This study examines whether adolescent violent offending mediates the association between childhood adversity and suicide in early adulthood.
Key Points
Question
Does adolescent violent offending mediate the association between childhood adversity and early adulthood suicide?
Findings
In this population-based cohort study of 476 103 young adults, individuals with a history of childhood adversity who were convicted of violent offending had an 8-fold higher risk of suicide compared with those not convicted after adjusting for important background factors and psychiatric disorder. Adolescent violent offending partly mediated the association between childhood adversity and suicide.
Meaning
Interventions to prevent externalizing behavior during childhood and increased support to youths with delinquent behavior may have the potential to prevent suicide associated with childhood adversity.
Abstract
Importance
Childhood adversity (CA) is associated with an increased risk of suicide in young adulthood that might be explained by maladaptive trajectories during adolescence. Although adolescent violent offending is linked with suicide, little is known about its role in the association between CA and suicide.
Objective
To examine whether adolescent violent offending mediates the association between CA and suicide in early adulthood.
Design, Setting, and Participants
This population-based, longitudinal cohort study with a follow-up time spanning 5 to 9 years included 476 103 individuals born in Sweden between 1984 and 1988. The study population was prospectively followed up from 20 years of age until December 31, 2013, with respect to suicide. Data analysis was performed from January 1, 1984, to December 31, 2013.
Exposures
Register-based CAs included parental death, parental substance abuse and psychiatric disorder, parental criminal offending, parental separation, public assistance recipiency, child welfare intervention, and residential instability. Adolescent violent offending was defined as being convicted of a violent crime between the ages of 15 and 19 years.
Main Outcomes and Measures
Estimates of risk of suicide after 20 years of age (from 2004 if born in 1984 and from 2008 if born in 1988) until the end of 2013 were calculated as incidence rate ratios (IRRs) with 95% CIs using Poisson regression analysis. Adjustments were made for demographics and psychiatric disorder. In addition, binary mediation analysis with logistic regression was used.
Results
A total of 476 103 individuals (231 699 [48.7%] female) were included in the study. Those with a conviction for violent offending had been exposed to all CAs to a greater extent than those with no violent offending. Cumulative CA was associated with risk of suicide in nonconvicted (adjusted IRR, 2.4; 95% CI, 1.5-3.9) and convicted youths, who had a higher risk of suicide (adjusted IRR, 8.5; 95% CI, 4.6-15.7). Adolescent violent offending partly mediated the association between CA and suicide.
Conclusions and Relevance
Individuals with a history of CA who also engage in violent offending in adolescence have a high risk of suicide. Interventions to prevent externalizing behavior during childhood and increased support to youths with delinquent behavior may have the potential to prevent suicide related to CA.
Introduction
Despite the overall decrease in suicide rates in most Western countries during recent decades, no similar decrease has been observed among adolescents and young adults. In fact, suicide is ranked as one of the leading causes of death among those aged 15 to 29 years, and in the United States, suicide in young people is increasing.
Identification of risk factors for suicide early during the life course has important implications for designing effective public health interventions. Previous studies have indicated that childhood adversities (CAs) are particularly detrimental because of their association with suicide. Usually, CA is denoted by a range of indicators, such as parental divorce, death in the family, substance abuse and criminality in the home, poverty, residential instability, and parental psychopathologic disorders.
Among different mechanisms through which exposure to CA may be associated with later suicide risk, adolescent criminal offending has been suggested as one pathway. Certain maladaptive behavioral patterns, such as childhood aggression and impulsivity, that are more prevalent among young suicide attempters and young individuals with delinquent behavior may also be more prevalent among those who have experienced CA. Subsequently, studies have found significantly higher prevalence rates of CA among young individuals with delinquent behavior, particularly those engaged in violent offending.
The association between adolescent offending and later risk of attempted and completed suicide is well established, and the risk is higher among those engaged in violent offending. The association appears to be 2-way, with self-harm also predicting violent offending.
Some studies have placed adolescent violent offending as a possible link between cumulative CA and later suicidal behavior. These studies have focused on the mediating effect of factors related to violent behavior, such as personality traits, and none of them concerned completed suicides or were population-based. The current register-based study used a large cohort of approximately 476 000 individuals born in Sweden between 1984 and 1988 to test the following hypotheses: (1) exposure to cumulative CA and adolescent violent offending is associated with high risk of suicide in young adulthood and (2) the association between cumulative CA and suicide is mediated by adolescent violent offending.
Methods
Study Population
The study population was defined as all individuals born in Sweden between 1984 and 1988 (n = 503 851) as recorded in the Medical Birth Register. This register contains data on all births in Sweden since 1973. Owing to a high proportion of missing data, those who were adopted (n = 330) and those who emigrated before 20 years of age (n = 11 954) were excluded. We also excluded those who died before their 20th birthday (n = 4809) because we did not have information on violent offending for these individuals. Those who were granted a disability pension before 23 years of age were also excluded (n = 10 269, mainly persons with severe learning disabilities or multiple disabilities). Finally, we excluded 386 individuals for whom we lacked parental information. Our final analytical sample included 476 103 individuals. The study population was prospectively followed up from 20 years of age until December 31, 2013, with respect to suicide. Data analysis was performed from January 1, 1984, to December 31, 2013. The unique Swedish personal identity number was used to link this cohort to multiple health care and administrative registers (eTable 1 in the Supplement). This study was approved by the ethical review board of Stockholm, Sweden. In accordance with the Swedish Personal Data Act of 1998 (www.datainspektionen.se/in-english/legislation/the-personal-data-act/) and the decision of the ethical review board, we did not obtain informed consent from the study participants. All study data were anonymized.
Measures
Indicators of CA
The CA indicators (Table 1) were selected based on prior research demonstrating that they had significant adverse health and social implications. We included 8 CAs that occurred between birth and 14 years of age: parental death, parental substance abuse, substantial parental criminal offending, parental psychiatric disorder, parental separation, public assistance recipiency, substantial child welfare intervention before 12 years of age (out-of-home care), and residential instability. To assess cumulative exposure to the studied CAs, the total number of CAs was summed and grouped into 0, 1, 2, 3, and 4 or more CAs. Each indicator was weighted equivalently in the analyses.
