Key Points
Question
What is the current electronic health record (EHR) adoption rate among ophthalmologists in the United States, and what is their perception of financial and clinical productivity following implementation?
Findings
In this population-based, cross-sectional survey, the adoption rate of EHRs among ophthalmologists was 72.1%. Ophthalmologists reported that their net revenues and productivity have declined and that practice costs are higher with EHR use.
Meaning
The EHR adoption rate has doubled since a previous EHR survey of American ophthalmologists in 2011, and in comparison with 2 previous EHR surveys, perceptions of practice costs and clinical productivity are more negative.
Abstract
Importance
Assessing the rate of electronic health record (EHR) adoption and ophthalmologists’ perceptions on financial and clinical productivity is important in understanding how to direct future design and health care policy.
Objective
To assess adoption rate and perceptions of financial and clinical outcomes of EHRs among ophthalmologists in the United States.
Design, Setting, and Participants
Population-based, cross-sectional study. A random sample of 2000 ophthalmologists was generated on the basis of mailing address zip codes from the 2015 American Academy of Ophthalmology US active membership database, which included more than 18 000 ophthalmologists. A survey was sent by email to assess adoption rate of EHRs, perceptions of financial and clinical productivity, and engagement with Medicare and Medicaid programs that incentivize the use of EHRs. The survey was conducted between 2015 and 2016.
Main Outcomes and Measures
Adoption rate of EHRs and perceptions of financial and clinical productivity.
Results
The adoption rate of EHRs among surveyed ophthalmologists (348 respondents) was 72.1%. The responding ophthalmologists perceived that their net revenues and productivity have declined and that practice costs are higher with EHR use. Of those who attested for stage 1 of the EHR incentive program, 83% had already or were planning to attest to stage 2, but 9% had no plans.
Conclusions and Relevance
The adoption of EHRs by ophthalmologists has more than doubled since a 2011 survey and is similar to that of primary care physicians (79%). In comparison with 2 previous surveys of ophthalmologists, respondents had more negative perceptions of EHR productivity outcomes and effect on practice costs, although financial data were not collected in this survey to support these opinions. These negative perceptions suggest that more attention should be placed on improving the efficiency and usability of EHR systems.
This ppulation-based survey assesses adoption rate and perceptions of financial and clinical outcomes of electronic health records among ophthalmologists in the United States.
Introduction
In 2006, a survey of American ophthalmologists assessed adoption and perceptions of electronic health record (EHR) systems and found that the adoption rate of EHRs was low (19%) but in line with that of other medical specialties in the United States at the time. The satisfaction rate of ophthalmologists already using an EHR in this survey was high (69% satisfied or extremely satisfied). Soon after the completion of this survey, the Health Information Technology for Economic and Clinical Health Act created financial incentives that accelerated the use of EHRs in the years to follow. In 2011, a follow-up survey was conducted that showed that the adoption rate of EHR had more than doubled to 47% among surveyed ophthalmologists. However, the satisfaction of ophthalmologists with their EHR and their perception of beneficial effects on practice productivity and costs had fallen in comparison with 2006. To continue to track the evolving perceptions of the deployment of EHRs in ophthalmology, this survey was administered at a time when the incentive payments from the Health Information Technology for Economic and Clinical Health Act were scheduled to wind down. This latest survey continues to assess the adoption rate of EHR and also focuses on subjective clinical and financial productivity effect in more detail than in the former 2 surveys. It also reports on ophthalmologists’ success with qualifying for the “meaningful use” financial incentive program and their plans to continue to participate in the program.
Methods
Survey Instrument
The EHR survey instrument was derived from questions used for the 2006 and 2011 surveys on EHR adoption. Questions were added to assess subjective changes in financial results, clinical productivity, engagement in the Medicare EHR incentive program, and awareness of documentation integrity of the medical record. The complete survey is available in the eMethods in the Supplement. Because the survey information was anonymous and no personal health information was collected, this study was exempt from requirement for institutional review board approval, and informed consent was not required.
