Abstract
Study Objectives:
Sleep deprivation can impair attention, mood, and performance; however, few effective sleep education programs are available. The aim of this study was to assess the effect of a sleep education website, Sleep to Stay Awake (sleeptostayawake.org), on sleep behaviors of college students.
Methods:
College students (age 18 years or older) attending a public Midwestern university were randomized to control or intervention groups. All subjects completed baseline surveys that included demographics, Pittsburgh Sleep Quality Index, Patient Health Questionnaire, sleep knowledge, and measures of sleepiness and circadian rhythm. The intervention group then undertook the online intervention. Surveys were repeated at 1 week and at 8 weeks.
Results:
Students who participated included 295 controls and 254 intervention subjects. The mean age was 21.9 ± 4.1 years and 41.7% were male. Survey results at 8 weeks showed that more intervention subjects reported improved sleep behaviors (50.3% versus 39.5%, P = .04). Intervention subjects were more likely to stop electronics use earlier (odds ratio [95% confidence interval] = 1.5 [1.0–2.4]), keep a more regular sleep schedule (1.6 [1.06–2.4]), have an earlier weekday rise time (2.4 [1.3–4.4]), and have a lower likelihood of insufficient sleep prior to examinations (0.46 [0.28–0.76]). The intervention group had improvement in mean sleep quality (odds ratio = 5.8 versus 6.6, P < .001) and depression scores (odds ratio = 4.6 versus 5.6, P = .03). No significant differences were found in the other measures.
Conclusions:
A brief and personalized online sleep education intervention improved sleep behaviors, sleep quality, and depressions scores. This novel approach to address sleep deprivation, poor sleep habits, and mood among college students may offer an effective and inexpensive remedy.
Citation:
Hershner S, O'Brien LM. The impact of a randomized sleep education intervention for college students. J Clin Sleep Med. 2018;14(3):337–347.
Keywords: college student, depression, sleep deprivation, sleep education, sleep hygiene, sleep quality
BRIEF SUMMARY
Current Knowledge/Study Rationale: College students report inadequate sleep, daytime sleepiness, and erratic sleep schedules, which can affect academic performance and mood. Despite the known consequences of sleep deprivation few sleep education programs exist, with some programs only evaluating a change in sleep knowledge, rather than a change in sleep behaviors, whereas other programs are classroom based, which can limit access.
Study Impact: This randomized controlled study of an online sleep education intervention demonstrates both an improvement in sleep behaviors and depression scores. An effective and brief online sleep education intervention could be implemented among a large number of students without utilizing classroom resources and may improve the public health consequences of sleep deprivation, daytime sleepiness, and depression that is rampant among college students.
INTRODUCTION
Sleep is a fundamental human need for survival, health, and well-being, but more than half of all college students report feeling “tired, dragged out, or sleepy” during the day.1 Seventy percent of college students obtain fewer than 8 hours of sleep nightly during the school week.2 College students often have a delayed circadian rhythm that encourages late bedtimes.3 This in combination with early class times, frequent use of technology before bed, and caffeine consumption place college students at risk for insufficient sleep.2,4 This can compromise learning, attention, academic performance, and driving performance.5,6 Insufficient sleep may also increase the use of marijuana, smoking, and alcohol.7
Although the negative consequences of sleep deprivation are increasingly well known, there is a paucity of research on educational programs that teach college students the importance of sleep and how to improve sleep behaviors. Sleep education literature is more robust for high school students than for college students. Many high school sleep education programs are based in the classroom, may not use validated surveys measures, and often focus primarily on a change in sleep knowledge, and if sleep behaviors are measured, find that a change in sleep knowledge only marginally results in a change in behavior.8–13 In a review of sleep education programs only 2 out of the 12 studies were conducted among college-aged students.11,14,15 Other college-specific sleep education programs target a specific subset of students; for example, college nursing students may include mostly women, and thus may not be applicable to a broader range of college students.16,17 Many programs, both high school and collegiate, use extensive classroom resources, which limits availability to students.11,18–20 College students, as compared to high school students, have later bed and rise times, minimal if any parental oversight, and increased caffeine and nonprescribed stimulant use.2,4 Therefore, it cannot be assumed that educational programs for high school students will be effective among college or older students. Despite the known consequences of sleep deprivation among college students there is limited guidance on effective sleep education programs.
The purpose of our study was to assess the effect of the sleep education website Sleep to Stay Awake (sleeptostayawake.org) on the sleep knowledge and sleep behaviors of a diverse group of college students at a university in the Midwest. We tested the hypothesis that the sleep education intervention would enhance sleep knowledge and encourage sleep behavior change because it has several elements that are personalized and applicable to a broad range of students and could be implemented outside of the classroom.
METHODS
Subjects
The Institutional Review Board of the University of Michigan approved the study. All students age 18 years and older were eligible. Exclusion criteria included age younger than 18 years or nonstudent status. The Office of the Registrar performed randomization to the intervention (sleeptostayawake.org online education) or control group (no education) using simple number randomization and directly emailed the recruitment email to students. One thousand two hundred students each in the control and intervention group were contacted via email and invited to participate. Students were offered enrollment in the study twice more, with each invitation approximately 1 week apart. Students were broadly representative of the student population from freshman to professional students (medicine, dentistry, PhD) and included students living on and off campus. As an incentive, students were registered in a lottery to win one of two tablets. The study was performed during the winter semester of 2015.
Study Design
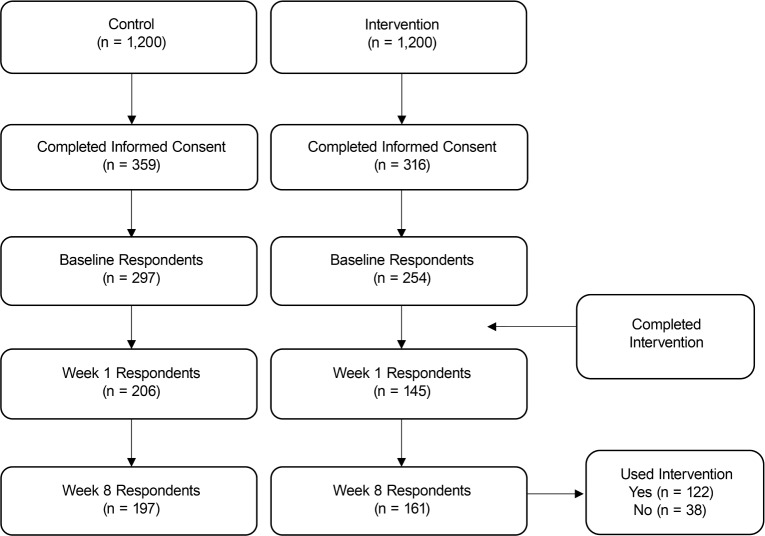
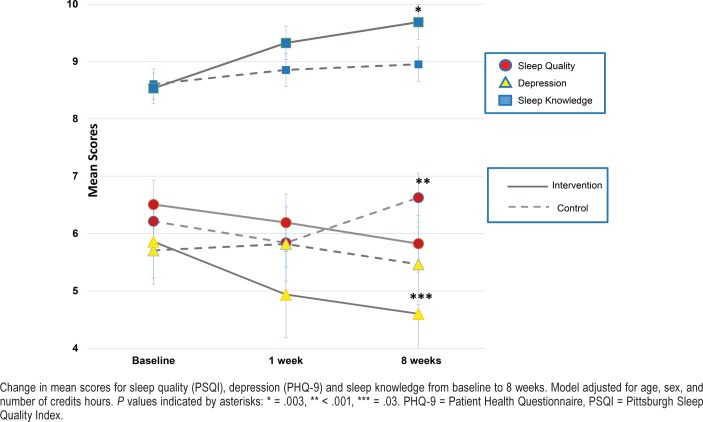
A link from the recruitment email connected to an online survey. Following recruitment, baseline surveys were completed by all subjects. Those randomized to the intervention group then received the intervention via a link in an email. Surveys were repeated at 1 week and 8 weeks postintervention for both groups (Figure 1). The week 8 survey was sent to all subjects who had completed the baseline survey regardless if they completed the week 1 survey.
