Abstract
Study Objectives:
Obstructive sleep apnea (OSA) and chronic insomnia are two common sleep disorders and both are considered independent risk factors for heart disease. The aim of this study was to investigate the prevalence of comorbid insomnia with OSA and to compare its clinical characteristics with those of OSA without insomnia.
Methods:
Patients who visited two tertiary university hospital sleep centers were screened. Those with a diagnosis of OSA using polysomnography were divided into two groups based on their scores on the Korean version of the Insomnia Severity Index (ISI-K): OSA with insomnia (OSA+I) (ISI-K score ≥ 15) and OSA without insomnia (OSA−I) (ISI-K score < 15). Subjective symptoms were evaluated using sleep questionnaires including ISI-K. Demographic and clinical characteristics of OSA+I and OSA−I were compared.
Results:
Out of 476 patients with OSA, 139 (29.2%) had significant insomnia. Patients in the OSA+I group had a higher percentage of females (35.3% versus 19.6%, P < .001) and have higher rates of heart disease (19.4% versus 8.6%, P < .001). OSA+I group showed lower quality of life, lower quality of sleep, higher sleep propensity, and higher depression as measured by the Korean versions of the Short-Form 36-Item Health Survey, Pittsburgh Sleep Quality Index, Epworth Sleepiness Scale, and Beck Depression Inventory, respectively. There were no significant differences in adherence to continuous positive airway pressure between the groups.
Conclusions:
There is a high prevalence of comorbid insomnia with OSA (29.2%), consistent with previous findings in Western studies. Comorbid insomnia with OSA may constitute a cumulative risk factor for cardiovascular disease. These findings warrant further investigation into the mechanisms involved in its pathogenesis and devising more efficient treatments.
Citation:
Cho YW, Kim KT, Moon H, Korostyshevskiy VR, Motamedi GK, Yang KI. Comorbid insomnia with obstructive sleep apnea: clinical characteristics and risk factors. J Clin Sleep Med. 2018;14(3):409–417.
Keywords: comorbid insomnia, heart disease, obstructive sleep apnea
BRIEF SUMMARY
Current Knowledge/Study Rationale: Obstructive sleep apnea (OSA) and insomnia are very common and both have been independently associated with other serious medical conditions such as cardiovascular disease, cerebrovascular disease, depression, dementia, and cancer. There is some evidence indicating a high prevalence of coexisting insomnia in OSA; however, there are insufficient data on its epidemiology, risk factors, and possibly added risks associated with it.
Study Impact: We have studied the prevalence, associated risk factors, and potential consequences of comorbid insomnia with OSA. There are a fair number of patients with comorbid insomnia and OSA with worsened quality of life and sleep. Comorbid insomnia in OSA is linked to heart disease. Further characterization of this syndrome may help to increase awareness and promote further investigation into its pathogenesis, prevention, and treatment.
INTRODUCTION
Obstructive sleep apnea (OSA) and insomnia are among the most common sleep disorders. They are often thought of as opposing clinical conditions, with OSA viewed as a contributing factor to daytime somnolence, in contrast, insomnia being closely related to nighttime hyperarousal.1 OSA is characterized by repetitive upper airway closure or narrowing during sleep, causing snoring, sleep fragmentation, oxygen desatu-ration, and sleep propensity, whereas insomnia is associated with difficulty initiating or maintaining sleep, waking earlier than desired with inability to return to sleep, or a combination of all three, resulting in significant daytime impairment. Polysomnography (PSG) is essential for the diagnosis of OSA and measuring its severity by establishing apnea-hypopnea index (AHI). The Insomnia Severity Index (ISI) is widely used as a valid screening measure of insomnia as well as an outcome measure following treatment.2,3
Since the “sleep-insomnia apnea syndrome” was reported in 1973,4 this clinical syndrome has gained attention and prompted additional studies. Emerging data suggest that insomnia and OSA often coexist. In 2001, the term “sleep disordered breathing-plus” was used to refer to patients with coexisting OSA and chronic insomnia with a high prevalence of 50% among patients with OSA.5 A prospective study reported that 39% of patients with OSA had comorbid insomnia.6 However, it has been shown that 10.7% of patients in whom insomnia has been diagnosed have clinically significant OSA.7
Despite its significant prevalence, the association between the insomnia/sleep apnea syndrome and risk of cardiovascular disease has not been extensively studied. Although OSA is an established risk factor for cardiovascular disease,8 data on insomnia are inconsistent,9,10 with some evidence supporting its role as a risk factor for cardiovascular diseases.11–13 Therefore, patients with OSA with comorbid insomnia may carry an equal or higher risk of cardiovascular diseases compared to individuals with OSA alone.13–15
The aim of this study was to investigate the prevalence of comorbid insomnia in a group of patients in whom OSA was previously diagnosed, and to compare the clinical characteristics of patients with OSA and insomnia to patients with OSA without insomnia.
METHODS
Participants and Data
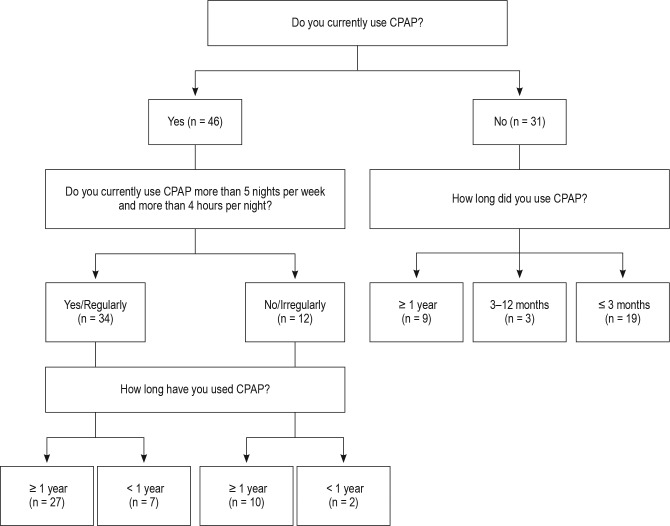
The study was approved and conducted in compliance with the regulations set by the Institutional Review Board. We retrospectively screened all adult patients who had a full-night PSG at two different tertiary university hospital sleep centers in South Korea between January 2013 and November 2015. Based on the PSG and clinical findings, 594 patients received a diagnosis of OSA16,17; no patients had prior history of treatment for OSA. Inclusion criteria were ages 20–75 years and an AHI of ≥ 5 events/h. In our sleep laboratories, we use AHI to define the severity of OSA instead of respiratory effort-related arousals and the respiratory disturbance index. We excluded OSA with comorbid sleep disorders other than insomnia (ie, restless legs syndrome, narcolepsy, parasomnia, and epilepsy) (Figure 1). A total of 476 adult patients with OSA were enrolled in this study.
