This editorial refers to ‘Increasing sex differences in the use of cardiac resynchronization therapy with or without implantable cardioverter-defibrillator’†, by N.A. Chatterjee et al., on page 1485.
A basic tenet of precision medicine is that individual variability can be harnessed to provide patients with tailored therapies for optimal outcomes.1 In this way, sex-specific medicine is a subset of precision medicine in which a major genetic difference (sex) and associated environmental and lifestyle factors may impact substantially upon clinical phenotypes. In cardiovascular disease (CVD), important sex differences in the rates of diagnosis, utilization of care, response to therapy, and clinical outcomes have been described.2,3 Compared with men, women have a higher prevalence of persistent angina, non-obstructive coronary artery disease, coronary microvascular dysfunction, stress-induced cardiomyopathy, and heart failure with preserved ejection fraction.4,5 CVD risk factors including diabetes mellitus6 and atrial fibrillation7 are associated with higher rates of vascular complications in women vs. men. Women presenting with acute coronary syndromes experience higher mortality as compared with men,8 and are also referred for cardiac transplantation at later stages of heart failure.9
An emerging area of disparity concerns the underutilization in women of cardiac devices, including implantable cardiac defibrillations (ICDs) and cardiac resynchronization therapy (CRT) devices. Among patients hospitalized for heart failure, eligible women are significantly less likely than men to receive ICDs10 and CRT,11 and counselling for ICDs.12 Underscoring the importance of sex-specific research in cardiovascular care,13 sex-specific analyses of clinical practice data demonstrated similarly improved survival in women and men following ICD implant,14 and subgroup analyses of randomized controlled trial data showed that female sex is associated with improved responsiveness to CRT.15 So why are women receiving less cardiac device therapy as compared with men, when it is women who may benefit the most?
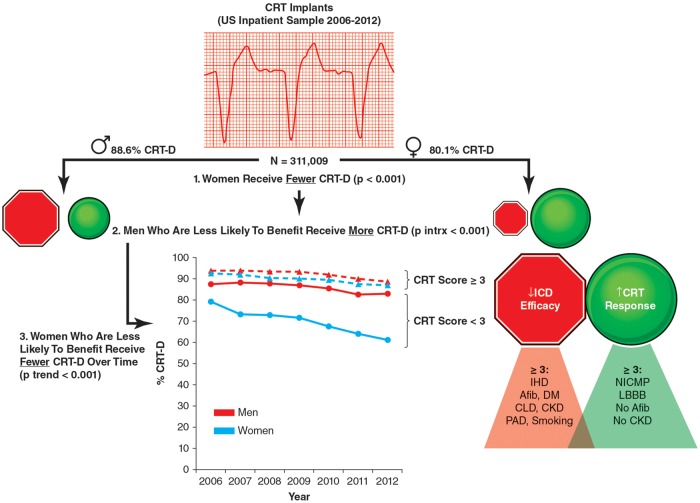
In this issue of the journal, Chatterjee et al.16 contribute another piece of the paradox by describing increasing sex differences in the use of CRT ± ICD across a large and contemporary cohort of patients. The authors performed a retrospective cross-sectional analysis of 311 009 patients (29.6% female) who underwent CRT implant with or without ICD between 2006 and 2012 using the National Inpatient Sample, a publicly available all-payer inpatient database in the USA. They found that sex differences in CRT-D implant were inversely related to predicted CRT efficacy (i.e. among patients with the least likelihood of CRT response, fewer women than men received CRT-D), and that this trend has increased over time. By defining two clinical scores, one for increased CRT responsiveness and another for reduced ICD efficacy using baseline clinical covariates known to be associated with these outcomes (Figure 1), the authors showed that women, as compared with men, were more likely to demonstrate a higher CRT response score (≥3, 47.3 vs. 33.3%, P < 0.001) and less likely to demonstrate a reduced ICD efficacy score (≥3, 27.0 vs. 37.3%, P < 0.001). Despite this, women paradoxically comprised only 27.6% of patients undergoing CRT-D (86.1% of the overall CRT cohort).
Figure 1.
Trends in sex differences in the use of CRT-D in the USA from 2006 to 2012. CRT-D, cardiac resynchronization therapy with implantable cardioverter defibrillator; ICD, implantable cardioverter defibrillator; IHD, ischaemic heart disease; AFib, atrial fibrillation; DM, diabetes mellitus; CLD, chronic lung disease; CKD, chronic kidney disease; PAD, peripheral arterial disease; NICMP, non-ischaemic cardiomyopathy; LBBB, left bundle branch block.
