Abstract
Background
Interferon-free treatment can achieve higher sustained virological response (SVR) rates, even in patients in whom hepatitis C virus (HCV) could not be eradicated in the interferon treatment era. Immune restoration in the liver is occasionally associated with HCV infection. We examined the safety and effects of interferon-free regimens on HCV patients with autoimmune liver diseases.
Results
All 7 HCV patients with autoimmune hepatitis (AIH) completed treatment and achieved SVR. Three patients took prednisolone (PSL) at baseline, and 3 did not take PSL during interferon-free treatment. In one HCV patient with AIH and cirrhosis, PSL were not administered at baseline, but she needed to take 40 mg/day PSL at week 8 for liver dysfunction. She also complained back pain and was diagnosed with vasospastic angina by coronary angiography at week 11. However, she completed interferon-free treatment. All 5 HCV patients with primary biliary cholangitis (PBC) completed treatment and achieved SVR. Three of these HCV patients with PBC were treated with UDCA during interferon-free treatment.
Conclusions
Interferon-free regimens could result in higher SVR rates in HCV patients with autoimmune liver diseases. As interferon-free treatment for HCV may have an effect on hepatic immunity and activity of the autoimmune liver diseases, careful attention should be paid to unexpected adverse events in their treatments.
Methods
Total 12 patients with HCV and autoimmune liver diseases [7 AIH and PBC], who were treated with interferon-free regimens, were retrospectively analyzed.
Keywords: hepatitis C virus, direct-acting antivirals, autoimmune hepatitis, primary biliary cholangitis, sustained virological response
INTRODUCTION
Hepatitis C virus (HCV) causes chronic and persistent infection and is an important etiologic factor of advanced fibrosis/cirrhosis and hepatocellular carcinoma (HCC) [1]. Eradication of HCV could reduce the risk of the occurrence of HCC and liver-related deaths as well as liver-unrelated deaths, although it is difficult to eliminate HCV [2]. Interferon-free treatment can achieve higher sustained virological response (SVR) rates, even in patients in whom HCV could not be eradicated in the interferon treatment era [3].
Autoimmune hepatitis (AIH) and primary biliary cholangitis (PBC) are representative autoimmune liver diseases [4, 5]. AIH possesses a chronic active hepatitis histologically with autoimmune features and poor prognosis without immune suppressive therapies [4, 6]. PBC is diagnosed based on the presence of an antimitochondrial antibody (AMA), elevated cholestatic liver enzyme and/or histologically by chronic non-suppurative destructive cholangitis (CNSDC) [5, 7].
Patients with autoimmune liver diseases and hepatitis C virus (HCV) infection are occasionally observed [8, 9]. Patients with autoimmune hepatitis (AIH) and HCV infection often have advanced liver diseases at initial clinical and histological assessments [8]. PBC diagnosis in HCV patients is difficult and usually delayed [9]. Those with HCV and PBC do not have better outcomes than those with only HCV [9].
Immune restoration in the liver is occasionally associated with HCV infection [10, 11]. Studies using interferon-free regimens demonstrated an immune restoration of immunologic responses after HCV clearance [12–14]. Thus, HCV clearance has effects on the human immunologic response. HCV patients with autoimmune liver diseases could not be treated by interferon-including regimens because such regimens were contraindicated in these patients in the interferon era [15]. In the present study, we retrospectively examined the safety and effects of interferon-free regimens on HCV-patients with autoimmune liver diseases.
RESULTS
Treatment response in HCV patients with AIH
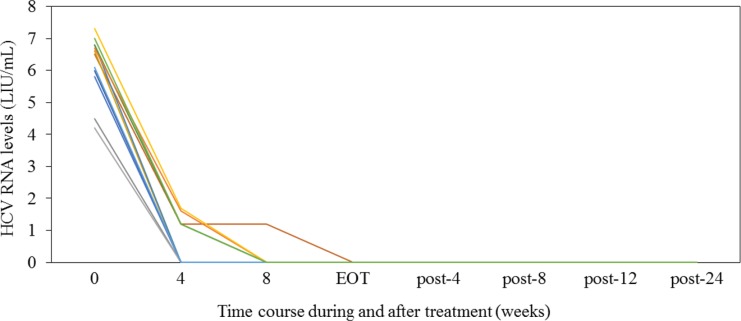
All 12 patients with autoimmune liver diseases completed treatment and achieved SVR (Figures 1 and 2). In the 7 patients with AIH, 4 and 3 were HCV genotypes (GTs) 1 and 2, respectively, and 3, 1 and 3 patients were treated with SOF/LDV, DCV/ASV and SOF/RBV, respectively. In 50% (2/4) of HCV GT-1 and 33% (1/3) of HCV GT-2 patients, RVR was achieved (Table 1 and Figure 1). Four patients with AIH and non-RVR achieved HCV RNA negativity at week 8. Three patients (nos. 6, 7 and 8) took prednisolone (PSL) at baseline, and 4 (nos. 9, 10, 11 and 12) did not take PSL at baseline.
