Key Points
Question
Does ground emergency medical services transport confer a survival advantage vs private vehicle transport for patients with penetrating injuries?
Findings
In this cohort study of 103 029 patients included in the National Trauma Data Bank, individuals transported by private vehicle were significantly less likely to die than similarly injured patients transported by ground emergency medical services, even when controlling for injury severity.
Meaning
Ground emergency medical services transport is not associated with improved survival compared with private vehicle transport among patients with penetrating injuries in urban trauma systems, suggesting prehospital trauma care may have a limited role in this subset of patients.
Abstract
Importance
Time to definitive care following injury is important to the outcomes of trauma patients. Prehospital trauma care is provided based on policies developed by individual trauma systems and is an important component of the care of injured patients. Given a paucity of systems-level trauma research, considerable variability exists in prehospital care policies across trauma systems, potentially affecting patient outcomes.
Objective
To evaluate whether private vehicle prehospital transport confers a survival advantage vs ground emergency medical services (EMS) transport following penetrating injuries in urban trauma systems.
Design, Setting, and Participants
Retrospective cohort study of data included in the National Trauma Data Bank from January 1, 2010, through December 31, 2012, comprising 298 level 1 and level 2 trauma centers that contribute data to the National Trauma Data Bank that are located within the 100 most populous metropolitan areas in the United States. Of 2 329 446 patients assessed for eligibility, 103 029 were included in this study. All patients were 16 years or older, had a gunshot wound or stab wound, and were transported by ground EMS or private vehicle.
Main Outcome and Measure
In-hospital mortality.
Results
Of the 2 329 446 records assessed for eligibility, 103 029 individuals at 298 urban level 1 and level 2 trauma centers were included in the analysis. The study population was predominantly male (87.6%), with a mean age of 32.3 years. Among those included, 47.9% were black, 26.3% were white, and 18.4% were Hispanic. Following risk adjustment, individuals with penetrating injuries transported by private vehicle were less likely to die than patients transported by ground EMS (odds ratio [OR], 0.38; 95% CI, 0.31-0.47). This association remained statistically significant on stratified analysis of the gunshot wound (OR, 0.45; 95% CI, 0.36-0.56) and stab wound (OR, 0.32; 95% CI, 0.20-0.52) subgroups.
Conclusions and Relevance
Private vehicle transport is associated with a significantly lower likelihood of death when compared with ground EMS transport for individuals with gunshot wounds and stab wounds in urban US trauma systems. System-level evidence such as this can be a valuable tool for those responsible for developing and implementing policies at the trauma system level.
This study evaluates whether private vehicle prehospital transport confers a survival advantage vs ground emergency medical services transport following penetrating injuries in urban trauma systems.
Introduction
The time immediately following injury can be vitally important to the clinical outcomes of severely injured trauma patients. The term the golden hour is commonly used to emphasize the importance of time in trauma care. Trauma systems are developed at the local, state, or regional level to optimize the delivery of care to seriously injured patients and are associated with increased survival after injury. Although the focal points of trauma systems are specialized trauma centers, the prehospital care provided to injured patients prior to arriving at trauma centers is important because this care has implications on clinical outcomes. Prehospital care policies are typically established at the trauma system level. In accordance with these policies, first responders must determine what, if any, interventions should be performed prior to and during transport to the hospital. To our knowledge, most of the previous research into optimal prehospital trauma care policies has not evaluated their effects at a system level, limiting the generalizability of their findings and resulting in persistent variability in prehospital protocols and procedures across trauma systems.
The spectrum of prehospital care provided to injured patients ranges from no intervention to advanced life support, fluid resuscitation, and endotracheal intubation with mechanical ventilation. Although optimal prehospital care strategies following injury remain undefined, within the last 2 years, several major national initiatives have aimed to improve early bystander and first responder response to injury, including the Stop the Bleed campaign based primarily on the Hartford Consensus. Training of the lay public in hemorrhage control has also become increasingly common in urban areas with high levels of violence.