Table 1. Definitions and Classification of Childhood Adversity.
| Childhood Adversity | Definition | ICD Classification | Data Source |
|---|---|---|---|
| Parental death | Parental death | NA | Causes of Death Register |
| Parental suicide | Parental suicide |
ICD-9: 950-59, 980-89; ICD-10: X60-84, Y10-34 |
Causes of Death Register |
| Parental substance abuse | At least 1 hospitalization for alcohol and/or narcotic-related substance abuse |
ICD-9: 291, 303, 304.0-304.9, 305.0, 305.2-305.7, 305.9; ICD-10: F10-F19 |
National Patient Register |
| Substantial parental criminal offending | At least 1 parent sentenced to prison, probation, or forensic psychiatric care | NA | Register of Court Convictions |
| Parental psychiatric disorder | At least 1 hospitalization for psychiatric disorder (excluding substance abuse–related disorders) | ICD-9: 290-319; ICD-10: F00-F99 | National Patient Register |
| Parental separation | Having separated parents | NA | Longitudinal Integration Database for Health Insurance and Labor Market Studies |
| Household living on public assistance | Public assistance during at least 1 y, when >50% of the yearly income constituted public assistance | NA | Total Enumeration Income Survey |
| Substantial child welfare intervention | At least 1 placement in out-of-home care before age 12 y | NA | Child Welfare Register |
| Residential instability | ≥3 Changes in place of residence | NA | Total Population Register |
Abbreviations: ICD-9, International Classification of Diseases, Ninth Revision; ICD-10, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; NA, not applicable.
Adolescent Violent Offending
In contrast to many other European countries, Sweden has few individuals younger than 18 years in prison, even though the age of criminal responsibility is 15 years. The political consensus in Sweden has, during several decades, agreed on keeping offending youths out of prisons to avoid the risk of becoming apprentices in crime. Thus, the standard procedure for courts is to give cases of youths suspected of delinquency to the social services without any other legal sanctions imposed on the individual offender.
We retrieved all conviction data for violent crimes between the ages of 15 and 19 years from the Register of Court Convictions. Violent crime was defined as homicide, assault, robbery, arson, any sexual offense (rape, sexual coercion, child molestation, indecent exposure, or sexual harassment), illegal threats, or intimidation (burglary and other property offenses and drug offenses were excluded).
Suicide
The study population was prospectively followed up from 20 years of age until December 31, 2013, with respect to suicide. Suicide was defined by the presence of International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes X60 to X84 or as death with undetermined intent (codes Y10-Y34) as the underlying cause of death in the causes of death register. The latter reduces spatial and secular trends in detecting and classifying cases of suicide when intent was indeterminable.
Confounders
Several confounding factors related to parental demographic and socioeconomic circumstances were included. Parental country of birth was categorized as Sweden (both parents Swedish-born), mixed (one Swedish-born), other Nordic (Denmark, Finland, Norway, or Iceland), other European Union, and non–European Union. Highest parental educational attainment, measured when the child was 15 years of age, was classified as compulsory school (≤9 years), secondary school (10-12 years), and university or college (>12 years).
Early psychiatric disorder, including substance abuse, self-harm, and antisocial behavior, is associated with adolescent criminal offending and suicide. Psychiatric disorder up until 20 years of age was obtained from the National Patient Register.
Statistical Analysis
Statistical analyses were conducted using SAS, version 9.4 (SAS Institute Inc) and Stata, version 13 (StataCorp). Multivariate analyses were performed using Poisson regression models of time to suicide. We assessed person-years at risk by totaling the years that the individuals were living in Sweden during the follow-up period (entry date defined as the date of the 20th birthday and exit date as the date of suicide, date of death from other causes, date of emigration, or the end of follow-up [December 31, 2013]). We examined the association between indicators of CA and suicide in adulthood in 4 regression models. Model 1 was adjusted for sex and birth year. Model 2 was further adjusted for parental country of birth and parental educational level. In model 3, psychiatric disorder before 20 years of age was included. In model 4, all CAs were included simultaneously.
To establish whether violent offending mediates the association between CA and suicide, a series of regression analyses were performed as suggested by Baron and Kenny. We first regressed the hypothesized mediator (violent offending) on the independent variable (ie, cumulative CA). Second, the dependent variable (ie, suicide) was regressed on the independent variable. Third, the dependent variable was regressed on the independent variable and the hypothesized mediator. Separate coefficients for each equation were estimated, and mediation was considered to occur if the association between the independent and dependent variables could be partially or totally accounted for by the hypothesized mediator and if significant indirect effects were demonstrated. We assessed the statistical significance of the mediation effect using the binary mediation command in Stata. The binary mediation command computes the indirect effect of a mediating variable using standardized coefficients. The CI and statistical test of significance for the proportion mediated were estimated using bootstrapping with 5000 replications. Because self-harm was associated with suicide and violent behavior, we performed sensitivity analyses in which we stratified the cohort based on history of care for self-harm and repeated the analyses.
Results
A total of 476 103 individuals (231 699 [48.7%] female) were included in the study. Cohort characteristics of the study population, by sex and exposure to adolescent violent offending, are presented in Table 2. A total of 146 820 (30.8%) were exposed to at least 1 CA. The most prevalent CAs were parental separation (114 432 [24.0%]) and parental psychiatric disorder (24 212 [5.1%]). eTable 2 in the Supplement gives the number of individuals who had experienced the 8 different CAs and a combination thereof. Among female participants, 1616 (0.7%) had been convicted of violent offending between the ages of 15 and 19 years. The corresponding number for male participants was 7533 (3.1%). It was more common among convicted individuals to have parents born outside Sweden and to have parents with lower levels of education. Individuals exposed to CA were more likely to be convicted of violent offending during adolescence in multivariate models (eTable 3 in the Supplement). During the follow-up, 623 individuals (0.1%) died by suicide (149 [23.9%] were classified as undetermined intent).
