Key Points
Question
What is the association between growth in Medicare expenditures and decreased mortality between January 1, 1999, and June 30, 2014?
Findings
In this cross-sectional analysis study of Medicare beneficiaries with acute myocardial infarction, reductions in mortality varied by hospital and were associated with diffusion of cost-effective care, such as early percutaneous coronary interventions, rather than overall spending.
Meaning
Increased adoption of cost-effective care at the hospital level could improve patient outcomes and, if accompanied by cuts in cost-ineffective care (whether in the acute care or postacute care setting), may also reduce expenditures.
Abstract
Importance
Many studies have considered the association between Medicare spending and health outcomes at a point in time; few have considered the association between the long-term growth in spending and outcomes.
Objective
To assess whether components of growth in Medicare expenditures are associated with mortality rates between January 1, 1999, and June 30, 2014, for beneficiaries hospitalized for acute myocardial infarction.
Design, Setting, and Participants
Cross-sectional analysis of a random 20% sample of fee-for-service Medicare beneficiaries from January 1, 1999, through December 31, 2000 (n=72 473) and January 1, 2004, through December 31, 2004 (n=38 248), and 100% sample from January 1, 2008, through December 31, 2008 (n=159 558) and January 1, 2013, through June 30, 2014 (n=209 614) admitted with acute myocardial infarction to 1220 hospitals.
Main Outcomes and Measures
Primary exposure measures include the growth of 180-day expenditure components (eg, inpatient, physician, and postacute care) and early percutaneous coronary intervention by hospitals adjusted for price differences and inflation. The primary outcome is the risk-adjusted 180-day case fatality rate.
Results
Patients in each of the years 2004, 2008, and 2013-2014 (relative to those in 1999-2000) were qualitatively of equivalent age, less likely to be white or female, and more likely to be diabetic (all P < .001). Adjusted expenditures per patient increased 13.9% from January 1, 1999, through December 31, 2000, and January 1, 2013, through June 30, 2014, but declined 0.5% between 2008 and 2013-2014. Mean (SD) expenditures in the 5.0% of hospitals (n = 61) with the most rapid expenditure growth between 1999-2000 and 2013-2014 increased by 44.1% ($12 828 [$2315]); for the 5.0% of hospitals with the slowest expenditure growth (n = 61), mean expenditures decreased by 18.7% (−$7384 [$4141]; 95% CI, $8177-$6496). The growth in early percutaneous coronary intervention exhibited a negative association with 180-day case fatality. Spending on cardiac procedures was positively associated with 180-day mortality, while postacute care spending exhibited moderate cost-effectiveness ($455 000 per life saved after 180 days; 95% CI, $323 000-$833 000). Beyond spending on noncardiac procedures, growth in other components of spending was not associated with health improvements.
Conclusions and Relevance
Health improvements for patients with acute myocardial infarction varied across hospitals and were associated with the diffusion of cost-effective care, such as early percutaneous coronary intervention and, to a lesser extent, postacute care, rather than overall expenditure growth. Interventions designed to promote hospital adoption of cost-effective care could improve patient outcomes and, if accompanied by cuts in cost-ineffective care (inside and outside of the hospital setting), also reduce expenditures.
This study examines whether growth in Medicare expenditures is associated with mortality rates for Medicare beneficiaries with acute myocardial infarction.
Introduction
With potential cuts in federal support for health insurance, the question of how these spending reductions might adversely affect population health is of particular importance. There is little agreement regarding the association between health care expenditures and outcomes, with estimates ranging from large and positive to 0 or negative. Although it is well understood that not all spending is cost-effective, nearly all studies have summarized the multidimensional components of patient care by a single dollar measure—total expenditures—rather than considering how the money is spent (ie, for cost-effective or ineffective services).
To address these knowledge gaps, we use a large longitudinal patient-level database from the Medicare fee-for-service population of elderly patients admitted to the hospital for acute myocardial infarction (AMI) between January 1, 1999, and June 30, 2014. Based on previous evidence documenting differential rates of spending growth across the United States, we hypothesized that hospitals have experienced different patterns of growth (or even decline) in treatment intensity for patients with AMI, with some hospitals investing most heavily in postacute care and others focusing on increasing the use of early percutaneous coronary interventions (PCIs), other cardiac procedures, imaging, or physician services.
We further hypothesized that risk- and inflation-adjusted growth in total Medicare spending is not the most important determinant of overall health outcomes, but that the components of spending growth, whether on cost-effective or cost-ineffective services, should have a greater impact on health outcomes. We therefore consider, separately, the association between the change in health outcomes from 1999 through 2014 and the diffusion of several treatment modalities during the same period, including those previously found to be cost-effective (ie, early PCI) and those less supported by evidence, such as testing and imaging, physician visits, cardiac and noncardiac procedures, outpatient care, and postacute care (including skilled nursing facilities, home health agencies, hospice, and durable medical equipment).
Methods
This study was approved by the Dartmouth institutional review board. Given the retrospective nature of this study, participant informed consent was not required.