Figure 1. Serum HCV RNA levels (LIU/mL) during and after interferon-free treatment in the present study.
EOT, end of the treatment response.
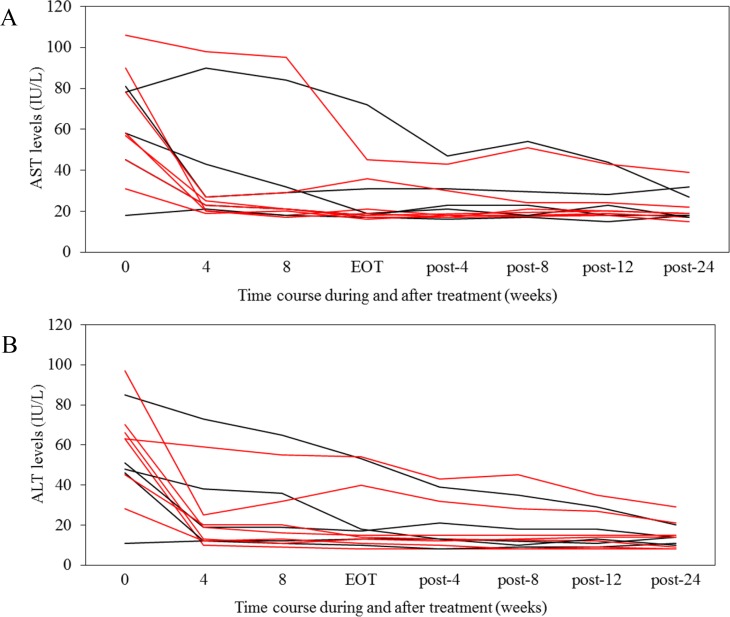
Figure 2. Serum transaminase levels during and after interferon free treatment.
(A) Aspartate transaminase (AST) (IU/L). (B) Alanine transaminase (ALT) (IU/L). AIH, red line; PBC, black line. EOT, end of the treatment response.
Table 1. Patient characteristics.
| No. | PBC/AIH | Age (y) /Sex | HCV GTs | HCV RNA (LIU/mL) | PH of IFNs | BMI (kg /m2) | Liver biopsy findings | LS (kPa) | Concomitant Drugs: UDCA (mg/d) /PSL (mg/d) /Aza (mg/d) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | PBC | 58/F | 1b | 6 | Naïve | 20.7 | N.D. | 6.6 | 600/0/0 |
| 2 | PBC | 79/F | 1b | 6.5 | Naïve | 16.7 | N.D. | 10.5 | 0/0/0 |
| 3 | PBC | 80/M | 1b | 4.5 | Naïve | 19.4 | N.D. | 7.7 | 600/0/0 |
| 4 | PBC | 62/F | 1b | 6.6 | Naïve | 21.7 | N.D. | 6.2 | 0/0/0 |
| 5 | PBC | 57/F | 1b | 6.8 | Naïve | 27.1 | Stage 2 CNSDC+ Vanishing bile duct (+) | 10.4 | 900/0/0 |
| 6 | AIH | 77/F | 1b | 6.8 | Naïve | 24.5 | F2/A3 | N.D. | 900/5/0 |
| 7 | AIH | 72/F | 1b | 5.8 | Naïve | 21.6 | F3/A3 | N.D. | 600/10/0 |
| 8 | AIH | 69/F | 1b | 6.7 | Naïve | 22.9 | F2/A2 | 9.3 | 600/5/25 |
| 9 | AIH | 59/F | 1b | 4.2 | Naïve | 22.8 | F4/A3 | N.D. | 0/40(8W-)/0 |
| 10 | AIH | 71/F | 2a | 7.3 | Naïve | 21 | N.D. | N.D. | 600/0/0 |
| 11 | AIH | 62/M | 2a | 6.1 | Naïve | 21.3 | F2/A3 | 15.1 | 600/0/0 |
| 12 | AIH | 73/M | 2b | 7 | PR-Null | 23.1 | F3/A3 | 12.6 | 0/0/0 |
PBC, primary biliary cholangitis; AIH, autoimmune hepatitis; GTs, genotypes; PH of IFNs: past medical history of interferon treatment, BMI, body mass index; LS, liver stiffness; UDCA, ursodeoxycholic acid; PSL, prednisone; Aza, azathioprine; N.D., not done
| No. | ANA (−fold) | AMA M2 (U/mL) | ASMA (−fold) | LKM-1 | IgG (mg/dL) | IgM (mg/dL) | AST (IU/L) | ALT (IU/L) />500 | PLT (× 104/μL) | Tx |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Neg | 156 | Neg | Neg | 2946 | 368 | 18 | 10/− | 17.2 | SOF/LDV |
