Abstract
This study uses National Inpatient Sample survey data to characterize trends in red blood cell, plasma, and platelet transfusions in the United States between 1993 and 2014, a period of time during which trials were demonstrating the safety of restrictive red blood cell transfusion strategies.
Blood transfusions are one of the most common hospital procedures. Randomized trials have demonstrated the safety of restrictive transfusion strategies. Hospitals have subsequently implemented patient blood management programs to facilitate restrictive transfusion practices aimed to improve patient outcomes, reduce costs, and conserve blood. We are unaware of nationally representative studies evaluating temporal trends in red blood cell (RBC), plasma, and platelet transfusions while accounting for the influence of patient-level or hospital-level characteristics.
Methods
The National Inpatient Sample uses a stratified probability sample of 20% of all inpatient discharges (representing approximately 96% of the US population). Analyses were weighted to account for the sampling design and generate nationally representative estimates. This analysis was deemed exempt from obtaining informed consent by the Weill Cornell Medicine institutional review board.
The unit of analysis was a hospitalization. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure codes were used to identify transfusion procedures. The primary outcome was percentage of hospitalizations with 1 or more RBC transfusions (ICD-9-CM code, 99.04) because the majority of transfusions are RBCs; secondary outcomes included percentage of hospitalizations with 1 or more plasma (ICD-9-CM code, 99.07) and 1 or more platelet (ICD-9-CM code, 99.05) transfusions.
Transfusion trends of all 3 components were descriptively examined from 1993 to 2014. Because there was an inflection point in RBC transfusion in 2011 as determined by joinpoint analysis, the analysis focused on trends from 2011 to 2014. Multivariable Poisson regression was used to estimate adjusted risk ratios (aRRs) and 95% CIs comparing the risk of transfusion in 2011 vs 2014. Subgroup analyses were conducted to further explore trends in RBC transfusion by testing statistical interactions between time and each covariate using a design-adjusted Wald F test (P < .05). It was hypothesized a priori that decreases in RBC transfusion might vary by admission type.