Data
We used a random 20% sample of Medicare beneficiaries for 1999, 2000, and 2004, and a 100% sample for 2008, 2013, and 2014 (through June 30, 2014). To increase statistical power in smaller hospitals, we combined 2 years of data for both January 1, 1999, through December 31, 2000, and January 1, 2013, through June 30, 2014, when calculating changes. Eligible patients were fee-for-service Medicare enrollees with the primary diagnosis of AMI based on appropriate diagnosis codes from the International Classification of Diseases, Ninth Revision (410.xx [except 410.x2]), during each year.
The sample included those (1) enrolled in Medicare (Part A and Part B, as identified through the Medicare denominator file) for the entire year beyond their index admission (or until the month of their death), (2) aged at least 65 years at the time of their index admission, and (3) enrolled in a non–health maintenance organization plan for at least 1 month during each of the 12-month periods. Data from the Medicare provider analysis and review files were linked to other files (carrier file, home health agency, durable medical equipment, outpatient, and hospice) containing claims that represented services associated with the patient’s index admission and subsequent services (and expenditures) for a 180-day period following admission. Outpatient claims include bills from rehabilitation facilities, hospital outpatient departments, and other institutional outpatient health care providers.
We excluded patients admitted to a non–acute care hospital with a primary diagnosis of AMI, those transferred to an acute care hospital with a primary diagnosis other than AMI, and those discharged alive and not transferred with a total length of stay of 1 day or less. We defined a transfer as occurring if the date of discharge was the same as the date of admission between 2 mutually exclusive hospitals. The total length of stay for the index admission was defined from the date of admission to discharge, including any transfers.
Primary Outcome
The primary outcome measure is the risk-adjusted 180-day case fatality (or mortality) rate. In the sensitivity analysis, we also considered the risk-adjusted 30-day and 31- to 180-day (conditional on surviving 30 days) case fatality rates.
Calculation of Exposure Variables
We report price-standardized Medicare payments for the index admission and postindex utilization up to 180 days following the initial admission date. Standardized payments adjust for differences across regions in Medicare reimbursement rates for services attributed to costs of living, graduate medical education, and disproportionate-share hospital payments. Annual spending is converted to 2014 dollars after adjustment for general inflation, using the chain-weighted gross domestic product price deflator. Spending measures calculated at 180 days were conditional on survival to 180 days.
Hospital Payments
Hospital payments included those associated with the acute index hospitalization (diagnosis related group payment plus outlier payments when present) and other hospitalizations occurring within 180 days of the initial admission date. Expenditures included actual payments to health care professionals, absent amounts billed to patients or their supplemental insurance policies.
Physician Payments and Utilization
We provide utilization and payments for physician services based on Current Procedural Terminology and Berenson-Eggers Type of Service (BETOS) codes. Through these codes, we identified utilization of PCI and coronary artery bypass grafting (CABG) surgery. The BETOS codes create clinically relevant service categories for analyzing payments (eg, testing and imaging, physician visits, and cardiac and noncardiac procedures).
Other Expenditures After the Index Hospitalization
We included expenditures for skilled nursing facilities, outpatient services, home health agencies, hospice, and durable medical equipment.
Statistical Analysis
The analysis was performed at the individual patient level for 1999, 2000, 2004, 2008, 2013, and 2014. Logistic regressions, restricted to hospitals appearing in all years and treating at least 10 patients hospitalized with AMI per year, were used to estimate the models, with marginal probability estimates (using the “margin dydx(), atmeans” command in Stata version 14.0 Statistical Software [StataCorp LP]) reported in the tables and with standard errors clustered at the hospital referral region level appearing in parentheses (using the “cluster(hrr)” command in Stata version 14.0).
We used 2 types of exposure measures, calculated at the hospital level. Our first exposure was based on overall 180-day price- and inflation-adjusted expenditures dollar levels. Given that marginal health benefits may vary according to how money is spent, we further stratified spending into 6 categories: (1) testing and imaging, (2) physician visits, (3) cardiac procedures, (4) other procedures, (5) hospital care based on Medicare Part A spending, and (6) postacute care (with further breakdown into skilled nursing facility, home health, hospice, and durable medical equipment). Components of physician spending were categorized using BETOS codes.
The second exposure focused on utilization for a highly effective AMI treatment: the share of patients receiving PCI on the first day of the index hospitalizations for AMI (early PCI). To understand whether PCI substituted for other types of services, we also assessed whether changes in early PCI rates were associated with changes in 180-day spending and 180-day CABG surgery.
To account for differences across patients (and over time) in underlying health status, we adjusted for the beneficiary’s age, sex, race/ethnicity, and Charlson comorbidity index (presence of vascular disease, pulmonary disease, asthma, dementia, diabetes mellitus, liver and renal disorders, and cancer). To adjust further for potential confounding, we measured hospital-level exposure rates for those surviving the entire 180 days after index hospitalization.
We included hospital-level categorical variables to adjust for unmeasured differences in health status across hospitals that may otherwise bias our results. We included categorical variables for the admission year, to adjust for general trends and other unobservable confounding factors that evolve over time. Statistical analyses were performed using Stata version 14 and SAS version 9.4 (SAS Institute Inc) statistical software.
We additionally tested interaction terms for quartiles of AMI volume and early PCI utilization rates, and additionally by ST–elevation myocardial infarction (STEMI) vs non–ST–elevation myocardial infarction (NSTEMI) (eTable 1 in the Supplement). We also conducted sensitivity analyses (eAppendix in the Supplement).