| 2 | Neg | 16.2 | Neg | Neg | 1518 | 115 | 74 | 44/− | 9.2 | SOF/LDV |
| 3 | 80 | 10.8 | Neg | Neg | 1953 | 82 | 78 | 85/− | 17 | SOF/LDV |
| 4 | Neg | 141 | Neg | Neg | 1486 | 280 | 45 | 51/− | 19 | SOF/LDV |
| 5 | Neg | 218 | Neg | Neg | 1615 | 101 | 63 | 68/− | 13.8 | OMV/PTV/r |
| 6 | 160 | Neg | Neg | Neg | 1565 | 117 | 77 | 62/− | 9.3 | DCV/ASV |
| 7 | 80 | Neg | Neg | Neg | 2308 | 248 | 43 | 44/− | 20.2 | SOF/LDV |
| 8 | 160 | Neg | Neg | Neg | 1947 | 36 | 32 | 31/− | 9.4 | SOF/LDV |
| 9 | >1280 | Neg | Neg | Neg | 4304 | 127 | 107 | 61/− | 10.9 | SOF/LDV |
| 10 | Neg | Neg | Neg | Neg | 1636 | 229 | 88 | 96/+ | 8.3 | SOF/RBV |
| 11 | 640 | Neg | Neg | Neg | 2208 | 160 | 50 | 56/+ | 17.7 | SOF/RBV |
| 12 | 80 | Neg | Neg | 63 | 2465 | 86 | 84 | 115/− | 14.3 | SOF/RBV |
ANA, anti-nuclear antibody; AMA, anti-mitochondrial antibody; ASMA, anti-smooth muscle antibody; LKM-1, anti-liver/kidney microsome type 1 antibody; Ig, immunoglobulin; AST, aspartate aminotransferase; ALT, alanine aminotransferase; PLT, platelets; Tx, DAA treatment for HCV; Neg, negative; +/−, with or without experience; SOF, sofosbuvir; LDV, ledipasvir; OBV/PTV/r, ombitasvir/paritaprevir/ritonavir; DCV/ASV, daclatasvir/asunaprevir; RBV, ribavirin.
In a female HCV GT-1-patient with AIH and cirrhosis (no. 9), PSL was not administered at baseline, but she needed to take 40 mg/day PSL at week 8 for liver dysfunction after HCV treatment. She complained of back pain and was diagnosed with vasospastic angina by coronary angiography at 11 weeks but completed her treatment (Figure 3).
Figure 3. Electrocardiograms (ECGs) of patient no. 9.
59-year female with chronic hepatitis (F4/A3), HCV and autoimmune liver diseases. She had hypertension. (A)Asymptomatic. (B) Backpain. (C) Asymptomatic. (D) Backpain.
Before treatment, in 7 HCV patients with AIH, 6 and 6 patients had abnormal aspartate aminotransferase (AST) and alanine aminotransferase (ALT) (more than 40 IU/L), respectively. At week 24 post-treatment, in all 7 of these patients, both AST and ALT were normalized.
