Scientific statement of the transnational alliance for regenerative therapies in cardiovascular syndromes (TACTICS) international group for the comprehensive cardiovascular application of regenerative medicinal products
Introduction
Based on the increasingly understood regenerative capacity of the human heart and vascular system,1 cardiovascular regenerative medicine (CRM) encompasses all potential diagnostic and therapeutic strategies aimed at restoring organ health. Envisioned to enhance the innate regenerative response of cardiovascular tissues, diverse and often complementary products and strategies have been investigated (e.g. stem and progenitor cells, stromal cells, extracellular vesicles such as microvesicles and exosomes, growth factors, non-coding RNAs, episomes and other gene therapies, biomaterials, tissue engineering products, and neo-organogenesis). Despite promising results based on 20 years of research, next generation CRM treatments have yet to transform cardiovascular practice.
Given the compelling need for a thorough critical debate on the past, present, and future of CRM, the international consortium Transnational AllianCe for regenerative Therapies In Cardiovascular Syndromes (TACTICS, www.tacticsalliance.org)2 summarizes the shared vision of leading expert teams in the field (for a complete list of TACTICS members please see Annex 1). The document addresses key priorities and challenges, including basic and translational research, clinical practice, regulatory hurdles, and funding sources. The methodological procedure included the following: (i) identification of strengths, weaknesses, opportunities, and threats (SWOT analysis) by means of an open poll; (ii) distribution of the main topics between at least two worldwide key opinion leaders, who prepared proposals for each topic; (iii) open discussion and consensus on each proposal between all members of TACTICS; and (iv) review of the document by an independent committee.
Annex 1.
| SURNAME, NAME | INSTITUTION |
|---|---|
| Anker, Stefan | Charité Medical School (BERLIN, GERMANY) |
| Anversa, Piero | Harvard Medical School (BOSTON, USA) |
| Atsma, Douwe | Leiden University Medical Center (LEIDEN, THE NETHERLANDS) |
| Badimon, Lina | Cardiovascular Research Center -CSIC (BARCELONA, SPAIN) |
| Balkan, Wayne | University of Miami Miller School of Medicine (MIAMI, USA) |
| Bartunek, Jozef | Cardiovascular Center, OLV Hospital (AALST, BELGIUM) |
| Bayés-Genís, Antoni | Hospital German Trias y Pujol (BARCELONA, SPAIN) |
| Behfar, Atta | Mayo Clinic (ROCHESTER, USA) |
| Bergmann, Martin | Asklepios Klinik St. Georg (HAMBURG, GERMANY) |
| Bolli, Roberto | University of Louisville, (LOUISVILLE, USA) |
| Brofman, Paulo | Pontifícia Universidade Católica do Paraná, (CURITIBA, BRASIL) |
| Broughton, Kathleen | San Diego State University (SAN DIEGO, USA) |
| Campos de Carvalho, Antonio C | Federal Univ Rio de Janeiro, (RIO DE JANEIRO, BRASIL) |
| Chachques, Juan Carlos | Hopital George Pompidou (PARIS, FRANCE) |
| Chamuleau, Steven | University Medical Centre (UTRECHT, THE NETHERLANDS) |
| Charron, Dominique | Hopital Saint Louis (PARIS, FRANCE) |
| Climent, Andreu M | Hospital Gregorio Marañon (MADRID, SPAIN) |
| Crea, Filippo | Universita Cattolica de Sacro Cuore (ROME, ITALY) |
| D´Amario, Domenico | Universita Cattolica de Sacro Cuore (ROME, ITALY) |
| Davidson, Sean M | University College London, (LONDON, UK) |
| Dib, Nabil | University of Arizona Medical College (PHOENIX, USA) |
| DiFede, Darcy | University of Miami (MIAMI, USA) |
| Dimmeler, Stefanie | University Frankfurt, (FRANKFURT, GERMANY) |
| do Rosario, Luis Bras | Instituto Gulbenkian de Ciência (LISBON, PORTUGAL) |
| Duckers, Eric | University Medical Center Utrecht (UTRECTH, NETHERLANDS) |
| Engel, Felix B | Friedrich-Alexander-Universität Erlangen-Nürnberg, (ERLANGEN, GERMANY) |
| Eschenhagen, Thomas | University Medical Center Hamburg-Eppendorf (HAMBURG, GERMANY) |
| Ferdinandy, Péter | Semmelweis University (BUDAPEST, HUNGARY) |
| Fernández Santos, María Eugenia | Hospital Gregorio Marañon (MADRID, SPAIN) |
| Fernández-Avilés, Francisco | Hospital Gregorio Marañon (MADRID, SPAIN) |
| Filippatos, Gerasimos | Athens University Hospital, (ATHENS, GREECE) |
| Fuster, Valentin | The Mount Sinai Hospital (NEWYORK, USA) |
| Gersh, Bernard | Mayo Clinic (ROCHESTER, USA) |
| Goliasch, Georg | Medical University of Vienna (VIENNA, AUSTRIA) |
| Görbe, Anikó | Semmelweis University (BUDAPEST, HUNGARY) |
| Gyöngyösi, Mariann | Univ. Klinik für Innere Medizin II (VIENA, AUSTRIA) |
| Hajjar, Roger J | The Mount Sinai Hospital (BOSTON, USA) |
| Hare, Joshua M | University of Miami (MIAMI, USA) |
| Hausenloy, Derek J | University College London (LONDON, UK) |
| Henry, Timothy D | Cedars Sinai (LOS ANGELES, USA) |
| Izpisua, Juan Carlos | Salk Institue (LA JOLLA, USA) |
| Janssens, Stefan | KU Leuven (LEUVEN, BELGIUM) |
| Jiménez Quevedo, Pilar | Hospital Clínico San Carlos (MADRID, SPAIN) |
| Kastrup, Jens | Rigshospitalet University (COPENHAGUEN, DENMARK) |
| Kim, Hyo-Soo | Seoul National University Hospital, (SEOUL, KOREA) |
| Landmesser, Ulf | Universitätsmedizin Berlin (BERLIN, GERMANY) |
| Lecour, Sandrine | Tel-Aviv University and Sheba Medical Center (TEL HASHOMER, ISRAEL) |
| Leor, Jonathan | Tel-Aviv University (TEL HASHOMER, ISRAEL) |
| Lerman, Amir | Mayo Clinic (ROCHESTER, USA) |
| Losordo, Douglas | Caladrius Biosciences, Northwestern University, New York University (NEWYORK USA) |
| Lüscher, Thomas F | Zurich Heart House (ZURICH, SWITZERLAND) |
| Madeddu, Paolo | University of Bristol (BRISTOL, UK) |
| Madonna, Rosalinda | Institute of Cardiology, Center of Excellence on Aging, “G. D'Annnunzio” University - (CHIETI, ITALY) |
| Majka, Marcin | Jagiellonian University (KRAKOW, POLAND) |
| Marban, Eduardo | Cedars-Sinai Heart Institute (LOS ANGELES, USA) |
| Martin Rendon, Enca | University of Oxford (OXFORD, UK) |
| Martin, John F | University College (LONDON, UK) |
| Mathur, Anthony | Queen Mary and Barts University Hospitals (LONDON, UIK) |
| Menasche, Philippe | Hopital George Pompidou (PARIS, FRANCE) |
| Metra, Marco | Universita degli Studi di Brescia (BRESCIA, ITALY) |
| Montserrat, Nuria | Institute for Bioengineering of Catalonia (BARCELONA, SPAIN) |
| Mummery, Christine L | Leiden University Medical Center (LEIDEN, THE NETHERLANDS) |
| Musialek, Piotr | Jagiellonian University (KRAKOW, POLAND) |
| Nadal, Bernardo | King's College (LONDON, UK) |
| Navarese, Eliano | Heinrich-Heine-University, (DÜSSELDORF, GERMANY) |
| Pelacho, Beatriz | Clinica Universitaria de Navarra (PAMPLONA, SPAIN) |
| Penn, Marc S | Summa Cardiovascular Institute (OHIO, USA) |
| Perin, Emerson C | Texas Heart Institute (HOUSTON, USA) |
| Perrino, Cinzia | Federico II University, (NAPLES, ITALY) |
| Pinto, Fausto | Santa Maria University Hospital (LISBON, PORTUGAL) |
| Pompilio, Giulio | Centro Cardiologico Monzino (MILAN, ITALY) |
| Povsic, Thomas J | Duke Clinical Research Institute (DURHAM, USA) |
| Prosper, Felipe | Clinica Universitaria de Navarra (PAMPLONA, SPAIN) |
| Quyyumi, Arshed Ali | Emory University School of Medicine (ATLANTA, USA) |
| Roncalli, Jerome | Rangueil University Hospital (TOULOUSE, FRANCE) |
| Rosenthal, Nadia | Australian Regenerative Medicine Institute (MELBOURNE, AUSTRALIA) |
| San Roman, Alberto | Hospital Clínico Universitario (VALLADOLID, SPAIN) |
| Sanchez, Pedro L | Hosp Univ de Salamanca (SALAMANCA, SPAIN) |
| Sanz-Ruiz, Ricardo | Hospital Gregorio Marañon (MADRID, SPAIN) |
| Schaer, Gary | Rush University Medical Center (CHICAGO, USA) |
| Schatz, Richard A | Duke University (LA JOLLA, USA) |
| Schulz, Rainer | Justus-Liebig Giessen University of Giessen (GIEßEN, GERMANY) |
| Sherman, Warren | Cardiovascular Center, OLV Hospital (AALST, BELGIUM) |
| Simari, Robert D | University of Kansas Medical Center (KANSAS, USA) |
| Sluijter, Joost PG | University Medical Center Utrecht (UTRECTH,THE NETHERLANDS) |
| Steinhoff, Gustav | Universitat Rostock, (ROSTOCK, GERMANY) |
| Stewart, Duncan J | Ottawa Hospital Research Institute (OTTAWA, CANADA) |
| Stone, Gregg | Columbia University (NEWYORK, USA) |
| Sürder, Daniel | University of Zurich (ZURICH, SPAIN) |
| Sussman, Mark A | San Diego State University (SAN DIEGO, USA) |
| Taylor, Doris A | Texas Heart Institute (HOUSTON, USA) |
| Terzic, André | Mayo Clinic (ROCHESTER, USA) |
| Tompkins, Bryon A | University of Miami Miller School of Medicine (MIAMI, USA) |
| Traverse, Jay | Minneapolis Heart Institute Foundation (MINNEAPOLIS, USA) |
| Van Laake, Linda W | University Medical Center Utrecht (UTRECHT, THE NETHERLANDS) |
| Vrtovec, Bojan | University Medical Center Ljubljana (LJUBLJANA, SLOVENIA) |
| Willerson, James T | Texas Heart Institute (HOUSTON, USA) |
| Winkler, Johannes | Medical University of Vienna (VIENNA, AUSTRIA) |
| Wojakowski, Wojtek | Medical University of Silesia (KATOWICE, POLAND) |
| Wollert, Kai C | Kardiologie und Angiologie Medizinische Hochschule (HANNOVER, GERMANY) |
| Wu, Joseph C | Stanford University (STANFORD, USA) |
| Yang, Phillip | Stanford University, (STANFORD, CA, USA) |
| Yla-Herttuala, Seppo | University of Eastern Finland (KOUPIO, FINLAND) |
| Ytrehus, Kirsti | The Arctic University of Norway (TROMSØ, NORWAY) |
| Zamorano, José Luis | Hospital Ramón y Cajal, (MADRID, SPAIN) |
| Zeiher, Andreas | Goethe University (FRANKFURT, GERMANY) |
| Zuba-Surma, Ewa | Jagiellonian University (KRAKOW, POLAND) |
Cardiovascular regenerative medicine in perspective
This section summarizes existing knowledge pertinent to the mechanisms of cardiovascular regeneration, the attempts to apply that knowledge in the preclinical arena, and the main achievements and obstacles in translation to clinical practice.
Mechanisms of cardiovascular regenerative response
Cardiac regenerative response
Available evidence indicates that ongoing cell turnover in the adult human heart involves the death of cardiomyocytes and generation of new tissue.1,3 Furthermore, the myocardium, like other parenchymal organs, contains endogenous stem cells with the ability to proliferate and replace cardiomyocytes that die due to apoptosis or oncosis.4 Therefore, the paradigm that cardiomyocytes are terminally differentiated cells incapable of proliferation or renewal has shifted, and the heart is recognized to be a self-renewing organ.
However, the regenerative capacity of the adult human heart is limited and insufficient to overcome the massive loss of cardiomyocytes during acute damage or prolonged remodelling, in which cardiomyocyte death exceeds cardiomyocyte renewal. Such a limitation contrasts with the active cardiomyocyte turnover observed during embryogenesis and with the intense regenerative capacity of the adult heart in some species. In certain mammals, cardiac muscle cells remain mitotically active through the foetal and early perinatal periods, although shortly after birth, mitotic division of cardiomyocytes becomes undetectable, supporting the long-held belief that mature mammalian cardiomyocytes are terminally differentiated. In contrast, an adult zebrafish can fully regenerate its heart even after amputation of 20% of the ventricular mass.5 Mammalian neonates have the potential to regenerate injured hearts in much the same way as lower vertebrates.6 Although still a controversial concept, the mechanisms by which these processes occur form the basis of regenerative therapies and include various non-exclusive and probably interacting possibilities. These healing mechanisms are still in debate but include the following: (i) Endogenous cardiac progenitor cells (CPC)7 in distinctive architectural microenvironments known as 'cardiac stem cell niches', which have demonstrated their capacity to differentiate into several cardiac cell types under specific circumstances and constitute a source of new cardiac cells during cardiac regenerative processes; (ii) Dedifferentiation, proliferation, and reprograming of pre-existing adult cardiomyocytes to produce new cardiomyocytes.8,9 This process is the main component in the regeneration of damaged myocardium in zebrafish and mammalian neonates. The mechanisms underlying this process may shed light on how to revert the inhibition of the mitotic capability of human adult cardiomyocytes and enable in situ cell reprogramming10,11; and (iii) Activation of cells from the epicardium as a reminiscence of its involvement in cardiogenesis during embryonic life.12 Although this mechanism remains controversial, the contribution of epicardial cells to the whole process of heart regeneration, and particularly to the inflammatory response after injury, has been extensively documented and confirms the role of the epicardium in regeneration.13
Vascular regenerative response
Cardiovascular regenerative medicine is also a promising approach for refractory angina and peripheral artery disease (PAD).14 Dysfunction of the endothelial monolayer is the key initiation event of vascular diseases and is caused by a variety of stimuli including hypertension, diabetes, dyslipidaemia, and oxidative stress. After endothelial dysfunction and denudation, endogenous resident endothelial progenitor cells (EPC) tend to proliferate and replace the injured endothelium.15 However, this endogenous mechanism of regeneration is a relatively slow and inefficient process.16 Preclinical and clinical studies indicate that a variety of CRM therapies provide growth factors and cytokines for therapeutic angiogenesis, both in the heart and throughout the vascular system.17–20 The mechanisms by which those treatments yield positive results are being steadily unmasked.21
Cardiovascular regenerative products
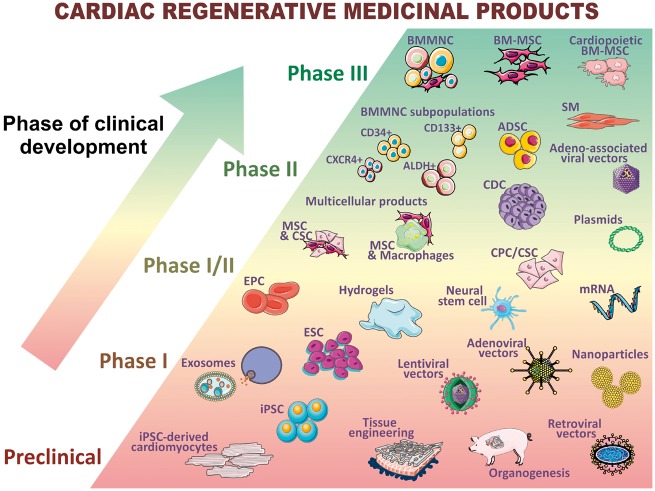
Products used for CRM can serve two complementary strategies according to the target processes (Figure 1): (i) exogenous regenerative responses, in which implanted products, cells, or tissues are expected to replace the structure of damaged or dysfunctional tissue; and (i) stimulation of endogenous regenerative responses, in which the products delivered are aimed at enhancing the efficiency of endogenous reparative mechanisms.