Figure 1. Flow chart of respondent enrollment.
Measures
Demographic questions included age, sex, academic major, grade point average, and sleep patterns. Frequency of all-night study sessions and partial all-night study sessions, defined as getting 2 to 4 hours of sleep before an examination were ascertained.
Survey Instruments
Epworth Sleepiness Scale
The Epworth Sleepiness Scale (ESS) is an eight-question survey that measures the general propensity to fall asleep. A score of 10 or higher indicates sleepiness.21
Morning-Eveningness Questionnaire
The Morning-Eveningness Questionnaire (MEQ) has 19 questions with a final score ranging from 16 to 86. Five categories indicate circadian preference and range from definitely morning type (70–86), moderately morning type (59–69), neither type (42–58), moderately evening type (31–41), to definitely evening type (16–30).22
Pittsburgh Sleep Quality Index
The Pittsburgh Sleep Quality Index (PSQI) has 19 questions with 7 subcategories: sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction.23,24 A final composite global score of 5 or higher indicates poor sleep quality.
Sleep Hygiene Index
The Sleep Hygiene Index (SHI) measures wake behaviors that may adversely affect sleep; it has 13 questions rated on a scale of 1 (never) to 5 (always) with total scores range from 13 to 65.25 Higher scores indicate worse sleep hygiene.
Patient Health Questionnaire
To evaluate depression, the Patient Health Questionnaire (PHQ-9) was used with removal of the question asking about suicidal intent.26 Items are scored 0 (not at all) to 3 (nearly every day) with a total score of depression severity: none (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), and severe (20–27).
General Health Questionnaire
To evaluate for psychiatric morbidity, the General Health Questionnaire 12 (GHQ-12) was utilized. The GHQ-12 is a shortened version of the original.27 It comprises 12 items describing mood states, 6 of which are positively phrased and 6 negatively phrased. It was scored as a Likert scale, with all items coded as 0, 1, 2, and 3 with a final summed answer.
Sleep Knowledge
Sleep knowledge was ascertained by 14 questions related to sleep hygiene, physiology of sleep, effect of technology on sleep, and the interaction of sleep on learning, memory, and grades. Because there are no available validated sleep knowledge questionnaires the content of these questions were developed from validated sleep hygiene questionnaires, textbooks on sleep, the effect of technology and substances on sleep, and clinical experience.9,25 Three student-led focus groups, each with 15 students, evaluated and provided feedback on these questions.
Alterations in sleep-related behaviors were determined by self-report on the final survey and by changes in scores of the survey instruments.
Intervention
Sleep to Stay Awake (sleeptostayawake.org) is an online sleep education module with several components; a sleep personality profile, two videos, and information on healthy sleep behaviors. The “sleep personality profile” is a composite score of two questionnaires, the Epworth Sleepiness Scale and the Morning-Eveningness Questionnaire. After completion of these two surveys, subjects received their sleep personality profile. This allowed some degree of personalization with regard to the subjects' own level of sleepiness (sleepy or not sleepy) and circadian chronotype. Each personality profile had its own name and image, for example, “a sleepy night-owl” (Figure 2). Two videos highlighted various aspects of sleep hygiene and the effect of sleep deprivation on memory, learning, and driving. Additionally, the site included information on studying, daytime alertness, and naps that linked specifically to each student's sleep personality profile. Typical time for completion was 20 minutes.
Figure 2. The sleep personality profile.
Statistical Analysis
For continuous variables independent sample t test and for categorical variables Pearson chi-square tests were used to compare demographic information and sleep characteristics. All-night study sessions and partial all-night study sessions were evaluated with a chi-square test. Sleep knowledge was calculated as the number of correct responses.
To analyze the effect of time, linear mixed-model analysis was performed on the outcomes of PSQI, ESS, PHQ-9, MEQ, GHQ, SHI, and sleep knowledge. Linear mixed modeling is appropriate for these analyses because it can accommodate repeated measurements within each individual and missing data. Thus, it does not exclude individuals without follow-up data, and does not require balanced data. Each outcome variable had 3 time points: baseline, 1 week, and 8 weeks. Time was considered a categorical variable with the baseline as the reference. All predictors were included as fixed effects. To test the interaction with time and intervention such that the estimate is the difference (intervention at 8 weeks − intervention at baseline) with the control group difference (control at 8 weeks − control at baseline) as the reference. The model was adjusted for age, sex, and number of credit hours that semester; these were used covariates. Credit hours were included from the first author's clinical experience that the number of credit hours taken per semester influence students' studying and sleep patterns. A recent study conducted by Jawbone reported that students attending more rigorous schools may have shorter sleep durations.28 Howell et al. has shown that a full academic course load with a lower sleep quality performed worse on academic measures.6
At 8 weeks, binary logistic regression was performed for categorical variable of self-reported behavior change. This was adjusted for age, sex, and number of credit hours. A sensitivity analysis was also performed separately on subjects who reported at 8 weeks that they had visited the Sleep to Stay Awake web-site. All tests were two-sided. Statistical analysis was performed using IBM SPSS version 22 (IBM Corp, Armonk, New York, United States). Data are presented as mean ± standard deviation or proportions where appropriate.
