Abstract
Aim:
The aim of this study was the evaluation of the prevalence of NAFLD in patients with type 2 diabetes mellitus.
Background:
Non-alcoholic fatty liver disease (NAFLD) is an emerging disease with high prevalence in patients with type 2 diabetes mellitus (T2DM). Many studies have reported the prevalence of NAFLD in type 2 diabetes mellitus patients. However, these results are inconsistent.
Methods:
A Literature search was conducted in PubMed, Scopus, web of science and Science Direct from 2005 to August 2017. The necessary information was extracted. Heterogeneity was evaluated using I2 statistic. Meta-regression analyses were performed to the estimation of the relationship between the year of study and sample size with the prevalence of NAFLD. Publication bias was assessed by both Begg rank correlation and Egger tests. Subgroup analysis was performed for identification of sources heterogeneity.
Results:
Seventeen studies involving 10897 type 2 diabetes mellitus patients with NAFLD were included in this meta-analysis. The overall prevalence of NAFLD in type 2 diabetes mellitus patients by random effects models was 54% (95% CI, 45%- 64%). There is a significant heterogeneity across studies with (I2= 99%, p> 0.01). The funnel plot as graphically and Begg and Egger as statistically showed no publication bias among studies. Subgroup analysis indicated that the prevalence of NAFLD in type 2 diabetes mellitus patients differed in predictive factors such as lipid profile, BMI, HbA1c, AST, and ALT. This finding in spite of heterogeneity of documents is corresponding to the positive correlation between NAFLD and type 2 diabetes mellitus.
Conclusion:
The findings indicated that the overall prevalence of NAFLD among type 2 diabetes mellitus patients is significantly higher. It can be concluded that type 2 diabetes mellitus patients should be managed to prevent NAFLD.
Key Words: NAFLD, Type 2 diabetes mellitus, Fatty liver, Meta-analysis
Introduction
Non-alcoholic fatty liver disease (NAFLD) as one of the most common liver diseases is emerging as a public health problem issue worldwide(1). The disease occurs when fat forms more than 10 to 5% of the liver's weight. The disease involves a wide range of liver diseases but occurs in people who either do not drink alcohol or only use moderate amounts of alcohol(2). NAFLD incorporates histologically and clinically different non-alcoholic entities; fatty liver (NAFL, steatosis hepatic) and steatohepatitis (NASH characterized by hepatocyte ballooning and lobular inflammation ± fibrosis) might progress to cirrhosis and rarely to hepatocellular cancer(3). Obesity and physical inactivity are interlinked risk factors for the development of diabetes NAFLD(4). Diagnosis of NAFLD based on liver biopsy, ultrasound evidence of bright liver, and posterior attenuation in people without alcohol or low alcohol consumption(5). In an extensive study about the prevalence of NAFLD in type 2 diabetes mellitus in Italy, the results indicated the 70% prevalence of NAFLD in type 2 diabetes mellitus patients. Also recently, several studies have been reported that the prevalence of NAFLD in type 2 diabetes mellitus patients ranges broadly between 34% - 94%(6). The prevalence of NAFLD is increasing and approximately 34%-46% of obese adult in developed countries have NAFLD(7). It is well known that the prevalence of NAFLD associated with several risk factors such as obesity, metabolic syndrome, insulin resistance and type 2 diabetes(8, 9). There is a strong association between NAFLD and diabetes risk. An individual's risk of developing diabetes is increased approximately 5-fold if they have NAFLD(10, 11). The association between NAFLD and type 2 diabetes could be explained by the insulin resistance, dyslipidemia and hepatic triglyceride (TG) accumulation in NAFLD and defective B-cell in type 2 diabetes mellitus (9). Compared to healthy populations, type 2 diabetes mellitus patients show increased risk for catching of advanced liver disease including fibrosis, cirrhosis and hepatocellular carcinoma(12). In this regard, an accurate estimate of NAFLD prevalence in type 2 diabetes mellitus patients is important. However, there was high inconsistency across the results of studies in the estimated prevalence of NAFLD in type 2 diabetes mellitus patients. Therefore, the aim of this meta- analysis is a determination of the overall prevalence of NAFLD and its predictive variables in type 2 diabetes mellitus patients.