A 2-sided P value less than .05 was considered significant. Data analysis was performed using Stata/MP (StataCorp), version 14.
Results
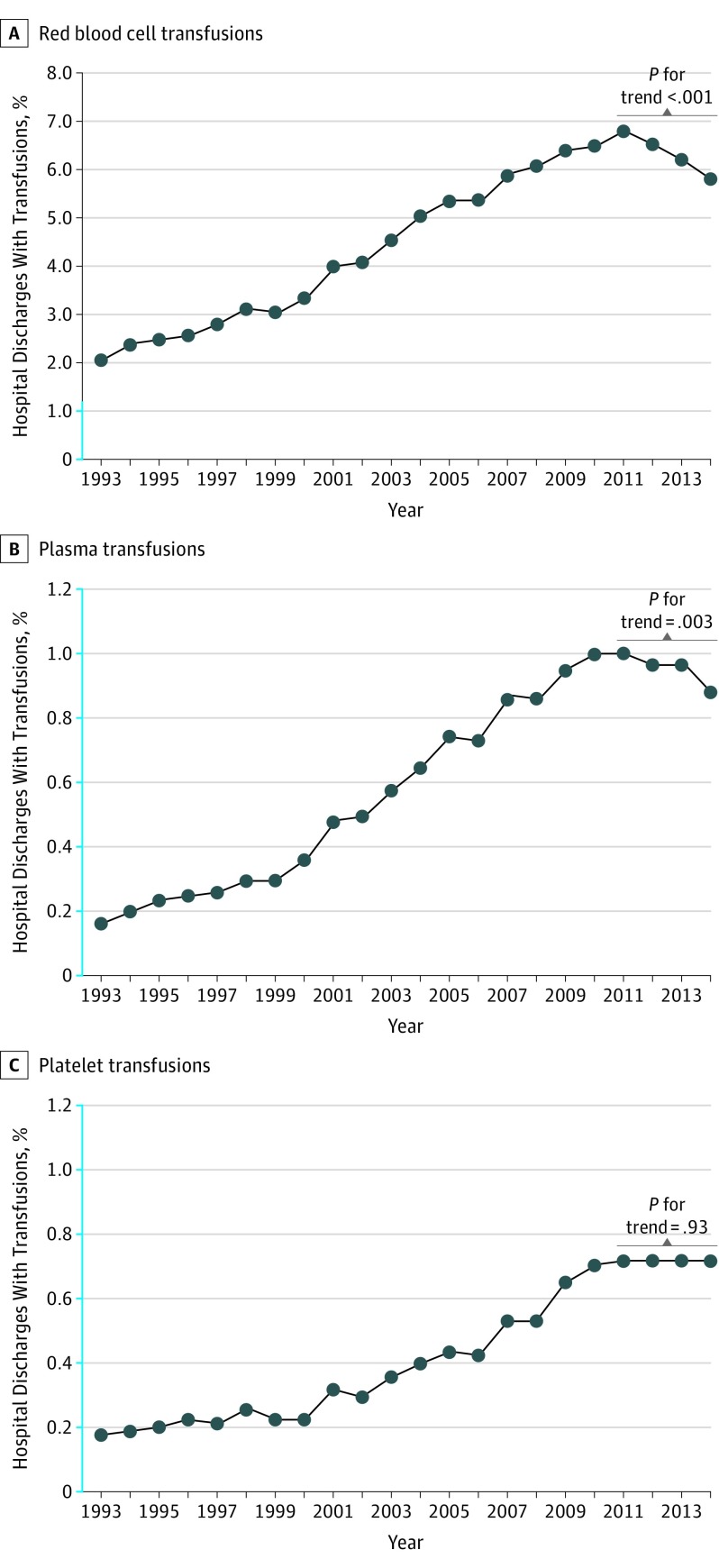
For RBC, platelet, and plasma transfusions, the proportion of patients transfused during a hospitalization increased from 1993 to 2011 (Figure).
Figure. Temporal Trends in Red Blood Cell, Plasma, and Platelet Transfusions Among US Hospitalizations, 1993-2014.
The y-axis scale shown in blue indicates range from 0% to 1.2%. The graphs represent the proportion of discharges transfused with a given blood component each year. The data represent weighted estimates for 33 million to 38 million discharges each year in the National Inpatient Sample (1993-2014). The P values for trend shown were calculated by the Cochran-Armitage test for linear trend in transfusion from 2011 through 2014.
RBC transfusions decreased from 6.8% (95% CI, 6.4%-7.2%) in 2011 to 5.7% (95% CI, 5.6%-5.9%) in 2014 (aRR, 0.83 [95% CI, 0.78-0.88]). Plasma transfusions decreased from 1.0% (95% CI, 0.93%-1.1%) in 2011 to 0.87% (95% CI, 0.83%-0.91%) in 2014 (aRR, 0.87 [95% CI, 0.80-0.95]). Platelet transfusions remained stable between 2011 and 2014 (aRR, 0.99 [95% CI, 0.89-1.10]).
From 2011 to 2014, statistically significant reductions in RBC transfusions were seen among all sexes, race/ethnicities, patient risk severities, payer types, and admission types (Table). No statistically significant reductions in RBC transfusions were seen in children (aged <18 years) or private investor–owned hospitals. Significant interactions were observed for time and all covariates (P for interaction < .05). A significantly greater decrease in RBC transfusions was seen for elective admissions (aRR, 0.74 [95% CI, 0.67-0.80]) compared with nonelective admissions (aRR, 0.86 [95% CI, 0.81-0.91]; P for interaction < .001).