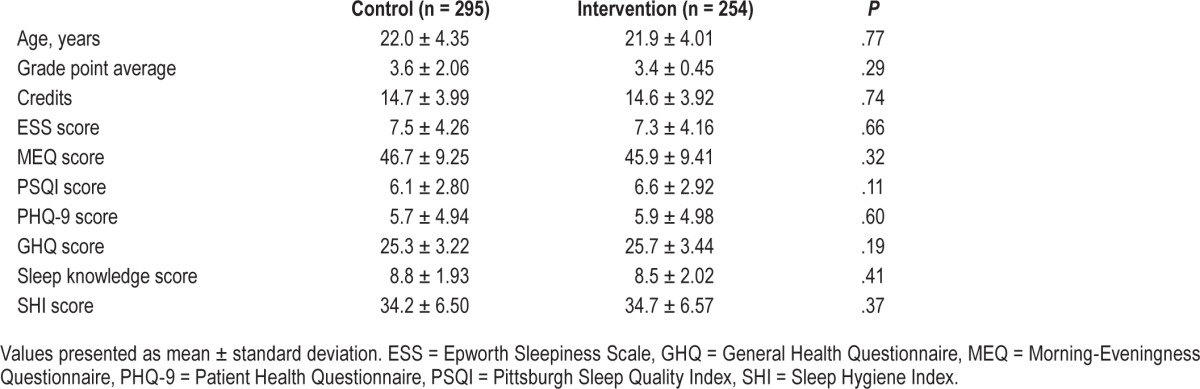
RESULTS
Overall, 1,200 subjects in each group were contacted via email and invited to participate. A total of 675 subjects completed the informed consent, providing a response rate of 28%. However, not all subjects completed baseline surveys after completing the informed consent. Of those who completed the baseline survey, 295 were in the control and 254 in the intervention group. Of the 549 students, 41.7% were male and the mean age was 21.9 ± 4.1 years. Study population demographics and sleep characteristics did not differ between the two groups (Table 1 and Table 2). A broad range of academic majors was represented. Most students lived in a rented apartment (51%) with 44.9% living in university housing (dormitories, graduate housing, and living learning communities). A small portion lived at other locations (home 2.1% and in fraternities/sororities 1.4%). In the intervention group, all students were included in the analysis regardless of whether they indicated they had visited the intervention site.
Table 1.
Baseline characteristics in the control and intervention group.
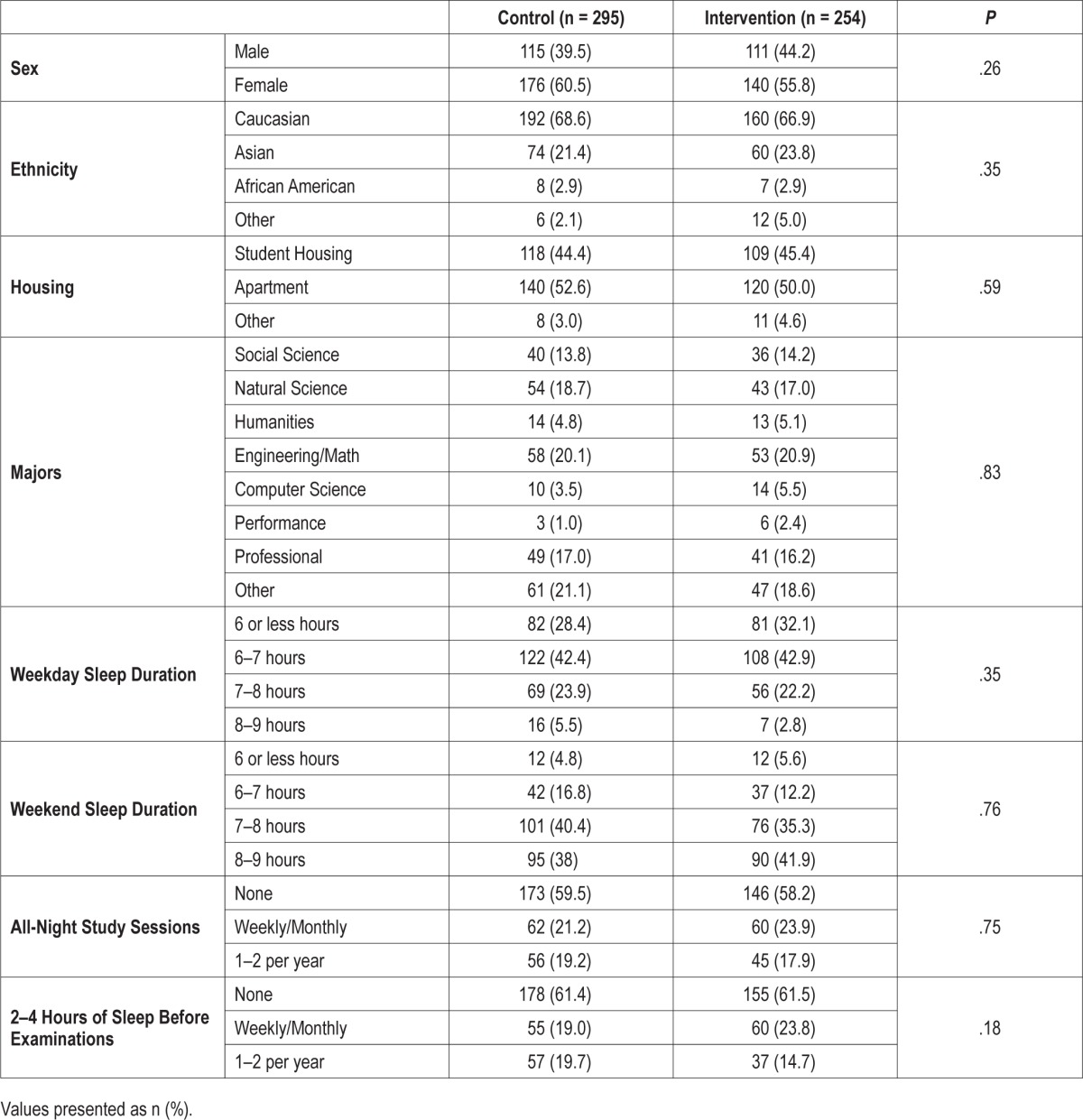
Table 2.
Baseline continuous variables of the control and intervention group.