Results
We identified 479 893 Medicare beneficiaries who were hospitalized for an AMI (72 473 from the 20% sample of enrollees in 1999-2000, 38 248 from the 20% sample of enrollees in 2004, and 159 558 and 209 614 from the 100% samples in 2008 and 2013-2014, respectively).
As shown in Table 1, patients with AMI in 2004, 2008, and 2013-2014 (relative to those in 1999-2000) were qualitatively of equivalent older age (eg, >85%: 0.22 in 2004, 0.26 in 2008, 0.25 in 2013-2014 vs 0.20 in 1999-2000), less likely to be white (0.90, 0.89, 0.87 vs 0.91) or female (0.50, 0.49, 0.47 vs 0.50), and more likely to be diabetic (0.31, 0.32, 0.35 vs 0.30 [all P < .001]).
Table 1. Characteristics of Patients and Care Provided to Medicare Beneficiaries Admitted for Acute Myocardial Infarctions, 1999-2014a.
| Characteristics | Proportion, Mean (SE) | |||
|---|---|---|---|---|
| 1999-2000 (20% Sample) (72 473) |
2004 (20% Sample) (38 248) |
2008 (100% Sample) (159 558) |
2013-2014 (100% Sample) (209 614) |
|
| Demographic | ||||
| Age groups, y | ||||
| 65-74 | 0.38 (0.49) | 0.36 (0.48) | 0.36 (0.48) | 0.40 (0.49) |
| 75-84 | 0.42 (0.49) | 0.41 (0.49) | 0.39 (0.49) | 0.36 (0.48) |
| ≥85 | 0.20 (0.40) | 0.22 (0.42) | 0.26 (0.44) | 0.25 (0.43) |
| Race | ||||
| White | 0.91 (0.29) | 0.90 (0.30) | 0.89 (0.31) | 0.87 (0.33) |
| Black | 0.06 (0.25) | 0.07 (0.26) | 0.07 (0.26) | 0.08 (0.27) |
| Other | 0.03 (0.68) | 0.03 (0.17) | 0.03 (0.18) | 0.05 (0.21) |
| Female | 0.50 (0.50) | 0.50 (0.50) | 0.49 (0.50) | 0.47 (0.50) |
| Comorbid conditions | ||||
| Ischemic heart disease | 0.45 (0.50) | 0.48 (0.50) | 0.42 (0.49) | 0.43 (0.50) |
| Peripheral vascular disease | 0.12 (0.32) | 0.13 (0.33) | 0.12 (0.33) | 0.11 (0.32) |
| Cerebrovascular disease | 0.12 (0.32) | 0.11 (0.31) | 0.11 (0.31) | 0.10 (0.30) |
| Diabetes | 0.30 (0.46) | 0.31 (0.46) | 0.32 (0.47) | 0.35 (0.48) |
| Mortality, d | ||||
| 30 and 31-180 | 0.27 (0.44) | 0.25 (0.44) | 0.24 (0.43) | 0.22 (0.41) |
| 30 | 0.17 (0.38) | 0.15 (0.36) | 0.14 (0.35) | 0.12 (0.33) |
| 31-180b | 0.11 (0.32) | 0.12 (0.33) | 0.12 (0.32) | 0.10 (0.31) |
International Classification of Diseases, Ninth Revision codes are as follows: ischemic heart disease (428), peripheral vascular disease (440-448), cerebrovascular disease (430-438), and diabetes (250).
The 31- to 180-day rate is conditional on surviving the first 30 days.
Decline in Overall 180-Day Case Fatality
Overall, 180-day case fatality rates per patient with AMI declined from 26.9% in 1999-2000 to 21.5% in 2013-2014, with most of the decline attributed to the 30-day period. The rate for days 31 to 180 (among patients surviving for 30 days after an AMI) was relatively unchanged from 1999-2000 to 2013-2014.
Growth in Total 180-Day Medicare Expenditures
Overall inflation- and risk-adjusted 180-day mean expenditures per patient increased by 13.9% ($4486) between 1999-2000 and 2013-2014 (Table 2). All of the increase occurred by 2008, 14.5% ($4654), with a 0.5% decline in risk- and inflation-adjusted spending between 2008 and 2013-2014. Total spending grew 6.1% up to 30 days beyond the index admission, and 31.0% from 31 to 365 days beyond the index admission. There was considerable heterogeneity in 180-day growth rates across hospitals. Spending in the 61 hospitals (or 5% of all hospitals) with the slowest expenditure growth decreased 18.7% (−$7384; 95% CI, −$8177 to −$6496), while spending in the 61 hospitals with fastest expenditure growth grew increased 44.1% ($12 828; 95% CI, $12 084 to $13 890).