Table 2. Cohort Characteristics and Prevalence of Childhood Adversity by Sex and Exposure to Adolescent Violent Offending.
| Variable | Women, No. (%) | Men, No. (%) | Total, No. (%) | |||
|---|---|---|---|---|---|---|
| Total (n = 231 699) |
Violent Conviction (n = 1616) |
Total (n = 244 404) |
Violent Conviction (n = 7533) |
Total (N = 476 103) |
Violent Conviction (n = 9149) |
|
| Characteristics | ||||||
| Parental educational level (years of education) | ||||||
| 9 | 15 787 (6.8) | 243 (15.0) | 16 354 (6.7) | 1070 (14.2) | 32 141 (6.8) | 1313 (14.4) |
| 10-12 | 115 297 (49.8) | 1046 (64.7) | 121 718 (49.8) | 4836 (64.2) | 237 015 (49.8) | 5882 (64.3) |
| >12 | 99 009 (42.7) | 320 (19.8) | 104 625 (42.8) | 1603 (21.3) | 203 634 (42.8) | 1923 (21.0) |
| Missing | 1606 (0.7) | 7 (0.4) | 1707 (0.7) | 24 (0.3) | 3313 (0.7) | 31 (0.3) |
| Parental country of birth | ||||||
| Both born in Sweden | 192 985 (83.3) | 1202 (74.4) | 203 456 (83.2) | 5322 (70.6) | 396 441 (83.3) | 6524 (71.3) |
| Mixed | 24 131 (10.4) | 262 (16.2) | 25 483 (10.4) | 1174 (15.6) | 49 614 (10.4) | 1436 (15.7) |
| Other Nordica | 4639 (2.0) | 60 (3.7) | 5098 (2.1) | 260 (3.5) | 9737 (2.0) | 320 (3.5) |
| European Union | 3364 (1.5) | 26 (1.6) | 3517 (1.4) | 196 (2.6) | 6881 (1.4) | 222 (2.4) |
| Non–European Union | 6580 (2.8) | 66 (4.1) | 6850 (2.8) | 581 (7.7) | 13 430 (2.8) | 647 (7.1) |
| Indicators of childhood adversity | ||||||
| Parental death | 5332 (2.3) | 87 (5.4) | 5733 (2.3) | 309 (4.1) | 11 065 (2.3) | 396 (4.3) |
| Parental suicide | 1074 (0.5) | 22 (1.4) | 1175 (0.5) | 80 (1.1) | 2249 (0.5) | 102 (1.1) |
| Parental substance abuse | 7010 (3.0) | 183 (11.3) | 7347 (3.0) | 736 (9.8) | 14 357 (3.0) | 919 (10.0) |
| Substantial parental criminality | 9561 (4.1) | 271 (16.8) | 10 115 (4.1) | 1154 (15.3) | 19 676 (4.1) | 1425 (15.6) |
| Parental psychiatric disorder | 11 746 (5.1) | 191 (11.8) | 12 466 (5.1) | 806 (10.7) | 24 212 (4.5) | 997 (10.9) |
| Parental separation | 56 169 (24.2) | 802 (49.6) | 58 263 (23.8) | 3221 (42.8) | 114 432 (24.0) | 4023 (44.0) |
| Public assistance recipiency | 10 234 (4.4) | 304 (18.8) | 10 710 (4.4) | 1307 (17.4) | 20 944 (4.4) | 1611 (17.6) |
| Child welfare intervention | 2995 (1.1) | 129 (8.0) | 3447 (1.4) | 499 (6.6) | 6442 (1.4) | 628 (6.9) |
| Residential instability | 3082 (1.3) | 82 (5.1) | 3016 (1.2) | 294 (3.9) | 6098 (1.3) | 376 (4.1) |
| No. of indicators of childhood adversity | ||||||
| 0 | 159 794 (69.0) | 561 (34.7) | 169 489 (69.3) | 3142 (41.7) | 329 283 (69.2) | 3703 (40.5) |
| 1 | 49 850 (21.5) | 530 (32.8) | 51 720 (21.2) | 2441 (32.4) | 101 570 (21.3) | 2971 (32.5) |
| 2 | 14 289 (6.2) | 247 (15.3) | 14 878 (6.1) | 1088 (14.4) | 29 167 (6.1) | 1335 (14.6) |
| 3 | 4747 (2.0) | 152 (9.4) | 5132 (2.1) | 571 (7.6) | 9879 (2.1) | 723 (7.9) |
| ≥4 | 3019 (1.1) | 126 (7.8) | 3185 (1.3) | 491 (6.5) | 6204 (1.3) | 617 (6.7) |
| Suicide from age 20 y | 155 (0.1) | 7 (0.4) | 468 (0.2) | 74 (0.1) | 623 (0.1) | 81 (0.9) |
Denmark, Finland, Norway, and Iceland.
Table 3 presents the crude and multiadjusted incidence rate ratios (IRRs) with 95% CIs for suicide by adolescent violent offending and exposure to CAs. In the absence of adolescent violent offending, CAs except for parental death, residential instability, and childhood welfare intervention were associated with risk of suicide (parental death: IRR, 1.0; 95% CI, 0.6-1.7; parental substance abuse: IRR, 2.6; 95% CI, 2.0-3.5; parental criminality: IRR, 1.7; 95% CI, 1.3-2.3; parental psychiatric disorder: IRR, 1.5; 95% CI, 1.2-2.1; parental separation: IRR, 1.3; 95% CI, 1.1-1.6; public assistance: IRR, 2.1; 95% CI, 1.6-2.8; child welfare intervention: IRR, 1.5; 95% CI, 0.9-2.4; and residential instability: IRR, 0.6; 95% CI, 0.3-1.5) (Table 3). All CAs entailed a high risk of suicide among individuals who were convicted for violent offending in adolescence (parental death: IRR, 5.6; 95% CI, 2.6-11.9; parental substance abuse: IRR, 6.8; 95% CI, 4.3-10.7; parental criminality: IRR, 4.6; 95% CI, 3.0-7.3; parental psychiatric disorder: IRR, 2.7; 95% CI, 1.4-5.3; parental separation: IRR, 4.0; 95% CI, 2.8-5.5; public assistance: IRR, 4.7; 95% CI, 3.1-7.3; child welfare intervention: IRR, 2.3; 95% CI, 1.0-5.2; and residential instability: IRR, 3.4; 95% CI, 1.3-9.1) (Table 3). The highest IRR was observed for convicted with a history of parental substance abuse (multiadjusted IRR, 6.8; 95% CI, 4.3-10.7). The IRRs decreased when all CAs were included in the same model (model 4).
