Abstract
Background: The causes of stillbirth are poorly understood, including whether elevated outdoor temperatures increase risk. We assessed the relationship between elevated ambient temperatures and risk of stillbirth by gestational age and cause of death during warm months in a temperate region.
Methods: We performed a case-crossover study of 5047 stillbirths in continental Quebec, Canada, between the months of April through September from 1981 to 2011. Using data on maximum daily temperatures adjusted for relative humidity, we estimated associations with stillbirth, comparing temperatures before fetal death with temperatures on adjacent days. The main outcomes were stillbirth according to age of gestation (term, preterm), and cause of death (undetermined, maternal, placenta/cord/membranes, birth asphyxia, congenital anomaly, other).
Results: Elevated outdoor temperatures the week before the death were more strongly associated with risk of term than preterm stillbirth. Odds of term stillbirth for temperature 28 °C the day before death were 1.16 times greater relative to 20 °C (95% confidence interval, CI 1.02-1.33). Elevated outdoor temperature was associated with stillbirth due to undetermined and maternal causes, but not other causes. Compared with 20 °C, the odds of stillbirth at 28 °C were 1.19 times greater for undetermined causes (95% CI 1.02-1.40) and 1.46 times greater for maternal complications (95% CI 1.03-2.07).
Conclusions: Elevated outdoor temperatures may be a risk factor for term stillbirth, including stillbirth due to undetermined causes or maternal complications.
Keywords: Cause of death, gestational age, heat stress disorders, hot temperature, stillbirth
Introduction
Stillbirth is a major global problem. Stillbirths account for 3.1 of every 1000 deliveries in high-income countries.1 Rates have decreased in many regions, but further declines have been difficult to achieve.2 The cause of death is hard to pinpoint or unknown in many stillbirths.2 Risk factors for stillbirth are also very poorly understood. Smoking, obesity, and maternal morbidities account for only a small fraction of deaths.2,3 Few studies have sought to determine if environmental exposures are associated with stillbirth. Air pollution appears to be harmful,4,5 but other meteorological exposures have received little attention. This is particularly true for outdoor heat, a problem expected to increase during this century.
Pregnant women are potentially affected by heat because of physiological changes that alter capacity to regulate body temperature. Pregnancy is a hypervolaemic state, with blood volume expanding by 3 litres or 40-45% at term.6 Pregnant women experience several changes in normal physiological function that alter tolerance to extreme heat,7,8 such as reduced systemic vascular resistance and increased heart rate.6 Few population studies have considered the possibility that elevated temperatures increase risk of stillbirth, despite evidence that pregnant women have greater chance of delivery during hot weather.9–11 In one subtropical region with warm weather during most of the year, risk of stillbirth was greater above mean temperatures of 21 °C compared with cooler temperatures, suggesting a plausible association.12 However, subtropical climates are not representative of temperate regions where seasonal weather fluctuates widely, and where women are not accustomed to heat. A number of studies on seasonality of stillbirth report that rates are higher during summer and winter when temperature extremes are greatest.13
Our objective was to determine the relationship between elevated temperatures and risk of stillbirth. We analysed stillbirths in a continental Canadian province with a temperate climate characterized by warm summers and cold winters.
Methods
Data
We included all singleton fetal deaths between the months of April and September recorded in the provincial stillbirth registry of Quebec, Canada, from 1981 through 2011. In Quebec, all stillborn fetuses weighing 500 g or more are registered regardless of gestational age, and receive a certificate confirming delivery. There were 5047 stillbirths during the study. This sample excludes 268 stillbirths due to pregnancy termination, a cause less likely related to temperature. We did not include stillbirths between October and March, when temperatures are much cooler or subzero.
Stillbirth
The outcome was stillbirth by gestational age and cause. We analysed gestational age because heat stress may be especially problematic late in pregnancy when physiological changes are well advanced.8 Furthermore, heat stress may be more strongly implicated in some causes of stillbirth than others, especially those originating from maternal sources. In particular, elevated temperatures may be implicated in stillbirths with undetermined cause,2 many of which may involve maternal responses to external stress. A proportion of stillbirths with undetermined cause are thought to be incompletely investigated,2 and heat stress is unlikely to have been considered in these cases.
To evaluate risk by gestational age, we separated term from preterm stillbirths. We defined term stillbirth as delivery at 37 completed weeks of gestation or more, and preterm stillbirth as delivery at 36 weeks or less. At 37 weeks, pregnancy is advanced, and environmental heat could potentially be a greater strain compared with preterm. Nonetheless, the specific point in gestation when heat stress may disproportionately affect women is unclear. To assess the possibility that heat affects risk earlier, we evaluated stillbirth using alternate cutpoints, including 35, 33, 31 and 28 weeks. Evidence suggests that 28 weeks distinguishes avoidable from unavoidable stillbirth.14
To classify the principal cause of death we used the method of the Canadian Perinatal Surveillance System,15 grouping International Classification of Disease codes into six possible categories: undetermined (779.9, P95, P96.9); maternal complications (761, P01); disorders of the placenta, cord or membranes (762, P02); birth asphyxia (768, P20-P21); congenital anomaly (740-759, Q00-Q99); and any remaining causes. International Classification of Disease codes were available for the 9th revision before 2000 and 10th thereafter. This classification system comprises several causes less plausibly linked with temperature, such as birth asphyxia, as well as causes that may be disproportionately related to heat stress, including undetermined and maternal complications. Finding a relationship between elevated temperatures and stillbirth for biologically plausible but not other causes would reinforce the results.
