and fatal ASCVD (ESC/EAS) are recommended for statin therapy. The risk prediction model recommended in the USA by the ACC and AHA is the newly introduced Pooled Cohort Equations (US-PCE) to predict any ASCVD,9,10 and in Europe by the ESC and EAS is the Systematic COronary Risk Evaluation system (European-SCORE) to predict fatal ASCVD.7,8
Which risk prediction model to prefer for optimal primary prevention of ASCVD is unknown because the US-PCE and European-SCORE prediction models have not been compared head-to-head in the target population. Despite this, a recent current opinion paper discussed the potential implications of adopting the ACC/AHA guidelines in Europe and concluded that the ESC/EAS guidelines using the European-SCORE model seem to be the most wide ranging, pragmatic, and appropriate choice for European countries.11 However, this conclusion was based on the opinion of experts, not a direct head-to-head comparison of the clinical performance of the guidelines using different risk prediction models and Class I and IIa recommendations. This is what we are providing in this study based on a large, contemporary, population-based European cohort.
Methods
Copenhagen General Population Study
The Copenhagen General Population Study (CGPS) is an ongoing prospective cohort study of the Danish general population.12–16 Enrolment began in November 2003, and participants are randomly selected through the Danish Civil Registration system to reflect the Danish population aged 20–100 years. All individuals aged 40+ years in Copenhagen are invited along with a random selection of 25% of individuals aged 20–39 years. The CGPS covers all regions of Copenhagen including surrounding countryside, and both high- and low-income areas. Information on baseline examination is provided in the Supplementary material online, Supplementary material. For this study, we included individuals enrolled between 2003 and 2009 to secure at least 5 years of follow-up for all individuals. All individuals were white and of Danish descent. In the main analysis we excluded individuals with diabetes, pre-existing ASCVD, statin use or with missing information at baseline examination, resulting in 54 017 individuals available for this study (see Supplementary material online, Figure S1). Statin users at baseline were excluded because both US-PCE and European-SCORE were designed to predict the natural history of ASCVD in the absence of intervention. The study was conducted in accordance with the Declaration of Helsinki and approved by Herlev and Gentofte Hospital. Written informed consent was obtained from all individuals.
Predictors and recommended age range
The predictors used to estimate risk for a first any or fatal ASCVD event included age, sex, smoking status, total cholesterol, HDL cholesterol, systolic blood pressure, and treatment for high blood pressure (only required for risk estimated by US-PCE). US-PCE also includes diabetes, but for the purpose of this study in which we wanted to compare risk prediction of US-PCE and European-SCORE in the same population we excluded individuals with diabetes because European-SCORE is not applicable in individuals with diabetes.
US Pooled Cohort Equations and European-SCORE vary in the age ranges to which they apply. European-SCORE is recommended for use in the 40- to 65-year age range,17,18 and the ESC/EAS guidelines only provide SCORE-based guidance in this age range.7,8 The electronic version of SCORE, HeartScore,19 however, allows entry of age up to 100 years, but the age-related fatal ASCVD risk does not increase beyond age 65. The age range for US-PCE is 40–79 years,10 but the ACC/AHA guidelines only provide Class I and IIa guidance based on US-PCE in the 40- to 75-year age range.9 Thus, in the main analysis we compared the clinical performance of the ACC/AHA and ESC/EAS guidelines in individuals aged 40–75. To comply with real-life clinical use of the ESC/EAS guidelines, the absolute fatal ASCVD risk for those aged 66–75 was corresponding to the risk at age 65 when assessing calibration. In the sensitivity analysis, to follow the ESC/EAS guidelines closely, the study population was limited to those aged 40–65 (European-SCORE age-range).
Predicted outcomes
With European-SCORE, the predicted outcome is fatal cardiovascular disease assumed to be caused by atherosclerosis (=fatal ASCVD).17 The endpoint defined by US-PCE is first hard ASCVD event, including non-fatal myocardial infarction, coronary death, and stroke (=any ASCVD).10 How these outcomes were identified and ascertained for this study is described in the Supplementary material online, Supplementary material.
Recommendations for statin therapy
The recommended USA and European indications for primary prevention with statins or other lipid-lowering drugs applied in this study are summarized in Table 1 and specified in the Supplementary material online, Supplementary material.
Table 1.