Figure 1.
Schematic representation of cardiovascular regenerative advanced therapy medicinal products according to the pre/clinical phase of development. ADSC, adipose tissue-derived stem cells; BMMNC, bone marrow mononuclear cells; BM-MSC, bone marrow-derived mesenchymal stem cells; CDC, cardiosphere-derived cells; CPC, cardiac progenitor cells; CSC, cardiac stem cells; EPC, endothelial progenitor cells; ESC, embryonic stem cells; iPSC, induced pluripotent stem cells; MSC, mesenchymal stem cells; SM, skeletal myoblasts.
Approaches based on ‘exogenous regenerative responses' include in vitro-differentiated cardiomyocytes, cardiovascular and EPC, and tissue-engineered cardiac and vascular patches with some degree of electromechanical functional maturation. In recent years, considerable advances have been made with this strategy,22–25 which has proven to be effective in primates.26,27 However, although the complex mechanisms underlying in vitro differentiation and maturation have limited its application in clinical practice, a first-in-man clinical trial is already assessing the feasibility and the safety of the transplantation of human embryonic stem cell-derived cardiovascular progenitors.28
Cardiovascular regenerative medicine products focused on the modulation, enhancement and activation of ‘endogenous regenerative responses' can be subdivided into three main groups, which could be eventually combined:
Cell implantation: several types of stem, progenitor and stromal cells have been investigated. These include both pluripotent stem cells, such as embryonic stem cells (ESC) and induced pluripotent stem cells (iPSC), and adult stem cells, including cells of cardiac origin [e.g. CPC and cardiosphere-derived cells (CDCs)] and cells from other sources [e.g. bone marrow-derived mononuclear stem cells (BMMNC), bone marrow-derived mesenchymal stem cells (BM-MSC), adipose tissue-derived mesenchymal stem cells (AT-MSCs), EPC and adventitial progenitor cells]. Excellent reviews summarizing their distinctive characteristics and outcomes have been published elsewhere.29,30
Injection of biological or synthetic factors with active functions in endogenous regenerative processes, which emulate the benefits of cell therapy without the need for living cells. Products in this category include extracellular vesicles (microvesicles, nanoparticles, and exosomes)31–33 isolated from in vitro cell secretomes and synthetic growth factors. All these products can be generated in clinical grade and injected using various delivery strategies.34,35
Genetic and epigenetic modifications that modulate the expression of genes and mRNA involved in the endogenous regenerative capacity of the heart and vessels. Increasing knowledge of the genetic pathways that govern cardiovascular generation and regeneration processes, which are active during the embryonic and neonatal stages, enables identification of factors that could be reactivated during adult life using genetic approaches.11,36 From the administration of mRNA produced in vitro to in vivo modifications of human DNA, the therapeutic regulation of gene expression and regeneration pathways may dramatically increase the possibilities of repairing the human cardiovascular system.37,38
Preclinical therapeutic application of basic science
Preclinical development depends on the use of appropriate animal models that accurately reflect human disease. In contrast with other areas, cardiovascular in vitro models provide limited information, which is restricted mainly to the assessment of drug toxicity and specific cellular and molecular aspects.39 Functional hearts and vessels are necessary to evaluate and optimize regenerative therapies.
Most of the mechanisms of CRM have been clarified thanks to preclinical research on small animals,29,30,40 although their practical and translational significance can be undermined by anatomical and functional deviations from human organs. In order to obtain a more comprehensive picture and better translational value, large animals such as pigs, sheep, and perhaps monkeys are needed.41–43 It is noteworthy that with large mammals, research has focused on acute myocardial infarction (AMI), chronic ischaemic cardiomyopathy (CIC), and, more sporadically, on dilated cardiomyopathy (DCM) and other forms of non-ischaemic heart disease (NIHD). The study of other cardiovascular diseases, such as Chagas disease,44,45 requires more complex animal models, in which the availability of transgenic and knock-out mice is proving particularly useful for assessing genetic factors and inducers of cardiovascular diseases.
Lessons learned from clinical research
Stem cells were first used in to prevent heart failure (HF) in clinical practice in 2002.46 Ever since, ischaemic heart disease (IHD) has been the most prominently evaluated disease, with more than 100 and 90 clinical trials carried out in the settings of AMI and chronic ischaemic HF, respectively. Table 1 provides a brief description of the products and results of individual trials. The literature has been further enriched with 48 systematic reviews and meta-analyses,47 which have consistently shown the feasibility and safety of the aforementioned regenerative strategies, as well as promising functional and clinical improvements in patients with AMI and chronic ischaemic left ventricular dysfunction, thus warranting appropriately powered and well-designed phase III clinical trials. In summary, the application of regenerative strategies in patients with IHD is feasible and safe. However, although promising, regenerative therapies have yet to demonstrate definitive clinical benefit over standard-of-care. Table 1 also details previous experiences in refractory angina, NIHD, PAD and stroke, for which the results are similar.
Table 1.
Summary of randomized clinical trials in cardiovascular diseases with regenerative products
| Disease (patients treated) | Regenerative product | Safety | Overall efficacya (surrogate endpoints) |
|---|---|---|---|
| Acute myocardial infarction (n = 2732) | BMMNC48–63 | Favourable | Inconsistent |
| BM-MSC64 | Favourable | Inconsistent | |
| Specific BM cells65–69 | Favourable | Inconsistent | |
| ADSC70 | Favourable | Inconsistent | |
| CDC71 | Favourable | Positive | |
| Growth factors72–77 | Favourable | Inconsistent | |
| Ischaemic heart failure (n = 2035) | SM78–81 | Favourableb | Inconsistent |
| BMMNC82–85 | Favourable | Inconsistent | |
| BM-MSC86–88 | Favourable | Positive | |
| Specific BM cells89–96 | Favourable | Positive | |
| CSC97 | Favourable | Positive | |
| Gene therapy37,98–101 | Favourable | Inconsistent | |
| Refractory angina (n = 353) | BMMNC102–106 | Favourable | Positive |
| Specific BM cells107–109 | Favourable | Positive | |
| ADSC110 | Favourable | Positive | |
| Non-ischaemic heart failure (n = 166) | BMMNC111,112 | Favourable | Inconsistent |
| Specific BM cells113,114 | Favourable | Inconsistent | |
| BM-MSC115 | Favourable | Inconsistent | |
| Peripheral artery disease (n = 1217) | BMMNC116 | Favourable | Positive |
| Specific BM cells117–119 | Favourable | Positive | |
| Gene therapy120–124 | Favourable | Inconsistent | |
| Stroke (n = 95) | Neural stem cells125 | Favourable | Inconsistent |
| BMMNC125 | Favourable | Inconsistent | |
| Specific BM cells125 | Favourable | Inconsistent |
ADSC, adipose tissue-derived stem cells; BMMNC, bone marrow mononuclear cells; BM-MSC, bone marrow-derived mesenchymal stem cells; CDC, cardiosphere-derived cells; CSC, cardiac stem cells; SM, skeletal myoblasts. ‘Specific BM cells’ means either modified or selected subpopulations of the bone marrow mononuclear fraction.
Note that all randomized clinical trials evaluated efficacy with surrogate endpoints.
Main safety concerns after skeletal myoblast transplantation in humans include an increased probability of arrhythmic events, so these cell type should be viewed with extreme caution in further clinical trials.
Regenerative therapies are currently being investigated in other cardiac conditions (e.g. valvular heart disease, rhythm disorders, and congenital myopathies), although clinical research is currently in very early stages.
The main obstacles that clinical CRM has encountered since its inception and that have hampered its large-scale adoption in daily clinical practice are depicted in Table 2 and include incomplete understanding of cardiovascular regenerative mechanisms, heterogeneity of study protocols and underestimation of aspects such as delivery methods, extracellular structure, dose, and patient selection. Furthermore, surrogate and clinical endpoints have been inconsistently used and are usually misinterpreted. Finally, multidisciplinary/multinational collaborations to unravel and resolve the limitations identified have been insufficient.
Table 2.
Main obstacles encountered by clinical CRM
| 1. The complex molecular, cellular and organ-based mechanisms that govern the cardiovascular reparative process as a whole have yet to be understood. Consequently, it has been difficult to design clinical trials. Since many cardiovascular diseases are syndromes, the future identification of specific molecular or cellular causes will help to increase the chances of success in clinical trials. |
| 2. The results of clinical trials are often contradictory because of non-homogeneous study protocols with inter-trial and inter-patient variability and the lack of standardization and scalability of investigational products. |
| 3. Focus on cell phenotype initially led to underestimation of the importance of delivery methods, thereby leading to low initial cell retention rates, poor survival in the host tissue, and subsequent loss of efficacy. |
| 4. Efforts have focused mainly on the loss of the myocardial parenchyma, thus leading to underestimation of the importance of other key aspects of a functional heart, such as the extracellular matrix or the appropriate cell patterning and electromechanical coupling required for a well-co-ordinated improvement in contractility. |
| 5. Key aspects of clinical trial design that have been systematically underestimated and not sufficiently investigated in phase I trials include optimal dosage (dose-escalation studies), timing of delivery (especially in the case of AMI), cell type and delivery method in the specific condition under study. |
| 6. Patient selection is paramount, given the critical influence that comorbidities, aging and medications have on the quality of source cells (if autologous) and on the response of host tissue to regenerative products. Predictors and scores that would enable appropriate identification of specific target populations that benefit most from CRM have not been described/validated. |
| 7. Surrogate imaging and hard clinical endpoints have been inconsistently used in clinical trials and are usually misinterpreted when translating clinical research for a specific product. In addition, surrogate endpoints need further standardization. |
| 8. Limited multidisciplinary/multinational collaborations to unravel and resolve identified limitations, which could increase our knowledge of regenerative therapies and facilitate definitive large-scale preclinical and clinical trials. |
Challenges of cardiovascular regenerative medicine
The following section summarizes the outlook for the next decade. Specifically, the main challenges and priorities of each area involved in the clinical application of CRM are identified.
Priorities in cardiovascular regenerative medicine: diseases and disease stages
The ultimate goal of CRM is the prevention and treatment of cardiovascular failure and its consequences, including the protection and repair of tissue necrosis caused by ongoing myocardial ischaemia and reversal of chronic ischaemic dysfunction at all stages of disease progression. In addition, vascular damage in pulmonary or systemic circulations is a key target in CRM.
The application of regenerative strategies in the setting of AMI takes advantage of preserved extracellular tissue architecture, although it is subject to the inflammatory hostility of the milieu in the context of excellent initial and long-term results of standard-of-care approaches (e.g. reperfusion strategies). Therefore, given the results of research already carried out in this setting, new initiatives should focus on patients at risk of developing HF and should depend on findings from ongoing large-scale clinical trials and from translational and phase I/II clinical studies analysing new regenerative products and mechanistic aspects, such as timing, dose, therapeutic combinations, and single vs. sequential delivery.
In patients with chronic ischaemic or non-ischaemic HF, the histopathological, and functional substrate is crucial and underlies the choice, design, and methodology of regenerative applications. In this setting, coronary tree status, myocardial perfusion and viability, together with the extent and characteristics of maladaptive myocardial remodelling and influence of chronic inflammatory processes, will help to choose between therapies aimed at stimulating endogenous repair and/or at replacing a functional scar with healthy tissue.
Priorities and methods for basic research
Enhancement of endogenous cardiac regeneration is limited by the lack of knowledge regarding the mechanisms of modulation of the regeneration capacity in the adult mammalian heart. Accordingly, basic research focuses with the potential to revolutionize clinical practice are summarized in Table 3.
Table 3.
Recommendations for basic research
| Strategies for the enhancement of endogenous regenerative responses |
| 1. Better understanding of the underlying biology that leads to significant loss of regeneration capacity in the adult mammalian cardiovascular system. |
| 2. Breakdown of the regeneration process in clinically relevant models, from the niche of adult stem cells to active dedifferentiation, proliferation, and/or transdifferentiation. |
| 3. Identification of molecular mechanisms that control the post-infarction inflammatory response and the remodelling process in order to redirect healing towards regeneration instead of scar formation. |
| 4. Identification of endogenous regeneration triggers that would enable the production of biological or synthetic CRM products, ideally for a prolonged and efficient outcome. |
| 5. Evaluation of potential differences between males and females in terms of their ability to generate a regenerative response. |
| Strategies for cardiovascular tissue replacement |
| 1. Identification of the most appropriate in vitro—and eventually in vivo—maturation processes to mimic adult cardiac tissue (e.g. in terms of cell structure and electromechanical function). |
| 2. Evaluation of disruptive organogenesis strategies (e.g. chimeric approaches to produce human organs in pigs).126 |
Priorities and methods for translational research: animal models
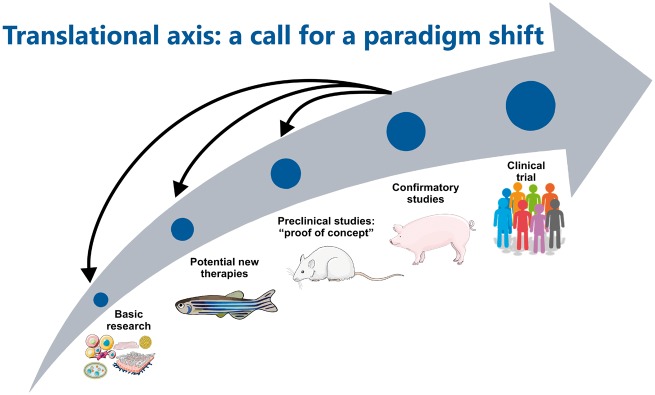
The three stages in the development of new therapeutic products comprise discovery and development of leading products, exploratory studies, and confirmatory studies (Figure 2). The first two stages usually involve small animal models (e.g. zebrafish and rodents), which enable affordable and rapid experiments. Confirmatory studies are typically performed in large mammals, which are more representative of human disease, in order to assess the risks of a new therapy and to predict safety, feasibility, and efficacy. Although studies in large animal models are expensive, complex, and technically demanding, they offer the advantage of being conducted in settings that more closely mimic clinical practice. Therefore, large animal studies are essential if we are to justify the risks and costs of clinical trials and to improve the clinical outcomes of regenerative therapies. However, publication bias is a major concern in preclinical trials. As is the case in other medical fields (e.g. cancer studies), the lack of interest in negative or neutral findings may translate in a disproportional body of positive published results. In order to overcome this overestimation, one suggestion would be that preclinical research with large mammals follows standards used in clinical trials (see Table 4).127
Figure 2.