Meteorological variables
We obtained historical weather data from Environment Canada for meteorological stations in each of the 18 health regions of Quebec. There are 478 meteorological stations in inhabited areas of Quebec, of which we selected 18 representative of each region, following previous validation work.16 We used continuous maximum daily temperature in each region as the main exposure, as means are less likely to capture acute spikes in temperature. In addition, we included mean percent relative humidity in tertiles (< 65.1, 65.1-76.2, ≥ 76.3%). We did not have data on air pollution. However, elevated temperatures are in the catalytic pathway and a precursor to pollutants.17 To estimate total effects, there should be no adjustment for intermediates such as pollution which mediate the impact of temperature on stillbirth.18
We had data on the date of delivery but not the date of fetal death, a limitation common to stillbirth data in general. In high-income countries only 9-14% of stillbirths are intrapartum, the majority occurring before onset of labour.1,2 For most stillbirths, death occurs 2 days before delivery.3 In this study, the focus was outdoor temperature at time of death, defined as 2 days before delivery. We analysed maximum temperature on the estimated day before death (i.e. 3 days before delivery), providing a window of approximately 24 h for heat to stress pregnant women and the fetus before death. As a secondary exposure, we evaluated maximum temperature the estimated day of death and each day of the week before death. Maximum temperatures the day of death, however, may disproportionately reflect temperatures after the event for some fetuses since the exact time of death was unknown.
Study design
We used a time-stratified case-crossover design to estimate the association between maximum daily temperature and stillbirth, a method ideal for acute exposures and rare outcomes. With case-crossover designs, the case is the day of fetal death and controls consist of nearby days, with each stillbirth its own control.19 The temperature of case days is compared with control days. As stillbirths are perfectly matched to themselves, this method automatically adjusts for characteristics that change little in time among women,19,20 such as age, ethnicity, socioeconomic status, smoking, comorbidity, year and season of conception.21 Case-crossover designs account for unknown confounders that may otherwise have biased the analysis.
To select controls, we extracted days from the same calendar month death occurred.20 If death occurred on a Monday, we selected all other Mondays in the same month as control days, even those after death. This time-stratified method of selecting controls avoids bias from time trends in the exposure.20
Data analysis
We calculated the proportion of stillbirths according to maximum temperature the estimated day before death, and compared the temperature of case days with control days. We used conditional logistic regression to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for the association between stillbirth and maximum daily temperatures on the day of death and each of the 6 preceding days (in separate models), adjusting for relative humidity. To model temperature continuously, we used cubic splines with knots at the 5th, 50th and 95th percentiles.22 We used 20 °C as reference, following research suggesting this is a comfortable temperature unlikely to be associated with heat stress.10 To facilitate the presentation of results for the preceding week, we also analysed temperature categorically (< 15, 15-19.9, 20-27.9, ≥ 28 °C). Analyses were carried out according to gestational age (term, preterm) and cause of death (undetermined, maternal complications, placenta/cord/membranes, birth asphyxia, congenital anomaly, remainder).
Sensitivity analysis
We carried out several sets of sensitivity analyses. To exclude the impact of bridge months with slightly cooler temperatures, we restricted data to June, July and August, the three hottest months of the year. We assessed the relationship between temperature and stillbirth for multiple pregnancies (n = 393). Finally, we restricted analyses to southern urban regions (Laval, Montreal and Montérégie), in case temperatures in northern areas were disproportionately misclassified given the larger areas covered.
We carried out analyses in SAS version 9.3 (SAS Institute Inc., Cary, NC) using the restricted cubic spline macro.23 As the study conformed to Tri-Council Policy requirements, the institutional review board of the University of Montreal Hospital Centre waived ethics review.
Results
There were 5047 stillbirths during the study, including 1693 (33.5%) at term (Table 1). The two most common causes of death were disorders of the placenta, cord and membranes (33.1%) and undetermined (23.6%). Maternal complications accounted for 4.9% of stillbirths, among which premature rupture of membranes (53.2%), oligohydramnios (16.5%) and incompetent cervix (16.1%) were most frequent. Maximum temperature the estimated day before death (3 days before delivery) was ≥ 28 °C for 11.6% of stillbirths. This proportion did not change with gestational age, but was slightly higher for undetermined causes (12.6%), maternal complications (12.5%), birth asphyxia (13.0%) and congenital anomaly (12.3%).
Table 1.
Distribution of stillbirths according to maximum temperature the estimated day before death, Quebec, April through September, 1981–2011a
|
No. stillbirths (%) |
Total no. stillbirths | ||||
|---|---|---|---|---|---|
| < 15 °C | 15-19.9 °C | 20-27.9 °C | ≥ 28 °C | ||
| Gestational age | |||||
| Term | 365 (21.6) | 310 (18.3) | 824 (48.7) | 194 (11.5) | 1693 |
| Preterm | 698 (21.8) | 661 (20.7) | 1467 (45.9) | 372 (11.6) | 3198 |
| Cause of death | |||||
| Undetermined | 272 (22.9) | 232 (19.5) | 536 (45.0) | 150 (12.6) | 1190 |
| Maternal | 65 (26.2) | 39 (15.7) | 113 (45.6) | 31 (12.5) | 248 |
| Placenta, cord, membranes | 335 (20.0) | 352 (21.1) | 804 (48.1) | 180 (10.8) | 1671 |
| Birth asphyxiab | 67 (22.3) | 52 (17.3) | 143 (47.5) | 39 (13.0) | 301 |
| Congenital anomaly | 164 (23.5) | 136 (19.5) | 311 (44.6) | 86 (12.3) | 697 |
| Remaining causes | 200 (21.3) | 196 (20.9) | 446 (47.4) | 98 (10.4) | 940 |
| Total | 1103 (21.9) | 1007 (20.0) | 2353 (46.6) | 584 (11.6) | 5047 |
The distribution of stillbirths for temperature on the estimated day of death resembled the day before death, and is not shown.