Methods
Search strategy
This meta-analysis was carried out with literature search of the electronic databases of PubMed, Scopus, web of science, ScienceDirect and Embase from 2005 to August 2017. Key words: (“Non-alcoholic Fatty Liver disease” AND Diabetes Mellitus, type 2), (NAFLD AND T2DM), (NAFLD, Diabetes Mellitus) were used to identify relevant studies. Meanwhile, the reference lists of full articles were reviewed.
Study inclusion/ exclusion criteria
The studies were included if they had the following inclusion criteria: 1) studies published in English language, 2) reported the prevalence of NAFLD in T2DM patients and 3) provided the necessary information of relevant studies and also studies exclude if they had following criteria: reviews, case-reports, comments, brief reports abstracts or book chapters because of limited data.
Data extraction
All studies were assessed independently by two reviewers and extracted data from included studies in this meta-analysis. The extracted data as follows: first author, publication year, sample size, mean age of type 2 diabetes mellitus patients, the prevalence of NAFLD (%)in type 2 diabetes mellitus and laboratory parameters including mean (SD) total cholesterol, HGL, LDL, HbA1c, ALT and AST.
Quality assessment
In this meta-analysis, the PRISMA was used to evaluate the quality of eligible studies. PRISMA focuses on ways in which authors can ensure the transparent and complete reporting of systematic reviews and meta-analysis. It does not address directly or in a detailed manner the conduct of systematic review and meta-analysis. The PRISMA statement consists of 27-item checklist. The checklist includes items seem to be essential for transparent reporting of systematic review and meta-analysis.
Statistical analysis
Statistical analyses for this meta-analysis were performed using STATA version 14.0 (STATA Corporation, College Station, TX, USA). The pooled prevalence of NAFLD in type 2 diabetes mellitus patients was performed as a percentage with corresponding 95% CI by a random- effects model when significant heterogeneity was observed (p<0.1 and I2>50%). The association between the prevalence of NAFLD in type 2 diabetes mellitus patients with publication year across studies was performed by meta-regression analyses. Publication bias was assessed using both Begg rank correlation test as statistically and funnel plot as graphically. Subgroup analysis were performed to identify the possible sources of heterogeneity. P-value of <0.05 was considered significant.
