Abstract
This is a rare case of non-24-hour sleep-wake rhythm disorder in a sighted male with normal functioning. The patient, a 23-year-old doctorate graduate student, presented with difficulty falling asleep and excessive daytime sleepiness. He reported variable sleep and wake times. Overnight baseline polysomnography was unremarkable and his Multiple Sleep Latency Test was significant for short mean sleep latency. Sleep diary and actigraphy were obtained, which demonstrated a pattern of delaying of sleep and wake times each day. He had excellent symptom response to nightly melatonin.
Citation:
Solaiman SS, Agrawal R. Non-24-hour sleep-wake circadian rhythm disorder in a sighted male with normal functioning. J Clin Sleep Med. 2018;14(3):483–484.
Keywords: actigraphy, circadian rhythm disorder, melatonin, non-24-hour
INTRODUCTION
Non-24-hour sleep-wake rhythm disorder (N24SWD) is rare in nonblind patients. Sighted patients reported in the literature have had significant psychiatric, intellectual, developmental, or medical comorbidities. We report a rare case of N24SWD in a sighted patient with normal functioning and no significant comorbidities.
REPORT OF CASE
A 23-year-old male doctorate graduate student presented with a 5-year history of difficulty falling asleep and excessive daytime sleepiness. His sleep and wake times were variable, but he averaged 8 hours of sleep in 24 hours. Two years before presenting to our sleep center, he underwent overnight baseline polysomnography and Multiple Sleep Latency Testing. Overnight baseline polysomnography revealed an apnea-hypopnea index of 5.1 events/h and a 92% oxygen nadir. His Multiple Sleep Latency Testing was significant for mean sleep latency of 5.5 minutes and absence of sleep onset rapid eye movement periods. Daily armodafinil was started by his previous sleep physician for a possible diagnosis of idiopathic hypersomnia. Armodafinil helped with his hypersomnia, but he would only use it when he needed to stay awake, for example, when studying for an upcoming exam. For insomnia, his previous sleep physician trialed the patient on temazepam, zolpidem, and diphenhydramine with minimal success.
His medical history was significant for mild depression and anxiety, diagnosed 3 years after the onset of his sleep symptoms. He had been tried on sertraline and lamotrigine, which did not help and therefore were discontinued. He stated his anxiety and depression largely stemmed from his sleep problems. When he would sleep during the day, it would be socially isolating and when he would be sleep deprived, it would lead to unstable mood. His social history was significant for him being a student in a highly regarded science doctorate program. He denied substance abuse and reported drinking alcohol occasionally.
At our institution, the patient's physical examination was unremarkable. For workup, 4 weeks of sleep diary data were requested, but the patient provided 20 weeks of sleep diary data. During this time, he was on leave from school and allowed himself to wake and sleep without external restrictions. He also abstained from all pharmacotherapy and caffeine during this time. The sleep diary data showed progressive delays in sleep and wake times by 1 to 3 hours daily, consistent with N24SWD (Figure 1). Subsequently, 2 weeks of actigraphy were obtained, confirming these findings (Figure 2). Endogenous melatonin levels were not measured in this patient. The lack of data concerning the endogenous melatonin secretory profile is a study limitation.
Figure 1. Sleep diary data showing progressive daily delays in sleep and wake times.
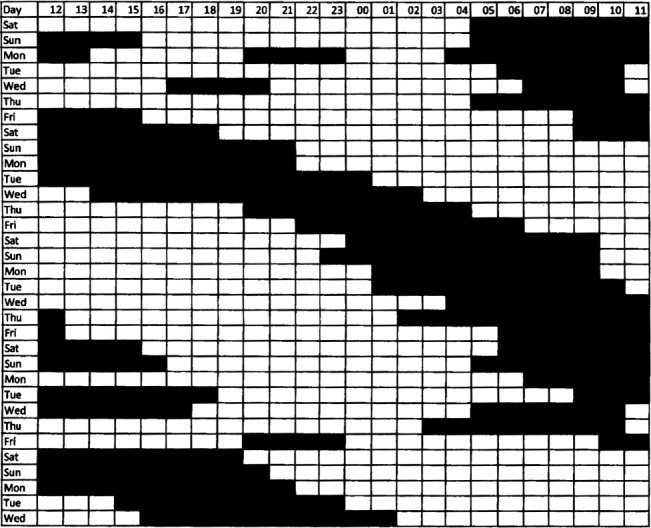
Each row represents one day. Each box represents 1 hour. The first column represents 12:00 PM – 1:00 PM and the last column represents 11:00 AM – 12:00 PM. This figure represents 4.7 out of the 20 weeks of sleep diary data that the patient provided.
Figure 2. Actigraphy data showing progressive daily delays in sleep and wake times.