Guideline recommendations for primary prevention with statins based on total and low-density lipoprotein cholesterol concentrations and estimated 10-year risk of atherosclerotic cardiovascular disease used in this study
| Recommendation | ACC/AHA guidelines | ESC/EAS guidelines |
|---|---|---|
| Class I | Lipid-based: | Lipid-based: |
| LDL-C ≥ 190 mg/dL (4.9 mmol/L) | LDL-C >6 mmol/L (232 mg/dL) | |
| Age ≥ 21 years | or TC > 8 mmol/L (309 mg/dL) | |
| Class I | Risk-based: | Risk-based: |
| LDL-C 70–189 mg/dL (1.8-4.9 mmol/L) | LDL-C ≥ 4.0 mmol/L (155 mg/dL) | |
| US-PCE ≥ 7.5% | European-SCORE 5% to < 10% (high risk) | |
| Age 40–75 years | Age 40–65 years | |
| LDL-C ≥ 2.5 mmol/L (100 mg/dL) | ||
| European-SCORE ≥ 10% (very high risk) | ||
| Age 40–65 years | ||
| Class IIa | Risk-based: | Risk-based: |
| LDL-C 70–189 mg/dL (1.8–4.9 mmol/L) | LDL-C < 4.0 mmol/L (155 mg/dL) | |
| US-PCE 5% to < 7.5% | European-SCORE 5% to < 10% (high risk) | |
| Age 40–75 years | Age 40–65 years | |
| LDL-C <2.5 mmol/L (100 mg/dL) | ||
| European-SCORE ≥ 10% (very high risk) | ||
| Age 40–65 years |
TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; PCE, pooled cohort equations; SCORE, Systematic COronary Risk Evaluation.
Statistical analyses
Calibration of the equations used to estimate predicted risk (US-PCE and European-SCORE) was assessed by the predicted-to-observed (P/O) event ratio. As the CGPS has not yet completed 10 years of follow-up for all individuals, and as all were followed for at least 5 years, we calculated 5-year predicted and observed any ASCVD event rates when assessing calibration of US-PCE, using the 5-year equations provided by the REGARDS study.20 Similarly, when assessing calibration of the European-SCORE equations we calculated the predicted 5-year risk of fatal ASCVD, and compared predicted with observed 5-year fatal ASCVD event rates. In the subpopulation recruited in 2004 with complete 10 years of follow-up, we also assessed calibration of US-PCE and European-SCORE using the 10-year equations. The observed number of any and fatal ASCVD events at 5 and 10 years was adjusted for variable follow-up time using the Kaplan–Meier estimate, when assessing calibration. All other analysis was performed using total number of events.
The discriminative power of the US-PCE and European-SCORE equations was compared with Harrell’s c-statistics, which takes into account the timing of events.
The proportion of individuals in the CGPS eligible for statin treatment by the ACC/AHA and ESC/EAS guidelines was calculated using the Class I and IIa recommendations for primary prevention with statins. These recommendations are shown in Table 1.
To compare the clinical performance of the guidelines, we calculated sensitivity, specificity, and the binary net reclassification index (NRI) across the guideline-defined treatment threshold when comparing the ACC/AHA and ESC/EAS guidelines. Differences in sensitivity and specificity were statistically compared with the McNemar test. The binary NRI is the sum of Δsensitivity and Δspecificity and the theoretical range is −2 to 2.21,22
Additional information on statistics is provided in the Supplementary material online, Supplementary material. Analyses were performed using Stata version 13.1 SE (StataCorp LP, College Station, TX, USA).
Results
Baseline characteristics and observed events among the 44 889 individuals aged 40–75 from the CGPS are shown in Table 2; 57% were women. There were 10 and 14 times more any ASCVD events (used in US-PCE) than fatal ASCVD events (used in European-SCORE) in men and women. Supplementary material online, Figure S2 depicts any and fatal ASCVD event rates stratified by 5-year age groups.
Table 2.
Baseline characteristics and observed events in individuals in the Copenhagen General Population Study
|
Age 40–75 years |
|||
|---|---|---|---|
| Characteristics | All | Men | Women |
| Individuals, n | 44 889 | 19 383 | 25 506 |
| Age, years | 56(48–64) | 56(48–64) | 56(48–64) |
| Systolic blood pressure, mmHg | 138(125–152) | 140(130–155) | 135(122–150) |
| Total cholesterol, mmol/L | 5.7(5.1–6.5) | 5.7(5.1–6.4) | 5.8(5.1–6.5) |
| High-density lipoprotein cholesterol, mmol/L | 1.6(1.3–2.0) | 1.4(1.1–1.7) | 1.8(1.4–2.1) |
| Low-density lipoprotein cholesterol, mmol/L | 3.3(2.8–4.0) | 3.4(2.8–4.0) | 3.3(2.7–3.9) |
| Current smokers, % | 22 | 23 | 21 |
| US-PCE 10-year any ASCVD risk, % | 5.3(1.9–12.3) | 9.4(4.2–17.5) | 3.1(1.1–7.7) |
| European-SCORE 10-year fatal ASCVD risk, % | 1.6(0.5–4.2) | 2.7(1.0–6.0) | 0.9(0.2–2.9) |
| US-PCE-defined any ASCVD events, n | 2217 | 1205 | 1012 |
| European-SCORE-defined fatal ASCVD events, n | 199 | 126 | 73 |
Continuous values are shown as median (interquartile range).
PCE, pooled cohort equations; SCORE, Systematic COronary Risk Evaluation; ASCVD, atherosclerotic cardiovascular disease.