Survey Population
A random sample of 2000 ophthalmologists was obtained on the basis of mailing address zip codes from the 2015 American Academy of Ophthalmology (AAO) US active membership database, which included more than 18 000 ophthalmologists. Each unique zip code was represented in the list of potential participants. If more than 1 member was listed with the same zip code, a random assignment process was used to select the person who would receive the survey. This sampling process was intended to provide a geographically diverse population of ophthalmologists while minimizing the opportunity for multiple responses from physicians who practiced within the same group.
Survey Administration
The survey was sent by email to a total of 2000 ophthalmologists between 2015 and 2016. For those members who still had not responded after 1 month, subsequent emails were sent monthly during the following 4 months to encourage physicians to complete the survey. The 2015/2016 survey was conducted via email only because analysis of the results from 2011 showed no difference in findings between those who responded by email vs facsimile, telephone call, or paper.
Data Analysis
Differences between practices with and without EHRs and differences between physicians with regard to number of years in practice were assessed using the Fisher exact test for categorical variables and the Mann-Whitney test for continuous variables. All statistical analyses were performed using R, version 3.3.2 (The R Foundation) with the Hmisc and HH libraries. Significance was achieved with P less than .05, and a 2-tailed test was used for statistical analysis.
Results
Practice and Physician Characteristics
Of the 2000 surveys emailed to American Academy of Ophthalmology members, 348 were completed (17.4%). Practices with an EHR had a higher mean number of ophthalmologists than those without EHR (Table 1). Respondents from practices with and without an EHR were both predominantly “ophthalmology only” and were predominantly physician-owned. However, ophthalmologists from practices that were part of an integrated health system, government health system, or university were more likely to have adopted EHR than not. Physicians who responded to this survey had been practicing for a mean of 22 years, had been using an EHR for 5.3 years, and 99.7% had used paper records before. Of respondents from practices with an EHR, 88% were practicing during the transition from paper records to EHR.
Table 1. Characteristics of Practices With and Without an EHR.
| Characteristic | With EHR, No. (%) (n = 265) |
Without EHR, No. (%) (n = 83) |
P Value |
|---|---|---|---|
| Ophthalmologists, mean (SD) | 8.8 (17) | 2.8 (3.1) | <.001 |
| Practice type | |||
| Ophthalmology | 205 (79) | 77 (96) | <.001 |
| Multispecialty | 56 (21) | 3 (4) | |
| Other | 0 | 0 | |
| Subspecialties | |||
| Comprehensive | 207 (79) | 65 (81) | <.001 |
| Cornea | 105 (45) | 23 (29) | |
| Cataract | 152 (58) | 34 (43) | |
| Glaucoma | 118 (45) | 29 (36) | |
| Neuro-ophthalmology | 64 (24) | 8 (10) | |
| Pathology | 23 (8.8) | 2 (2.5) | |
| Pediatrics | 71 (27) | 2 (20) | |
| Strabismus | 67 (26) | 9 (11) | |
| Plastics | 104 (40) | 22 (28) | |
| Refractive | 91 (35) | 17 (21) | |
| Uveitis | 58 (22) | 6 (7.5) | |
| Medical retina | 120 (46) | 19 (24) | |
| Surgical retina | 106 (41) | 10 (13) | |
| Practice type | |||
| Physician owned | 203 (77) | 79 (95) | .003 |
| University | 30 (11) | 2 (2.4) | |
| Government | 7 (2.6) | 0 | |
| Hospital or integrated | 15 (5.7) | 0 | |
| Health maintenance organization | 3 (1) | 0 | |
| Other academic | 3 (1) | 2 (2.4) |
Abbreviation: EHR, electronic health record.