Flow-chart of translational research.
Table 4.
Recommendations for translational research with large animal models
| 1. Prospective online and public registration of preclinical trials, including the description of the study and research model, primary and secondary outcomes, number of animals, and duration of follow-up. |
| 2. Obligatory publication of results required for grant fund release (e.g. funding depends on the dissemination of results, independently of whether they are positive or negative). Use of the ARRIVE guidelines for the reporting of preclinical study results.128 |
| 3. Prioritization of multicentre studies and development of collaborative consortia consisting of independent core laboratories specialized in large animal models (e.g. the CAESAR consortium).129 |
| 4. Blinded and randomized studies in the confirmatory stage. |
| 5. Establishment, optimization, and sharing of standard animal models and protocols. Funding agencies should provide guidelines for the generation of animal models, which should include the definition of a standard model for AMI and CIC. |
| 6. Standardization of software protocols for the analysis and quantification of the main outcomes by means of open-source solutions and platforms for data sharing (e.g. scar size, left ventricular ejection fraction). |
| 7. Prioritization of animal models that include comorbidities (e.g. old-animal models), cardiovascular medication use and clinically relevant scenarios (e.g. surrogate cell products or xenoregulated animals that do not require immunosuppression). |
| 8. Mandatory evaluation of gender differences. |
Priorities and methods for tissue engineering and biomaterials
Despite the regenerative capacity of mammalian hearts and vessels, experience with highly damaged tissues indicates that, at a certain point of damage (e.g. homogenous fibrotic scars and highly calcified valves or arteries), endogenous recovery is impossible. In such cases, substitution of the tissue may be the only possible strategy. Given the small number of transplant donors, tissue engineering has emerged as an attractive approach. However, in order to become clinically useful, major challenges have to be resolved (Table 5).
Table 5.
Main challenges of cardiovascular tissue engineering
| 1. Enormous number of cells needed to build a heart (e.g. around 10 billion for a whole human heart)130 |
| 2. Anatomically realistic scaffolds (e.g. natural or synthetic biomaterials with vasculature and anisotropic structures). |
| 3. Differentiation of cells into several cardiac lineages (e.g. endothelial cells, fibroblasts, cardiomyocytes) |
| 4. Mature electrophysiological properties (e.g. action potential duration and conduction velocities, avoidance of autoexcitability) to ensure co-ordinated contraction without arrhythmias.131 |
| 5. Mature mechanical function (e.g. sarcomere constructs, troponin orientation) to achieve efficient contraction. |
| 6. Bioreactors that allow maturation under sterile conditions for long culture periods. |
| 7. Development of easy-to-use and safe, minimally-invasive, delivery technologies. |
The aforementioned challenges in the generation of clinically useful cardiac muscle tissue are not present in other cardiovascular structures, for which the tissue engineering approach is already producing clinically viable and useful products. Such is the case of cardiac valves and large vessels.132–135 Nevertheless, technical improvements are required in order to extend their applicability to a larger number of patients. These improvements include standardized production units, the identification of the most appropriate materials, control of long-term degradation and integration in the body, and the development of minimally invasive delivery devices.136
In addition to the clinical usefulness of cardiovascular tissue engineering solutions, the possibility of producing personalized monolayer cultures and three-dimensional human engineered cardiac tissues heralds a new era for the in vitro identification of pathophysiological mechanisms and for the development of tailored novel treatments (e.g. by using human cardiomyocytes obtained by directed differentiation of iPSC derived from patients with cardiomyopathy).137,138
Priorities and methods for production, delivery, tracking, and assessment
Cardiovascular regenerative medicine products have special characteristics that differentiate them from classic pharmacological treatments in terms of production, delivery, tracking, and assessment (Figure 3). The manufacturing of these advanced therapy medicinal products (ATMP) includes multiple step from the acquisition of biological samples to the delivery of a personalized product for each patient. Given the heterogeneity present in the generation of most biological CRM products, the process of manufacturing and the delivery technology need to be considered as part of the CRM product itself. The functionality of a cell-based product is influenced by multiple factors, including the initial source, harvesting and isolation techniques, and manufacturing. Standardization of these procedures and methods is especially important, as lack of uniformity in cell manufacturing may influence clinical outcome.139 Moreover, standardization permits direct comparisons between trials and indirect comparisons through meta-analyses. Several reviews have already provided guidance for the technological progress and challenges towards manufacturing of CRM products based on the principles of Good Manufacturing Practice.140–142
Figure 3.
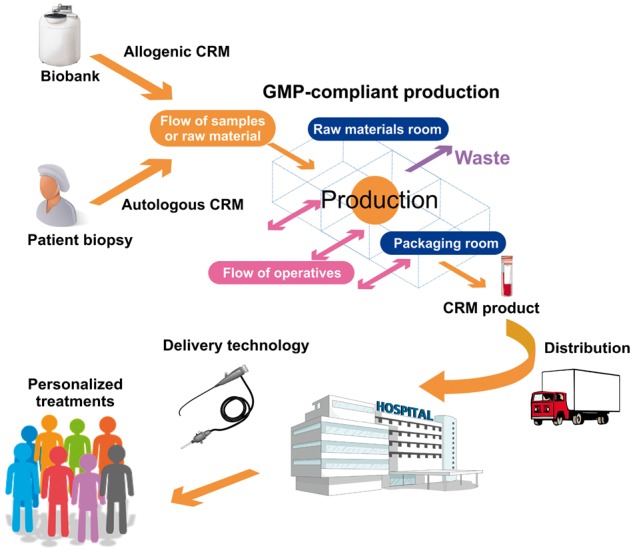
Supply chain of cardiac regenerative advanced therapy medicinal products.
The main objective of delivery technologies is to achieve the optimal dosage of biological material needed to provide benefits in the region of interest of the host tissue. Although all available modalities of regenerative product delivery display—to varying degrees—the four desired characteristics (safety, ease of use, clinical utility, and low cost), after 20 years of research we can conclude the following:
Surgical transepicardial delivery has been relegated to patients with a formal indication for open-chest surgery. However, minimally invasive approaches, such as lateral minithoracotomy, video-assisted thoracoscopy and robotic surgery, are currently being investigated.
Percutaneous catheter-based delivery has been the most extensively used modality for cardiac diseases. Intracoronary infusion of regenerative products has been the mainstay in the setting of acute coronary syndromes, whereas more sophisticated catheters—with or without navigation platforms—for endomyocardial delivery have been specifically used in HF and refractory angina.
Intravenous infusion of products was discontinued owing to low selective engraftment rates, subsequent to early trapping in remote organs (primarily the lungs), although it may play a role in the delivery of products with high tropism for the target tissue after AMI (e.g. viral vectors).
Tissue engineering products require more specific transplantation technologies. These products may prove easier for injection of biomaterials, but will require highly sophisticated systems in the case of matrixes or patches if they are to be minimally invasive or even administered percutaneously.
In the case of PAD and stroke, intra-arterial and intramuscular injections have been used extensively, and no relevant advances in delivery technologies are anticipated in the short-term.
Few preclinical studies have compared delivery modalities.143–145 It seems that the intracoronary and endomyocardial approaches are the most efficient, depending on the phase of myocardial ischaemia (acute vs. chronic).146 However, evidence is scarce with humans, and the efficiency of product delivery is a complex, multifactorial variable that is influenced by several factors, including cell type, timing of delivery, device design, and cell dose. Moreover, the implications of these experimental findings for clinical practice are not completely clear, and it is now well known that retention rates may not determine the effect of a given product.147–149
Our recommendations are shown in Table 6.
Table 6.
Recommendations for production, delivery, navigation, tracking, and assessment
| 1. Identification of optimal delivery technologies for each novel or ‘conventional’ regenerative product (e.g. viral vectors, stem cells, growth factors and molecules). Other variables, such as timing, dose, microenvironment, clinical scenario, and location, need to be considered when designing new delivery technologies. |
| 2. Development of minimally invasive methodologies, ideally percutaneous approaches, for tissue engineering solutions. |
| 3. Optimization of delivery modalities to improve accuracy by means of fusion imaging tools. |
| 4. New imaging and automated software to guide and improve CRM product delivery and retention: real-time, non-invasive imaging and/or integrating computed tomography, magnetic resonance and ultrasound into the catheter navigation process. |
| 5. New imaging and automated software for in vivo tracking of CRM products in humans. |
Identification of regenerative products ready for clinical trials: recommendations regarding clinical investigation tracks
‘First-generation' cell types include a series of heterogeneous adult stem cell populations that were first used (unmodified) in CRM at the beginning of this century (e.g. unfractionated BMMNC and selected subpopulations thereof, CPC, EPC, SM, MSC, and ADSC).29 These types of cells are believed to induce myocardial repair through the secretion of cytokines and growth factors that activate innate regeneration pathways (paracrine activity). Most have already been investigated in depth in clinical practice (see ‘Lessons learned from clinical research’ section) and have passed through phase I and II studies with consistent and solid safety profiles. Furthermore, and although several issues concerning their regenerative capacity remain unresolved (e.g. mechanisms of action, dose, and timing), in some cases, they have already been considered as the most suitable types for investigation in phase III clinical trials.
In contrast, ‘second-generation' cells include purified cardiac cell subpopulations (CDCs and CSC), ‘potency-enhanced' cells with genetic or pharmacological modifications (e.g. ‘cardiopoietic' BM-MSC), cells of allogeneic origin (MSC and CSC), and novel pluripotent sources (iPSC and ESC). Despite their robust paracrine activity, these cell types are also—theoretically—able to replace the damaged myocardium with the formation of new cardiomyocytes, smooth muscle cells, and endothelial cells to a greater or lesser extent. Although a first experiment with ESC-derived CPCs in chronic HF has been initiated in humans,28 we can consider iPSC and ESC to be at the preclinical stage because of safety concerns (e.g. uncontrolled proliferation, transfection-related mutagenesis in iPSC).136 The remaining cell types have also been considered to be ready for phase III experimentation. However, additional safety studies (e.g. immunogenicity and tumorigenicity) are required with some allogeneic sources before genuine phase II clinical trials can be considered.
The field of ‘cell-free' products has evolved rapidly from the first unsuccessful experiences with growth factors (e.g. granulocyte colony-stimulating factor) used as soluble injectates to more sophisticated products, such as episomes, microRNA (mi-RNA), and exosomes, either alone or embedded in hydrogels or encapsulated in nanoparticles. Although these new approaches that mimic the secretome of donor cells could soon be used in clinical practice, further investigations on their characterization, bioavailability (dose, timing), organ distribution (delivery), and efficiency (outcomes) are warranted.
With regards to gene therapy, after 14 years of clinical research, angiogenic factors, calcium-handling proteins, and homing factors have been investigated in phase I/II trials. Given the limited results of gene therapy in clinical trials compared with preclinical models, several obstacles need to be overcome before clinical application of gene therapy can be considered realistic. These obstacles include, but are not limited, to: (i) technical challenges regarding viral and non-viral constructs (e.g. tissue-specific promoters and chemical ligands); (ii) grounded choice of therapeutic targets and clinical conditions; (iii) safety, transfection efficacy, and production costs; and (iv) optimization of delivery systems for precise administration and appropriate bioavailability with minimal off-target effects. Finally, the field of tissue engineering is one of the most promising in CRM and is currently initiating phase I first-in-man experiences.150
Clinical research tracks in CRM must be based on an evidence-based translational rationale. When ready for clinical testing, any regenerative product should follow the traditional four phases of clinical research (see also Table 8).29,151 Of note, some currently researched CRM products do not comply with these principles.
Table 8.
Requirements for each phase of clinical research
| Preclinical, Phase I | Phase II | Phase III | |
|---|---|---|---|
| Product regulatory requirements |
|
|
Performed after preliminary evidence suggesting effectiveness of particular regenerative product |
| Objective |
|
Safety/surrogate endpoints | Safety/therapeutic benefit/improved survival |
| Patients restriction/criteria | Identify target group (safety analysis) | Identify potential responders and non-responders | Include only responders |
| Sample size | Usually 20 per cohort | From a few dozen to a few hundred | Several hundred or more |
| Design | Randomized, open label or placebo/sham | Randomized, double-blind, placebo or sham controlled | Randomized, double-blind, placebo or sham controlled |
| Endpoints (feasibility/product and procedure related) | Procedural safety, biological activity of the regenerative product | Safety/feasibility of the procedure, adequate number of cells/dose response | Long-term, substantial evidence of previously observed feasibility/safety |
| Safety endpoints | Patient tolerance, abnormal cell growth, mutagenesis, tumorigenicity | Patient tolerance, tissue injury, clinical major adverse cardiac events, arrhythmias | Clinically relevant endpoints: death, adverse clinical events |
| Efficacy endpoints | Detect surrogate endpoints that are sufficiently sensitive to track the therapeutic benefit |
|
|
Table 7 summarizes our recommendations on the identification of regenerative products ready for clinical trials.
Table 7.
Identification of regenerative products ready for clinical trials
| 1. ‘First-generation’ and ‘second-generation’ stem cells (except for iPSC and ESC), including those used in allogeneic transplants, are ready for phase III clinical trials. However, issues such as best tolerated doses, benefits of repetitive administration, optimal timing, and most efficient delivery modality still need further research. |
| 2. Emphasis should be placed on comparison between products, doses and delivery strategies. |
| 3. Cell-based and other regenerative products, especially when evaluated in multicentre/international trials, should be standardized. Standardization includes quality assessments of the final product before release (viability, surface markers, potency, stability, and sterility tests). |
| 4. Safety and efficacy issues in gene therapy should be solved before moving forward to new phase I or more phase II trials. Novel ‘cell-free’ products and tissue engineering approaches must progressively enter the clinical stage. |
| 5. Efforts should be made to include biomarkers, new imaging/tracking and delivery techniques in phase I trials with the aim of unraveling the complex mechanisms of action of regenerative products. |
Priorities and proposals regarding clinical trial design
Before the promise of biologic-based interventions can be translated into clinical benefits, appropriate endpoints must be selected to facilitate the regulatory path that regenerative interventions are subject to. Regulatory bodies in the US and Europe stipulate generic and disease-specific requirements and rigorous criteria for good clinical practice and clinical research. These requirements are summarized in Table 8 (reprinted from152 with permission).
Interestingly, some of the aforementioned variables have been systematically ignored or not investigated in depth in phase I/II trials. The shortcomings of previous approaches include the following:
Safety and efficacy endpoints have been used consistently, although not in a standardized/uniform manner between trials, and sometimes not correctly according to the corresponding clinical research phase. No novel endpoints that could allow us to increase our knowledge of CRM (‘mechanistic' endpoints) have been put forward.
Surrogate endpoints have been assessed in several trials with very different imaging modalities and sometimes with high inter- and intra-observer variability (e.g. echocardiography).