Calibration and discrimination
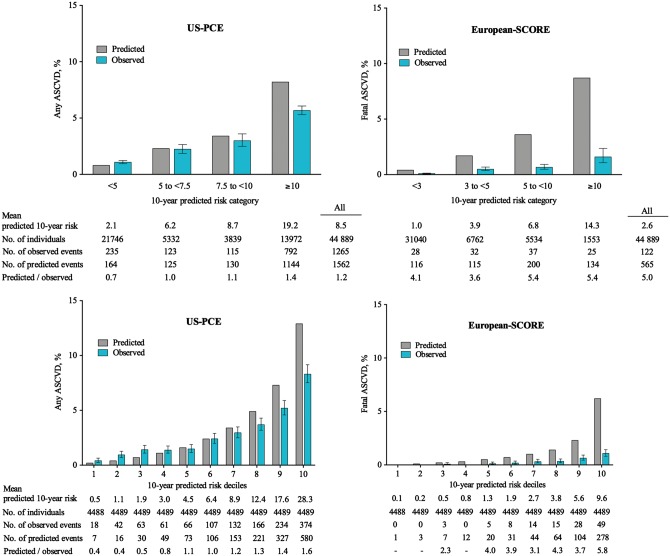
First, we assessed how accurate the predicted events matched the observed events (=calibration). The overall P/O event ratio was 1.2 using US-PCE for any ASCVD compared with 5.0 using European-SCORE for fatal ASCVD (Figure 1). The US-PCE was well calibrated around the guideline-defined decision thresholds for statin therapy of 7.5% and 5% (P/O ratio = 1.0–1.1), but overestimated risk slightly when the predicted risk was high (≥10%, P/O ratio = 1.4). In contrast, the European-SCORE overestimated risk markedly across all categories and deciles of predicted risk, with overestimation around both the high-risk (5%, P/O ratio = 3.6–5.4) and very-high-risk (10%, P/O ratio = 5.4) thresholds for statin therapy (Figure 1). In the 6802 individuals with 10 years of follow-up, we observed similar results using the 10-year prediction models (see Supplementary material online, Figure S3).
Figure 1.
Calibration comparing observed and predicted events in 40- to 75-year-old individuals in the Copenhagen General Population Study. US PCE performed well below 10% any atherosclerotic cardiovascular disease 10-year risk, with good calibration around the guideline-defined decision thresholds of 5% and 7.5% for statin therapy (left panel). In contrast, European SCORE overestimated risk across all deciles and categories of fatal atherosclerotic cardiovascular disease 10-year predicted risk, with substantial overestimation around both the high-risk (5%) and very-high-risk (10%) thresholds for statin therapy (right panel). Observed events were Kaplan–Meier adjusted. Error bars indicate 95% confidence interval. PCE, pooled cohort equations; SCORE, Systematic COronary Risk Evaluation.
Next, we assessed the ability of US-PCE and European-SCORE to discriminate between those who developed events defined by US-PCE (any ASCVD) and European-SCORE (fatal ASCVD) and those who did not, after calculating 10-year risk for each individual. For all comparisons, US-PCE discriminated as well or better than European-SCORE between cases and non-cases with c-statistics ranging from 0.71 to 0.85 for US-PCE compared with 0.69–0.84 for European-SCORE (Table 3).
Table 3.
Sensitivity, specificity, and net reclassification based on Class I recommendations for statin eligibility among individuals aged 40–75 years in the Copenhagen General Population Study
| Model comparison | Sensitivity (%) | Specificity (%) | ΔSensitivity (%) | ΔSpecificity (%) | NRI | c-Statisticsa | P/O |
|---|---|---|---|---|---|---|---|
| All | |||||||
| Any ASCVD | |||||||
| ESC/EAS | 10 | 95 | Ref | Ref | Ref | 0.70 | |
| ACC/AHA | 72 | 60 | 62 (P < 0.0001) | −35 (P < 0.0001) | 0.27 (P < 0.0001) | 0.72 (P < 0.0001) | 1.2 |
| Fatal ASCVD | |||||||
| ESC/EAS | 11 | 94 | Ref | Ref | Ref | 0.80 | 5.0 |
| ACC/AHA | 87 | 59 | 76 (P < 0.0001) | −36 (P < 0.0001) | 0.40 (P < 0.0001) | 0.82 (P = 0.007) | |
| Men | |||||||
| Any ASCVD | |||||||
| ESC/EAS | 14 | 92 | Ref | Ref | Ref | 0.69 | |
| ACC/AHA | 83 | 43 | 70 (P < 0.0001) | −49 (P < 0.0001) | 0.21 (P < 0.0001) | 0.71 (P < 0.0001) | 1.4 |
| Fatal ASCVD | |||||||
| ESC/EAS | 13 | 92 | Ref | Ref | Ref | 0.75 | 5.1 |
| ACC/AHA | 89 | 41 | 75 (P < 0.0001) | −50 (P < 0.0001) | 0.26 (P = 0.001) | 0.77 (P = 0.01) | |
| Women | |||||||
| Any ASCVD | |||||||
| ESC/EAS | 6 | 97 | Ref | Ref | Ref | 0.70 | |
| ACC/AHA | 58 | 73 | 52 (P < 0.0001) | −24 (P < 0.0001) | 0.28 (P < 0.0001) | 0.71 (P < 0.0001) | 0.9 |
| Fatal ASCVD | |||||||
| ESC/EAS | 7 | 97 | Ref | Ref | Ref | 0.84 | 4.0 |
| ACC/AHA | 84 | 72 | 77 (P < 0.0001) | −25 (P < 0.0001) | 0.52 (P = 0.0001) | 0.85 (P = 0.18) |
c-Statistics for discrimination between events and non-events using US-PCE and European-SCORE.
