Abstract
Study Objectives:
Insomnia and short or long sleep duration are important comorbid conditions in adults with attention-deficit hyperactivity disorder (ADHD), but reports of the association vary. In a general population study, we evaluated the relationship between ADHD symptom severity, insomnia symptoms, and sleep duration in adults.
Methods:
Data were from the third wave of the Netherlands Mental Health Survey and Incidence Study-2 (NEMESIS-2; n = 4,618). ADHD symptom severity and symptom dimensions (hyperactivity and inattention) were assessed using the Adult ADHD Self-Report Scale screener. Self-reported insomnia symptoms (Insomnia Rating Scale; IRS) were defined as clinically relevant if IRS ≥ 9. Self-reported short sleep duration was defined as ≤ 6 hours, and long sleep duration as ≥ 10 hours.
Results:
Within the group with clinically relevant ADHD symptoms, 43% reported significant insomnia symptoms (odds ratio [OR] = 2.66, 95% confidence interval [CI] 1.74–4.07); 41% short sleep duration (relative risk ratio [RRR] = 1.94, 95% CI 1.31–2.85) and 6% long sleep (RRR = 5.87, 95% CI 1.97–17.45). Increased inattention symptoms were associated with IRS ≥ 9, short and long sleep duration in fully adjusted models (OR = 1.10, 95% CI 1.06–1.14; RRR = 1.06, 95% CI 1.02–1.09; RRR = 1.16, 95% CI 1.05–1.28, respectively). Increased hyperactivity symptoms were associated with IRS ≥ 9 (OR = 1.17, 95% CI 1.11–1.23) and short sleep duration (RRR = 1.12, 95% CI 1.05–1.19).
Conclusions:
Both clinically significant ADHD symptoms and inattention and hyperactivity symptom dimensions were consistently associated with insomnia symptoms and altered sleep duration. These associations confirm that sleep disturbances should be assessed and given appropriate clinical attention in adults with ADHD.
Citation:
Wynchank D, ten Have M, Bijlenga D, Penninx BW, Beekman AT, Lamers F, de Graaf R, Kooij JJ. The association between insomnia and sleep duration in adults with attention-deficit hyperactivity disorder: results from a general population study. J Clin Sleep Med. 2018;14(3):349–357.
Keywords: ADHD, adults, attention-deficit hyperactivity disorder, general population survey, insomnia, sleep duration
BRIEF SUMMARY
Current Knowledge/Study Rationale: Insomnia and altered sleep duration are important comorbid conditions in adults with attention-deficit hyperactivity disorder (ADHD). Several cross-sectional clinical and population studies reported a prevalence of insomnia of 43% to 80% in adults with ADHD. One longitudinal study described an association between ADHD and insomnia; another did not. In a general population study, we evaluated the relationship between self-reported ADHD symptom severity, ADHD symptom dimensions, insomnia symptoms, and sleep duration in adults.
Study Impact: Clinically significant ADHD symptoms (four to six symptoms on the Adult ADHD Self-Report Screener) and the inattention and hyperactivity symptom dimensions were consistently associated with insomnia and altered sleep duration. We have confirmed that insomnia and altered sleep duration occur commonly in adults with ADHD; hence, they should be appropriate assessed and treated.
INTRODUCTION
Attention-deficit hyperactivity disorder (ADHD) is a childhood-onset neurodevelopmental disorder that is marked by inattention and impulsivity, with or without hyperactivity.1 ADHD persists into adulthood in two-thirds of children with ADHD,2 where the cross-national estimated prevalence of ADHD is 2.8%.3 Some researchers view ADHD as a dimensional disorder, where symptoms are best considered as continuous traits across the general population.4 At a certain threshold of symptom severity, in combination with significant dysfunction in daily life, a clinical diagnosis of ADHD may be made.1 Adult ADHD is highly comorbid with other psychiatric disorders: 52% of adults with ADHD have any comorbid psychiatric disorder.3 The most common comorbidities are anxiety, mood, behavioral, and sleep disorders.3
There is evidence for an increased prevalence of several sleep disorders in adult ADHD, including insomnia, circadian rhythm disturbances, restless legs syndrome, and obstructive sleep apnea, comprehensively reviewed by Instanes et al.5 Several cross-sectional, clinical, and population studies reported a prevalence of insomnia in adults with ADHD ranging from 43% to 80%.6–9 Two longitudinal studies described conflicting findings; in one there was a significant association between persistent childhood ADHD and insomnia at age 18.10 The other showed no association between childhood or adolescent ADHD and insomnia diagnosed at age 38 years.11 ADHD symptom severity correlated with worsening of sleep quality in a small study among adults,12 but a community study of young adults (aged 18–20 years) did not find this association.13 Some studies within adult ADHD populations have examined insomnia symptoms, such as subjective sleep quality, which was reported as poorer in adults with ADHD than in controls (reviewed in Instanes et al.).5
Reports of sleep duration in adult ADHD vary, with the literature reporting no change as well as a combination of both short and long sleep duration. A very large population study (n = 30,858; ADHD cases n = 1,122) found that both increased and decreased sleep duration were associated with increasing odds of reporting ADHD symptoms.14 Two other studies reported a mean total sleep duration less than 6 hours in adults with ADHD15,16; however, the latter included a very small ADHD sample (n = 24). In contrast, in three small studies (ADHD samples n = 20–40) measuring total sleep duration objectively using actigraphy or polysomnography, no significant difference in sleep duration was found between those with ADHD and healthy controls.17–19 Two large studies using self-reported sleep duration also showed no difference in sleep duration in (young) adults with and without ADHD (n = 64 and n = 175, respectively).13,20
The clinical implications of suboptimal sleep include worsening of ADHD symptoms, as sleep regulates learning and consolidation of memory.21 Sleep loss in the general population is well known to impair performance on attention and executive control tasks.22 These authors showed that 6 hours of sleep restriction for 14 days produced detrimental effects on sustained attention and working memory that were comparable to the effects of 2 nights of full sleep deprivation. In view of the deleterious effects of sleep loss on cognitive functioning, and the conflicting results in the literature, it is important to clarify the relationship between ADHD and sleep duration in a larger adult sample.
Two main symptom dimensions are present in ADHD: hyperactivity/impulsivity and inattention.1 Research specifically investigating sleep disorders and these two symptom dimensions is preliminary and has given mixed results in adults, as reported in two reviews.5,23 The relationship between specific ADHD symptom dimensions and sleep problems is important because patients with these separate clinical profiles may require different treatments.