Traditionally, phase II clinical trials have been misused to confirm efficacy, which is the final aim of phase III studies. Ambitious efficacy results have been frequently incorporated into phase II trials with the purpose of shortcutting development expenses and obtaining scientific recognition, frequently resulting in global scientific disappointment.153 Phase II trials should be carried out with many primary ‘surrogate' endpoints (such as functional and structural measures, biomarkers, quality of life, and functional capacity) to test a range of efficacy domains and to broadly survey the possible benefits of the study product, with little regard for ‘P' values. On the contrary, hard clinical endpoints (such as all-cause mortality or cause-specific mortality) that are applicable in daily clinical practice should be tested in well-designed phase III trials, although other endpoints of cardiovascular improvement/impairment may be included.152
Patient-related modifiers: Age, gender, and comorbidities may alter the reparative proficiency of cardiac regenerative products. For instance, patients with cardiovascular disease rarely harbour cells with an acceptable regenerative capacity, an issue that we will be able to assess through the development of biomarkers and potency assays. Furthermore, clinical trials should include only patients under optimal medical treatments, given that concomitant medications may also modify the final effect of cell/gene therapy, either by affecting the quality of source cells or the response of the host tissue. Some scores predict the impact of these variables on the outcome of regenerative therapies,154 although their use has been marginal to date.
Patient selection: Inclusion and exclusion criteria should focus on specific subpopulations with poor prognosis that could benefit the most from CRM and should clearly identify target patient populations. It is increasingly recognized that standard-of-care medications and interventions lead to a high rate of spontaneous recovery in some settings (e.g. post-AMI), thus underpowering the potential beneficial effects of CRM. On the other hand, in many cases regenerative strategies have been applied to ‘low-risk' patients, thus also precluding the observation of positive beneficial results. Finally, level of treatment and disease severity must be well balanced between treatment and control groups.
Sample size has frequently been calculated by imitating the approach adopted in previous trials or based on preclinical models that do not predict human responses and on weak surrogate-based results. These calculations must be drawn only from well-founded and reliable data, once the primary endpoint and the trial objective have been identified and the magnitude of difference for detection and acceptability of errors has been specified. If data are not available, the most reliable resources must be used.
Cell dosing: As mentioned above, in most cases, the number of cells to be delivered in a clinical trial is empirically determined (e.g. subject to manufacturing capacities) or simply copied from previous trials; genuine dose-escalating studies are lacking. A feasible, safe, and eventually efficient dose of the regenerative product should be anticipated from the results of preclinical research and tested in phase I trials.
Specific studies to determine the ideal timing for cell delivery (mainly in the acute phase) are lacking. Furthermore, the effect of repetitive injections of CRM products has not been sufficiently assessed.
Other aspects that should be borne in mind when designing future clinical trials include ethics issues (e.g. the choice of control group, which is mandatory in phase II/III trials, and the correct assessment of the risk/benefit ratio), the eventual role of conflicts of interest (mainly commercial interests), and the major impact of CRM results on the scientific community and, in a broader sense, on decision makers and the public.
Table 9 shows our recommendations on translational clinical research with ATMP.
Table 9.
Recommendations for advanced therapy medicinal product-based translational clinical research
| 1. Clinical research planning should include ‘proof-of-principle’ studies, bio-distribution studies, and dose-escalation studies before safety and efficacy can be validated. |
| 2. Confirmatory ‘proof-of-efficacy’ trials should comply with disease-specific guidelines and target specific, well-defined patient subpopulations. |
| 3. Traditional safety and efficacy endpoints (clinical/surrogate) will be used in the future when appropriate. However, new mechanistic endpoints to corroborate unanswered hypotheses (e.g. on mechanisms of action) should be incorporated after proper validation in the preclinical field and standardized according to regulatory recommendations. In the event that surrogate endpoints are anticipated, the most reproducible techniques must be used (MRI, PET), and core laboratories should be established for centralized analysis. |
| 4. The timing and route of delivery must also be re-considered from the early phases, taking into account the underlying disease, previous hard preclinical observations, and plausible assumptions. |
| 5. Patient selection is crucial. Confounders such as age, gender, comorbidities, disease vulnerability and severity, and concomitant medications should always be taken into consideration when designing a new clinical trial (using predictive scores of outcomes, if possible). |
| 6. Sample size calculations should be rigorous, and general requirements and safety/efficacy profiles for phases I, II, and III should be strictly adhered to. Specifically, phase II clinical trials must be conducted in order to generate hypotheses and foundational (although not significant) evidence for the appropriate design of meaningful confirmatory phase III clinical trials. |
| 7. Adequate inclusion of control/placebo patients should be ensured and strict blinding methods should be followed. The risk/benefit ratio should be defined, and the interference of eventual commercial interests should be avoided. |
| 8. The costs of clinical evaluation phases have been frequently underestimated, thus forcing the interruption of ongoing trials. Strong support and collaboration between academia and industry and an appropriated economic plan are mandatory if we are to provide patients with the most efficient treatments. |
Priorities and proposals regarding regulatory hurdles
Biological products are subject to significantly different regulatory requirements throughout the world. In the United States, regulation of cellular and gene therapy products falls under the auspices of the Center for Biologics Evaluation and Research (CBER). In the European Union (EU), cellular and gene therapies are regulated by the European Medicines Agency (EMA) and undergo evaluation by the Committee of ATMP. In addition, each European country has its own agencies and procedures. In Japan, regulation is the responsibility of the Pharmaceuticals and Medical Devices Agency (PMDA), which recently prioritized biologics, thus enabling the approval of stem cell therapies with only basic demonstrations of safety and trends toward efficacy (phase II clinical trials). Similarly, other countries are developing their own regulations. Each agency periodically publishes its own guidelines, which are frequently subject to discrepancies in terms of objectives and methods. Meanwhile, alternative strategies are often used by small clinics and unscrupulous people to minimize regulatory requirements and obtain profits from patients desperate for ‘magic’ options.155
To address the needs of patients, researchers, sponsors, and regulatory agencies, we propose the recommendations detailed in Table 10.
Table 10.
Recommendations regarding regulatory hurdles
| 1. Additional workshops should be organized and sponsored to establish excellence networks comprising patient advocacy groups, researchers, clinical trialists, industry representatives, specialists in clinical-grade production of biologics and representatives of regulatory agencies from around the world. |
| 2. Development of international mechanisms for the oversight of regenerative treatments. To support regulatory mechanisms that would offer patients access to CRM therapies that have proven to be safe and efficient. |
| 3. The standardization of biological therapies presents specific characteristics that cannot be evaluated following the procedures developed for the pharmaceutical industry. Specific tracks need to be considered for measuring the safety, purity, potency, and efficacy of products. |
| 4. Special care and protection needs to be offered to patients with critical diseases who may be subject to hype rather than true hope. |
Priorities and proposals regarding strategies for public and private funding
The funding challenges facing the CRM community are considerable, and the solutions are demanding. Regenerative medicine raises general questions about the appropriate allocation of government and private resources, thus casting doubt on the relative priority of the translational approach over health care in funding decisions. The research portfolios of pharmaceutical companies and non-profit organizations also reveal an array of promising lines, although neither the public sector nor the private sector can support each and every promising research project. In summary, no single strategy will likely prove itself sufficient to meet the patient’s needs. In order to guarantee quality (both in healthcare and research) and private-sector financial support in the CRM field, investors and governments should be prepared to collaboratively support a range of strategies aimed at increasing funding, improving operational efficiency (both administrative and academic) and generating additional revenues through royalties, patent registration, and other models. Only countries and investors with an efficient strategy for market positioning and promotion of translational research in the healthcare system will obtain profits from the revolution of CRM and offer improvements to their citizens in terms of quality of life.
Vision and global perspectives
The TACTICS consortium is the first worldwide cooperative research network in the field of CRM. In this consensus document, the Writing Group of the TACTICS Task Force presents a critical summary of the state of the art in CRM, covering basic and translational research, clinical practice, regulatory pathways, and funding strategies. Our end objectives are to describe the priorities and challenges in the field for the next decade and to provide evidence-based recommendations to guide the future application of regenerative products in the fight against cardiovascular failure. The most relevant challenges are summarized in Table 11.
Table 11.
Global aims of TACTICS
| 1. A comprehensive increase in our knowledge of the complex molecular, cellular, and tissue mechanisms that govern regenerative homeostasis and the cardiovascular repair process. |
| 2. Standardization of small and large animal models for cardiovascular research so that they can reach the standards required for clinical research. |
| 3. Collaborative performance of large-scale and optimally designed phase III multicentre clinical trials to demonstrate the clinical efficacy of regenerative therapies and to advance the standard of care in human cardiovascular medicine. |
| 4. Transnational standardization of regulatory requirements to ensure adoption of approved therapies. |
| 5. Communication and demonstration of best practices of all those working in the field of CRM to the scientific community, decision makers and the public. Mitigating a main risk challenging the field—the lack of credibility—requires the organization of robust evidence-based investigational team tracks with the scientific support of a large and committed multidisciplinary/multinational consortium. |
In conclusion, the opportunity to optimize the regenerative medicine armamentarium and to make real progress in the regeneration of human cardiovascular tissue is through worldwide multidisciplinary cooperation. By pooling the efforts of leading expert groups, we will collectively be able to develop effective treatments that will improve the prognosis of patients with a wide range of heart and vascular diseases.
Acknowledgements
The authors would like to thank Ana Fernández-Baza for her outstanding support and invaluable unceasing work during the conception, organization, and development of the TACTICS Alliance.
Funding
Spanish Ministry of Economy through the Instituto de Salud Carlos III-FEDER (Fondo Europeo de Desarrollo Regional) (PLE2009-0152, IJCI-2014-22178, PI13-01882, SAF2016-76819-R, CPII15/00017), the Red de Investigación Cardiovacular (RIC. RD12.0042.0001) and the Red of Terapia Celular (TERCEL. RD12.0019.0021, RD16/00110018 and CB16/11/0041); FEDER ‘Una Manera de Hacer Europa’; and ‘CERCA Programme/Generalitat de Catalunya’ Spain (in part); BAMI (7th FP); SCIENCE (Horizon 2020), Pegasus, Circulate (STRATEGMED by Polish Natinal Centre for Research and Development), statutory funds Medical University of Silesia; NIH and the Mayo Foundation. Netherlands CardioVascular Research Initiative (CVON): The Dutch Heart Foundation, Dutch Federation of University Medical Centers, the Netherlands Organization for Health Research and Development and the Royal Netherlands Academy of Science. Academy of Finland. National Institutes of Health (R01HL084275, R01HL107110, UM1HL113460, and R01HL110737); Starr and Soffer Family Foundations; HLA&MEDECINE.NIH (R01HL067245, R37HL091102, R01HL105759, R01HL113647, R01HL117163, P01HL085577, R01HL122525, P01 HL-78825, and 1 UM1 HL-113530 (CCTRN)) (in part). A.T. reports research grants, administered by Mayo Clinic, from Marriott Foundation, Michael S. and Mary Sue Shannon Family, Russ and Kathy VanCleve Foundation, Leducq Foundation, Florida Heart Research Institute, Celyad, and National Institutes of Health. Ministerio de Educaciœn Ciencia (SAF2014-59892), Fundaciœ MARATÓ de TV3 (201502, 201516), Red de Terapia Celular - TerCel (RD16/0011/0006) and CIBER Cardiovascular (CB16/11/00403) as part of the Plan Nacional de I+D+I, and AdvanceCat 2014-2020 to A.B.G.
Conflicts of interest: K.C.W. has applied for a patent describing the therapeutic potential of bone marrow cell-derived growth factors in cardiovascular disease (PCT/EP2014/050788). B.G. is consultant in Celyad Inc. T.J.P. has received research funding to his institution from Baxter Healthcare and Janssen Pharmaceuticals, and minimal consulting fees from Pluristem Inc., Capricor, and Recardio Inc. J.B. is a member of an institution which has been a co-founder of Cardio3Biosciences, now Celyad. J.H. reports having a patent for cardiac cell-based therapy and holds equity in Vestion Inc. and maintains a professional relationship with Vestion Inc. as a consultant and member of the Board of Directors and Scientific Advisory Board. Vestion Inc. did not play a role in the design and conduct of the study. He holds a relationship with Longeveron LLC, Heart Genomics and Biscayne Pharma. M.A.S. is Chief Science Officer and co-founder of CardioCreate, Inc. The rest of the authors declare no conflict of interest.