Figure 1. Patient selection flowchart.
AHI = apnea-hypopnea index, ISI-K = Insomnia Severity Index, Korean version, OSA = obstructive sleep apnea, PSG = polysomnography, RLS = restless legs syndrome.
The PSG tests were performed using 32-channel Grass-Telefactor Comet digital recording polysomnographic system (Natus Medical Incorporated, Pleasanton, California, United States) and were manually scored.18 Scoring of sleep stages, respiratory events including apneas, hypopneas, arousal, and periodic limb movement were performed according to the American Academy of Sleep Medicine guidelines.19 Apnea was defined as a drop in the peak signal excursion by greater than or equal to 90% of the preevent baseline using an oronasal thermal sensor lasting for 10 seconds or longer. Hypopnea was defined as a nasal pressure signal drop to more than 30% of baseline that lasted for 10 seconds or longer and was associated with either more than 3% oxygen desaturation or an arousal.20 Sleep onset latency, wake after sleep onset, and sleep efficiency were recorded. Arousal index was recorded both as total, as well as three subcategories of apnea-related, periodic limb movement-related, and spontaneous.
Health conditions were evaluated using a questionnaire inquiring about heart disease, hypertension (HTN), diabetes mellitus (DM), hyperlipidemia (HL), and current smoking habits. Smokers were classified by their use of tobacco, regardless of the amount. Heart disease included ischemic heart disease, arrhythmia, and valvular disease. Subjects with any cardiac history or current medications for heart disease were classified as having heart disease. There were no subjects with congenital heart disease. All subjects with HTN, DM, and HL were under the care of a physician. All subjects completed sleep-related and psychiatric questionnaires including the Korean versions of the Insomnia Severity Index (ISI-K),2 the Pittsburgh Sleep Quality Index (PSQI-K),21 the Epworth Sleepiness Scale (ESS-K),22 the Beck Depression Inventory (BDI-2-K),23 and the Short-Form 36-Item Health Survey (SF-36-K).24 The results from these questionnaires were compared between male and female patients. As the ISI-K measures symptoms other than sleepiness (eg, worry, distress, and daytime interference, which are shared with OSA), we analyzed the results using the subtotal of ISI-K score in the first three sleep items.25
We considered insomnia as an independent entity as defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)26 without stratifying it into different subtypes. A validated questionnaire, ISI-K, was used to measure the patients' perception of insomnia.2 ISI-K is a seven-item self-reported questionnaire measuring daytime effect as well as impairments caused by insomnia. An ISI score of 15 or greater is considered clinically significant.2 The patients were divided into two groups based on their ISI-K score. Those with an ISIK score ≥ 15 were categorized as OSA with insomnia (OSA+I), and those with an ISI-K score < 15 were categorized as OSA without insomnia (OSA−I). Given the mismatch between abnormal PSG findings and clinical symptoms in some elderly patients, prior studies have used sleepiness as an added screening tool.27 Sleep propensity was defined as ESS-K score ≥ 11.22 In what follows, we refer to OSA+I and OSA−I groups as “the two groups” for brevity.
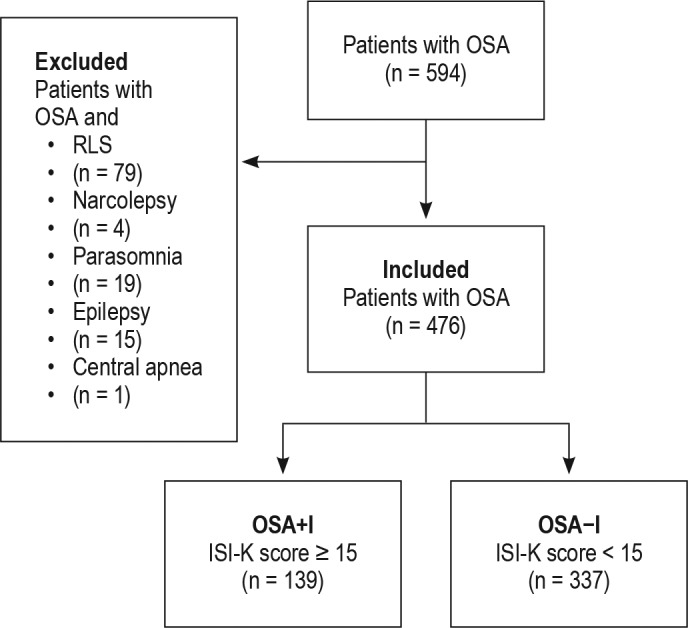
Demographic and clinical characteristics were compared between the two groups, as well as the subgroups of OSA−I based on ESS-K (Table 1). We also screened 77 patients who had started treatment with continuous positive airway pressure (CPAP), and telephone interviews were conducted in order to investigate differences in CPAP adherence between the two groups. A questionnaire was used for the telephone interviews that included current use of CPAP, average hours used per night, the number of nights per week, duration of use, and the reason for discontinuation. We defined adherence as using CPAP for more than 4 hours per night and more than 5 nights per week.28 All subjects were contacted in order to assess their adherence by using a questionnaire that was designed for this purpose (Figure 2).
Table 1.
Demographic and clinical characteristics.