In this study, we aimed to clarify if the burden of insomnia and disturbed sleep duration increases with higher ADHD symptom severity. We examined ADHD symptom severity, ADHD symptom dimensions, insomnia symptoms, and sleep duration among the Dutch general population, taking a range of sociodemographic and lifestyle factors, comorbid mental disorders, and medical conditions into account.
METHODS
Participants
Subjects (aged 18–64 years) participated in the Netherlands Mental Health Survey and Incidence Study-2 (NEMESIS-2), an epidemiological study of the prevalence, incidence, course, and consequences of psychiatric disorders in the Dutch general population. A full description of NEMESIS-2 has been reported elsewhere.24 In short, NEMESIS-2 is based on a multistage, stratified, random sampling of households, with one respondent randomly selected from each household. Insufficient fluency in Dutch was an exclusion criterion.24 The baseline wave included 6,646 subjects, and was conducted from November 2007 to July 2009. The response rate was 65.1%. The sample was nationally representative, although younger participants were somewhat underrepresented.24 This study is based on wave 3, where 4,618 persons of the 5,303 who had completed wave 2 were interviewed (from November 2013 to June 2015). The response rate at wave 3 was 87.8%. Attrition at wave 3 was not significantly associated with all individual 12-month mental disorders at baseline after controlling for sociodemographics.25 The research proposal was approved by a medical ethics committee. At each wave, all participants gave written informed consent at enrollment, after the study procedures had been fully explained.
Measures
Adult ADHD Symptoms
At wave 3, the Adult ADHD Self-Report Scale (ASRS) Screener version 1.126 was used to assess adult ADHD symptoms. There are six items: four indicating inattention symptoms and two indicating hyperactivity symptoms. Symptom frequency was rated over the past 6 months, on a five-point Likert scale ranging from 0 (never) to 4 (very often). Scores on the six items were converted into binary values according to the official scoring system. The ASRS screener has been shown to have moderate sensitivity (68.7%), excellent specificity (99.5%), and excellent total classification accuracy (97.9%) for ADHD.26 Internal consistency reliability of the ASRS Screener has been shown to fall in the range 0.63–0.72.27 Compared to the 18-item version, the ASRS screener is more sensitive and specific, suggesting better classification accuracy.26,27 In this study, severity of ADHD symptoms was determined by the number of scored ADHD symptoms on the ASRS screener, where 0 symptoms was labeled “none,” 1–3 symptoms as “few,” and 4–6 as “clinically relevant ADHD symptoms” which is an indication for a diagnosis of ADHD.27,28 In addition, we assessed ADHD symptoms continuously, using a sum score of possible ratings on the six questions, (range 0–24). For this sum score, we allowed for a maximum of two missing items on the six questions. Where there were missing values, we used the mean of the responses of that individual for the other questions. The ADHD symptom dimensions of hyperactivity and inattention were assessed as continuous variables using a sum score, with a range of 0–8 for the hyperactivity (no missings imputed) and 0–16 for the inattention symptom dimensions (maximally one missing imputed by the mean), respectively.
Sleep Measures
Insomnia symptoms were measured with the Women's Health Initiative Insomnia Rating Scale (IRS),29 which consists of five questions addressing sleep in the past 4 weeks. These address difficulties initiating and maintaining sleep, early morning awakening (two questions), and overall sleep quality. Answers were on a five-point scale, ranging from 0 “less than once a week” to 4 “five times or more a week” for the first four questions, and the last question on sleep quality ranged from 0 “very sound or restful” to 4 “very restless.” For each item, a score of 3 or 4 was considered to suggest pathology. The IRS has good test-retest reliability and has high convergent correlation with objective actigraphy sleep measures.30 In all analyses, the total summary IRS score (0–20) was dichotomized at the cutoff point of 9 or higher, which indicated clinically signifi-cant insomnia symptoms.29 We were interested in the contribution of each of the four domains of insomnia symptoms; hence, we examined these separately in relation to ADHD symptoms.
An additional question investigated total sleep duration. Participants were asked to estimate the average number of hours of sleep per night during the past 4 weeks. Answer options were: “10 or more hours,” “9 hours,” “8 hours,” “7 hours,” “6 hours,” “5 or less hours.” In all analyses, the single variable sleep duration was subcategorized into short (≤ 6 h/night), normal (7–9 h/night), and long (≥ 10 h/night), in accordance with the American Academy of Sleep Medicine and the Sleep Research Society's consensus statement on the recommended amount of sleep for healthy adults.31
Covariates
Worse insomnia symptoms have previously been associated with increased age, female sex, partner status, and lower income.32 Shorter sleep duration has been associated with worse health status, increased cardiovascular risk, presence of depression, and increased body mass index (BMI).33 In the NEMESIS cohort, insomnia was found to be prevalent across different categories of mental disorders.34 Therefore, in this study, we controlled for age, sex, living with a partner (yes/ no), having a paid job (yes/no), chronic somatic disease (presence of one or more of 17 chronic physical disorders treated or monitored by a medical doctor in the previous 12 months, as assessed with a standard checklist), BMI, smoking last month (yes/no), exercise (< 1 h/wk versus ≥ 1 h/wk); and the presence of any 12-month period of a mood, anxiety, or substance use disorder, as determined by the Composite International Diagnostic Interview, version 3.0—a fully structured, lay-administered diagnostic interview. Very few participants (n = 11, 0.2%) reported ADHD medication use. Therefore, we did not include ADHD medication use as a covariate.
Statistical Analyses
We reported general characteristics of the sample using frequencies and percentages for categorical data, in terms of ADHD symptom severity (none, few, clinically relevant). Multivariate logistic regression analyses were performed to demonstrate how the sum scores of ADHD symptom severity and ADHD symptom subtype dimension (hyperactive or inattentive) were associated with the outcome, insomnia symptoms. Multivariate multinomial regression analyses were performed to demonstrate how these associated with sleep duration. Results were adjusted for sex and age in model 1, and additionally for partner status, job status, any chronic somatic disorder, BMI, smoking last month, exercise last week, any 12-month mood, anxiety or substance use disorder in model 2. Results were expressed as adjusted odds ratios or relative risk ratios. All analyses were performed with STATA version 12.1 (Stata-Corp, College Station, Texas, United States), using weighted data to correct for differences in the response rates in several sociodemographic groups and differences in the probability of selection of respondents within households at baseline, with statistical significance inferred at α < .05.