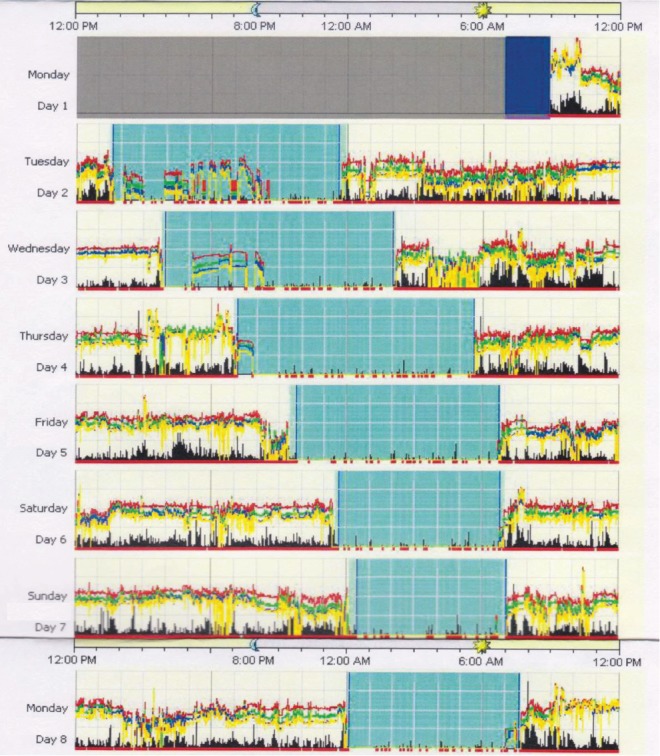
This figure represents 7 days of actigraphy obtained by this patient. He did not wear the device on the first day.
For N24SWD, tasimelteon was recommended; however, the patient did not start the treatment due to high cost concerns. He was started on nightly melatonin for his N24SWD and noted a drastic improvement in symptoms. He has been taking 3 mg of melatonin every night for 6 months at 11:00 pm, his desired bedtime, and is asleep by 11:30 pm, helping to regulate his sleep schedule. Although this dose and timing of melatonin administration worked well for this patient, there are no current guidelines on dose and timing of melatonin for treatment of N24SWD. Morning light therapy and armodafinil were also prescribed, which the patient has not yet started. Since starting melatonin, his sleep disorder has been under adequate control, resulting in no significant symptoms of anxiety or depression, despite being off psychotropic medications. Beck Depression Inventory was found to be negative. He has minimal complaints of insomnia or hypersomnia. His performance at his graduate school has significantly improved.
DISCUSSION
This patient met diagnostic criteria for N24SWD with a history of insomnia and excessive daytime sleepiness, alternating with asymptomatic periods, and sleep diary and actigraphy data that showed a pattern of sleep and wake times that were delayed each day.1 The patient's sleep disturbance was not explained by any other sleep disorder or medical condition.1
Total blindness is the most common predisposing condition for N24SWD.2 Sighted patients with N24SWD are so uncommon that they have mostly been described in case reports.3 Hayakawa et al. reported 57 sighted patients with N24SWD.4 Most previously reported cases of N24SWD in sighted patients involve patients with substantial medical, psychiatric, or developmental impairment, causing these patients to have limited or inappropriate exposure to environmental entraining cues, such as light or social interaction.1,2 Psychiatric conditions, such as severe anxiety, can limit social interaction, and medical conditions, such as traumatic brain injury, can force prolonged inactivity. These situations place sighted patients in circumstances where they have limited exposure to environmental entraining cues.
Our patient, however, did not have any significant medical or developmental disabilities. His depression and anxiety were only mild in nature and resolved with treatment of his sleep disorder, suggesting that they were secondary to his N24SWD. In many previously reported cases, limited or inappropriate exposure to light or other entraining cues from structured social and physical activity were noted. This is one of the only reports of a case of N24SWD in a sighted individual with normal functioning, no significant comorbidities, and absence of compromised entraining cues.
DISCLOSURE STATEMENT
Work for this study was performed at Baylor College of Medicine, Houston, TX. All authors have seen and have approved the manuscript. The authors report no conflicts of interest.
REFERENCES
- 1.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 2.Kryger MH, Roth T, Dement WC. Principles and Practice of Sleep Medicine. 6th ed. Philadelphia, PA: Elsevier; 2016. [Google Scholar]
- 3.Sack R, Auckley D, Auger RR, et al. Circadian rhythm sleep disorders: part II, advanced sleep phase disorder, delayed sleep phase disorder, free-running disorder, and irregular sleep-wake rhythm. Sleep. 2007;30(11):1484–1501. doi: 10.1093/sleep/30.11.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayakawa T, Uchiyama M, Kamei Y, et al. Clinical analyses of sighted patients with non-24-hour sleep-wake syndrome: a study of 57 consecutively diagnosed cases. Sleep. 2005;28(8):945–952. doi: 10.1093/sleep/28.8.945. [DOI] [PubMed] [Google Scholar]