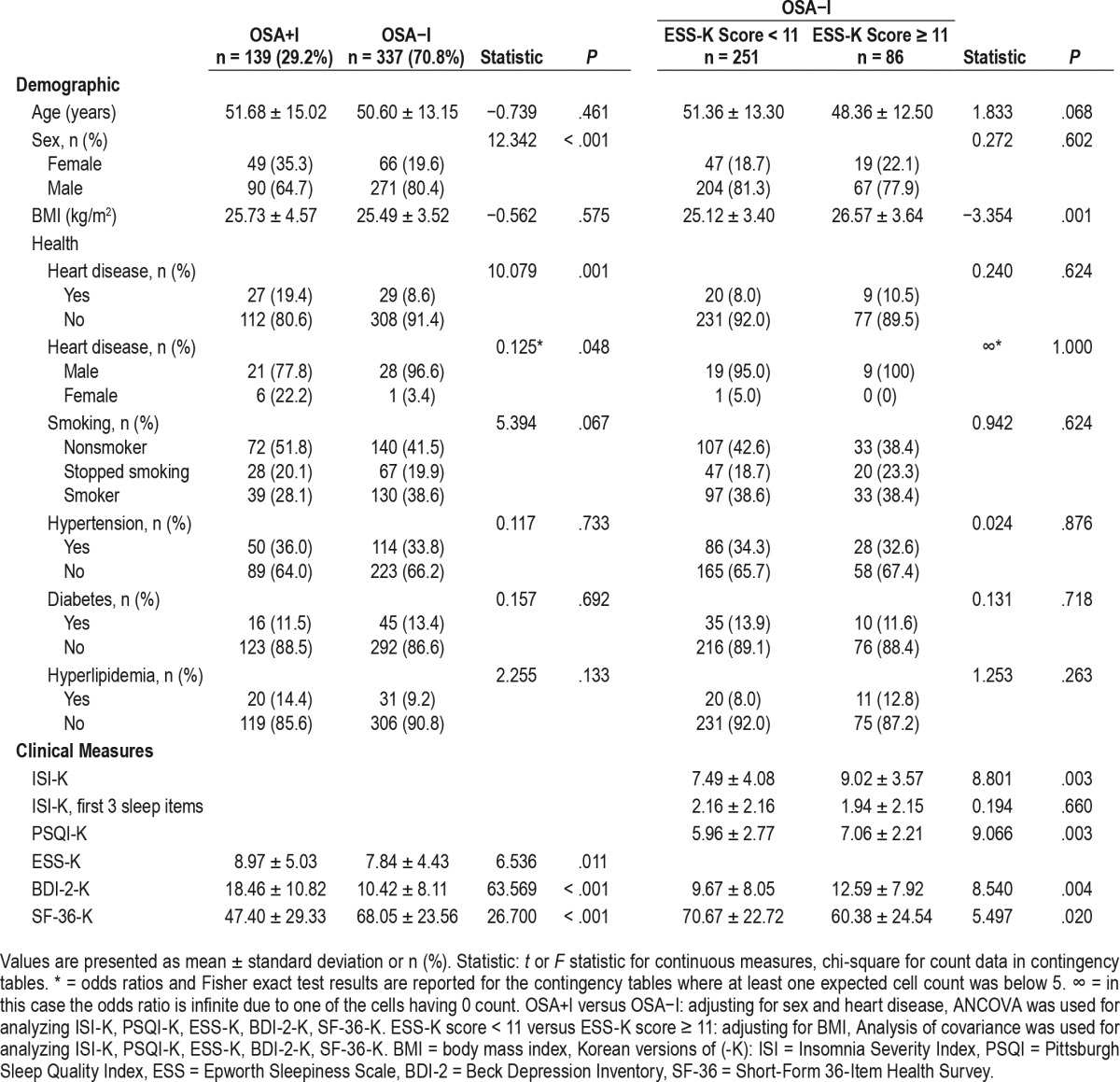
Figure 2. Telephone interview questionnaire.
This algorithm was used to determine CPAP adherence in patients with OSA. CPAP = continuous positive airway pressure, OSA = obstructive sleep apnea.
Statistical Analysis
Data analysis was performed using SPSS version 25 (IBM Corp., Armonk, New York, United States). Values of P < .05 were considered statistically significant. The reported P values were rounded to the third decimal point or reported as < .001 when applicable. Chi-square test and Fisher exact test were used to analyze count data (sex and medical conditions), and independent t test was used to analyze continuous data between the two groups (age and body mass index [BMI]). For analyzing the differences in sleep-related (severity of insomnia and sleep propensity, sleep quality, PSG data) and psychiatric-related characteristics (depressive mood, quality of life [QoL], and anxiety) between the two groups, we used analysis of covariance to adjust for sex and heart disease (which showed significant differences in demographic characteristics). Logistic regression was used to determine the risk factors for insomnia in patients with OSA. Pearson correlation was used to analyze correlation between severity of insomnia, sleep propensity, and severity of OSA.
RESULTS
Of the 476 patients with OSA (mean age 50.91 ± 13.71 years; 115 [24.2%] female) that were diagnosed by PSG, 139 patients (29.2%) had clinically significant insomnia (ISI-K score ≥ 15). This OSA+I group had a higher percentage of females than the OSA−I group consisting of 337 subjects (35.3% versus 19.6%, P < .001), and an increased risk of heart disease (19.4% versus 8.6%, P < .001) (Table 1). There were no statistically signifi-cant differences in age, BMI, and vascular risk factors (HTN, smoking, DM, and HL) between the two groups. Subjects in the OSA+I group had lower QoL (SF-36-K: 47.40 ± 29.33 versus 68.05 ± 23.56, P < .001), and more depressed mood (BDI-2-K: 18.46 ± 10.82 versus 10.42 ± 8.11, P < .001) (Table 1). Patients in the OSA+I group were sleepier than those in the OSA−I group. When comparing subgroups, those with an ESS-K score ≥ 11 in the OSA−I group were sleepier than those in the OSA+I group, and had a higher PSQI-K score and a lower SF-36-K score than those in the OSA−I group with an ESS-K score < 11.
Comparing OSA and insomnia severity between males and females showed that females had more insomnia symptoms (42.6% versus 24.9%, P < .001), while males had more severe OSA (52.4% versus 27.0%, AHI ≥ 30, P < .001). In the absence of detailed information about the presence or absence of menopause, an age cutoff of 50 years was used for females for further analysis. There was no statistically significant difference in OSA and insomnia severity between females older and younger than 50 years.