Temperatures are for 3 days before delivery, and the estimated date of death is 2 days before delivery for all causes except birth asphyxia which occurs intrapartum.
Maximum temperature the estimated day before death ranged from -12.4 to 36.1 °C (Table 2). Temperature of case and control days differed little when stillbirths were examined monthly, regardless of gestational age or cause. Differences were widest in August for maternal complications (1.3 °C higher for case days, 95% CI 0.4, 2.3) and May for remaining causes (1.0 °C higher for case days, 95% CI -0.8, 2.0).
Table 2.
Maximum temperature the estimated day before death, Quebec, April through September, 1981–2011
|
Maximum temperature, mean °C (range) |
||||||
|---|---|---|---|---|---|---|
| April | May | June | July | August | September | |
| (N = 800 stillbirths) | (N = 871 stillbirths) | (N = 852 stillbirths) | (N = 874 stillbirths) | (N = 825 stillbirths) | (N = 825 stillbirths) | |
| Gestational time | ||||||
| Term | ||||||
| Cases | 9.1 (-10.5-27.1) | 18.0 (-0.6-32.3) | 23.0 (7.0-34.0) | 25.4 (11.3-33.5) | 25.1 (12.2-33.9) | 20.0 (8.7-31.9) |
| Controls | 9.8 (-7.5-30.4) | 17.4 (-1.1-31.8) | 22.7 (6.6-36.1) | 25.4 (11.0-35.6) | 24.5 (7.4-35.4) | 20.2 (5.6-34.2) |
| Preterm | ||||||
| Cases | 9.9 (-4.5-30.7) | 17.8 (2.5-34.9) | 22.7 (3.9-34.5) | 25.3 (11.3-35.1) | 24.5 (11.4-34.0) | 20.3 (3.8-33.9) |
| Controls | 9.6 (-12.4-30.0) | 17.5 (-2.5-34.9) | 22.8 (4.6-34.5) | 25.3 (12.2-34.8) | 24.5 (9.2-35.4) | 20.2 (4.1-33.6) |
| Cause of death | ||||||
| Undetermined | ||||||
| Cases | 9.6 (-10.5-27.5) | 17.2 (-0.6-32.8) | 23.0 (3.9-34.5) | 25.6 (11.3-34.2) | 25.0 (12.6-34.0) | 20.3 (7.8-33.3) |
| Controls | 9.6 (-6.0-30.0) | 17.5 (-1.1-33.0) | 22.7 (4.6-33.5) | 25.1 (11.0-34.7) | 24.5 (9.2-35.4) | 20.1 (5.6-33.6) |
| Maternal complications | ||||||
| Cases | 8.2 (-3.4-23.6) | 17.5 (9.0-29.5) | 23.0 (9.4-32.2) | 25.5 (15.9-34.7) | 25.7 (18.2-32.3) | 19.6 (3.8-29.8) |
| Controls | 9.3 (-3.9-21.9) | 17.2 (3.8-34.9) | 22.6 (10.3-33.6) | 25.7 (16.0-33.7) | 24.4 (16.1-33.8) | 19.3 (4.1-31.1) |
| Placenta, cord, membranes | ||||||
| Cases | 9.8 (-1.0-27.5) | 18.0 (5.5-32.3) | 22.7 (8.5-33.0) | 25.3 (11.3-35.1) | 24.7 (12.2-33.8) | 20.3 (8.7-31.8) |
| Controls | 9.9 (-7.5-30.4) | 17.5 (1.8-34.7) | 22.7 (7.8-34.5) | 25.6 (13.3-35.6) | 24.6 (7.4-35.4) | 20.1 (5.6-34.2) |
| Birth asphyxiaa | ||||||
| Cases | 8.9 (-1.6-26.5) | 18.3 (4.1-31.0) | 22.4 (12.7-34.0) | 24.7 (16.1-33.1) | 25.5 (11.4-32.3) | 19.9 (10.0-33.9) |
| Controls | 9.2 (-4.4-29.4) | 17.5 (6.2-30.0) | 22.6 (10.5-33.4) | 25.7 (12.2-33.9) | 24.6 (14.0-33.8) | 20.0 (7.7-30.5) |
| Congenital anomaly | ||||||
| Cases | 9.6 (-3.8-26.8) | 17.3 (2.5-29.9) | 22.9 (7.8-33.9) | 25.9 (16.5-33.6) | 24.0 (16.1-34.0) | 19.8 (9.8-31.1) |
| Controls | 9.4 (-12.4-26.8) | 17.4 (4.3-32.7) | 22.9 (10.0-33.1) | 25.3 (14.3-34.8) | 24.7 (9.7-34.4) | 20.4 (7.6-33.0) |
| Remaining causes | ||||||
| Cases | 10.5 (-4.6-30.7) | 18.5 (4.4-34.9) | 22.4 (7.4-33.8) | 24.7 (12.5-34.0) | 24.3 (14.8-33.5) | 20.4 (7.4-31.9) |
| Controls | 10.0 (-7.0-30.0) | 17.5 (-2.5-33.5) | 22.6 (4.8-36.1) | 25.3 (15.8-34.8) | 24.2 (12.6-32.7) | 20.3 (7.8-32.1) |
| Total | ||||||
| Cases | 9.7 (-10.5-30.7) | 17.8 (-0.6-34.9) | 22.8 (3.9-34.5) | 25.3 (11.3-35.1) | 24.7 (11.4-34.0) | 20.2 (3.8-33.9) |
| Controls | 9.7 (-12.4-30.4) | 17.5 (-2.5-34.9) | 22.7 (4.6-36.1) | 25.4 (11.0-35.6) | 24.5 (7.4-35.4) | 20.2 (4.1-34.2) |
Temperatures are for 3 days before delivery, and the estimated date of death is 2 days before delivery for all causes except birth asphyxia which occurs intrapartum.