Private vehicle transportation to a trauma center represents perhaps the most basic form of prehospital care, where no intervention is performed and only transportation is provided. In essence, private vehicle transport is a pure example of the “scoop and run” approach to prehospital trauma care. In patients with penetrating injures where time to definitive treatment is paramount, private vehicle transportation has been shown to be associated with improved survival when compared with transportation via ground emergency medical services (EMS). Although compelling, the results of this study are at the patient level and thus have been difficult to translate into trauma system–level policy. The objective of our study was to evaluate the association between the mode of transportation and mortality among individuals with penetrating injuries within urban trauma systems. We hypothesized that private vehicle transport is associated with a decreased mortality for penetrating injuries when compared with ground EMS transport.
Methods
The data source for this study was the American College of Surgeons National Trauma Databank (NTDB); the largest aggregation of US trauma registry data assembled. Data are entered into the NTDB by trained data abstractors, and the quality of the data is maintained through extensive statistical analyses and hospital audits performed by the American College of Surgeons Committee on Trauma. For this study, data from January 1, 2010, through December 31, 2012, were analyzed. Patients were included if they were aged 16 years or older, had a gunshot wound (GSW) or stab wound, were transported to the hospital by ground EMS or private vehicle, and were treated at a level 1 or level 2 trauma center. The design of this study is similar to previously published work comparing ground EMS and police department prehospital transport. Analyses were restricted to patients treated at trauma centers located within the 100 most populous US trauma systems to generate results capable of driving prehospital policy changes within large urban trauma systems. Cities were not used to define trauma systems because doing so would exclude trauma centers located outside a city’s limits that still provide trauma care to the city’s population. Patients were excluded if they had incomplete records for the primary outcome of in-hospital mortality or were transferred to or from another hospital.
Study participants were limited to individuals with GSWs or stab wounds because they represent a unique subpopulation of trauma patients most likely to benefit from timely surgical intervention and least likely to derive significant benefit from prehospital interventions. These mechanisms of injury were identified by International Classification of Diseases, Ninth Revision external causes of injury codes that are provided for each record in the NTDB. The 100 most populous US trauma systems were defined using 2010 US census information that ranks metropolitan areas based on Metropolitan Statistical Areas, an approach previously used in aggregating trauma centers into defined trauma systems. Metropolitan Statistical Areas are geographic areas containing a large population nucleus and adjacent communities with a high degree of integration with the population nucleus. Adult level 1 and level 2 trauma centers located within the most populous metropolitan areas were assigned to their respective trauma system. Institutional review board exemption was obtained from the Northwestern University Feinberg School of Medicine institutional review board. Individual patient consent was waived because all data used in this study were deidentified in the NTDB dataset prior to this study being conducted.
Baseline characteristics and unadjusted mortality rates between patients transported by ground EMS and those transported by private vehicle were compared using χ2 and t tests. Unadjusted mortality rates by mode of transport were compared between GSW and stab wound subgroups of the patient sample. The primary outcome of in-hospital mortality included deaths in the emergency department (ED) and all deaths occurring prior to hospital discharge. We considered excluding ED deaths from our analysis to determine the correlation of transport mode with survival of only salvageable patients. However, this approach could introduce selection bias. For example, it cannot be determined whether ED deaths within the private vehicle cohort were owing to lack of prehospital intervention or rapid transport of patients with nonsurvivable injuries who EMS may have pronounced dead at the scene. Excluding these patients could bias important mortality data among these patients to favor a lower mortality rate, when prehospital cardiac arrest may in fact occur at higher rates and result in more deaths among these patients. Similarly, ED deaths could potentially have occurred in EMS-transported patients who might have survived if they had been transported by private vehicle with a shorter delay to definitive care. Patients with a documented discharge disposition of hospice were also defined as in-hospital deaths, as has been previously described for risk-adjusted mortality calculations in trauma.