Results
Selection of studies
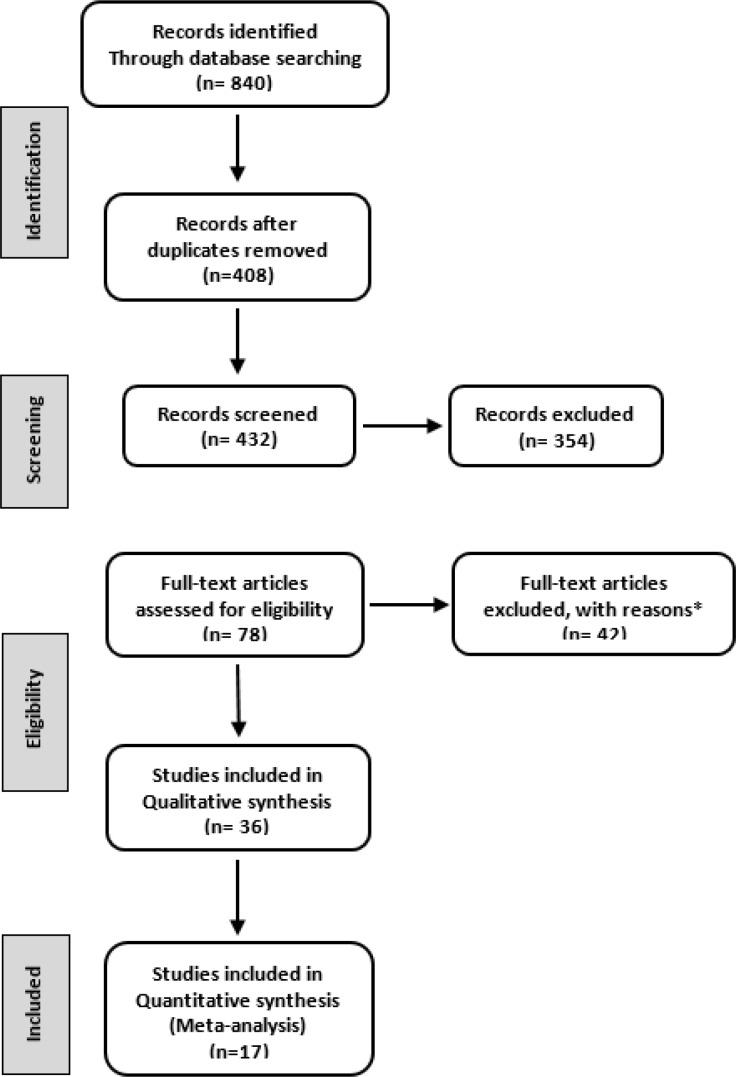
Initially, a total of 840 articles were searched in this study. Of these 408 articles were excluded due to duplicate data, 354 articles were excluded for not reporting the prevalence of NAFLD in type 2 diabetes mellitus patients, 42 articles excluded for not having available data, 19 articles were excluded for not being review article, abstract or a brief report. Finally, 17 eligible articles were selected in this meta-analysis (Figure 1).
Figure 1.
The flow chart of studies selection
Study characteristics
We identified 17 articles that reported the prevalence of NAFLD in type 2 diabetes mellitus patients. Table 1 lists the studies used in this meta-analysis along with baseline characteristics. A total of 10897 individuals participated in 17 articles.
Table 1.
The studies characteristics included in this meta-analysis. TG: Triglyceride, HLD: High lipoprotein density, LDL: Low density lipoprotein, BMI: Body mass index
| ALT (M±SD) |
AST (M±SD) |
BMI (M±SD) |
HbA1C (M±SD) |
LDL (M±SD) |
HDL (M±SD) |
TG (M±SD) |
Total cholesterol (M±SD) |
Prevalence (%) |
Age (M±SD) |
Sample size |
Country | Year | First author (references) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| - | - | 31.3±5.7 | 7.2±1.1 | 84.6±26.5 | 48±13.3 | 147.7±80.1 | 161.9±31.6 | 42.6 | 68.9±4.2 | 939 | UK | 2011 | Williamson (13) |
| 25±3 | 23±3 | 28.3±4 | 7.3±1.1 | 131.4±15.6 | 52.3±15.6 | 149.5±89 | 69.5 | 65±6 | 2839 | Italy | 2007 | Targher (14) |
|
| 20.3±26 | 15.6±11.3 | 33.9±8.3 | 103.5±57 | 36.6±15.1 | 100.6±61.3 | 170.7±100.5 | 9.5 | 52.5±10.9 | 150 | Nigeria | 2011 | Onyekwere (15) |
|
| 21.8±10.3 | 18.9±5.7 | 29.5±4.8 | 8.8±2.7 | 122.3±41.3 | 48.4±10.4 | 164.1±84.4 | 204.7±49.5 | 47 | 57.3±10.3 | 87 | Brazil | 2010 | Ferreira (16) |
| 33±14 | 26±12 | 29±4 | 7.2±0.9 | 127.5±19.5 | 48.8±15.6 | 144.2±53.4 | - | 75 | 66±4 | 2103 | Italy | 2005 | Targher (17) |