Table 3. Incidence Rate Ratios (95% CIs) for Risk of Suicide by Adolescent Violent Offending and Exposure to Childhood Adversity.
| Variable | Model 1a | Model 2b | Model 3c | Model 4d | ||||
|---|---|---|---|---|---|---|---|---|
| No Violent Offending | Violent Offending | No Violent Offending | Violent Offending | No Violent Offending | Violent Offending | No Violent Offending | Violent Offending | |
| Parental death | ||||||||
| No | 1 [Reference] | 5.7 (4.5-7.3) | 1 [Reference] | 5.2 (4.1-6.7) | 1 [Reference] | 3.0 (2.3-3.9) | 1 [Reference] | 2.6 (2.0-3.4) |
| Yes | 1.2 (0.7-2.0) | 12.5 (5.9-26.4) | 1.1 (0.7-1.9) | 10.9 (5.1-23.1) | 1.0 (0.6-1.7) | 5.6 (2.6-11.9) | 0.9 (0.5-1.4) | 4.1 (1.9-8.9) |
| Parental suicide | ||||||||
| No | 1 [Reference] | 5.9 (4.7-7.5) | 1 [Reference] | 5.4 (4.2-6.9) | 1 [Reference] | 3.1 (2.4-4.0) | 1 [Reference] | 2.7 (2.1-3.5) |
| Yes | 2.4 (1.1-5.4) | 14.0 (3.5-56.3) | 2.2 (1.0-4.9) | 12.7 (3.2-51.2) | 1.8 (0.8-3.9) | 6.8 (1.7-27.3) | 1.4 (0.6-3.3) | 4.7 (1.2-19.1) |
| Parental substance abuse | ||||||||
| No | 1 [Reference] | 5.2 (4.0-6.9) | 1 [Reference] | 4.9 (3.7-6.4) | 1 [Reference] | 2.9 (2.2-3.9) | 1 [Reference] | 2.8 (2.1-3.7) |
| Yes | 3.7 (2.8-4.9) | 17.2 (11.1-26.7) | 3.3 (2.5-4.4) | 14.8 (9.5-23.1) | 2.6 (2.0-3.5) | 6.8 (4.3-10.7) | 2.2 (1.6-3.1) | 5.7 (3.5-9.3) |
| Substantial parental criminality | ||||||||
| No | 1 [Reference] | 5.5 (4.2-7.2) | 1 [Reference] | 5.1 (3.9-6.7) | 1 [Reference] | 3.0 (2.3-4.0) | 1 [Reference] | 2.8 (2.1-3.7) |
| Yes | 2.4 (1.7-3.2) | 10.7 (6.9-16.6) | 2.1 (1.6-2.9) | 9.3 (5.9-14.4) | 1.7 (1.3-2.3) | 4.6 (3.0-7.3) | 1.2 (0.9-1.7) | 3.1 (1.9-5.0) |
| Parental psychiatric disorder | ||||||||
| No | 1 [Reference] | 6.2 (4.9-8.0) | 1 [Reference] | 5.7 (4.4-7.4) | 1 [Reference] | 3.4 (2.6-4.4) | 1 [Reference] | 3.0 (2.3-3.9) |
| Yes | 2.1 (1.5-2.7) | 6.5 (3.-12.7) | 1.9 (1.5-2.6) | 5.9 (3.0-11.4) | 1.5 (1.2-2.1) | 2.7 (1.4-5.3) | 1.2 (0.9-1.6) | 1.8 (0.9-3.5) |
| Parental separation | ||||||||
| No | 1 [Reference] | 5.6 (4.0-7.8) | 1 [Reference] | 5.2 (3.7-7.3) | 1 [Reference] | 3.0 (2.2-4.3) | 1 [Reference] | 2.7 (1.9-3.8) |
| Yes | 1.6 (1.3-1.9) | 8.2 (6.0-11.4) | 1.5 (1.2-1.8) | 7.4 (5.3-10.2) | 1.3 (1.1-1.6) | 4.0 (2.8-5.5) | 1.2 (1.0-1.5) | 3.3 (2.3-4.7) |
| Public assistance recipiency | ||||||||
| No | 1 [Reference] | 5.5 (4.2-7.3) | 1 [Reference] | 5.2 (3.9-6.9) | 1 [Reference] | 3.1 (2.3-4.1) | 1 [Reference] | 2.9 (2.2-3.9) |
| Yes | 2.9 (2.2-3.8) | 10.7 (7.1-16.3) | 2.7 (2.0-3.5) | 9.5 (6.2-14.6) | 2.1 (1.6-2.8) | 4.7 (3.1-7.3) | 1.6 (1.1-2.2) | 3.5 (2.2-5.5) |
| Child welfare intervention | ||||||||
| No | 1 [Reference] | 6.0 (4.7-7.7) | 1 [Reference] | 5.6 (4.3-7.2) | 1 [Reference] | 3.3 (2.6-4.3) | 1 [Reference] | 2.9 (2.2-3.7) |
| Yes | 2.9 (1.8-4.6) | 6.8 (3.1-15.3) | 2.5 (1.6-3.9) | 5.8 (2.6-13.0) | 1.5 (0.9-2.4) | 2.3 (1.0-5.2) | 0.9 (0.5-1.4) | 1.2 (0.5-2.9) |
| Residential instability | ||||||||
| No | 1 [Reference] | 5.9 (4.6-7.5) | 1 [Reference] | 5.4 (4.2-6.9) | 1 [Reference] | 3.1 (2.4-4.0) | 1 [Reference] | 2.7 (2.1-3.5) |
| Yes | 0.9 (0.4-2.2) | 8.3 (3.1-22.3) | 0.8 (0.3-2.0) | 6.9 (2.6-18.5) | 0.6 (0.3-1.5) | 3.4 (1.3-9.1) | 0.5 (0.2-1.2) | 2.5 (0.9-6.7) |
Adjusted for sex and birth year.