To evaluate the independent association between mode of prehospital transport and mortality, a general linear mixed-effects model accounting for hospital-level clustering was created. Consideration was given to using propensity score–matched cohorts, but this did not confer an advantage over multivariate modeling. Variables included in the risk adjustment for mortality were presenting heart rate, presenting systolic blood pressure, presenting Glasgow Coma Scale Motor Score, Injury Severity Score (ISS), age, sex, race/ethnicity, insurance status, and year of admission. Heart rate, systolic blood pressure, ISS, and age were treated as continuous variables, while sex, race/ethnicity, insurance status, and year of admission were categorical. Insurance status was categorized as private, governmental, self-pay, or other. Missing data for heart rate (n = 1624; 1.6%), systolic blood pressure(n = 2065; 2.0%), Glasgow Coma Scale Motor Score (n = 2119; 2.1%), ISS (n = 411; 0.4%), and sex (n = 18; 0.02%) were addressed using multiple imputation. Risk-adjusted mortality was assessed for all penetrating injuries as well as for the GSW and stab wound subgroups. Risk-adjusted mortality was also evaluated after stratifying by injury severity. Two stratified analyses were performed, 1 stratifying patients into ISS 15 or less and ISS greater than 15 categories and the other stratifying into mild (ISS ≤9), moderate (ISS, 9-15), severe (ISS, 16-24), and very severe (ISS ≥25) injury severity categories. To confirm the applicability of results to the top 100 most populous US trauma systems, sensitivity analyses were performed to evaluate risk-adjusted mortality across population strata. These strata included the most populous 10, 25, 50, and 75 systems, as well as the least populous 10, 25, 50, and 75 trauma systems within the 100 most populous US trauma systems (eTable in the Supplement). The results of this study were 2-sided and considered to be statistically significant at an α level of P < .05. SAS, version 9.4 (SAS Institute Inc), was used to perform all statistical analyses for this study.
Results
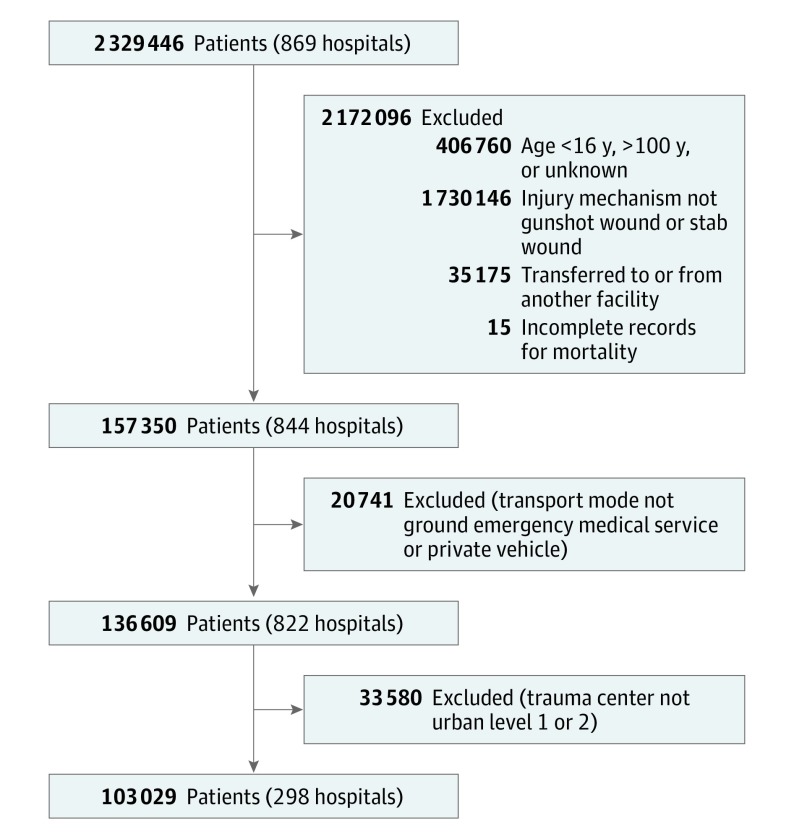
Of the 2 329 446 patients at 869 hospitals included in the NTDB from January 1, 2010, to December 31, 2012, a total of 103 029 patients at 298 hospitals were included in the study sample after applying the inclusion and exclusion criteria (Figure 1). Of the included patients, black and Hispanic patients were more frequently transported by private vehicle than by ground EMS (8545 [50.5%] vs 40 775 [47.4%] and 3472 [20.5%] vs 15 430 [17.9%], respectively), while white patients were more frequently transported by ground EMS than by private vehicle (23 420 [27.2%] vs 3663 [21.6%]). Patients with stab wounds were more likely to be transported by private vehicle than those with GSWs (9462 [55.9%] vs 7470 [44.1%], P < .001). The mean ISS was significantly lower for patients transported by private vehicle than those transported by ground EMS (5.5 vs 10.1, P < .001). Full demographic and injury information is provided in Table 1.