Table 2. Total and Component Spending and Utilization Among Medicare Beneficiaries Admitted for Acute Myocardial Infarctions, 1999-2014a.
| Spending or Utilization | Mean (SD) | Change, % | ||||
|---|---|---|---|---|---|---|
| 1999-2000 (n = 72 473) | 2004 (n = 38 248) | 2008 (n = 159 558) | 2013-2014 (n = 209 614) | |||
| 2008 to 2013-2014 | 1999-2000 to 2013-2014 | |||||
| Spending, $ | ||||||
| Total spending, 180 d | 32 182 (25 503) | 31 439 (33 007) | 36 836 (33 058) | 36 668 (33 665) | −0.5 | 13.9 |
| Index admission | 20 327 (16 598) | 19 182 (22 556) | 21 104 (20 941) | 20 747 (20 879) | −1.7 | 2.1 |
| Up to 30 d After index admission | 22 082 (14 902) | 21 097 (21 228) | 23 450 (17 644) | 23 430 (18 982) | −0.1 | 6.1 |
| 31-180 d After index admission | 10 101 (17 726) | 10 343 (19 452) | 13 386 (23 298) | 13 237 (22 880) | −1.1 | 31 |
| Components of spending | ||||||
| Inpatient services | 23 734 (19 621) | 22 515 (20 928) | 25 140 (25 986) | 24 151 (25 871) | −3.9 | 1.8 |
| Skilled nursing facility | 1545 (4514) | 2016 (5166) | 3080 (7542) | 3127 (7921) | 1.5 | 102.4 |
| Physician payment | 5304 (5064) | 4606 (19 297) | 5165 (4750) | 5041 (4889) | −2.4 | −5.0 |
| Outpatient services | 673 (1863) | 992 (2468) | 1500 (3467) | 2491 (5032) | 66.1 | 270.1 |
| Home health, hospice, or DME | 998 (2536) | 1380 (2862) | 2058 (4131) | 2002 (3999) | −2.7 | 100.6 |
| Procedures by BETOS codeb | ||||||
| Cardiac | 1867 (2567) | 1677 (7686) | 2002 (3489) | 2551 (4996) | 27.4 | 36.6 |
| Noncardiac | 631 (1544) | 769 (7374) | 917 (2209) | 1141 (3115) | 24.4 | 80.8 |
| Testing and imaging | 1220 (1694) | 1398 (1472) | 1647 (1748) | 1444 (1720) | −12.3 | 18.4 |
| Office visits | 775 (881) | 668 (579) | 812 (674) | 812 (943) | 0 | 4.8 |
| Emergency department | 184 (238) | 186 (218) | 250 (330) | 311 (476) | 24.4 | 69 |
| Hospital visit | 1319 (1917) | 1145 (1616) | 1402 (2045) | 1666 (2355) | 18.8 | 26.3 |
| Utilization rates, No. | ||||||
| Any PCI | 0.309 (0.462) | 0.385 (0.487) | 0.401 (0.490) | 0.460 (0.498) | 14.7 | 48.9 |
| Early PCIc | 0.173 (0.379) | 0.258 (0.438) | 0.294 (0.456) | 0.351 (0.477) | 19.4 | 102.9 |
| CABG, 180 d | 0.167 (0.373) | 0.133 (0.339) | 0.114 (0.318) | 0.108 (0.310) | −5.3 | −35.3 |
| Length of stay, median (IQR), d | 6.00 (4 to 11) | 5.00 (3 to 11) | 5.00 (3 to 11) | 4.00 (2 to 9) | −20.0 | −33.3 |
Abbreviations: BETOS, Berenson-Eggers Type of Service codes; CABG, coronary artery bypass grafting; DME, durable medical equipment; IQR, interquartile range; PCI, percutaneous coronary intervention.
Spending in 2014 dollars.
Physician and outpatient spending.
Early PCI occurs on the same day as the admission.
Spending on inpatient services per beneficiary grew by just $417 (1.8%) between 1999-2000 and 2013-2014, and median length of stay decreased by 2 days during the same period (P < .001). During this same period, physician and outpatient spending increased by $1582 (outpatient spending increased by $1818 per beneficiary); 44% of the change in physician and outpatient spending was associated with cardiac procedures(change in spending for cardiac procedures/change in physician and outpatient spending, $684), while hospital visits accounted for an additional 22% of spending (change in mean spending for hospital visits/change in physician and outpatient spending, $347).
Growth in PCI Rates and Decline in CABG Rates
Utilization of PCI through 180 days increased by 48.9% between 1999-2000 and 2013-2014 (mean, 0.309 vs 0.460, respectively), while early (same day as admission) PCI utilization increased by 102.9% (mean, 0.173 vs 0.351, respectively). Only 1.7% of patients with AMI were treated in hospital-years in which no other patient at the hospital received early PCI. Between 1999-2000 and 2013-201414, 180-day CABG rates decreased by 35.3% (mean, 0.167 vs 0.108, respectively). This latter finding may be explained by the fact that we restricted to hospitals with at least 11 patients with AMI every year.
We investigated whether hospitals that increased their early PCI use simultaneously decreased their use of other services. Changes in 180-day CABG rates were only weakly correlated with changes in early (r = −0.099) or 180-day (r = −0.164) PCI rates. We further decomposed the type of postacute care spending associated with growth in early PCI. We found that hospitals that increased their use of early PCI the most (ie, fourth quartile), relative to the lowest growth quartile, had lower 180-day per-beneficiary mean spending for skilled nursing facilities (−$700) as well as home health agency, hospice, and durable medical equipment (−$298)( eTable 2 in the Supplement).