| 47.7±21.9 | 27.3±12.3 | 27.6±4.1 | 7.2±1.3 | - | - | 161.5±75.7 | 183.9±38 | 60.7 | 60.47±9.8 | 141 | Thailand | 2015 | Sobhonslids (18) |
| 37±18 | 23±12 | 29.7±7.9 | 8.31±1.7 | 82.7±68.2 | 46.8±14.4 | 133.5±106.8 | 165.8±62.4 | 49.6 | 60.7±11.2 | 399 | Malaysia | 2013 | Chan (19) |
| - | - | - | 7.9 | 126.75 | 41.3±16.7 | - | - | 79 | 55.7±8.9 | 381 | Romania | 2016 | Silaghi (20) |
| 39 | 20 | 31.3±5.4 | 7.3 | 130±44.8 | 43.3±12.5 | 113.92 | 202.8±52.7 | 69.4 | 55.6±7.1 | 180 | Brazil | 2008 | Leite (21) |
| 28.6±19.2 | 23.7±11.1 | 25.2±4 | 6.7±1.6 | - | - | 128 | 185±36 | 54.5 | 46±12 | 541 | India | 2009 | Mohan (22) |
| 23.7±12.08 | 26.97±8.1 | 26.6±3.85 | 7.69±1.5 | 110.3±41.6 | 46.2±9.4 | 173.5±68.8 | 190.6±44 | 87 | 54.2±9.2 | 204 | India | 2008 | Prashanth (23) |
| 23 | 34.7±5.3 | - | 7 | 91±34 | 40±12 | 142 | 164±40 | 5 | 58±8 | 103 | USA | 2015 | Portillo-Sanchez (24) |
| 25.72±13.1 | 22.34±9 | 27.5±3.37 | 8.9±2.5 | 115±32 | 45.6±11 | 188.7±127.3 | 196.6±47.6 | 61 | 62.3±12.5 | 1217 | China | 2013 | Lv (25) |
| - | - | - | - | - | - | - | - | 45.2 | - | 186 | Indonesia | 2017 | Prasetya (26) |
| - | - | - | - | - | - | - | - | 50.3 | - | 167 | Sudan | 2015 | Almobarak (27) |
| - | - | - | - | - | - | - | - | 16.7 | 53.2±8.6 | 336 | Nigeria | 2015 | Olusanya (28) |
| 55.6±39.8 | 54.8±36.1 | - | - | - | - | - | - | 56.5 | 52.2±10.8 | 924 | India | 2013 | Kalra (29) |
AST: Aspartate aminotransferase, ALT: Alanine aminotransferase
The prevalence of NAFLD in patients with type 2 diabetes mellitus
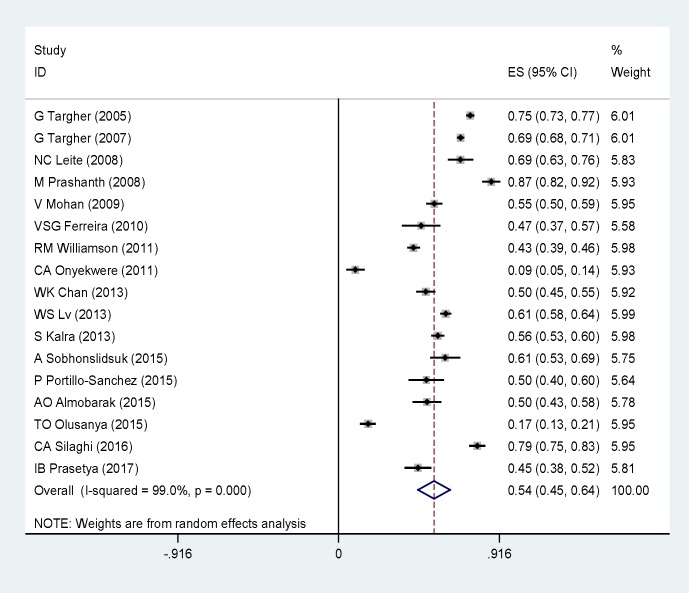
Figure 2 presents the results of the overall prevalence of NAFLD in type 2 diabetes mellitus patients that calculated as percentage with corresponding 95% CI by a random effects model. The pooled prevalence of NAFLD in type 2 diabetes mellitus patients was 54% (95% CI 45%- 64%). The prevalence of NAFLD as outcome was significantly high in type 2 diabetes mellitus. There was statistically significant heterogeneity between studies (p< 0.01, I2= 99%). To explore reasons for heterogeneity, we conducted subgroup analysis. We found significant heterogeneity for total cholesterol and TG that were (I2= 98%) and (I2= 97%) respectively. The pooled prevalence of NAFLD in type 2 diabetes mellitus patients with high BMI was 29% (28.09 – 29.91), (I2= 98.9%).
Figure 2.