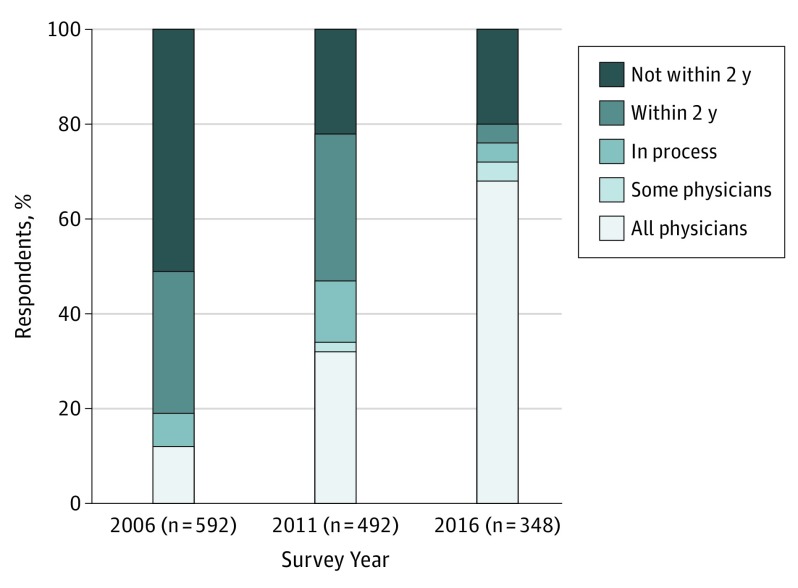
Use of Computers in Clinical Practice
Among respondents, 72.1% (n = 251 of 348) had implemented EHR for some or all physicians in their practice vs 47% (n = 231 of 492) in the 2011 survey and 19% (n = 113 of 592) in the 2006 survey (Figure 1). Compared with the 2011 survey, a greater proportion were using computer-based systems (eFigure in the Supplement). For example, in 2011, only one-third of respondents were using the computer for clinical documentation in comparison with more than two-thirds of respondents in the 2015/2016 survey. The greatest proportional change in computerization was for functions directly related to patient care (e-prescribing, image management, and clinical documentation) compared with administrative functions (billing and practice management). When asked about the location of their EHR data, 52% of respondents (n = 181 of 348) reported hosting their own data at or near their practice, 34% (n = 118) had data on a server located outside of their practice (cloud-based), 3.4% (n = 12) indicated “other,” and 10% (n = 35) did not know where their EHR data resided. Between 2011 and 2015, there was a decline in physician documentation via typing and dictation and an increase in the use of scribes (Table 2).
Figure 1. Electronic Health Record Implementation Status by Year of Survey.
Table 2. Methods of Data Entry for the 2011 (243 Respondents) and 2016 (261 Respondents) Survey for Respondents Who Were Not All Paper-Based With Regard to Clinical Documentation.
| Method of Data Entry | No. (%)a | |
|---|---|---|
| 2011 | 2016 | |
| Physician typing | 220 (91) | 198 (76) |
| Scribe | 88 (36) | 126 (48) |
| Dictation | 53 (22) | 15 (5.7) |
| Voice recognition | NA | 12 (4.6) |
| Paper | 37 (15) | 31 (12) |
| Scan | 34 (14) | 22 (8.4) |
Abbreviation: NA, not applicable.
Percentages do not add to 100 because practices were allowed to report more than 1 method of data entry and more than 1 type of person doing data entry.
When viewing the results of in-office testing, 46% of ophthalmologists used paper reports (n = 160 of 348), 39% used vendor software (n = 136), 24% scanned printed images (n = 84), 21% used a picture archiving and communication system (n = 73), 37% viewed images in their EHR (n = 129), and 1.7% were unsure (n = 6) (percentages do not add to 100 because practices were allowed to report more than 1 method of integration). Satisfaction with image management systems and clinical documentation systems was similar, with 49% of respondents being satisfied or extremely satisfied with their image management system vs 50% being satisfied with their clinical documentation system. Sixteen percent were unsatisfied or extremely unsatisfied with their image management system, while 27% expressed dissatisfaction with their clinical documentation system.