RESULTS
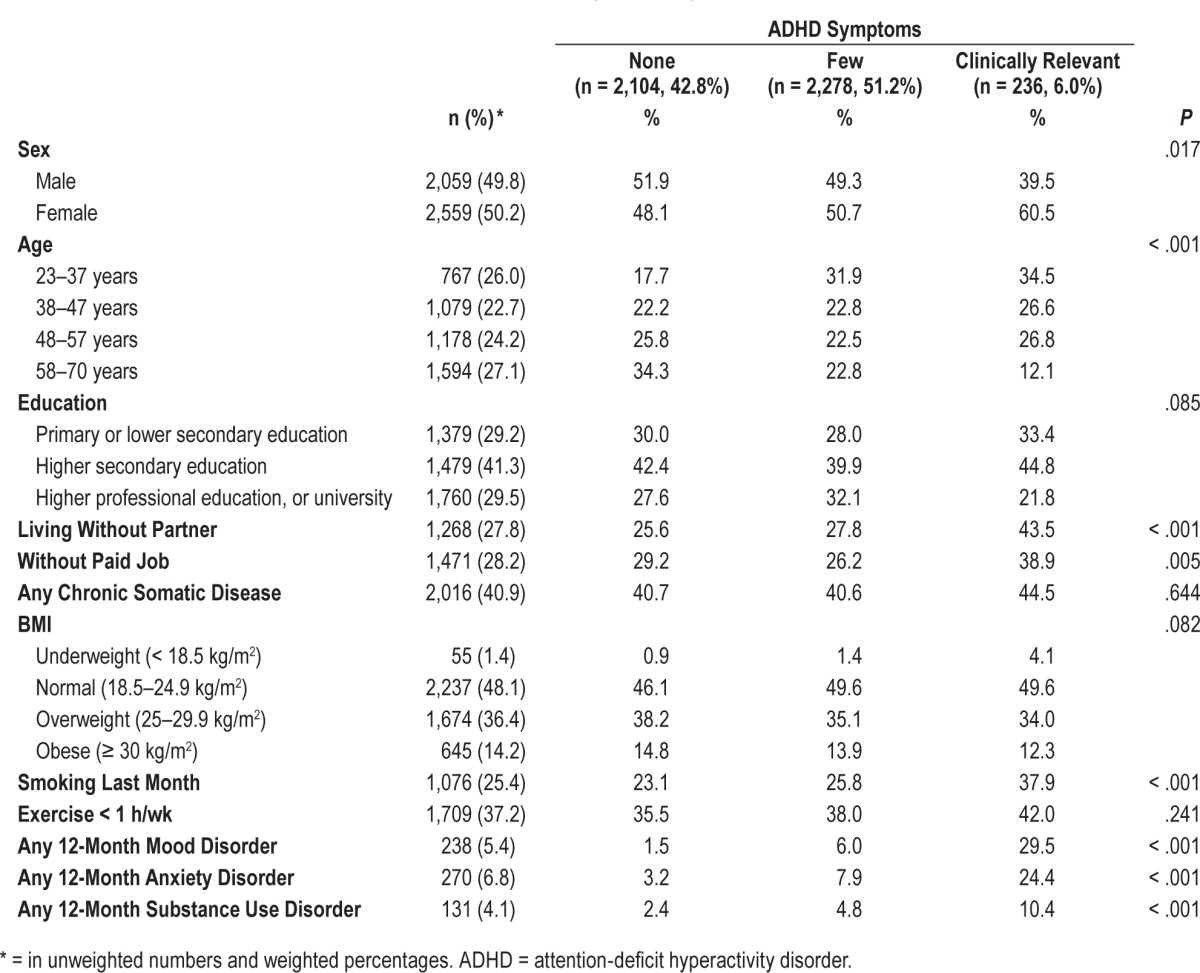
Table 1 describes the sample characteristics of the total sample, across ADHD symptom severity categories (none, few, and clinically relevant). No ADHD symptoms were found in 43% of the sample, 51% reported few symptoms, and 6% reported clinically relevant ADHD symptoms. Clinically relevant ADHD symptoms were significantly associated with female sex (P = .017), younger age group (P < .001), living without a partner (P < .001), not having a paid job (P < .005), smoking in the past month (P < .001), and any 12-month mood/ anxiety/substance use disorder (all P < .001).
Table 1.
Sociodemographic and health characteristics of the total Dutch general population sample (n = 4,618) and across ADHD symptom severity categories (none, few and clinically relevant).
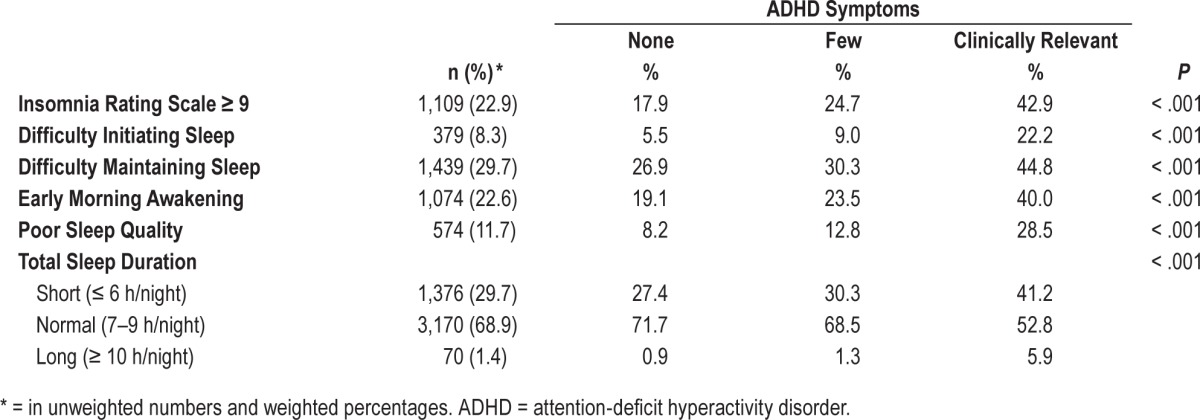
The prevalence of insomnia symptoms and sleep duration across the three ADHD symptom severity groups is described in Table 2. The group with clinically relevant ADHD symptoms had the highest prevalence of clinically significant insomnia symptoms (IRS ≥ 9): 43% reported significant insomnia symptoms, as opposed to 18% in the group with no ADHD symptoms. Those with clinically relevant ADHD symptoms also had the highest prevalence of the separate symptoms defining insomnia (difficulty initiating and maintaining sleep, early morning awakening, poor sleep quality); all P < .001. They also reported longer sleep duration as well as shorter sleep duration more often.
Table 2.
Percentages of insomnia symptoms and other sleeping problems across ADHD symptom severity categories (none, few and clinically relevant) in the general Dutch population sample (n = 4,618).