Sleep Characteristics
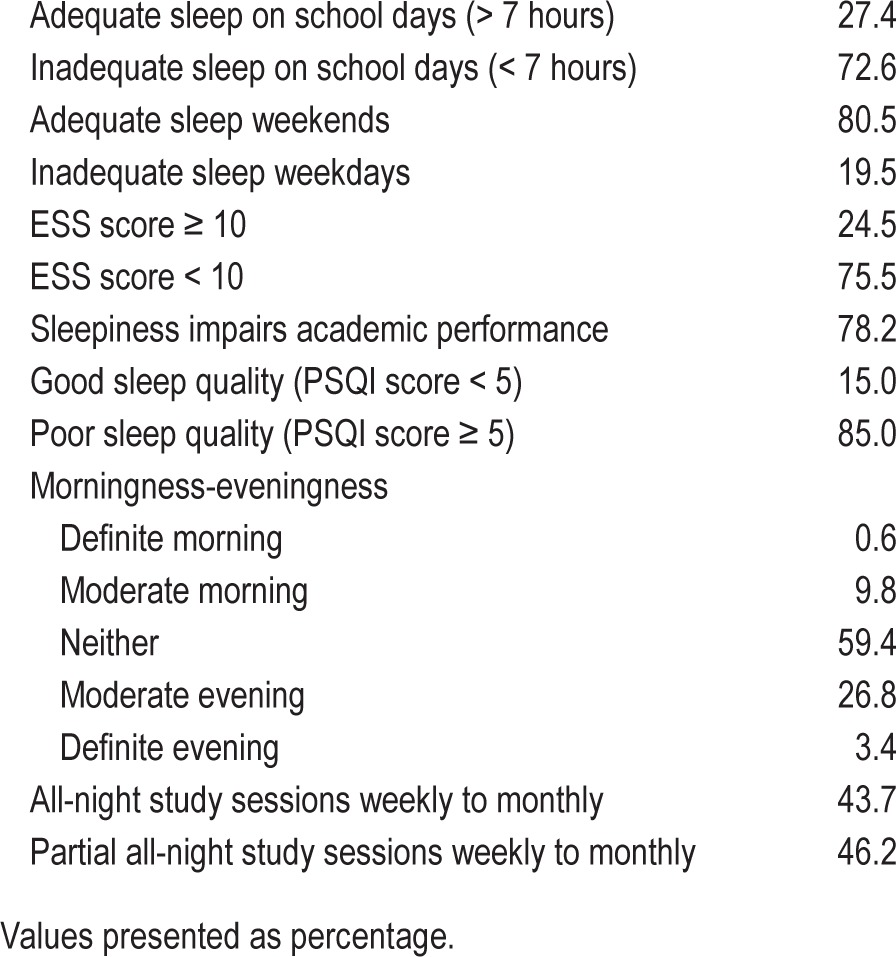
When viewed as a whole prior to the intervention, insufficient sleep, defined as fewer than 7 hours of nightly sleep, was widespread, with 72.6% of students reporting insufficient weeknight sleep (Table 3). Catch-up sleep on the weekends was prevalent as only 19.5% of students reported insufficient sleep on the weekends. Although most college students (78.2%) reported that sleepiness impairs their academic performance, only 24.5% had an ESS score of 10 or higher, indicative of excessive daytime sleepiness. According to the authors of the PSQI, a global score higher than 5 indicates that a subject is having severe difficulties in at least two of the seven components areas or moderate difficulties in more than three areas. Poor sleep quality was ubiquitous, because 85% of subjects had a PSQI of 5 or higher. A “neither” chronotype, which is a tendency to be between an evening and a morning circadian rhythm, was the most common, whereas the next largest percentage was an evening-type chronotype. A morning tendency was uncommon. All-night study sessions and partial all-night study sessions, defined as sleeping 2 to 4 hours, occurred weekly to a few times a year for almost half of the students. No significant differences existed between the intervention and control group at baseline (Table 2).
Table 3.
Baseline sleep behaviors as a group prior to the intervention.
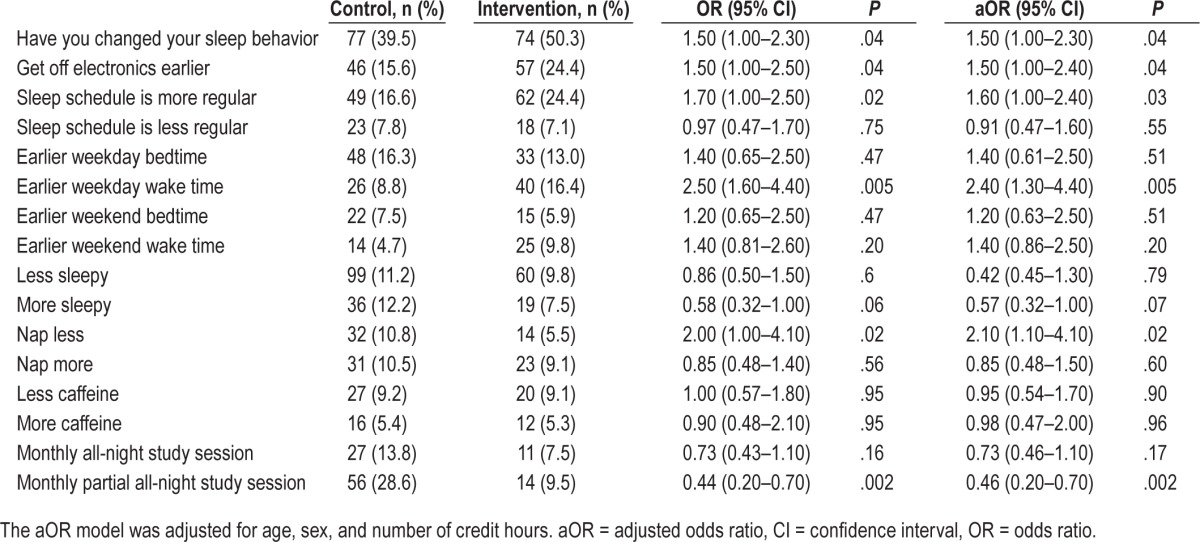
Self-Reported Behavior Change
At 8 weeks, a greater percentage of intervention subjects reported behavior changes to their sleep and wake behaviors as compared to controls (50.3% versus 39.5%, P = .04) (Table 4). The intervention subjects stopped electronics earlier, kept a more regular sleep schedule, and woke earlier during the week. The intervention group had less frequent partial all-night study sessions, with monthly partial all-night study sessions decreasing. No significant changes were noted for all-night study sessions. The model was adjusted to age, sex, and number of credit hours without a change in significance.
Table 4.
Self-reported behavioral change at 8 weeks.