The forest plot of NAFLD prevalence in type 2 diabetes patients. Square represents effect estimate of individual studies with more than 95 % confidence intervals with the size of squares proportional to the weight assigned to the study in the meta-analysis. In this chart, studies are stored in order of the year of publication and author’s names, based on a random effects model
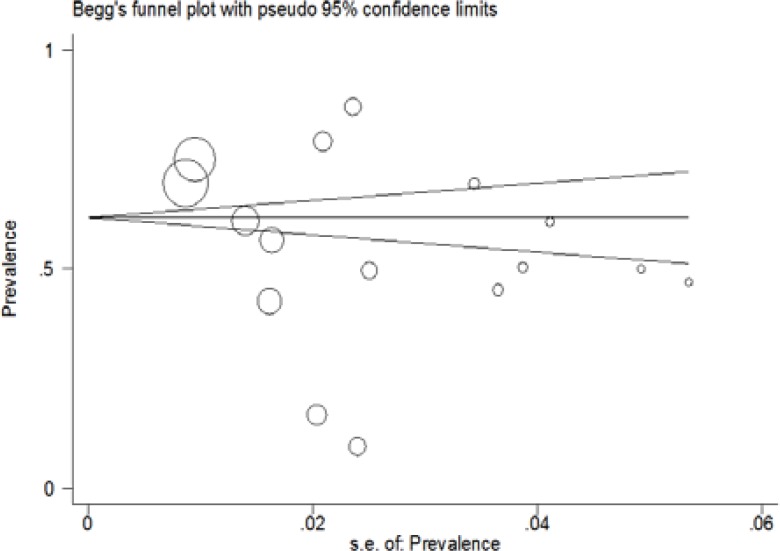
The subgroup analyses indicated that the prevalence of NAFLD in type 2 diabetes mellitus differed to assess total cholesterol, TG, BMI, ALT, and AST. Table 2 shows the results of subgroup analyses. Visual inspection of the funnel plot and the Begg rank correlation method (p= 0.11) (Fig 3) have not shown any publication bias. We performed meta-regression test for the association between the prevalence of NAFLD in type 2 diabetes mellitus patients with publication year of articles that no significant change observed (p= 0.16) (Fig 4). Taken together, these findings suggest that the prevalence of NAFLD in type 2 diabetes mellitus patients is high. Therefore, the early diagnosis of NAFLD is essential for NAFLD management in type 2 diabetes mellitus patients.
Table 2.
The result of subgroup analysis.
| Subgroup | Study number | I2 | SEM(95%CI) |
|---|---|---|---|
| Total Prevalence of NAFLD in People With Type 2 Diabetes | 17 | 99 | 54(45-64) |
| Cholesterol | 10 | 98/4 | 182.63(171.46-193.79) |
| Triglycerides | 9 | 97 | 151.29(140.25 -162.33) |
| HDL | 11 | 98 | 45.31(43.10 -47.53) |
| LDL | 11 | 99.7 | 111.49(102.27-120.72) |
| HbA1C | 12 | 98.8 | 7.60(7.35-7.84) |
| BMI | 11 | 98.9 | 29 (28.09 -29.91) |
| AST | 11 | 100 | 24.59(15.54-33.64) |
| ALT | 10 | 99.4 | 31.77(28.09-35.44) |
Figure 3.
The prevalence of NAFLD in type 2 diabetes patients based on year of study. The fitted line shows meta-regression line
Figure 4.