When we tested the associations between the insomnia variables and ADHD symptom severity groups (with no symptoms as the reference) in partially and fully adjusted logistic regression analyses, the groups with few and clinically relevant ADHD symptoms were significantly associated with all outcome variables in both models (Table 3). The P for trend was also significant for each outcome variable, meaning that across the three categories of increasing ADHD symptom severity (none, few, clinically relevant), there was a significant increase in the odds ratios for insomnia symptoms and relative risk ratios of short and long sleep duration. In the fully adjusted models, the group with clinically relevant ADHD symptoms had more than double the risk of insomnia symptoms and almost double the risk of short sleep duration, compared to the group with no ADHD symptoms.
Table 3.
Ratios of insomnia symptoms and other sleeping problems across ADHD symptom severity categories (none, few, and clinically relevant) in the general Dutch population sample (n = 4,618), using partly and fully adjusted models.
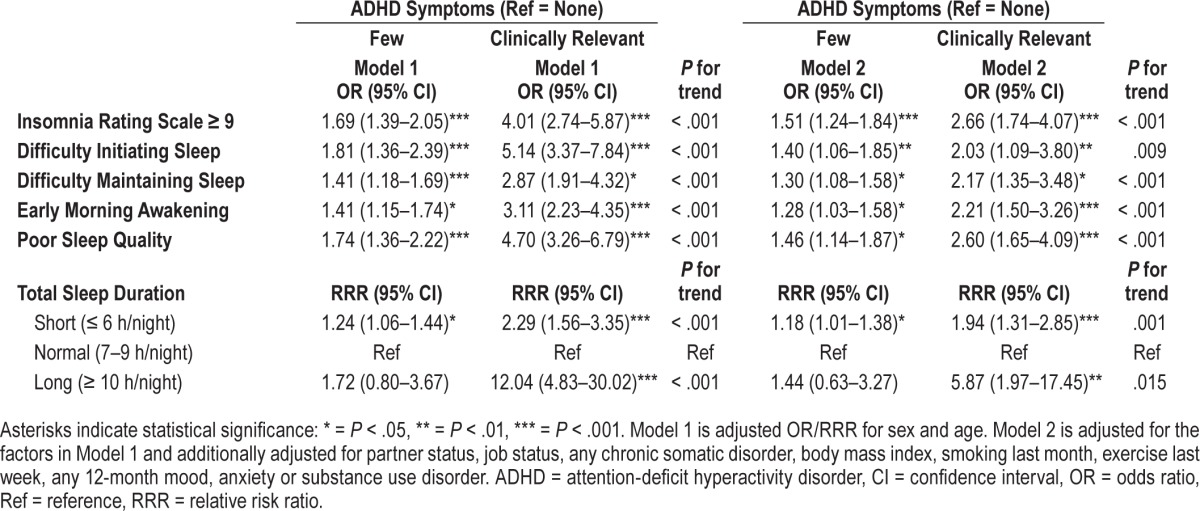
The prevalence of both short (≤ 6 h/night) and long (≥ 10 h/ night) sleep duration was highest in subjects with clinically relevant ADHD symptoms: 6% had long sleep duration, and 41% had short sleep duration (Table 2). An unexpected finding was the significant relationship between clinically relevant ADHD symptoms and long sleep duration (≥ 10 h/night), although the significance level was less strong and the confidence interval quite large (for this specific category P < .01). Overall, these findings as well as those in Table 3 suggest that worsening ADHD symptom severity is significantly associated with insomnia symptoms and altered sleep duration, after adjustment for a wide range of possible confounders, indicating a dose-response association.
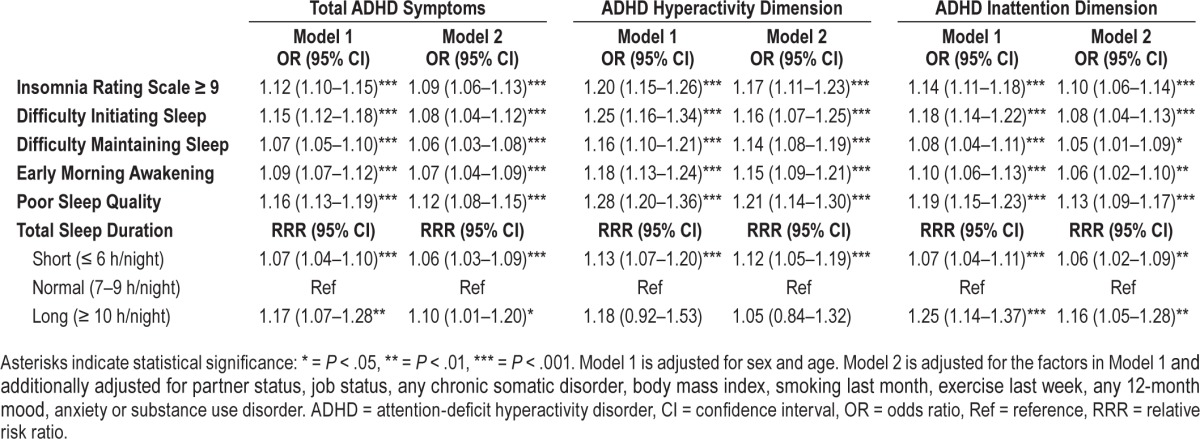
Table 4 describes the associations between insomnia symptoms, sleep duration, total ADHD symptom score, and the two symptom dimensions hyperactivity and inattention. Again, the continuous variables for ADHD symptoms, including hyper-activity and inattention, all show a strongly significant relationship with clinically significant insomnia symptoms in the fully adjusted models (all P < .001). All the separate symptoms defining insomnia showed a significant relationship with ADHD symptoms, hyperactivity and inattention dimensions, assessed continuously, in both models. The predictor variables for all insomnia and sleep duration outcomes did not change markedly with full correction in model 2, demonstrating that the association between ADHD and sleep disturbance is robust, and not attributable to confounding factors. The hyperactivity dimension was significantly associated with short sleep, but not related to long sleep duration.
Table 4.
Ratios of insomnia symptoms and other sleeping problems across total ADHD symptoms, hyperactivity and inattention as continuous ADHD dimension variables, in the general Dutch population sample (n = 4,618), using partly and fully adjusted models.
DISCUSSION
In this study, we evaluated the independent association between adult ADHD symptom severity, ADHD symptom dimensions, insomnia symptoms, and sleep duration. Our results showed two main findings. First, clinically significant insomnia symptoms were strongly and consistently associated with increasing severity of ADHD symptoms, and with the symptom dimensions of hyperactivity and inattention. There was a dose-response relationship between insomnia symptoms and ADHD symptom severity and ADHD symptom dimensions. Second, although self-reported short sleep duration was significantly associated with both inattentive and hyperactive symptom dimensions, long sleep duration was only associated with inattention and not with hyperactivity. After correcting for comorbid psychiatric disorders in the past year (mood, anxiety, and substance use disorders), these associations remained significant. This is noteworthy, because it indicates that even in the general population, these relationships are not attributable to another comorbid disorder.
