Abstract
Objective
We aimed at determining whether gender modified associations between ADHD and psychiatric comorbidities in adults.
Method
We identified adults with ADHD by linking Norwegian national registries and compared them with the remaining adult population (born 1967–1997, ADHD and bipolar during 2004–2015, other psychiatric disorders 2008–2015). Prevalence differences (PDs) and prevalence ratios (PRs) of psychiatric disorders were determined by Poisson regression. Interaction by gender was evaluated on additive (PDs) and multiplicative (PRs) scales. Proportions of psychiatric disorders attributable to ADHD were calculated.
Results
We identified 40 103 adults with ADHD (44% women) and 1 661 103 adults (49% women) in the remaining population. PDs associated with ADHD were significantly larger in women than in men for anxiety, depression, bipolar and personality disorders, for example depression in women: 24.4 (95% CI, 23.8–24.9) vs. in men: 13.1 (12.8–13.4). PDs were significantly larger in men for schizophrenia and substance use disorder (SUD), for example SUD in men: 23.0 (22.5–23.5) vs. in women: 13.7 (13.3–14.0). Between 5.6 and 16.5% of psychiatric disorders in the population were attributable to ADHD.
Conclusion
The association between ADHD and psychiatric comorbidities differed significantly among men and women. Clinicians treating adults with ADHD should be aware of these frequent and gender‐specific comorbidities, such that early treatment can be offered.
Keywords: attention deficit hyperactivity disorder, gender, epidemiology, psychiatric disorders, comorbidity
Significant outcomes.
Both men and women with ADHD had a 4–9 times higher prevalence of anxiety, depression, bipolar and personality disorders, schizophrenia and substance use disorder (SUD) than the remaining adult population.
Differences in prevalence between ADHD and non‐ADHD adults were significantly larger in women than in men for all psychiatric disorders except schizophrenia and SUD, indicating the larger potential for introducing preventive measures in women with ADHD.
A considerable proportion of cases of anxiety, depression, bipolar and personality disorders, schizophrenia and SUD in the population can be attributed to an underlying comorbid ADHD.
Limitations.
This study employed a cross‐sectional design, limiting the possibility of making causal conclusions.
Information on ADHD and psychiatric comorbid disorders was based on data registered in the Norwegian Prescription Database from 2004 to 2015 and in the Norwegian Patient Registry from 2008 to 2015, limiting the study of temporal relations.
Information on psychiatric comorbid disorders was based on diagnoses registered in secondary health care, missing comorbidities registered in primary care.
Introduction
Attention deficit hyperactivity disorder (ADHD) 1, 2 is an impairing and prevalent childhood‐onset disorder that frequently persists into adulthood 3, 4, 5. Based on an estimated worldwide prevalence of 2.5% among adults, ADHD affects millions of individuals across the world and is of major public health concern 3, 6, 7. The strong male predominance among children with ADHD decreases with age; further, comorbidity with other psychiatric disorders is the rule rather than the exception, particularly in adults with ADHD 8, 9, 10, 11, 12. It is also known that women with ADHD are more frequently diagnosed with the inattentive subtype, as defined in DSM‐IV/DSM‐5 1, 13, with more internalizing comorbid disorders such as depression and anxiety. Women also report more impairment than men 11, 14, 15, 16, 17, and a study based on self‐reports among adults showed that women with ADHD, more often than men, reported a history of treatment for other psychiatric disorders than ADHD 8. The combined subtype, with more externalizing symptoms, is more frequent in men 17. This subtype is more often linked to antisocial personality disorder and substance use disorder (SUD) 11, 18.
Several studies have focused on psychiatric comorbidity in adults with ADHD, for example anxiety and major depressive disorder (depression) 3, 11, bipolar disorder 9, 10, 11, 19, personality disorders 20, 21, schizophrenia spectrum disorders (schizophrenia) 19, 22, 23 and SUD 11, 24. However, existing studies of gender differences in such comorbidity have shown conflicting results in adults with ADHD, possibly because of varying outcome measures, sample characteristics and methodologies. To gain a better understanding of gender differences is important in order to be in a position to provide suitable treatment and prevention strategies for both men and women with ADHD 18, 25. Few studies have investigated whether these comorbidities differ between men and women 26, 27, and large epidemiological studies of good quality are still lacking 7, 18.
In the present work, we use the term ‘gender’ instead of ‘sex’ because the study concerns adults, and ‘gender’ is shaped by environment and experience in addition to the biological characteristics determined by sex 28.
Aims of the study
We aimed at determining whether gender modified associations between ADHD and psychiatric comorbidities. We also aimed at determining the proportion of psychiatric disorders among men and women in the population that could be attributed to a comorbid ADHD.
Method
Study population
We conducted a cross‐sectional analysis in a cohort of adults in Norway, by linking information from four nationwide, population‐based registries: The Medical Birth Registry of Norway (MBRN), established in 1967 29, the Norwegian Prescription Database (NorPD) 30, established in 2004, the Norwegian Patient Registry (NPR) 31, with data from 2008, and the National Educational Database (NUDB) from Statistics Norway 32, 33. See Appendix S1 for Supporting Information and details about the registries. The study included all individuals born between 1967 and 1997, alive and resident in Norway at record linkage in 2015 (n = 1 701 206). Record linkage was established using the national identification number unique to every Norwegian resident.
The study was approved by the Regional Ethics Committee in Norway (2011/2272). No informed consent was required for the analysis of anonymized registry data.
We defined adults with ADHD as those who had been dispensed their last prescription of ADHD medication at 18 years of age or more during 2004–2015 (NorPD), or with an ADHD diagnosis registered at 18 years or higher in the period 2008–2015 (NPR). The ADHD medications identified were the central stimulants: methylphenidate, racaemic amphetamine and dexamphetamine, and the non‐stimulant drug atomoxetine, see Appendix S2 for ADHD medication used for narcolepsy.
The remaining population included all adults (18 years or older by record linkage) who had neither been dispensed ADHD medication nor had an ADHD diagnosis, in the NorPD and NPR respectively. Parents to adults with and without ADHD were also identified through the MBRN, to evaluate the influence of factors known to be associated with both ADHD and other psychiatric disorders (sociodemographic variables, pregnancy‐related risk factors and parental psychiatric disorders).