Figure 1. Consort Diagram Illustrating the Selection of Patients From the National Trauma Data Bank Between January 1, 2010, and December 31, 2012.
Table 1. Sample Population Characteristics by Mode of Prehospital Transportation.
| Characteristic | No. (%) | P Value | ||
|---|---|---|---|---|
| All Patients | Ground EMS | Private Vehicle | ||
| Population size | 103 029 (100) | 86 097 (83.6) | 16 932 (16.4) | |
| Sex | ||||
| Male | 90 259 (87.6) | 75 141 (87.3) | 15 118 (89.3) | <.001 |
| Female | 12 770 (12.4) | 10 956 (12.7) | 1814 (10.7) | |
| Age, y | ||||
| Mean (SD) | 32.3 (13.2) | 32.7 (13.4) | 30.4 (12.2) | <.001 |
| Median | 29.0 | 29.0 | 27.0 | <.001 |
| Race/ethnicity | ||||
| Black | 49 320 (47.9) | 40 775 (47.4) | 8545 (50.5) | <.001 |
| White | 27 083 (26.3) | 23 420 (27.2) | 3663 (21.6) | |
| Hispanic | 18 902 (18.4) | 15 430 (17.9) | 3472 (20.5) | |
| Asian | 1458 (1.4) | 1232 (1.4) | 226 (1.3) | |
| Other | 4437 (4.3) | 3725 (4.3) | 712 (4.2) | |
| Unknown | 1829 (1.8) | 1515 (1.8) | 314 (1.9) | |
| Insurance | ||||
| Private | 18 480 (17.9) | 15 111 (17.6) | 3369 (19.9) | <.001 |
| Governmental | 29 783 (28.9) | 25 496 (29.6) | 4287 (25.3) | |
| Self-pay | 37 765 (36.7) | 31 015 (36.0) | 6750 (39.9) | |
| Other | 8941 (8.7) | 7700 (8.9) | 1241 (7.3) | |
| Unknown | 8060 (7.8) | 6775 (7.9) | 1285 (7.6) | |
| Admission year | ||||
| 2010 | 34 259 (33.3) | 28 651 (33.3) | 5608 (33.1) | .85 |
| 2011 | 34 340 (33.3) | 28 665 (33.3) | 5675 (33.5) | |
| 2012 | 34 430 (33.4) | 28 781 (33.4) | 5649 (33.4) | |
| Injury mechanism | ||||
| GSW | 53 052 (51.5) | 45 582 (52.9) | 7470 (44.1) | <.001 |
| Stab wound | 49 977 (48.5) | 40 515 (47.1) | 9462 (55.9) | |
| HR, bpm | ||||
| Mean (SD) | 91.5 (30.2) | 90.6 (31.1) | 96.3 (24.6) | <.001 |
| Median | 94.0 | 94.0 | 96.0 | <.001 |
| SBP, mm Hg | ||||
| Mean (SD) | 125.3 (39.7) | 123.6 (41.2) | 134.0 (29.3) | <.001 |
| Median | 132.0 | 131.0 | 136.0 | <.001 |
| GCS motor scorea | <.001 | |||
| Mean (SD) | 5.4 (1.5) | 5.4 (1.6) | 5.9 (0.8) | <.001 |
| % GCS motor <6 | 14.1 | 15.9 | 5.9 | <.001 |
| ISSb | ||||
| Mean (SD) | 9.3 (12.0) | 10.1 (12.5) | 5.5 (7.8) | <.001 |
| Median | 5.0 | 8.0 | 2.0 | <.001 |
Abbreviations: EMS, emergency medical service; GCS, Glasgow Coma Scale; GSW, gunshot wound; HR, heart rate; ISS, Injury Severity Score; SBP, systolic blood pressure.
GCS motor scores range from 1 to 6, with 6 being normal.
ISS ranges from 0 to 75, with 75 being an injury resulting in death.
Overall, unadjusted mortality was lower for private vehicle transport than for ground EMS (378 [2.2%] vs 9986 [11.6%], P < .001). Among patients with GSWs, unadjusted mortality was significantly lower for those transported by private vehicle when compared with ground EMS (339 [4.5%] vs 18 807 [9.3%], P < .001). This difference was also found for the stab wound subgroup (39 [0.2%] vs 1179 [2.9%], P < .001). Private vehicle transport was associated with a lower unadjusted rate of death in the ED compared with ground EMS transport (1.2% vs 6.8%, P < .001). Unadjusted mortality rates are provided in Table 2.