Stated differently, more men than women receiving CRT underwent implant of CRT-D devices (88.6 vs. 80.1%, P < 0.001), especially for patients with lower CRT response scores (<3) and higher reduced ICD efficacy scores (≥1), introducing the hypothesis that previously described sex differences in this area may be due to both overtreatment of men and undertreatment of women (Figure 1). Sex differences appeared to be less pronounced in patients undergoing CRT-D following ventricular arrhythmia or cardiac arrest (a secondary prevention indication for ICD), or in those with non-ischaemic cardiomyopathy and left bundle branch block (LBBB) [guideline-emphasized factors associated with left ventricular (LV) reverse remodelling and CRT response], and were most notable in patients with atrial fibrillation, chronic kidney disease (CKD), and ≥80 years of age. Although the relatively high rate of CRT-D utilization in both women and men with greatest predicted benefit of CRT and ICD was reassuring, the relative excess of men receiving CRT-D among those with a lower predicted benefit raised the possibility of sex-related differences in ‘appropriateness’ of CRT-D implant practices among heart failure inpatients. Multivariable logistic regression analysis confirmed that although patients with the least likelihood of CRT response were indeed less likely to undergo CRT-D [adjusted odds ratio (OR) 0.27, 95% confidence interval (CI) 0.24–0.31], men in this category were much more likely than women to undergo CRT-D implant (P for sex interaction <0.001).
These data prompt us to ask: in patients admitted with heart failure, are we implanting too few CRT-Ds in women, or, possibly, too many in men? If CRT-D implant rates in those with the highest likelihood of CRT response was similarly high in women and men (but also high in men with lower likelihood of CRT response), then are we appropriately optimizing this technology in women, but not in men? When stratified by sex and likelihood of predicted CRT response, only women with a decreased likelihood of CRT response demonstrated a significantly lower rate of CRT-D implant (P for trend <0.001). This finding increased over the 6-year study period (P for trend 0.012), despite greater understanding of predicted CRT and ICD efficacy in women compared with men in more recent times. Furthermore, ICD-only use among women remained stable and low (and between 20% and 30% of cases) throughout the study period.
Perhaps, as with other cases of widespread variations in healthcare utilization, optimal practices may lie somewhere in between. Taken together, these findings suggest that something about CRT-D (and ICD use in particular) rendered it more likely that male vs. female patients were offered and/or more were likely to accept device implant. Although unmeasured confounding (i.e. from baseline differences in demographics, socio-economic state, and healthcare access) remains a possibility, another is that men undergo implant of advanced cardiac device therapy without having to cross a nearly as restrictive perceived cost–benefit threshold as women. Thus, in order to optimize American ‘bang for the buck’ in optimal patient selection for costly device therapy, a two-fold strategy could involve: (i) decreasing the rate of CRT-D implant in men unlikely to benefit (i.e. older men and those with ischaemic heart disease, atrial fibrillation, and/or CKD); and (ii) increasing the rate of CRT-D (and possibly, ICD) implant in women at intermediate likelihood of benefit. Of note, any of these strategies is complicated by the possibility that improved responsiveness to CRT (with associated decrease in heart failure morbidity and mortality, including from ventricular tachyarrhythmia), may also change the calculus for ICD efficacy over the remaining life span, and additional research is needed to tease out potential dynamic effects within the context of sex-specific investigations.
Another limitation of this serial cross-sectional study design relates to its reliance on the use of ICD-9-CM (International Classification of Disease Ninth Revision, Clinical Modification) diagnosis codes to classify groups without consideration of relevant echocardiographic or electrocardiographic data. As published recently in the European Society of Cardiology (ESC) guidelines for the management of patients with ventricular arrhythmias and prevention of sudden cardiac death,17 CRT indications vary according to heart failure symptoms, LV ejection fractiion (LVEF), and QRS morphology and duration. Recommendations for ICD implant for primary prevention of sudden cardiac death in symptomatic heart failure patients similarly incorporate assessments of LVEF and estimated prognosis. As a result, stratifications of likelihood of CRT response or ICD benefit in the current analysis were based on assumptions using an incomplete subset of historical predictors, and outcomes were not measured directly.
Nevertheless, the authors are to be commended for this work, which illustrates the critical importance of performing sex-specific analyses to generate new hypotheses in cardiovascular care. Insights like these may inform future trials and, possibly, the implementation of sex-specific thresholds within clinical guidelines for more optimal patient management. Doing so may allow us to learn not only what we are doing ‘wrong’ or ‘right’ in women, but in all of our male and female patients. Sex-secific medicine is just a form of precision medicine, after all.
Funding
This work was supported by contracts from the National Heart, Lung and Blood Institutes, nos. N01-HV-68161, N01-HV-68162, N01-HV-68163, N01-HV-68164, grants U01 64829, U01 HL649141, U01 HL649241, T32 HL69751, 1R03 AG032631 from the National Institute on Aging, K12 HD051959 Building Interdisciplinary Research Careers in Women’s Health (Taqueti), GCRC grant MO1-RR00425 from the National Center for Research Resources and grants from the Gustavus and Louis Pfeiffer Research Foundation, Danville, NJ, The Women’s Guild of Cedars-Sinai Medical Center, Los Angeles, CA, The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, PA, QMED, Inc., Laurence Harbor, NJ, the Edythe L. Broad Women’s Heart Research Fellowship, Cedars-Sinai Medical Center, Los Angeles, California, and the Barbra Streisand Women’s Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles.