Measures
We analysed the association between ADHD and psychiatric disorders among men and women, ADHD being our ‘exposure’, and evaluated effect modification by gender. Our main aim was to evaluate psychiatric comorbidity in adults with ADHD, and for this analysis, no confounding variables are relevant; thus, we only adjusted for age (birth year; 5‐year groups from 1967 to 1997, with 1967–1973 as the reference period). To evaluate how risk factors for both ADHD and other psychiatric disorders influenced the prevalence ratios, we ran two regression models, including the following covariates that all have been documented as risk factors for ADHD and psychiatric disorders 34, 35, 36, 37, 38, 39, 40, 41: Model 1: birth year, maternal marital status (single, married/cohabiting (reference category), other), maternal age (<20, 20–24, 25–29 (reference value), 30–34, 35–39, 40+) and paternal age (<20, 20–24, 25–29, 30–34 (reference value), 35–39, 40–44, 45–49, 50+) at delivery, parent's highest attained educational level at record linkage (low (<10 years of education), middle (10–12 years of education) and high level (>12 years of education (reference category)), the individual's gestational age in weeks (<27, 28–31, 32–34, 35–36, 37–41 (reference value), 42+) and gestational age‐ and sex‐specific birthweight z‐scores (<‐2.0; −2.0 to −0.51; −0.5 to 0.5 (reference value); 0.51 to 2.0; 2.01+).
Model 2 further included mothers’ and fathers’ psychiatric diagnoses (yes/no), including ADHD or any other psychiatric diagnosis from NPR, 2008–2015.
We studied the following major comorbid psychiatric disorders, typically diagnosed in late adolescence and adulthood, and all registered at 18 years or more: anxiety (ICD‐10 codes; F40‐F42), depression (F32‐F33), bipolar (F30‐F31) and personality disorders (F60‐F61), schizophrenia (F20‐F29) and SUD (F10‐F19).
To define bipolar disorder, we used data from the NorPD in addition to the NPR including individuals who had been prescribed and dispensed either lithium during 2004–2015 or anti‐epileptic drugs with mood disorders as the indication during 2008–2015 (indications for psychotropic medications are only available in the NorPD since 2008).
Statistical analysis
Absolute prevalence differences (PD) of psychiatric disorders between persons with and without ADHD among men and women were calculated using predicted prevalences from a Poisson regression model with adjustment for birth year (5‐year periods). Significance of interaction by gender on the additive scale was evaluated using relative excess risk due to interaction (RERI) 42. While it has been suggested that effect measures and interactions on the multiplicative scale are better suited to ‘assess causality’, risk differences and interactions on the additive scale are the most important to assess public health relevance, indicating which group may benefit the most from treatment or preventive measures 42. To examine the association between ADHD and other psychiatric disorders on a multiplicative scale, we estimated prevalence ratios (PR) using Poisson regression with robust standard errors 43. Significance of interaction by gender on the multiplicative scale was evaluated by comparing Poisson regression models with and without the interaction term (gender x ADHD) included, as tested by likelihood ratio tests. Finally, we estimated the proportion of psychiatric comorbidities attributable to ADHD among men and women with ADHD (attributable fractions in the exposed—AFE) and in the population (population attributable fractions—PAF) 44. Two‐sided tests with a significance level of 0.05 were used in all analyses. Analyses were carried out with PASW Statistics 23 45 and STATA intercooled v.14 46 from 3 January 2016 to 24 July 2017.
Sensitivity analysis
We conducted several sensitivity analyses to test the robustness of the results, see Appendix S3 in Supporting Information for details: for all psychiatric disorders, we excluded individuals with a diagnosis of mental retardation, and when analysing prevalences of bipolar disorder, we excluded individuals with comorbid schizophrenia. We repeated analyses including only individuals with one psychiatric comorbid diagnosis alone. Analyses were also repeated requiring the psychiatric diagnosis to be registered at least twice in the NPR. Finally, when adjusting for covariates, we used multiple imputation with chained equations (MICE) 47 to evaluate possible biases due to missing information for gestational age. In the main analyses, missing values in covariates (6% for gestational age and birthweight z‐scores, other variables <1%) were handled by listwise deletion. To impute for missing values in gestational age and z‐scores, we ran sensitivity analyses using MICE, where the outcome variables, all specified covariates and also birthweight, maternal preeclampsia and mother's chronic diseases (yes/no), were used for information.
Results
Study groups
We identified a total of 40 103 adults with ADHD (2.4% of the population), 17 815 women (44.4%), with a total mean age of 31 years in 2015. The remaining population consisted of 1 661 103 adults, 812 061 women (48.9%) and a mean age for the total sample of 33 years in 2015. The male : female ratio in the ADHD group was 1.3 : 1. As shown in Table 1, more mothers of ADHD adults than remaining mothers had the lowest educational level (34.9% vs. 26.2%) and were single when giving birth (16.8% vs. 9.2%). Also, parents of ADHD adults had significantly more psychiatric disorders than parents of the remaining population (mothers: 27.3 vs. 13.4%; fathers: 17.3 vs. 9.9%).
Table 1.
Sample characteristics of the study population, 1 701 206 adults in Norway
| Variable | ADHD, No. (%) | Non‐ADHD, No. (%) | ADHD Women, No. (%) | ADHD Men, No. (%) |
|---|---|---|---|---|
| No. (%) | 40 103 (2.4) | 1 661 103 (97.6) | 17 815 (44.4) | 22 288 (55.6) |
| Gender | ||||
| Women | 17 815 (44.4) | 812 061 (48.9) | ||
| Men | 22 288 (55.6) | 849 042 (51.1) | ||
| M:F ratio | 1.25 | 1.05 | ||
| Mean age in 2015 (years) (SD) | P < 0.001a | P < 0.001b | ||
| 31.2 (8.3) | 33.1 (9.3) | 31.4 (8.4) | 31.0 (8.2) | |
| Gestational age (weeks) | P < 0.001a | P < 0.001b | ||
| <27 | 113 (0.3) | 2464 (0.2) | 43 (0.3) | 70 (0.3) |
| 28–31 | 283 (0.8) | 7835 (0.5) | 101 (0.6) | 182 (0.9) |
| 32–34 | 677 (1.9) | 22 239 (1.4) | 270 (1.7) | 407 (2.0) |
| 35–36 | 1313 (3.6) | 49 624 (3.2) | 532 (3.3) | 781 (3.8) |
| 37–41 | 28 552 (77.9) | 1 250 422 (80.3) | 12 660 (77.8) | 15 892 (78.1) |
| 42+ | 5701 (15.6) | 223 779 (14.4) | 2661 (16.4) | 3040 (14.9) |
| Missing | 3464 (8.6) | 104 740 (6.3) | 1548 (8.7) | 1916 (8.6) |
| Maternal marital status | P < 0.001a | P = 0.9b | ||
| Married/cohabitant | 32 342 (80.9) | 1 489 193 (89.8) | 14 354 (80.8) | 17 988 (80.9) |
| Single | 6708 (16.8) | 152 884 (9.2) | 2996 (16.9) | 3712 (16.7) |
| Other | 944 (2.4) | 16 250 (1.0) | 419 (2.4) | 525 (2.4) |
| Missing | 109 (0.3) | 2776 (0.2) | 46 (0.3) | 63 (0.3) |
| Maternal educational status | P < 0.001a | P = 0.8b | ||
| Low | 13 892 (34.9) | 432 778 (26.2) | 6197 (35.0) | 7695 (34.7) |
| Middle | 17 061 (42.8) | 771 795 (46.7) | 7629 (43.1) | 9432 (42.6) |
| High | 8903 (22.3) | 449 945 (27.2) | 3877 (21.2) | 5026 (22.7) |
| Missing | 247 (0.6) | 6585 (0.4) | 112 (0.6) | 135 (0.6) |
| Paternal educational status | P < 0.001a | P = 0.006b | ||
| Low | 12 889 (33.0) | 382 793 (23.4) | 5695 (32.8) | 7194 (33.2) |
| Middle | 19 320 (49.5) | 838 027 (51.2) | 8746 (50.4) | 10 574 (48.8) |
| High | 6827 (17.5) | 416 636 (25.4) | 2914 (16.8) | 3913 (18.1) |
| Missing | 1067 (2.7) | 23 647 (1.4) | 460 (2.6) | 607 (2.7) |
| Maternal psychiatric disorder | P < 0.001a | P = 0.99b | ||
| None | 29 149 (72.7) | 1 437 851 (86.6) | 12 977 (72.8) | 16 172 (72.6) |
| Any, including ADHD | 10 953 (27.3) | 223 216 (13.4) | 4838 (27.2) | 6115 (27.4) |
| Paternal psychiatric disorder | P < 0.001a | P = 0.06b | ||
| None | 32 667 (82.7) | 1 485 656 (90.1) | 14 609 (83.2) | 18 058 (82.2) |
| Any, including ADHD | 6848 (17.3) | 162 779 (9.9) | 2941 (16.8) | 3907 (17.8) |
P‐value (Pearson's chi‐square test and t‐test for equality of means) for the difference in ADHD total relative to the comparison population.