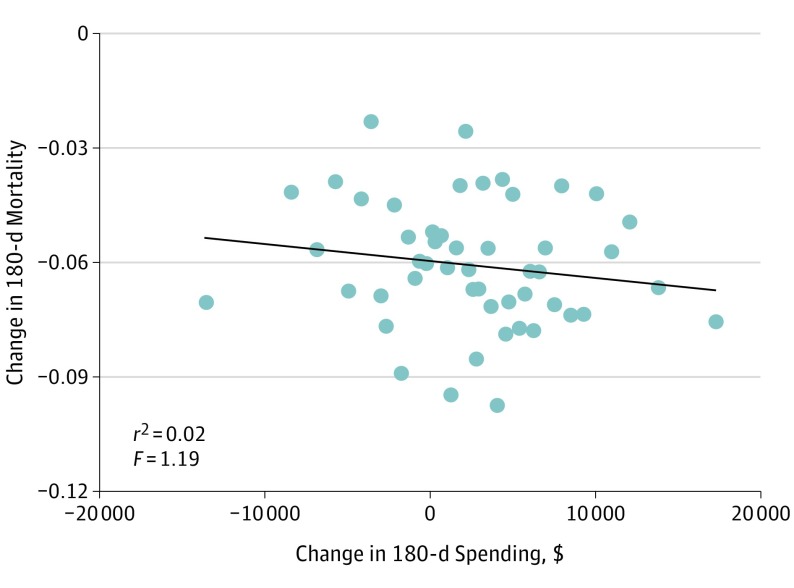
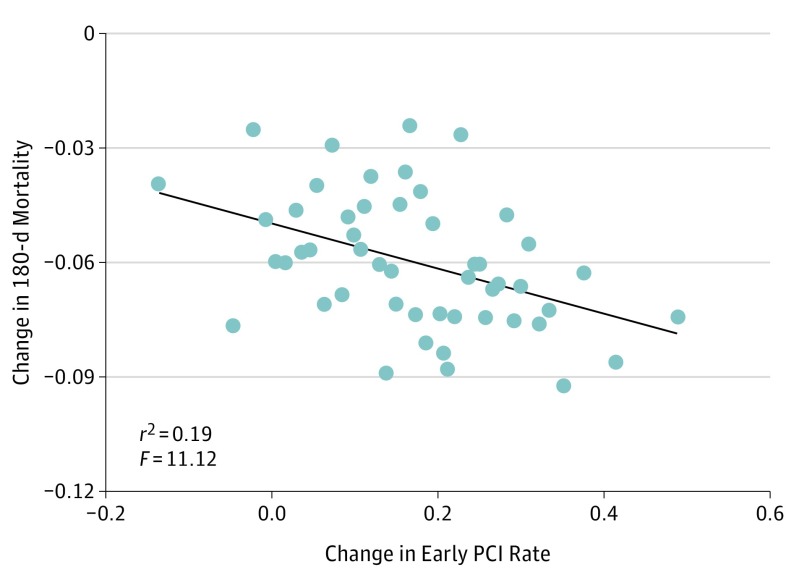
Association Between Health Care Spending and Case Fatality Rates
Changes in 180-day spending were weakly associated with risk-adjusted case fatality, using either bivariate correlations at the hospital level (Figure 1) or multivariate regression analysis at the patient level (Table 3). However, changes in early PCI were strongly and inversely associated with 180-day case fatality (Figure 2). In multivariable analysis controlling for other measures of 180-day spending, early PCI rates were inversely associated with 180-day mortality (β = −0.079, P < .001) (Table 3). This finding was stronger among patients with STEMI (β = −0.172, P < .001) relative to those with NSTEMI (β = −0.0912, P < .001), and persisted even after controlling for CABG utilization (β = −0.078, P < .001) and other spending components (β = −0.078, P < .001) (eTable 3 in the Supplement). We found a significant interaction between quartiles of AMI volume and early PCI rates on 180-day mortality, whereby the greatest reductions in mortality attributed to early PCI were among those hospitals with the highest average AMI volume. This volume effect occurred solely among patients with NSTEMI (P = .008) (eTable 4 in the Supplement).
Figure 1. Change in 180-Day Risk-Adjusted Case Fatality vs Change in 180-Day Spending for 2013-2014 vs 1999-2000.
Changes in hospital rates of early percutaneous coronary interventions, performed within a day of admission. Solid line represents fitted values.
Table 3. Association of Early PCI and Hospital Spending on 180-Day Acute Myocardial Infractions Mortality Ratesa,b.