Treatment response in HCV patients with PBC
In 5 HCV GT-1 patients with PBC, 4 and 1 were treated with SOF/LDV and OBV/PTV/r, respectively, resulting in 75% (3/4) and 100% (1/1) RVR. One non-RVR patient achieved HCV RNA negativity at week 12. Three of 5 patients were treated with UDCA during HCV treatment (Table 1 and Figure 1).
Before treatment, in 5 HCV patients with PBC, 4 and 4 patients had abnormal AST and ALT (more than 40 IU/L), respectively. At week 24 post-treatment, in all 5 of these patients, both AST and ALT were normalized.
Case presentation of a HCVGT-1 patient with AIH (no. 9)
Before commencement of SOF/LDV, she felt general fatigue, and her liver function tests showed ALT 61 IU/L, total bilirubin (T. Bil) 1.7 mg/dL, prothrombin time (PT) 47%, and immunoglobulin (Ig) G 4301 mg/dL. At week 8, co-administration of PSL was started for liver dysfunction (ALT 55 IU/L, T. Bil 2.2 mg/dL, PT 52%, and IgG 3743 mg dL). At week 11, back pain appeared, and electrocardiogram (ECG) showed ST-segment depression. She was diagnosed with vasospastic angina by coronary angiography but completed her treatment (Figure 3). Finally, SVR24 was achieved (ALT 29 IU/L, T. Bil 0.9 mg/dL, PT 104%, and IgG 1629 mg/dL). At present, she takes UDCA 600 mg/day and PSL 15 mg/day, and she is well.
DISCUSSION
In 9 HCV GT-1-patients with autoimmune liver diseases, RVR rates, end of treatment response (EOT) rates and SVR rates were 66.7, 100 and 100%, respectively. In 3HCV GT-2-patients with autoimmune liver diseases, RVR rates, EOT rates and SVR rates were 33.3, 100 and 100%, respectively. The present study found higher SVR rates in HCV patients with autoimmune liver diseases.
Concerning safety, in one patient with AIH, PSL was needed for liver dysfunction during the treatment of SOF/LDV. If liver dysfunction is due to autoimmune liver diseases, it may be important to treat autoimmune liver diseases before or during interferon-free treatment for HCV. Unexpectedly, in this case, vasospastic angina also developed as a complication during the treatment of SOF/LDV. Recently, Nirei et al. [16] reported ventricular tachycardia as a complication of SOF/LDV treatment. We do not know the association between the use of SOF/LDV and vasospastic angina.
Vento et al. [10] reported two patients with HCV who developed fulminant liver failure after stopping chemotherapy, indicating an immune-mediated mechanism for hepatocyte damage in HCV infection. These patients with liver failure seem to have developed immune restoration in the liver after stopping chemotherapy. HCV-positive mothers with increased ALT in the post-partum period, also presented a significant decrease in serum HCV RNA in the post-delivery period, and this event was concomitant with an increase in Th1 cytokine levels [11].
In the present study, one patients with AIH (no. 12) was classified into the AIH type 2, which is positive for anti-liver/kidney microsome type 1 (anti-LKM1) antibody. It has been reported that anti-LKM-1 was occasionally positive in patients with chronic active hepatitis C [17]. Further studies about the effects of DAAs on this type AIH will be needed.
Restoration of immunologic responses after HCV clearance with interferon-free treatment has also been reported [12–14]. Hepatitis B reactivation during or after interferon-free treatment for HCV may be associated with the restoration of adaptive and innate immune responses [12–14, 18, 19]. Thus, interferon-free treatment for HCV may have an effect on hepatic immunity and activity of autoimmune liver diseases. Exacerbation of AIH and PBC during the interferon-including regimens for chronic HCV infection has been observed [20–22]. Although interferon-free regimens seem safer than interferon-including regimens in patients with autoimmune liver diseases, clinician should pay a special attention to acute exacerbation of liver diseases and unexpected adverse events.
CONCLUSIONS
The interferon-free regimens were relatively safe and effective for HCV-infected patients with autoimmune liver diseases. Some patients with active AIH may require immune therapy before HCV treatment. Close monitoring and careful attention are needed to handle unexpected adverse events.