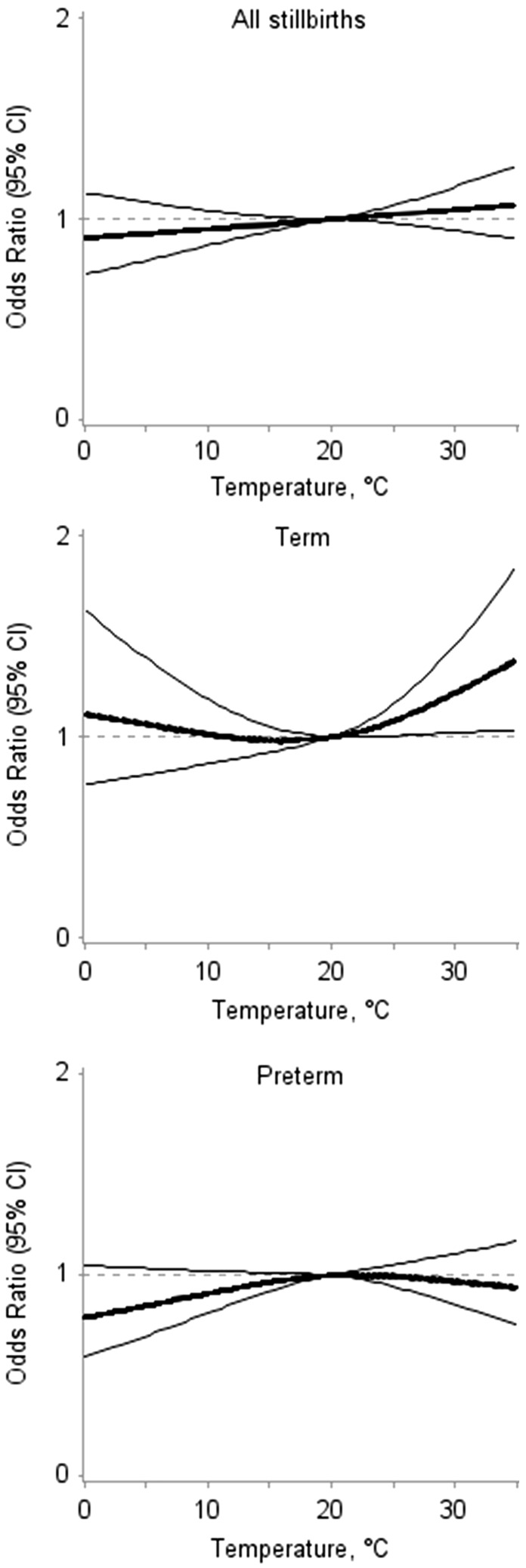
In regression models adjusted for relative humidity, elevated maximum temperatures the estimated day before death were weakly associated with term but not preterm stillbirth (Figure 1). Relative to 20 °C, a maximum temperature of 28 °C the estimated day before death was associated with 1.16 times the odds of term stillbirth (95% CI 1.02-1.33). Temperatures of 30 °C were associated with 1.22 times (95% CI 1.02-1.46) and 32 °C with 1.28 times (95% CI 1.03-1.60) the odds of term stillbirth. Associations were also present for stillbirths ≥ 35 weeks, but decreased progressively with lower gestational age, and were completely masked at 28 weeks. At cooler temperatures, the odds of preterm stillbirth appeared slightly protective.
Figure 1.
Association between stillbirth and maximum temperature the estimated day before death by gestational age, Quebec, April through September, 1981–2011. *Odds ratio (central line) and 95% confidence interval (outer bands), relative to 20 °C.