The top 10 EHR and top 8 image management systems used by respondents in this survey by frequency can be found in the eTable in the Supplement.
Perceived Financial and Clinical Effect of EHR
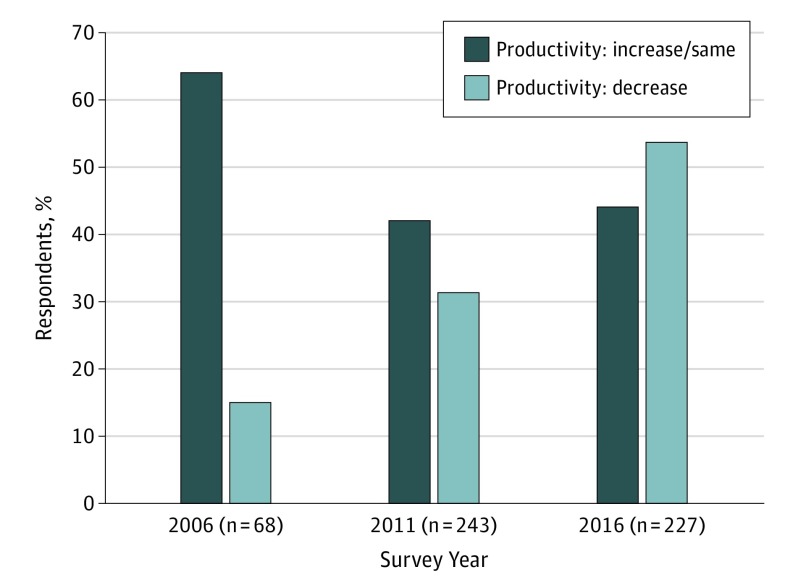
Respondents who were present during the conversion from paper records to EHR were asked questions about the perceived financial and clinical effect on their practice. Respondents were asked about productivity changes in terms of number of patients seen per day. Figure 2 shows that a growing proportion of respondents perceive that productivity had decreased after EHR adoption when comparing results from the 3 surveys.
Figure 2. Perception of Productivity Changes (Number of Patients Seen per Day) After Electronic Health Record (EHR) Adoption.
Perception of productivity changes (number of patients seen per day) after EHR adoption from the 2006 and 2011 ophthalmology surveys and in the current 2016 survey.
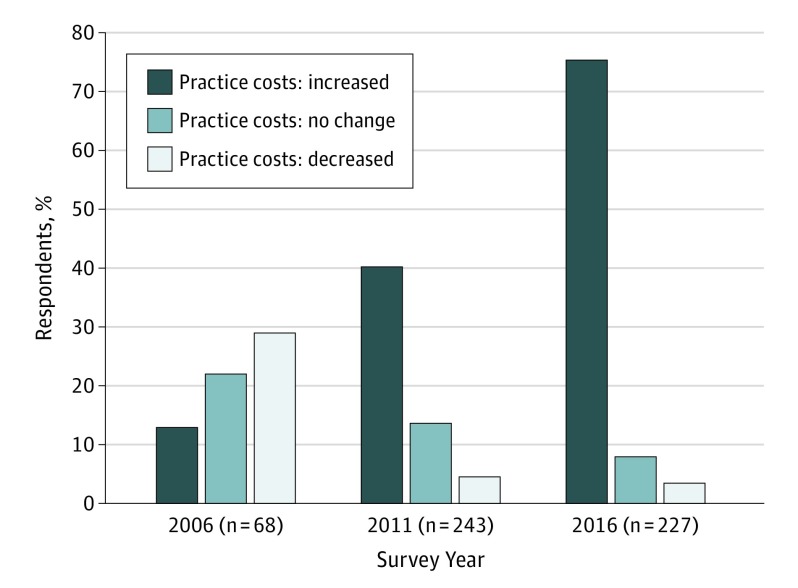
Perceptions of overall practice costs have changed since the 2006 survey, and the proportion of ophthalmologists who felt that costs were higher after the implementation of EHR had increased (Figure 3). The perception of net practice revenue after EHR was mixed; 35% (n = 79 of 227) thought it had stayed the same after EHR adoption and 41% (n = 93) thought it had decreased. Almost 9% (n = 20) felt that net revenue had increased, and 1.6% (n = 4) were unsure.