A dose-response relationship between ADHD symptom severity and insomnia was also found in two large studies8,35 and one smaller clinical study.12 Ours and these three studies included adults aged up to 74 years.8,12,35 However, in a community study of young adults (18–20 years), Gau et al. found no such dose response relationship (n = 2,284).13 The study of Gau et al. may indicate that in young adults, there is less difference in insomnia between those with and without ADHD. Our larger age range may account for more variability in self-reported ADHD and insomnia symptoms. It is also recognized that ADHD persisting into adulthood causes more severe impairment.36 Similarly, insomnia symptoms worsen with increasing age37 and poorer sleep quality in adult ADHD has been attributed to the presence of depressive symptoms.35 We therefore also adjusted for mood and anxiety disorders and yet still found a dose-response relationship between increasing ADHD symptom severity and insomnia.
In terms of the ADHD symptom dimensions and insomnia symptoms, we found that clinically significant insomnia symptoms correlated strongly and significantly with both inattention and hyperactivity symptom dimensions. The research on ADHD subtypes and sleep disturbance to date has been mixed. Insomnia symptoms have been associated with: (1) the number of hyperactivity/impulsivity symptoms12; (2) the combined ADHD and inattentive subtype8; (3) inattentive symptoms only.7,13,38,39 However, one study reported no association.6 We found that insomnia correlated strongly with both inattentive and hyperactive symptoms, even after adjusting for multiple possible confounders, and despite using a population sample, where symptoms tend to be milder than in clinical studies. The clinical study by Fisher et al. (1,163 adults with ADHD) also demonstrated a strong association between adults with ADHD and insomnia, in both ADHD subtypes.6
Our second significant finding was that ADHD symptoms were associated with self-reported short and long sleep duration, as opposed to normal sleep. Our finding replicates the large population study of Bogdan and Reeves, although they did not correct for comorbid affective disorder.14 In other clinical studies, ADHD patients reported shorter sleep duration than controls.40,41 When sleep duration was objectively measured, it was found to be normal in three studies.17–19 Normal sleep duration was also found in two studies using self-report measures.13,20 It is possible that findings for altered sleep duration are less strong when objective sleep measures are used. Finally, a study of 22 adults with ADHD found no correlation between number of ADHD symptoms and sleep duration, a negative finding that may be explained by the small sample size.12
Short sleep duration has been well described in the ADHD literature. Some authors have related it to increased nocturnal motor activity, as measured objectively by polysomnography,17,42–44 although one study did not confirm this.45 Our results significantly associated short sleep and ADHD symptoms. This relationship may be also explained by the presence of a comorbid delayed circadian rhythm disorder, such as delayed sleep phase syndrome.5 Generally, delayed sleep phase syndrome is characterized by a preference for sleep onset after midnight, with consequent difficulty awaking, daytime sleepiness, and impaired functioning.1 Individuals with delayed sleep phase syndrome have sleep onset insomnia when trying to fall asleep early.46 When early rising is necessary, a cumulative sleep debt may arise—meaning that total sleep duration is shorter.
In terms of long sleep in ADHD, we found a strong and significant association with ADHD symptom severity and the inattention symptom dimension, showing a dose-response relationship. Long sleep was far less prevalent than short sleep duration in the ADHD group.
A first possible way to explain long sleep duration associated with ADHD is the presence of an (undiagnosed) comorbid disorder.14 In general, sleep duration shows a U-shaped association with overall mortality, cardiovascular disease, obesity, and diabetes.47 Hence, both short and long sleep duration are detrimental to health. In ADHD, such a comorbid disorder might include hypersomnia, affective disorder, or medical illness. Just as it is important to control for comorbid disorders when investigating insomnia (as mentioned previously), this is also true when investigating sleep duration. We did correct for mood, anxiety, substance, and somatic disorders in the past year, unlike some other studies.12,14,19,48,49 Still, we found that ADHD symptoms and long sleep duration were significantly associated. This implies that an (atypical) subgroup of those with ADHD may exist on the continuum of adult ADHD. Hypersomnia, characterized by excessive daytime sleepiness and prolonged night time sleep, is increased in adults with ADHD compared to controls.5 Hypersomnia may be misdiagnosed as ADHD.5 Hence, where ADHD patients present with long sleep duration, hypersomnia should be excluded or treated. In general, the group with ADHD and long sleep may be at increased risk for overall mortality.47
A second possible explanation for long sleep in ADHD comes from the pediatric literature, where some authors have proposed that instability of the sleep-wake system is a characteristic of children with ADHD.50 This instability (some with long sleep duration, some with short) may also be present in adult ADHD.
Regarding the two ADHD symptom dimensions and sleep duration in adults, there is a dearth of literature. Concurring with two studies, we found that short sleep duration was significantly associated with hyperactivity symptoms.12,13 In a minority of subjects, long sleep duration was significantly associated with both hyperactive and inattentive symptoms. Regarding insomnia symptoms, significant findings in hyper-activity and inattention dimensions were very similar.
A question we were unable to address in our study is whether the treatment of sleep problems in those with ADHD improves the symptoms of inattention and hyperactivity. The cross-sectional nature of our analysis prevented us from analyzing this; however, future studies should examine this important clinical outcome.
Another striking finding was that 60.5% of those with clinically significant ADHD symptoms were females, as opposed to 39.5% males. This result contrasts with findings from the pediatric literature, where male children are more than twice as likely to have ADHD than female children.51 However, ADHD in adult females has been described as underdiagnosed because the symptoms are less overt.52 It has also been shown that the higher prevalence of ADHD in males tends to decrease with increasing age.52 A recent study using the ASRS showed that although more males screened positive for ADHD, a difference between the sexes was not statistically significant.52 Beyond this, we are unable to explain the increased prevalence of clinically relevant ADHD symptoms in females.