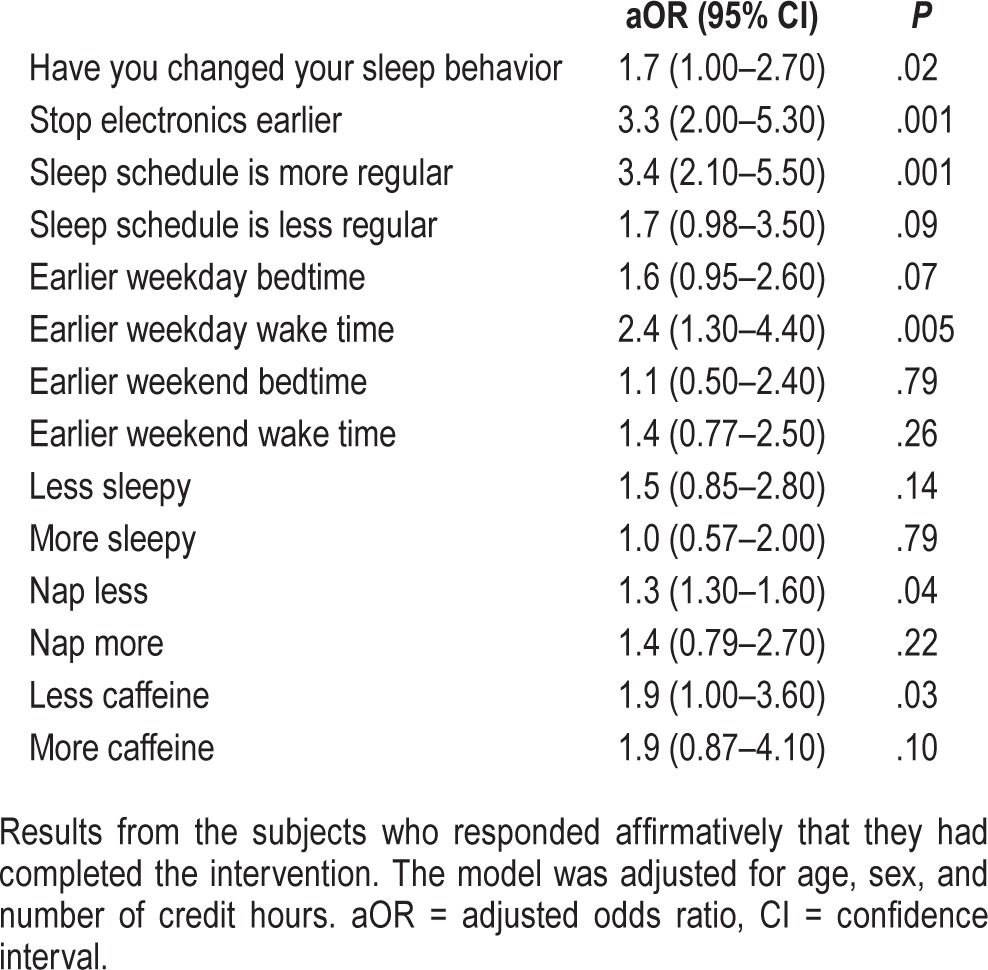
A sensitivity analysis was performed that included only intervention subjects who reported utilization of the intervention at 8 weeks (Table 5). The sensitivity analysis supported that the sleep education intervention increased the likelihood that subjects made positive changes to their sleep and wake behaviors. The subjects who positively affirmed use of the intervention compared to control subjects had an odds ratio of 1.7 for self-reported behavior change. Subjects had a threefold increased odds of stopping electronics earlier and having a more regular sleep schedule. As compared with the whole intervention group, subjects were more likely to have an earlier wake time during the week and drink less caffeine.
Table 5.
Self-reported behavioral change.
At 8 weeks, there was no significant difference in total sleep time on school nights and weekends between both groups. The intervention group had a decreased frequency of being unable to fall asleep within 30 minutes and a decreased weekly frequency 31 to ≥ 60 minutes sleep latency.
Sixty-six percent of respondents thought that Sleep to Stay Awake provided new information and 62.6% thought that it was helpful.
Linear Mixed Modeling
To evaluate the effect of time, an interaction term was utilized with Intervention Group × Time (1 week) and Intervention Group × Time (8 weeks). The model adjusted for age, sex, and number of credit hours. At 8 weeks, there was an improvement in the intervention group for sleep knowledge, sleep quality, and depression scores (Table 6). In the control group, sleep quality significantly worsened (beta coefficient 1.09 [95% confidence interval (CI) 0.51–1.65] P < .001) with the baseline PSQI of 6.1 increasing to 6.6 at 8 weeks. Sleep hygiene was nearly significant (P = .05). No significant changes effects were observed at 1 week for the outcome variables, except for sleep knowledge in the intervention group. Because these variables were not significant they are not included in the accompanying table (Table 6 and Figure 3).
Table 6.
Change in mean scores.
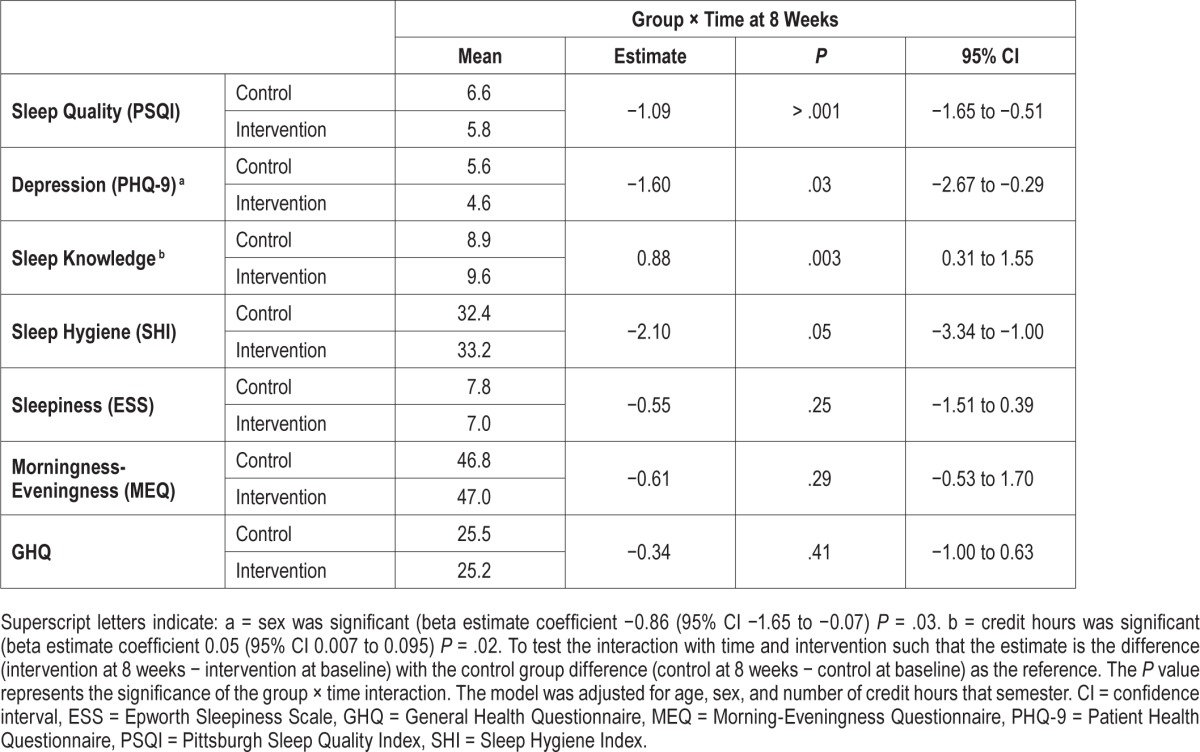
Figure 3. Change in sleep quality, depression, and sleep knowledge.
Change in mean scores for sleep quality (PSQI), depression (PHQ-9) and sleep knowledge from baseline to 8 weeks. Model adjusted for age, sex, and number of credits hours. P values indicated by asterisks: * = .003, ** < .001, *** = .03. PHQ-9 = Patient Health Questionnaire, PSQI = Pittsburgh Sleep Quality Index.