Model 1 with additional adjustments for parental country of birth and parental educational level.
Model 2 with additional adjustments for psychiatric disorder before 20 years of age.
Model 3 with additional adjustments for all childhood adversities simultaneously.
In a graded manner, cumulative exposure CA was associated with higher IRR for suicide regardless of adolescent criminal offending (Table 4). Compared with those with no CAs and no adolescent violent offending, individuals with 4 or more CAs had a 21-fold elevated risk of suicide (IRR, 20.6; 95% CI, 11.3-37.5). A large part of the elevated risk was associated with psychiatric disorder (Table 4); the IRR decreased to 8.5 (95% CI, 4.6-15.7). The corresponding IRR among nonconvicted youths was 2.4 (95% CI, 1.5-3.9).
Table 4. Incidence Rate Ratios (95% CIs) for Risk of Suicide by Adolescent Violent Offending and Exposure to Cumulative Childhood Adversity .
| No. of Childhood Adversities | Model 1a | Model 2b | Model 3c | |||
|---|---|---|---|---|---|---|
| No Violent Offending | Violent Offending | No Violent Offending | Violent Offending | No Violent Offending | Violent Offending | |
| 0 | 1 [Reference] | 6.4 (4.1-9.9) | 1 [Reference] | 6.1 (4.0-9.5) | 1 [Reference] | 4.2 (2.7-6.5) |
| 1 | 1.5 (1.3-1.9) | 7.3 (4.5-11.7) | 1.5 (1.2-1.8) | 6.8 (4.2-11.0) | 1.3 (1.1-1.7) | 4.1 (2.5-6.6) |
| 2 | 2.4 (1.9-3.2) | 15.8 (9.9-25.1) | 2.3 (1.7-3.0) | 14.5 (9.1-23.1) | 1.9 (1.4-2.5) | 8.4 (5.2-13.4) |
| 3 | 2.8 (1.9-4.3) | 15.7 (8.4-29.5) | 2.6 (1.7-4.0) | 14.1 (7.5-26.6) | 2.0 (1.3-3.0) | 7.0 (3.7-13.2) |
| ≥4 | 4.1 (2.6-6.4) | 20.6 (11.3-37.5) | 3.6 (2.3-5.7) | 18.2 (9.9-33.4) | 2.4 (1.5-3.9) | 8.5 (4.6-15.7) |
Adjusted for sex and birth year.
Model 1 with additional adjustments for parental country of birth and parental education.
Model 2 with additional adjustments for psychiatric disorder before 20 y of age.
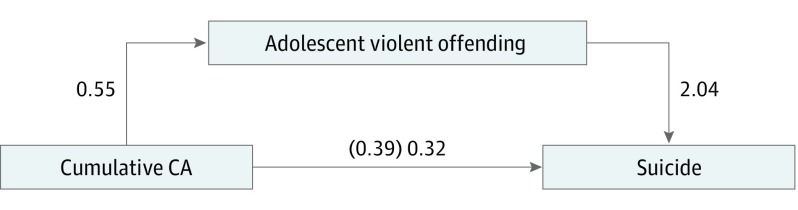
In the mediation (first step) analyses (Figure), cumulative CA (independent variable) was associated with violent offending (mediator) (β1 = 0.54, P < .001). In the second step, cumulative CA (independent variable) was associated with suicide (dependent variable) (β1 = 0.39, P < .001). In the third step, which included all 3 variables, the association of cumulative CA (independent variable) with suicide (dependent variable) decreased but remained significant (β1 = 0.32, P < .001). The mediation analysis further estimated the indirect effect to be 0.03 (95% CI, 0.03-0.04), indicating a small but significant mediation effect of violent offending. Associations between cumulative CA and violent offending are presented in eTable 3 in the Supplement.
Figure. Model of the Association Among Childhood Adversity (CA), Violent Offending, and Suicide.
Logistic regression coefficients are as follows: β0 = −4.32, β1 = 0.55 × cumulative CA, for the association of cumulative CA with adolescent violent offending; β0 = −6.77, β1 = 2.04 × adolescent violent offending, for the association of adolescent violent offending with suicide; β0 = −6.89, β1 = 0.39 × cumulative CA, for total effect (association of cumulative CA with suicide); and β0 = −6.94, β1 = 0.32 × cumulative CA for direct effect (association of cumulative CA with suicide). The value in parentheses is the coefficient for the direct (ie, unmediated) path. P < .001 for all associations.
Both CA and violent offending were associated with increased risk of suicide in the subset of individuals without earlier care for self-harm, and the IRRs were higher compared with those for the whole study cohort (sensitivity analyses) (eTables 4 and 5 in the Supplement). The associations were weaker in the subset of individuals with a history of self-harm (n = 5194, of whom 68 later died by suicide).
Discussion
The present study examined the associations among cumulative CA, adolescent criminal offending, and early adulthood suicide by using Swedish data on a total population cohort of 476 103 individuals. Our findings indicate that adolescent violent offenders often have a history of CA. Furthermore, violent offenders with indicators of adversity in their childhood have a high risk of suicide. The risk is increased 8-fold for violent offenders with a history of cumulative exposure to CA. Last, we observed evidence of mediation of the association between CA and suicide in young adulthood by adolescent violent offending.
The positive associations between multiple types of CAs and adolescent violent offending observed in our study are in line with previous research. In particular, parental criminal behavior has been indicated as a key risk factor for offspring offending. In our cohort, 15.6% of violent offenders had grown up with incarcerated parents compared with 4.1% in the total cohort. Furthermore, our findings revealed that violent offenders more often had experienced cumulative CA, which has been reported by others.