Despite the strengths of our study, several limitations should be noted. First, as this study is based on the third wave only and thus uses cross-sectional analyses, a clear causal direction of the relationships found cannot be demonstrated. Second, we relied on retrospective self-reports for ADHD symptoms present over the past 6 months using the Adult ADHD Self-Report Scale screener, which did not include a question about childhood onset of the symptoms. We used retrospective self-reporting for insomnia symptoms (present over the past 4 weeks). According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition diagnostic criteria, insomnia occurs when symptoms occur at least 3 nights/wk over a period of 3 months.1 The IRS does not take duration of symptoms into account; therefore, we probably studied subjects with less severe symptoms, yet still we found significant associations between ADHD and insomnia symptoms. Sleep duration in the past 4 weeks were self-reported measures, where the categories of sleep duration may have limited variability. Yet, previous studies using both self-report measures and polysomnography indicate that long sleepers overestimate and short sleepers underestimate their true sleep duration.47 Third, we controlled for anxiety, depressive, and bipolar disorders but we did not explore the potential overlap between ADHD and bipolar disorders. Bipolar disorder 2 can remain undiagnosed for years and exhibit similar symptoms to ADHD. In NEMESIS-2, the prevalence of all bipolar disorders was 0.8% in the past 12 months.53 The 12-month prevalence of bipolar 2 disorder was 0.6%. This potential overlap would be interesting to investigate further. Fourth, regarding concomitant medication use, very few subjects used ADHD medication (0.2%), so we did not correct for them because we thought the results would not be meaningful. Neither did we correct for medications treating insomnia or hypersomnia. It would be interesting to note whether treatment of sleep disturbance in ADHD improves the core symptoms of this disorder. Finally, in terms of the ADHD symptom dimensions, hyperactivity was determined by only two questions and there was no assessment of impulsivity, a component of ADHD, meaning that we are unable to comment on the relationship between impulsivity symptoms and insomnia/sleep duration.
In conclusion, we have confirmed that increasing symptom severity of ADHD is significantly associated with clinically significant insomnia symptoms, long and short sleep duration, after correction for a range of potential confounders. Both long and short sleep duration were also significantly associated with inattentive symptoms, in fully adjusted models, whereas hyperactive symptoms were associated with short sleep duration only. Adult ADHD and sleep disturbance symptoms are therefore linked with consistent and strong associations. This has serious implications for morbidity in ADHD, as insomnia, short and long sleep duration are all associated with significantly worse daily functioning34 and adverse health outcomes33,47 Where the comorbidities of adult ADHD are unrecognized and untreated, it has been shown that treatment costs increase and patients suffer more adverse long-term outcomes.54 Sleep deprivation also worsens cognitive function.22 In adult ADHD, attention and executive control are already compromised; therefore, insomnia should be recognized and treated. Insomnia can be successfully managed pharmacologically55 and with cognitive behavioral therapy and light therapy.56,57 Such treatments could be used to ameliorate the sleep disturbance we have found to be so prevalent in ADHD. Comorbid insomnia and altered sleep duration should be considered by clinicians treating these complex patients, to reduce suffering and improve functioning.
DISCLOSURE STATEMENT
Work for this study was performed at PsyQ Expertise Center Adult ADHD, The Hague and Trimbos Institute, Utrecht. All authors have seen and approve of the manuscript. The Netherlands Mental Health Survey and Incidence Study-2 (NEMESIS-2) is conducted by the Netherlands Institute of Mental Health and Addiction (Trimbos Institute) in Utrecht, The Netherlands. Financial support has been received from the Ministry of Health, Welfare and Sport, with supplemental support from the Netherlands Organization for Health Research and Development (ZonMw) and the Genetic Risk and Outcome of Psychosis (GROUP) investigators. These organizations had no further role in study design, collection, analysis and interpretation of data, writing of the report, and in the decision to submit the paper for publication. D. Wynchank has served on the advisory boards of Janssen BV, Novartis and Eli Lilly for activities outside the scope of this paper (2009–2014). Dr. Lamers has received funding from the European Union Seventh Framework Program (FP7/2007-2013) under grant agreement n° PCIG12-GA-2012-334065 for other activities outside the scope of this paper. Prof. Penninx has received research grants from Johnson & Johnson, Boehringer Ingelheim, NWO, BBRMI-NL, NIMH, and the EU-FP7 program (2014–2021) for research in the Netherlands Study of Depression and Anxiety (NESDA), activities outside the scope of this paper. Prof. Beekman has received funds through the speakers' bureau of Lundbeck and Eli Lilly. Dr. Kooij, Dr. Bijlenga, Dr. ten Have, and Dr. de Graaf declare no financial or other relationship relevant to the subject of this article.
ABBREVIATIONS
- ADHD
attention-deficit hyperactivity disorder
- ASRS
Adult ADHD Self-Report Scale Screener, version 1.1
- BMI
body mass index
- IRS
Women's Health Initiative Insomnia Rating Scale
- NEMESIS-2
Netherlands Mental Health Survey and Incidence Study-2
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington DC: American Psychiatric Association; 2013. [Google Scholar]
- 2.Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- 3.Fayyad J, Sampson NA, Hwang I, et al. The descriptive epidemiology of DSMIV Adult ADHD in the World Health Organization World Mental Health Surveys. Atten Defic Hyperact Disord. 2017;9(1):47–65. doi: 10.1007/s12402-016-0208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marcus DK, Barry TD. Does attention-deficit/hyperactivity disorder have a dimensional latent structure? A taxometric analysis. J Abnorm Psychol. 2011;120(2):427–442. doi: 10.1037/a0021405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Instanes JT, Klungsoyr K, Halmoy A, Fasmer OB, Haavik J. Adult ADHD and comorbid somatic disease: a systematic literature review. J Atten Disord. 2018;22(3):203–228. doi: 10.1177/1087054716669589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fisher BC, Garges DM, Yoon SYR, Maguire K, Zipay D, Gambino AM. Sex differences and the interaction of age and sleep issues in neuropsychological testing performance across the lifespan in an add/adhd sample from the years 1989 to 2009. Psychol Rep. 2014;114(2):404–438. doi: 10.2466/15.10.PR0.114k23w0. [DOI] [PubMed] [Google Scholar]