Contributor Information
Authors/Task Force Members. Chairpersons::
Francisco Fernández-Avilés and Andre Terzic
Basic Research Subcommittee::
Lina Badimon, Kathleen Broughton, Darcy L. DiFede, Stefanie Dimmeler, Rosalinda Madonna, Marc S. Penn, Mark A. Sussman, Joost P.G. Sluijter, and Kai C. Wollert
Translational Research Subcommittee::
Wayne Balkan, Roberto Bolli, Steven Chamuleau, Dominique Charron, María Eugenia Fernández-Santos, Valentin Fuster, Georg Goliasch, Mariann Gyöngyösi, Joshua M. Hare, Thomas F. Lüscher, Bryon A. Tompkins, and Johannes Winkler
Challenges of Cardiovascular Regenerative Medicine Subcommittee::
Antoni Bayés-Genís, Timothy D. Henry, and Doris A. Taylor
Tissue Engineering Subcommittee::
Andreu M. Climent, Amir Lerman, Beatriz Pelacho, and Felipe Prosper
Delivery, Navigation, Tracking and Assessment Subcommittee::
Ricardo Sanz-Ruiz, Emerson C. Perin, and Giulio Pompilio
Clinical Trials Subcommittee::
Bernard Gersh, Jozef Bartunek, Eric Duckers, Péter Ferdinandy, Stefan Janssens, Douglas W. Losordo, Pedro L. Sánchez, Warren Sherman, Wojtek Wojakowski, Andreas Zeiher, Jens Kastrup, Jerome Roncalli, and Anthony Mathur
Regulatory and funding strategies subcommittee::
Filippo Crea, Domenico D´Amario, Thomas J. Povsic, Jay Traverse, and Seppo Ylä-Herttuala
References
- 1. Bergmann O, Zdunek S, Felker A, Salehpour M, Alkass K, Bernard S, Sjostrom SL, Szewczykowska M, Jackowska T, Dos Remedios C, Malm T, Andrä M, Jashari R, Nyengaard JR, Possnert G, Jovinge S, Druid H, Frisén J.. Dynamics of cell generation and turnover in the human heart. Cell 2015;161:1566–1575. [DOI] [PubMed] [Google Scholar]
- 2. Sanz-Ruiz R, Bolli R, Gersh BJ, Janssens S, Menasché P, Perin EC, Taylor DA, Terzic A, Willerson F, Fernández-Avilés F.. The TACTICS intitiative: time for a global alliance on cardiovascular regenerative medicine. Eur Heart J 2016;37:2208–2211.27444374 [Google Scholar]
- 3. Aguirre A, Sancho-Martinez I, Izpisua Belmonte JC.. Reprogramming toward heart regeneration: stem cells and beyond. Cell Stem Cell 2013;12:275–284. [DOI] [PubMed] [Google Scholar]
- 4. Beltrami AP, Urbanek K, Kajstura J, Yan SM, Finato N, Bussani R, Nadal-Ginard B, Silvestri F, Leri A, Beltrami CA, Anversa P.. Evidence that human cardiac myocytes divide after myocardial infarction. N Engl J Med 2001;344:1750–1757. [DOI] [PubMed] [Google Scholar]
- 5. Kikuchi K, Poss KD.. Cardiac regenerative capacity and mechanisms. Annu Rev Cell Dev Biol 2012;28:719–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Porrello ER, Mahmoud AI, Simpson E, Hill JA, Richardson JA, Olson EN, Sadek HA.. Transient regenerative potential of the neonatal mouse heart. Science 2011;331:1078–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Beltrami AP, Barlucchi L, Torella D, Baker M, Limana F, Chimenti S, Kasahara H, Rota M, Musso E, Urbanek K, Leri A, Kajstura J, Nadal-Ginard B, Anversa P.. Adult cardiac stem cells are multipotent and support myocardial regeneration. Cell 2003;114:763–776. [DOI] [PubMed] [Google Scholar]
- 8. Porrello ER, Olson EN.. A neonatal blueprint for cardiac regeneration. Stem Cell Res 2014;13:556–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jopling C, Boue S, Izpisua Belmonte JC.. Dedifferentiation, transdifferentiation and reprogramming: three routes to regeneration. Nat Rev Mol Cell Biol 2011;12:79–89. [DOI] [PubMed] [Google Scholar]
- 10. Kovacic JC, Fuster V.. Cell therapy for patients with acute myocardial infarction: ACCRUEd evidence to date. Circ Res 2015;116:1287–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sadahiro T, Yamanaka S, Ieda M.. Direct cardiac reprogramming. Circ Res 2015;116:1378–1391. [DOI] [PubMed] [Google Scholar]
- 12. Zhou B, Ma Q, Rajagopal S, Wu SM, Domian I, Rivera-Feliciano J, Jiang D, von Gise A, Ikeda S, Chien KR, Pu WT.. Epicardial progenitors contribute to the cardiomyocyte lineage in the developing heart. Nature 2008;454:109–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ruiz-Villalba A, Simón AM, Pogontke C, Castillo MI, Abizanda G, Pelacho B, Sánchez-Domínguez R, Segovia JC, Prósper F, Pérez-Pomares JM.. Interacting resident epicardium-derived fibroblasts and recruited bone marrow cells form myocardial infarction scar. J Am Coll Cardiol 2015;65:2057–2066. [DOI] [PubMed] [Google Scholar]
- 14. Botham CM, Bennett WL, Cooke JP.. Clinical trials of adult stem cell therapy for peripheral artery disease. Methodist Debakey Cardiovasc J 2013;9:201–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hagensen MK, Vanhoutte PM, Bentzon JF.. Arterial endothelial cells: Still the craftsmen of regenerated endothelium. Cardiovasc Res 2012;95:281–289. [DOI] [PubMed] [Google Scholar]
- 16. Hirase T, Node K.. Endothelial dysfunction as a cellular mechanism for vascular failure. Am J Physiol Heart Circ Physiol 2012;302:H499–H505. [DOI] [PubMed] [Google Scholar]
- 17. Hong X, Le Bras A, Margariti A, Xu Q.. Reprogramming towards endothelial cells for vascular regeneration. Genes Dis 2016;3:186–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mocharla P, Briand S, Giannotti G, Dörries C, Jakob P, Paneni F, Lüscher T, Landmesser U.. AngiomiR-126 expression and secretion from circulating CD34+ and CD14+ PBMCs: role for proangiogenic effects and alterations in type 2 diabetics. Blood 2013;121:226–236. [DOI] [PubMed] [Google Scholar]
- 19. Jakob P, Doerries C, Briand S, Mocharla P, Krankel N, Besler C, Mueller M, Manes C, Templin C, Baltes C, Rudin M, Adams H, Wolfrum M, Noll G, Ruschitzka F, Luscher TF, Landmesser U.. Loss of AngiomiR-126 and 130a in angiogenic early outgrowth cells from patients with chronic heart failure: role for impaired in vivo neovascularization and cardiac repair capacity. Circulation 2012;126:2962–2975. [DOI] [PubMed] [Google Scholar]
- 20. Giannotti G, Doerries C, Mocharla PS, Mueller MF, Bahlmann FH, Horvàth T, Jiang H, Sorrentino SA, Steenken N, Manes C, Marzilli M, Rudolph KL, Lüscher TF, Drexler H, Landmesser U.. Impaired endothelial repair capacity of early endothelial progenitor cells in prehypertension: relation to endothelial dysfunction. Hypertension 2010;55:1389–1397. [DOI] [PubMed] [Google Scholar]
- 21. Paneni F, Costantino S, Kränkel N, Cosentino F, Lüscher TF.. Reprogramming ageing and longevity genes restores paracrine angiogenic properties of early outgrowth cells. Eur Heart J 2016;37:1733–1737. [DOI] [PubMed] [Google Scholar]
- 22. Ott HC, Matthiesen TS, Goh S, Black LD, Kren SM, Netoff TI, Taylor DA.. Perfusion-decellularized matrix: using nature’s platform to engineer a bioartificial heart. Nat Med 2008;14:213–221. [DOI] [PubMed] [Google Scholar]
- 23. Sánchez PL, Fernández-Santos ME, Costanza S, Climent AM, Moscoso I, Gonzalez-Nicolas MA, Sanz-Ruiz R, Rodríguez H, Kren SM, Garrido G, Escalante JL, Bermejo J, Elizaga J, Menarguez J, Yotti R, Pérez del Villar C, Espinosa MA, Guillem MS, Willerson JT, Bernad A, Matesanz R, Taylor DA, Fernández-Avilés F.. Acellular human heart matrix: a critical step toward whole heart grafts. Biomaterials 2015;61:279–289. [DOI] [PubMed] [Google Scholar]
- 24. Guyette JP, Charest JM, Mills RW, Jank BJ, Moser PT, Gilpin SE, Gershlak JR, Okamoto T, Gonzalez G, Milan DJ, Gaudette GR, Ott HC.. Bioengineering human myocardium on native extracellular matrix. Circ Res 2016;118:56–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Garreta E, de Oñate L, Fernández-Santos ME, Oria R, Tarantino C, Climent AM, Marco A, Samitier M, Martínez E, Valls-Margarit M, Matesanz R, Taylor DA, Fernández-Avilés F, Izpisua Belmonte JC, Montserrat N.. Myocardial commitment from human pluripotent stem cells: Rapid production of human heart grafts. Biomaterials 2016;98:64–78. [DOI] [PubMed] [Google Scholar]
- 26. Chong JJH, Yang X, Don CW, Minami E, Liu Y-W, Weyers JJ, Mahoney WM, Van Biber B, Cook SM, Palpant NJ, Gantz JA, Fugate JA, Muskheli V, Gough GM, Vogel KW, Astley CA, Hotchkiss CE, Baldessari A, Pabon L, Reinecke H, Gill EA, Nelson V, Kiem H-P, Laflamme M, Murry CE.. Human embryonic-stem-cell-derived cardiomyocytes regenerate non-human primate hearts. Nature 2014;510:273–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Blin G, Nury D, Stefanovic S, Neri T, Guillevic O, Brinon B, Bellamy V, Rücker-Martin C, Barbry P, Bel A, Bruneval P, Cowan C, Pouly J, Mitalipov S, Gouadon E, Binder P, Hagège A, Desnos M, Renaud JF, Menasché P, Pucéat M.. A purified population of multipotent cardiovascular progenitors derived from primate pluripotent stem cells engrafts in postmyocardial infarcted nonhuman primates. J Clin Invest 2010;120:1125–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Menasché P, Vanneaux V, Hagège A, Bel A, Cholley B, Cacciapuoti I, Parouchev A, Benhamouda N, Tachdjian G, Tosca L, Trouvin J, Fabreguettes J, Bellamy V, Guillemain R, Suberbielle Boissel C, Tartour E, Desnos M, Larghero J.. Human embryonic stem cell-derived cardiac progenitors for severe heart failure treatment: first clinical case report. Eur Heart J 2015;36:2011–2017. [DOI] [PubMed] [Google Scholar]
- 29. Madonna R, Van Laake L, Davidson S, Engel F, Hausenloy D, Lecour S, Leor J, Perrino C, Schulz R, Ytrehus K, Landmesser U, Mummery C, Janssens S, Willerson J, Eschenhagen T, Ferdinandy P, Sluijter J.. Position Paper of the European Society of Cardiology Working Group Cellular Biology of the Heart: cell-based therapies for myocardial repair and regeneration in ischemic heart disease and heart failure. Eur Heart J 2016;37:1789–1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Broughton KM, Sussman MA.. Empowering adult stem cells for myocardial regeneration V2.0. Circ Res 2016;118:867–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zafiriou MP, Noack C, Unsöld B, Didie M, Pavlova E, Fischer HJ, Reichardt HM, Bergmann MW, El-Armouche A, Zimmermann WH, Zelarayan LC.. Erythropoietin responsive cardiomyogenic cells contribute to heart repair post myocardial infarction. Stem Cells 2014;32:2480–2491. [DOI] [PubMed] [Google Scholar]
- 32. Barile L, Lionetti V, Cervio E, Matteucci M, Gherghiceanu M, Popescu LM, Torre T, Siclari F, Moccetti T, Vassalli G.. Extracellular vesicles from human cardiac progenitor cells inhibit cardiomyocyte apoptosis and improve cardiac function after myocardial infarction. Cardiovasc Res 2014;103:1–24. [DOI] [PubMed] [Google Scholar]
- 33. Emanueli C, Shearn AIU, Angelini GD, Sahoo S.. Exosomes and exosomal miRNAs in cardiovascular protection and repair. Vascul Pharmacol 2015;71:24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. De Jong R, Van Hout GPJ, Houtgraaf JH, Kazemi K, Wallrapp C, Lewis A, Pasterkamp G, Hoefer IE, Duckers HJ.. Intracoronary infusion of encapsulated glucagon-like peptide-1-eluting mesenchymal stem cells preserves left ventricular function in a porcine model of acute myocardial infarction. Circ Cardiovasc Interv 2014;7:673–683. [DOI] [PubMed] [Google Scholar]
- 35. Seif-Naraghi SB, Singelyn JM, Salvatore MA, Osborn KG, Wang JJ, Sampat U, Kwan OL, Strachan GM, Wong J, Schup-Magoffin PJ, Braden RL, Bartels K, DeQuach JA, Preul M, Kinsey AM, DeMaria AN, Dib N, Christman KL.. Safety and efficacy of an injectable extracellular matrix hydrogel for treating myocardial infarction. Sci Transl Med 2013;5:173ra25.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Madonna R, Taylor DA, Geng YJ, De Caterina R, Shelat H, Perin EC, Willerson JT.. Transplantation of mesenchymal cells rejuvenated by the overexpression of telomerase and myocardin promotes revascularization and tissue repair in a murine model of hindlimb ischemia. Circ Res 2013;113:902–914. [DOI] [PubMed] [Google Scholar]
- 37. Chung ES, Miller L, Patel AN, Anderson RD, Mendelsohn FO, Traverse J, Silver KH, Shin J, Ewald G, Farr MJ, Anwaruddin S, Plat F, Fisher SJ, AuWerter AT, Pastore JM, Aras R, Penn MS.. Changes in ventricular remodelling and clinical status during the year following a single administration of stromal cell-derived factor-1 non-viral gene therapy in chronic ischaemic heart failure patients: the STOP-HF randomized Phase II trial. Eur Heart J 2015;36:2228–2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bär C, Bernardes de Jesus B, Serrano R, Tejera A, Ayuso E, Jimenez V, Formentini I, Bobadilla M, Mizrahi J, de Martino A, Gomez G, Pisano D, Mulero F, Wollert KC, Bosch F, Blasco MA.. Telomerase expression confers cardioprotection in the adult mouse heart after acute myocardial infarction. Nat Commun 2014;5:5863.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Vunjak Novakovic G, Eschenhagen T, Mummery C, Novakovic GV, Eschenhagen T, Mummery C.. Myocardial tissue engineering: in vitro models. Cold Spring Harb Perspect Med 2014;4:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Breckwoldt K, Weinberger F, Eschenhagen T.. Heart regeneration. Biochim Biophys Acta 2016;1863:1749–1759. [DOI] [PubMed] [Google Scholar]
- 41. Van Der Spoel TIG, Jansen Of Lorkeers SJ, Agostoni P, Van Belle E, Gyngysi M, Sluijter JPG, Cramer MJ, Doevendans PA, Chamuleau SAJ, Gyöngyösi M, Sluijter JPG, Cramer MJ, Doevendans PA, Chamuleau SAJ.. Human relevance of pre-clinical studies in stem cell therapy: systematic review and meta-analysis of large animal models of ischaemic heart disease. Cardiovasc Res 2011;91:649–658. [DOI] [PubMed] [Google Scholar]
- 42. Jansen Of Lorkeers SJ, Eding JEC, Vesterinen HM, van der Spoel TIG, Sena ES, Duckers HJ, Doevendans PA, Macleod MR, Chamuleau SAJ.. Similar effect of autologous and allogeneic cell therapy for ischemic heart disease: systematic review and meta-analysis of large animal studies. Circ Res 2015;116:80–86. [DOI] [PubMed] [Google Scholar]