Conflict of interest: none declared.
References
- 1. Collins FS, Varmus H.. A new initiative on precision medicine. N Engl J Med 2015;372:793–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bairey Merz CN. Sex, death, and the diagnosis gap. Circulation 2014;130:740–742. [DOI] [PubMed] [Google Scholar]
- 3. Bairey Merz CN, Regitz-Zagrosek V.. The case for sex- and gender-specific medicine. JAMA Intern Med 2014;174:1348–1349. [DOI] [PubMed] [Google Scholar]
- 4. Pepine CJ, Anderson RD, Sharaf BL, Reis SE, Smith KM, Handberg EM, Johnson BD, Sopko G, Bairey Merz CN.. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia: results from the National Heart, Lung and Blood Institute WISE (Women’s Ischemia Syndrome Evaluation) study. J Am Coll Cardiol 2010;55:2825–2832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Taqueti VR, Shaw LJ, Cook NR, Murthy VL, Shah NR, Foster CR, Hainer J, Blankstein R, Dorbala S, Di Carli MF.. Excess cardiovascular risk in women relative to men referred for coronary angiography is associated with severely impaired coronary flow reserve, not obstructive disease. Circulation 2016;in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huxley R, Barzi F, Woodward M.. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ 2006;332:73–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Køber L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Rønnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A; ESC Committee for Practice Guidelines. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Eur Heart J 2012;33:1787–1847. [DOI] [PubMed] [Google Scholar]
- 8. Champney KP, Frederick PD, Bueno H, Parashar S, Foody J, Merz CN, Canto JG, Lichtman JH, Vaccarino V; NRMI Investigators. The joint contribution of sex, age and type of myocardial infarction on hospital mortality following acute myocardial infarction. Heart 2009;95:895–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Regitz-Zagrosek V, Petrov G, Lehmkuhl E, Smits JM, Babitsch B, Brunhuber C, Jurmann B, Stein J, Schubert C, Merz NB, Lehmkuhl HB, Hetzer R.. Heart transplantation in women with dilated cardiomyopathy. Transplantation 2010;89:236–244. [DOI] [PubMed] [Google Scholar]
- 10. Hernandez AF, Fonarow GC, Liang L, Al-Khatib SM, Curtis LH, LaBresh KA, Yancy CW, Albert NM, Peterson ED.. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA 2007;298:1525–1532. [DOI] [PubMed] [Google Scholar]
- 11. Zusterzeel R, Selzman KA, Sanders WE, Caños DA, O’Callaghan KM, Carpenter JL, Piña IL, Strauss DG.. Cardiac resynchronization therapy in women: US Food and Drug Administration meta-analysis of patient-level data. JAMA Intern Med 2014;174:1340–1348. [DOI] [PubMed] [Google Scholar]
- 12. Hess PL, Hernandez AF, Bhatt DL, Hellkamp AS, Yancy CW, Schwamm LH, Peterson ED, Schulte PJ, Fonarow GC, Al-Khatib SM.. Sex and race/ethnicity differences in implantable cardioverter-defibrillator counseling and use among patients hospitalized with heart failure: findings from the Get With The Guidelines-Heart Failure Program. Circulation 2016;134:517–526. [DOI] [PubMed] [Google Scholar]
- 13. Wenger NK, Ouyang P, Miller VM, Bairey Merz CN.. Strategies and methods for clinical scientists to study sex-specific cardiovascular health and disease in women. J Am Coll Cardiol 2016;67:2186–2188. [DOI] [PubMed] [Google Scholar]
- 14. Zeitler EP, Hellkamp AS, Schulte PJ, Fonarow GC, Hernandez AF, Peterson ED, Sanders GD, Yancy CW, Al-Khatib SM.. Comparative effectiveness of implantable cardioverter defibrillators for primary prevention in women. Circ Heart Fail 2016;9:e002630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, Estes NA 3rd, Foster E, Greenberg H, Higgins SL, Pfeffer MA, Solomon SD, Wilber D, Zareba W; MADIT-CRT Trial Investigators. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med 2009;361:1329–38. [DOI] [PubMed] [Google Scholar]
- 16. Chatterjee NA, Borgquist R, Chang Y, Lewey J, Jackson VA, Singh JP,, Metlay JP, Lindvall C.. Increasing sex differences in the use of cardiac resynchronization therapy with or without implantable cardioverter-defibrillator. Eur Heart J 2017;38:1485–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Priori SG, Blomstrom-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, Elliott PM, Fitzsimons D, Hatala R, Hindricks G, Kirchhof P, Kjeldsen K, Kuck KH, Hernandez-Madrid A, Nikolaou N, Norekvål TM, Spaulding C, Van Veldhuisen DJ.. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Eur Heart J 2015;36:2793–2867. [DOI] [PubMed] [Google Scholar]