- 7.Voinescu BI, Szentagotai A, David D. Sleep disturbance, circadian preference and symptoms of adult attention deficit hyperactivity disorder (ADHD) J Neural Transm (Vienna) 2012;119(10):1195–1204. doi: 10.1007/s00702-012-0862-3. [DOI] [PubMed] [Google Scholar]
- 8.Brevik EJ, Lundervold AJ, Halmoy A, et al. Prevalence and clinical correlates of insomnia in adults with attention-deficit hyperactivity disorder. Acta Psychiatr Scand. 2017;136(2):220–227. doi: 10.1111/acps.12756. [DOI] [PubMed] [Google Scholar]
- 9.Fuller-Thomson E, Lewis DA, Agbeyaka SK. Attention-deficit/hyperactivity disorder casts a long shadow: findings from a population-based study of adult women with self-reported ADHD. Child Care Health Dev. 2016;42(6):918–927. doi: 10.1111/cch.12380. [DOI] [PubMed] [Google Scholar]
- 10.Gregory AM, Agnew-Blais JC, Matthews T, Moffitt TE, Arseneault L. ADHD and sleep quality: longitudinal analyses from childhood to early adulthood in a twin cohort. J Clin Child Adolesc Psychol. 2017;46(2):284–294. doi: 10.1080/15374416.2016.1183499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldman-Mellor S, Gregory AM, Caspi A, et al. Mental health antecedents of early midlife insomnia: evidence from a four-decade longitudinal study. Sleep. 2014;37(11):1767–1775. doi: 10.5665/sleep.4168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahajan N, Hong N, Wigal TL, Gehricke JG. Hyperactive-impulsive symptoms associated with self-reported sleep quality in nonmedicated adults with ADHD. J Atten Disord. 2010;14(2):132–137. doi: 10.1177/1087054709347170. [DOI] [PubMed] [Google Scholar]
- 13.Gau SS, Kessler RC, Tseng WL, et al. Association between sleep problems and symptoms of attention-deficit/hyperactivity disorder in young adults. Sleep. 2007;30(2):195–201. doi: 10.1093/sleep/30.2.195. [DOI] [PubMed] [Google Scholar]
- 14.Bogdan AR, Reeves KW. Sleep duration in relation to attention deficit hyperactivity disorder in American adults. Behav Sleep Med. 2016. Jun 20, doi: 10.1080/15402002.2016.1188391. [Epub ahead of print] [DOI] [PubMed]
- 15.Bron TI, Bijlenga D, Kooij JJ, et al. Attention-deficit hyperactivity disorder symptoms add risk to circadian rhythm sleep problems in depression and anxiety. J Affect Disord. 2016;200:74–81. doi: 10.1016/j.jad.2016.04.022. [DOI] [PubMed] [Google Scholar]
- 16.Gamble KL, May RS, Besing RC, Tankersly AP, Fargason RE. Delayed sleep timing and symptoms in adults with attention-deficit/hyperactivity disorder: a controlled actigraphy study. Chronobiol Int. 2013;30(4):598–606. doi: 10.3109/07420528.2012.754454. [DOI] [PubMed] [Google Scholar]
- 17.Philipsen A, Feige B, Hesslinger B, et al. Sleep in adults with attention-deficit/ hyperactivity disorder: a controlled polysomnographic study including spectral analysis of the sleep EEG. Sleep. 2005;28(7):877–884. doi: 10.1093/sleep/28.7.877. [DOI] [PubMed] [Google Scholar]
- 18.Sobanski E, Schredl M, Kettler N, Alm B. Sleep in adults with attention deficit hyperactivity disorder (ADHD) before and during treatment with methylphenidate: a controlled polysomnographic study. Sleep. 2008;31(3):375–381. doi: 10.1093/sleep/31.3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Veen MM, Kooij JJ, Boonstra AM, Gordijn MC, van Someren EJ. Delayed circadian rhythm in adults with attention-deficit/hyperactivity disorder and chronic sleep-onset insomnia. Biol Psychiatry. 2010;67(11):1091–1096. doi: 10.1016/j.biopsych.2009.12.032. [DOI] [PubMed] [Google Scholar]
- 20.Wynchank DS, Bijlenga D, Lamers F, et al. ADHD, circadian rhythms and seasonality. J Psychiatr Res. 2016;81:87–94. doi: 10.1016/j.jpsychires.2016.06.018. [DOI] [PubMed] [Google Scholar]
- 21.Hobson JA, Pace-Schott EF. The cognitive neuroscience of sleep: neuronal systems, consciousness and learning. Nat Rev Neurosci. 2002;3(9):679–693. doi: 10.1038/nrn915. [DOI] [PubMed] [Google Scholar]
- 22.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117–126. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 23.Yoon SYR, Jain U, Shapiro C. Sleep in attention-deficit/hyperactivity disorder in children and adults: past, present, and future. Sleep Med Rev. 2012;16(4):371–388. doi: 10.1016/j.smrv.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 24.de Graaf R, Ten Have M, van Dorsselaer S. The Netherlands Mental Health Survey and Incidence Study-2 (NEMESIS-2): design and methods. Int J Methods Psychiatr Res. 2010;19(3):125–141. doi: 10.1002/mpr.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Graaf R, van Dorsselaer S, Tuithof M, ten Have M. Sociodemographic and psychiatric predictors of attrition in the third wave of the Netherlands Mental Health Survey and Incidence Study-2 (NEMESIS-2) Utrecht, The Netherlands: Trimbos Institute; 2015. [Google Scholar]
- 26.Kessler RC, Adler L, Ames M, et al. The World Health Organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35(2):245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, Adler LA, Gruber MJ, Sarawate CA, Spencer T, Van Brunt DL. Validity of the World Health Organization Adult ADHD Self-Report Scale (ASRS) screener in a representative sample of health plan members. Int J Methods Psychiatr Res. 2007;16(2):52–65. doi: 10.1002/mpr.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vogel SW, Ten Have ML, Bijlenga D, de Graaf R, Beekman AT, Kooij JJ. Seasonal variations in the severity of ADHD symptoms in the Dutch general population. J Atten Disord. 2016 May 19; doi: 10.1177/1087054716649663. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Levine DW, Kaplan RM, Kripke DF, Bowen DJ, Naughton MJ, Shumaker SA. Factor structure and measurement invariance of the Women's Health Initiative Insomnia Rating Scale. Psychol Assess. 2003;15(2):123–136. doi: 10.1037/1040-3590.15.2.123. [DOI] [PubMed] [Google Scholar]
- 30.Levine DW, Kripke DF, Kaplan RM, et al. Reliability and validity of the Women's Health Initiative Insomnia Rating Scale. Psychol Assess. 2003;15(2):137–148. doi: 10.1037/1040-3590.15.2.137. [DOI] [PubMed] [Google Scholar]