- 43. Zwetsloot PP, Végh AM, Jansen Of Lorkeers SJ, van Hout GP, Currie GL, Sena ES, Gremmels H, Buikema JW, Goumans MJ, Macleod MR, Doevendans PA, Chamuleau SA, Sluijter JP.. Cardiac stem cell treatment in myocardial infarction: a systematic review and meta-analysis of preclinical studies. Circ Res 2016;118:1223–1232. [DOI] [PubMed] [Google Scholar]
- 44. Soares MBP, Lima RS, Rocha LL, Takyia CM, Pontes-de-Carvalho L, de Carvalho AC, Ribeiro-dos-Santos R.. Transplanted bone marrow cells repair heart tissue and reduce myocarditis in chronic chagasic mice. Am J Pathol 2004;164:441–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Goldenberg RCS, Jelicks LA, Fortes FSA, Weiss LM, Rocha LL, Zhao D, de Carvalho AC, Spray DC, Tanowitz HB.. Bone marrow cell therapy ameliorates and reverses chagasic cardiomyopathy in a mouse model. J Infect Dis 2008;197:544–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Strauer BE, Brehm M, Zeus T, Köstering M, Hernandez A, Sorg RV, Kögler G, Wernet P.. Repair of infarcted myocardium by autologous intracoronary mononuclear bone marrow cell transplantation in humans. Circulation 2002;106:1913–1918. [DOI] [PubMed] [Google Scholar]
- 47. Peruzzi M, De Falco E, Abbate A, Biondi-Zoccai G, Chimenti I, Lotrionte M, Benedetto U, Delewi R, Marullo AGM, Frati G, Peruzzi M, De Falco E, Abbate A, Biondi-Zoccai G, Chimenti I, Lotrionte M, Benedetto U, Delewi R, Marullo AGM, Frati G.. State of the art on the evidence base in cardiac regenerative therapy: overview of 41 systematic reviews. Biomed Res Int 2015;2015:613782.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cao F, Sun D, Li C, Narsinh K, Zhao L, Li X, Feng X, Zhang J, Duan Y, Wang J, Liu D, Wang H.. Long-term myocardial functional improvement after autologous bone marrow mononuclear cells transplantation in patients with ST-segment elevation myocardial infarction: 4 years follow-up. Eur Heart J 2009;30:1986–1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Choudry F, Hamshere S, Saunders N, Veerapen J, Bavnbek K, Knight C, Pellerin D, Locca D, Westwood M, Rakhit R, Crake T, Kastrup J, Parmar M, Agrawal S, Jones D, Martin J, Mathur A.. A randomized double-blind control study of early intra-coronary autologous bone marrow cell infusion in acute myocardial infarction: the REGENERATE-AMI clinical trial. Eur Heart J 2016;37:256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hirsch A, Nijveldt R, van der Vleuten PA, Tio RA, van der Giessen WJ, Marques KMJ, Doevendans PA, Waltenberger J, Ten Berg JM, Aengevaeren WRM, Biemond BJ, Tijssen JGP, van Rossum AC, Piek JJ, Zijlstra F.. Intracoronary infusion of autologous mononuclear bone marrow cells in patients with acute myocardial infarction treated with primary PCI: pilot study of the multicenter HEBE trial. Catheter Cardiovasc Interv 2008;71:273–281. [DOI] [PubMed] [Google Scholar]
- 51. Huikuri HV, Kervinen K, Niemelä M, Ylitalo K, Säily M, Koistinen P, Savolainen ER, Ukkonen H, Pietilä M, Airaksinen JKE, Knuuti J, Mäkikallio TH.. Effects of intracoronary injection of mononuclear bone marrow cells on left ventricular function, arrhythmia risk profile, and restenosis after thrombolytic therapy of acute myocardial infarction. Eur Heart J 2008;29:2723–2732. [DOI] [PubMed] [Google Scholar]
- 52. Janssens S, Dubois C, Bogaert J, Theunissen K, Deroose C, Desmet W, Kalantzi M, Herbots L, Sinnaeve P, Dens J, Maertens J, Rademakers F, Dymarkowski S, Gheysens O, Van Cleemput J, Bormans G, Nuyts J, Belmans A, Mortelmans L, Boogaerts M, Van De Werf F.. Autologous bone marrow-derived stem-cell transfer in patients with ST-segment elevation myocardial infarction: double-blind, randomised controlled trial. Lancet 2006;367:113–121. [DOI] [PubMed] [Google Scholar]
- 53. Lunde K, Solheim S, Aakhus S, Arnesen H, Abdelnoor M, Egeland T, Endresen K, Ilebekk A, Mangschau A, Fjeld JG, Smith HJ, Taraldsrud E, Grøgaard HK, Bjørnerheim R, Brekke M, Müller C, Hopp E, Ragnarsson A, Brinchmann JE, Forfang K.. Intracoronary injection of mononuclear bone marrow cells in acute myocardial infarction. N Engl J Med 2006;355:1199–1209. [DOI] [PubMed] [Google Scholar]
- 54. Meluzín J, Mayer J, Groch L, Janousek S, Hornácek I, Hlinomaz O, Kala P, Panovský R, Prásek J, Kamínek M, Stanícek J, Klabusay M, Korístek Z, Navrátil M, Dusek L, Vinklárková J.. Autologous transplantation of mononuclear bone marrow cells in patients with acute myocardial infarction: the effect of the dose of transplanted cells on myocardial function. Am Heart J 2006;152:975.e9–915. [DOI] [PubMed] [Google Scholar]
- 55. Plewka M, Krzeminska-Pakula M, Lipiec P.. Effect of intracoronary injection of mononuclear bone marrow stem cells on left ventricular function in patients with acute myocardial infarction. Am J Cardiol 2009;104:1336–1342. [DOI] [PubMed] [Google Scholar]
- 56. Roncalli J, Mouquet F, Piot C, Trochu JN, Le Corvoisier P, Neuder Y, Le Tourneau T, Agostini D, Gaxotte V, Sportouch C, Galinier M, Crochet D, Teiger E, Richard MJ, Polge AS, Beregi JP, Manrique A, Carrie D, Susen S, Klein B, Parini A, Lamirault G, Croisille P, Rouard H, Bourin P, Nguyen JM, Delasalle B, Vanzetto G, Van Belle E, Lemarchand P.. Intracoronary autologous mononucleated bone marrow cell infusion for acute myocardial infarction: results of the randomized multicenter BONAMI trial. Eur Heart J 2011;32:1748–1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. San Roman JA, Sánchez PL, Villa A, Sanz-Ruiz R, Fernandez-Santos ME, Gimeno F, Ramos B, Arnold R, Serrador A, Gutiérrez H, Martin-Herrero F, Rollán MJ, Fernández-Vázquez F, López-Messa J, Ancillo P, Pérez-Ojeda G, Fernández-Avilés F.. Comparison of different bone marrow-derived stem cell approaches in reperfused STEMI: a multicenter, prospective, randomized, open-labeled TECAM trial. J Am Coll Cardiol 2015;65:2372–2382. [DOI] [PubMed] [Google Scholar]
- 58. Schächinger V, Erbs S, Elsässer A, Haberbosch W, Hambrecht R, Hölschermann H, Yu J, Corti R, Mathey DG, Hamm CW, Süselbeck T, Assmus B, Tonn T, Dimmeler S, Zeiher AM.. Intracoronary bone marrow-derived progenitor cells in acute myocardial infarction. N Engl J Med 2006;355:1210–1221. [DOI] [PubMed] [Google Scholar]
- 59. Sürder D, Manka R, Lo Cicero V, Moccetti T, Rufibach K, Soncin S, Turchetto L, Radrizzani M, Astori G, Schwitter J, Erne P, Zuber M, Auf der Maur C, Jamshidi P, Gaemperli O, Windecker S, Moschovitis A, Wahl A, Bühler I, Wyss C, Kozerke S, Landmesser U, Lüscher TF, Corti R.. Intracoronary injection of bone marrow-derived mononuclear cells early or late after acute myocardial infarction: effects on global left ventricular function. Circulation 2013;127:1968–1979. [DOI] [PubMed] [Google Scholar]
- 60. Traverse JH, Henry TD, Pepine CJ, Willerson JT, Zhao DX, Ellis SG, Forder JR, Anderson RD, Hatzopoulos AK, Penn MS, Perin EC, Chambers J, Baran KW, Raveendran G, Lambert C, Lerman A, Simon DI, Vaughan DE, Lai D, Gee AP, Taylor DA, Cogle CR, Thomas JD, Olson RE, Bowman S, Francescon J, Geither C, Handberg E, Kappenman C, Westbrook L, Piller LB, Simpson LM, Baraniuk S, Loghin C, Aguilar D, Richman S, Zierold C, Spoon DB, Bettencourt J, Sayre SL, Vojvodic RW, Skarlatos SI, Gordon DJ, Ebert RF, Kwak M, Moyé LA, Simari RD.. Effect of the use and timing of bone marrow mononuclear cell delivery on left ventricular function after acute myocardial infarction: the TIME randomized trial. JAMA 2012;308:2380–2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wöhrle J, Merkle N, Mailänder V, Nusser T, Schauwecker P, von Scheidt F, Schwarz K, Bommer M, Wiesneth M, Schrezenmeier H, Hombach V.. Results of intracoronary stem cell therapy after acute myocardial infarction. Am J Cardiol 2010;105:804–812. [DOI] [PubMed] [Google Scholar]
- 62. Wollert KC, Meyer GP, Lotz J, Ringes-Lichtenberg S, Lippolt P, Breidenbach C, Fichtner S, Korte T, Hornig B, Messinger D, Arseniev L, Hertenstein B, Ganser A, Drexler H.. Intracoronary autologous bone-marrow cell transfer after myocardial infarction: the BOOST randomised controlled clinical trial. Lancet 2004;364:141–148. [DOI] [PubMed] [Google Scholar]
- 63. Sürder D, Manka R, Moccetti T, Lo Cicero V, Emmert MY, Klersy C, Soncin S, Turchetto L, Radrizzani M, Zuber M, Windecker S, Moschovitis A, Bühler I, Kozerke S, Erne P, Lüscher TF, Corti R.. The effect of bone marrow derived mononuclear cell treatment, early or late after acute myocardial infarction: twelve months CMR and long-term clinical results. Circ Res 2016;119:481–490. [DOI] [PubMed] [Google Scholar]
- 64. Lee JW, Lee SH, Youn YJ, Ahn MS, Kim JY, Yoo BS, Yoon J, Kwon W, Hong IS, Lee K, Kwan J, Park KS, Choi D, Jang YS, Hong MK.. A randomized, open-label, multicenter trial for the safety and efficacy of adult mesenchymal stem cells after acute myocardial infarction. J Korean Med Sci 2014;29:23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Assmus B, Schächinger V, Teupe C, Britten M, Lehmann R, Döbert N, Grünwald F, Aicher A, Urbich C, Martin H, Hoelzer D, Dimmeler S, Zeiher AM.. Transplantation of progenitor cells and regeneration enhancement in acute myocardial infarction (TOPCARE-AMI). Circulation 2002;106:3009–3017. [DOI] [PubMed] [Google Scholar]
- 66. Bartunek J, Vanderheyden M, Vandekerckhove B, Mansour S, De Bruyne B, De Bondt P, Van Haute I, Lootens N, Heyndrickx G, Wijns W.. Intracoronary injection of CD133-positive enriched bone marrow progenitor cells promotes cardiac recovery after recent myocardial infarction: feasibility and safety. Circulation 2005;112:178–183. [DOI] [PubMed] [Google Scholar]
- 67. Colombo A, Castellani M, Piccaluga E, Pusineri E, Palatresi S, Longari V, Canzi C, Sacchi E, Rossi E, Rech R, Gerundini P, Viecca M, Deliliers GL, Rebulla P, Soligo D, Giordano R.. Myocardial blood flow and infarct size after CD133+ cell injection in large myocardial infarction with good recanalization and poor reperfusion: results from a randomized controlled trial. J Cardiovasc Med (Hagerstown) 2011;12:239–248. [DOI] [PubMed] [Google Scholar]
- 68. Quyyumi AA, Waller EK, Murrow J, Esteves F, Galt J, Oshinski J, Lerakis S, Sher S, Vaughan D, Perin E, Willerson J, Kereiakes D, Gersh BJ, Gregory D, Werner A, Moss T, Chan WS, Preti R, Pecora AL.. CD34(+) cell infusion after ST elevation myocardial infarction is associated with improved perfusion and is dose dependent. Am Heart J 2011;161:98–105. [DOI] [PubMed] [Google Scholar]
- 69. Tendera M, Wojakowski W, Ruzyłło W, Chojnowska L, Kepka C, Tracz W, Musiałek P, Piwowarska W, Nessler J, Buszman P, Grajek S, Breborowicz P, Majka M, Ratajczak MZ.. Intracoronary infusion of bone marrow-derived selected CD34+CXCR4+ cells and non-selected mononuclear cells in patients with acute STEMI and reduced left ventricular ejection fraction: results of randomized, multicentre Myocardial Regeneration by Intracor. Eur Heart J 2009;30:1313–1321. [DOI] [PubMed] [Google Scholar]
- 70. Houtgraaf JH, den Dekker WK, van Dalen BM, Springeling T, de Jong R, van Geuns RJ, Geleijnse ML, Fernandez-Aviles F, Zijlsta F, Serruys PW, Duckers HJ.. First experience in humans using adipose tissue-derived regenerative cells in the treatment of patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 2012;59:539–540. [DOI] [PubMed] [Google Scholar]
- 71. Makkar RR, Smith RR, Cheng K, Malliaras K, Thomson LEJ, Berman D, Czer LSC, Marbán L, Mendizabal A, Johnston PV, Russell SD, Schuleri KH, Lardo AC, Gerstenblith G, Marbán E.. Intracoronary cardiosphere-derived cells for heart regeneration after myocardial infarction (CADUCEUS): a prospective, randomised phase 1 trial. Lancet 2012;379:895–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Hibbert B, Hayley B, Beanlands RS, Le May M, Davies R, So D, Marquis J-F, Labinaz M, Froeschl M, O’brien ER, Burwash IG, Wells G. A, Pourdjabbar A, Simard T, Atkins H, Glover C.. Granulocyte colony-stimulating factor therapy for stem cell mobilization following anterior wall myocardial infarction: the CAPITAL STEM MI randomized trial. CMAJ 2014;186:427–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Ince H, Petzsch M, Kleine HD, Schmidt H, Rehders T, Körber T, Schümichen C, Freund M, Nienaber CA.. Preservation from left ventricular remodeling by front-integrated revascularization and stem cell liberation in evolving acute myocardial infarction by use of granulocyte-colony-stimulating factor (FIRSTLINE-AMI). Circulation 2005;112:3097–3106. [DOI] [PubMed] [Google Scholar]
- 74. Kang HJ, Lee HY, Na SH, Chang SA, Park KW, Kim HKHS, Kim SY, Chang HJ, Lee W, Kang WJ, Koo BK, Kim YJ, Lee DS, Sohn DW, Han KS, Oh BH, Park YB, Kim KH.. Differential effect of intracoronary infusion of mobilized peripheral blood stem cells by granulocyte colony-stimulating factor on left ventricular function and remodeling in patients with acute myocardial infarction versus old myocardial infarction. Circulation 2006;114:145–151. [DOI] [PubMed] [Google Scholar]
- 75. Lipinski MJ, Biondi-Zoccai GGL, Abbate A, Khianey R, Sheiban I, Bartunek J, Vanderheyden M, Kim HS, Kang HJ, Strauer BE, Vetrovec GW.. Impact of intracoronary cell therapy on left ventricular function in the setting of acute myocardial infarction. A collaborative systematic review and meta-analysis of controlled clinical trials. J Am Coll Cardiol 2007;50:1761–1767. [DOI] [PubMed] [Google Scholar]
- 76. Ripa RS, Jorgensen E, Wang Y, Thune JJ, Nilsson JC, Sondergaard L, Johnsen HE, Kober L, Grande PKJ.. Stem cell mobilization induced by subcutaneous granulocyte-colony stimulating factor to improve cardiac regeneration after acute ST-elevation myocardial infarction: result of the double-blind, randomized, placebo-controlled stem cells in myocardial infarc. Circulation 2006;113:1983–1992. [DOI] [PubMed] [Google Scholar]