| Early PCI or Spending | Model 1, Full Sample (n=479 873)c | Model 2, Full Sample (n=479 873)d | Model 3, NSTEMI (n=331 635)c | Model 4, NSTEMI (n=331 635)d | Model 5, STEMI (n=148 077)c | Model 6, STEMI (n=148 077)d |
|---|---|---|---|---|---|---|
| Early PCI rate, No. | ||||||
| β (SE) | −0.068 (0.0094)e | −0.079 (0.0094)e | −0.080 (0.012)e | −0.0917 (0.0122)e | −0.155 (0.010)e | −0.172 (0.0099)e |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
| With $1000 increase in total spending | ||||||
| 180-d Mortality | ||||||
| β (SE) | −0.0002 (0.0001) | −0.0002 (0.0001) | −0.0002 (0.0001) | |||
| P value | .04 | .12 | .10 | |||
| 180-d Testing | ||||||
| β (SE) | −0.0041 (0.0027) | 0.0027 (0.0028) | 0.0053 (0.0027) | |||
| P value | .13 | .34 | .05 | |||
| 180-d Visits | ||||||
| β (SE) | −0.0043 (0.0023) | −0.0061 (0.0023) | −0.0062 (0.0028) | |||
| P value | .06 | .01 | .03 | |||
| 180-d Cardiac procedures | ||||||
| β (SE) | 0.0042 (0.0016)e | 0.0049 (0.0017)e | 0.0042 (0.0014)e | |||
| P value | .01 | .003 | .002 | |||
| 180-d Other procedures | ||||||
| β (SE) | −0.0042 (0.0017) | −0.0050 (0.0019) | −0.0050 (0.0016)e | |||
| P value | .02 | .01 | .002 | |||
| 180-d Part A | ||||||
| β (SE) | 0.0002 (0.0003) | 0.0002 (0.0003) | 0.0006 (0.0003) | |||
| P value | .40 | .50 | .04 | |||
| 180-d Postacute care | ||||||
| β (SE) | −0.0022 (0.0005)e | −0.0016 (0.0005)e | −0.0042 (0.0006)e | |||
| P value | <.001 | .003 | <.001 |
Abbreviations: NSTEMI, non-ST–elevation myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction.
Sample includes patients who visited hospitals that appeared in the data in all years and that treated at least 10 patients with acute myocardial infarction per year.
Logit model estimated; marginal effects reported using “margins, dydx() atmeans” in Stata. All regressions control for patient characteristics, hospital fixed effects, and year fixed effects. All spending measures are calculated for each hospital-year using patients who live 6 months. Includes years 1999, 2000, 2004, 2008, 2013, and quarters 1 and 2 of 2014. Standard errors are clustered at the hospital level.
P < .025 for 5% significance level using Bonferroni correction; P < .005 for 1% significance level using Bonferroni correction.
P < .0071 for 5% significance level using Bonferroni correction; P < .0014 for 1% significance level using Bonferroni correction.
Statistical significance after conducting the Bonferroni correction.
Figure 2. Change in 180-Day Risk-Adjusted Case Fatality vs Change in Early PCI Utilization for 2013-2014 vs 1999-2000.
Changes in 180-day risk-adjusted case fatality by hospital rates of early percutaneous coronary interventions performed within a day of admission. Solid line represents fitted values; PCI, percutaneous coronary intervention.
Increases in 180-day case fatality rate were associated positively with cardiac procedure spending (β = 0.004, P = .007), and negatively with postacute care (β = −0.002, P < .001), the latter of which translates to a cost-effectiveness ratio of $455 000 per life saved (95% CI, $323 000-$833 000) (Table 3). In a sensitivity analysis that examined the composition of postacute care spending (eTable 3 in the Supplement), only spending on skilled nursing facilities and early PCI rates exhibited significant negative associations with case fatality rates (P < .001). After holding early PCI rates constant, no other component of spending had a statistically significant association with 180-day fatality, including spending on physician visits.
Discussion
Overall inflation- and risk-adjusted 180-day expenditures per patient with AMI have increased by 14.4% since 1999-2000, yet this growth masks substantial variation in hospital spending growth. For example, the top 5.0% of hospitals in terms of growth rates (61 hospitals) averaged 44.1% increased growth rate during this period, while the bottom 5.0% of hospitals with the slowest expenditure growth decreased spending by 18.7%. Nonetheless, hospitals with more rapid increases in spending did not experience larger case fatality rate declines.
Spending growth occurred principally during 31 to 180 days following admission, with a doubling of nursing home and home health care expenditures. Beyond growth in postacute spending, outpatient services tripled, contributing importantly to 180-day spending increases. While use of noninvasive procedures by cardiologists grew between 1998 and 2008, our present data suggest imaging and testing modestly increased, accounting for 14.4% of overall physician and outpatient spending growth.
The estimated association of early PCI with case fatality is large, statistically significant, and robust, with larger effects among patients with STEMI. Use of PCI is indicated for treating patients with a number of conditions (including STEMI), and as an early invasive strategy for NSTEMI (eTable 1 in the Supplement). Aasa et al found early PCI costs for STEMI to be nonsignificantly different relative to thrombolytic therapy (PCI, $25 315 vs thrombolytic therapy, $27 819), a result consistent with our data. Our estimated coefficients imply case fatality effects that are larger than trial reports, which may be explained if diffusion of early PCI was also associated with other improvements (eg, quicker door-to-balloon time). We found no evidence that hospitals scaling back on CABG surgery increased early PCI use.
We previously argued that when different components of health care spending exhibit higher or lower cost-effectiveness, total expenditures and growth are poor predictors of overall health benefits. Our results are consistent with this hypothesis. Factors leading to improved outcomes have little impact on spending, while the factors leading to the highest impact on spending have a modest impact on health outcomes. Postacute care, specifically, nursing home care, which grew rapidly, offered a cost-effectiveness of $455 000 per additional life saved at 180 days. Unlike previous studies that did not find reduced case fatality attributed to postacute care, we consider only patients with AMI, and for these patients cardiac rehabilitation has previously been associated with a 20% reduction in all-cause mortality and a cost-effectiveness of $8691 (in 2014 dollars) per year of life saved.