Figure 3. Perception of Change in Overall Practice Costs After Electronic Health Record (EHR) Adoption.
Perception of change in overall practice costs after EHR adoption from the 2006 and 2011 ophthalmology surveys and in the 2016 survey.
Most respondents felt that the level of coding (Evaluation and Management and Eye Codes) had not changed (175 of 227 respondents [77%]), while 13% (n = 30) felt that the level of coding was higher, 3.1% (n = 7) felt it was lower, and 6.2% (n = 14) were unsure. Regarding charge capture (proportion of charges captured for office visits, procedures, and tests), 19% (n = 43) felt that the ability to capture charges was greater with EHR, 56% (n = 127) felt it was the same, 5.3% (n = 12) felt it was lower, and 19% (n = 43) were unsure. Most respondents reported that patient attitudes toward the EHR were mostly positive or neutral (76%; n = 172), 18% (n = 41) thought they were negative, and 6% (n = 14) were unsure. When asked how EHR affected the quality of care provided, 25% (n = 57) believed it was easier to provide quality care vs paper, 36% (n = 82) believed it was about the same, 35% (n = 80) believed it was harder, and 4% (n = 9) were unsure. Respondents were asked about their overall experience providing care in their practice using the EHR vs paper, and 25% (n = 57) felt the experience was better, 28% (n = 64) felt it was about the same, 44% (n = 100) felt it was worse than paper, and 3% (n = 7) were unsure. As in previous surveys, respondents were asked whether they would recommend their EHR to another ophthalmologist. In this survey, 55% (n = 141) would do so vs 55% (n = 271 of 492) in the 2011 survey and 76% (n = 83 of 109) in the 2006 survey. A subanalysis of this data according to number of years in practice showed no significant difference between junior and senior ophthalmologists. Of those in practice 10 years or less (n = 40), 52% would recommend their EHR compared with 59% of those in practice at least 27 years (n = 58) (P = .40). When asked whether they would return to paper, 36% of 227 respondents answered yes (n = 82), 53% answered no (n = 120), and 11% were unsure (n = 25). No statistically significant difference existed between junior ophthalmologists (n = 32) and senior ophthalmologists (n = 74) for this question (P > .99).
Federal EHR Incentive Programs
Sixty-three percent of ophthalmologists (n = 219 of 348) responded that they had enough knowledge of the program to make a decision about participating (44% [n = 217 of 492] in 2011 survey), 25% (n = 87) felt they had some knowledge of the program (43.7% [n = 215 of 492] in 2011 survey), and 11% (n = 38) felt that they had little or no knowledge of the program (12% [n = 60 of 492] in 2011 survey). Among all respondents, 60% (n = 209) had already attested to stage 1 of the incentive program, 7.5% (n = 26) were planning to, 21% (n = 73) were not planning to, and 12% (n = 42) were unsure. Reasons for not attesting to stage 1 were that their EHR was not certified (4% of respondents [n = 3 of 73]), the incentive was not relevant to their practice (23%; n = 17), the cost of participating was too high (45%; n = 33), the complexity of participating was too high (38%; n = 28), and other (30%; n = 22). When asked about plans to attest to stage 2 of the incentive program, 41% of respondents had already attested (n = 85 of 207), 42% were planning to (n = 87), 9% were not planning to (n = 2), 6% were unsure (n = 12), and 2% responded other (n = 4). Reasons for not planning on stage 2 attestation were the incentive was not relevant to their practice (5%; n = 1 of 19), the cost of participating was too high (63%; n = 12), the complexity of participating was too high (68%; n = 13), and other (42%; n = 8). Percentages add up to more than 100 because respondents could select more than 1 reason. To compare the participation of ophthalmologists in the meaningful use program with other surgical subspecialties, we used data available from the Centers for Medicare and Medicaid Services to calculate the proportional representation of eligible clinicians in those specialties in the attestation data as well as the proportion of payments each received from 2011 to 2015. Ophthalmologists represented 3.2% of all meaningful use attestations and received 3.4% of all payments. For dermatology, those values were 1.8% and 1.9%; for otolaryngology, 1.8% and 1.9%; and for urology. 2.2% and 2.3%. These numbers suggest that specialists in these fields had similar rates of remaining in the meaningful use program during the 5 years for which data were available.