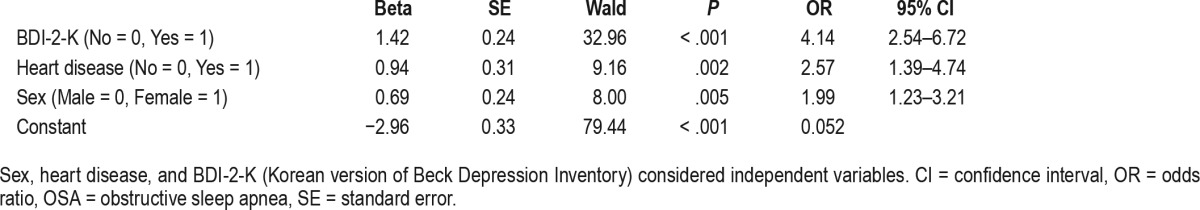
The OSA+I group had lower total sleep time (313.06 ± 80.88 versus 337.14 ± 70.28 minutes, P = .006), lower sleep efficiency (75.45 ± 17.30 versus 80.06 ± 14.74 %, P = .006), and longer sleep onset latency (19.12 ± 39.27 versus 12.78 ± 22.83 minutes, P = .013) compared to the OSA−I group (Table 2). However, there were no statistically significant differences in percentage of sleep stages or AHI between the two groups. When comparing the subgroups of the OSA−I group, there were no significant differences in sleep parameters between those with an ESS-K score ≥ 11 and those with an ESS-K score < 11. Analyzing the data stratified by OSA severity (5 ≤ AHI < 15, 15 ≤ AHI < 30, AHI ≥ 30), the AHI ≥ 30 group showed higher rates of HTN and DM. Correlation analysis did not show any association between severity of OSA and severity of insomnia (P = .999) or sleep propensity (P = .359) (Table 3). In logistic regression, in order to compare the OSA+I and OSA−I groups, the following factors were included as independent variables: sex, heart disease, and BDI-2-K score. The results showed that the contributing factors to insomnia symptoms in patients with OSA were depressive mood (odds ratio: 4.14), heart disease (odds ratio: 2.57), and sex (odds ratio: 1.99), with heart disease being the second most influential factor (Table 4).
Table 2.
Polysomnography results.
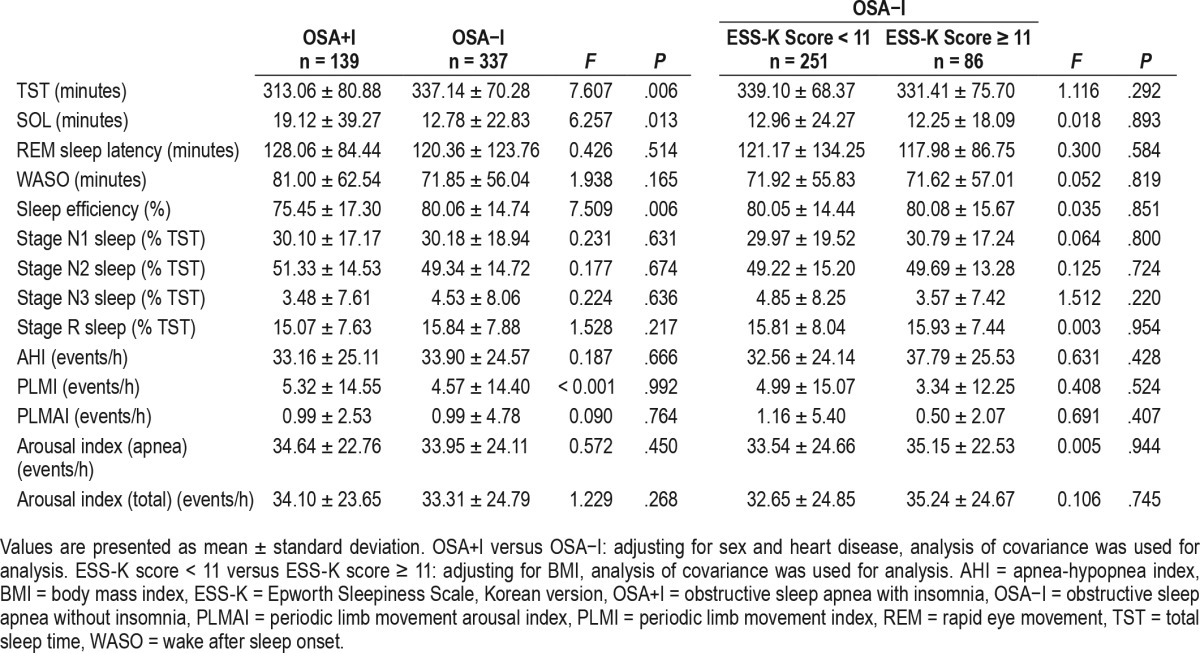
Table 3.
Medical conditions and OSA severity.
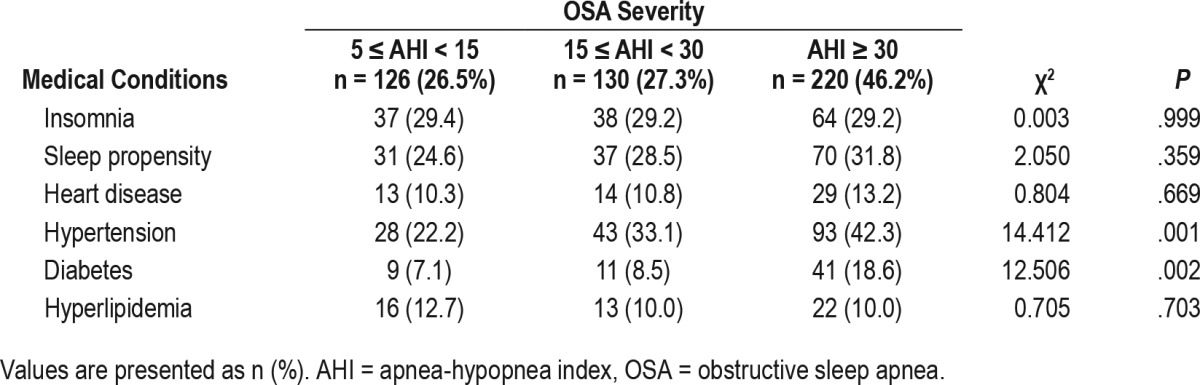
Table 4.