- 77. Zohlnhöfer D, Ott I, Mehilli J, Schömig K, Michalk F, Ibrahim T, Meisetschläger G, von Wedel J, Bollwein H, Seyfarth M, Dirschinger J, Schmitt C, Schwaiger M, Kastrati A, Schömig A.. Stem cell mobilization by granulocyte colony-stimulating factor in patients with acute myocardial infarction: a randomized controlled trial. JAMA 2006;295:1003–1010. [DOI] [PubMed] [Google Scholar]
- 78. Dib N, Dinsmore J, Lababidi Z, White B, Moravec S, Campbell A, Rosenbaum A, Seyedmadani K, Jaber WA, Rizenhour CS, Diethrich E.. One-year follow-up of feasibility and safety of the first U.S., randomized, controlled study using 3-dimensional guided Catheter-Based Delivery of Autologous Skeletal Myoblasts for Ischemic Cardiomyopathy (CAuSMIC Study). JACC Cardiovasc Interv 2009;2:9–16. [DOI] [PubMed] [Google Scholar]
- 79. Duckers HJ, Houtgraaf J, Hehrlein C, Schofer J, Waltenberger J, Gershlick A, Bartunek J, Nienaber C, Macaya C, Peters N, Smits P, Siminiak T, Van Mieghem W, Legrand V, Serruys PW.. Final results of a phase IIa, randomised, open-label trial to evaluate the percutaneous intramyocardial transplantation of autologous skeletal myoblasts in congestive heart failure patients: the SEISMIC trial. EuroIntervention 2011;6:805–812. [DOI] [PubMed] [Google Scholar]
- 80. Menasché P, Alfieri O, Janssens S, McKenna W, Reichenspurner H, Trinquart L, Vilquin JT, Marolleau JP, Seymour B, Larghero J, Lake S, Chatellier G, Solomon S, Desnos M, Hagège AA.. The myoblast autologous grafting in ischemic cardiomyopathy (MAGIC) trial: first randomized placebo-controlled study of myoblast transplantation. Circulation 2008;117:1189–1200. [DOI] [PubMed] [Google Scholar]
- 81. Povsic TJ, O’connor CM, Henry T, Taussig A, Kereiakes DJ, Fortuin FD, Niederman A, Schatz R, Spencer R, Owens D, Banks M, Joseph D, Roberts R, Alexander JH, Sherman W.. A double-blind, randomized, controlled, multicenter study to assess the safety and cardiovascular effects of skeletal myoblast implantation by catheter delivery in patients with chronic heart failure after myocardial infarction. Am Heart J 2011;162:654–662.e1. [DOI] [PubMed] [Google Scholar]
- 82. Hendrikx M, Hensen K, Clijsters C, Jongen H, Koninckx R, Bijnens E, Ingels M, Jacobs A, Geukens R, Dendale P, Vijgen J, Dilling D, Steels P, Mees U, Rummens JL.. Recovery of regional but not global contractile function by the direct intramyocardial autologous bone marrow transplantation: results from a randomized controlled clinical trial. Circulation 2006;114:101–107. [DOI] [PubMed] [Google Scholar]
- 83. Hu S, Liu S, Zheng Z, Yuan X, Li L, Lu M, Shen R, Duan F, Zhang X, Li J, Liu X, Song Y, Wang W, Zhao S, He Z, Zhang H, Yang K, Feng W, Wang X.. Isolated coronary artery bypass graft combined with bone marrow mononuclear cells delivered through a graft vessel for patients with previous myocardial infarction and chronic heart failure: a single-center, randomized, double-blind, placebo-controlled Cl. J Am Coll Cardiol 2011;57:2409–2415. [DOI] [PubMed] [Google Scholar]
- 84. Mozid A, Yeo C, Arnous S, Ako E, Saunders N, Locca D, Brookman P, Archbold RA, Rothman M, Mills P, Agrawal S, Martin J, Mathur A.. Safety and feasibility of intramyocardial versus intracoronary delivery of autologous cell therapy in advanced heart failure: the REGENERATE-IHD pilot study. Regen Med 2014;9:269–278. [DOI] [PubMed] [Google Scholar]
- 85. Yao K, Huang R, Qian J, Cui J, Ge L, Li Y, Zhang F, Shi H, Huang D, Zhang S, Sun A, Zou Y, Ge J.. Administration of intracoronary bone marrow mononuclear cells on chronic myocardial infarction improves diastolic function. Heart 2008;94:1147–1153. [DOI] [PubMed] [Google Scholar]
- 86. Chen S, Liu Z, Tian N, Zhang J, Yei F, Duan B, Zhu Z, Lin S, Kwan TW.. Intracoronary transplantation of autologous bone marrow mesenchymal stem cells for ischemic cardiomyopathy due to isolated chronic occluded left anterior descending artery. J Invasive Cardiol 2006;18:552–556. [PubMed] [Google Scholar]
- 87. Heldman AW, DiFede DL, Fishman JE, Zambrano JP, Trachtenberg BH, Karantalis V, Mushtaq M, Williams AR, Suncion VY, McNiece IK, Ghersin E, Soto V, Lopera G, Miki R, Willens H, Hendel R, Mitrani R, Pattany P, Feigenbaum G, Oskouei B, Byrnes J, Lowery MH, Sierra J, Pujol MV, Delgado C, Gonzalez PJ, Rodriguez JE, Bagno LL, Rouy D, Altman P, Foo CW, da Silva J, Anderson E, Schwarz R, Mendizabal A, Hare JM.. Transendocardial mesenchymal stem cells and mononuclear bone marrow cells for ischemic cardiomyopathy: the TAC-HFT randomized trial. JAMA 2014;311:62–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Mathiasen AB, Qayyum AA, Jørgensen E, Helqvist S, Fischer-Nielsen A, Kofoed KF, Haack-Sørensen M, Ekblond A, Kastrup J.. Bone marrow-derived mesenchymal stromal cell treatment in patients with severe ischaemic heart failure: a randomized placebo-controlled trial (MSC-HF trial). Eur Heart J 2015;36:1744–1753. [DOI] [PubMed] [Google Scholar]
- 89. Assmus B, Honold J, Schächinger V, Britten MB, Fischer-Rasokat U, Lehmann R, Teupe C, Pistorius K, Martin H, Abolmaali ND, Tonn T, Dimmeler S, Zeiher AM.. Transcoronary transplantation of progenitor cells after myocardial infarction. N Engl J Med 2006;355:1222–1232. [DOI] [PubMed] [Google Scholar]
- 90. Honold J, Fischer-Rasokat U, Lehmann R, Leistner DM, Seeger FH, Schachinger V, Martin H, Dimmeler S, Zeiher AM, Assmus B.. G-CSF stimulation and coronary reinfusion of mobilized circulating mononuclear proangiogenic cells in patients with chronic ischemic heart disease: five-year results of the TOPCARE-G-CSF trial. Cell Transplant 2012;21:2325–2337. [DOI] [PubMed] [Google Scholar]
- 91. Patel AN, Geffner L, Vina RF, Saslavsky J, Urschel HC, Kormos R, Benetti F.. Surgical treatment for congestive heart failure with autologous adult stem cell transplantation: a prospective randomized study. J Thorac Cardiovasc Surg 2005;130:1631–1638. [DOI] [PubMed] [Google Scholar]
- 92. Nasseri BA, Ebell W, Dandel M, Kukucka M, Gebker R, Doltra A, Knosalla C, Choi YH, Hetzer R, Stamm C.. Autologous CD133+ bone marrow cells and bypass grafting for regeneration of ischaemic myocardium: the Cardio133 trial. Eur Heart J 2014;35:1263–1274. [DOI] [PubMed] [Google Scholar]
- 93. Perin EC, Silva GV, Zheng Y, Gahremanpour A, Canales J, Patel D, Fernandes MR, Keller LH, Quan X, Coulter SA, Moore WH, Herlihy JP, Willerson JT.. Randomized, double-blind pilot study of transendocardial injection of autologous aldehyde dehydrogenase-bright stem cells in patients with ischemic heart failure. Am Heart J 2012;163:415–421. [DOI] [PubMed] [Google Scholar]
- 94. Patel AN, Henry TD, Quyyumi AA, Schaer GL, Anderson RD, Toma C, East C, Remmers AE, Goodrich J.. Ixmyelocel-T for patients with ischaemic heart failure: a prospective randomised double-blind trial. Lancet 2016;6736:1–10. [DOI] [PubMed] [Google Scholar]
- 95. Bartunek J, Behfar A, Dolatabadi D, Vanderheyden M, Ostojic M, Dens J, El Nakadi B, Banovic M, Beleslin B, Vrolix M, Legrand V, Vrints C, Vanoverschelde JL, Crespo-Diaz R, Homsy C, Tendera M, Waldman S, Wijns W, Terzic A.. Cardiopoietic stem cell therapy in heart failure: the C-CURE (Cardiopoietic stem Cell therapy in heart failURE) multicenter randomized trial with lineage-specified biologics. J Am Coll Cardiol 2013;61:2329–2338. [DOI] [PubMed] [Google Scholar]
- 96. Assmus B, Walter DH, Seeger FH, Leistner DM, Lutz A, Dimmeler S, Steiner J, Ziegler I, Lutz A, Khaled W, Klotsche J, Tonn T, Dimmeler S, Zeiher AM.. Effect of shock wave-facilitated intracoronary cell therapy on LVEF in patients with chronic heart failure: the CELLWAVE randomized clinical trial. JAMA 2013;309:1622–1631. [DOI] [PubMed] [Google Scholar]
- 97. Bolli R, Chugh AR, D’amario D, Loughran JH, Stoddard MF, Ikram S, Beache GM, Wagner SG, Leri A, Hosoda T, Sanada F, Elmore JB, Goichberg P, Cappetta D, Solankhi NK, Fahsah I, Rokosh DG, Slaughter MS, Kajstura J, Anversa P.. Cardiac stem cells in patients with ischaemic cardiomyopathy (SCIPIO): initial results of a randomised phase 1 trial. Lancet 2011;378:1847–1857. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 98. Simons M, Annex BH, Laham RJ, Kleiman N, Henry T, Dauerman H, Udelson JE, Gervino EV, Pike M, Whitehouse MJ, Moon T, Chronos NA.. Pharmacological treatment of coronary artery disease with recombinant fibroblast growth factor-2: double-blind, randomized, controlled clinical trial. Circulation 2002;105:788–793. [DOI] [PubMed] [Google Scholar]
- 99. Henry TD, Annex BH, McKendall GR, Azrin MA, Lopez JJ, Giordano FJ, Shah PK, Willerson JT, Benza RL, Berman DS, Gibson CM, Bajamonde A, Rundle AC, Fine J, McCluskey ER.. The VIVA trial: vascular endothelial growth factor in ischemia for vascular angiogenesis. Circulation 2003;107:1359–1365. [DOI] [PubMed] [Google Scholar]
- 100. Kastrup J, Jørgensen E, Rück A, Tägil K, Glogar D, Ruzyllo W, Bøtker HE, Dudek D, Drvota V, Hesse B, Thuesen L, Blomberg P, Gyöngyösi M, Sylvén C.. Direct intramyocardial plasmid vascular endothelial growth factor-A165 gene therapy in patients with stable severe angina pectoris A randomized double-blind placebo-controlled study: the Euroinject One trial. J Am Coll Cardiol 2005;45:982–988. [DOI] [PubMed] [Google Scholar]
- 101. Greenberg B, Butler J, Felker GM, Ponikowski P, Voors AA, Desai AS, Barnard D, Bouchard A, Jaski B, Lyon AR, Pogoda JM, Rudy JJ, Zsebo KM.. Calcium upregulation by percutaneous administration of gene therapy in patients with cardiac disease (CUPID 2): a randomised, multinational, double-blind, placebo-controlled, phase 2b trial. Lancet 2016;387:1178–1186. [DOI] [PubMed] [Google Scholar]
- 102. Perin EC, Silva GV, Henry TD, Cabreira-Hansen MG, Moore WH, Coulter SA, Herlihy JP, Fernandes MR, Cheong BY, Flamm SD, Traverse JH, Zheng Y, Smith D, Shaw S, Westbrook L, Olson R, Patel D, Gahremanpour A, Canales J, Vaughn WK, Willerson JT.. A randomized study of transendocardial injection of autologous bone marrow mononuclear cells and cell function analysis in ischemic heart failure (FOCUS-HF). Am Heart J 2011;161:1078–1087. [DOI] [PubMed] [Google Scholar]
- 103. Perin EC, Willerson JT, Pepine CJ, Henry TD, Ellis SG, Zhao DX, Silva GV, Lai D, Thomas JD, Kronenberg MW, Martin AD, Anderson RD, Traverse JH, Penn MS, Anwaruddin S, Hatzopoulos AK, Gee AP, Taylor DA, Cogle CR, Smith D, Westbrook L, Chen J, Handberg E, Olson RE, Geither C, Bowman S, Francescon J, Baraniuk S, Piller LB, Simpson LM, Loghin C, Aguilar D, Richman S, Zierold C, Bettencourt J, Sayre SL, Vojvodic RW, Skarlatos SI, Gordon DJ, Ebert RF, Kwak M, Moyé LA, Simari RD.. Effect of transendocardial delivery of autologous bone marrow mononuclear cells on functional capacity, left ventricular function, and perfusion in chronic heart failure: the FOCUS-CCTRN trial. JAMA 2012;307:1717–1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Pokushalov E, Romanov A, Chernyavsky A, Larionov P, Terekhov I, Artyomenko S, Poveshenko O, Kliver E, Shirokova N, Karaskov A, Dib N.. Efficiency of intramyocardial injections of autologous bone marrow mononuclear cells in patients with ischemic heart failure: a randomized study. J Cardiovasc Transl Res 2010;3:160–168. [DOI] [PubMed] [Google Scholar]
- 105. Tse HF, Thambar S, Kwong YL, Rowlings P, Bellamy G, McCrohon J, Thomas P, Bastian B, Chan JJKF, Lo G, Ho CL, Chan WS, Kwong RY, Parker A, Hauser TH, Chan JJKF, Fong DYT, Lau CP.. Prospective randomized trial of direct endomyocardial implantation of bone marrow cells for treatment of severe coronary artery diseases (PROTECT-CAD trial). Eur Heart J 2007;28:2998–3005. [DOI] [PubMed] [Google Scholar]
- 106. van Ramshorst J, Bax JJ, Beeres SL, Dibbets-Schneider P, Roes SD, Stokkel MPM, de Roos A, Fibbe WE, Zwaginga JJ, Boersma E, Schalij MJ, Atsma DE.. Intramyocardial bone marrow cell injection for chronic myocardial ischemia: a randomized controlled trial. JAMA 2009;301:1997–2004. [DOI] [PubMed] [Google Scholar]
- 107. Losordo DW, Henry TD, Davidson C, Sup Lee J, Costa MA, Bass T, Mendelsohn F, Fortuin FD, Pepine CJ, Traverse JH, Amrani D, Ewenstein BM, Riedel N, Story K, Barker K, Povsic TJ, Harrington RA, Schatz RA.. Intramyocardial, autologous CD34+ cell therapy for refractory angina. Circ Res 2011;109:428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Losordo DW, Schatz RA, White CJ, Udelson JE, Veereshwarayya V, Durgin M, Poh KK, Weinstein R, Kearney M, Chaudhry M, Burg A, Eaton L, Heyd L, Thorne T, Shturman L, Hoffmeister P, Story K, Zak V, Dowling D, Traverse JH, Olson RE, Flanagan J, Sodano D, Murayama T, Kawamoto A, Kusano KF, Wollins J, Welt F, Shah P, Soukas P, Asahara T, Henry TD.. Intramyocardial transplantation of autologous CD34+ stem cells for intractable angina: a phase I/IIa double-blind, randomized controlled trial. Circulation 2007;115:3165–3172. [DOI] [PubMed] [Google Scholar]
- 109. Wang WE, Yang D, Li L, Wang WE, Peng Y, Chen C, Chen P, Xia X, Wang H, Jiang J, Liao Q, Li Y, Xie G, Huang H, Guo Y, Ye L, Duan DD, Chen X, Houser SR, Zeng C.. Prolyl hydroxylase domain protein 2 silencing enhances the survival and paracrine function of transplanted adipose-derived stem cells in infarcted myocardium. Circ Res 2013;113:288–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Perin EC, Sanz-Ruiz R, Sánchez PL, Lasso J, Pérez-Cano R, Alonso-Farto JC, Pérez-David E, Fernández-Santos ME, Serruys PW, Duckers HJ, Kastrup J, Chamuleau S, Zheng Y, Silva GV, Willerson JT, Fernández-Avilés F.. Adipose-derived regenerative cells in patients with ischemic cardiomyopathy: the PRECISE Trial. Am Heart J 2014;168:88–95.e2. [DOI] [PubMed] [Google Scholar]
- 111. Seth S, Narang R, Bhargava B, Ray R, Mohanty S, Gulati G, Kumar L, Reddy KS, Venugopal P.. Percutaneous intracoronary cellular cardiomyoplasty for nonischemic cardiomyopathy: clinical and histopathological results: the first-in-man ABCD (Autologous Bone Marrow Cells in Dilated Cardiomyopathy) Trial. J Am Coll Cardiol 2006;48:2350–2351. [DOI] [PubMed] [Google Scholar]