P‐value (Pearson's chi‐square test and t‐test for equality of means) for the difference in men with ADHD vs. women with ADHD.
Association between ADHD and psychiatric comorbidities in men and women
Adults with ADHD had a much higher prevalence of additional psychiatric disorders compared to the remaining population, as shown in Fig. 1. As many as 53.5% of women and 48.5% of men with ADHD had one or more of the six studied psychiatric comorbidities, compared to 13.7% of women and 9.1% of men in the remaining population. Women with ADHD had the highest prevalence of all disorders except schizophrenia and SUD (Fig. 1).
Figure 1.
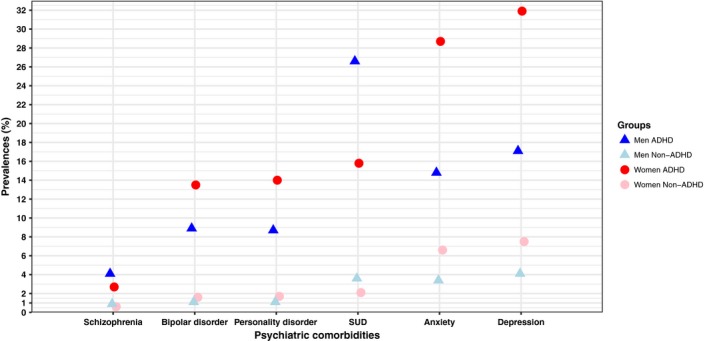
Adjusted* prevalences of psychiatric disorders in men and women with and without ADHD. *Prevalences was adjusted for birth year, 5‐year groups, from 1967 to 1997, with 1967–1973 as the reference. SUD, Substance use disorder.
Evaluated on an absolute scale, the prevalence differences (PD) between adults with and without ADHD were statistically significant for all the psychiatric disorders and ranged from 2.1% (95% CI 2.0–2.3) for schizophrenia to 24.4% (23.8–24.9) for depression, both in women, see Table 2.
Table 2.
Prevalence differences in psychiatric disorders in men and women with and without ADHD. Effect modification by gender evaluated on an additive scale
| Psychiatric disorders (ICD‐10) | Crude prevalences, No. (%) | Prevalence, % (95% CI)a | Additive effect modificationb | |||
|---|---|---|---|---|---|---|
| ADHD | Non‐ADHD | ADHD | Non‐ADHD | PDc (95% CI) | RERId (95% CI) | |
| Anxiety disorders (F40–42) | ||||||
| Women | 4676 (26.3) | 54 479 (6.7) | 28.7 (28.2–29.3) | 6.6 (6.6–6.7) | 22.1 (21.6–22.6) | 1.4 (1.2–1.7)a, e |
| Men | 4054 (18.2) | 28 364 (3.3) | 14.8 (14.5–15.1) | 3.4 (3.4–3.5) | 11.4 (11.1–11.7) | |
| Bipolar disorder (F30–31 or medication)f | ||||||
| Women | 2290 (12.9) | 13 183 (1.6) | 13.5 (13.1–13.9) | 1.6 (1.6–1.6) | 11.9 (11.5–12.3) | 3.4 (2.7–4.0)a |
| Men | 1981 (8.9) | 9009 (1.1) | 8.9 (8.7–9.2) | 1.1 (1.0–1.1) | 7.9 (7.6–8.1) | |
| Major depressive disorder (F32–33) | ||||||
| Women | 5138 (28.8) | 61 880 (7.6) | 31.9 (31.4–32.5) | 7.5 (7.5–7.6) | 24.4 (23.8–24.9) | 1.3 (1.1–1.5)a |
| Men | 4516 (20.3) | 33 733 (4.0) | 17.1 (16.8–17.5) | 4.1 (4.0–4.1) | 13.1 (12.8–13.4) | |
| Personality disorder (F60–61) | ||||||
| Women | 2428 (13.6) | 14 079 (1.7) | 14.0 (13.6–14.5) | 1.7 (1.7–1.7) | 12.3 (11.9–12.7) | 3.8 (3.2–4.4)a |
| Men | 2030 (9.1) | 8909 (1.1) | 8.7 (8.4–8.9) | 1.1 (1.0–1.1) | 7.6 (7.3–7.9) | |
| Schizophrenia spectrum disorder (F20–29) | ||||||
| Women | 444 (2.5) | 4621 (0.6) | 2.7 (2.5–2.8) | 0.6 (0.5–0.6) | 2.1 (2.0–2.3) | −1.8 (−2.2; −1.3)a |
| Men | 928 (4.2) | 7352 (0.9) | 4.1 (3.9–4.3) | 0.9 (0.8–0.9) | 3.3 (3.0–3.5) | |
| Substance use disorder (F10–19) | ||||||
| Women | 2878 (16.2) | 17 200 (2.1) | 15.8 (15.4–16.1) | 2.1 (2.1–2.1) | 13.7 (13.3–14.0) | −2.9 (−3.1; −2.7)a |
| Men | 6135 (27.5) | 30 233 (3.6) | 26.6 (26.1–27.1) | 3.6 (3.5–3.6) | 23.0 (22.5–23.5) | |
ICD‐10, International Statistical Classification of Diseases and Related Health Problems 10th Revision, World Health Organization; CI, confidence interval; PD, prevalence difference; RERI, relative excess in risk due to interaction.