Table 2. Unadjusted Overall Mortality for All Penetrating Injuries, GSWs, and Stab Wounds by Mode of Prehospital Transportation.
| Overall Mortality | No. (%) | P Value | ||
|---|---|---|---|---|
| All Patients | Ground EMS | Private Vehicle | ||
| All GSWs and stab wounds (n = 103 029) | 10 364 (10.1) | 9986 (11.6) | 378 (2.2) | <.001 |
| GSWs only (n = 53 052) | 9146 (17.2) | 8807 (19.3) | 339 (4.5) | <.001 |
| Stab wounds only (n = 49 977) | 1218 (2.4) | 1179 (2.9) | 39 (0.2) | <.001 |
Abbreviations: EMS, emergency medical service; GSW, gunshot wound.
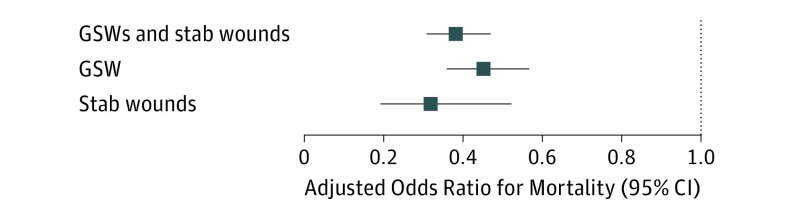
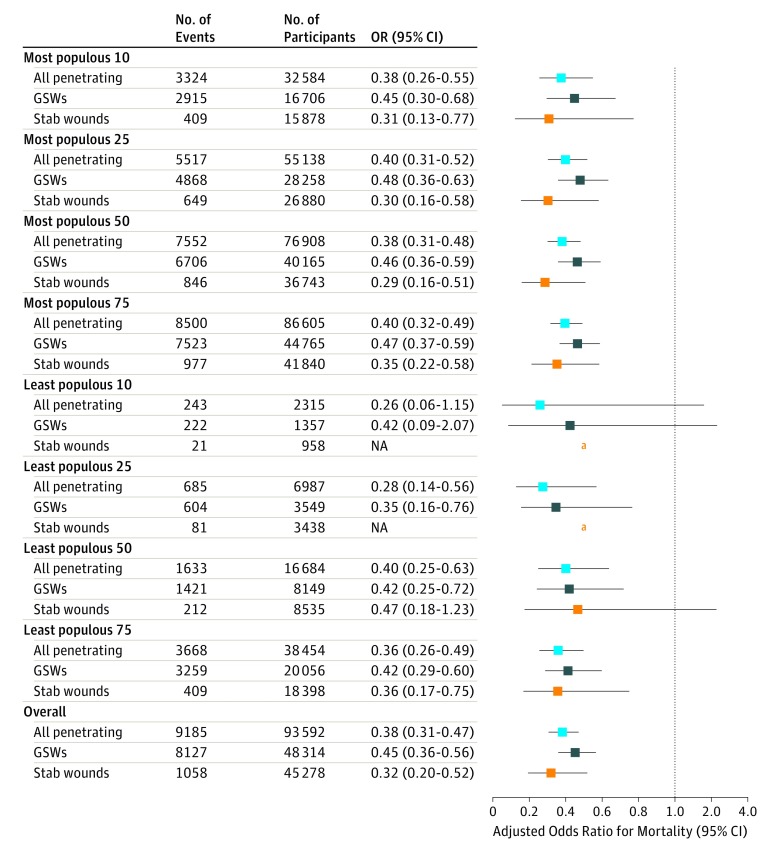
After risk adjustment, patients with penetrating injuries transported by private vehicle were significantly less likely to die than patients transported by ground EMS (OR, 0.38; 95% CI, 0.31-0.47) (Figure 2). This association remained statistically significant on stratified analysis of the GSW (OR, 0.45; 95% CI, 0.36-0.56) and stab wound (OR, 0.32; 95% CI, 0.20-0.52) subgroups (Figure 2). Stratified injury severity analyses demonstrated a qualitatively similar survival benefit associated with private vehicle transport when compared with ground EMS transport for all but the lowest injury severity strata. Sensitivity analyses revealed statistically significant mortality benefits for patients with penetrating injures transported by private vehicle when compared with ground EMS in 8 of 9 trauma system cohorts. Sensitivity analyses revealed the only group of trauma systems failing to demonstrate statistically significant risk-adjusted mortality differences was the 91 to 100 most populous trauma systems, where the sample size was too small to detect a significant difference (OR, 0.26; 95% CI, 0.06-1.15) (Figure 3).