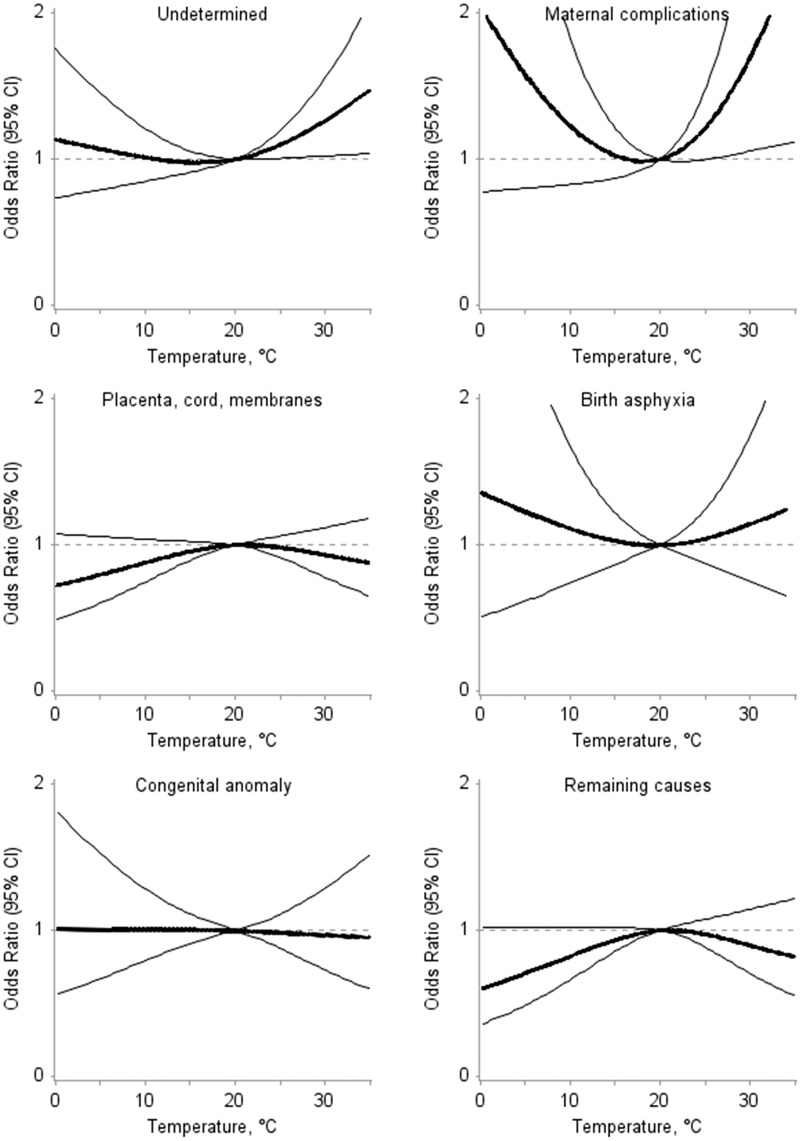
Maximum temperatures above 20 °C were weakly associated with stillbirth due to undetermined causes and maternal complications, but not other causes (Figure 2). Compared with 20 °C, a temperature of 28 °C on the estimated day before death was associated with 1.19 higher odds of stillbirth from undetermined causes (95% CI 1.02-1.40), and 1.46 higher odds of stillbirth from maternal complications (95% CI 1.03-2.07). At 32 °C, the odds of stillbirth were 1.35 times greater for undetermined causes (95% CI 1.03-1.77), and 1.98 times greater for maternal complications (95% CI 1.08-3.60). Temperatures below 20 °C appeared to decrease the odds of stillbirth due to disorders of the placenta, cord, and membranes and remaining causes, and increase the odds of stillbirth due to maternal complications and birth asphyxia.
Figure 2.
Association between stillbirth and maximum temperature the estimated day before death by cause, Quebec, April through September, 1981–2011 *Odds ratio (central line) and 95% confidence interval (outer bands), relative to 20 °C. Temperatures are for 3 days before delivery, and the estimated date of death is 2 days before delivery for all causes except birth asphyxia which occurs intrapartum.
When the week preceding death was examined, there tended to be associations with maximum temperatures for up to 4 days before term stillbirth, and stillbirth due to undetermined causes or maternal complications (Table 3; Figure S1, available as Supplementary data at IJE online). Four days before death, maximum temperatures of ≥ 28 °C were associated with 1.14 higher odds of any stillbirth (95% CI 1.00-1.29) and 1.32 higher odds of term stillbirth (95% CI 1.06-1.65) relative to 15-19.9 °C. Five days before death, however, there was little evidence that temperature was associated with stillbirth. For undetermined causes, associations were strongest the estimated day of and day before death, and for maternal complications, the associations were strongest 2 days before death.
Table 3.