NRI, net reclassification index; ESC/EAS, European Society of Cardiology/European Atherosclerosis Society; ACC/AHA, American College of Cardiology/American Heart Association; ASCVD, atherosclerotic cardiovascular disease; P/O, predicted/observed events using European-SCORE and US-PCE.
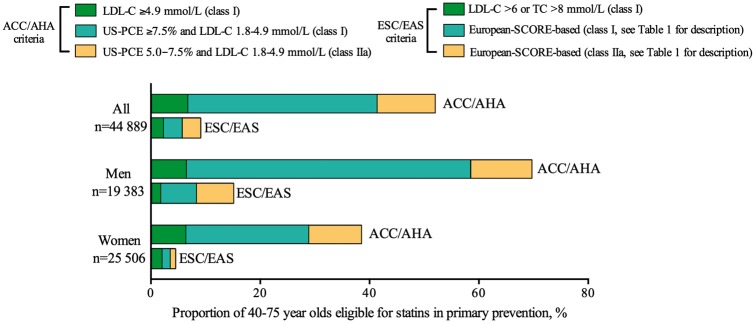
Eligibility for statin therapy
Then, we assessed the proportion of individuals who at baseline examination would have been eligible for statin therapy according to the ACC/AHA and ESC/EAS guidelines. We compared corresponding Class I and IIa recommendations as shown in Table 1. For a Class I recommendation, 42% of individuals qualified for statins using the ACC/AHA guidelines vs. 6% with the ESC/EAS guidelines (Figure 2). Baseline characteristics of these individuals are shown in the Supplementary material online, Table S1. All who qualified for statin therapy by the ESC/EAS guidelines also did so with the ACC/AHA guidelines; in consequence, 36% of all individuals in the CGPS were furthermore eligible for statin therapy based on Class I recommendations with the ACC/AHA guidelines, but not with the ESC/EAS guidelines.
Figure 2.
Eligibility for statin therapy using ACC/AHA and ESC/EAS guidelines in individuals aged 40–75 years in the Copenhagen General Population Study. Proportion of individuals who qualified for primary prevention with statins based on Class I and IIa recommendations as shown in Table 1. A larger proportion of individuals qualified for statins with the ACC/AHA guidelines compared with the ESC/EAS guidelines. For conversion of cholesterol values in mmol/L to mg/dL, multiply by 38.6. ACC/AHA, American College of Cardiology/American Heart Association; ESC/EAS, European Society of Cardiology/European Atherosclerosis Society; PCE, pooled cohort equations; SCORE, Systematic COronary Risk Evaluation; LDL-C , Low-density lipoprotein cholesterol; TC , Total cholesterol.
A similar difference between ACC/AHA and ESC/EAS guidelines was found for men and women separately, and for Class IIa recommendations (Figure 1).
Sensitivity, specificity, and net reclassification
To compare the ability of ACC/AHA and ESC/EAS guidelines to allocate statin therapy to individuals who later developed any or fatal ASCVD events, we calculated sensitivity, specificity, and binary NRI based on Class I recommendations for statin therapy (Table 3 and see Supplementary material online, Table S2). The ACC/AHA compared with ESC/EAS guidelines increased the eligibility for statin therapy both among those who developed any ASCVD (increase in sensitivity from 10% to 72%) and those who did not develop any ASCVD (decrease in specificity from 95% to 60%), together yielding a positive NRI of 0.27. Likewise, the ACC/AHA compared with ESC/EAS guidelines increased the eligibility for statin therapy among those who developed fatal ASCVD (increase in sensitivity from 11% to 87%) and those who did not develop fatal ASCVD (decrease in specificity from 94% to 59%), yielding a positive NRI of 0.40. Similar results were seen for men and women separately.
Using the Class IIa recommendations for ACC/AHA compared with ESC/EAS guidelines, we also observed a large gain in sensitivity and a positive NRI for both any and fatal ASCVD (see Supplementary material online, Table S3).