Table. Change in RBC Transfusions From 2011 to 2014 Stratified by Patient-Level and Hospital-Level Characteristics.
| Characteristic | Sample Size, No.a | RBC Transfusion | P for Interaction | |||
|---|---|---|---|---|---|---|
| 2011 | 2014 | 2011, % | 2014, % | aRR (95% CI)b | ||
| Sex | <.001 | |||||
| Male | 15 503 375 | 15 095 708 | 6.8 | 5.9 | 0.84 (0.79-0.90)c | |
| Female | 21 386 074 | 20 255 555 | 6.8 | 5.6 | 0.82 (0.78-0.88)c | |
| Age, y | .002 | |||||
| <18 | 5 460 644 | 5 595 114 | 1.3 | 1.4 | 1.02 (0.88-1.19) | |
| 18-44 | 9 009 023 | 8 714 895 | 3.3 | 3.0 | 0.87 (0.81-0.94)c | |
| 45-64 | 9 283 947 | 8 709 298 | 7.6 | 6.5 | 0.82 (0.77-0.88)c | |
| ≥65 | 13 179 551 | 12 327 770 | 10.9 | 9.1 | 0.82 (0.77-0.87)c | |
| Raced | .046 | |||||
| White | 21 977 732 | 21 914 442 | 7.1 | 5.7 | 0.81 (0.76-0.86)c | |
| African American | 4 989 477 | 4 944 337 | 8.2 | 7.3 | 0.88 (0.81-0.96)e | |
| Hispanic | 4 160 276 | 4 038 136 | 5.5 | 5.0 | 0.88 (0.80-0.97)e | |
| Asian or Pacific Islander | 804 366 | 962 795 | 7.1 | 5.8 | 0.82 (0.74-0.91)c | |
| Other | 1 334 951 | 1 401 104 | 5.4 | 5.3 | 0.92 (0.83-1.02) | |
| APR-DRG risk severity subclassf | .01 | |||||
| 1 | 12 076 672 | 11 575 197 | 1.7 | 1.4 | 0.79 (0.74-0.84)c | |
| 2 | 13 210 349 | 13 025 518 | 4.9 | 4.2 | 0.80 (0.75-0.85)c | |
| 3 | 8 844 474 | 8 380 167 | 11.5 | 10.0 | 0.82 (0.77-0.88)c | |
| 4 | 2 784 963 | 2 348 271 | 23.2 | 20.3 | 0.82 (0.77-0.88)c | |
| Primary payer | .002 | |||||
| Medicaid | 7 299 408 | 7 993 545 | 3.9 | 3.6 | 0.89 (0.83-0.95)c | |
| Medicare | 14 620 864 | 13 795 116 | 10.4 | 8.7 | 0.83 (0.78-0.88)c | |
| Private | 11 742 140 | 10 833 048 | 4.7 | 3.9 | 0.81 (0.75-0.86)c | |
| Self-pay | 1 801 403 | 1 513 071 | 4.7 | 4.1 | 0.87 (0.80-0.95)e | |
| No charge | 181 286 | 137 390 | 5.9 | 4.7 | 0.85 (0.75-0.97)g | |
| Admission type | <.001 | |||||
| Nonelective | 28 165 369 | 27 540 471 | 6.9 | 6.0 | 0.86 (0.81-0.91)c | |
| Elective | 8 605 628 | 7 701 297 | 6.6 | 4.8 | 0.74 (0.67-0.80)c | |
| Hospital controlh | .01 | |||||
| Government, nonfederal | 3 901 967 | 4 310 458 | 6.5 | 5.6 | 0.85 (0.75-0.98)g | |
| Private, nonprofit | 27 407 405 | 25 831 562 | 6.9 | 5.7 | 0.80 (0.75-0.86)c | |
| Private, investor-owned | 5 144 700 | 5 216 798 | 6.6 | 6.2 | 0.98 (0.85-1.12) | |
Abbreviation: APR-DRG, All Patient Refined Diagnosis Related Groups; aRR, adjusted risk-ratio; RBC, red blood cell.
The overall weighted sample size was 36 962 415 for 2011 and 35 358 818 for 2014. The sample sizes shown for each covariate may not sum to the overall sample size due to a complete-case analytic approach.