Factors contributing to insomnia symptoms among patients with OSA.
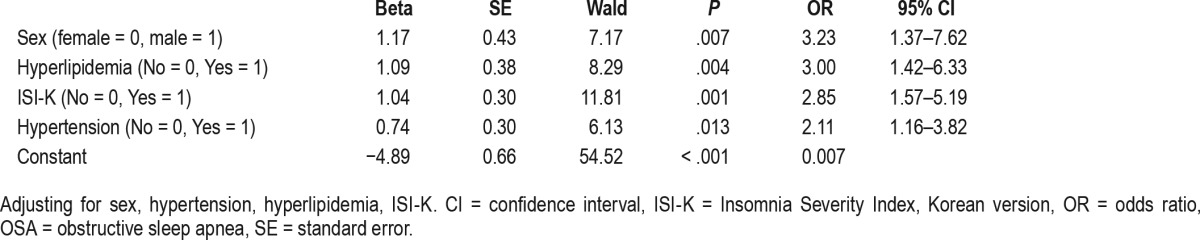
In order to compare heart disease and non-heart disease groups, the following factors were included as independent variables: sex, HTN, HL, ISI. The results showed that the contributing factors to heart disease in patients with OSA were sex (odds ratio: 3.23), HL (odds ratio: 3.00), insomnia symptoms (odds ratio: 2.85), and HTN (odds ratio: 2.11), with sex being the most influential factor (Table 5).
Table 5.
Factors associated with heart disease among patients with OSA.
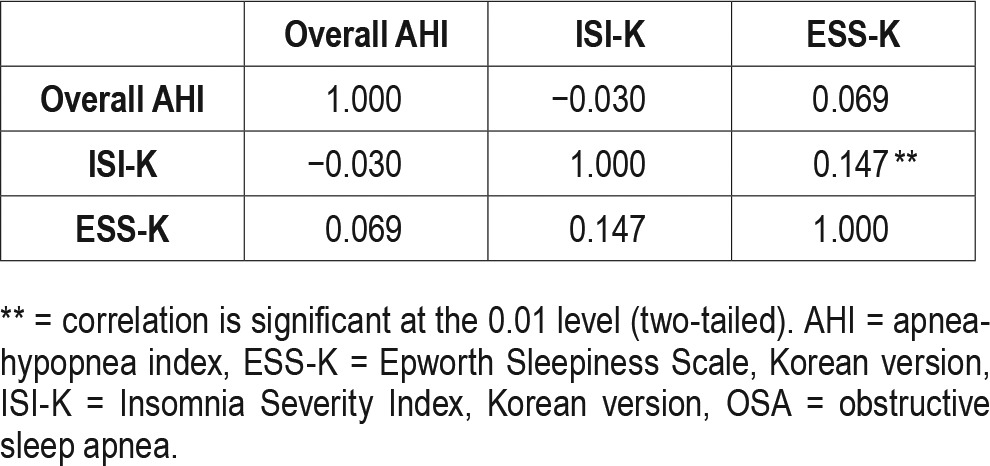
In the CPAP treatment group (n = 77), 22 subjects (28.6%) had insomnia. Risk of insomnia in the OSA+I (22/77) and OSA−I (55/77) groups was not affected by CPAP adherence (54.5% versus 61.8%, P = .557). There was no correlation between the ISI-K score and CPAP use among these 77 patients. In addition, patients who were adherent and nonadherent to CPAP showed no difference in clinical characteristics and PSG results (Table 6). Using correlational analyses examining the relationships between ISI-K, ESS-K and AHI, there was no correlation between ISI-K and AHI, but there was a significant correlation between ISI-K and ESS (r = 0.147, P = .01) (Table 7).
Table 6.
Adherence to CPAP therapy.
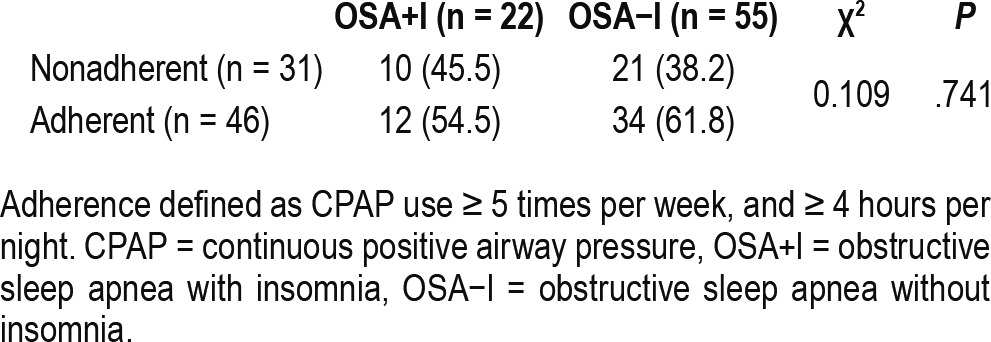
Table 7.
Correlation between severity of OSA, insomnia, and sleep propensity.
DISCUSSION
In this study, the OSA+I group showed greater sleep disturbance and higher rate of heart disease. Prevalence of comorbid insomnia in patients with OSA varies depending on the population, methods, and diagnostic questionnaires.1,13,29–32 Studies that have used the ISI to measure insomnia in patients with PSG-confirmed OSA have reported a prevalence of 32% to 84% in Western countries.32–34 The wide range of prevalence is due to variable insomnia definitions and inconsistent criteria for insomnia and OSA used in these studies. Our study showed that 29.2% of patients with OSA have significant insomnia symptoms. This finding is similar to the previously reported rate of 27.4% in Korean patients with PSG-confirmed OSA.35 There was a higher percentage of females in the OSA+I group (35.3% of 139) than in the OSA−I group (19.6% of 337). This finding is consistent with previous studies that reported significantly higher odds of having comorbid insomnia in females with OSA compared to males with OSA.13,31,36 Additionally, we showed that depressive mood was a statistically significant contributing factor to insomnia; this, again, is consistent with previous studies done in the United States general population.13
The PSG results of OSA+I group (shorter total sleep time, lower sleep efficiency, and longer sleep onset latency) represent the characteristics of insomnia (ie, difficulty falling asleep and maintaining sleep). The OSA+I group showed greater sleep disturbance than the patients in the OSA−I group. This finding is consistent with a previous study comparing PSG results between patients with OSA with and without comorbid insomnia.5,37 However, the characteristics of sleep architecture have been inconsistent as another study reported increased stage N1 sleep and decreased slow sleep,7 whereas other studies have shown no significant differences in this patient population.31,38 This inconsistency may be due to differences in diagnostic and inclusion criteria used in those studies.