- 31.Watson NF, Badr MS, Belenky G, et al. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. J Clin Sleep Med. 2015;11(8):931–952. doi: 10.5664/jcsm.4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grandner MA, Petrov ME, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9(9):897–905. doi: 10.5664/jcsm.2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cepeda MS, Stang P, Blacketer C, Kent JM, Wittenberg GM. Clinical relevance of sleep duration: results from a cross-sectional analysis using NHANES. J Clin Sleep Med. 2016;12(6):813–819. doi: 10.5664/jcsm.5876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ten Have M, Penninx BW, van Dorsselaer S, Tuithof M, Kleinjan M, de Graaf R. Insomnia among current and remitted common mental disorders and the association with role functioning: results from a general population study. Sleep Med. 2016;25:34–41. doi: 10.1016/j.sleep.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 35.Schredl M, Alm B, Sobanski E. Sleep quality in adult patients with attention deficit hyperactivity disorder (ADHD) Eur Arch Psychiatry Clin Neurosci. 2007;257(3):164–168. doi: 10.1007/s00406-006-0703-1. [DOI] [PubMed] [Google Scholar]
- 36.Lara C, Fayyad J, de Graaf R, et al. Childhood predictors of adult attention-deficit/hyperactivity disorder: results from the World Health Organization World Mental Health Survey Initiative. Biol Psychiatry. 2009;65(1):46–54. doi: 10.1016/j.biopsych.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vaz Fragoso CA, Gill TM. Sleep complaints in community-living older persons: a multifactorial geriatric syndrome. J Am Geriatr Soc. 2007;55(11):1853–1866. doi: 10.1111/j.1532-5415.2007.01399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kass SJ, Wallace JC, Vodanovich SJ. Boredom proneness and sleep disorders as predictors of adult attention deficit scores. J Atten Disord. 2003;7(2):83–91. doi: 10.1177/108705470300700202. [DOI] [PubMed] [Google Scholar]
- 39.Arns M, Feddema I, Kenemans JL. Differential effects of theta/beta and SMR neurofeedback in ADHD on sleep onset latency. Front Hum Neurosci. 2014;8:1019. doi: 10.3389/fnhum.2014.01019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bijlenga D, Van Someren EJ, Gruber R, et al. Body temperature, activity and melatonin profiles in adults with attention-deficit/hyperactivity disorder and delayed sleep: a case-control study. J Sleep Res. 2013;22(6):607–616. doi: 10.1111/jsr.12075. [DOI] [PubMed] [Google Scholar]
- 41.Voinescu B, Szentagotai A, Thome J. Sleep disturbance and attention deficit/ hyperactivity symptoms [abstract] European Psychiatry. 2012;27(Suppl 1):1. [Google Scholar]
- 42.Middelkoop HA, Van Gils K, Kooij JJ. Adult attention-deficit hyperactivity disorder (ADHD): actimetric evaluation of nocturnal motor activity and subjective sleep characteristics. [Accessed January 30, 2018]. http://www.nswo.nl/publicaties/jaarboeken/jaarboek-1997. Published 1997.
- 43.Kooij JJ, Middelkoop HA, van Gils K, Buitelaar JK. The effect of stimulants on nocturnal motor activity and sleep quality in adults with ADHD: an open-label case-control study. J Clin Psychiatry. 2001;62(12):952–956. doi: 10.4088/jcp.v62n1206. [DOI] [PubMed] [Google Scholar]
- 44.Sobanski E, Bruggemann D, Alm B, et al. Subtype differences in adults with attention-deficit/hyperactivity disorder (ADHD) with regard to ADHD-symptoms, psychiatric comorbidity and psychosocial adjustment. Eur Psychiatry. 2008;23(2):142–149. doi: 10.1016/j.eurpsy.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 45.Boonstra AM, Kooij JJS, Oosterlaan J, Sergeant JA, Buitelaar JK, Van Someren EJW. Hyperactive night and day? Actigraphy studies in adult ADHD: a baseline comparison and the effect of methylphenidate. Sleep. 2007;30(4):433–442. doi: 10.1093/sleep/30.4.433. [DOI] [PubMed] [Google Scholar]
- 46.Bijlenga D, Van Someren EJW, Gruber R, et al. Body temperature, activity and melatonin profiles in adults with attention-deficit/hyperactivity disorder and delayed sleep: a case-control study. J Sleep Res. 2013;22(6):607–616. doi: 10.1111/jsr.12075. [DOI] [PubMed] [Google Scholar]
- 47.Patel SR, Zhu X, Storfer-Isser A, et al. Sleep duration and biomarkers of inflammation. Sleep. 2009;32(2):200–204. doi: 10.1093/sleep/32.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sangal RB, Sangal JM. Rating scales for inattention and sleepiness are correlated in adults with symptoms of sleep disordered breathing syndrome, but not in adults with symptoms of attention-deficit/hyperactivity disorder. Sleep Med. 2004;5(2):133–135. doi: 10.1016/j.sleep.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 49.Baird AL, Coogan AN, Siddiqui A, Donev RM, Thome J. Adult attention-deficit hyperactivity disorder is associated with alterations in circadian rhythms at the behavioural, endocrine and molecular levels. Mol Psychiatry. 2012;17(10):988–995. doi: 10.1038/mp.2011.149. [DOI] [PubMed] [Google Scholar]
- 50.Gruber R, Sadeh A, Raviv A. Instability of sleep patterns in children with attention- deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2000;39(4):495–501. doi: 10.1097/00004583-200004000-00019. [DOI] [PubMed] [Google Scholar]
- 51.Ramtekkar UP, Reiersen AM, Todorov AA, Todd RD. Sex and age differences in attention-deficit/hyperactivity disorder symptoms and diagnoses: implications for DSM-V and ICD-11. J Am Acad Child Adolesc Psychiatry. 2010;49(3):217–228.e3. [PMC free article] [PubMed] [Google Scholar]
- 52.Corbisiero S, Hartmann-Schorro RM, Riecher-Rössler A, Stieglitz RD. Screening for adult attention-deficit/hyperactivity disorder in a psychiatric outpatient population with specific focus on sex differences. Front Psychiatr. 2017;30(8):115. doi: 10.3389/fpsyt.2017.00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.de Graaf R, ten Have M, van Gool C, van Dorsselaer S. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health and Incidence Study-2. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):203–213. doi: 10.1007/s00127-010-0334-8. [DOI] [PubMed] [Google Scholar]
- 54.Kawatkar AA, Knight TK, Moss RA, et al. Impact of mental health comorbidities on health care utilization and expenditure in a large US managed care adult population with ADHD. Value Health. 2014;17(6):661–668. doi: 10.1016/j.jval.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 55.Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(2):307–349. doi: 10.5664/jcsm.6470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ballesio A, Aquino MR, Feige B, et al. The effectiveness of behavioural and cognitive behavioural therapies for insomnia on depressive and fatigue symptoms: a systematic review and network meta-analysis. Sleep Med Rev. 2018;37:114–129. doi: 10.1016/j.smrv.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 57.van Maanen A, Meijer AM, van der Heijden KB, Oort FJ. The effects of light therapy on sleep problems: a systematic review and meta-analysis. Sleep Med Rev. 2016;29:52–62. doi: 10.1016/j.smrv.2015.08.009. [DOI] [PubMed] [Google Scholar]