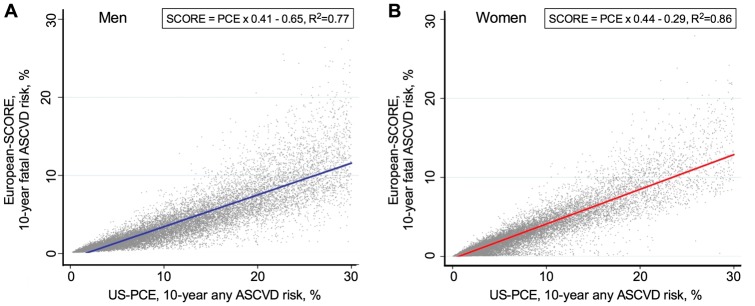
Thresholds of European-SCORE corresponding to decision thresholds of US-PCE
Predicted 10-year risk calculated by US-PCE and European-SCORE correlated strongly (spearman 0.95, P < 0.0001) and linearly (Figure 3). The sensitivity and specificity of a US-PCE risk of 5% were similar to those of a European-SCORE risk of 1.4%, while a US-PCE risk of 7.5% was similar to a European-SCORE risk of 2.4% (Table 4).
Figure 3.
Correlation between European SCORE fatal atherosclerotic cardiovascular disease 10-year risk and US PCE any atherosclerotic cardiovascular disease 10-year risk. Risk estimated by European SCORE and US PCE correlated strongly in the decision interval of interest in both men (A) and women (B). Analyses were by linear regression. The fitted regression lines include 95% confidence bands (too narrow to be seen). ASCVD, atherosclerotic cardiovascular disease; PCE, pooled cohort equations; SCORE, Systematic COronary Risk Evaluation.
Table 4.
Thresholds of European Systematic COronary Risk Evaluation corresponding to decision thresholds of US Pooled Cohort Equations and vice versa
|
Any ASCVD
|
Fatal ASCVD
|
||||
|---|---|---|---|---|---|
|
Cut-point (10-year risk)
|
Sensitivity (%) PCE/SCORE | Specificity (%) PCE/SCORE | Sensitivity (%) PCE/SCORE | Specificity (%) PCE/SCORE | |
| US-PCE (%) | European-SCORE (%) | ||||
| All | |||||
| 14.6 | 5.0 | 47/47 | 74/75 | 68/67 | 79/80 |
| 10.0 | 3.4 | 62/62 | 70/71 | 80/80 | 69/70 |
| 7.5 | 2.4 | 71/71 | 62/62 | 88/86 | 61/61 |
| 5.0 | 1.4 | 81/81 | 50/49 | 94/94 | 48/49 |
| Men | |||||
| 15.7 | 5.0 | 58/58 | 71/72 | 74/71 | 70/71 |
| 10.0 | 3.0 | 77/77 | 54/55 | 86/84 | 53/54 |
| 7.5 | 2.1 | 84/84 | 44/45 | 92/90 | 42/43 |
| 5.0 | 1.3 | 92/92 | 31/32 | 96/97 | 30/31 |
| Women | |||||
| 13.0 | 5.0 | 34/34 | 87/88 | 59/54 | 87/87 |
| 10.0 | 3.4 | 45/45 | 83/81 | 71/75 | 83/82 |
| 7.5 | 2.7 | 55/55 | 76/75 | 82/81 | 74/74 |
| 5.0 | 1.6 | 68/67 | 64/64 | 89/89 | 63/62 |
SCORE , Systematic COronary Risk Evaluation; PCE , pooled cohort equations.
Sensitivity analysis
In sensitivity analysis we limited the study population to individuals aged 40–65 to fully comply with the European-SCORE age-range, and re-assessed risk prediction and clinical performance of ACC/AHA and ESC/EAS guidelines. In this age group consisting of 36 482 individuals (see Supplementary material online, Table S4), the US-PCE likewise were better calibrated than the European-SCORE (P/O ratio of 1.1 vs. 5.2; see Supplementary material online, Figure S4). Similar results were observed using the 10-year prediction models among the 5595 individuals with 10 years of follow-up (see Supplementary material online, Figure S3). For a Class I recommendation, 30% of individuals qualified for statins using the ACC/AHA guidelines vs. 6% with the ESC/EAS guidelines (see Supplementary material online, Figure S5). The ACC/AHA guidelines increased the sensitivity for both any and fatal ASCVD events considerably, accompanied by smaller decreases in specificity (see Supplementary material online, Table S5). Thus, for individuals aged 40–65 the ACC/AHA compared with ESC/EAS guidelines yielded positive NRI of 0.16 for any ASCVD and of 0.23 for fatal ASCVD. Similar results were observed in men and women separately, and for Class IIa recommendations (see Supplementary material online, Figure S5 and Table S6). In a second sensitivity analysis, we included diabetic patients (free of ASCVD at baseline) resulting in a study population of 46 656 individuals [1767(4%) with diabetes]. For a Class I recommendation, 43% qualified for statins using the ACC/AHA guidelines vs. 9% with the ESC/EAS guidelines yielding similar clinical performance as in the main analysis (see Supplementary material online, Table S7). Finally, including statin users (7% of the population) at baseline examination did not explain the observed mismatch between the predicted and observed event rates (see Supplementary material online, Figure S6), and did not change the clinical performance of guidelines (see Supplementary material online, Table S8).
