Abstract
This study uses the Medicare Provider Analysis and Review file to examine whether coded severity of illness is associated with reduced rates of readmission after implementation of the Hospital Readmissions Reduction Program.
The Hospital Readmission Reduction Program (HRRP), established in 2010, placed significant financial penalties on hospitals with rates of readmission that were higher than expected for 3 targeted medical conditions. Under the program, a hospital’s readmission rate is adjusted based on patients’ coded severity of illness. Although these adjustments reflect an effort from the Centers for Medicare & Medicaid Services to avoid unfairly penalizing hospitals caring for patients with higher severity of illness, hospitals can improve their calculated rates of readmission by increasing their coded level of severity. It is unknown whether changes in coded severity of illness explain the previously described reductions in readmissions after implementation of the HRRP.
Methods
Data for this study came from discharges from the Medicare Provider Analysis and Review file between January 1, 2008, and November 30, 2014. The post-HRRP period included admissions on or after April 1, 2010. Readmissions were defined as any inpatient hospitalization within 30 days of discharge from the index hospitalization. The study sample included Medicare beneficiaries admitted for 1 of 3 targeted medical conditions (acute myocardial infarction, heart failure, or pneumonia) to acute care hospitals exposed to the HRRP and to critical access hospitals that were exempt from the HRRP (controls). We performed a difference-in-differences analysis to compare changes in 30-day rates of readmission between exposed and control hospitals. We estimated the following 2 episode-level logistic models: the first adjusted for admitting diagnosis, demographics (age, sex, race/ethnicity [white or nonwhite]), and season of admission; the second also adjusted for coded severity of illness based on comorbidities as described by Elixhauser et al. Both models used inclusion criteria from the Centers for Medicare & Medicaid Services to identify the eligible sample of index admissions.
Standard errors were calculated to be robust to hospital-level clustering. P < .05 (2-sided) was considered statistically significant. Analyses were performed using Stata, version 14 (Stata Corp).
Results
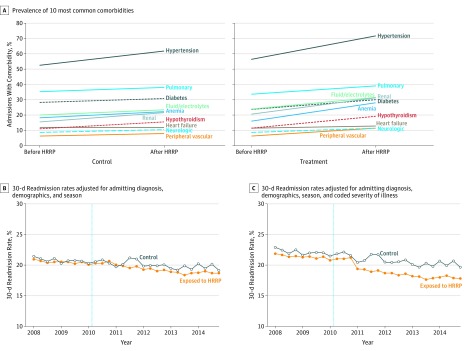
A total of 6 302 389 beneficiary episodes—spanning the interval between admission and 30 days after discharge—at 3259 HRRP-exposed hospitals and 1115 control hospitals were included. The mean number of comorbidities during index admissions as defined by Elixhauser et al per admission at control hospitals increased 19.6% (from 2.50 to 2.99) vs 38.8% (from 2.50 to 3.47) at hospitals exposed to the HRRP (Table). Exposed hospitals had larger increases in the frequency of coding each of the 10 most common comorbidities during the study period (Figure, A).
Table. Coded Risk and Readmissions Rates After the Hospital Readmission Reduction Program.
| Characteristic | Control Hospitals (n = 1115) | HRRP-Exposed Hospitals (n = 3259) | Difference-in-Differences Estimate, % (95% CI) | ||
|---|---|---|---|---|---|
| Pre-HRRP | Post-HRRP | Pre-HRRP | Post-HRRP | ||
| Outcome, No. (%) | |||||
| Acute myocardial infarction | 5919/127 200 (4.7) | 8882/208 589 (4.3) | 386 399/2 113 298 (18.3) | 740 908/3 853 302 (19.2) | NA |
| Chronic heart failure | 43 144/127 200 (33.9) | 68 331/208 589 (32.8) | 877 695/2 113 298 (41.5) | 1 588 481/3 853 302 (41.2) | NA |
| Pneumonia | 78 137/127 200 (61.4) | 131 376/208 589 (63.0) | 849 204/2 113 298 (40.2) | 1 523 913/3 853 302 (39.6) | NA |
| Comorbidity count per admission, meana | 2.50 | 2.99 | 2.50 | 3.47 | NA |
| Readmission rates, % | |||||
| Adjusted for admitting diagnosis, demographics, and season | 20.71 | 19.94 | 20.44 | 19.30 | −0.38 (−0.72 to −0.04) |
| Adjusted for admitting diagnosis, demographics, season, and coded severity | 21.97 | 20.60 | 21.24 | 18.83 | −1.03 (−1.39 to −0.68) |
Abbreviations: HRRP, Hospital Readmission Reduction Program; NA, not applicable.
As defined by Elixhauser et al.
Figure. Readmission Rates Before and After the Hospital Readmission Reduction Program (HRRP).
Anemia indicates deficiency anemia; diabetes, diabetes, uncomplicated; fluid/electrolytes, fluid and electrolyte disorders; heart failure, congestive heart failure; hypertension, hypertension, complicated and uncomplicated; neurologic, other neurologic disorders; peripheral vascular, peripheral vascular disorders; pulmonary, chronic pulmonary disease; and renal, renal failure.
Trends in rates of readmission were parallel between control and exposed hospitals before implementation of the HRRP (Figure, B and C). Rates of readmission adjusted for patient demographics, admitting diagnosis, and season decreased from 20.71% to 19.94% at control hospitals and 20.44% to 19.30% at HRRP-exposed hospitals, with a resultant difference-in-differences estimate of –0.38% (95% CI, –0.72% to –0.04%) (Table). After adjustment for severity of illness, the difference-in-differences estimate was –1.03% (95% CI, –1.39% to –0.68%). Sensitivity analysis using hierarchical condition categories to assess severity and using linear models with hospital fixed effects confirmed our results.
Discussion
Our findings raise concern that a substantial portion of estimated reductions in readmissions after implementation of the HRRP are the result of hospital documentation rather than underlying improvements in the delivery of care. A total of 63.1% of the reduction in the risk-adjusted rate of readmission after implementation of the HRRP was due to increases in coded severity ([–0.38% – (–1.03%)]/–1.03% = 63.1%). This finding is consistent with prior evidence that 40% of the reduction in risk-adjusted coronary artery bypass graft mortality rates after public reporting in New York State were the result of increases in coded severity of illness. Moreover, the finding extends concerns about other performance measures used by payers that are also influenced by coded severity of illness and exclusion criteria.
Our study is limited by administrative data that could not be used to determine the appropriateness of the increases in coding severity of illness. It is possible that hospitals exposed to the HRRP coded illnesses as less severe prior to implementation of the HRRP, rather than coding illnesses as more severe after implementation of the program. Regardless of whether changes in coded severity of illness appropriately reflect clinical risk, our study demonstrates that increases in coding were responsible for a large share of the observed reduction in risk-adjusted rates of readmission.
References
- 1.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543-1551. [DOI] [PubMed] [Google Scholar]
- 2.Desai NR, Ross JS, Kwon JY, et al. . Association Between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016;316(24):2647-2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services Measure methodology. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Accessed September 26, 2017.
- 5.Green J, Wintfeld N. Report cards on cardiac surgeons: assessing New York state’s approach. N Engl J Med. 1995;332(18):1229-1232. [DOI] [PubMed] [Google Scholar]
- 6.Sjoding MW, Iwashyna TJ, Dimick JB, Cooke CR. Gaming hospital-level pneumonia 30-day mortality and readmission measures by legitimate changes to diagnostic coding. Crit Care Med. 2015;43(5):989-995. [DOI] [PMC free article] [PubMed] [Google Scholar]