Funnel Plot to assess Publication Bias. The diameter of each circle represents the weight in the meta-analysis
Discussion
In this systematic review and meta-analysis, prevalence of NAFLD in type 2 diabetes mellitus patients is investigated. A significant increase in the prevalence of NAFLD in type 2 diabetes mellitus patients was observed. The pooled prevalence was 54% (95% CI 45% - 64%). Whereas, in eligible studies involved in this meta-analysis, the prevalence of NAFLD in type 2 diabetes mellitus patients ranged from 5% (24) to 87%(23). Here, the high prevalence of NAFLD in type 2 diabetes mellitus patients indicated the importance of management and early evaluation of NAFLD in type 2 diabetes mellitus patients. The heterogeneity was significant across studies; therefore, subgroup analysis was performed. Subgroup analysis indicated that the prevalence of NAFLD in type 2 diabetes mellitus patients differed by total cholesterol, TG, BMI, HbA1c and HDL, LDL, AST, and ALT. The prevalence of NAFLD in type 2 diabetes mellitus patients was 182.63%, 151.29%, 45.31%, 111.49%, 29%, 24.59% and 31.77% for total cholesterol, triglyceride (TG), HDL, LDL, BMI, AST and ALT, respectively. In a recent study, Yi et al. demonstrated that the prevalence of NAFLD in men is higher than females in type 2 diabetes mellitus patients(30). This gender difference in the prevalence of NAFLD could be attributed to the lipid value in female(31). The triglyceride/high density lipoprotein cholesterol (TG/HDLC) ratio seems to be higher in men than women(30). Obesity is one of the most important factors involved in NAFLD that also has been reported in various other studies(32). In our meta-analysis, high BMI in type 2 diabetes mellitus patients is associated with NAFLD. Bhatt .K et al. found that BMI was significantly higher in patients with NAFLD than a control group without NAFLD(33). We observed that transaminases (ALT and AST) levels in the prevalence of NAFLD in type 2 diabetes mellitus patients were not statistically high in subgroup analysis versus the pooled prevalence of NAFLD. However, several studies have shown that there is no correlation between transaminases levels and the prevalence of NAFLD in type 2 diabetes mellitus patients(32). Whereas, Lu et al. reported the prevalence of NAFLD in type 2 diabetes mellitus patients was significantly associated with elevated ALT(34). In this meta-analysis, we found that the subgroup analysis of HbA1c in the prevalence of NAFLD is lower than the pooled prevalence of NAFLD in type 2 diabetes mellitus patients, as, it is suggested that there is an unusual relationship between HbA1c and NAFLD.
This systematic review and meta-analysis have several strengths. This review obtained the most comprehensive data from relevant studies pertaining to the prevalence of NAFLD in type 2 diabetes mellitus patients.
Our search strategy was very detailed. Statistical tests showed no evidence of publication bias in the analyses. Subgroup analyses was conducted to explore possible sources of heterogeneity.
In the other hand, this systematic review and meta-analysis also have several limitations: first, owing to the small number of studies for a specific outcome, we were not able to better deduce from this studies. Second, we pooled prevalence from studies that appeared to be consisted of adults with mean ages from 46 to 69, whereas, in this meta-analysis adolescent remains unclear. Third, there was substantial heterogeneity between eligible studies. Given the limitations, the finding should be interpreted with caution.
It can be concluded that overall prevalence of NAFLD among type 2 diabetes mellitus patients is significantly higher than the other types of diabetes mellitus. It implies more cares in the type 2 diabetes mellitus patients to prevent NAFLD.
Conflict of interests
The authors declare that they have no conflict of interest.
References