Documentation in EHR
Documentation integrity in the use of the EHR is a prominent safety and compliance issue in the United States. In this survey, most had a copy forward function in their EHR (88%; n = 226 of 257), and when asked how often documentation errors occur (eg, outdated information copied forward, contradictory statements, authorship confusion, and data entered for wrong patient), 60% responded sometimes or frequently (n = 154), 34% rarely (n = 87), and 3.1% never (n = 8). Most (71%; n = 183) reported having policies and/or guidelines in place in their practice to govern the integrity of documentation in their EHR, 11% did not have one (n = 28), and 17.5% did not know or were unsure whether a policy existed (n = 45).
Discussion
The EHR adoption rate among US ophthalmologists has more than doubled, from 47% in the 2011 survey to 72.1% in the 2015/2016 survey. Ophthalmologists who responded to this survey perceive that productivity and net revenues have declined and that costs associated with the use of the EHR have increased in comparison with 2 previous surveys. More than half of ophthalmologists in this survey had attested to stage 1 of the meaningful use incentive, and roughly 80% of respondents who had attested to stage 1 stated they had either already attested or were planning to attest to stage 2.
The National Ambulatory Medical Care Survey conducted by the US Centers for Disease Control and Prevention found that a greater proportion of primary care physicians (79%) in the United States in 2014 had a certified EHR technology in comparison with that of all specialty care physicians (70%). The adoption rate for ophthalmologists in our survey (72.1%) was in line with that of other specialties. Past publications using National Ambulatory Medical Care Survey data from 2005 to 2009 have indicated a slower adoption rate for specialty physicians. The authors comment that slower adoption rate for specialties such as ophthalmology may be owing to factors such as high patient volume, requirements for integration of specialized images, and the combination of outpatient practice and surgical procedures.
Perceived Financial and Clinical Productivity Outcomes
Although our survey respondents had negative perceptions of the financial effects of EHR implementation, 2 prior studies of large ophthalmology practices showed no significant differences in net revenues or charge capture before and after EHR implementation during short-term and long-term follow-up periods.
In 2012, the Office of the Inspector General released a report indicating that between 2001 and 2010, physicians in the United States increased their proportion of billing to higher-level, more complex, expensive codes for outpatient office visits and cited overdocumentation via EHR as a possible reason. In our survey, most physicians felt that their level of coding was unchanged after EHR implementation. Three studies have assessed coding levels in ophthalmology before and after EHR adoption, and 2 of those found no changes in coding level, while 1 found a significant increase in higher-level codes after EHR adoption.
Ophthalmologists in this survey felt that productivity in terms of number of patients seen per day dropped after EHR implementation; however, 3 studies in large academic ophthalmology practices found that patient volume did not change after implementation. One study did find a decrease in patient visits per clinician for a small sample of ophthalmologists, and patient volume never returned to pre-EHR levels. The perception of productivity decline may be partially owing to the multiple tasks that are required to obtain incentive payments. In a survey of physicians in Washington State, 70% felt that meeting these requirements would decrease their clinical productivity. In free comments, several respondents mentioned the burdensome and complicated nature of meaningful use and felt that it distracted from patient care. These sentiments are mirrored in this survey, in which most ophthalmologists who had not attested to stage 1 or stage 2 of federal EHR incentive programs named complexity and cost of reporting as barriers.