Prevalence adjusted for birth year (5‐year groups, from 1967 to 1997, with 1967–1973 as the reference period).
Female gender as reference group.
Prevalence Difference (PD) between adults with and without ADHD, adjusted for birth year as above.
Relative Excess in Risk due to Interaction (RERI) adjusted for birth year as above.
P‐value of interaction on an additive scale, all P < 0.001.
Medication: lithium during 2004–2015 or anti‐epileptic drugs with mood disorders as the indication during 2008–2015.
Evaluated on a multiplicative scale, adult ADHD was most closely associated with bipolar disorder, personality disorders and SUD, with PR estimates ranging from 7.2 (95% CI, 7.0–7.5) for SUD in women to 8.9 (8.5–9.3) for bipolar and personality disorders in men. Associations with anxiety, depression and schizophrenia were weaker, though still strong, with a four to five times higher prevalence of these disorders in both men and women with ADHD than those without, see Table 3.
Table 3.
Prevalence ratios of psychiatric disorders men and women with and without ADHD. Effect modification by gender evaluated on a multiplicative scale
| Psychiatric disorders | Crude prevalences, No. (%) | Prevalence ratios (95% CI) | Attributable fraction (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| ADHD | Non‐ADHD | Crudea | Model 1b | Model 2c | AFEd | PAFe | |
| Anxiety Disorders | P < 0.001f | P < 0.001 | P < 0.001 | g | |||
| Women | 4676 (26.3) | 54 479 (6.7) | 3.7 (3.7–3.8) | 3.6 (3.5–3.7) | 3.4 (3.3–3.5) | 73.3 (72.6–74.0) | 5.8 (5.6–6.0) |
| Men | 4054 (18.2) | 28 364 (3.3) | 5.3 (5.2–5.5) | 5.1 (4.9–5.2) | 4.7 (4.5–4.8) | 81.2 (80.6–81.7) | 10.2 (9.8–10.5) |
| Bipolar Disorder | P = 0.03 | P = 0.03 | P = 0.07 | ||||
| Women | 2290 (12.9) | 13 183 (1.6) | 8.0 (7.7–8.3) | 7.8 (7.5–8.2) | 7.2 (6.8–7.5) | 87.5 (87.0–88.0) | 13.0 (12.4–13.5) |
| Men | 1981 (8.9) | 9009 (1.1) | 8.9 (8.5–9.3) | 8.9 (8.5–9.4) | 8.1 (7.7–8.5) | 88.8 (88.2–89.3) | 16.0 (15.3–16.7) |
| Major depressive disorder | P < 0.001 | P < 0.001 | P < 0.001 | ||||
| Women | 5138 (28.8) | 61 880 (7.6) | 3.7 (3.6–3.8) | 3.6 (3.5–3.7) | 3.3 (3.2–3.4) | 72.9 (72.2–73.5) | 5.6 (5.4–5.8) |
| Men | 4516 (20.3) | 33 733 (4.0) | 5.1 (5.0–5.3) | 4.9 (4.8–5.0) | 4.5 (4.4–4.6) | 80.5 (79.9–81.0) | 9.5 (9.2–9.8) |
| Personality disorder | P = 0.001 | P = 0.008 | P = 0.02 | ||||
| Women | 2428 (13.6) | 14 079 (1.7) | 7.7 (7.3–8.0) | 7.1 (6.8–7.4) | 6.5 (6.2–6.8) | 86.9 (86.4–87.5) | 12.8 (12.3–13.3) |
| Men | 2030 (9.1) | 8909 (1.1) | 8.9 (8.5–9.3) | 8.1 (7.7–8.5) | 7.3 (6.9–7.7) | 88.8 (88.2–89.3) | 16.5 (15.8–17.2) |
| Schizophrenia spectrum disorder | P = 0.08 | P = 0.07 | P = 0.1 | ||||
| Women | 444 (2.5) | 4621 (0.6) | 4.5 (4.1–4.9) | 4.5 (4.1–5.0) | 4.1 (3.7–4.6) | 77.7 (75.4–79.7) | 6.8 (6.0–7.6) |
| Men | 928 (4.2) | 7352 (0.9) | 4.9 (4.6–5.2) | 4.8 (4.5–5.2) | 4.3 (4.0–4.7) | 79.5 (78.0–80.8) | 8.9 (8.2–9.6) |
| Substance use disorder | P = 0.4 | P = 0.7 | P = 0.98 | ||||
| Women | 2878 (16.2) | 17 200 (2.1) | 7.2 (7.0–7.5) | 6.3 (6.1–6.6) | 5.8 (5.6–6.0) | 86.2 (85.7–86.7) | 12.4 (11.9–12.8) |
| Men | 6135 (27.5) | 30 233 (3.6) | 7.6 (7.4–7.8) | 6.6 (6.5–6.8) | 6.1 (6.0–6.3) | 86.8 (86.5–87.1) | 14.6 (14.3–15.0) |
CI, Confidence interval; ADHD, adults with ADHD; non‐ADHD, remaining population without ADHD; AFE, attributable fraction among the exposed; PAF, population attributable fraction.
Adjusted for birth year (5‐year groups from 1967 to 1997, with 1967–1973 as the reference period).
Model 1: Adjusted for birth year, maternal marital status (single, married/cohabiting (reference category), other), maternal and paternal education (low (<10 years of education), middle (10–12 years of education and high level (>12 years of education (reference category)), maternal age (<20, 20–24, 25–29 (reference value), 30–34, 35–39, 40+) and paternal age (<20, 20–24, 25–29, 30–34 (reference value), 35–39, 40–44, 45–49, 50+) at delivery, gestational age (<27, 28–31, 32–34, 35–36, 37–41 (reference value), 42+), gestational age and sex‐specific birthweight z‐scores (<−2.0; −2.0 to −0.51; −0.5 to 0.5 (reference value); 0.51–2.0; 2.01+).
Model 2: As in Model 1 and additionally adjusted for maternal and paternal psychiatric disorders (yes/no).
Attributable fraction among the exposed (AFE) (%) (=ADHD population), based on crude model.
Population attributable fraction (PAF) (%), based on crude model.
P‐value of the interaction between ADHD and sex on a multiplicative scale.
Statistical significant difference between men and women with ADHD based on non‐overlapping 95% confidence intervals.