At the final survey, intervention subjects' mean depression scores were lower such that only 14% of intervention subjects met criteria for depression as compared to 35.8% of control subjects (P = .005). The PSQI score improved at 8 weeks for the intervention group, decreasing by 0.8, a 10% improvement. The PSQI score worsened for the control group. At 8 weeks, 33.3% of the intervention group reported good sleep quality compared to only 21.3% of the control group (P = .04). Both the control and intervention group had higher sleep knowledge scores at 8 weeks. No significant differences were present for the MEQ, GHQ, or ESS.
DISCUSSION
This study shows that the online sleep educational website Sleep to Stay Awake improved sleep knowledge and prompted sleep-related behavior changes among a group of college students. Most importantly, at the end of 8 weeks, several cardinal areas improved, including depression scores and sleep quality. Although the SHI was not significantly different at the end of the intervention, there were important improvements in self-reported sleep behaviors including stopping electronics earlier, waking earlier during the week, keeping a more regular sleep schedule, and napping less.
Important features of this study that differ from previous approaches include a broad demographic of students, no requirement to use classroom resources, use of validated surveys, and personalization.
Many sleep education programs utilize significant resources in terms of space, personnel, and classroom time.11,16,18,19,29,30 Some programs utilized 50 minutes, and a nursing sleep education program had up to 10 hours of material.16,20 “Sleep 101,” is a psychoeducational program consisting of two 90-minute workshops.19 It had features less commonly used in sleep education programs as it not only focused on sleep hygiene, but also mal-adaptive thoughts about sleep. It improved sleep hygiene and sleep knowledge, and reduced sleep onset latency and maladaptive thoughts about sleep, but did not affect sleep quality. A pilot college sleep education program with a didactic lecture utilized the Sleep Beliefs Scale to access sleep knowledge.17 This scale asks if specific behaviors have a positive, negative, or neutral effect on sleep. This improvement in knowledge did not change total sleep time (except among students with a shorter sleep duration), and students went to bed later and woke earlier. In a sleep education review, many studies reported that students preferred more interactive activities rather than traditional didactic methods.9 Non-classroom–based programs have utilized electronic interaction with students, but these programs go beyond a sleep education program and are based on electronically delivered cognitive behavioral therapy.31,32 This involves a much broader amount of information and repeated interactions with students; therefore, these programs should not be considered a sleep education intervention. All classroom-based programs will limit the number of students who can access the material. A benefit of this current study is that the program is brief, online, and available to a large number of students without utilizing classroom resources.
There are several reasons why the Sleep to Stay Awake educational program may have encouraged behavior change. There was some degree of personalization, with each participant getting feedback on their own level of sleepiness and circadian chronotype. There is growing evidence in health behavior literature that tailored messages may have greater effect.33,34 For example, patients given a tailored behavior change recommendation were 18% more likely to change at least one risk behavior than patients receiving typical feedback or no feedback (odds ratio = 1.18 [95% CI 1.00–1.39]).33 Tailoring can be defined as “any combination of strategies and information intended to reach one specific person, based on characteristics that are unique to that person, related to the outcome of interest, and derived from an individual assessment.”35 Levenson et al. reported that personalized feedback on sleep diaries encouraged behavior change.17 In the current study, the sleep personality profile gives some degree of individual assessment and 69.8% of students “strongly agree to agree” that the personalization was important.
The content of this educational program may also have encouraged behavior change as information provided attempted to link sleep and sleep behaviors to learning, and grade point average. This allows the content to be more applicable to college students. According to Noar et al., the social cognitive theory suggests that in addition to confidence in performing a behavior, an individual must also believe that engaging in the behavior will lead to desirable outcomes.34 Grades and grade point average are important to college students; therefore, linking sleep behaviors to academic performance may have encouraged behavior change. Specific behaviors here may also be important to academic performance. High academic performers showed earlier bed and rise times, with similar overall total sleep time.36 More regular sleep has been associated with improved academic performance.37 The current study found that following the intervention students were more likely to have a regular sleep schedule, earlier wake time, and a trend to an earlier weekday bedtime.
This study showed improvement in sleep quality. Multiple studies have shown that sleep quality has an association with academic performance, with some studies having a stronger association than total sleep time.6,38,39 Poor global sleep quality can negatively affect both psychological and physical disorders including increased antisocial personality problems, anxiety, attention deficit/hyperactivity problems, and somatic complaints as well as increased risk of diabetes and infections.40–43 Poor sleep quality is commonly reported by college students and in this study 85% of students reported poor sleep quality.2 Interventions that improved sleep quality could have a far-reaching effect on the health of college students.
Depression scores improved at 8 weeks for the intervention group, with a 20% reduction in the number of students meeting depression criteria. According to the American College Health Association's National College Health Assessment in the spring of 2015, 13% of students had received a diagnosis of or were in treatment for depression. This likely underestimates the frequency as per the same report, 26.5% reported they “felt very sad” in the past 2 weeks.44 Other studies support a similar depression prevalence whereas some studies have a prevalence as high as 43%.45,46 Sleep quality and sleep disturbances have a bidirectional relationship with depression.46–48 Female college students with poor sleep quality have an adjusted odd ratio of 2.8 (95% CI 1.3–5.8) for depression.45
There is a growing body of evidence that improving sleep symptoms can improve depression.49,50 Among college students with poor sleep quality, a cognitive behavioral therapy intervention targeted at improving sleep (that was sent via email) decreased depression scores more than the intervention targeting mood and resilience to stress.32 In a pilot of a sleep health promotion program, lower sleep disturbances resulted in lower depression scores as measured by the Patient Reported Outcomes Measurement Information System, despite no significant change in total sleep time.17 Irregular sleep-wake patterns and insufficient sleep have been associated with more depressive symptoms.46 Irregular sleep patterns may lead to desensitization of serotonergic receptor systems, further linking sleep and depression.51 In this current study, subjects were more likely to report a more regular sleep schedule. A study evaluating the emergence of depressive symptoms found that prolonged sleep latency was associated with symptoms of loss of pleasure, punishment feelings, self-dislike, loss of interest, irritability, and fatigue.46 Intervention subjects in the current study had shorter sleep latency; this may be because they stopped electronic use earlier. Use of electronics at bedtime is associated with a longer sleep latency, shorter sleep duration, more nocturnal alertness, and next-day sleepiness.52 It may be that these improvements in specific sleep-related behaviors along with an improvement in sleep quality resulted in the observed improvement in depression scores.
It is not clear why sleep knowledge improved in both groups. Because this was a campus-wide study at a large university, it is unlikely that there was significant interaction between the intervention and control groups. A more likely explanation is that completing the repetitive questions from the surveys may have prompted an improvement in sleep knowledge or at least improved sleep awareness.
It is important to note that our results were observed at 8 weeks. Studies have shown that sleep quality and sleep behavior worsen during the semester; therefore, the response at 8 weeks strengthens the findings of this study.30,53 Many people require time to adapt behavioral changes into their routine. In a study among university students asked to choose a healthy eating, drinking, or exercise behavior that they wished to make a habit, on average the new habit formation took 66 days.54
A strength of this study is the intent to treat analysis. Most of the statistical analysis of this study was performed as if all of the subjects had utilized the intervention, regardless of their response to “Have you used the Sleep to Stay Awake intervention?” The sensitivity analysis with only subjects who confirmed use of the program further substantiates the benefit of this program because subjects were more likely to report positive changes to their sleep behavior.