PATIENTS AND METHODS
Patients
A total of 467 HCV-infected patients, some of whom were described previously [23–25], started treatment with interferon-free treatment by 2016 at the Department of Gastroenterology, Chiba University Hospital. Among them, 12 patients with autoimmune liver diseases (7 AIH and 5 PBC) were analyzed [25% male, mean age 68±8.4 years, 92% treatment-naive, 75% GT-1b, 33% cirrhosis] (Table 1). This retrospective study was approved by Ethics Committee of Chiba University School of Medicine (numbers 1462 and 1753). Participants in the study were recruited from Chiba University Hospital. This study was conducted in accordance with the Declaration of Helsinki.
Diagnosis of AIH and PBC
AIH is diagnosed by the international autoimmune hepatitis criteria for the diagnosis of autoimmune hepatitis [26, 27]. PBC was diagnosed based on the presence of AMA, elevated cholestatic liver enzyme and/or histologically by CNSDC as described previously [5, 7].
Treatment protocol
In total, 9 HCV GT-1b patients were included: 7, 1 and 1 were treated with sofosbuvir/ledipasvir (SOF/LDV) for 12 weeks, ombitasvir/paritaprevir/ritonavir (OBV/PTV/r) for 12 weeks and daclatasvir/asunaprevir (DCV/ASV) for 24 weeks, respectively. All 3 HCV GT-2 patients were treated with SOF/ribavirin (RBV) for 12 weeks (Table 1). Before the use of OBV/PTV/r or DCV/ASV, HCV NS5A resistance associated variants (RAVs) were excluded as described previously [23].
Laboratory tests
Laboratory tests were measured by standard laboratory techniques at a central laboratory in Chiba University Hospital. Blood samples were obtained at the baseline, at weeks 4, 8 and 12 of treatment, and then 4, 8, 12 and 24 weeks after the end of treatment [24].
Measurement of HCV RNA
HCV RNA was measured by COBAS TaqMan HCV assay version 2.0 (Roche Diagnostics, Tokyo, Japan), with a lower limit of quantification of 15 IU/mL. We used the definition of rapid virological response (RVR), consisting of HCV RNA <15 IU/mL at week 4 according to the 2014 EASL guidelines. SVR was defined as negativity of HCV RNA at 24 weeks after stopping treatment. HCV genotyping was performed as previously described [24].
Statistical analysis
Data are expressed as the mean ± standard deviation (SD). Statistical analyses were performed by univariate analyses using Student’s t-test or the chi-square test. p < 0.05 was considered statistically significant. Statistical analysis was performed using Excel Statistics program for Windows 2010 (SSRI, Tokyo, Japan) and DA Stats software (O. Nagata, Nifty Serve: PAF01644).
Acknowledgments
We thank Dr. Makoto Arai, Prof. Osamu Yokosuka and all other medical staffs for patients’ care.
Footnotes
CONFLICTS OF INTEREST
Tatsuo Kanda received research grants from AbbVie, MSD, Sysmex and Chugai Pharmaceutical. Naoya Kato received grants from AbbVie, MSD, Sysmex, Chugai Pharmaceutical, Gilead Sciences and BMS. The founding sponsors played no role in the study design, data collection, analyses, or interpretation, writing of the manuscript, or in the decision to publish the results. The other authors have declared no conflicts of interest.
FUNDING
This work was partially supported by grants from the Japan Agency for Medical Research and Development (AMED).