Association between maximum temperature and stillbirth in the week before the death, Quebec, April–September, 1981–2011a
|
Odds ratio (95% CI) |
|||||
|---|---|---|---|---|---|
| All stillbirths (N = 5047) | Term (N = 1693) | Preterm (N = 3198) | Undetermined (N = 1190) | Maternal complications (N = 248) | |
| Day of death | |||||
| 15, 19.9 °C | Referent | Referent | Referent | Referent | Referent |
| 20, 27.9 °C | 1.04 (0.95-1.13) | 0.98 (0.84-1.15) | 1.07 (0.95-1.20) | 1.14 (0.94-1.39) | 1.44 (0.93-2.22) |
| ≥ 28 °C | 1.10 (0.97-1.25) | 1.01 (0.81-1.25) | 1.16 (0.99-1.35) | 1.29 (0.99-1.69) | 1.06 (0.56-2.02) |
| Day before death | |||||
| 15, 19.9 °C | Referent | Referent | Referent | Referent | Referent |
| 20, 27.9 °C | 1.06 (0.97-1.17) | 1.19 (1.01-1.39) | 1.02 (0.91-1.14) | 1.07 (0.88-1.29) | 1.32 (0.84-2.06) |
| ≥ 28 °C | 1.08 (0.95-1.22) | 1.16 (0.93-1.45) | 1.06 (0.91-1.24) | 1.26 (0.97-1.62) | 1.57 (0.87-2.83) |
| 2 days before death | |||||
| 15, 19.9 °C | Referent | Referent | Referent | Referent | Referent |
| 20, 27.9 °C | 0.96 (0.88-1.05) | 1.00 (0.85-1.17) | 0.92 (0.83-1.04) | 0.90 (0.74-1.08) | 1.57 (1.00-2.47) |
| ≥ 28 °C | 1.09 (0.96-1.24) | 1.13 (0.91-1.40) | 1.05 (0.90-1.23) | 1.09 (0.84-1.42) | 2.18 (1.21-3.92) |
| 3 days before death | |||||
| 15, 19.9 °C | Referent | Referent | Referent | Referent | Referent |
| 20, 27.9 °C | 0.99 (0.91-1.09) | 1.03 (0.88-1.20) | 0.98 (0.88-1.10) | 1.00 (0.83-1.20) | 1.33 (0.87-2.03) |
| ≥ 28 °C | 1.11 (0.98-1.26) | 1.20 (0.96-1.49) | 1.08 (0.92-1.27) | 1.07 (0.82-1.39) | 1.47 (0.82-2.63) |
| 4 days before death | |||||
| 15, 19.9 °C | Referent | Referent | Referent | Referent | Referent |
| 20, 27.9 °C | 1.12 (1.02-1.22) | 1.19 (1.01-1.41) | 1.08 (0.96-1.21) | 1.11 (0.92-1.35) | 1.00 (0.66-1.51) |
| ≥ 28 °C | 1.14 (1.00-1.29) | 1.32 (1.06-1.65) | 1.06 (0.91-1.25) | 1.01 (0.77-1.33) | 0.84 (0.47-1.49) |
| 5 days before death | |||||
| 15, 19.9 °C | Referent | Referent | Referent | Referent | Referent |
| 20, 27.9 °C | 1.09 (1.00-1.20) | 1.07 (0.91-1.26) | 1.12 (1.00-1.25) | 1.09 (0.90-1.31) | 1.11 (0.72-1.70) |
| ≥ 28 °C | 0.90 (0.78-1.02) | 0.98 (0.78-1.22) | 0.88 (0.74-1.03) | 0.88 (0.67-1.15) | 0.68 (0.36-1.30) |
| 6 days before death | |||||
| 15, 19.9 °C | Referent | Referent | Referent | Referent | Referent |
| 20, 27.9 °C | 1.04 (0.95-1.14) | 1.14 (0.97-1.34) | 1.02 (0.91-1.14) | 0.94 (0.78-1.13) | 0.99 (0.65-1.50) |
| ≥ 28 °C | 1.04 (0.91-1.18) | 1.06 (0.84-1.33) | 1.05 (0.90-1.24) | 0.80 (0.61-1.06) | 1.21 (0.67-2.20) |
Temperatures < 15 °C were used in the analysis, but are not shown to conserve space. Similarly, stillbirths from other causes are not shown.
When we restricted the sample to June through August, and to southern parts of Quebec, we obtained similar results. For multiple pregnancies, we found a similar pattern of increasing associations at 37 weeks or more, but not at lower gestational ages. Excluding humidity from regression models did not affect the results. Finally, alternate knot locations and a greater quantity of knots in splines did not impact on results.
Discussion
Main findings
This study suggests that elevated outdoor temperatures may be weakly associated with risk of stillbirth at term and stillbirth due to undetermined causes or maternal complications. We found no association with preterm stillbirth, or stillbirth due to other causes including placenta, cord and membranes, congenital anomaly, birth asphyxia and the remainder. Thus, this study provides novel evidence of an association between elevated temperatures and risk of stillbirth, suggesting in particular that undetermined or maternal causes may account for a portion of fetal deaths at term. The findings are timely in light of the challenge of climate change and possibility of increasing heat waves this century. Pregnant women may merit closer monitoring at term during hot weather.
Timing of stillbirth
Only one study has to our knowledge examined the association between ambient temperature and stillbirth by gestational age, but in subtropical weather. The study, carried out in Brisbane, Australia, found no association between elevated temperatures and term stillbirth but did report greater risk of preterm stillbirth.12 We in contrast found an association primarily at term. Why our findings differed is not clear, but the study analysed mean temperature in the preceding week and month as a chronic rather than acute exposure. Also, subtropical regions are warm throughout the year and contain populations more acclimatized to heat. In temperate regions such as Quebec, temperatures fluctuate widely and women may not be as resilient to sudden heat exposures at advanced gestation. A study in Sweden investigated the association with cold exposures, but did not examine if risk varied for term and preterm stillbirth.24
In pregnancy, several physiological changes occur that affect temperature regulation. Near term, weight increases by around 12.5 kilograms6 along with fat deposits that retain body heat25 and diminish the ratio of surface area to body mass, affecting heat loss through sweating.8 Thermoregulation may equally be affected by blood shunted disproportionately to the fetus and vital organs, rather than the skin surface.9 The growing fetus further increases the basal metabolic rate through its own metabolism.6,8 These physiological changes all peak at term, and may be compounded by physical challenges of advanced pregnancy. Elevated temperatures may be particularly relevant during the 4 days before death, as associations at term were strongest during this time.