- 1.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—Meta‐analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 2.Feldstein AE, Canbay A, Angulo P, Taniai M, Burgart LJ, Lindor KD, et al. Hepatocyte apoptosis and fas expression are prominent features of human nonalcoholic steatohepatitis. Gastroenterology. 2003;125:437–43. doi: 10.1016/s0016-5085(03)00907-7. [DOI] [PubMed] [Google Scholar]
- 3.Firneisz G. Non-alcoholic fatty liver disease and type 2 diabetes mellitus: the liver disease of our age? World J Gastroenterol. 2014;20:9072. doi: 10.3748/wjg.v20.i27.9072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol. 2010;53:372–84. doi: 10.1016/j.jhep.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Moosavi A, Haghighi A, Mojarad EN, Zayeri F, Alebouyeh M, Khazan H, et al. Genetic variability of Blastocystis sp isolated from symptomatic and asymptomatic individuals in Iran. Parasitol Res. 2012;111:2311–15. doi: 10.1007/s00436-012-3085-5. [DOI] [PubMed] [Google Scholar]
- 6.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–31. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 7.Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–31. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 8.Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M, et al. Nonalcoholic fatty liver disease. Diabetes. 2001;50:1844–50. doi: 10.2337/diabetes.50.8.1844. [DOI] [PubMed] [Google Scholar]
- 9.Forlani G, Giorda C, Manti R, Mazzella N, De Cosmo S, Rossi MC, et al. The burden of NAFLD and its characteristics in a nationwide population with type 2 diabetes. J Diabetes Res. 2016:9. doi: 10.1155/2016/2931985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jäger S, Jacobs S, Kröger J, Stefan N, Fritsche A, Weikert C, et al. Association between the fatty liver index and risk of type 2 diabetes in the EPIC-Potsdam Study. PLoS One. 2015;10:0124749. doi: 10.1371/journal.pone.0124749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hazlehurst JM, Woods C, Marjot T, Cobbold JF, Tomlinson JW. Non-alcoholic fatty liver disease and diabetes. Metabolism. 2016;65:1096–108. doi: 10.1016/j.metabol.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bondini S, Kleiner DE, Goodman ZD, Gramlich T, Younossi ZM. Pathologic assessment of non-alcoholic fatty liver disease. Clin Liver Dis. 2007;11:17–23. doi: 10.1016/j.cld.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Williamson RM, Price JF, Glancy S, Perry E, Nee LD, Hayes PC, et al. Prevalence of and risk factors for hepatic steatosis and nonalcoholic Fatty liver disease in people with type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabetes Care. 2011;34:1139–44. doi: 10.2337/dc10-2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sahebekhtiari N, Nochi Z, Eslampour MA, Dabiri H, Bolfion M, Taherikalani M, et al. Characterization of Staphylococcus aureus strains isolated from raw milk of bovine subclinical mastitis in Tehran and Mashhad. Acta Microbiol Immunol Hung. 2011;58:113–21. doi: 10.1556/AMicr.58.2011.2.4. [DOI] [PubMed] [Google Scholar]
- 15.Onyekwere CA, Ogbera AO, Balogun BO. Non-alcoholic fatty liver disease and the metabolic syndrome in an urban hospital serving an African community. Ann Hepatol. 2011;10:119–24. [PubMed] [Google Scholar]
- 16.Ferreira VS, Pernambuco RB, Lopes EP, Morais CN, Rodrigues MC, Arruda MJ, et al. Frequency and risk factors associated with non-alcoholic fatty liver disease in patients with type 2 diabetes mellitus. Arq Bras Endocrinol Metabol. 2010;54:362–8. doi: 10.1590/s0004-27302010000400004. [DOI] [PubMed] [Google Scholar]
- 17.Targher G, Bertolini L, Poli F, Rodella S, Scala L, Tessari R, et al. Nonalcoholic fatty liver disease and risk of future cardiovascular events among type 2 diabetic patients. Diabetes. 2005;54:3541–6. doi: 10.2337/diabetes.54.12.3541. [DOI] [PubMed] [Google Scholar]
- 18.Sobhonslidsuk A, Pulsombat A, Kaewdoung P, Petraksa S. Non-alcoholic fatty liver disease (NAFLD) and significant hepatic fibrosis defined by non-invasive assessment in patients with type 2 diabetes. Asian Pac J Cancer Prev. 2015;16:1789–94. doi: 10.7314/apjcp.2015.16.5.1789. [DOI] [PubMed] [Google Scholar]