REFERENCES
- 1.Westbrook RH, Dusheiko G. Natural history of hepatitis C. J Hepatol. 2014;61:S58–S68. doi: 10.1016/j.jhep.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 2.Kanda T, Imazeki F, Yokosuka O. New antiviral therapies for chronic hepatitis C. Hepatol Int. 2010;4:548–561. doi: 10.1007/s12072-010-9193-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kanda T. Interferon-free treatment for HCV-infected patients with decompensated cirrhosis. Hepatol Int. 2017;11:38–44. doi: 10.1007/s12072-016-9749-y. [DOI] [PubMed] [Google Scholar]
- 4.Takahashi A, Arinaga-Hino T, Ohira H, Torimura T, Zeniya M, Abe M, Yoshizawa K, Takaki A, Suzuki Y, Kang JH, Nakamoto N, Fujisawa T, Yonemoto K, et al. Autoimmune hepatitis in Japan: trends in a nationwide survey. J Gastroenterol. 2017;52:631–640. doi: 10.1007/s00535-016-1267-0. [DOI] [PubMed] [Google Scholar]
- 5.Beuers U, Gershwin ME, Gish RG, Invernizzi P, Jones DE, Lindor K, Ma X, Mackay IR, Parés A, Tanaka A, Vierling JM, Poupon R. Changing nomenclature for PBC: From ‘cirrhosis’ to ‘cholangitis’. Hepatology. 2015;62:1620–1622. doi: 10.1002/hep.28140. [DOI] [PubMed] [Google Scholar]
- 6.Kumagai J, Kanda T, Yasui S, Haga Y, Sasaki R, Nakamura M, Wu S, Nakamoto S, Arai M, Iino Y, Yokosuka O. Autoimmune hepatitis following drug-induced liver injury in an elderly patient. Clin J Gastroenterol. 2016;9:156–159. doi: 10.1007/s12328-016-0648-5. [DOI] [PubMed] [Google Scholar]
- 7.Kanda T, Yokosuka O, Imazeki F, Saisho H. Bezafibrate treatment: a new medical approach for PBC patients? J Gastroenterol. 2003;38:573–578. doi: 10.1007/s00535-002-1102-7. [DOI] [PubMed] [Google Scholar]
- 8.Rigopoulou EI, Zachou K, Gatselis N, Koukoulis GK, Dalekos GN. Autoimmune hepatitis in patients with chronic HBV and HCV infections: patterns of clinical characteristics, disease progression and outcome. Ann Hepatol. 2013;13:127–135. 2014. [PubMed] [Google Scholar]
- 9.Rigopoulou EI, Zachou K, Gatselis NK, Papadamou G, Koukoulis GK, Dalekos GN. Primary biliary cirrhosis in HBV and HCV patients: Clinical characteristics and outcome. World J Hepatol. 2013;5:577–583. doi: 10.4254/wjh.v5.i10.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vento S, Cainelli F, Mirandola F, Cosco L, Di Perri G, Solbiati M, Ferraro T, Concia E. Fulminant hepatitis on withdrawal of chemotherapy in carriers of hepatitis C virus. Lancet. 1996;347:92–93. doi: 10.1016/s0140-6736(96)90212-3. [DOI] [PubMed] [Google Scholar]
- 11.Ruiz-Extremera A, Muñoz-Gámez JA, Abril-Molina A, Salmerón-Ruiz MA, Muñoz-de-Rueda P, Pavón-Castillero EJ, Quiles-Pérez R, Carazo A, Gila A, Jimenez-Ruiz SM, Casado J, Martín AB, Sanjuán-Núñez L, et al. Variation of transaminases, HCV-RNA levels and Th1/Th2 cytokine production during the post-partum period in pregnant women with chronic hepatitis C. PLoS One. 2013;8:e75613. doi: 10.1371/journal.pone.0075613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burchill MA, Golden-Mason L, Wind-Rotolo M, Rosen HR. Memory re-differentiation and reduced lymphocyte activation in chronic HCV-infected patients receiving direct-acting antivirals. J Viral Hepat. 2015;22:983–991. doi: 10.1111/jvh.12465. [DOI] [PubMed] [Google Scholar]
- 13.Werner JM, Adenugba A, Protzer U. Immune Reconstitution After HCV Clearance With Direct Antiviral Agents: Potential Consequences for Patients With HCC? Transplantation. 2017;101:904–909. doi: 10.1097/TP.0000000000001606. [DOI] [PubMed] [Google Scholar]
- 14.Carlton-Smith C, Holmes JA, Naggie S, Lidofsky A, Lauer GM, Kim AY, Chung RT, of the ACTG A5327 study group IFN-free therapy is associated with restoration of type I IFN response in HIV-1 patients with acute HCV infection who achieve SVR. J Viral Hepat. 2017 Nov;29 doi: 10.1111/jvh.12836. https://doi.org/10.1111/jvh.12836 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Omata M, Kanda T, Yu ML, Yokosuka O, Lim SG, Jafri W, Tateishi R, Hamid SS, Chuang WL, Chutaputti A, Wei L, Sollano J, Sarin SK, et al. APASL consensus statements and management algorithms for hepatitis C virus infection. Hepatol Int. 2012;6:409–435. doi: 10.1007/s12072-012-9342-y. [DOI] [PubMed] [Google Scholar]