Cause of stillbirth
The relation between elevated temperatures and specific causes of stillbirth has received less attention. In this study, maximum temperatures were associated with undetermined causes of stillbirth, suggesting that heat may be part of the pathway for at least some of these deaths. By definition, the cause of undetermined deaths is unknown, and possible involvement of temperature in at least some of these deaths has not been raised, despite evidence that heat affects infant and elderly mortality.26,27 Our results suggest that temperature was most strongly associated with undetermined cases on the day of and day before death but also 2 and 3 days previously, which may be informative for future research to determine underlying mechanisms.
Maternal complications were the only other cause where we found a relationship, with evidence of an association with temperature up to 3 days before death. Most maternal complications involved premature rupture of membranes, and less frequently oligohydramnios. Oligohydramnios, or insufficient amniotic fluid, sometimes results from preterm premature rupture of membranes6 but also is affected by dehydration, fetal or placental causes,28 all factors which plausibly respond to temperature within 3 days of exposure. In a Parisian study of a small sample of pregnant women at term, oligohydramnios was more frequent during the August 2003 heat wave than at other comparable times.29 In southern Israel, preterm premature rupture of membranes was common on days with wide differences in temperature.30
The association with maternal complications is also interesting in light of research suggesting that heat can trigger early delivery,9–11 possibly by increasing uterine contractility.7 The pathways have yet to be elucidated, but some propose that heat-shock proteins are released during heat stress.31 Heat-shock proteins may be linked with preterm births,32 some of which may be due to premature rupture of membranes. These pathways have been raised for preterm birth, but may also be present for stillbirth caused by premature rupture of membranes.
Others have reported that heat may be associated with congenital anomalies,33 but we found no evidence of an association with stillbirth due to anomalies. Some have proposed that placental disorders interfere in heat exchange through umbilical vessels,8 but we found no association between maximum temperatures and stillbirth due to placental disorders. Seasonality of stillbirth varies with context, but some studies report high rates in summer and winter,13 though these data mask temperature variation in any given season.
Limitations
We used temperatures recorded in meteorological stations representative of regions in Quebec, but misclassification of exposure may still be present. Interior temperatures were not available, which is problematic if women spent the majority of their time indoors, lived in urban heat islands or had air conditioning. Results for cooler temperatures should be interpreted with caution since minimum temperature is more relevant during cold, and winter months were excluded from the analysis. We used cubic splines to estimate associations, and do not know whether results would have differed with an alternative analytical method. We were limited by the data available on cause of death, which may have led to misclassification (though we have no reason to suspect this varied by temperature). Numerous classification systems exist, but we only had International Classification of Disease codes, although in Quebec the majority of stillbirths are autopsied (71%). We used 2 days before delivery as the estimated day of death, but do not know if this varied by cause.
Conclusions
We found associations between elevated outdoor temperatures and stillbirth at term, potentially explained by undetermined causes and maternal complications. These findings are informative for research on the causes of stillbirth, and demonstrate a possible link with environmental temperature. The possibility that heat will contribute to more stillbirths in the future requires evaluation, including the effectiveness of preventive measures such as air conditioning and self-hydration. In the meantime, early warning systems for heat alerts should consider including pregnant women as a group at risk.
Supplementary Data
Supplementary data are available at IJE online.
Funding
This work was supported by the Canadian Institutes of Health Research (grant number MOP-142277). N.A. acknowledges a career award from the Fonds de recherche du Québec-Santé (grant number 25128).
Conflict of interest: None.
Key Messages
Impacts of climate on risk of stillbirth are poorly understood.
Using a case-crossover design, we examined the association between elevated outdoor temperatures and stillbirth.
Elevated temperatures were associated with increased risk of stillbirth at advanced gestational ages.
Risk at higher temperatures was greater for stillbirth due to undetermined and maternal causes.
Supplementary Material
References
- 1. Lawn JE, Blencowe H, Pattinson R. et al. Stillbirths: Where? When? Why? How to make the data count? Lancet 2011;377:1448–63. [DOI] [PubMed] [Google Scholar]
- 2. Flenady V, Middleton P, Smith GC. et al. Stillbirths: the way forward in high-income countries. Lancet 2011;377:1703–17. [DOI] [PubMed] [Google Scholar]
- 3. Gardosi J, Madurasinghe V, Williams M, Malik A, Francis A.. Maternal and fetal risk factors for stillbirth: population based study. BMJ 2013;346:f108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Green R, Sarovar V, Malig B, Basu R.. Association of stillbirth with ambient air pollution in a California cohort study. Am J Epidemiol 2015;181:874–82. [DOI] [PubMed] [Google Scholar]