Discussion
In this large, contemporary, population-based European cohort, the US-PCE recommended by the ACC/AHA guidelines was better calibrated around decision thresholds for statin therapy than the European-SCORE model recommended by the ESC/EAS guidelines. Further, the ACC/AHA guidelines were superior to the ESC/EAS guidelines for primary prevention of ASCVD, that is, for assigning statin therapy to those who would benefit the most. Thus, based on the CGPS, these results suggest that the US guidelines have favourable effects on ASCVD prevention compared with the European guidelines.
The European perspective
In individuals aged 40–75, recruited from the general population and free of ASCVD, diabetes and statin use at baseline, <10% qualified for a Class I or IIa recommendation for statin therapy by ESC/EAS guidelines. Because the recommended ‘low-risk’ SCORE equations overestimated fatal ASCVD risk substantially in this cohort, even fewer people would have qualified for statin therapy if well-calibrated equations had been used as recommended.15 Equally troublesome, in people aged 40–75 <15% of those who later developed a first any or fatal ASCVD event qualified at baseline for a Class I recommendation for primary prevention with statin by ESC/EAS guidelines.
European-SCORE overestimated risk substantially in our study, confirming results obtained recently in another ‘low-risk’ European cohort, the Rotterdam Study.23 However, we could not confirm the observed high eligibility for statin treatment by the ESC/EAS guidelines, most likely because the applicable age range for European-SCORE was violated in the Rotterdam Study of elderly people (mean age 66 years), and because the weak Class IIb recommendation for statin therapy in elderly subjects7 was not complied with in the Rotterdam Study. In principle, beyond the age range of 40–65 years for European-SCORE, the ESC/EAS guidelines only provide Class I recommendations for statin therapy to patients with well-defined medical conditions known to be associated with high- or very-high risk, such as established ASCVD (secondary prevention), diabetes, chronic kidney disease and familial hypercholesterolaemia.7,8
The US perspective
When treatment decisions are based on absolute risk for developing any or fatal ASCVD, accurate estimation of absolute risk is essential to treat people as intended by the guidelines. Since its introduction with the 2013 ACC/AHA guidelines, the accuracy (calibration) of the US PCE calculator24 has been questioned, being accused of overestimating risk.23,25,26 Others, however, have found PCE to be well calibrated.11,20 In our contemporary European cohort of whites, US-PCE was much better calibrated than the European-SCORE model. Most importantly, and in contrast to European-SCORE, US-PCE was reasonable well calibrated around the guideline-defined decision thresholds for statin therapy and thus performed as intended clinically. In our study, the PCE-based ACC/AHA recommendations resulted in 5–6 times more individuals from the general population being eligible for statin therapy compared with the SCORE-based ESC/EAS recommendations. It should be noted that the ACC/AHA guidelines recommend a clinician–patient discussion to consider potential benefits and harms of statin therapy, which might lead to decisions other than those indicated by the Class I and IIa recommendations, including withholding statins in individuals with favourable risk factors.
Decision thresholds: to treat or not to treat
Net reclassification index was introduced to evaluate the incremental value of adding predictors and new biomarkers to established risk prediction models,27 such as adding HDL-C to SCORE.28 However, NRI may also be used to compare the clinical performance of different risk prediction models,29 as done in this study. Using a clinically meaningful reclassification approach reflecting the decision ‘to treat or not to treat’ with statins, the binary NRI was positive and high for both any and fatal ASCVD when we used the US-PCE-based ACC/AHA guidelines rather than the European-SCORE-based ESC/EAS guidelines. Interestingly, although US-PCE discriminated better than European-SCORE between cases and non-cases the main reason for the positive NRI was the higher sensitivity of the decision thresholds defined by ACC/AHA compared with those defined by ESC/EAS. Consistently, we found that the sensitivity and specificity of a US-PCE risk of 7.5% were similar to a European-SCORE risk of 2.4%, that is, well below the currently used 5% high-risk threshold. Interestingly, we have recently demonstrated that a substantial gain in sensitivity with a smaller loss in specificity is obtainable by lowering the SCORE-based decision thresholds.15,30 In support of this, risk–benefit9 and cost-effectiveness analyses31 indicate that an ideal risk threshold for primary prevention with statins is around 7.5% 10-year risk for any ASCVD estimated with well-calibrated US-PCE. Recently, it was suggested that an even lower threshold might also be cost-effective.32
Strength and limitations
A potential limitation of our study is that we only studied white Europeans, and extrapolation of our results to non-white populations should be done cautiously. Also, as mean follow-up in the CGPS was <10 years, we assessed calibration of US-PCE and European-SCORE using 5-year models, assuming that the correlation of 5- to 10-year ASCVD events in the CGPS is similar to that observed in the US-PCE and European-SCORE cohorts. However, in the subpopulation of individuals with 10 years of follow-up we observed similar calibration results using 10-year models. Finally, we were not able to adjust for prescription of preventive medication during follow-up, which might have contributed to some of the mismatch between predicted and observed event rates especially among those at higher risk.