- 16.Nirei K, Nakamura H, Matsuoka S, Yamana Y, Yoda S, Hirayama A, Moriyama M. Ventricular Tachycardia as a Complication of Ledipasvir and Sofosbuvir Treatment for HCV Infection. Intern Med. 2017;56:787–790. doi: 10.2169/internalmedicine.56.7948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishioka M, Morshed SA, Kono K, Himoto T, Parveen S, Arima K, Watanabe S, Manns MP. Frequency and significance of antibodies to P450IID6 protein in Japanese patients with chronic hepatitis C. J Hepatol. 1997;26:992–1000. doi: 10.1016/s0168-8278(97)80107-9. [DOI] [PubMed] [Google Scholar]
- 18.Holmes JA, Yu ML, Chung RT. Hepatitis B reactivation during or after direct acting antiviral therapy - implication for susceptible individuals. Expert Opin Drug Saf. 2017;16:651–672. doi: 10.1080/14740338.2017.1325869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vionnet J, Pascual M, Testoni B, Combet C, Godat S, Vijgen S, Aubert V, Rubbia-Brandt L, Zoulim F, Moradpour D. Late hepatitis B reactivation following DAA-based treatment of recurrent hepatitis C in an anti-HBc-positive liver transplant recipient. Hepatology. 2017 Sep;16 doi: 10.1002/hep.29528. https://doi.org/10.1002/hep.29528 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Shindo M, Di Bisceglie AM, Hoofnagle JH. Acute exacerbation of liver disease during interferon alfa therapy for chronic hepatitis C. Gastroenterology. 1992;102:1406–1408. [PubMed] [Google Scholar]
- 21.Maeda T, Onishi S, Miura T, Iwamura S, Tomita A, Saibara T, Yamamoto Y. Exacerbation of primary biliary cirrhosis during interferon-alpha 2b therapy for chronic active hepatitis C. Dig Dis Sci. 1995;40:1226–1230. doi: 10.1007/BF02065528. [DOI] [PubMed] [Google Scholar]
- 22.D’Amico E, Paroli M, Fratelli V, Palazzi C, Barnaba V, Callea F, Consoli G. Primary biliary cirrhosis induced by interferon-alpha therapy for hepatitis C virus infection. Dig Dis Sci. 1995;40:2113–2116. doi: 10.1007/BF02208992. [DOI] [PubMed] [Google Scholar]
- 23.Kanda T, Yasui S, Nakamura M, Suzuki E, Arai M, Haga Y, Sasaki R, Wu S, Nakamoto S, Imazeki F, Yokosuka O. Daclatasvir plus Asunaprevir Treatment for Real-World HCV Genotype 1-Infected Patients in Japan. Int J Med Sci. 2016;13:418–423. doi: 10.7150/ijms.15519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kanda T, Yasui S, Nakamura M, Suzuki E, Arai M, Ooka Y, Ogasawara S, Chiba T, Saito T, Haga Y, Takahashi K, Sasaki R, Wu S, et al. Real-World Experiences with the Combination Treatment of Ledipasvir plus Sofosbuvir for 12 Weeks in HCV Genotype 1-Infected Japanese Patients: Achievement of a Sustained Virological Response in Previous Users of Peginterferon plus Ribavirin with HCV NS3/4A Inhibitors. Int J Mol Sci. 2017;18:E906. doi: 10.3390/ijms18050906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kanda T, Nakamura M, Yasui S, Haga Y, Tawada A, Suzuki E, Ooka Y, Takahashi K, Sasaki R, Wu S, Nakamoto S, Arai M, Imazeki F, et al. Treatment of Real-World HCV Genotype 2-Infected Japanese Patients with Sofosbuvir plus Ribavirin. Biology (Basel) 2017;6:E30. doi: 10.3390/biology6020030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, Chapman RW, Cooksley WG, Czaja AJ, Desmet VJ, Donaldson PT, Eddleston AL, Fainboim L, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;31:929–938. doi: 10.1016/s0168-8278(99)80297-9. [DOI] [PubMed] [Google Scholar]
- 27.Hennes EM, Zeniya M, Czaja AJ, Parés A, Dalekos GN, Krawitt EL, Bittencourt PL, Porta G, Boberg KM, Hofer H, Bianchi FB, Shibata M, Schramm C, et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008;48:169–176. doi: 10.1002/hep.22322. [DOI] [PubMed] [Google Scholar]