Interaction by gender
Interaction by gender was tested both on the additive and the multiplicative scales, see Tables 2 and 3. When testing for interaction by gender on an additive scale, the PDs were significantly larger in women than in men for all psychiatric comorbidities except schizophrenia and SUD, where the PDs were larger in men. On the multiplicative scale, the associations with ADHD were significantly stronger in men than in women for anxiety, depression, bipolar and personality disorders, see Table 3.
Attributable proportions
A large proportion of psychiatric disorders among adults with ADHD could be attributed to their existing ADHD condition, with AFE ranging from 72.9% to 87.5% in women and 79.5% to 88.8% in men, see Table 3. The proportions of psychiatric disorders in the adult population that could be attributed to a comorbid ADHD were also high, with PAF ranging from 5.6% to 13.0% in women and from 8.9% to 16.5% in men.
Sensitivity analysis
The results of the sensitivity analyses are shown in Supporting Information, Tables S1–S3. All sensitivity analyses were compatible with the results of the main analyses.
Discussion
This is the first large population‐based study performed on adults clinically diagnosed with ADHD to evaluate gender differences in major psychiatric comorbidities and testing for interaction by gender on both multiplicative and additive scales. Both men and women with ADHD had 4–9 times higher prevalences of all the studied psychiatric disorders than the remaining adult population. However, on an absolute scale, differences in prevalence between ADHD and non‐ADHD adults were significantly larger in women than in men for all psychiatric disorders except schizophrenia and SUD, indicating the larger potential for preventive measures in women with ADHD. The proportions of psychiatric disorders in the population attributable to a comorbid ADHD were large for both genders.
In line with previous studies in the literature, we found higher prevalences of all the studied comorbidities in adults with ADHD than in those without 3, 10. However, few previous studies have evaluated gender differences in comorbidity among adults with ADHD, and results from existing studies are conflicting. A study of 219 clinically diagnosed adults with ADHD, including 37.4% women, found no gender difference in risk of anxiety, bipolar disorder, depression, SUD and antisocial personality disorder, but that study was in all likelihood underpowered 11. One of the largest population‐based studies until now, a twin‐study using self‐reported symptom scores for both ADHD and other psychiatric disorders, studied anxiety, bipolar disorder, depression and alcohol dependence. Similar relative risk estimates for anxiety and bipolar disorder as in our study were reported, but gender differences were not found 26. In another recent twin‐study based on self‐reported symptom scores, a high risk of comorbid SUD in adults with ADHD was reported, but this did not report finding any gender differences 24. Among studies showing high risk of comorbid bipolar disorder, one was large and population‐based, but involved both children and adults 19; another study was small with low female representation 11. Both studies considered gender differences, but none were found. A large Swedish study analysed risk of comorbid schizophrenia, but did not focus on adults and did not evaluate gender differences 19. A smaller Danish study found the same relative risk of comorbid psychosis as observed here, but in adults diagnosed with ADHD as children. The study only included a small proportion of women, and an evaluation of gender differences was thus not possible 22. A large study from Taiwan with over 70 000 individuals with ADHD diagnosed in childhood reported a five times higher risk of developing some form of psychotic disorder. The male proportion was 80%, and mean age at diagnosed psychosis was only 15 years. An increased risk for psychosis in women with ADHD was, however, found 23. The number of studies on ADHD and different personality disorders is smaller and mostly performed on young adults and adolescents, where ADHD was diagnosed in childhood. Hazard ratios of 5.8 for personality disorders ‘not specified’ and 3.1 for antisocial personality disorder have been reported without specification of gender 21, 48.
Most previous studies have their limitations: they have either relied on self‐reported diagnosis of ADHD diagnosis or screening questionnaires, many studies are small, and most of them have a low proportion of females or include individuals younger than 18 years at the time of comorbid diagnosis. Few studies have been population‐based or focused specifically on gender differences in risk of comorbidities in adults.
In a recent narrative meta‐analysis of gender differences in adult ADHD, Williamson and Johnston found that only three of 11 studies included appropriate comparison groups 18. However, the most important difference, and novelty of the present study, is that we tested for interaction by gender on an additive scale, thus using the prevalence differences to estimate the prevention potential. We also calculated the proportion of major psychiatric disorders that could be attributed to ADHD in the adult population.
Testing for interaction on the additive scale is informative for clinical and public health questions, because it may indicate which subgroups need to be prioritized such that preventive measures and interventions can be introduced 42. We found that differences in prevalences of anxiety, depression, bipolar and personality disorders between adults with and without ADHD were significantly larger for women than for men, while the opposite was true for SUD and schizophrenia. Previous investigations have failed to show these gender differences in psychiatric comorbidities, and none have evaluated interactions on an additive scale. Women with ADHD have been shown to report more symptoms and impairments resulting from their condition than men, thus possibly predisposing them to a higher level of psychiatric comorbidity 11, 14, 15, 16, 49. Our results show that there is a relatively higher increase in prevalence of most psychiatric comorbidities associated with ADHD in women with ADHD fitting this. Detecting and treating ADHD in girls and women may prove to be an important preventive measure in order to reduce the risk of future psychiatric comorbidity. Paying more attention towards girls and women with ADHD, who have less hyperactivity and therefore may go undiagnosed during childhood years, may thus be warranted, both among clinicians and researchers 25. The larger increase in SUD and schizophrenia associated with ADHD in men is also of importance, and clinicians treating adults with ADHD should be aware of the gender‐specific comorbidities described in our study, both with respect to detection and the offer of early treatment following diagnosis.
The larger increase in prevalence of schizophrenia associated with ADHD in men might be related to the larger increase in prevalence of SUD, also found in men. Both having ADHD 10, 24 and being a male 50, 51 increase the risk of SUD, and SUD itself may increase the risk of psychosis 52. To test this hypothesis, we excluded all individuals with SUD in the study population (n = 62 434) and reran the PD analyses for schizophrenia. The PDs of schizophrenia in women with and without ADHD changed from 2.1 (95% CI, 2.1–2.1) to 1.1 (1.0–1.3) and in men from 3.3 (3.0–3.5) to 1.4 (1.2–1.6). The gender difference was still statistically significant (RERI −0.66, 95% CI, −1.3 – −0.07). We therefore believe that the increased risk of schizophrenia in men with ADHD may be partly, although not fully explained, by a comorbid SUD. The apparent increased vulnerability to schizophrenia in men with ADHD could be of clinical importance. In contrast, when excluding all cases with SUD, the PD for women was no longer significant when compared to women without ADHD.
The relatively increased risk of anxiety and depression in men with ADHD on the multiplicative scale may partly be explained by the low prevalence of these disorders in men without ADHD, who generally have lower health‐seeking behaviour 53. Men with ADHD are already in contact with the health services and may therefore get these comorbid disorders diagnosed more easily than their non‐ADHD counterparts. Although both men and women with ADHD are in contact with the health services, women, independently of ADHD, are generally in closer contact with the health services than men, due to, for example, maternal health issues (fertility regulation, pregnancy and childbirth) 54. This may partly explain why disorders such as depression and anxiety are more easily detected in women than in men in the general population 50, 55.