We confirmed the subtotal of the ISI-K through the first three sleep items to ensure that they are measuring insomnia symptoms rather than OSA symptoms. However, insomnia and OSA share many clinical symptoms including frequent awakenings, difficulty falling asleep, daytime dysfunction, and decreased QoL.13,37 Our findings showed more sleep propensity (as measured by ESS-K) in the OSA+I than in the OSA−I patient group. Although patients with insomnia have difficulty initiating or maintaining sleep, as a result of overall lack of night sleep these patients suffer from daytime sleepiness. However, this might be caused by the poorer sleep quality and co-morbid mood problems present in patients with insomnia. The lower QoL and higher levels of depressed mood (as measured by the SF-36-K and BDI-2-K, respectively) can also worsen sleep quality, exacerbate insomnia symptoms, and affect sleep architecture by shortening total sleep time and increasing sleep onset latency.
There have been several theories suggesting reciprocal relationships between insomnia and OSA. One theory suggests that the presence of insomnia can exacerbate, or contribute to the development of OSA, and vice versa. Another theory suggests that repetitive apnea or hypopnea and the following arousals during sleep may result in difficulty maintaining sleep, hence poor sleep quality, which may explain the common notion that nighttime awakenings may contribute to development of insomnia. A third theory states that sleep disruption associated with comorbid insomnia can result in more sleep fragmentation and sleep deprivation, two clinical symptoms that would add to severity of OSA.4,29,39 Our study confirmed such reciprocal association between insomnia and OSA and also detected depressive mood and heart disease as contributing factors to insomnia symptoms in patients with OSA.
Previous studies linked insomnia and OSA to hyperactivity of the hypothalamic-pituitary-adrenal axis and the sympathetic nervous system.29,31 Based on measurements of the sympathetic nervous system activity,40–44 it has been shown that in patients with OSA, increased sympathetic tone (associated with physiologic arousal) is correlated with the occurrence of insomnia at high levels,45 and hypersomnolence which begins at lower levels.46 Furthermore, Amdo et al.45 have reported that when comparing sympathetic response between sexes, females have a higher sympathetic response to sleep-disordered breathing than males. This observation may explain why females make up a higher percentage of the OSA+I group compared to the OSA−I group. Therefore, because insomnia and OSA are engaged in a mutual relationship, one can initiate or exacerbate the other.
In our study, despite similar prevalence rates of cardiovascular risk factors in the two groups, the OSA+I group showed a higher prevalence of heart disease than the OSA−I group. Logistic regression revealed heart disease as one of the most affected factors contributing to insomnia symptoms. Both OSA and insomnia have been independently linked to heart disease, although we cannot know the direction of causality.47,48
There is significant evidence indicating an association between comorbid OSA and insomnia and ischemic heart disease and heart failure,11–15,49 and also between OSA and valvular heart disease.50,51 However, there have been no studies about the relationship between comorbid OSA and insomnia and valvular heart disease. Further studies with stringent inclusion criteria and more specific classification of comorbidity may lead to more accurate results. In previous studies, insomnia had a negative influence on CPAP adherence.52,53 However, we did not find an association between AHI and ISI-K scores, or between the insomnia symptoms and CPAP adherence.
There are several limitations in our study. Lack of a control group consisting of patients with insomnia without OSA limits our ability to sort out factors specific to each condition per se. We did not collect data regarding menopause in female subjects, which may be considered a limitation given its independent association with both insomnia and OSA.54 However, in order to compensate for that, we performed a comparison between females younger than 50 years and those older than 50 years. Due to the lack of a follow-up evaluation, the CPAP outcome of those with OSA and comorbid OSA and insomnia cannot be presented. Availability of more detailed medical history on our subjects could have also modified our results. The definition of “heart disease” in our study can be another limitation. Previous studies have often considered cardiovascular disease as a comorbidity. Also, we did not include objective data on CPAP adherence as it was not the focus of this study, which may be considered a limitation. Moving forward, each type of heart disease should be analyzed separately if the sample size is sufficient.