- 112. Vrtovec B, Poglajen G, Sever M, Lezaic L, Domanovic D, Cernelc P, Haddad F, Torre-Amione G.. Effects of intracoronary stem cell transplantation in patients with dilated cardiomyopathy. J Card Fail 2011;17:272–281. [DOI] [PubMed] [Google Scholar]
- 113. Bocchi EA, Bacal F, Guimaraes G, Mendroni A, Mocelin A, Filho AE, Dores da Cruz F, Resende MC, Chamone D.. Granulocyte-colony stimulating factor or granulocyte-colony stimulating factor associated to stem cell intracoronary infusion effects in non ischemic refractory heart failure. Int J Cardiol 2010;138:94–97. [DOI] [PubMed] [Google Scholar]
- 114. Vrtovec B, Poglajen G, Lezaic L, Sever M, Domanovic D, Cernelc P, Socan A, Schrepfer S, Torre-Amione G, Haddad F, Wu JC.. Effects of intracoronary CD34+ stem cell transplantation in nonischemic dilated cardiomyopathy patients: 5-year follow-up. Circ Res 2013;112:165–173. [DOI] [PubMed] [Google Scholar]
- 115. Mushtaq M, DiFede DL, Golpanian S, Khan A, Gomes SA, Mendizabal A, Heldman AW, Hare JM.. Rationale and design of the Percutaneous Stem Cell Injection Delivery Effects on Neomyogenesis in Dilated Cardiomyopathy (the POSEIDON-DCM study): a phase I/II, randomized pilot study of the comparative safety and efficacy of transendocardial injection of autologous mesenchymal stem cell vs. allogeneic mesenchymal stem cells in patients with non-ischemic dilated cardiomyopathy. J Cardiovasc Transl Res 2014;7:769–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Procházka V, Gumulec J, Jalůvka F, Salounová D, Jonszta T, Czerný D, Krajča J, Urbanec R, Klement P, Martinek J, Klement GL.. Cell therapy, a new standard in management of chronic critical limb ischemia and foot ulcer. Cell Transplant 2010;19:1413–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Ozturk A, Kucukardali Y, Tangi F, Erikci A, Uzun G, Bashekim C, Sen H, Terekeci H, Narin Y, Ozyurt M, Ozkan S, Sayan O, Rodop O, Nalbant S, Sildiroglu O, Yalniz FF, Senkal IV, Sabuncu H, Oktenli C.. Therapeutical potential of autologous peripheral blood mononuclear cell transplantation in patients with type 2 diabetic critical limb ischemia. J Diabetes Complications 2012;26:29–33. [DOI] [PubMed] [Google Scholar]
- 118. Losordo DW, Kibbe MR, Mendelsohn F, Marston W, Driver VR, Sharafuddin M, Teodorescu V, Wiechmann BN, Thompson C, Kraiss L, Carman T, Dohad S, Huang P, Junge CE, Story K, Weistroffer T, Thorne TM, Millay M, Runyon JP, Schainfeld R.. A randomized, controlled pilot study of autologous CD34+ cell therapy for critical limb ischemia. Circ Cardiovasc Interv 2012;5:821–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Perin EC, Silva G, Gahremanpour A, Canales J, Zheng Y, Cabreira-Hansen MG, Mendelsohn F, Chronos N, Haley R, Willerson JT, Annex BH.. A randomized, controlled study of autologous therapy with bone marrow-derived aldehyde dehydrogenase bright cells in patients with critical limb ischemia. Catheter Cardiovasc Interv 2011;78:1060–1067. [DOI] [PubMed] [Google Scholar]
- 120. Rajagopalan S, Mohler E, Lederman RJ, Saucedo J, Mendelsohn FO, Olin J, Blebea J, Goldman C, Trachtenberg JD, Pressler M, Rasmussen H, Annex BH, Hirsch AT.. Regional angiogenesis with vascular endothelial growth factor (VEGF) in peripheral arterial disease: design of the RAVE trial. Am Heart J 2003;145:1114–1118. [DOI] [PubMed] [Google Scholar]
- 121. Belch J, Hiatt WR, Baumgartner I, Driver IV, Nikol S, Norgren L, Van Belle E.. Effect of fibroblast growth factor NV1FGF on amputation and death: a randomised placebo-controlled trial of gene therapy in critical limb ischaemia. Lancet 2011;377:1929–1937. [DOI] [PubMed] [Google Scholar]
- 122. Powell RJ, Simons M, Mendelsohn FO, Daniel G, Henry TD, Koga M, Morishita R, Annex BH.. Results of a double-blind, placebo-controlled study to assess the safety of intramuscular injection of hepatocyte growth factor plasmid to improve limb perfusion in patients with critical limb ischemia. Circulation 2008;118:58–65. [DOI] [PubMed] [Google Scholar]
- 123. Creager MA, Olin JW, Belch JJF, Moneta GL, Henry TD, Rajagopalan S, Annex BH, Hiatt WR.. Effect of hypoxia-inducible factor-1alpha gene therapy on walking performance in patients with intermittent claudication. Circulation 2011;124:1765–1773. [DOI] [PubMed] [Google Scholar]
- 124. Grossman PM, Mendelsohn F, Henry TD, Hermiller JB, Litt M, Saucedo JF, Weiss RJ, Kandzari DE, Kleiman N, Anderson RD, Gottlieb D, Karlsberg R, Snell J, Rocha-Singh K.. Results from a phase II multicenter, double-blind placebo-controlled study of Del-1 (VLTS-589) for intermittent claudication in subjects with peripheral arterial disease. Am Heart J 2007;153:874–880. [DOI] [PubMed] [Google Scholar]
- 125. Misra V, Ritchie MM, Stone LL, Low WC, Janardhan V.. Stem cell therapy in ischemic stroke: role of IV and intra-arterial therapy. Neurology 2012;79:S207–S212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Wu J, Okamura D, Li M, Suzuki K, Luo C, Ma L, He Y, Li Z, Benner C, Tamura I, Krause MN, Nery JR, Du T, Zhang Z, Hishida T, Takahashi Y, Aizawa E, Kim NY, Lajara J, Guillen P, Campistol JM, Esteban CR, Ross PJ, Saghatelian A, Ren B, Ecker JR, Izpisua Belmonte JC.. An alternative pluripotent state confers interspecies chimaeric competency. Nature 2015;521:316–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Jansen Of Lorkeers SJ, Doevendans PA, Chamuleau SAJ.. All preclinical trials should be registered in advance in an online registry. Eur J Clin Invest 2014;44:891–892. [DOI] [PubMed] [Google Scholar]
- 128. Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG.. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 2010;8:e1000412.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Jones SP, Tang X-L, Guo Y, Steenbergen C, Lefer DJ, Kukreja RC, Kong M, Li Q, Bhushan S, Zhu X, Du J, Nong Y, Stowers HL, Kondo K, Hunt GN, Goodchild TT, Orr A, Chang CC, Ockaili R, Salloum FN, Bolli R.. The NHLBI-sponsored Consortium for preclinicAl assESsment of cARdioprotective therapies (CAESAR): a new paradigm for rigorous, accurate, and reproducible evaluation of putative infarct-sparing interventions in mice, rabbits, and pigs. Circ Res 2015;116:572–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Bianconi E, Piovesan A, Facchin F, Beraudi A, Casadei R, Frabetti F, Vitale L, Pelleri MC, Tassani S, Piva F, Perez-Amodio S, Strippoli P, Canaider S.. An estimation of the number of cells in the human body. Ann Hum Biol 2013;40:301–4460. [DOI] [PubMed] [Google Scholar]
- 131. Liu J, Laksman Z, Backx PH.. The electrophysiological development of cardiomyocytes. Adv Drug Deliv Rev 2015;96:253–273. [DOI] [PubMed] [Google Scholar]
- 132. Fallahiarezoudar E, Ahmadipourroudposht M, Idris A, Mohd Yusof N, Mohd N, Mohd Yusof N.. A review of: application of synthetic scaffold in tissue engineering heart valves. Mater Sci Eng C 2015;48:556–565. [DOI] [PubMed] [Google Scholar]
- 133. Jana S, Lerman A.. Bioprinting a cardiac valve. Biotechnol Adv 2015;33:1503–1521. [DOI] [PubMed] [Google Scholar]
- 134. Namiri M, Ashtiani MK, Mashinchian O, Hasani-Sadrabadi MM, Mahmoudi M, Aghdami N, Baharvand H.. Engineering natural heart valves: possibilities and challenges. J Tissue Eng Regen Med 2016;1:1–9. [DOI] [PubMed] [Google Scholar]
- 135. Tudorache I, Horke A, Cebotari S, Sarikouch S, Boethig D, Breymann T, Beerbaum P, Bertram H, Westhoff-Bleck M, Theodoridis K, Bobylev D, Cheptanaru E, Ciubotaru A, Haverich A.. Decellularized aortic homografts for aortic valve and aorta ascendens replacement. Eur J Cardio-Thoracic Surg 2016;50:89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Neofytou E, O’brien CG, Couture LA, Wu JC, Brien CGO, Couture LA, Wu JC.. Hurdles to clinical translation of human induced pluripotent stem cells. J Clin Invest 2015;125:2551–2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Mathur A, Ma Z, Loskill P, Jeeawoody S, Healy KE.. In vitro cardiac tissue models: current status and future prospects. Adv Drug Deliv Rev 2015;96:203–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Stillitano F, Turnbull IC, Karakikes I, Nonnenmacher M, Backeris P, Hulot JS, Kranias EG, Hajjar RJ, Costa KD.. Genomic correction of familial cardiomyopathy in human engineered cardiac tissues. Eur Heart J 2016;103:472–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Terzic A, Behfar A, Filippatos G.. Clinical development plan for regenerative therapy in heart failure. Eur J Heart Fail 2016;18:142–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Bayon Y, Vertès AA, Ronfard V, Egloff M, Snykers S, Salinas GF, Thomas R, Girling A, Lilford R, Clermont G, Kemp P.. Translating cell-based regenerative medicines from research to successful products: challenges and solutions. Tissue Eng Part B Rev 2014;20:246–256. [DOI] [PubMed] [Google Scholar]
- 141. Eaker S, Armant M, Brandwein H, Burger S, Campbell A, Carpenito C, Clarke D, Fong T, Karnieli O, Niss K, Van’t Hof W, Wagey R.. Concise review: guidance in developing commercializable autologous/patient-specific cell therapy manufacturing. Stem Cells Transl Med 2013;2:871–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Abbasalizadeh S, Baharvand H.. Technological progress and challenges towards cGMP manufacturing of human pluripotent stem cells based therapeutic products for allogeneic and autologous cell therapies. Biotechnol Adv 2013;31:1600–1623. [DOI] [PubMed] [Google Scholar]
- 143. Freyman T, Polin G, Osman H, Crary J, Lu M, Cheng L, Palasis M, Wilensky RL.. A quantitative, randomized study evaluating three methods of mesenchymal stem cell delivery following myocardial infarction. Eur Heart J 2006;27:1114–1122. [DOI] [PubMed] [Google Scholar]
- 144. Hou D, Youssef EAS, Brinton TJ, Zhang P, Rogers P, Price ET, Yeung AC, Johnstone BH, Yock PG, March KL.. Radiolabeled cell distribution after intramyocardial, intracoronary, and interstitial retrograde coronary venous delivery: implications for current clinical trials. Circulation 2005;112:I150–I156. [DOI] [PubMed] [Google Scholar]
- 145. van der Spoel TIG, Vrijsen KR, Koudstaal S, Sluijter JPG, Nijsen JFW, de Jong HW, Hoefer IE, Cramer M-JM, Doevendans PA, van Belle E, Chamuleau SAJ.. Transendocardial cell injection is not superior to intracoronary infusion in a porcine model of ischaemic cardiomyopathy: a study on delivery efficiency. J Cell Mol Med 2012;16:2768–2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. van den Akker F, Feyen DAM, van den Hoogen P, van Laake LW, van Eeuwijk ECM, Hoefer I, Pasterkamp G, Chamuleau SAJ, Grundeman PF, Doevendans PA, Sluijter JPG.. Intramyocardial stem cell injection: go(ne) with the flow. Eur Heart J 2017;38:184–186. [DOI] [PubMed] [Google Scholar]
- 147. Gyöngyösi M, Wojakowski W, Lemarchand P, Lunde K, Tendera M, Bartunek J, Marban E, Assmus B, Henry TD, Traverse JH, Moyé LA, Sürder D, Corti R, Huikuri H, Miettinen J, Wöhrle J, Obradovic S, Roncalli J, Malliaras K, Pokushalov E, Romanov A, Kastrup J, Bergmann MW, Atsma DE, Diederichsen A, Edes I, Benedek I, Benedek T, Pejkov H, Nyolczas N, Pavo N, Bergler-Klein J, Pavo IJ, Sylven C, Berti S, Navarese EP, Maurer G.. Meta-analysis of cell-based CaRdiac stUdiEs (ACCRUE) in patients with acute myocardial infarction based on individual patient data. Circ Res 2015;116:1346–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Feyen D, Gaetani R, Liu J, Noort W, Martens A, Den Ouden K, Doevendans PA, Sluijter JPG.. Increasing short-term cardiomyocyte progenitor cell (CMPC) survival by necrostatin-1 did not further preserve cardiac function. Cardiovasc Res 2013;99:83–91. [DOI] [PubMed] [Google Scholar]
- 149. Vrtovec B, Poglajen G, Lezaic L, Sever M, Socan A, Domanovic D, Cernelc P, Torre-Amione G, Haddad F, Wu JC.. Comparison of transendocardial and intracoronary CD34+ cell transplantation in patients with nonischemic dilated cardiomyopathy. Circulation 2013;128:S42–S49. [DOI] [PubMed] [Google Scholar]
- 150. Costa KD. Decellularized scaffold hydrogel materials for MI treatment. J Am Coll Cardiol 2016;67:1087–1090. [DOI] [PubMed] [Google Scholar]
- 151. Stanley K. Design of randomized controlled trials. Circulation 2007;115:1164–1169. [DOI] [PubMed] [Google Scholar]
- 152. Banovic M, Loncar Z, Behfar A, Vanderheyden M, Beleslin B, Zeiher A, Metra M, Terzic A, Bartunek J.. Endpoints in stem cell trials in ischemic heart failure. Stem Cell Res Ther 2015;6:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Hare JM, Bolli R, Cooke JP, Gordon DJ, Henry TD, Perin EC, March KL, Murphy MP, Pepine CJ, Simari RD, Skarlatos SI, Traverse JH, Willerson JT, Szady AD, Taylor DA, Vojvodic RW, Yang PC, Moyé LA; Cardiovascular Cell Therapy Research Network. Phase II clinical research design in cardiology: learning the right lessons too well: observations and recommendations from the Cardiovascular Cell Therapy Research Network (CCTRN). Circulation 2013;127:1630–1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. De Groot V, Beckerman H, Lankhorst GJ, Bouter LM.. How to measure comorbidity: a critical review of available methods. J Clin Epidemiol 2003;56:221–229. [DOI] [PubMed] [Google Scholar]
- 155. Turner LGL, Knoepfler PPS, Chirba M, Garfield S, Connolly R, O’brien T, Flaherty G, Knoepfler PPS, Lau D, Ogbogu U, Taylor B, Stafinski T, Menon D, Caulfield T, McAllister TN, Audley D, L’heureux N, Ogbogu U, Rachul C, Caulfield T, Regenberg AC, Hutchinson LA, Schanker B, Mathews DJ, Turner LGL, Turner LGL.. Selling stem cells in the USA: assessing the direct-to-consumer industry. Cell Stem Cell 2016;1:233–272. [DOI] [PubMed] [Google Scholar]