The gender‐specific pattern of psychiatric disorders that we find among adults with ADHD in our study is similar to the pattern found in the general population 50, 51, 56. The absolute prevalence rates are, however, much higher for both men and women with ADHD, as shown in Fig. 1. Although the presence of ADHD enhances the trend among men and women in the general population, it is evident that the magnitude of this enhancement differs between men and women and is also dependent on the specific disorder.
To evaluate how associations between ADHD and psychiatric comorbidities were influenced by common risk factors for both ADHD and other psychiatric disorders, we adjusted for socioeconomic and perinatal risk factors (Model 1). This hardly changed the PR estimates. When also including psychiatric disorders of the parents in the model (Model 2), the estimates were slightly attenuated, suggesting that genetic predisposition or problems linked to having parents suffering from psychiatric diseases are important, see Table 3. This calls for increased attention regarding children of parents being treated for psychiatric disorders.
Strengths and limitations
Our study has several strengths. We used data from nationwide health registries of good quality and with mandatory, prospective reporting, minimizing selection bias and loss to follow‐up and eliminating recall bias. Bipolar disorder and schizophrenia registration in the NPR have been validated with good results 31. Due to the large study population with almost 45% women with ADHD, we could evaluate less prevalent disorders, such as schizophrenia, and compare psychiatric comorbidity in men and women with representative numbers in both groups. We had prospectively registered data on perinatal factors (birthweight and gestational age) for the whole study population, and we had information on psychiatric diagnoses, including ADHD, for the parents. Therefore, we could adjust for these covariates to evaluate whether these risk factors explained the increased prevalence of psychiatric comorbidities in adults with ADHD.
Unlike some other large Scandinavian population‐based studies, we did not use ADHD symptom ratings or self‐reports to define ADHD. ADHD medication is restricted in Norway, and medical treatment in adults is initiated only after thorough assessment by a specialist in psychology or psychiatry. Therefore, we believe that a prescribed and dispensed prescription of ADHD medication is a good proxy for a clinical ADHD diagnosis. Calculating PDs and testing for interaction by gender on the additive scale give relevant information concerning which comorbid diagnoses clinicians should be especially aware of when following men and women with ADHD. Our estimates of attributable risk of comorbid disorders in men and women with ADHD underscore the gender‐specific prevention potential.
We are aware that our study also has some limitations: analyses were cross‐sectional and based on data registered in the NorPD from 2004–15 and in the NPR from 2008–15, limiting the study of temporal relations. However, as ADHD is defined as a neuropsychiatric disorder with onset in childhood, we may assume that ADHD was present before the comorbid psychiatric disorders, which all are typically diagnosed in late adolescence and adulthood. Since the NorPD was established in 2004, adults diagnosed and treated for ADHD only before 2004 and not after will be undetected. However, ADHD was not understood as a disorder of adulthood before the late 1990s, and during 1997–2005, adults in Norway were only allowed to receive medical treatment with central stimulants after a thorough evaluation by one of three regional diagnostic committees 8. Further, some ADHD patients will not receive medication because of contraindications or other causes; these patients are identified in the NPR, but only from 2008 and onwards. During 2008–2015, a total of 9346 (23.3%) adults with ADHD were registered with ADHD in the NPR without receiving medication.
The NPR was the data source for defining psychiatric comorbidities. In Norway, many psychiatric patients are followed in primary health care after diagnosis, and treatment is established in secondary care, for example patients with bipolar disorder who are stable on medication. A recent study from Sweden reported that almost 80% of the most common mental disorders were treated in primary care 57. For bipolar disorder, we therefore used the NorPD as an additional data source. It is likely that patients with the more severe disorders such as schizophrenia 31 and severe personality disorders will likely have some contact with specialist health care throughout life and should therefore be captured by the NPR.
As discussed above, it may be argued that adults with ADHD could more easily be diagnosed with other psychiatric disorders because they are already in contact with the health services 55. This may be true, especially for depression and anxiety in men, who in general have little contact with the health service before old‐age 54. However, adults with bipolar disorder, schizophrenia, personality disorders and SUD are likely to be referred to secondary health care also in the non‐ADHD population.
To conclude, a large proportion of both men and women with ADHD have comorbid psychiatric disorders, and a considerable proportion of anxiety, bipolar disorder, depression, schizophrenia, SUD and personality disorders in the population can be attributed to an underlying comorbid ADHD. The differences in prevalence of anxiety, depression, bipolar and personality disorders in adults with and without ADHD are larger for women than for men. Clinicians treating women with ADHD should be aware of these comorbidities, to both detect the conditions and offer early treatment if diagnosed. Similarly, the possibility of a comorbid SUD or schizophrenia spectrum disorder is particularly relevant when treating men with ADHD. Importantly, clinicians should also be aware of a possible underlying ADHD when adults present with symptoms of other psychiatric disorders. Identifying children and adolescents with ADHD at earlier stages may be an important preventive measure to reduce the risk of future psychiatric comorbidity. This may be particularly important in girls and women with ADHD, who often have a lower degree of hyperactivity and are therefore at an increased risk of being undiagnosed in childhood, with a higher risk of developing other psychiatric disorders as a possible consequence.
Declaration of interests
J.H. has served as a speaker for Eli‐Lilly, HB Pharma and Shire. The other authors declare no conflict of interests.
Supporting information
Table S1. Prevalence ratio of psychiatric disorders comparing adults with and without ADHD when (a) mental retardation is excluded and (b) schizophrenia is excluded from bipolar.
Table S2. Prevalence ratio of psychiatric disorders comparing adults with and without ADHD when (a) all individuals have only one (additional) psychiatric disorder or (b) psychiatric disorders registered at least twice in the Norwegian Patient Registry (NPR).
Table S3. Prevalence ratio of psychiatric disorders comparing adults with and without ADHD, using missing imputation for gestational age and sex‐specific birthweight by gestational age z‐scores.
Appendix S1. Registries.
Appendix S2. Narcolepsy.
Appendix S3. Sensitivity Analysis.
Acknowledgements
We wish to thank Tor Arne Hegvik, MD, for contributions with the graphics.
Funding
This study was supported by Stiftelsen Kristian Gerhard Jebsen, University of Bergen and European Union's Horizon 2020 research and innovation programme under grant agreement 667302 (CoCA).
Solberg BS, Halmøy A, Engeland A, Igland J, Haavik J, Klungsøyr K. Gender differences in psychiatric comorbidity: a population‐based study of 40 000 adults with attention deficit hyperactivity disorder.