Figure 2. Risk-Adjusted Odds Ratios for Mortality for Private Vehicle Transport When Compared With Ground Emergency Medical Services Transport .
GSW indicates gunshot wound.
Figure 3. Trauma System Subgroup Analyses of Risk-Adjusted Odds Ratios (ORs) for Mortality for Private Vehicle Transport When Compared With Ground Emergency Medical Services Transport.
GSW indicates gunshot wound; NA, not applicable.
Odds ratios cannot be derived due to small sample size.
Discussion
This study demonstrates that for individuals with penetrating injuries in urban trauma systems, private vehicle transport to a level 1 or level 2 trauma center is associated with significantly lower mortality when compared with similarly injured individuals who are transported by ground EMS. This mortality benefit holds true on subgroup analyses of the 100 most populous US trauma systems, making these findings generalizable at the trauma system level for the large urban trauma systems included in this study. These results are important because they identify a component of prehospital trauma care that is associated with significant differences in mortality and may present an opportunity to improve trauma care at the system level.
Previous research has demonstrated that variations in prehospital care can affect mortality among seriously injured patients, often in ways that may not be expected. For example, prehospital advanced life support care has been shown in multiple studies to be associated with higher mortality rates than basic life support when similarly injured patients are compared. Additionally, prehospital interventions, including endotracheal intubation, intravenous fluid administration, and spine immobilization, have been found to be associated with higher rates of mortality in certain groups of trauma patients. Previous work has also demonstrated outcome differences, or an absence of differences, based on mode of prehospital transportation including helicopter, ground EMS, police department transport, and private vehicle. These studies highlight the significance of prehospital trauma care and the effect that trauma system–level first responder policies can have on patient outcomes. However, these studies examine outcomes within single centers or aggregated at a national level, rather than the trauma system level, which has limited the ability to use the results to drive system-level policy change.
The results of this study confirm those that have been previously reported on mortality differences between ground EMS and private vehicle transport, but represent, to our knowledge, the first time the results have been analyzed on a trauma system level. Additionally, the results of this study were obtained through a larger patient sample that contained data through 2012, which is more recent than previous studies. The ability to use unblinded NTDB hospital identifiers to conduct system-level analyses that can inform trauma system policy is a major strength of this study and, to our knowledge, has never been published. Because trauma system policies are developed and implemented at the system level, it is important to provide system-level evidence to support the implementation of policies and protocols within each system. For example, consideration could be given to educating those at high risk for penetrating injury that individuals with these injuries may benefit from rapid private vehicle transport to the nearest level 1 trauma center instead of waiting for first responders to arrive. Furthermore, although EMS “scoop and run” policy was unable to be compared with EMS “stay and stabilize” policy in this analysis, these results suggest that a “scoop and run” policy for EMS may be beneficial given the similarities between private vehicle transport and “scoop and run” by EMS. Other strengths of this study include the large sample size and the consistently statistically significant results in nearly all strata, subgroups, and sensitivity analyses.