Federal EHR Incentive Programs
In the 2011 survey of ophthalmologists, only 30% of those who responded had an EHR that was ready to attest to stage 1 at the time of the survey, and 18% had no intentions of attesting. The engagement of ophthalmologists in meaningful use has increased in the 2015/2016 survey (83% had already or were planning to attest to stage 2), although a significant percentage (21%) of respondents still had no plans to attest to stage 1. Our data regarding the EHR incentive program suggest that ophthalmology was comparable with other surgical subspecialties with regard to consistency of participation.
Potential Documentation Errors
With the evolution of EHR, unintended consequences have arisen, and one such area concerns the accuracy of the medical record. Tools that EHRs provide to increase efficiency in documenting the patient’s medical course, such as copy forward, drop-down menus, pick lists, and templates, can lead to the entry of erroneous information. These errors can reduce the utility of electronic documentation when clinicians begin to doubt the veracity of what was entered. In our survey, most respondents had a copy forward function available in their EHR, and almost 70% recognized errors in their electronic notes. A systematic review of 51 publications that studied documentation error revealed that 66% to 90% of clinicians routinely use copy and paste. One of these studies found that copy and paste led to 2.6% of errors in which a missed diagnosis required patients to seek additional unplanned care. In 2015, guidelines were published for ensuring integrity of EHR documentation, and this and other reports outline practical, safe recommendations that any clinician can adopt in their practice.
Limitations
The response rate for the 2015/2016 survey may result in incomplete representation of the demographics and opinions of American ophthalmologists. Some of the opinions expressed in this survey were more negative than in previous surveys, and it is possible that those who responded to the survey were more likely to have negative opinions of the EHR or that early, more enthusiastic adopters were more likely to have been included in the 2006 EHR survey and that this may account for the shift in opinions. In addition, it is important to keep in mind that the more negative responses regarding financial performance are opinion only, and no financial data were collected as part of this survey. The survey was conducted solely by email, which may bias the responses in favor of ophthalmologists who may be more computer savvy. However, analysis of the 2011 EHR survey did not show a difference between respondents who took the survey by email, facsimile, telephone call, or by paper with regard to the size of practice, mix of specialties, practice ownership, or degree of computerization.
Conclusions
Opinions from this survey suggest a need for improvement in 2 areas: usability of EHR and meaningful use requirements. For example, more streamlined methods of viewing and interpreting diagnostic images and faster data entry for high-volume practices are necessary. Finally, while a significant proportion of respondents are engaged in federal EHR incentive programs, the cost and complexity of the programs are potential barriers to participation, and this emphasizes the need to simplify measures that are a part of the new Advancing Care Information program that is the successor to meaningful use.
eMethods. Electronic Health Record (EHR) Survey 2016
eTable. The Top Electronic Health Record (EHR) and Image Management Systems Used by Respondents in This Survey by Frequency.
eFigure. Computerization of Clinical Information Systems in the 2011 Ophthalmology EHR Survey (Left) and in the 2016 Survey (Right).
References
- 1.Chiang MF, Boland MV, Margolis JW, Lum F, Abramoff MD, Hildebrand PL; American Academy of Ophthalmology Medical Information Technology Committee . Adoption and perceptions of electronic health record systems by ophthalmologists: an American Academy of Ophthalmology survey. Ophthalmology. 2008;115(9):1591-1597. [DOI] [PubMed] [Google Scholar]
- 2.Hsiao CJ, Hing E. Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001-2012. NCHS Data Brief. 2012;(111):1-8. [PubMed] [Google Scholar]
- 3.Hsiao C-J, Jha AK, King J, Patel V, Furukawa MF, Mostashari F. Office-based physicians are responding to incentives and assistance by adopting and using electronic health records. Health Aff (Millwood). 2013;32(8):1470-1477. [DOI] [PubMed] [Google Scholar]
- 4.Boland MV, Chiang MF, Lim MC, et al. ; American Academy of Ophthalmology Medical Information Technology Committee . Adoption of electronic health records and preparations for demonstrating meaningful use: an American Academy of Ophthalmology survey. Ophthalmology. 2013;120(8):1702-1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CMS Medicare and Medicaid EHR Incentive Program; Office of the National Coordinator for Health Information Technology, Department of Health and Human Services. Electronic health record products used for attestation. https://catalog.data.gov/dataset/cms-medicare-and-medicaid-ehr-incentive-program-electronic-health-record-products-used-for-f4247. Published 2017. Accessed November 1, 2017.