Previous presentations: Oral presentation at the 6th World Congress on ADHD, Vancouver, Canada, 20–23 April 2017.
References
- 1. American Psychiatric Association . Fifth Edition of Diagnostic and Statistical Manual of Mental Disorders, DSM‐5, 2013.
- 2. World Health Organization . The ICD‐10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization; 1993. [Google Scholar]
- 3. Kessler RC, Adler L, Barkley R et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiat 2006;163:716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Faraone SV, Biederman J, Mick E. The age‐dependent decline of attention deficit hyperactivity disorder: a meta‐analysis of follow‐up studies. Psychol Med 2006;36:159–165. [DOI] [PubMed] [Google Scholar]
- 5. Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet 2016;387:1240–1250. [DOI] [PubMed] [Google Scholar]
- 6. Staller J, Faraone SV. Attention‐deficit hyperactivity disorder in girls: epidemiology and management. CNS Drugs 2006;20:107–123. [DOI] [PubMed] [Google Scholar]
- 7. Simon V, Czobor P, Balint S, Meszaros A, Bitter I. Prevalence and correlates of adult attention‐deficit hyperactivity disorder: meta‐analysis. Brit J Psychiat 2009;194:204–211. [DOI] [PubMed] [Google Scholar]
- 8. Halmoy A, Fasmer OB, Gillberg C, Haavik J. Occupational outcome in adult ADHD: impact of symptom profile, comorbid psychiatric problems, and treatment: a cross‐sectional study of 414 clinically diagnosed adult ADHD patients. J Attent Dis 2009;13:175–187. [DOI] [PubMed] [Google Scholar]
- 9. Halmoy A, Halleland H, Dramsdahl M, Bergsholm P, Fasmer OB, Haavik J. Bipolar symptoms in adult attention‐deficit/hyperactivity disorder: a cross‐sectional study of 510 clinically diagnosed patients and 417 population‐based controls. J Clin Psychiat 2010;71:48–57. [DOI] [PubMed] [Google Scholar]
- 10. Sobanski E. Psychiatric comorbidity in adults with attention‐deficit/hyperactivity disorder (ADHD). Eur Arch Psychiatry Clin Neurosci 2006;256(Suppl 1):i26–i31. [DOI] [PubMed] [Google Scholar]
- 11. Biederman J, Faraone SV, Monuteaux MC, Bober M, Cadogen E. Gender effects on attention‐deficit/hyperactivity disorder in adults, revisited. Biol Psychiat 2004;55:692–700. [DOI] [PubMed] [Google Scholar]
- 12. Maibing CF, Pedersen CB, Benros ME, Mortensen PB, Dalsgaard S, Nordentoft M. Risk of Schizophrenia increases after all child and adolescent psychiatric disorders: a nationwide study. Schizophr Bull 2014;41:963–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. American Psychiatric Association . Diagnostic and statistical manual of mental disorders, 4th edn, Text Revision (DSM‐IV‐TR). Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 14. Vildalen VU, Brevik EJ, Haavik J, Lundervold AJ. Females with ADHD report more severe symptoms than males on the adult ADHD self‐report scale. J Attent Dis 2016. https://doi.org/10.1177/1087054716659362 [DOI] [PubMed] [Google Scholar]
- 15. Hinshaw SP, Owens EB, Zalecki C et al. Prospective follow‐up of girls with attention‐deficit/hyperactivity disorder into early adulthood: continuing impairment includes elevated risk for suicide attempts and self‐injury. J Consult Clin Psych 2012;80:1041–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fedele DA, Lefler EK, Hartung CM, Canu WH. Sex differences in the manifestation of ADHD in emerging adults. J Attent Dis 2012;16:109–117. [DOI] [PubMed] [Google Scholar]
- 17. Willcutt EG. The prevalence of DSM‐IV attention‐deficit/hyperactivity disorder: a meta‐analytic review. Neurotherapeutics: the journal of the American Society for Experimental. Neurotherapeutics 2012;9:490–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Williamson D, Johnston C. Gender differences in adults with attention‐deficit/hyperactivity disorder: A narrative review. Clin Psychol Rev 2015;40:15–27. [DOI] [PubMed] [Google Scholar]
- 19. Larsson H, Ryden E, Boman M, Langstrom N, Lichtenstein P, Landen M. Risk of bipolar disorder and schizophrenia in relatives of people with attention‐deficit hyperactivity disorder. Brit J Psychiat 2013;203:103–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Matthies S, Philipsen A. Comorbidity of personality disorders and adult attention deficit hyperactivity disorder (ADHD)‐review of recent findings. Curr Psychiatry Rep 2016;18:33. [DOI] [PubMed] [Google Scholar]
- 21. Biederman J, Monuteaux MC, Mick E et al. Young adult outcome of attention deficit hyperactivity disorder: a controlled 10‐year follow‐up study. Psychol Med 2006;36:167–179. [DOI] [PubMed] [Google Scholar]
- 22. Dalsgaard S, Mortensen PB, Frydenberg M, Maibing CM, Nordentoft M, Thomsen PH. Association between attention‐deficit hyperactivity disorder in childhood and schizophrenia later in adulthood. Eur Psychiatry 2014;29:259–263. [DOI] [PubMed] [Google Scholar]
- 23. Shyu YC, Yuan SS, Lee SY et al. Attention‐deficit/hyperactivity disorder, methylphenidate use and the risk of developing schizophrenia spectrum disorders: a nationwide population‐based study in Taiwan. Schizophr Res 2015;168:161–167. [DOI] [PubMed] [Google Scholar]
- 24. Capusan AJ, Bendtsen P, Marteinsdottir I, Larsson H. Comorbidity of adult ADHD and its subtypes with substance use disorder in a large population‐based epidemiological study. J Attent Dis 2016. https://doi.org/10.1177/1087054715626511 [DOI] [PubMed] [Google Scholar]
- 25. Rucklidge JJ. Gender differences in attention‐deficit/hyperactivity disorder. Psychiatr Clin North Am 2010;33:357. [DOI] [PubMed] [Google Scholar]
- 26. Friedrichs B, Igl W, Larsson H, Larsson JO. Coexisting psychiatric problems and stressful life events in adults with symptoms of ADHD–a large Swedish population‐based study of twins. J Attent Dis 2012;16:13–22. [DOI] [PubMed] [Google Scholar]
- 27. Ottosen C, Petersen L, Larsen JT, Dalsgaard S. Gender differences in associations between attention‐deficit/hyperactivity disorder and substance use disorder. J Am Acad Child Adolesc Psychiatry 2016;55(–34):227–234. e4 [DOI] [PubMed] [Google Scholar]
- 28. IOM (INSTITUTE OF MEDICINE) . Exploring the biological contributions to human health: does sex matter? Washington, DC: National Academy Press, 2001. [PubMed] [Google Scholar]
- 29. Irgens LM. The Medical Birth Registry of Norway. Epidemiological research and surveillance throughout 30 years. Acta Obstet Gynecol Scand 2000;79:435–439. [PubMed] [Google Scholar]
- 30. Furu K, Wettermark B, Andersen M, Martikainen JE, Almarsdottir AB, Sorensen HT. The Nordic countries as a cohort for pharmacoepidemiological research. Basic Clin Pharmacol Toxicol 2010;106:86–94. [DOI] [PubMed] [Google Scholar]
- 31. Nesvag R, Jonsson EG, Bakken IJ et al. The quality of severe mental disorder diagnoses in a national health registry as compared to research diagnoses based on structured interview. BMC Psychiat 2017;17:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Steingrimsdottir OA, Naess O, Moe JO et al. Trends in life expectancy by education in Norway 1961‐2009. Eur J Epidemiol 2012;27:163–171. [DOI] [PubMed] [Google Scholar]
- 33. Statistics Norway . www.ssb.no/english/. Oslo, 2016.