Limitations
This study is not without limitations. As with all large, multicenter database analyses, data quality is dependent on the accuracy of the data abstraction process and the amount of missing data. Although there are auditing mechanisms in place to identify errors in abstraction, errors cannot be entirely eliminated. Missing data were not a major factor in this analysis, but where they were present, the missing data were imputed. Another limitation of this study was the risk adjustment for mortality calculations, which was limited to the data available in the NTDB. As a result, it is likely that potential confounding risk factors for mortality were unable to be included in the risk-adjustment process. Specifically, prehospital transport time is one of the major confounders we were unable to include owing to the large amount of missing data. However, because patients transported by private vehicle do not wait for EMS to arrive and do not undergo any prehospital interventions, their prehospital times are unlikely to be longer than those transported by ground EMS. Differences in baseline characteristics between modes of transport, most notably mechanism of injury and injury severity, are also a limitation. Although patient randomization would optimally eliminate these differences, this was not (and realistically, will never be) feasible, and we accounted for these differences by adjusting for them in our mortality models. Furthermore, the results of this study only reflect the data from trauma centers that contribute to the NTDB. Although more than 800 centers contribute data to the NTDB each year, it is not a requirement for all US trauma centers, and thus, not all centers participate. Lastly, although the results of this study demonstrate a mortality benefit associated with private vehicle transport, such approaches may be associated with unintended consequences unable to be assessed by this study. Consequently, further study is necessary before private vehicle transport initiatives or “scoop and run” EMS transport policies can be definitively recommended for all urban gunshot and stab wound patients.
Conclusions
Private vehicle transport is associated with a significantly lower likelihood of death when compared with ground EMS transport for individuals with GSWs and stab wounds in urban US trauma systems. System-level data such as these can be a valuable tool for use in the development and implementation of policies at the trauma system level. The goal of trauma systems is to deliver optimal care to injured patients. An important part of accomplishing this is determining what constitutes optimal care in each trauma system because it may be different. The results of this study highlight the importance of system-level research and the need for additional such work to be conducted in the future.
eTable. Table of the 100 Most Populous Urban Trauma Systems
References:
- 1.Gervin AS, Fischer RP. The importance of prompt transport of salvage of patients with penetrating heart wounds. J Trauma. 1982;22(6):443-448. [DOI] [PubMed] [Google Scholar]
- 2.Feero S, Hedges JR, Simmons E, Irwin L. Does out-of-hospital EMS time affect trauma survival? Am J Emerg Med. 1995;13(2):133-135. [DOI] [PubMed] [Google Scholar]
- 3.Swaroop M, Straus DC, Agubuzu O, Esposito TJ, Schermer CR, Crandall ML. Pre-hospital transport times and survival for Hypotensive patients with penetrating thoracic trauma. J Emerg Trauma Shock. 2013;6(1):16-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.West JG, Trunkey DD, Lim RC. Systems of trauma care: a study of two counties. Arch Surg. 1979;114(4):455-460. [DOI] [PubMed] [Google Scholar]
- 5.Cales RH. Trauma mortality in Orange County: the effect of implementation of a regional trauma system. Ann Emerg Med. 1984;13(1):1-10. [DOI] [PubMed] [Google Scholar]
- 6.Esposito TJ, Sanddal TL, Reynolds SA, Sanddal ND. Effect of a voluntary trauma system on preventable death and inappropriate care in a rural state. J Trauma. 2003;54(4):663-669. [DOI] [PubMed] [Google Scholar]
- 7.Liberman M, Mulder D, Sampalis J. Advanced or basic life support for trauma: meta-analysis and critical review of the literature. J Trauma. 2000;49(4):584-599. [DOI] [PubMed] [Google Scholar]
- 8.Liberman M, Mulder D, Lavoie A, Denis R, Sampalis JS. Multicenter Canadian study of prehospital trauma care. Ann Surg. 2003;237(2):153-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bochicchio GV, Ilahi O, Joshi M, Bochicchio K, Scalea TM. Endotracheal intubation in the field does not improve outcome in trauma patients who present without an acutely lethal traumatic brain injury. J Trauma. 2003;54(2):307-311. [DOI] [PubMed] [Google Scholar]
- 10.Haut ER, Kalish BT, Efron DT, et al. Spine immobilization in penetrating trauma: more harm than good? J Trauma. 2010;68(1):115-120. [DOI] [PubMed] [Google Scholar]
- 11.Haut ER, Kalish BT, Cotton BA, et al. Prehospital intravenous fluid administration is associated with higher mortality in trauma patients: a National Trauma Data Bank analysis. Ann Surg. 2011;253(2):371-377. [DOI] [PubMed] [Google Scholar]
- 12.Zafar SN, Haider AH, Stevens KA, et al. Increased mortality associated with EMS transport of gunshot wound victims when compared to private vehicle transport. Injury. 2014;45(9):1320-1326. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs LM; Joint Committee to Create a National Policy to Enhance Survivability from Intentional Mass-Casualty and Active Shooter Events . The Hartford Consensus III: implementation of bleeding control: if you see something do something. Bull Am Coll Surg. 2015;100(1)(suppl):40-46. [PubMed] [Google Scholar]
- 14.Levy MJ, Jacobs LM. A call to action to develop programs for bystanders to control severe bleeding. JAMA Surg. 2016;151(12):1103-1104. [DOI] [PubMed] [Google Scholar]
- 15.Bui L. Trauma kits help police control severe bleeding, saving lives. The Washington Post https://www.washingtonpost.com/local/crime/trauma-kits-help-police-control-severe-bleeding-saving-lives/2015/01/26/a6d0dcde-8ade-11e4-8ff4-fb93129c9c8b_story.html?utm_term=.358fe789eedf Published 2015.