A previous study found that CA is associated with suicide in early adulthood, especially when accumulated. The current study extends existing research by taking into account the role of adolescent violent offending. Interpersonal violence and violent criminal offending have been identified as risk factors for suicide, although the mechanisms underlying these associations are not fully clear. To our knowledge, the current study is the first to examine the mediating role of violent offending in the association between CA and completed suicide in the general population. One recent study based solely on a cohort of youths in the juvenile justice system examined the association between CA and suicide attempts and the mediating role of adolescent problem behaviors in this population. The study found an association between cumulative CA and suicide attempts in young offenders that was partly mediated by aggression and impulsivity.
Our findings shed further light on the mechanisms underlying the link between CA and death from suicide. One possible mechanism is that exposure to adversity early in life causes emotional dysregulation (poorly modulated emotional response) and subsequently maladaptive behaviors, such as aggression, hostility, and violence, as a means for reducing negative emotion. Furthermore, a less supportive and adverse early-life environment might deter an individual’s self-esteem and self-worth, which in turn are related to reactive aggression and antisocial behavior. Aggression, impulsivity, and violence are linked to violent crime and suicide and may thus play an important role in explaining the association between CA and suicidal behavior. Alternatively, a negative life course trajectory during adolescence, such as one that includes violent delinquency, may reinforce the negative consequences of CA on an individual´s interpersonal functioning, reduce social support, and hinder successful transitioning to adult life, resulting in heightened suicide risk during young adulthood. The risk of suicide was even higher among individuals exposed to CA without a history of self-harm in our study, supporting the notion that adolescent violent offending represents a circle of adversity and negative life trajectory that increases the risk of suicide rather than being a marker of previous psychiatric disorder or personality traits related to suicidal behavior.
Last, research indicates that most children and youths in correctional settings have 1 or more mental disorders. In our cohort, 23.6% of those convicted of violent offending had been diagnosed with a psychiatric disorder before their 20th birthday compared with 7.0% in the total cohort (eTable 6 in the Supplement). Adjustment for psychiatric disorder largely attenuated but did not fully explain the association between CA and suicide among convicted youths. Because our definition of psychiatric disorder included only diagnosed cases, we cannot rule out the possibility that psychiatric disorder among youths with delinquent behavior who are exposed to cumulative adversity are less often diagnosed and given proper treatment compared with others in the population and that this might affect suicide risk in this group.
With these lines of reasoning, our findings have some important implications. Efforts that target the excess suicide risk among disadvantaged children should take a life course approach. Apart from interventions during early childhood, particularly those that target emotional regulation, aggression, and impulsivity, our findings highlight a need for interventions during adolescence, including prevention of juvenile delinquency. Young individuals who engage in violent criminality and have a history of cumulative exposure to CA are a group with markedly high risk of suicide independent of their history of self-harm and/or psychiatric disorder. This group can be identified through their contacts in the corrections settings and the health care system and, thus, benefit from targeted suicide prevention interventions and improved overall support. Furthermore, screening for psychiatric disorder should be especially meticulous in this group.
Last, our study indicates that antisocial behavior, resulting in violent offending, may be considered a link between CA and suicide. In the 1980s, Patterson et al formulated a model of parent-child interactions in families in which children develop antisocial behavior. This model proposes that parents in families with children who act out tend to be noncontingent and therefore unsuccessful when attempting to reinforce prosocial behavior and discourage negative behavior. A variety of preventive interventions based on parent training programs have been developed from this model and similar theory, typically targeting children in late preschool or early school age in socially adverse neighborhoods. Lundahl et al included 63 controlled studies in a meta-analysis of such parent training programs and found considerable evidence of positive short-term effects. More recent studies have found family preventive interventions aimed at the prevention of delinquency and substance abuse to have positive long-term effects on suicidal ideation. In addition, prevention programs aimed at reducing aggressive, disruptive behavior in children may delay or prevent suicide ideation. Our study suggests that these parent training programs could also be useful in preventing suicide in children growing up with adversity. Future long-term follow-up studies of parent training programs should also include suicidal behavior as an outcome to prove this point.
Strengths and Limitations
This study has several strengths, including the longitudinal, population-based design and use of national registers with high completeness and validity. Most existing CA studies have been based on self-reported information entailing risk of recall bias. Despite these strengths, our findings should be interpreted in the context of the following limitations. First, the range of CAs is far from exhaustive, and we did not assess the severity, duration, or sequencing of any of these CAs. Several of the CAs capture only the most severe cases (parental substance abuse, parental psychiatric disorder, substantial parental criminality), which should be considered when interpreting the results. Another limitation is that we did not examine the fluidity of CAs but rather, as done by others, treated them as discrete life events. However, the consistency of our results with other studies and the large cohort with high-quality data lend confidence to the validity of our findings.
Conclusions
This study found that one of the mediators of the well-established link between CA and suicide in young adulthood is adolescent violent criminality. Young adults with a history of violent delinquency during adolescence and cumulative exposure to CA have a high risk of suicide, which should be considered by professionals in social and health services. Reducing the excess suicide risk related to CA might benefit from interventions to prevent antisocial behavior and improved support to youths with delinquent behavior.
eTable 1. Description of the Registers Used
eTable 2. Number of Individuals Who Had Experienced Different Childhood Adversities and Combination of Adversities.