A major strength of our study is that the results originate from a contemporary, population-based, and large cohort with not a single person lost to follow-up. Any and fatal ASCVD events were appropriately identified, which is essential for the assessment of calibration, and the results are most likely generalizable to most other non-Eastern European countries, the USA and similar countries. Finally, our results were robust to several sensitivity analyses.
Conclusion
In this contemporary European cohort with no losses to follow-up, the ACC/AHA US-PCE model was better calibrated than the ESC/EAS European-SCORE model. Compared with the ESC/EAS guidelines, the ACC/AHA guidelines were superior for primary prevention of ASCVD, that is, for assigning statin therapy to those who would benefit the most. Our results thus suggest that the US guidelines have favourable effects on ASCVD prevention compared with the European guidelines.
Supplementary material
Supplementary material is available at European Heart Journal online.
Supplementary Material
Acknowledgement
We thank staff and participants of the Copenhagen General Population Study for their contributions.
Funding
Herlev and Gentofte Hospital, Copenhagen University Hospital, the Copenhagen County Foundation, and Aarhus University, all from Denmark. These are all publicly funded, and neither have any influence on the research conducted.
Conflict of interest: none declared.
References
- 1. Murray CJ, Lopez AD.. Measuring the global burden of disease. N Engl J Med 2013;369:448–457. [DOI] [PubMed] [Google Scholar]
- 2. Laslett LJ, Alagona P Jr, Clark BA III, Drozda JP Jr, Saldivar F, Wilson SR, Poe C, Hart M.. The worldwide environment of cardiovascular disease: prevalence, diagnosis, therapy, and policy issues: a report from the American College of Cardiology. J Am Coll Cardiol 2012;60:S1–S49. [DOI] [PubMed] [Google Scholar]
- 3. Dudas K, Lappas G, Stewart S, Rosengren A.. Trends in out-of-hospital deaths due to coronary heart disease in Sweden (1991 to 2006). Circulation 2011;123:46–52. [DOI] [PubMed] [Google Scholar]
- 4. Capewell S, O’Flaherty M.. Rapid mortality falls after risk-factor changes in populations. Lancet 2011;378:752–753. [DOI] [PubMed] [Google Scholar]
- 5. Jørgensen T, Capewell S, Prescott E, Allender S, Sans S, Zdrojewski T, De Bacquer D, de Sutter J, Franco OH, Løgstrup S, Volpe M, Malyutina S, Marques-Vidal P, Reiner Z, Tell GS, Verschuren WM, Vanuzzo D, PEP Section of EACPR. Population-level changes to promote cardiovascular health. Eur J Prev Cardiol 2013;20:409–421. [DOI] [PubMed] [Google Scholar]
- 6. Lloyd-Jones DM. Cardiovascular risk prediction: basic concepts, current status, and future directions. Circulation 2010;121:1768–1777. [DOI] [PubMed] [Google Scholar]
- 7. Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P, Erdine S, Halcox J, Hobbs R, Kjekshus J, Filardi PP, Riccardi G, Storey RF, Wood D.. ESC/EAS Guidelines for the management of dyslipidaemias: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J 2011;32:1769–1818. [DOI] [PubMed] [Google Scholar]
- 8. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corrà U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, L� M-L, Löllgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM, Authors/Task Force Members. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC, Watson K, Wilson PWF.. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. Circulation 2014;129:S1–S45. [DOI] [PubMed] [Google Scholar]
- 10. Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC, Sorlie P, Stone NJ, Wilson PWF.. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. Circulation 2014;129:S49–S73. [DOI] [PubMed] [Google Scholar]
- 11. Ray KK, Kastelein JJP, Boekholdt SM, Nicholls SJ, Khaw K-T, Ballantyne CM, Catapano AL, Reiner Z, Lüscher TF.. The ACC/AHA 2013 guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: the good the bad and the uncertain: a comparison with ESC/EAS guidelines for the management of dyslipidaemias 2011. Eur Heart J 2014;35:960–968. [DOI] [PubMed] [Google Scholar]
- 12. Thomsen M, Nordestgaard BG.. Myocardial infarction and ischemic heart disease in overweight and obesity with and without metabolic syndrome. JAMA Intern Med 2014;174:15–22. [DOI] [PubMed] [Google Scholar]
- 13. Nordestgaard BG, Palmer TM, Benn M, Zacho J, Tybjaerg-Hansen A, Davey Smith G, Timpson NJ.. The effect of elevated body mass index on ischemic heart disease risk: causal estimates from a Mendelian randomisation approach. PLoS Med 2012;9:e1001212.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG, Tybjaerg-Hansen A.. Loss-of-function mutations in APOC3 and risk of ischemic vascular disease. N Engl J Med 2014;371:32–41. [DOI] [PubMed] [Google Scholar]
- 15. Mortensen MB, Afzal S, Nordestgaard BG, Falk E.. The high-density lipoprotein-adjusted SCORE model worsens SCORE-based risk classification in a contemporary population of 30 824 Europeans: the Copenhagen General Population Study. Eur Heart J 2015;36:2446–2453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mortensen MB, Afzal S, Nordestgaard BG, Falk E.. Primary prevention with statins: ACC/AHA risk-based approach versus trial-based approaches to guide statin therapy. J Am Coll Cardiol 2015;66:2699–2709. [DOI] [PubMed] [Google Scholar]
- 17. Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetière P, Jousilahti P, Keil U, Njølstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM.. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003;24:987–1003. [DOI] [PubMed] [Google Scholar]
- 18. Cooney MT, Dudina AL, Graham IM.. Value and limitations of existing scores for the assessment of cardiovascular risk: a review for clinicians. J Am Coll Cardiol 2009;54:1209–1227. [DOI] [PubMed] [Google Scholar]
- 19. ESC HeartScore risk calculator. http://www.heartscore.org (14 September 2016, date last accessed)..