Our results may inform several policy debates. First, we have established that the decline and plateau in Medicare expenditures observed by Krumholz et al can also be found in disease-specific cohorts, in which the secular trends are not likely to be the consequence of healthier populations. Albeit focusing on the role of income on AMI mortality and hospitalizations, Spatz et al reported declines in AMI mortality among Medicare beneficiaries (irrespective of income level) over a 15-year period. Yet, this moderation in spending observed for patients with AMI masks substantial and continued hospital variability with regard to growth or declines in overall spending, suggesting that local factors and not just national policy changes continue to be important components of expenditure growth.
Second, policy makers seek to use bundled payments to incentivize coordination over care episodes, reduce spending, and maintain (or improve) quality. Prior work has highlighted postacute spending as a potential target for bundled payment programs. We found that spending was fairly well contained within 30 days after admission (6.1% inflation-adjusted increase in spending). The fixed diagnosis related group payment has likely contributed to reducing the length of stay by 2 days on average since 1999-2000. Most of the variation (in growth rates and variation therein) appears after 30 days. Given this finding, bundling payments to include services occurring beyond 30 days could further moderate expenditure growth.
Limitations
Our study has several limitations. First, our study was limited to fee-for-service Medicare beneficiaries. While an increasing portion of Medicare beneficiaries are covered by private plans, the majority remain covered through a traditional fee-for-service plan. Second, investigators have identified other factors that may influence 180-day case fatality rates, including evidence-based medical therapies and changes over time in socioeconomic status; however, previous work suggests modest effects of socioeconomic status once other measures of health status are controlled for. Third, we did not have a full accounting of all spending components (eg, pharmaceutical, supplemental insurance bills). Fourth, some potentially important components of spending were not accounted for in the present analysis (eg, pharmaceuticals). Fifth, while postacute care spending beyond 30 days may not be directly managed by the index hospital, there is increased awareness and management of postacute care by health systems attributed in part to further dissemination of Accountable Care Organizations and bundled payment programs. Sixth, we cannot rule out temporal differences in NSTEMI diagnosis attributed to the rapid diffusion of cardiac biomarkers during this period. Another limitation is a focus on mortality only rather than quality of life, a measure that is unfortunately beyond the scope of our nationally representative Medicare claims data.
Conclusions
While minimal hospital variation existed in spending within the traditional 30-day episode-based reimbursement window, large variation in growth rates and treatment diffusion existed between 31 and 180 days beyond the index admission. Hospitals that increased early PCI use experienced improvements in health outcomes but did not experience large overall cost increases. Policies encouraging hospitals to adopt early PCI, while supporting hospital-based and non–hospital-based reductions in spending on less cost-effective services (perhaps through newly designed bundled payment programs), may help improve patient outcomes without increasing costs.
eAppendix. Sensitivity Analysis
eTable 1. Association Between Early Percutaneous Coronary Intervention and 180-day Acute Myocardial Infarction Mortality, Stratified By Type of Acute Myocardial Infarction
eTable 2. Components of Spending Across Quartiles of Hospital Early Percutaneous Coronary Intervention Change, 1999-2014
eTable 3. Association Between Early Percutaneous Coronary Intervention and 180-day Acute Myocardial Infarction Mortality
eTable 4. The Return to Early PCI in High vs Low Volume Hospitals
References
- 1.Baicker K, Chandra A. Medicare spending, the physician workforce, and beneficiaries’ quality of care. Health Aff (Millwood). 2004;(suppl web exclusives):W4-184-97. [DOI] [PubMed] [Google Scholar]
- 2.Doyle JJ, Graves JA, Gruber J, Kleiner S. Measuring returns to hospital care: evidence from ambulance referral patterns. J Polit Econ. 2015;123(1):170-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Romley JA, Jena AB, Goldman DP. Hospital spending and inpatient mortality: evidence from California: an observational study. Ann Intern Med. 2011;154(3):160-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Likosky DS, Zhou W, Malenka DJ, Borden WB, Nallamothu BK, Skinner JS. Growth in medicare expenditures for patients with acute myocardial infarction: a comparison of 1998 through 1999 and 2008. JAMA Intern Med. 2013;173(22):2055-2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newhouse JP, Garber AM. Geographic variation in health care spending in the United States: insights from an institute of medicine report. JAMA. 2013;310(12):1227-1228. [DOI] [PubMed] [Google Scholar]
- 6.Rothberg MB, Cohen J, Lindenauer P, Maselli J, Auerbach A. Little evidence of correlation between growth in health care spending and reduced mortality. Health Aff (Millwood). 2010;29(8):1523-1531. [DOI] [PubMed] [Google Scholar]
- 7.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending, part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288-298. [DOI] [PubMed] [Google Scholar]
- 8.Fisher ES, Bynum JP, Skinner JS. Slowing the growth of health care costs—lessons from regional variation. N Engl J Med. 2009;360(9):849-852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krumholz HM, Nuti SV, Downing NS, Normand SL, Wang Y. Mortality, hospitalizations, and expenditures for the medicare population aged 65 years or older, 1999-2013. JAMA. 2015;314(4):355-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen DJ, Krumholz HM, Sukin CA, et al. ; Stent Restenosis Study Investigators . In-hospital and one-year economic outcomes after coronary stenting or balloon angioplasty: results from a randomized clinical trial. Circulation. 1995;92(9):2480-2487. [DOI] [PubMed] [Google Scholar]
- 11.Cohen DJ, Taira DA, Berezin R, et al. Cost-effectiveness of coronary stenting in acute myocardial infarction: results from the stent primary angioplasty in myocardial infarction (stent-PAMI) trial. Circulation. 2001;104(25):3039-3045. [DOI] [PubMed] [Google Scholar]
- 12.Doyle JJ Jr, Graves JA, Gruber J. Uncovering waste in US healthcare: Evidence from ambulance referral patterns. J Health Econ. 2017;54:25-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKnight R. Home care reimbursement, long-term care utilization, and health outcomes. J Public Econ. 2006;90 (1-2):293-323. doi: 10.1016/j:pubeco.2004.11.006 [DOI] [Google Scholar]
- 14.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don’t drive regional Medicare spending variations. Health Aff (Millwood). 2010;29(3):537-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Medicare & Medicaid Services HCPCS release & code sets. https://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/index.html?redirect=/hcpcsreleasecodesets/20_betos.asp. Published 2017. Accessed October 23, 2017.