Our prevalence rate of comorbid insomnia with OSA is comparable to the results of previous studies. Our findings revealed female predominance, greater degree of sleep disturbance, more depression, and lower QoL in patients in the OSA+I group. Most importantly, these patients had a higher rate of cardiovascular diseases. This finding establishes a strong association, rather than a causality; therefore, it warrants further investigations into its pathophysiology, which would help devise risk reduction strategies and treatment options.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korean Government (MSIP) (No. 2014R1A5A2010008), and by a grant from the Soonchunhyang University Research Fund. The authors report no conflicts of interest. Work for this study was performed at Keimyung University Dongsan Medical Center, and Soonchunhyang University Cheonan Hospital.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BDI-2
Beck Depression Inventory
- CPAP
continuous positive airway pressure
- ESS
Epworth Sleepiness Scale
- ISI
Insomnia Severity Index
- OSA
obstructive sleep apnea
- OSA+I
obstructive sleep apnea with insomnia
- OSA−I
obstructive sleep apnea without insomnia
- QoL
quality of life
- PSG
polysomnography
- PSQI
Pittsburgh Sleep Quality Index
- SF-36
Short-Form 36-Item Health Survey
- -K
Korean version
REFERENCES
- 1.Luyster FS, Buysse DJ, Strollo PJ., Jr Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196–204. [PMC free article] [PubMed] [Google Scholar]
- 2.Cho YW, Song ML, Morin CM. Validation of a Korean version of the insomnia severity index. J Clin Neurol. 2014;10(3):210–215. doi: 10.3988/jcn.2014.10.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morin CM, Belleville G, Belanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guilleminault C, Eldridge FL, Dement WC. Insomnia with sleep apnea: a new syndrome. Science. 1973;181(4102):856–858. doi: 10.1126/science.181.4102.856. [DOI] [PubMed] [Google Scholar]
- 5.Krakow B, Melendrez D, Ferreira E, et al. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest. 2001;120(6):1923–1929. doi: 10.1378/chest.120.6.1923. [DOI] [PubMed] [Google Scholar]
- 6.Smith S, Sullivan K, Hopkins W, Douglas J. Frequency of insomnia report in patients with obstructive sleep apnoea hypopnea syndrome (OSAHS) Sleep Med. 2004;5(5):449–456. doi: 10.1016/j.sleep.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Cronlein T, Geisler P, Langguth B, et al. Polysomnography reveals unexpectedly high rates of organic sleep disorders in patients with prediagnosed primary insomnia. Sleep Breath. 2012;16(4):1097–1103. doi: 10.1007/s11325-011-0608-8. [DOI] [PubMed] [Google Scholar]
- 8.Bradley TD, Floras JS. Obstructive sleep apnoea and its cardiovascular consequences. Lancet. 2009;373(9657):82–93. doi: 10.1016/S0140-6736(08)61622-0. [DOI] [PubMed] [Google Scholar]
- 9.Phillips B, Mannino DM. Do insomnia complaints cause hypertension or cardiovascular disease? J Clin Sleep Med. 2007;3(5):489–494. [PMC free article] [PubMed] [Google Scholar]
- 10.Luyster FS, Kip KE, Buysse DJ, Aiyer AN, Reis SE, Strollo PJ., Jr Traditional and nontraditional cardiovascular risk factors in comorbid insomnia and sleep apnea. Sleep. 2014;37(3):593–600. doi: 10.5665/sleep.3506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spiegelhalder K, Scholtes C, Riemann D. The association between insomnia and cardiovascular diseases. Nat Sci Sleep. 2010;2:71–78. doi: 10.2147/nss.s7471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kanno Y, Yoshihisa A, Watanabe S, et al. Prognostic significance of insomnia in heart failure. Circ J. 2016;80(7):1571–1577. doi: 10.1253/circj.CJ-16-0205. [DOI] [PubMed] [Google Scholar]
- 13.Vozoris NT. Sleep apnea-plus: prevalence, risk factors, and association with cardiovascular diseases using United States population-level data. Sleep Med. 2012;13(6):637–644. doi: 10.1016/j.sleep.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Sivertsen B, Bjornsdottir E, Overland S, Bjorvatn B, Salo P. The joint contribution of insomnia and obstructive sleep apnoea on sickness absence. J Sleep Res. 2013;22(2):223–230. doi: 10.1111/j.1365-2869.2012.01055.x. [DOI] [PubMed] [Google Scholar]
- 15.Gupta MA, Knapp K. Cardiovascular and psychiatric morbidity in obstructive sleep apnea (OSA) with insomnia (sleep apnea plus) versus obstructive sleep apnea without insomnia: a case-control study from a Nationally Representative US sample. PLoS One. 2014;9(3):e90021. doi: 10.1371/journal.pone.0090021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 18.Silber MH, Ancoli-Israel S, Bonnet MH, et al. The visual scoring of sleep in adults. J Clin Sleep Med. 2007;3(2):121–131. [PubMed] [Google Scholar]
- 19.Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504. doi: 10.5664/jcsm.6506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sohn SI, Kim DH, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012;16(3):803–812. doi: 10.1007/s11325-011-0579-9. [DOI] [PubMed] [Google Scholar]
- 22.Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW. The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath. 2011;15(3):377–384. doi: 10.1007/s11325-010-0343-6. [DOI] [PubMed] [Google Scholar]
- 23.Sung H, Kim J, Park Y, Bai D, Lee S, Ahn H. A study on the reliability and the validity of Korean version of the Beck Depression Inventory-II (BDI-II) J Korean Soc Biol Ther Psychiatry. 2008;14:201–212. [Google Scholar]
- 24.Han CW, Lee EJ, Iwaya T, Kataoka H, Kohzuki M. Development of the Korean version of Short-Form 36-Item Health Survey: health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med. 2004;203(3):189–194. doi: 10.1620/tjem.203.189. [DOI] [PubMed] [Google Scholar]