- 5. Hwang BF, Lee YL, Jaakkola JJ.. Air pollution and stillbirth: a population-based case-control study in Taiwan. Environ Health Perspect 2011;119:1345–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cunningham FG, Leveno KJ, Bloom SL. et al. Williams Obstetrics. 24th edn New York, NY: McGraw-Hill Professional, 2015. [Google Scholar]
- 7. Vaha-Eskeli K, Erkkola R.. The effect of short-term heat stress on uterine contractility, fetal heart rate and fetal movements at late pregnancy. Eur J Obstet Gynecol Reprod Biol 1991;38:9–14. [DOI] [PubMed] [Google Scholar]
- 8. Wells JC. Thermal environment and human birth weight. J Theor Biol 2002;214:413–25. [DOI] [PubMed] [Google Scholar]
- 9. Basu R, Malig B, Ostro B.. High ambient temperature and the risk of preterm delivery. Am J Epidemiol 2010;172:1108–17. [DOI] [PubMed] [Google Scholar]
- 10. Auger N, Naimi AI, Smargiassi A, Lo E, Kosatsky T.. Extreme heat and risk of early delivery among preterm and term pregnancies. Epidemiology 2014;25:344–50. [DOI] [PubMed] [Google Scholar]
- 11. Wang J, Williams G, Guo Y, Pan X, Tong S.. Maternal exposure to heatwave and preterm birth in Brisbane, Australia. BJOG 2013;120:1631–41. [DOI] [PubMed] [Google Scholar]
- 12. Strand LB, Barnett AG, Tong S.. Maternal exposure to ambient temperature and the risks of preterm birth and stillbirth in Brisbane, Australia. Am J Epidemiol 2012;175:99–107. [DOI] [PubMed] [Google Scholar]
- 13. Strand LB, Barnett AG, Tong S.. The influence of season and ambient temperature on birth outcomes: a review of the epidemiological literature. Environ Res 2011;111:451–62. [DOI] [PubMed] [Google Scholar]
- 14. Goldenberg RL, McClure EM, Bhutta ZA. et al. Stillbirths: the vision for 2020. Lancet 2011;377:1798–805. [DOI] [PubMed] [Google Scholar]
- 15. Public Health Agency of Canada. Canadian Perinatal Health Report. Ottawa: Ministry of Health, 2008. [Google Scholar]
- 16. Lebel G, Bustinza R.. Surveillance Des Impacts Sanitaires Des Vagues De Chaleur Au Québec, Bilan De La Saison Estivale 2010 [in French]. (In English: Surveillance of Impacts of Heat Waves on Health in Quebec, Summer 2010). Québec, QC: Institut national de santé publique du Québec, 2011. [Google Scholar]
- 17. Anderson GB, Krall JR, Peng RD, Bell ML.. Is the relation between ozone and mortality confounded by chemical components of particulate matter? Analysis of 7 components in 57 US communities. Am J Epidemiol 2012;176:726–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Buckley JP, Samet JM, Richardson DB.. Commentary: Does air pollution confound studies of temperature? Epidemiology 2014;25:242–45. [DOI] [PubMed] [Google Scholar]
- 19. Maclure M, Mittleman MA.. Should we use a case-crossover design? Annu Rev Public Health 2000;21:193–221. [DOI] [PubMed] [Google Scholar]
- 20. Janes H, Sheppard L, Lumley T.. Case-crossover analyses of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology 2005;16:717–26. [DOI] [PubMed] [Google Scholar]
- 21. Darrow LA, Strickland MJ, Klein M. et al. Seasonality of birth and implications for temporal studies of preterm birth. Epidemiology 2009;20:699–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Durrleman S, Simon R.. Flexible regression models with cubic splines. Stat Med 1989;8:551–61. [DOI] [PubMed] [Google Scholar]
- 23. Heinzl H, Kaider A.. Gaining more flexibility in Cox proportional hazards regression models with cubic spline functions. Comput Methods Programs Biomed 1997;54:201–08. [DOI] [PubMed] [Google Scholar]
- 24. Bruckner TA, Modin B, Vagero D.. Cold ambient temperature in utero and birth outcomes in Uppsala, Sweden, 1915-1929. Ann Epidemiol 2014;24:116–21. [DOI] [PubMed] [Google Scholar]
- 25. Wells JC, Cole TJ.. Birth weight and environmental heat load: a between-population analysis. Am J Phys Anthropol 2002;119:276–82. [DOI] [PubMed] [Google Scholar]
- 26. Basagana X, Sartini C, Barrera-Gomez J. et al. Heat waves and cause-specific mortality at all ages. Epidemiology 2011;22:765–72. [DOI] [PubMed] [Google Scholar]
- 27. Basu R,, Ostro BD.. A multicounty analysis identifying the populations vulnerable to mortality associated with high ambient temperature in California. Am J Epidemiol 2008;168:632–37. [DOI] [PubMed] [Google Scholar]
- 28. Flack NJ, Sepulveda W, Bower S,, Fisk NM.. Acute maternal hydration in third-trimester oligohydramnios: effects on amniotic fluid volume, uteroplacental perfusion, and fetal blood flow and urine output. Am J Obstet Gynecol 1995;173:1186–91. [DOI] [PubMed] [Google Scholar]
- 29. Luton D, Alran S, Fourchotte V, Sibony O, Oury JF.. Paris heat wave and oligohydramnios. Am J Obstet Gynecol 2004;191:2103–05. [DOI] [PubMed] [Google Scholar]
- 30. Yackerson N, Piura B, Sheiner E.. The influence of meteorological factors on the emergence of preterm delivery and preterm premature rupture of membrane. J Perinatol 2008;28:707–11. [DOI] [PubMed] [Google Scholar]
- 31. Daugaard M, Rohde M, Jaattela M.. The heat shock protein 70 family: Highly homologous proteins with overlapping and distinct functions. FEBS Lett 2007;581:3702–10. [DOI] [PubMed] [Google Scholar]
- 32. Fukushima A, Kawahara H, Isurugi C. et al. Changes in serum levels of heat shock protein 70 in preterm delivery and pre-eclampsia. J Obstet Gynaecol Res 2005;31:72–77. [DOI] [PubMed] [Google Scholar]
- 33. Van Zutphen AR, Lin S, Fletcher BA, Hwang SA. A population-based case-control study of extreme summer temperature and birth defects. Environ Health Perspect 2012;120:1443–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.