- 16.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending, part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273-287. [DOI] [PubMed] [Google Scholar]
- 17.Currie J, MacLeod WB, Van Parys J. Provider practice style and patient health outcomes: the case of heart attacks. J Health Econ. 2016;47:64-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228. [DOI] [PubMed] [Google Scholar]
- 19.O’Gara PT, Kushner FG, Ascheim DD, et al. ; American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions . 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78-e140. [DOI] [PubMed] [Google Scholar]
- 20.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. [DOI] [PubMed] [Google Scholar]
- 21.Skinner J. Causes and consequences of regional variation in health care In: Pauly M, Mcguire T, Barros P, eds. Handbook of Health Economics. Vol 2 Amsterdam, the Netherlands: Elsevier; 2012:45-94. [Google Scholar]
- 22.Finkelstein A, Gentzkow M, Williams H. Sources of geographic variation in health care: evidence from patient migration. Q J Econ. 2016;131(4):1681-1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andrus BW, Welch HG. Medicare services provided by cardiologists in the United States: 1999-2008. Circ Cardiovasc Qual Outcomes. 2012;5(1):31-36. [DOI] [PubMed] [Google Scholar]
- 24.Aasa M, Henriksson M, Dellborg M, et al. Cost and health outcome of primary percutaneous coronary intervention versus thrombolysis in acute ST-segment elevation myocardial infarction-results of the Swedish Early Decision reperfusion Study (SWEDES) trial. Am Heart J. 2010;160(2):322-328. [DOI] [PubMed] [Google Scholar]
- 25.Zijlstra F, Hoorntje JC, de Boer MJ, et al. Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction. N Engl J Med. 1999;341(19):1413-1419. [DOI] [PubMed] [Google Scholar]
- 26.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361(9351):13-20. [DOI] [PubMed] [Google Scholar]
- 27.Weinstein MC, Skinner JA. Comparative effectiveness and health care spending—implications for reform. N Engl J Med. 2010;362(5):460-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chandra A, Skinner JS. Technology growth and expenditure growth in health care. J Econ Lit. 2012;50(3):645-680. [Google Scholar]
- 29.Ades PA, Pashkow FJ, Nestor JR. Cost-effectiveness of cardiac rehabilitation after myocardial infarction. J Cardiopulm Rehabil. 1997;17(4):222-231. [DOI] [PubMed] [Google Scholar]
- 30.Shih T, Chen LM, Nallamothu BK. Will bundled payments change health care? examining the evidence thus far in cardiovascular care. Circulation. 2015;131(24):2151-2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chandra A, Dalton MA, Holmes J. Large increases in spending on postacute care in Medicare point to the potential for cost savings in these settings. Health Aff (Millwood). 2013;32(5):864-872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jacobson G, Casillas G, Damico A, Neuman T, Gold M.. Medicare Advantage 2016 Spotlight: Enrollment Market Update. Washington, DC: Kaiser Family Foundation; 2016. [Google Scholar]
- 33.Mukherjee D, Fang J, Chetcuti S, Moscucci M, Kline-Rogers E, Eagle KA. Impact of combination evidence-based medical therapy on mortality in patients with acute coronary syndromes. Circulation. 2004;109(6):745-749. [DOI] [PubMed] [Google Scholar]
- 34.Spatz ES, Beckman AL, Wang Y, Desai NR, Krumholz HM. Geographic variation in trends and disparities in acute myocardial infarction hospitalization and mortality by income levels, 1999-2013. JAMA Cardiol. 2016;1(3):255-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Sensitivity Analysis
eTable 1. Association Between Early Percutaneous Coronary Intervention and 180-day Acute Myocardial Infarction Mortality, Stratified By Type of Acute Myocardial Infarction
eTable 2. Components of Spending Across Quartiles of Hospital Early Percutaneous Coronary Intervention Change, 1999-2014
eTable 3. Association Between Early Percutaneous Coronary Intervention and 180-day Acute Myocardial Infarction Mortality
eTable 4. The Return to Early PCI in High vs Low Volume Hospitals