- 34. Kennedy M, Kreppner J, Knights N et al. Early severe institutional deprivation is associated with a persistent variant of adult attention‐deficit/hyperactivity disorder: clinical presentation, developmental continuities and life circumstances in the English and Romanian Adoptees study. J Child Psychol Psychiatry 2016;57:1113–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Halmoy A, Klungsoyr K, Skjaerven R, Haavik J. Pre‐ and perinatal risk factors in adults with attention‐deficit/hyperactivity disorder. Biol Psychiat 2012;71:474–481. [DOI] [PubMed] [Google Scholar]
- 36. Laurens KR, Luo L, Matheson SL et al. Common or distinct pathways to psychosis? A systematic review of evidence from prospective studies for developmental risk factors and antecedents of the schizophrenia spectrum disorders and affective psychoses. BMC Psychiat 2015;15:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mackinnon N, Kingsbury M, Mahedy L, Evans J, Colman I. The association between prenatal stress and externalizing symptoms in childhood: evidence from the Avon longitudinal study of parents and children. Biol Psychiat 2018;83:100–108. [DOI] [PubMed] [Google Scholar]
- 38. Wickham ME, Senthilselvan A, Wild TC, Hoglund WL, Colman I. Maternal depressive symptoms during childhood and risky adolescent health behaviors. Pediatrics 2015;135:59–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Goetz M, Sebela A, Mohaplova M, Ceresnakova S, Ptacek R, Novak T. Psychiatric disorders and quality of life in the offspring of parents with bipolar disorder. J Child Adolesc Psychopharmacol 2017;27:483–493. [DOI] [PubMed] [Google Scholar]
- 40. Goodday SM, Shuldiner J, Bondy S, Rhodes AE. Exposure to parental psychopathology and offspring's risk of suicide‐related thoughts and behaviours: a systematic review. Epidemiol Psychiatr Sci 2017;1–12. https://doi.org/10.1017/S2045796017000397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Skjaerven R, Gjessing HK, Bakketeig LS. Birthweight by gestational age in Norway. Acta Obstet Gynecol Scand 2000;79:440–449. [PubMed] [Google Scholar]
- 42. Vanderweele Tyler J, Knol Mirjam J. A tutorial on interaction. Epidemiol Meth 2014;3:33–72. [Google Scholar]
- 43. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–706. [DOI] [PubMed] [Google Scholar]
- 44. Eide GE. Attributable fractions for partitioning risk and evaluating disease prevention: a practical guide. Clin Respir J 2008;2:92–103. [DOI] [PubMed] [Google Scholar]
- 45. IBM CORP . RELEASED 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. [Google Scholar]
- 46. STATACORP. STATACORP LP . Stata statistical software: release 14. College Station, TX: STATACORP, 2015. [Google Scholar]
- 47. Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Meth Psych Res 2011;20:40–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yoshimasu K, Barbaresi WJ, Colligan RC et al. Childhood ADHD is strongly associated with a broad range of psychiatric disorders during adolescence: a population‐based birth cohort study. J Child Psychol Psychiatry 2012;53:1036–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Dalsgaard S, Mortensen PB, Frydenberg M, Thomsen PH. Conduct problems, gender and adult psychiatric outcome of children with attention‐deficit hyperactivity disorder. Brit J Psychiat 2002;181:416–421. [DOI] [PubMed] [Google Scholar]
- 50. Kessler RC, McGonagle KA, Zhao S et al. Lifetime and 12‐month prevalence of DSM‐III‐R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry 1994;51:8–19. [DOI] [PubMed] [Google Scholar]
- 51. Holden C. Sex and the suffering brain. Science 2005;308:1574. [DOI] [PubMed] [Google Scholar]
- 52. Addington J, Case N, Saleem MM, Auther AM, Cornblatt BA, Cadenhead KS. Substance use in clinical high risk for psychosis: a review of the literature. Early Interv Psychiatry 2014;8:104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Harris MG, Baxter AJ, Reavley N, Diminic S, Pirkis J, Whiteford HA. Gender‐related patterns and determinants of recent help‐seeking for past‐year affective, anxiety and substance use disorders: findings from a national epidemiological survey. Epidemiol Psych Sci. 2016;25:548–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Vanwijk CMTG, Kolk AM, Vandenbosch WJHM, Vandenhoogen HJM. Male and female morbidity in general‐practice – the nature of sex‐differences. Soc Sci Med 1992;35:665–678. [DOI] [PubMed] [Google Scholar]
- 55. Woodfine JD, Redelmeier DA. Berkson's paradox in medical care. J Intern Med 2015;278:424–426. [DOI] [PubMed] [Google Scholar]
- 56. Green CA. Gender and use of substance abuse treatment services. Alcohol Res Health 2006;29:55–62. [PMC free article] [PubMed] [Google Scholar]
- 57. Sundquist J, Ohlsson H, Sundquist K, Kendler KS. Common adult psychiatric disorders in Swedish primary care where most mental health patients are treated. BMC Psychiat 2017;17:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Prevalence ratio of psychiatric disorders comparing adults with and without ADHD when (a) mental retardation is excluded and (b) schizophrenia is excluded from bipolar.
Table S2. Prevalence ratio of psychiatric disorders comparing adults with and without ADHD when (a) all individuals have only one (additional) psychiatric disorder or (b) psychiatric disorders registered at least twice in the Norwegian Patient Registry (NPR).
Table S3. Prevalence ratio of psychiatric disorders comparing adults with and without ADHD, using missing imputation for gestational age and sex‐specific birthweight by gestational age z‐scores.
Appendix S1. Registries.
Appendix S2. Narcolepsy.
Appendix S3. Sensitivity Analysis.