- 19.Chan WK, Tan ATB, Vethakkan SR, Tah PC, Vijayananthan A, Goh KL. Non‐alcoholic fatty liver disease in diabetics–prevalence and predictive factors in a multiracial hospital clinic population in Malaysia. J Gastroenterol Hepatol. 2013;28:1375–83. doi: 10.1111/jgh.12204. [DOI] [PubMed] [Google Scholar]
- 20.Silaghi CA, Silaghi H, Colosi HA, Craciun AE, Farcas A, Cosma DT, et al. Prevalence and predictors of non-alcoholic fatty liver disease as defined by the fatty liver index in a type 2 diabetes population. Clujul Med. 2016;89:82. doi: 10.15386/cjmed-544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leite NC, Salles GF, Araujo AL, Villela‐Nogueira CA, Cardoso CR. Prevalence and associated factors of non‐alcoholic fatty liver disease in patients with type‐2 diabetes mellitus. Liver Int. 2009;29:113–9. doi: 10.1111/j.1478-3231.2008.01718.x. [DOI] [PubMed] [Google Scholar]
- 22.Mohan V, Farooq S, Deepa M, Ravikumar R, Pitchumoni CE. Prevalence of non-alcoholic fatty liver disease in urban south Indians in relation to different grades of glucose intolerance and metabolic syndrome. Diabetes Res Clin Pract. 2009;84:84–91. doi: 10.1016/j.diabres.2008.11.039. [DOI] [PubMed] [Google Scholar]
- 23.Prashanth M, Ganesh H, Vima M, John M, Bandgar T, Joshi SR, et al. Prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus. J Assoc Physicians India. 2009;57:205–10. [PubMed] [Google Scholar]
- 24.Portillo-Sanchez P, Bril F, Maximos M, Lomonaco R, Biernacki D, Orsak B, et al. High prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus and normal plasma aminotransferase levels. J Clin Endocrinol Metab. 2015;100:2231–8. doi: 10.1210/jc.2015-1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lv WS, Sun RX, Gao YY, Wen JP, Pan RF, Li L, et al. Nonalcoholic fatty liver disease and microvascular complications in type 2 diabetes. World J Gastroenterol. 2013;19:3134. doi: 10.3748/wjg.v19.i20.3134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prasetya IB, Hasan I, Wisnu W, Rumende CM. Prevalence and Profile of Fibrosis in Diabetic Patients with Non-alcoholic Fatty Liver Disease and the Associated Factors. Acta Med Indones. 2017;49:91. [PubMed] [Google Scholar]
- 27.Almobarak AO, Barakat S, Suliman EA, Elmadhoun WM, Mohamed NA, Abobaker IO, et al. Prevalence of and predictive factors for nonalcoholic fatty liver disease in Sudanese individuals with type 2 diabetes: Is metabolic syndrome the culprit? Arab J Gastroenterol. 2015;16:54–8. doi: 10.1016/j.ajg.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 28.Rezaei-Tavirani M, Zamanian-Azodi M, Rajabi S, Masoudi-Nejad A, Rostami-Nejad M, Rahmatirad S. Protein Clustering and Interactome Analysis in Parkinson and Alzheimer's Diseases. Arch Iran Med. 2016;19:101–109. [PubMed] [Google Scholar]
- 29.Kalra S, Vithalani M, Gulati G, Kulkarni C, Kadam Y, Pallivathukkal J, et al. Study of prevalence of nonalcoholic fatty liver disease (NAFLD) in type 2 diabetes patients in India (SPRINT) J Assoc Physicians India. 2013;61:448–53. [PubMed] [Google Scholar]
- 30.Yi M, Chen RP, Yang R, Chen H. Increased prevalence and risk of non‐alcoholic fatty liver disease in overweight and obese patients with Type 2 diabetes in South China. Diabet Med. 2017;34:505–13. doi: 10.1111/dme.13174. [DOI] [PubMed] [Google Scholar]
- 31.Moon SS. Relationship between serum uric acid level and nonalcoholic fatty liver disease in pre-and postmenopausal women. Ann Nutr Metab. 2013;62:158–63. doi: 10.1159/000346202. [DOI] [PubMed] [Google Scholar]
- 32.Reid AE. Nonalcoholic steatohepatitis. Gastroenterology. 2001;121:710–23. doi: 10.1053/gast.2001.27126. [DOI] [PubMed] [Google Scholar]
- 33.Bhatt KN, Pranav V, Dipika Y, Dharmesh N, Radhika N, Arvind S. Prevalence of nonalcoholic fatty liver disease in type 2 diabetes mellitus and its relation with insulin resistance in South Gujarat Region. J Mahatma Gandhi Inst Med Sci. 2017;22:8. [Google Scholar]
- 34.Lu H, Zeng L, Liang B, Shu X, Xie D. High prevalence of coronary heart disease in type 2 diabetic patients with non-alcoholic fatty liver disease. Arch Med Res. 2009;40:571–5. doi: 10.1016/j.arcmed.2009.07.009. [DOI] [PubMed] [Google Scholar]