There are several limitations to this study. Although this study attempted to be broadly representative of the student population (graduate, undergraduate, on-campus and off-campus student housing, multiple academic majors) it still may not be diverse enough to adequately represent the entire student population. Although this study was conducted at a public university, it is a selective university and therefore these findings may not be reflective of the college population at large. A recent study conducted by Jawbone reported that students attending more rigorous schools may have shorter sleep durations.28 Additionally, although many validated measures were included in this study, no validated sleep knowledge questionnaire is available.9 That said, these questions were developed from other studies that had included similar questions, and were based on many classic sleep hygiene recommendations and included important aspects of sleep and wake physiology. All questions underwent three focus groups with students for readability and targeting a correct response rate of 60% or less. The noted improvement in sleep behaviors are by self-report; this is typical for sleep education programs at all age levels.9,11 Last, it may be that students with the perception of sleep problems were more likely to respond to the survey request.
Future research would be important to determine if these improvements persist and if the changes in sleep behaviors affect students' academic performance. It is also important to assess if the improvement to mood persists. Ideally an assessment of which components of the Sleep to Stay Awake program prompted behavior changes, and if these can be specifically targeted to certain students it would be beneficial. Finally, it is essential to assess the optimal timing of a sleep education program as it pertains both to a student's year in school and their academic calendar. Freshman student orientation seems a logical timing for implementation, but that is also a time a student is most overwhelmed with learning their new environment, making friends/socializing, and coping with the stress of an absence from home and family. It may be that a sleep education program would be best later in the year. Programs may need to emphasize different aspects of sleep hygiene and sleep behaviors across a student's academic career (eg, from freshman to PhD), but further research is needed.
Summary
This study demonstrated that the brief online and personalized sleep educational website, Sleep to Stay Awake, improved sleep knowledge and resulted in improved sleep behaviors, sleep quality, and decreased depression scores. Of significance is that these changes were noted at 8 weeks rather than immediately, suggesting that these improvements may persist. Adequate sleep health is vital for the health and well-being of college students. An effective online sleep education intervention for college students could have substantial effect on the mood and sleep behaviors of college students.
DISCLOSURE STATEMENT
Shelley Hershner was supported by the Michigan Institute for Clinical and Health Research (MICHR) / Practice Oriented Research Training Program (PORT). Sleep to Stay Awake is a free online education resource owned by the Regents of the University of Michigan and developed by Shelley Hershner. All authors have seen and approved the final version of the manuscript. Work for this study was performed at the Department of Neurology, University of Michigan, Ann Arbor, MI.
ACKNOWLEDGMENTS
Author contributions: Shelley Hershner developed the study, performed the statistical analysis, reviewed and wrote the manuscript; Louise M. O'Brien designed the study, reviewed the results, and wrote the manuscript.
ABBREVIATIONS
- CI
confidence interval
- ESS
Epworth Sleepiness Scale
- GHQ
General Health Questionnaire
- MEQ
Morning-Eveningness Questionnaire
- PHQ
Patient Health Questionnaire
- PSQI
Pittsburgh Sleep Quality Index
- SHI
Sleep Hygiene Index
REFERENCES
- 1.American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2016. Hanover, MD: American College Health Association; 2016. [Google Scholar]
- 2.Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46(2):124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 3.Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep -Implications for behavior. Ann N Y Acad Sci. 2004;1021:276–291. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- 4.Orzech KM, Grandner MA, Roane BM, Carskadon MA. Digital media use in the 2 h before bedtime is associated with sleep variables in university students. Comput Human Behav. 2016;55:43–50. doi: 10.1016/j.chb.2015.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Curcio G, Ferrara M, De Gennaro L. Sleep loss learning capacity and academic performance. Sleep Med Rev. 2006;10(5):323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Howell AJ, Jahrig JC, Powell RA. Sleep quality sleep propensity and academic performance. Percept Mot Skills. 2004;99(2):525–535. doi: 10.2466/pms.99.2.525-535. [DOI] [PubMed] [Google Scholar]
- 7.Taylor DJ, Bramoweth AD. Patterns and consequences of inadequate sleep in college students: Substance use and motor vehicle accidents. J Adolesc Health. 2010;46(6):610–612. doi: 10.1016/j.jadohealth.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Brown FC, Buboltz WC, Soper B. Relationship of sleep hygiene awareness sleep hygiene practices and sleep quality in university students. Behav Med. 2002;28(1):33–38. doi: 10.1080/08964280209596396. [DOI] [PubMed] [Google Scholar]
- 9.Blunden S, Rigney G. Lessons learned from sleep education in schools: a review of dos and don'ts. J Clin Sleep Med. 2015;11(6):671–680. doi: 10.5664/jcsm.4782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wing YK, Chan NY, Man Yu MW, et al. A school-based sleep education program for adolescents: a cluster randomized trial. Pediatrics. 2015;135(3):e635–e643. doi: 10.1542/peds.2014-2419. [DOI] [PubMed] [Google Scholar]
- 11.Blunden SL, Chapman J, Rigney GA. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep Med Rev. 2012;16(4):355–370. doi: 10.1016/j.smrv.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Cain N, Gradisar M, Moseley L. A motivational school-based intervention for adolescent sleep problems. Sleep Med. 2011;12(3):246–251. doi: 10.1016/j.sleep.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Kira G, Maddison R, Hull M, Blunden S, Olds T. Sleep education improves the sleep duration of adolescents: a randomized controlled pilot study. J Clin Sleep Med. 2014;10(7):787–792. doi: 10.5664/jcsm.3874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown FC, Buboltz WC, Soper B. Development and evaluation of the sleep treatment and education program for students (STEPS) J Am Coll Health. 2006;54(4):231–237. doi: 10.3200/JACH.54.4.231-237. [DOI] [PubMed] [Google Scholar]
- 15.Cortesi F, Giannotti F, Sebastiani T, Bruni O, Ottaviano S. Knowledge of sleep in Italian high school students: pilot-test of a school-based sleep educational program. J Adoles Health. 2004:344–351. doi: 10.1016/j.jadohealth.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 16.Ye L, Smith A. Developing and testing a sleep education program for college nursing students. J Nurs Educ. 2015;54(9):532–535. doi: 10.3928/01484834-20150814-09. [DOI] [PubMed] [Google Scholar]
- 17.Levenson JC, Miller E, Hafer B, Reidell MF, Buysse DJ, Franzen PL. Pilot study of a sleep health promotion program for college students. Sleep Health. 2016;2(2):167–174. doi: 10.1016/j.sleh.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao R, Lv Y, Li XM, et al. Effects of comprehensive sleep management on sleep quality in university students in mainland China. Sleep Biol Rhythms. 2014;12(3):194–202. [Google Scholar]
- 19.Kloss JD, Nash CO, Walsh CM, Culnan E, Horsey S, Sexton-Radek K. A “sleep 101” program for college students improves sleep hygiene knowledge and reduces maladaptive beliefs about sleep. Behav Med. 2014;42(1):48–56. doi: 10.1080/08964289.2014.969186. [DOI] [PubMed] [Google Scholar]
- 20.Quan SF, Anderson JL, Hodge GK. Use of a supplementary internet based education program improves sleep literacy in college psychology students. J Clin Sleep Med. 2013;9(2):155–160. doi: 10.5664/jcsm.2414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 22.Horne JA, Östberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4(2):97–110. [PubMed] [Google Scholar]
- 23.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 24.Dietch JR, Taylor DJ, Sethi K, Kelly K, Bramoweth AD, Roane BM. Psychometric evaluation of the PSQI in U.S. college students. J Clin Sleep Med. 2016;12(8):1121–1129. doi: 10.5664/jcsm.6050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mastin DF, Bryson J, Corwyn R. Assessment of sleep hygiene using the sleep hygiene index. J Behav Med. 2006;29(3):223–227. doi: 10.1007/s10865-006-9047-6. [DOI] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9 - Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldberg D. Windsor, UK: Nfer-Nelson; 1992. General health questionnaire (GHQ-12) [Google Scholar]
- 28.Wilt B. How University Students Sleep. [Accessed January 21, 2018]. https://jawbone.com/blog/university-students-sleep. Published April 20, 2016.