- 25.Glidewell RN, Renn BN, Roby E, Orr WC. Predictors and patterns of insomnia symptoms in OSA before and after PAP therapy. Sleep Med. 2014;15(8):899–905. doi: 10.1016/j.sleep.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 26.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 27.Pavlova MK, Duffy JF, Shea SA. Polysomnographic respiratory abnormalities in asymptomatic individuals. Sleep. 2008;31(2):241–248. doi: 10.1093/sleep/31.2.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343–356. doi: 10.1016/j.smrv.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beneto A, Gomez-Siurana E, Rubio-Sanchez P. Comorbidity between sleep apnea and insomnia. Sleep Med Rev. 2009;13(4):287–293. doi: 10.1016/j.smrv.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 30.Mysliwiec V, Gill J, Lee H, et al. Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest. 2013;144(2):549–557. doi: 10.1378/chest.13-0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lichstein KL, Justin Thomas S, Woosley JA, Geyer JD. Co-occurring insomnia and obstructive sleep apnea. Sleep Med. 2013;14(9):824–829. doi: 10.1016/j.sleep.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 32.Al-Jawder SE, Bahammam AS. Comorbid insomnia in sleep-related breathing disorders: an under-recognized association. Sleep Breath. 2012;16(2):295–304. doi: 10.1007/s11325-011-0513-1. [DOI] [PubMed] [Google Scholar]
- 33.Lack L, Sweetman A. Diagnosis and treatment of insomnia comorbid with obstructive sleep apnea. Sleep Med Clin. 2016;11(3):379–388. doi: 10.1016/j.jsmc.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 34.Sweetman AM, Lack LC, Catcheside PG, et al. Developing a successful treatment for co-morbid insomnia and sleep apnoea. Sleep Med Rev. 2017;33:28–38. doi: 10.1016/j.smrv.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 35.Choi SJ, Joo EY, Lee YJ, Hong SB. Suicidal ideation and insomnia symptoms in subjects with obstructive sleep apnea syndrome. Sleep Med. 2015;16(9):1146–1150. doi: 10.1016/j.sleep.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 36.Krell SB, Kapur VK. Insomnia complaints in patients evaluated for obstructive sleep apnea. Sleep Breath. 2005;9(3):104–110. doi: 10.1007/s11325-005-0026-x. [DOI] [PubMed] [Google Scholar]
- 37.Bjornsdottir E, Janson C, Gislason T, et al. Insomnia in untreated sleep apnea patients compared to controls. J Sleep Res. 2012;21(2):131–138. doi: 10.1111/j.1365-2869.2011.00972.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee MH, Lee SA, Lee GH, et al. Gender differences in the effect of comorbid insomnia symptom on depression, anxiety, fatigue, and daytime sleepiness in patients with obstructive sleep apnea. Sleep Breath. 2014;18(1):111–117. doi: 10.1007/s11325-013-0856-x. [DOI] [PubMed] [Google Scholar]
- 39.Bonnet MH, Arand DL. Clinical effects of sleep fragmentation versus sleep deprivation. Sleep Med Rev. 2003;7(4):297–310. doi: 10.1053/smrv.2001.0245. [DOI] [PubMed] [Google Scholar]
- 40.Carlson JT, Hedner J, Elam M, Ejnell H, Sellgren J, Wallin BG. Augmented resting sympathetic activity in awake patients with obstructive sleep apnea. Chest. 1993;103(6):1763–1768. doi: 10.1378/chest.103.6.1763. [DOI] [PubMed] [Google Scholar]
- 41.Donadio V, Liguori R, Vetrugno R, et al. Daytime sympathetic hyperactivity in OSAS is related to excessive daytime sleepiness. J Sleep Res. 2007;16(3):327–332. doi: 10.1111/j.1365-2869.2007.00602.x. [DOI] [PubMed] [Google Scholar]
- 42.Narkiewicz K, Kato M, Phillips BG, Pesek CA, Davison DE, Somers VK. Nocturnal continuous positive airway pressure decreases daytime sympathetic traffic in obstructive sleep apnea. Circulation. 1999;100(23):2332–2335. doi: 10.1161/01.cir.100.23.2332. [DOI] [PubMed] [Google Scholar]
- 43.Narkiewicz K, van de Borne PJ, Cooley RL, Dyken ME, Somers VK. Sympathetic activity in obese subjects with and without obstructive sleep apnea. Circulation. 1998;98(8):772–776. doi: 10.1161/01.cir.98.8.772. [DOI] [PubMed] [Google Scholar]
- 44.Waradekar NV, Sinoway LI, Zwillich CW, Leuenberger UA. Influence of treatment on muscle sympathetic nerve activity in sleep apnea. Am J Respir Crit Care Med. 1996;153(4 Pt 1):1333–1338. doi: 10.1164/ajrccm.153.4.8616563. [DOI] [PubMed] [Google Scholar]
- 45.Amdo T, Hasaneen N, Gold MS, Gold AR. Somatic syndromes, insomnia, anxiety, and stress among sleep disordered breathing patients. Sleep Breath. 2016;20(2):759–768. doi: 10.1007/s11325-015-1296-6. [DOI] [PubMed] [Google Scholar]
- 46.Gold MS, Amdo T, Hasaneen N, Gold AR. Somatic arousal and sleepiness/ fatigue among patients with sleep-disordered breathing. Sleep Breath. 2016;20(2):749–758. doi: 10.1007/s11325-015-1294-8. [DOI] [PubMed] [Google Scholar]
- 47.Fava C, Montagnana M, Favaloro EJ, Guidi GC, Lippi G. Obstructive sleep apnea syndrome and cardiovascular diseases. Semin Thromb Hemost. 2011;37(3):280–297. doi: 10.1055/s-0031-1273092. [DOI] [PubMed] [Google Scholar]
- 48.Sofi F, Cesari F, Casini A, Macchi C, Abbate R, Gensini GF. Insomnia and risk of cardiovascular disease: a meta-analysis. Eur J Prev Cardiol. 2014;21(1):57–64. doi: 10.1177/2047487312460020. [DOI] [PubMed] [Google Scholar]
- 49.Johansson P, Alehagen U, Svanborg E, Dahlstrom U, Brostrom A. Sleep disordered breathing in an elderly community-living population: relationship to cardiac function, insomnia symptoms and daytime sleepiness. Sleep Med. 2009;10(9):1005–1011. doi: 10.1016/j.sleep.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 50.Pressman GS, Figueredo VM, Romero-Corral A, Murali G, Kotler MN. Effect of obstructive sleep apnea on mitral valve tenting. Am J Cardiol. 2012;109(7):1055–1059. doi: 10.1016/j.amjcard.2011.11.037. [DOI] [PubMed] [Google Scholar]
- 51.Ding N, Ni BQ, Zhang XL, et al. Prevalence and risk factors of sleep disordered breathing in patients with rheumatic valvular heart disease. J Clin Sleep Med. 2013;9(8):781–787. doi: 10.5664/jcsm.2920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pieh C, Bach M, Popp R, et al. Insomnia symptoms influence CPAP compliance. Sleep Breath. 2013;17(1):99–104. doi: 10.1007/s11325-012-0655-9. [DOI] [PubMed] [Google Scholar]
- 53.Wickwire EM, Smith MT, Birnbaum S, Collop NA. Sleep maintenance insomnia complaints predict poor CPAP adherence: a clinical case series. Sleep Med. 2010;11(8):772–776. doi: 10.1016/j.sleep.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 54.Collop NA, Adkins D, Phillips BA. Gender differences in sleep and sleep-disordered breathing. Clin Chest Med. 2004;25(2):257–268. doi: 10.1016/j.ccm.2004.01.002. [DOI] [PubMed] [Google Scholar]