eTable 3. Risk of Violent Offending by Exposure to Cumulative Childhood Adversity*
eTable 4. Risk of Suicide From Age 20, by Exposure to Adolescent Violent Offending and Childhood Adversity Stratified by History of Self-harm
eTable 5. Risk of Suicide From Age 20 by Exposure to Adolescent Violent Offending and Cumulative Childhood Adversity Stratified by History of Self-harm
eTable 6. Number of Individuals With Violent Offending and Suicide by Sex and Type of Psychiatric Disorder Before Age 20 Years
References
- 1.Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. 2016;387(10024):1227-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Preventing Suicide: A Global Imperative. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 3.Cash SJ, Bridge JA. Epidemiology of youth suicide and suicidal behavior. Curr Opin Pediatr. 2009;21(5):613-619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wasserman D, Cheng Q, Jiang GX. Global suicide rates among young people aged 15-19. World Psychiatry. 2005;4(2):114-120. [PMC free article] [PubMed] [Google Scholar]
- 5.Björkenstam C, Kosidou K, Björkenstam E. Childhood adversity and risk of suicide: cohort study of 548 721 adolescents and young adults in Sweden. BMJ. 2017;357:j1334. [DOI] [PubMed] [Google Scholar]
- 6.Brent DA, Melhem NM, Oquendo M, et al. . Familial pathways to early-onset suicide attempt: a 5.6-year prospective study. JAMA Psychiatry. 2015;72(2):160-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agerbo E, Nordentoft M, Mortensen PB. Familial, psychiatric, and socioeconomic risk factors for suicide in young people: nested case-control study. BMJ. 2002;325(7355):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brent DA, Bridge J, Johnson BA, Connolly J. Suicidal behavior runs in families: a controlled family study of adolescent suicide victims. Arch Gen Psychiatry. 1996;53(12):1145-1152. [DOI] [PubMed] [Google Scholar]
- 9.Bruffaerts R, Demyttenaere K, Borges G, et al. . Childhood adversities as risk factors for onset and persistence of suicidal behaviour. Br J Psychiatry. 2010;197(1):20-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hawton K, Saunders KE, O’Connor RC. Self-harm and suicide in adolescents. Lancet. 2012;379(9834):2373-2382. [DOI] [PubMed] [Google Scholar]
- 11.Borges G, Angst J, Nock MK, Ruscio AM, Kessler RC. Risk factors for the incidence and persistence of suicide-related outcomes: a 10-year follow-up study using the National Comorbidity Surveys. J Affect Disord. 2008;105(1-3):25-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. Am J Prev Med. 2010;39(1):93-98. [DOI] [PubMed] [Google Scholar]
- 13.Farrington WB. Saving Children from a Life of Crime. Oxford, England: Oxford University Press Inc; 2007. [Google Scholar]
- 14.Wilcox HC, Kuramoto SJ, Lichtenstein P, Långström N, Brent DA, Runeson B. Psychiatric morbidity, violent crime, and suicide among children and adolescents exposed to parental death. J Am Acad Child Adolesc Psychiatry. 2010;49(5):514-523. [DOI] [PubMed] [Google Scholar]
- 15.Perez NM, Jennings WG, Piquero AR, Baglivio MT. Adverse childhood experiences and suicide attempts: the mediating influence of personality development and problem behaviors. J Youth Adolesc. 2016;45(8):1527-1545. [DOI] [PubMed] [Google Scholar]
- 16.Roy A. Childhood trauma and impulsivity: possible relevance to suicidal behavior. Arch Suicide Res. 2005;9(2):147-151. [DOI] [PubMed] [Google Scholar]
- 17.Giegling I, Olgiati P, Hartmann AM, et al. . Personality and attempted suicide: analysis of anger, aggression and impulsivity. J Psychiatr Res. 2009;43(16):1262-1271. [DOI] [PubMed] [Google Scholar]
- 18.Ammerman BA, Kleiman EM, Uyeji LL, Knorr AC, McCloskey MS. Suicidal and violent behavior: the role of anger, emotion dysregulation, and impulsivity. Pers Individ Dif. 2015;79:57-62. [Google Scholar]
- 19.Conner K, Duberstein P, Conwell Y, Caine ED. Reactive aggression and suicide: Theory and evidence. Aggress Violent Behav. 2003;8(4):413-432. [Google Scholar]
- 20.Ruchkin V, Koposov RA, Koyanagi A, Stickley A. Suicidal behavior in juvenile delinquents: the role of ADHD and other comorbid psychiatric disorders [published online October 12, 2016]. Child Psychiatry Hum Dev. [DOI] [PubMed] [Google Scholar]
- 21.Murray J, Farrington DP, Sekol I. Children’s antisocial behavior, mental health, drug use, and educational performance after parental incarceration: a systematic review and meta-analysis. Psychol Bull. 2012;138(2):175-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sousa C, Herrenkohl TI, Moylan CA, et al. . Longitudinal study on the effects of child abuse and children’s exposure to domestic violence, parent-child attachments, and antisocial behavior in adolescence. J Interpers Violence. 2011;26(1):111-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duke NN, Pettingell SL, McMorris BJ, Borowsky IW. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics. 2010;125(4):e778-e786. [DOI] [PubMed] [Google Scholar]
- 24.Wallinius M, Delfin C, Billstedt E, Nilsson T, Anckarsäter H, Hofvander B. Offenders in emerging adulthood: school maladjustment, childhood adversities, and prediction of aggressive antisocial behaviors. Law Hum Behav. 2016;40(5):551-563. [DOI] [PubMed] [Google Scholar]
- 25.Baglivio M, Swartz K, Sayedul Huq M, Sheer A, Hardt N. The prevalence of adverse childhood experiences (ACE) in the lives of juvenile offenders. J Juv Justice. 2014;3(2):1-24. [Google Scholar]
- 26.Dierkhising CB, Ko SJ, Woods-Jaeger B, Briggs EC, Lee R, Pynoos RS. Trauma histories among justice-involved youth: findings from the National Child Traumatic Stress Network. Eur J Psychotraumatol. 2013;4:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fox BH, Perez N, Cass E, Baglivio MT, Epps N. Trauma changes everything: examining the relationship between adverse childhood experiences and serious, violent and chronic juvenile offenders. Child Abuse Negl. 2015;46:163-173. [DOI] [PubMed] [Google Scholar]
- 28.Basto-Pereira M, Miranda A, Ribeiro S, Maia Â. Growing up with adversity: from juvenile justice involvement to criminal persistence and psychosocial problems in young adulthood. Child Abuse Negl. 2016;62:63-75. [DOI] [PubMed] [Google Scholar]