- 16.American College of Surgeons National Trauma Data Bank 2013 Annual Report. Chicago, IL: American College of Surgeons; 2013. [Google Scholar]
- 17.Wandling MW, Nathens AB, Shapiro MB, Haut ER. Police transport versus ground EMS: A trauma system-level evaluation of prehospital care policies and their effect on clinical outcomes. J Trauma Acute Care Surg. 2016;81(5):931-935. [DOI] [PubMed] [Google Scholar]
- 18.Bickell WH, Wall MJ Jr, Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994;331(17):1105-1109. [DOI] [PubMed] [Google Scholar]
- 19.Seamon MJ, Fisher CA, Gaughan J, et al. Prehospital procedures before emergency department thoracotomy: “scoop and run” saves lives. J Trauma. 2007;63(1):113-120. [DOI] [PubMed] [Google Scholar]
- 20.Smith JP, Bodai BI, Hill AS, Frey CF. Prehospital stabilization of critically injured patients: a failed concept. J Trauma. 1985;25(1):65-70. [DOI] [PubMed] [Google Scholar]
- 21.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366-378. [DOI] [PubMed] [Google Scholar]
- 22.Crandall MA, Bradley DJ, Packer DL, Asirvatham SJ. Contemporary management of atrial fibrillation: update on anticoagulation and invasive management strategies. Mayo Clin Proc. 2009;84(7):643-662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kozar RA, Holcomb JB, Xiong W, Nathens AB. Are all deaths recorded equally? the impact of hospice care on risk-adjusted mortality. J Trauma Acute Care Surg. 2014;76(3):634-639. [DOI] [PubMed] [Google Scholar]
- 24.Galvagno SM Jr, Haut ER, Zafar SN, et al. Association between helicopter vs ground emergency medical services and survival for adults with major trauma. JAMA. 2012;307(15):1602-1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hemmila MR, Birkmeyer NJ, Arbabi S, Osborne NH, Wahl WL, Dimick JB. Introduction to propensity scores: a case study on the comparative effectiveness of laparoscopic vs open appendectomy. Arch Surg. 2010;145(10):939-945. [DOI] [PubMed] [Google Scholar]
- 26.Haider AH, Hashmi ZG, Zafar SN, et al. Developing best practices to study trauma outcomes in large databases: an evidence-based approach to determine the best mortality risk adjustment model. J Trauma Acute Care Surg. 2014;76(4):1061-1069. [DOI] [PubMed] [Google Scholar]
- 27.Haider AH, Saleem T, Leow JJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? J Am Coll Surg. 2012;214(5):756-768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oyetunji TA, Crompton JG, Ehanire ID, et al. Multiple imputation in trauma disparity research. J Surg Res. 2011;165(1):e37-e41. [DOI] [PubMed] [Google Scholar]
- 29.Band RA, Pryor JP, Gaieski DF, Dickinson ET, Cummings D, Carr BG. Injury-adjusted mortality of patients transported by police following penetrating trauma. Acad Emerg Med. 2011;18(1):32-37. [DOI] [PubMed] [Google Scholar]
- 30.Band RA, Salhi RA, Holena DN, Powell E, Branas CC, Carr BG. Severity-adjusted mortality in trauma patients transported by police. Ann Emerg Med. 2014;63(5):608-614.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cornwell EE III, Belzberg H, Hennigan K, et al. Emergency medical services (EMS) vs non-EMS transport of critically injured patients: a prospective evaluation. Arch Surg. 2000;135(3):315-319. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Table of the 100 Most Populous Urban Trauma Systems