- 29.Rigney G, Blunden S, Maher C, et al. Can a school-based sleep education programme improve sleep knowledge hygiene and behaviours using a randomised controlled trial. Sleep Med. 2015;16(6):736–745. doi: 10.1016/j.sleep.2015.02.534. [DOI] [PubMed] [Google Scholar]
- 30.Tsai LL, Li SP. Sleep education in college: a preliminary study. Percept Mot Skills. 2004;99(3):837–848. doi: 10.2466/pms.99.3.837-848. [DOI] [PubMed] [Google Scholar]
- 31.Morris J, Firkins A, Millings A, Mohr C, Redford P, Rowe A. Internet-delivered cognitive behavior therapy for anxiety and insomnia in a higher education context. Anxiety Stress Coping. 2016;29(4):415–431. doi: 10.1080/10615806.2015.1058924. [DOI] [PubMed] [Google Scholar]
- 32.Trockel M, Manber R, Chang V, Thurston A, Taylor CB. An Email delivered CBT for sleep-health program for college students: effects on sleep quality and depression symptoms. J Clin Sleep Med. 2011;7(3):273–278. doi: 10.5664/JCSM.1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kreuter MW, Strecher VJ. Do tailored behavior change messages enhance the effectiveness of health risk appraisal? Results from a randomized trial. Health Educ Res. 1996;11(1):97–105. doi: 10.1093/her/11.1.97. [DOI] [PubMed] [Google Scholar]
- 34.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 35.Kreuter MW, Skinner CS. Tailoring: what's in a name? Health Educ Res. 2000;15(1):1–4. doi: 10.1093/her/15.1.1. [DOI] [PubMed] [Google Scholar]
- 36.Eliasson AH, Lettieri CJ, Eliasson AH. Early to bed early to rise! Sleep habits and academic performance in college students. Sleep Breath. 2010;14(1):71–75. doi: 10.1007/s11325-009-0282-2. [DOI] [PubMed] [Google Scholar]
- 37.Phillips AJK, Clerx WM, O'Brien CS, et al. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci Rep. 2017;7(1):3216. doi: 10.1038/s41598-017-03171-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gomes AA, Tavares J, de Azevedo MH. Sleep and academic performance in undergraduates: a multi-measure multi-predictor approach. Chronobiol Int. 2011;28(9):786–801. doi: 10.3109/07420528.2011.606518. [DOI] [PubMed] [Google Scholar]
- 39.Gilbert SP, Weaver CC. Sleep quality and academic performance in university students: a wake-up call for college psychologists. Journal of College Student Psychotherapy. 2010;24(4):295–306. [Google Scholar]
- 40.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(2):414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cohen S, Doyle WJ, Alper CM, Janicki-Deverts D, Turner RB. Sleep habits and susceptibility to the common cold. Arch Intern Med. 2009;169(1):62–67. doi: 10.1001/archinternmed.2008.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Milojevich HM, Lukowski AF. Sleep and mental health in undergraduate students with generally healthy sleep habits. PLoS One. 2016;11(6):e0156372. doi: 10.1371/journal.pone.0156372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rose D, Gelaye B, Sanchez S, et al. Morningness/eveningness chronotype poor sleep quality and daytime sleepiness in relation to common mental disorders among Peruvian college students. Psychol Health Med. 2015;20(3):345–352. doi: 10.1080/13548506.2014.951367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.American College Health Association website. Reference Group Report, Spring 2015 (pdf) [Accessed September 24, 2016]. http://www.acha-ncha.org/reports_ACHA-NCHAIIb.html. Published August 26, 2015.
- 45.Wilson KT, Bohnert AE, Ambrose A, Davis DY, Jones DM, Magee MJ. Social behavioral and sleep characteristics associated with depression symptoms among undergraduate students at a women's college: a cross-sectional depression survey 2012. BMC Womens Health. 2014;14:8. doi: 10.1186/1472-6874-14-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brooks PR, Giigenti AA, Mills MJ. Sleep patterns and symptoms of depression in college students. Coll Stud J. 2009;43(2):464–472. [Google Scholar]
- 47.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39(6):411–418. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 48.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31(10):1351–1356. [PMC free article] [PubMed] [Google Scholar]
- 49.Rahimi A, Ahmadpanah M, Shamsaei F, et al. Effect of adjuvant sleep hygiene psychoeducation and lorazepam on depression and sleep quality in patients with major depressive disorders: results from a randomized three-arm intervention. Neuropsychiatr Dis Treat. 2016;12:1507–1515. doi: 10.2147/NDT.S110978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31(4):489–495. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roman V, Walstra I, Luiten PG, Meerlo P. Too little sleep gradually desensitizes the serotonin 1A receptor system. Sleep. 2005;28(12):1505–1510. [PubMed] [Google Scholar]
- 52.Chang AM, Aeschbach D, Duffy JF, Czeisler CA. Evening use of light-emitting eReaders negatively affects sleep circadian timing and next-morning alertness. Proc Natl Acad Sci U S A. 2015;112(4):1232–1237. doi: 10.1073/pnas.1418490112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Galambos NL, Howard AL, Maggs JL. Rise and fall of sleep quantity and quality with student experiences across the first year of university. J Res Adolesc. 2011;21(2):342–349. [Google Scholar]
- 54.Lally P, van Jaarsveld CH, Potts HW, Wardle J. How are habits formed: modelling habit formation in the real world. Eur J Soc Psychol. 2010;40(6):998–1009. [Google Scholar]