- 29.Corneau M, Lanctôt N. Mental health outcomes of adjudicated males and females: the aftermath of juvenile delinquency and problem behaviour. Crim Behav Ment Health. 2004;14(4):251-262. [DOI] [PubMed] [Google Scholar]
- 30.Fazel S, Doll H, Långström N. Mental disorders among adolescents in juvenile detention and correctional facilities: a systematic review and metaregression analysis of 25 surveys. J Am Acad Child Adolesc Psychiatry. 2008;47(9):1010-1019. [DOI] [PubMed] [Google Scholar]
- 31.Björkenstam E, Björkenstam C, Vinnerljung B, Hallqvist J, Ljung R. Juvenile delinquency, social background and suicide–a Swedish national cohort study of 992,881 young adults. Int J Epidemiol. 2011;40(6):1585-1592. [DOI] [PubMed] [Google Scholar]
- 32.Vaughn MG, Salas-Wright CP, DeLisi M, Maynard BR, Boutwell B. Prevalence and correlates of psychiatric disorders among former juvenile detainees in the United States. Compr Psychiatry. 2015;59:107-116. [DOI] [PubMed] [Google Scholar]
- 33.Wasserman G, McReynolds L, Schwalbe C, Keating J, Jones S. Psychiatric disorder, comorbidity, and suicidal behavior in juvenile justice youth. Crim Justice Behav. 2010;37(12):1361-1376. [Google Scholar]
- 34.Flannery DJ, Singer MI, Wester K. Violence exposure, psychological trauma, and suicide risk in a community sample of dangerously violent adolescents. J Am Acad Child Adolesc Psychiatry. 2001;40(4):435-442. [DOI] [PubMed] [Google Scholar]
- 35.Teplin LA, McClelland GM, Abram KM, Mileusnic D. Early violent death among delinquent youth: a prospective longitudinal study. Pediatrics. 2005;115(6):1586-1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24(11):659-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mok PL, Pedersen CB, Springate D, et al. . Parental psychiatric disease and risks of attempted suicide and violent criminal offending in offspring: a population-based cohort study. JAMA Psychiatry. 2016;73(10):1015-1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention (CDC) Adverse Childhood Experiences Study. 2017. https://www.cdc.gov/violenceprevention/acestudy. Accessed May 15 2017.
- 39.Jelleyman T, Spencer N. Residential mobility in childhood and health outcomes: a systematic review. J Epidemiol Community Health. 2008;62(7):584-592. [DOI] [PubMed] [Google Scholar]
- 40.Vinnerljung B, Sallnäs M. Into adulthood: a follow-up study of 718 young people who were placed in out-of-home care during their teens. Child Fam Soc Work. 2008;13:144-155. [Google Scholar]
- 41.Fazel S, Grann M. The population impact of severe mental illness on violent crime. Am J Psychiatry. 2006;163(8):1397-1403. [DOI] [PubMed] [Google Scholar]
- 42.Linsley KR, Schapira K, Kelly TP. Open verdict v. suicide: importance to research. Br J Psychiatry. 2001;178:465-468. [DOI] [PubMed] [Google Scholar]
- 43.Grann M, Fazel S. Substance misuse and violent crime: Swedish population study. BMJ. 2004;328(7450):1233-1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173-1182. [DOI] [PubMed] [Google Scholar]
- 45.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.UCLA Statistical Consulting Group How can I perform mediation with binary variables? 2013. https://www.stata.com/statalist/archive/2011-07/msg00062.html. Accessed June 23 2017.
- 47.Shapero BG, Steinberg L. Emotional reactivity and exposure to household stress in childhood predict psychological problems in adolescence. J Youth Adolesc. 2013;42(10):1573-1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sahlin H, Kuja-Halkola R, Bjureberg J, et al. . Association between deliberate self-harm and violent criminality. JAMA Psychiatry. 2017;74(6):615-621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Donnellan MB, Trzesniewski KH, Robins RW, Moffitt TE, Caspi A. Low self-esteem is related to aggression, antisocial behavior, and delinquency. Psychol Sci. 2005;16(4):328-335. [DOI] [PubMed] [Google Scholar]
- 50.Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. Am Psychol. 1989;44(2):329-335. [DOI] [PubMed] [Google Scholar]
- 51.Lundahl B, Risser HJ, Lovejoy MC. A meta-analysis of parent training: moderators and follow-up effects. Clin Psychol Rev. 2006;26(1):86-104. [DOI] [PubMed] [Google Scholar]
- 52.Vidot DC, Huang S, Poma S, Estrada Y, Lee TK, Prado G. Familias unidas’ crossover effects on suicidal behaviors among hispanic adolescents: results from an effectiveness trial. Suicide Life Threat Behav. 2016;46(S1)(suppl 1):S8-S14. [DOI] [PubMed] [Google Scholar]
- 53.Sandler I, Tein JY, Wolchik S, Ayers TS. The effects of the family bereavement program to reduce suicide ideation and/or attempts of parentally bereaved children six and fifteen years later. Suicide Life Threat Behav. 2016;46(S1)(suppl 1):S32-S38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wilcox HC, Kellam SG, Brown CH, et al. . The impact of two universal randomized first- and second-grade classroom interventions on young adult suicide ideation and attempts. Drug Alcohol Depend. 2008;95(S1)(suppl 1):S60-S73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Colman I, Kingsbury M, Garad Y, et al. . Consistency in adult reporting of adverse childhood experiences. Psychol Med. 2016;46(3):543-549. [DOI] [PubMed] [Google Scholar]
- 56.Felitti VJ, Anda RF, Nordenberg D, et al. . Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245-258. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Description of the Registers Used
eTable 2. Number of Individuals Who Had Experienced Different Childhood Adversities and Combination of Adversities.
eTable 3. Risk of Violent Offending by Exposure to Cumulative Childhood Adversity*
eTable 4. Risk of Suicide From Age 20, by Exposure to Adolescent Violent Offending and Childhood Adversity Stratified by History of Self-harm
eTable 5. Risk of Suicide From Age 20 by Exposure to Adolescent Violent Offending and Cumulative Childhood Adversity Stratified by History of Self-harm
eTable 6. Number of Individuals With Violent Offending and Suicide by Sex and Type of Psychiatric Disorder Before Age 20 Years