- 20. Muntner P, Colantonio LD, Cushman M, Goff DC, Howard G, Howard VJ, Kissela B, Levitan EB, Lloyd-Jones DM, Safford MM.. Validation of the atherosclerotic cardiovascular disease pooled cohort risk equations. JAMA 2014;311:1406–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Leening MJ, Vedder MM, Witteman JC, Pencina MJ, Steyerberg EW.. Net reclassification improvement: computation, interpretation, and controversies: a literature review and clinician’s guide. Ann Intern Med 2014;160:122–131. [DOI] [PubMed] [Google Scholar]
- 22. Kerr KF, Wang Z, Janes H, McClelland RL, Psaty BM, Pepe MS.. Net reclassification indices for evaluating risk prediction instruments: a critical review. Epidemiology 2014;25:114–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kavousi M, Leening MJG, Nanchen D, Greenland P, Graham IM, Steyerberg EW, Ikram MA, Stricker BH, Hofman A, Franco OH.. Comparison of application of the ACC/AHA guidelines, Adult Treatment Panel III guidelines, and European Society of Cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA 2014;311:1416–1423. [DOI] [PubMed] [Google Scholar]
- 24. ACC/AHA atherosclerotic cardiovascular disease risk calculator. http://tools.acc.org/ASCVD-Risk-Estimator/ (14 September 2016, date last accessed).
- 25. Cook NR, Ridker PM.. Further insight into the cardiovascular risk calculator: the roles of statins, revascularizations, and underascertainment in the Women’s Health Study. JAMA Intern Med 2014;174:1964–1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nissen SE. Prevention guidelines: bad process, bad outcome. JAMA Intern Med 2014;174:1972–1973. [DOI] [PubMed] [Google Scholar]
- 27. Pencina MJ, D’Agostino RB, Pencina KM, Janssens AC, Greenland P.. Interpreting incremental value of markers added to risk prediction models. Am J Epidemiol 2012;176:473–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cooney MT, Dudina A, De Bacquer D, Fitzgerald A, Conroy R, Sans S, Menotti A, De Backer G, Jousilahti P, Keil U, Thomsen T, Whincup P, Graham I, SCORE Investigators. How much does HDL cholesterol add to risk estimation? A report from the SCORE Investigators. Eur J Cardiovasc Prev Rehabil 2009;16:304–314. [DOI] [PubMed] [Google Scholar]
- 29. Leening MJ, Steyerberg EW, Van Calster B, D’Agostino RB Sr, Pencina MJ.. Net reclassification improvement and integrated discrimination improvement require calibrated models: relevance from a marker and model perspective. Stat Med 2014;33:3415–3418. [DOI] [PubMed] [Google Scholar]
- 30. Murphy TP, Dhangana R, Pencina MJ, Zafar AM, D’Agostino RB.. Performance of current guidelines for coronary heart disease prevention: optimal use of the Framingham-based risk assessment. Atherosclerosis 2011;216:452–457. [DOI] [PubMed] [Google Scholar]
- 31. Deaño RC, Pandya A, Jones EC, Borden WB.. A look at statin cost-effectiveness in view of the 2013 ACC/AHA cholesterol management guidelines. Curr Atheroscler Rep 2014;16:438.. [DOI] [PubMed] [Google Scholar]
- 32. Pandya A, Sy S, Cho S, Weinstein MC, Gaziano TA.. Cost-effectiveness of 10-year risk thresholds for initiation of statin therapy for primary prevention of cardiovascular disease. JAMA 2015;314:142–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.