- 6.Office of the National Coordinator for Health Information Technology EHR products used for meaningful use attestation. https://dashboard.healthit.gov/datadashboard/documentation/ehr-products-mu-attestation-data-documentation.php. Published 2017. Accessed November 1, 2017.
- 7.Centers for Medicare and Medicaid DoHaHS Documentation integrity in electronic health records. Published 2016. Accessed November 18, 2017.
- 8.Silverstone DE, Lim MC; American Academy of Ophthalmology Medical Information Technology Committee . Ensuring information integrity in the electronic health record: the crisis and the challenge. Ophthalmology. 2014;121(2):435-437. [DOI] [PubMed] [Google Scholar]
- 9.Jamoom EW, Yang N, Hing E. Adoption of certified electronic health record systems and electronic information sharing in physician offices: United States, 2013 and 2014. NCHS Data Brief. 2016;(236):1-8. [PubMed] [Google Scholar]
- 10.Grinspan ZM, Banerjee S, Kaushal R, Kern LM. Physician specialty and variations in adoption of electronic health records. Appl Clin Inform. 2013;4(2):225-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim MC, Patel RP, Lee VS, Weeks PD, Barber MK, Watnik MR. The long-term financial and clinical impact of an electronic health record on an academic ophthalmology practice. J Ophthalmol. 2015;2015:329819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh RP, Bedi R, Li A, et al. The practice impact of electronic health record system implementation within a large multispecialty ophthalmic practice. JAMA Ophthalmol. 2015;133(6):668-674. [DOI] [PubMed] [Google Scholar]
- 13.Levinson DR. Coding trends of medicare evaluation and management services. https://oig.hhs.gov/oei/reports/oei-04-10-00180.pdf. Accessed May 23, 2017.
- 14.Chiang MF, Read-Brown S, Tu DC, et al. Evaluation of electronic health record implementation in ophthalmology at an academic medical center (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2013;111:70-92. [PMC free article] [PubMed] [Google Scholar]
- 15.Lam JG, Lee BS, Chen PP. The effect of electronic health records adoption on patient visit volume at an academic ophthalmology department. BMC Health Serv Res. 2016;16:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weeks DL, Keeney BJ, Evans PC, Moore QD, Conrad DA. Provider perceptions of the electronic health record incentive programs: a survey of eligible professionals who have and have not attested to meaningful use. J Gen Intern Med. 2015;30(1):123-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hirschtick RE. A piece of my mind: John Lennon’s elbow. JAMA. 2012;308(5):463-464. [DOI] [PubMed] [Google Scholar]
- 18.Tsou AY, Lehmann CU, Michel J, Solomon R, Possanza L, Gandhi T. Safe practices for copy and paste in the ehr. systematic review, recommendations, and novel model for health IT collaboration. Appl Clin Inform. 2017;8(1):12-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arrowood D, Choate E, Curtis E, et al. Integrity of the healthcare record. Best practices for EHR documentation. J AHIMA. 2013;84(8):58-62. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Electronic Health Record (EHR) Survey 2016
eTable. The Top Electronic Health Record (EHR) and Image Management Systems Used by Respondents in This Survey by Frequency.
eFigure. Computerization of Clinical Information Systems in the 2011 Ophthalmology EHR Survey (Left) and in the 2016 Survey (Right).