The multivariable model was adjusted for factors shown to have an association with transfusion between 2011-2014 in univariate analysis (sex, age group, race, APR-DRG risk severity, primary payer, transfer status, elective admission, length of stay, number of diagnoses, number of procedures, hospital bed size, hospital teaching status and location, hospital region, hospital control). There was no multicollinearity observed in the multivariable models.
P ≤ .001.
The race categories were predefined by the Healthcare Cost and Utilization Project (HCUP) and included race and ethnicity in one data element. If the source supplied race and ethnicity in separate data elements, ethnicity took precedence over race in setting the HCUP value for race.
P ≤ .01.
APR-DRG severity of illness subclass: 0, no class specified; 1, minor loss of function (includes cases with no comorbidity or complications); 2, moderate loss of function; 3, major loss of function; 4, extreme loss of function. There were 45 957 patients with an unknown APR-DRG in 2011 and 29 665 in 2014. APR-DRG subclasses 1 and 2 were considered low risk and subclass 3 and 4 were considered high risk.
P ≤ .05.
The hospital's ownership and control category were obtained from the American Hospital Association Annual Survey of Hospitals and included categories for government nonfederal (public), private nonprofit (voluntary), and private investor–owned (proprietary).
Discussion
The observed decreases in RBC and plasma transfusions from 2011 to 2014 may reflect evidence demonstrating the safety of restricting RBC transfusions, patient blood management programs, conservation initiatives (eg, cell salvage, pharmacotherapy, improved surgical techniques), advocacy from medical organizations, and publication of transfusion guidelines. No decrease in RBC transfusion was seen in children or platelet transfusion overall, areas for which there is limited evidence to guide clinical practice.
This study has limitations inherent to any retrospective analysis of administrative data. The ICD-9-CM coding is carried out primarily for billing purposes and it is not possible to verify its accuracy, but National Inpatient Sample coding has been validated in other studies. The laboratory data supporting indication for transfusion was unknown. This study was also limited to inpatient transfusions, which might not be generalizable to outpatient settings. Except for the a priori hypothesis for admission type, subgroup analyses were not prespecified and significant interactions should be considered exploratory and tentative.
These data confirm and build upon previous descriptive studies. A statistical brief suggested RBC transfusions may be declining in the United States, but this study excluded children and did not examine trends in plasma or platelet transfusion. Preliminary data by the AABB (formerly the American Association of Blood Banks) and the US Centers for Disease Control and Prevention that focused on number of units of blood collected also suggested a decrease in the total number of RBC units transfused that may have begun as early as 2008. However, in this study the percentage of hospitalized patients receiving RBC transfusions did not decrease until 2011.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Carson JL, Guyatt G, Heddle NM, et al. Clinical practice guidelines from the AABB. JAMA. 2016;316(19):2025-2035. [DOI] [PubMed] [Google Scholar]
- 2.West KA, Barrett ML, Moore BJ, Miller JL, Steiner CA. Trends in Hospitalizations With a Red Blood Cell Transfusion, 2000-2013. Rockville, MD: Statistical Briefs; 2006. [PubMed] [Google Scholar]
- 3.Kaufman RM, Djulbegovic B, Gernsheimer T, et al. ; AABB . Platelet transfusion. Ann Intern Med. 2015;162(3):205-213. [DOI] [PubMed] [Google Scholar]
- 4.Whitaker B, Rajbhandary S, Kleinman S, Harris A, Kamani N. Trends in United States blood collection and transfusion. Transfusion. 2016;56(9):2173-2183. [DOI] [PubMed] [Google Scholar]
- 5.Chung KW, Basavaraju SV, Mu Y, et al. Declining blood collection and utilization in the United States. Transfusion. 2016;56(9):2184-2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ellingson KD, Sapiano MRP, Haass KA, et al. Continued decline in blood collection and transfusion in the United States—2015. Transfusion. 2017;57(suppl 2):1588-1598. [DOI] [PMC free article] [PubMed] [Google Scholar]